Abstract
Objectives.
This research analyzed the body mass index (BMI) level and rate of change, and their association with socioeconomic status among older Japanese adults.
Methods.
Data came from a national sample of over 4,800 Japanese adults aged 60 and older at baseline, with up to 7 repeated observations over a period of 19 years (1987–2006). Hierarchical linear modeling was used to analyze the intrapersonal and interpersonal differences in BMI.
Results.
Average BMI among older Japanese was 22.26 at baseline and decreased with an accelerating rate over time. Relative to those with less education, BMI among older Japanese with more education was lower and it declined linearly at a faster rate over time. In contrast, higher household income at baseline was associated with a higher level of BMI but similar rates of decline over time. Furthermore, we found no evidence for age variations in the SES–BMI linkage as predicted by prior investigators.
Discussion.
These findings provide new insights into the complex relationship between socioeconomic factors and BMI, and help to inform the design of health policies and interventions related to weight control among older adults with diverse socioeconomic backgrounds.
Key Words: Aging, Body mass index, Hierarchical linear modeling, Japan, Trajectory, Socioeconomic status.
Body mass index (BMI) is an important predictor of health outcomes, including all-cause mortality (Berrington de Gonzalez et al., 2010; Flegal, Kit, Orpana, & Graubard, 2013; Romero-Corral et al., 2006), cardiovascular mortality (Asia Pacific Cohort Studies Collaboration, 2004; Bogers et al., 2007), and health-care costs (Daviglus et al., 2004). Among older adults, although obesity (BMI ≥ 30) is positively associated with mortality, underweight (BMI < 18.5) is an even better predictor of an increased risk of dying (Flicker et al., 2010; Grabowski & Ellis, 2001). Additionally, given the compelling evidence that persons of lower socioeconomic status (SES) have worse health, understanding and alleviating SES-related health disparities have emerged as a key objective of public health research and policy (Adler & Newman, 2002; Robert & House, 2000). A better understanding of the level of BMI and its rate of change over time, and in particular how they are associated with SES, is necessary for assessing priorities related to weight control.
Research has been increasingly focused on how BMI changes over time among middle-aged and older adults. Among middle-aged Americans (51–61 at the baseline), BMI increased slightly over a period of 14 years, approximated by a quadric function (Botoseneanu & Liang, 2011, 2012), whereas among Americans aged 65 and over, BMI declined modestly over time (Kahng, Dunkle, & Jackson, 2004; Kuchibhatla, Fillenbaum, Kraus, Cohen, & Blazer, 2013). In addition, the trajectory of BMI is affected by individual SES, in that higher education and income are associated with lower levels of BMI (Botoseneanu & Liang, 2011; Kahng et al., 2004).
Concerning the linkage between SES and obesity, studies in many countries throughout the world indicate that a nation’s level of economic development may be an important moderator. While lower SES has been associated with obesity in highly developed countries, in middle- and low-income countries higher SES, particularly higher income, is associated with obesity (McLaren, 2007; Sobal & Stunkard, 1989). On the other hand, research on the relationship between SES and weight change over time is largely based on data from developed nations. Although higher education and occupation were inversely associated with weight gain, findings were less consistent when income was used as the measure for SES (Ball & Crawford, 2005).
Current research on BMI trajectories among older adults may be improved in at least two respects. First, the vast majority of research on BMI trajectories among older people is based on data derived from western developed nations, particularly the United States. In view of the substantial differences in social stratification, population health, health care, and life style between western and nonwestern societies, it is important to examine the trajectory of BMI and its socioeconomic determinants in nonwestern countries. Nonwestern countries may present socioeconomic conditions not observable in the United States, and thus the generalizability of findings from western countries needs to be evaluated by comparing the association between SES and BMI trajectories in western and nonwestern countries.
Japan is an ideal setting for further research on the linkages between SES and the evolution of BMI in old age. Although Japan has a highly developed economy, its population’s health and health behaviors differ significantly from those of other developed nations (Ikeda et al., 2011). For instance, the prevalence of obesity and overweight are substantially lower in Japan compared with the United States: 3% and 29% in men and 3% and 21% in women. In contrast, 32% and 72% of men and 36% and 64% of women in the United States are obese and overweight (Sassi, 2010). In addition, the SES–health relationship among Japanese population may be different from that among U.S. population, partially due to equal educational opportunities and access to medical care (Ikeda et al., 2011; Kagamimori, Gaina, & Nasermoaddeli, 2009). To our best knowledge, no study to date has focused on the linkage between SES and the trajectory of BMI among older Japanese.
Second, there is little understanding of how the linkage between SES and the trajectory of BMI among older adults interacts with age. The theory of age stratification suggests that age group represents a major source of inequality in access to society’s rewards, power, and privileges (Riley, 1971, 1987). These are closely associated with aging subculture and age norms, which may have major consequences for physical and mental health and may modify the influence of SES on health. Two theoretical perspectives inform our understanding in this regard. Based on the cumulative advantage theory, Ross & Wu (1996) assert that socioeconomic inequalities in health are larger among older compared with younger persons, because higher SES (i.e., education) increases resources which individuals can access and utilize (including economic, social, psychological, and healthy lifestyle resources), and the health benefits derived from these resources accumulate with time. On the other hand, House, Lantz, and Herd (2005) have suggested that socioeconomic disparities in health converge with age. Still, little is known about how well either of these theoretical perspectives apply to the issue of socioeconomic differences in BMI during old age, particularly in a nonwestern setting. Analyzing the SES-by-age interaction effect on the trajectory of BMI among older Japanese would represent a rigorous test of whether socioeconomic differences in the trajectory of BMI diverge or converge across age groups.
Given these considerations, our study has two specific aims. First, we offer quantitative estimates depicting the trajectory of BMI by analyzing 19 years of longitudinal data from a national sample of Japanese aged 60 and over at the baseline. Second, we examine how the level of BMI and its rate of change vary with SES (i.e., education and household income) and whether SES interacts with age in affecting the trajectory of BMI.
We pose the following hypotheses. First, based on prior observations (Kahng et al., 2004; Kuchibhatla et al., 2013; Usami & Sugawara, 2012), we hypothesize that among older Japanese, BMI decreases over time (H1). Second, we hypothesize that lower SES (i.e., education and household income) is associated with not only a higher level of BMI but also a faster rate of decline over time (H2 and H3). These two hypotheses are based on prior observations that lower SES was related to higher BMI among older Japanese women (Anzai, Ohkubo, Nishino, Tsuji, & Hisamichi, 2000; Tamakoshi et al., 2010), as well as that, among U.S. population, higher SES were associated with lower levels of BMI (Botoseneanu & Liang, 2011; Kahng et al., 2004) and slower rate of weight gain (Mujahid, Diez Roux, Borrell, & Nieto, 2005). Finally, based on the perspective of social stratification of aging and health (House et al., 2005), which states that health disparities converge with age, and on a previous Japanese study that identified a converging trend in the association between education and overweight (Anzai et al., 2000), we hypothsize that the association between SES and BMI trajectory is stronger among the young–old (i.e., 60–74), relative to the old–old (i.e., 75+) (H4).
Methods
Sample and Procedures
Data came from the National Survey of the Japanese Elderly (NSJE), a seven-wave (1987, 1990, 1993, 1996, 1999, 2002, and 2006) longitudinal data set based on a sample of 4,869 Japanese, 60 years of age and older, with 16,669 observations over a period of 19 years (1987–2006). NSJE began with 2,200 people aged 60 and over in 1987. The sample was subsequently supplemented in 1990 (N = 580) and 1996 (N = 1,210). An additional sample of those 70 years of age and older (N = 2,000) was added in 1999. The year when a respondent was first interviewed was regarded as the baseline year for each individual. Trained investigators visited the respondents’ homes, and face-to-face interviews employing a structured questionnaire were used to collect the data. Response rates for the 7 waves, calculated based on the number of people who answered as a proportion of those who were asked to participate at each wave, ranged from 67% to 93%. Responses obtained from proxy interviews were excluded. This study was approved by the Institutional Review Board of the Tokyo Metropolitan Institute of Gerontology.
Measures
Respondents’ self-reported height and weight were recorded at each wave. The dependent variable BMI was calculated according to the formula of weight/height2 (kg/m2). We used BMI as continuous variable in all the analytic models. Sample descriptive characteristics are presented according to BMI categories, defined as follows: underweight (BMI: < 18.5), normal weight (BMI: 18.5–24.9), and overweight (BMI: ≥25.0).
Socioeconomic status included education and annual household income. Education was indexed by the number of years of schooling, and household income was assessed by using five categories: “less than 1.2 million yen per year” (1), “1.2–3 million yen per year” (2), “3–5 million yen per year” (3), “5–10 million yen per year” (4) and “more than 10 million yen per year” (5). In the analysis, household income was treated as continuous variable (ranging 1–5).
Age, gender, household size, marital status, current working status and health status were incorporated as covariates in the appropriate models. Age differences were measured by age at baseline, whereas a binary indicator was created for gender (male [0] and female [1]). Household size (continuous variable) was included to account for higher household income in households with a larger number of family members. Marital status (not married [0] and married [1]) and current working status (not working [0] and working [1]) were indexed as binary indicators.
Multiple measures of health status were included. First, total condition was measured as a count of 16 health conditions (i.e., cancer, high blood pressure, heart conditions, diabetes, stroke, arthritis, eye disease, lung disease, chronic back pain, liver disease, trouble with circulation, stomach disease, kidney disease, anemia, Parkinson’s, and skin disease) (Ferraro & Farmer, 1999). Second, self-rated health was measured by a three-item composite (i.e., a rating of overall present health, satisfaction with one’s health, and comparison of one’s health with others of the same age), in accordance with previous studies (Liang et al., 2007). The self-rated health score ranges from 3 to 15 (Cronbach’s alpha = 0.85), with higher score indicating poorer health. Finally, functional status entailed a sum of difficulties with six activities of daily living (i.e., dressing, walking, bathing or showering, eating, getting in or out of bed, and using the toilet) and five instrumental activities of daily living (i.e., grocery shopping, phone calls, climbing stairs, walking a few blocks, and traveling by bus or train). All items except climbing stairs and walking a few blocks were coded from “no difficulty” (1) to “unable to do” (5). Climbing stairs and walking a few blocks were coded on a 5-point scale in waves 1 and 2, but coded on a 4-point scale in waves 3 through 7. Therefore, the 4-point scale in waves 3 through 7 was transformed into a 5-point scale. Scores for this composite ranged from 11.5 to 55 (Cronbach’s alpha = 0.92), with higher scores indicating greater difficulty.
In addition to these covariates, we used a dummy variable designating the entry wave for each respondent (i.e., baseline year; 1987, 1990, 1996, or 1999) to adjust for the difference by starting point of the survey participation. This variable was used as a categorical variable and added into the model as a dummy variable.
Data Analysis
Hierarchical linear models (HLMs) were used to chart the trajectory of BMI as a function of SES. The intrapersonal differences in the average BMI were modeled as follows in the Level 1 equation:
| (1) |
where Y iT is BMI by individual i at time T. π0i is the intercept (i.e., level), π1i is the linear slope (i.e., rate of linear change), and π2i is the quadratic slope (i.e., rate of acceleration) for individual i over time. Time is the distance (in years) of assessment from the baseline. πki represents the effect of X on individual i’s BMI, and εiT is a random error in BMI for individual i at time T. Time was centered on its grand mean (5.43 years).
Interpersonal variations in the trajectories of BMI were specified in the Level 2 equation:
| (2) |
where X qi is the qth covariate (e.g., age, gender, SES, household size, marital status, working status, health status, and entry wave) associated with individual i, and βpq represents the effect of variable Xq on the pth growth parameter (πp) (i.e., intercept and linear and quadratic slopes). rpi is a random effect with a mean of 0. All covariates (Level 2) were centered on their grand mean. All models were fitted by using HLM version 6.08.
To minimize missing data due to item nonresponse, multiple imputation was undertaken. In particular, three complete data sets were imputed with the NORM software developed by Schafer (1997), and analyses were run on each of these three data sets with parameter estimates derived by averaging across three imputations and by adjusting for their variance. Multilevel models are predicated on the assumption of missing at random (MAR), in that the probability of missing depends upon only the observed data for either the covariates or the outcome variables, hence permitting valid inference (Raudenbush & Bryk, 2002). In addition to MAR, to adjust for the selection bias, we included mortality and attrition due to nonresponse in the Level 2 equation. Mortality and attrition were viewed as confounding variables instead of predictors of BMI, because they can potentially bias the results toward healthier, longer living subjects who may differ in their level and rate of change in body weight from those who die or drop out during the study, particularly in older populations (Harel, Hofer, Hoffman, & Pedersen, 2007; Mroczek & Spiro, 2003). In accordance with previous studies (Botoseneanu & Liang, 2011, 2012), binary indicators were created for mortality (alive at the end of study [0] and died during the study [1]) and attrition (completed the study period [0] and dropped out for reasons other than mortality and did not return in subsequent waves [1]), and included in the Level 2 equations in the appropriate models.
The modeling strategy involved several steps. In Models 1 and 2, we focused on the associations of education and household income, respectively, with the level of BMI and its rate of change and acceleration, with adjustments for time-constant covariates (i.e., age, gender, household size, marital status, working status and health status at baseline, and death and attrition during the follow-up period). In Model 3, we controlled for the effect of both education and household income (i.e., these two SES variables were added into the model at the same time). Model 4 was additionally adjusted for baseline BMI and entry wave to examine how the net changes in body weight because the baseline vary by SES and whether entry wave differentially affects the trajectory of BMI. Finally, in Model 5, we examined age differences in the association between two SES variables and BMI by evaluating age-interaction effects.
Results
Table 1 presents the sample descriptive characteristics according to BMI category at the baseline. Mean BMI was 22.26, with 71.70% in the normal range, 10.72% underweight, and 17.58% overweight at baseline. Those who were underweight had a higher average age than the other groups. The proportion of female was the highest among the overweight. Educational level did not vary by body weight, while household income was the highest among those who were overweight. Education was positively correlated with household income at baseline (Spearman’s ρ = 0.251, p < .001; data not shown in the table). Mortality was the highest among those who were underweight (53.64%) and lowest among those who were overweight (28.62%).
Table 1.
Baseline Characteristics of the Participants (n = 4,869)
| Total sample | Underweight | Normal | Overweight | |
|---|---|---|---|---|
| BMI | 22.26±3.24 | 17.18±1.16 | 21.82±1.75 | 27.13±2.47 |
| Underweight (<18.5) | 10.72 | — | — | — |
| Normal (18.5–25.0) | 71.70 | — | — | — |
| Overweight (>25.0) | 17.58 | — | — | — |
| Age (years) | 69.85±7.20 | 72.94±7.46 | 69.65±7.19 | 68.81±6.58 |
| Female | 55.31 | 57.28 | 52.96 | 63.67 |
| Education (years) | 9.16±2.76 | 8.92±2.87 | 9.19±2.74 | 9.16±2.75 |
| Household income (range: 1–5) | 2.87±1.10 | 2.65±1.10 | 2.89±1.10 | 2.93±1.12 |
| <1.2 million yen (1) | 10.45 | 16.67 | 9.77 | 9.46 |
| 1.2–3 million yen (2) | 29.14 | 30.08 | 29.16 | 28.50 |
| 3–5 million yen (3) | 30.58 | 29.89 | 30.71 | 30.49 |
| 5–10 million yen (4) | 22.30 | 18.77 | 22.80 | 22.43 |
| More than 10 million yen (5) | 7.52 | 4.60 | 7.56 | 9.11 |
| Household size | 3.89±2.41 | 4.42±2.31 | 3.83±2.41 | 3.80±2.44 |
| Married | 67.06 | 56.13 | 68.03 | 69.74 |
| Current working | 31.65 | 21.65 | 32.74 | 33.29 |
| Total conditions (range: 0–16) | 1.23±1.36 | 1.36±1.60 | 1.16±1.28 | 1.42±1.51 |
| Self-rated poor health (range: 3–15) | 7.69±2.81 | 8.45±3.11 | 7.56±2.74 | 7.79±2.85 |
| Functional status (range: 11.5–55) | 12.56±3.81 | 13.51±5.46 | 12.42±3.53 | 12.52±3.60 |
| Mortality | 36.74 | 53.64 | 36.21 | 28.62 |
| Attrition | 20.99 | 15.52 | 21.03 | 24.18 |
| Entry wave | ||||
| Wave 1 (year of 1987) | 45.18 | 55.99 | 44.79 | 40.22 |
| Wave 2 (year of 1990) | 7.52 | 5.92 | 7.55 | 8.36 |
| Wave 4 (year of 1996) | 18.44 | 8.09 | 19.32 | 21.19 |
| Wave 5 (year of 1999) | 28.86 | 30.0 | 28.34 | 30.24 |
Values represent mean ± SD or %.
Using linear, quadratic and cubic functions, we mapped the trajectory of BMI between 1987 and 2006. Table 2 shows the results of the sequential multilevel models. The unconditional model (not shown in Table 2; available upon request) showed that BMI decreased following a quadratic (accelerating) trajectory, with an intercept (at mid-time point) of 22.084 (p < .001), linear slope of −0.041 (p < .001), and a quadratic slope of −0.0018 (p = .001), indicating that baseline BMI was 22.26 and declined to 21.18 over 19 years (approximately 1.1 BMI unit). As the cubic slope coefficient was not significant in the unconditional model, it was not included in subsequent analyses.
Table 2.
Hierarchical Linear Model for BMI
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | p | b | p | b | p | b | p | b | p | |
| Fixed effect | ||||||||||
| For intercept (π0i) | ||||||||||
| Intercept | 21.922 | <.001 | 21.921 | <.001 | 21.985 | <.001 | 21.933 | <.001 | 21.933 | <.001 |
| Age | −0.082 | <.001 | −0.083 | <.001 | −0.083 | <.001 | −0.041 | <.001 | −0.041 | <.001 |
| Female | 0.329 | .002 | 0.432 | <.001 | 0.363 | .002 | −0.064 | .279 | −0.062 | .287 |
| Education | −0.035 | .043 | −0.063 | .002 | −0.025 | .011 | −0.028 | .008 | ||
| Household income | 0.138 | .005 | 0.173 | .003 | 0.049 | .040 | 0.059 | .030 | ||
| Household size | −0.075 | .012 | −0.064 | .035 | 0.014 | .466 | 0.013 | .530 | ||
| Married | 0.221 | .042 | 0.167 | .132 | 0.111 | .359 | −0.112 | .110 | −0.109 | .122 |
| Current working | 0.114 | .260 | −0.197 | .215 | −0.172 | .279 | 0.071 | .467 | 0.066 | .527 |
| Total condition | 0.160 | <.001 | 0.150 | .001 | 0.149 | .001 | −0.017 | .487 | −0.016 | .513 |
| Self-rated health | −0.065 | .002 | −0.054 | .008 | −0.058 | .008 | −0.009 | .429 | −0.009 | .427 |
| Functional status | 0.029 | .177 | 0.029 | .173 | 0.003 | .880 | 0.026 | .083 | 0.025 | .090 |
| Mortality | −0.927 | <.001 | −0.833 | <.001 | −0.922 | <.001 | −0.425 | <.001 | −0.426 | <.001 |
| Attrition | 0.035 | 0.767 | 0.028 | .818 | 0.009 | .943 | 0.084 | .162 | 0.084 | .030 |
| Baseline BMI | 0.807 | <.001 | 0.807 | <.001 | ||||||
| Entry year: 1990a | −0.113 | .115 | −0.116 | .109 | ||||||
| Entry year: 1996a | 0.042 | .542 | 0.031 | .646 | ||||||
| Entry year: 1999a | 0.135 | .410 | 0.138 | .396 | ||||||
| Age × education | −0.002 | .253 | ||||||||
| Age × household income | 0.003 | .531 | ||||||||
| For linear slope (π1i) | ||||||||||
| Intercept | −0.023 | <.001 | −0.062 | <.001 | −0.063 | <.001 | −0.061 | <.001 | −0.061 | <.001 |
| Age | −0.005 | <.001 | −0.004 | <.001 | −0.004 | <.001 | −0.007 | <.001 | −0.007 | <.001 |
| Female | −0.020 | .073 | −0.024 | .025 | −0.026 | .018 | −0.013 | .226 | −0.012 | .236 |
| Education | −0.003 | .121 | −0.003 | .120 | −0.004 | .022 | −0.004 | .017 | ||
| Household income | 0.003 | .490 | 0.004 | .313 | 0.008 | .065 | 0.010 | .057 | ||
| Household size | 0.008 | .025 | 0.007 | .035 | 0.004 | .260 | 0.004 | .314 | ||
| Married | −0.029 | .008 | −0.032 | .004 | −0.032 | .004 | −0.020 | .074 | −0.020 | .086 |
| Current working | 0.000 | .961 | 0.029 | .111 | 0.027 | .138 | 0.014 | .446 | 0.013 | .500 |
| Total condition | −0.011 | .026 | −0.011 | .027 | −0.010 | .030 | −0.003 | .463 | −0.003 | .494 |
| Self-rated health | 0.000 | .827 | 0.001 | .656 | 0.001 | .682 | −0.001 | .505 | −0.001 | .502 |
| Functional status | 0.006 | .036 | 0.006 | .034 | 0.006 | .036 | 0.005 | .093 | 0.005 | .100 |
| Mortality | −0.056 | <.001 | −0.059 | <.001 | −0.061 | <.001 | −0.077 | <.001 | −0.077 | <.001 |
| Attrition | 0.011 | .288 | 0.010 | .331 | 0.010 | .336 | 0.013 | .214 | 0.013 | .211 |
| Baseline BMI | −0.031 | <.001 | −0.031 | <.001 | ||||||
| Entry year: 1990a | −0.021 | .094 | −0.022 | .085 | ||||||
| Entry year: 1996a | 0.006 | .608 | 0.004 | .731 | ||||||
| Entry year: 1999a | 0.023 | .468 | 0.024 | .453 | ||||||
| Age × education | 0.000 | .209 | ||||||||
| Age × household income | 0.001 | .493 | ||||||||
| For quadratic slope (π2i) | ||||||||||
| Intercept | −0.0025 | .008 | −0.0025 | .007 | −0.0024 | .009 | −0.0017 | .339 | −0.0017 | .339 |
| Age | −0.0001 | .317 | −0.0002 | .149 | −0.0002 | .227 | 0.0000 | .820 | 0.0000 | .956 |
| Female | 0.0005 | .682 | 0.0007 | .606 | 0.0011 | .417 | −0.0005 | .731 | −0.0005 | .734 |
| Education | 0.0004 | .052 | 0.0004 | .056 | 0.0006 | .021 | 0.0005 | .079 | ||
| Household income | −0.0001 | .822 | −0.0003 | .553 | −0.0006 | .396 | −0.0002 | .860 | ||
| Household size | −0.0007 | .180 | −0.0007 | .199 | −0.0005 | .387 | −0.0005 | .349 | ||
| Married | 0.0018 | .183 | 0.0021 | .133 | 0.0021 | .133 | 0.0016 | .311 | 0.0015 | .327 |
| Current working | 0.0005 | .628 | −0.0023 | .397 | −0.0022 | .422 | −0.0022 | .440 | −0.0022 | .414 |
| Total condition | 0.0001 | .820 | 0.0002 | .794 | 0.0001 | .825 | −0.0005 | .462 | −0.0005 | .466 |
| Self-rated health | 0.0001 | .666 | 0.0001 | .790 | 0.0001 | .753 | 0.0003 | .281 | 0.0003 | .296 |
| Functional status | 0.0009 | .161 | 0.0009 | .169 | 0.0009 | .164 | 0.0007 | .332 | 0.0007 | .330 |
| Mortality | 0.0022 | .237 | 0.0023 | .218 | 0.0025 | .188 | 0.0034 | .083 | 0.0034 | .084 |
| Attrition | 0.0008 | .523 | 0.0009 | .478 | 0.0009 | .494 | 0.0008 | .598 | 0.0008 | .563 |
| Baseline BMI | 0.0023 | <.001 | 0.0023 | <.001 | ||||||
| Entry year: 1990a | 0.0023 | .213 | 0.0025 | .151 | ||||||
| Entry year: 1996a | 0.0001 | .961 | 0.0004 | .874 | ||||||
| Entry year: 1999a | 0.0036 | .566 | 0.0034 | .602 | ||||||
| Age × education | 0.0000 | .807 | ||||||||
| Age × household income | 0.0001 | .725 | ||||||||
| Random effect (variance component) | ||||||||||
| Intercept | 7.745 | <.001 | 7.737 | <.001 | 8.234 | <0.001 | 1.536 | <.001 | 1.535 | <.001 |
| Linear slope | 0.021 | <.001 | 0.021 | <.001 | 0.021 | <0.001 | 0.043 | <.001 | 0.043 | <.001 |
| Quadratic slope | 0.000 | <.001 | 0.000 | <.001 | 0.000 | <0.001 | 0.001 | <.001 | 0.001 | <.001 |
| Level 1 ε | 2.241 | 2.241 | 2.241 | 1.364 | 1.364 | |||||
aRelative to entry year of 1987.
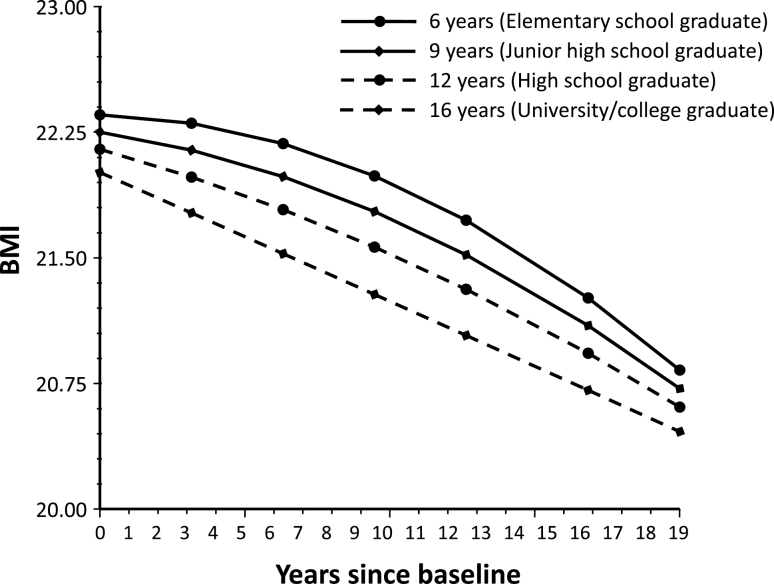
In Model 1, there was a significant association between higher education and lower BMI (b = −0.035, p = .043). This association remained significant when adjusting for household income at the same time in Model 3. When adjusting for baseline BMI and entry wave in conjunction with other time-constant covariates, mortality and attrition in Model 4, higher education was associated with lower BMI (b = −0.025, p = .011) and a greater rate of decline (b = −0.004, p = .022), although its acceleration (b = .0006, p = .021) slowed over time. As depicted in Figure 1, relative to those with less education, the BMI intercept among people with more education was lower, and declined linearly at a faster rate
Figure 1.
BMI trajectories by education at baseline (based on Model 3).
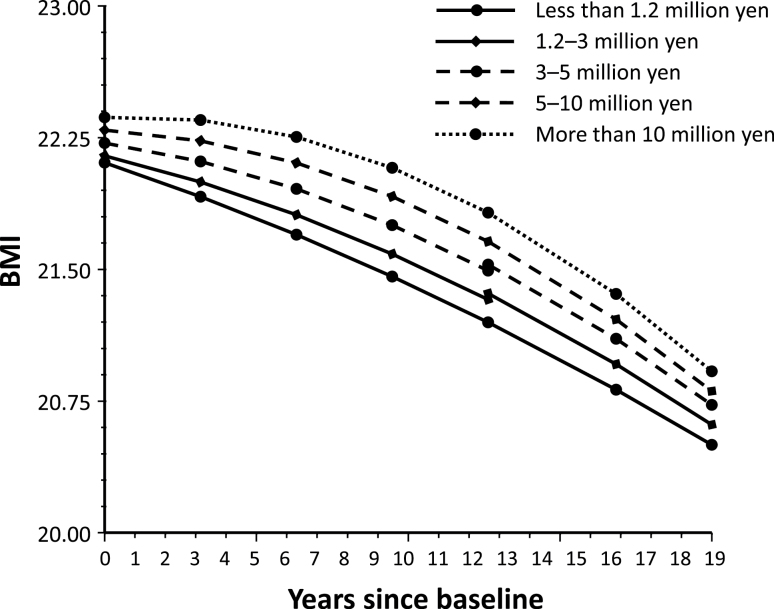
Higher household income at the baseline was associated with higher BMI (b = 0.138, p = .005, Model 2), and this association persisted after adjustment for educational level in Model 3, and baseline BMI and entry wave in Model 4. As shown in Figure 2, BMI was lower and declined at a relatively fast but steady pace in people with lower income.
Figure 2.
BMI trajectories by household income at baseline (based on Model 3).
The trajectory of BMI also exhibits significant age and gender variations. Older age was correlated with lower BMI (b = −0.083, p < .001, Model 4) as well as a greater rate of decline (b = −0.004, p < .001, Model 4), after adjusting for sociodemographic attributes and health status at baseline, mortality, and attrition. These age differences persisted after adjustment for baseline BMI and entry wave in Model 4. Compared with males, females had a higher level of BMI (b = 0.363, p = .002, Model 3) but a greater rate of decline (b = −0.026, p = .018, Model 3). However, gender variations might be accounted for by heterogeneity in baseline BMI and entry wave in Model 4.
Finally, we examined age variations in the SES–BMI linkages by evaluating the effects of interaction terms such as age-by-education and age-by-income on the trajectory of BMI in Model 5. However, these interactions were not statistically significant, offering no evidence for the hypothesized convergence of socioeconomic differences in BMI trajectory in old age.
Discussion
Based on 19 years of longitudinal data from a national sample, this is the first study to explore the relationship between SES and the trajectory of BMI in older Japanese. We found that BMI among older Japanese declined slightly but remained in the normal range (i.e., BMI: 18.5–24.9) over a 19-year period, from 22.26 to 21.18. This BMI level is substantially lower than the BMI level of 26 or greater observed among Americans aged 65 and over (Kahng et al., 2004; Kuchibhatla et al., 2013). Although both older Americans and older Japanese experienced a decrease in BMI over time, the rate of decline appeared to be slower among older Japanese.
The lower level of BMI among older Japanese may be partially explained by their dietary habits. Japanese people tend to consume less animal fat and more vegetables than people in other developed counties (Criqui & Ringel, 1994). Furthermore, older Japanese tend to spend more on seafood, fresh vegetable and fruits, and soybean products (e.g., tofu) than younger Japanese, who are more likely to purchase meat and dairy products (Ministry of Economy, Trade and Industry, 2012). To replicate our observations, further research on the trajectory of BMI among older adults is warranted, particularly using data from other Eastern Asian nations which share similar dietary habits with Japan.
Regarding the effect of education on BMI, our results were similar to those based on data derived from western developed nations in that higher education was associated with lower BMI, and BMI declined at a relatively faster rate over time among those with higher education compared to those with less education. These results lend support to our second hypothesis (H2), suggesting that the causal mechanisms underlying the education-BMI trajectory are similar between western developed nations and Japan, despite the significant cultural differences. With greater knowledge-related assets (e.g., knowledge and skills) (Galobardes, Shaw, Lawlor, Lynch, & Davey Smith, 2006b; Lynch & Kaplan, 2000) and socio-psychological resources (e.g., self-efficacy and problem-solving coping capacity) (Ross & Wu, 1995), better educated individuals are more likely to be able to control their weight.
Contrary to our third hypothesis (H3), there was an indication that higher household income was associated with higher BMI (Models 3 and 4). These results were robust regardless whether household income was modeled as a continuous variable (Table 2) or a discrete measure with five categories (data not shown; available upon request). These findings need to be interpreted in view of the following observations from prior researches. First, there is evidence that different measures of SES (e.g., education and income) have both common and independent pathways linking them to health (Robert & House, 2000). For instance, Herd, Goesling & House (2007) showed that education was more predictive than income of the onset of functional limitations and chronic conditions, whereas income was more strongly associated with the progression of both. Second, among the OECD member states, Japan is about average in terms of income inequality (i.e., Gini coefficient = 0.329 in late 2000s), which is substantially less than that in the United States (i.e., Gini coefficient = 0.378 in late 2000s) (OECD, 2011). BMI among older Japanese varied very modestly within the normal range over the 19-year period of observation, and was at a substantially lower level than that among older Americans on which most prior observations were based. Because of the relative egalitarian nature of the Japanese society and its substantially lower prevalence of obesity and overweight, it is conceivable that the income–BMI linkage may differ from that observed in western developed nations, particularly the United States. Third, research findings regarding the association between SES and BMI or obesity have been mixed, especially in nonwestern nations. For instance, Fukuda and Hiyoshi (2013) found a negative association between household expenditures and obesity among middle-aged Japanese women, but not among men. In addition, Martikainen, Ishizaki, Marmot, Nakagawa, and Kagamimori, (2001) reported that among employed Japanese men, higher occupational grades were associated with higher BMI and waist-to-hip-ratio, whereas in England, higher employment grades were advantaged with regard to most health risk factors. This suggests that cultural variations may exist in the income–body wieght relationship.
Hence, in Japan—a relatively egalitarian society, an observed positive correlation between income and BMI is indeed plausible. Income is generally considered to reflect access to material conditions affecting health (e.g., better health-improving commodities and services) (Galobardes, Shaw, Lawlor, Lynch, & Davey Smith, 2006a; Lynch & Kaplan, 2000). One factor accounting for the relationship between income and BMI may be food choice and intake. The variety of food choices that meet nutritional needs among the elderly is affected by economic assets such as income (Dean, Raats, Grunert, Lumbers, & The Food in Later Life Team, 2009). Among the Japanese, higher household expenditures are associated with higher nutritional intake (Fukuda & Hiyoshi, 2012). In addition, the residential environment might partially mediate the link between income and healthy food intake. While better access to supermarkets is related to healthier food intake (Larson, Story, & Nelson, 2009), poor people tend to live in areas with limited access to supermarkets and, at the same time, with greater exposure to fast food outlets (Block, Scribner, & DeSalvo, 2004) and thus may have less healthy diets. However, the impact of nutritious food intake or malnutrition may depend on cultures and countries (NU-AGE, 2012). Considering the relatively lower levels of BMI and its declining trajectory in our Japanese sample, nutritious food intake primarily contributes to maintaining an appropriate weight and preventing unhealthy weight loss. Indeed people with higher household expenditures not only have better nutritional intake, but also consume higher total energy (kcal/day) and total fat (% energy) (Fukuda & Hiyoshi, 2012). While U.S. studies have suggested that better access to supermarkets is related to lower levels of obesity (Larson et al., 2009), a recent Japanese study reported that better access to supermarkets was related to higher BMI among older people (Hanibuchi et al., 2011).
Another possible factor explaining the differential direction of the relationship between income and BMI is physical exercise. Indeed, U.S. studies have shown that older adults engaged in or initiating vigorous physical activity had lower BMI trajectories compared with those who were consistently inactive (Botoseneanu & Liang, 2012). In Japan, Murakami et al. (2011) revealed that higher income was associated with a higher likelihood of habitual exercise among younger cohort, but this association tended to be negative among people aged 60 and over, mainly because of time constraints, a shorter payoff period of health investment, and less feasibility of high intensity exercise. Further research concerning the roles of nutrition intake and physical exercise underlying the linkage between income and BMI among older Japanese is certainly warranted.
We evaluated the effects of interactions between age and SES on BMI trajectory (H4) in order to examine if socioeconomic disparities in BMI trajectories differed between early and late old age (House et al., 2005), and found no evidence for a convergence of socioeconomic disparities in BMI with age. This is consistent with prior observations that health disparities are smaller in Japan than in the United States, because of equal educational opportunities and access to medical care (Ikeda et al., 2011). Nonetheless, as noted by Kagamimori et al. (2009), health disparities have been increasing in Japan, which requires new policy initiatives, particularly given the rapid aging of the Japanese population. At the same time, the hypotheses of cumulative advantage (Ross & Wu, 1996) and convergence of socioeconomic disparities (House et al., 2005) need to be further evaluated, particularly with data from societies with socioeconomic profiles significantly different from those observed in the United States.
To ascertain the robustness of our results regarding the association between SES and BMI trajectory, we performed additional examinations. First, we determined that the correlation between education and household income was positive and statistically significant (i.e., higher education was associated with higher household income). Thus, the conflicting results for education and household income cannot be explained by a lack of correlation, or a negative correlation, between these variables. In addition, education and household income were added into the model separately (Models 1 and 2). The directions of the associations of education and household income (positive or negative) were the same as those in Model 3. Therefore, the perplexing finding of the contrasting results for education and household income appears to be robust; as such, further research to find an explanation for this finding is warranted. Second, because earlier articles suggested gender differences in the SES–BMI linkage (Ball & Crawford, 2005), we conducted a gender-stratified analysis (shown in the Supplementary Table). The directions of the associations between SES and BMI trajectory in both genders were similar to those found in the full sample (Table 2). Third, because several indicators, such as household income and health status, could have changed during the follow-up period, we performed additional analysis including time-varying covariates in the model. We treated household income, household size, marital status, current working status, and health status as not only time-constant variables but also time-varying variables, and added these time-varying covariates in the Level 1 equations of Models 3–5. However, the results were very similar to those generated from models without time-varying variables (data not shown; available upon request). Thus, the additional analyses confirmed the robustness of our findings.
In addition to sociodemographic factors, health status also had a significant impact on BMI trajectories. We included three health status indices and the direction of the association with the BMI trajectory varied among these indices. For example, a higher score of total condition (i.e., greater disease burden) was associated with a higher level of BMI (b = 0.149, p = .001, Model 3), while a higher score of self-rated health (i.e., worse self-rated health) was associated with a lower BMI level (b = −0.058, p = 0.008, Model 3). Moreover, we found a significant interaction between total condition and household income on the linear slope when adding this interaction term in Model 4 (data not shown; available upon request); this indicates that people with higher disease burden and lower household income had a faster linear decline in BMI over time compared with those with a lower disease burden and lower household income. Thus, disease burden had an important role on the relationship between household income and BMI. In previous research, Newsom et al. (2012) showed that the vast majority of individuals did not make major lifestyle changes following diagnosis of a serious chronic disease, either in the short term or in the long term. However, few have studied the role of health status on the trajectory of BMI. Further examination of not only the direct effect of health status on the BMI trajectory, but also a possible mediating effect of health status on the SES–BMI association should be conducted.
This research has several limitations. First, we relied on self-reported measures of height and weight instead of objectively measured values. People tend to over-report their height and underreport their weight (Gunnell et al., 2000), thus the level of BMI may be underestimated. However, if the level of under/over-reporting is relatively constant over time, the estimation of BMI trajectories over time should not be biased by misreporting. Second, because our sample consisted of only respondents aged 60 and over, a proper examination of whether one’s life history of BMI change (i.e., the levels of BMI in their young and middle age) moderates the effects of social stratification on the BMI trajectory was not possible. Previous studies using younger cohorts have shown that social stratification (e.g., age, gender, and SES) in young adulthood was associated with BMI trajectories (Clarke, O’Malley, Johnston, & Schulenberg, 2009; Fuemmeler et al., 2012). Therefore, future studies are needed to fully evaluate the lifelong relationship between socioeconomic factors and BMI trajectories. Third, period effects may influence the results of this study. For example, during our observation (1987–2006), several health policies to promote healthy lifestyles were initiated in Japan, such as the “Active 80 Health Plan” in 1988 and “Healthy Japan 21” in 2000. The trajectories of BMI may be influenced by these health policies related to weight control. Fourth, our analysis did not include variables assessing interpersonal relationships, such as spousal information (e.g., spouse’s weight level, educational level, and occupational status) or social networks. It has been previously reported that obesity spreads through social ties (Christakis & Fowler, 2007), so the effect of these factors on BMI trajectory should be tested in future studies.
This research provides new insights concerning the complex dynamics underlying the linkages between SES and BMI. It reveals that among older Japanese, the trajectory of BMI is at a substantially lower level and tends to be more stable relative to those reported in Western populations. Despite the fact that education and income are positively correlated, they appear to have distinct effects on how BMI evolves over time in old age. Whereas higher education is associated with a lower BMI and a faster rate of decline, higher income is correlated with higher BMI and a slower rate of decline. Furthermore, we did not find evidence that socioeconomic differences in the trajectory of BMI vary by age, as suggested by prior research in the United States. These results indicate cross-cultural differences the SES–BMI linkage and argue for the need for future research to specify the factors responsible for these differences and their association with various aging outcomes. Based on the findings, we can inform the design of health policies and interventions aimed at promoting and maintaining health in late life. It underscores the importance of targeting both socioeconomic factors as well as cultural factors, in the design of interventions for weight control. International health policies may require sensitivity to cross-national variations in the socioeconomic covariates of how BMI changes over time.
Supplementary Material
Supplementary material can be found at: http://psychsocgerontology.oxfordjournals.org/
Funding
This work was supported by the National Institute on Aging (R01 AG031109, P60 AG024824) at the National Institutes of Health.
Supplementary Material
Acknowledgments
H. Murayama planned the analysis, performed all statistical analyses, and wrote the article. J. Liang supervised the entire study project and the analysis and revised the article. J.M. Bennett supervised the analysis and revised the article. B.A. Shaw and A. Botoseneanu helped the analysis and revised the article. E. Kobayashi and T. Fukaya conducted the data collection and revised the article. S. Shinkai supervised the analysis and revised the article.
References
- Adler N. E., Newman K. (2002). Socioeconomic disparities in health: pathways and policies. Health Affairs (Project Hope), 21, 60–76. 10.1377/hlthaff.21.2.60 [DOI] [PubMed] [Google Scholar]
- Anzai Y., Ohkubo T., Nishino Y., Tsuji I., Hisamichi S. (2000). Relationship between health practices and education level in the rural Japanese population. Journal of Epidemiology/Japan Epidemiological Association, 10, 149–156. 10.2188/jea.10.149 [DOI] [PubMed] [Google Scholar]
- Asia Pacific Cohort Studies Collaboration. (2004). Body mass index and cardiovascular disease in the Asia-Pacific Region: an overview of 33 cohorts involving 310,000 participants. International Journal of Epidemiology, 33, 751–758. 10.1093/ije/dyh163 [DOI] [PubMed] [Google Scholar]
- Ball K., Crawford D. (2005). Socioeconomic status and weight change in adults: a review. Social Science & Medicine, 60, 1987–2010. 10.1016/j.socscimed.2004.08.056 [DOI] [PubMed] [Google Scholar]
- Block J. P., Scribner R. A., DeSalvo K. B. (2004). Fast food, race/ethnicity, and income: a geographic analysis. American Journal of Preventive Medicine, 27, 211–217. 10.1016/j.amepre.2004.06.007 [DOI] [PubMed] [Google Scholar]
- Bogers R. P., Bemelmans W. J., Hoogenveen R. T., Boshuizen H. C., Woodward M., Knekt P, … BMI-CHD Investigators. (2007). Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Archives of Internal Medicine, 167, 1720–1728. 10.1001/archinte.167.16.1720 [DOI] [PubMed] [Google Scholar]
- Botoseneanu A., Liang J. (2011). Social stratification of body weight trajectory in middle-age and older americans: results from a 14-year longitudinal study. Journal of Aging and Health, 23, 454–480. 10.1177/0898264310385930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botoseneanu A., Liang J. (2012). The effect of stability and change in health behaviors on trajectories of body mass index in older Americans: a 14-year longitudinal study. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 67, 1075–1084. 10.1093/gerona/gls073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis N. A., Fowler J. H. (2007). The spread of obesity in a large social network over 32 years. The New England Journal of Medicine, 357, 370–379. 10.1056/NEJMsa066082 [DOI] [PubMed] [Google Scholar]
- Clarke P., O’Malley P. M., Johnston L. D., Schulenberg J. E. (2009). Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986-2004. International Journal of Epidemiology, 38, 499–509. 10.1093/ije/dyn214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Criqui M. H., Ringel B. L. (1994). Does diet or alcohol explain the French paradox? Lancet, 344, 1719–1723. 10.1016/S0140-6736(94)92883–5 [DOI] [PubMed] [Google Scholar]
- Daviglus M. L., Liu K., Yan L. L., Pirzada A., Manheim L., Manning W. … Stamler J. (2004). Relation of body mass index in young adulthood and middle age to Medicare expenditures in older age. Journal of the American Medical Association, 292, 2743–2749. 10.1001/jama.292.22.2743 [DOI] [PubMed] [Google Scholar]
- Berrington de Gonzalez A., Hartge P., Cerhan J. R., Flint A. J., Hannan L., MacInnis R. J. … Thun M. J. (2010). Body-mass index and mortality among 1.46 million white adults. The New England Journal of Medicine, 363, 2211–2219. 10.1056/NEJMoa1000367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean M., Raats M. M., Grunert K. G., Lumbers M; Food in Later Life Team. (2009). Factors influencing eating a varied diet in old age. Public Health Nutrition, 12, 2421–2427. 10.1017/S1368980009005448 [DOI] [PubMed] [Google Scholar]
- Ferraro K. F, Farmer M. M. (1999). Utility of health data from social surveys: is there a gold standard for measuring morbidity? American Sociological Review, 64, 303–315. [Google Scholar]
- Flegal K. M., Kit B. K., Orpana H., Graubard B. I. (2013). Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. Journal of the American Medical Association, 309, 71–82. 10.1001/jama.2012.113905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flicker L., McCaul K. A., Hankey G. J., Jamrozik K., Brown W. J., Byles J. E., Almeida O. P. (2010). Body mass index and survival in men and women aged 70 to 75. Journal of the American Geriatrics Society, 58, 234–241. 10.1111/j.1532-5415.2009. 02677.x [DOI] [PubMed] [Google Scholar]
- Fuemmeler B. F., Yang C., Costanzo P., Hoyle R. H., Siegler I. C., Williams R. B., Ostbye T. (2012). Parenting styles and body mass index trajectories from adolescence to adulthood. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 31, 441–449. 10.1037/a0027927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuda Y., Hiyoshi A. (2012). High quality nutrient intake is associated with higher household expenditures by Japanese adults. Bioscience Trends, 6, 176–182. 10.5582/bst.2012.v6.4.176 [DOI] [PubMed] [Google Scholar]
- Fukuda Y., Hiyoshi A. (2013). Associations of household expenditure and marital status with cardiovascular risk factors in Japanese adults: analysis of nationally representative surveys. Journal of Epidemiology/Japan Epidemiological Association, 23, 21–27. 10.2188/jea.JE20120021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B., Shaw M., Lawlor D. A., Lynch J. W., Davey Smith G. (2006. a). Indicators of socioeconomic position (part 1). Journal of Epidemiology & Community Health, 60, 7–12. 10.1136/jech.2004.023531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B., Shaw M., Lawlor D. A., Lynch J. W., Davey Smith G. (2006. b). Indicators of socioeconomic position (part 2). Journal of Epidemiology & Community Health, 60, 95–101. 10.1136/jech.2004.028092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski D. C., Ellis J. E. (2001). High body mass index does not predict mortality in older people: analysis of the Longitudinal Study of Aging. Journal of the American Geriatrics Society, 49, 968–979. 10.1046/j.1532-5415.2001.49189.x [DOI] [PubMed] [Google Scholar]
- Gunnell D., Berney L., Holland P., Maynard M., Blane D., Frankel S., Smith G. D. (2000). How accurately are height, weight and leg length reported by the elderly, and how closely are they related to measurements recorded in childhood? International Journal of Epidemiology, 29, 456–464. 10.1093/ije/29.3.456 [PubMed] [Google Scholar]
- Hanibuchi T., Kondo K., Nakaya T., Nakade M., Ojima T., Hirai H., Kawachi I. (2011). Neighborhood food environment and body mass index among Japanese older adults: results from the Aichi Gerontological Evaluation Study (AGES). International Journal of Health Geographics, 10, 43. 10.1186/1476-072X-10-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harel O., Hofer S. M., Hoffman L., Pedersen N. L. (2007). Population inference with mortality and attrition in longitudinal studies on aging: a two-stage multiple imputation method. Experimental Aging Research, 33, 187–203. [DOI] [PubMed] [Google Scholar]
- Herd P., Goesling B., House J. S. (2007). Socioeconomic position and health: the differential effects of education versus income on the onset versus progression of health problems. Journal of Health and Social Behavior, 48, 223–238. 10.1177/002214650704800302 [DOI] [PubMed] [Google Scholar]
- House J. S., Lantz P. M., Herd P. (2005). Continuity and change in the social stratification of aging and health over the life course: evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans’ Changing Lives Study). The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, 15–26. 10.1093/geronb/60.Special_Issue_2 [DOI] [PubMed] [Google Scholar]
- Ikeda N., Saito E., Kondo N., Inoue M., Ikeda S., Satoh T. … Shibuya K. (2011). What has made the population of Japan healthy? Lancet, 378, 1094–1105. 10.1016/S0140-6736(11)61055-6 [DOI] [PubMed] [Google Scholar]
- Kagamimori S., Gaina A., Nasermoaddeli A. (2009). Socioeconomic status and health in the Japanese population. Social Science & Medicine, 68, 2152–2160. 10.1016/j.socscimed.2009.03.030 [DOI] [PubMed] [Google Scholar]
- Kahng S. K., Dunkle R. E., Jackson J. S. (2004). The relationship between the trajectory of body mass index and health trajectory among older adults: multilevel modeling analyses. Research on Aging, 26, 31–61. 10.1177/0164027503258734 [Google Scholar]
- Kuchibhatla M. N., Fillenbaum G. G., Kraus W. E., Cohen H. J., Blazer D. G. (2013). Trajectory classes of body mass index in a representative elderly community sample. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 68, 699–704. 10.1093/gerona/gls215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson N. I., Story M. T., Nelson M. C. (2009). Neighborhood environments: disparities in access to healthy foods in the U.S. American Journal of Preventive Medicine, 36, 74–81. 10.1016/j.amepre.2008.09.025 [DOI] [PubMed] [Google Scholar]
- Liang J., Shaw B. A., Bennett J. M., Krause N., Kobayashi E., Fukaya T., Sugihara Y. (2007). Intertwining courses of functional status and subjective health among older Japanese. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 62, S340–S348. 10.1093/gerona/gls215 [DOI] [PubMed] [Google Scholar]
- Lynch J., Kaplan G. (2000). Socioeconomic position. In Berkman L. F., Kawachi I. (Eds.), Social Epidemiology (pp. 13–35). New York, NY: Oxford University Press. [Google Scholar]
- Martikainen P., Ishizaki M., Marmot M. G., Nakagawa H., Kagamimori S. (2001). Socioeconomic differences in behavioural and biological risk factors: a comparison of a Japanese and an English cohort of employed men. International Journal of Epidemiology, 30, 833–838. 10.1093/ije/30.4.833 [DOI] [PubMed] [Google Scholar]
- McLaren L. (2007). Socioeconomic status and obesity. Epidemiologic Reviews, 29, 29–48. 10.1093/epirev/mxm001 [DOI] [PubMed] [Google Scholar]
- Ministry of Economy, Trade and Industry (2012). Analysis of all industrial activities: the first quarter of 2012. Tokyo, Japan: Ministry of Economy, Trade and Industry. [Google Scholar]
- Mroczek D. K., Spiro A. (2003). Modeling intraindividual change in personality traits: findings from the normative aging study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 58, P153–P165. 10.1093/geronb/58.3.P153 [DOI] [PubMed] [Google Scholar]
- Mujahid M. S., Diez Roux A. V., Borrell L. N., Nieto F. J. (2005). Cross-sectional and longitudinal associations of BMI with socioeconomic characteristics. Obesity Research, 13, 1412–1421. 10.1038/oby.2005.171 [DOI] [PubMed] [Google Scholar]
- Murakami K., Hashimoto H., Lee J. S., Kawakubo K., Mori K., Akabayashi A. (2011). Distinct impact of education and income on habitual exercise: a cross-sectional analysis in a rural city in Japan. Social Science & Medicine, 73, 1683–1688. 10.1016/j.socscimed.2011.09.024 [DOI] [PubMed] [Google Scholar]
- Newsom J. T., Huguet N., McCarthy M. J., Ramage-Morin P., Kaplan M. S., Bernier J. … Oderkirk J. (2012). Health behavior change following chronic illness in middle and later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 279–288. 10.1093/geronb/gbr103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NU-AGE. (2012). Report on the socio-economic determinants of food choices and preferences of the elderly Retrieved from http://www.nu-age.eu/socio-economic-determinants
- OECD (2011). An overview of growing income inequalities in OECD countries: main findings. Divided we stand: why inequality keeps rising (pp. 21–45). Paris, France: OECD Publishing. [Google Scholar]
- Raudenbush S. W., Bryk A. S. (2002). Hierarchical linear models: applications and data analysis methods (2nd ed.). Newbury Park, CA: Sage. [Google Scholar]
- Riley M. W. (1971). Social gerontology and the age stratification of society. The Gerontologist, 11, 79–87. 10.1093/geront/11.1_part_1.79 [DOI] [PubMed] [Google Scholar]
- Riley M. W. (1987). On the significance of age in sociology. American Sociological Review, 52, 1–14. 10.2307/2095388 [Google Scholar]
- Robert S. A., House J. S. (2000). Socioeconomic inequalities in health: an enduring sociological problem. In Bird C. E., Conrad P., Fremont A. M. (Eds.), Handbook of medical sociology (pp. 79–97) (5th ed.). Upper Saddle River, NJ: Prentice Hall. [Google Scholar]
- Romero-Corral A., Montori V. M., Somers V. K., Korinek J., Thomas R. J., Allison T. G. … Lopez-Jimenez F. (2006). Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet, 368, 666–678. 10.1016/S0140-6736(06)69251-9 [DOI] [PubMed] [Google Scholar]
- Ross C. E., Wu C. L. (1995). The Links between Education and Health. American Sociological Review, 60, 719–745. [Google Scholar]
- Ross C. E., Wu C. L. (1996). Education, age, and the cumulative advantage in health. Journal of Health and Social Behavior, 37, 104–120. [PubMed] [Google Scholar]
- Sassi F. (2010). Obesity and the economics of prevention: fit not fat. Paris, France: OECD publishing. [Google Scholar]
- Schafer J. L. (1997). Analysis of incomplete multivariatedata. London, UK: Chapman & Hall. [Google Scholar]
- Sobal J., Stunkard A. J. (1989). Socioeconomic status and obesity: a review of the literature. Psychological Bulletin, 105, 260–275. 10.1037/0033-2909.105.2.260 [DOI] [PubMed] [Google Scholar]
- Tamakoshi A., Yatsuya H., Lin Y. S., Tamakoshi K., Kondo T., Suzuki S. … JACC Study Group (2010). BMI and all-cause mortality among Japanese older adults: findings from the Japan Collaborative Cohort Study. Obesity, 18, 362–369. 10.1038/oby. 2009.190 [DOI] [PubMed] [Google Scholar]
- Usami S., Sugawara I. (2012). A longitudinal investigation of some physical traits of the Japanese old using latent curve models: analysis of Japanese longitudinal study data using MCMC method. Japanese Journal of Behavior Metrics, 39, 43–62. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.