Abstract
Peripheral T cell lymphoma not otherwise specified (PTCL-NOS) is a rare entity of lymphoma. We herein report an even rarer case of a 68-year-old male with PTCL-NOS presenting as an endobronchial lesion, and review previously published cases in the literature. Initially, he was referred to our hospital for further investigation of the right upper lobe consolidation on chest radiograph. Computed tomography and 18F-fludeoxyglucose positron emission tomography revealed a right hilar mass with obstruction of the main bronchus and submandibular, right axillary and mediastinal lymphadenopathy. Pathological examination of the biopsy specimens from of the endobronchial lesion and subcutaneous nodule revealed PTCL-NOS. Chemotherapy was started but he finally died due to septic shock after the second-line chemotherapy.
Keywords: Peripheral T cell lymphoma not otherwise specified, Airway lesion, Transbronchial biopsy
1. Introduction
The World Health Organization (WHO) classification defines peripheral T cell lymphoma not otherwise specified (PTCL-NOS) as a heterogeneous category of nodal and extranodal mature T cell lymphomas that do not correspond to any of the specifically defined entities of mature T cell lymphomas in the current classification [1]. Cases that do not match one of the defined entities of PTCL are best categorized as “not otherwise specified” (NOS), reflecting the fact that we do not yet understand everything about lymphomas or the immune system [2]. Generalized lymphadenopathy is the most common CT finding of PTCL-NOS, and an airway lesion is rarely reported. We herein report the rare case of PTCL-NOS with an airway lesion that was diagnosed by a transbronchial biopsy.
2. Case report
A 68-year-old Japanese male was indicated a chest radiographic abnormality in the right upper lung field by routine health check-up. One month later, a right chest pain occurred, and he was diagnosed with right upper lobe pneumonia at the previous hospital. Despite antibiotic treatment, chest radiographic abnormality got worse and he was referred to our hospital for more thorough examinations. The patient was a current smoker with a 24-pack-year history of smoking. He had no medical history. His vital signs were within the normal limits. A general physical examination revealed an enlarged lymph node in the right axillary region. His lymph node was firm, unmovable and non-tender and measured 3.0 × 3.0 cm. A chest X-ray showed consolidation in the right upper lung field (Fig. 1). Contrast-enhanced whole-body computed tomography (CT) disclosed a right axillary lymphadenopathy and a right hilar mass with obstruction of the main bronchus (Fig. 2). 18-F-fluorodeoxyglucose (FDG) positron emission tomography (PET) revealed an abnormal FDG accumulation in the subcutaneous nodules on the mandibular and left chest wall, a part of the trachea, lymph nodes (submandibular, right axillary and mediastinal), right hilar mass, retroperitoneal mass and mass in the right femoral muscle with high metabolic activity (SUVmax: 5.75–21.1) (Fig. 3).
Fig. 1.

A chest X-ray revealed consolidation of the right upper lung field.
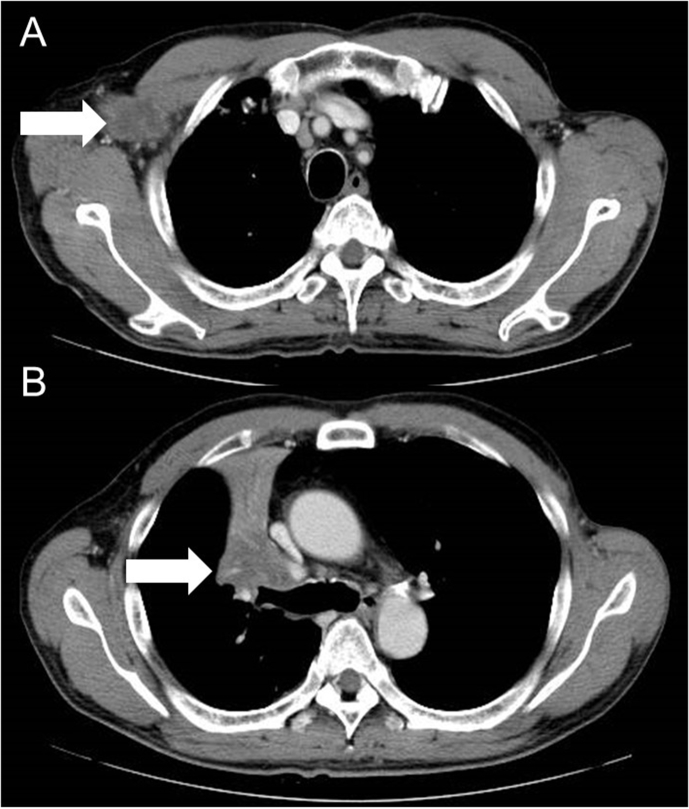
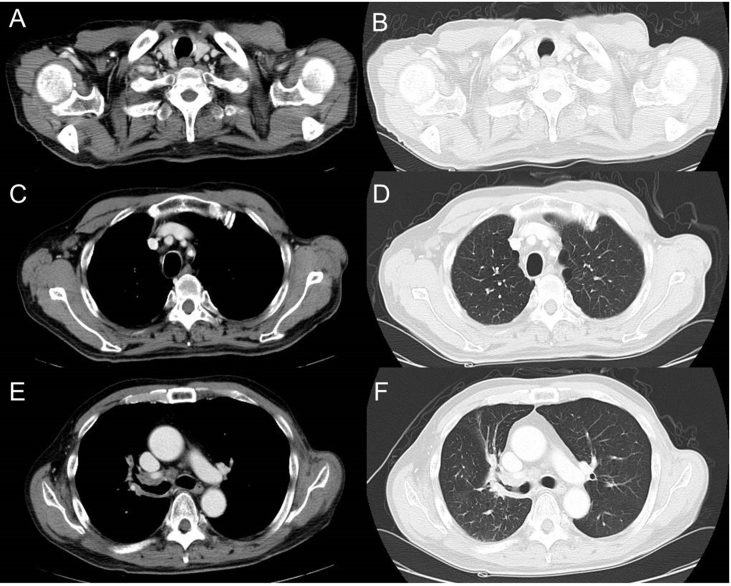
Fig. 2.
Contrast-enhanced whole-body CT disclosed a right axillary lymphadenopathy (A), a tumor mass in the right hilum and partial right upper lobe atelectasis (B).
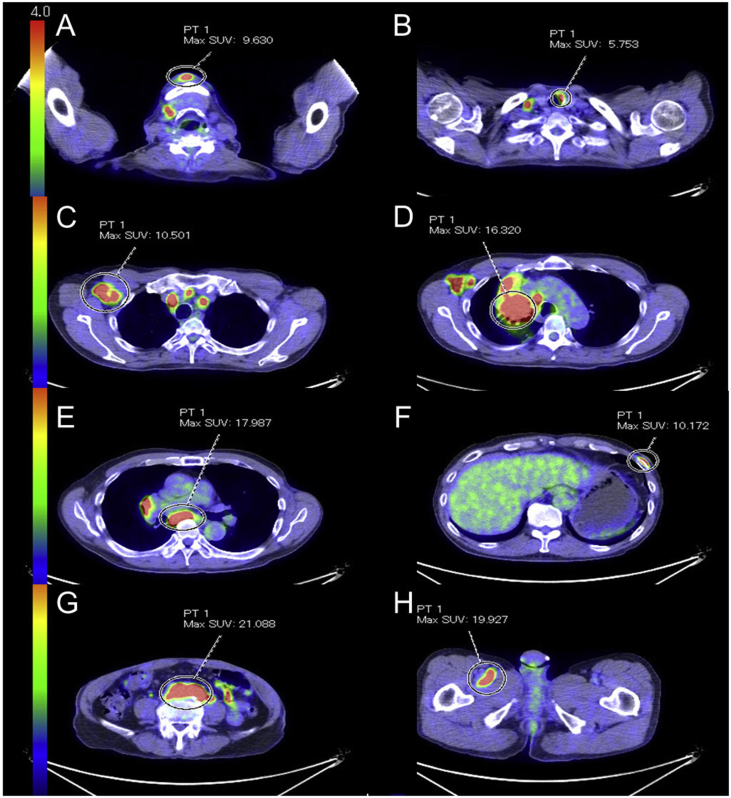
Fig. 3.
FDG PET revealed an abnormal FDG accumulation in the subcutaneous nodules on the mandibular (A) and left chest wall (F), a part of the trachea (B), lymph nodes (submandibular, right axillary and mediastinal), right hilar mass (C,D,E), retroperitoneal mass (G) and mass in the right femoral muscle (H) with high metabolic activity (SUVmax: 5.75–21.1).
Bronchoscopy showed a white, moss-like appearance of the trachea just below the glottis and right B3 entrance stenosis with a large amount of purulent discharge (Fig. 4). A transbronchial biopsy (TBB) was performed on both lesions, and atypical medium-to large-sized cells were found arranged in nests with marked lymphocyte infiltration. An immunohistochemical study revealed focal positive staining for CD3, CD8, TIA-1, and C—C chemokine receptor type 4 (CCR4), and negative staining for CD4, CD20, and EBV (Fig. 5A and B). In addition, a biopsy of the subcutaneous nodules on the left chest wall also showed the same findings (Fig. 5C and D). A bone marrow biopsy showed hypoplastic marrow, and invasion of lymphoma was not suspected. From these results, the patient was diagnosed with stage IVA PTCL-NOS, and chemotherapy was started. The chemotherapy regimen included cyclophosphamide, adriamycin, vincristine, and prednisolone (CHOP therapy). Grade 4 neutropenia and Grade 1 thrombocytopenia were observed during the treatment. After five cycles of chemotherapy, contrast-enhanced whole-body CT showed a reduction in the right hilar mass and all of the lymph nodes (right axillary, mental, submandibular, cervical, subcarinal, splenic hilar and retroperitoneal region) (Fig. 6), with a partial response according to the Response Evaluation Criteria in Solid Tumors (version 1.1). After six courses of CHOP, contrast whole-body CT revealed an enlargement of the tumor mass in the right hilum, and salvage chemotherapy (CHASE therapy: cyclophosphamide, cytarabine, etoposide, and dexamethasone) was started. The patient ultimately died because of septic shock after undergoing three courses of CHASE therapy.
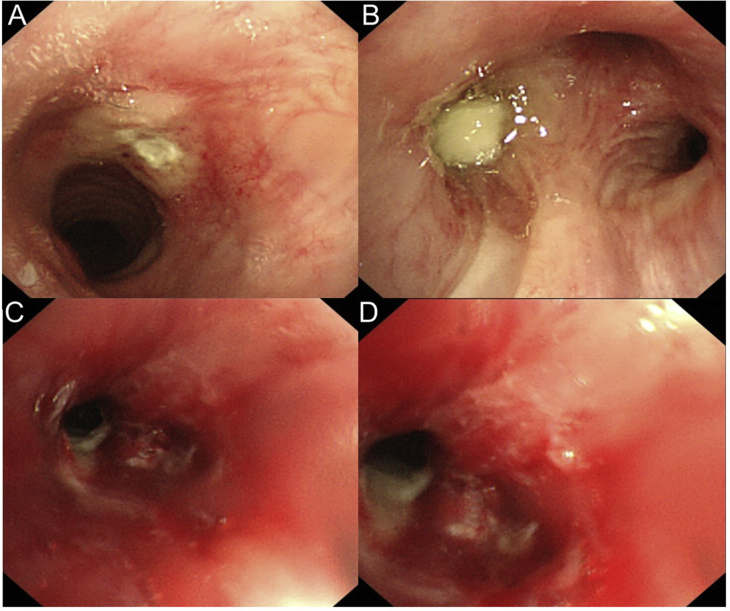
Fig. 4.
Bronchoscopy showed an ulcerative lesion just below the glottis (A), and a white necrotic material block in the right upper bronchus (B). C and D are bronchoscopic findings of the right upper bronchus after removal of necrotic material. The bronchial mucosa was hemorrhagic and highly stenosed.
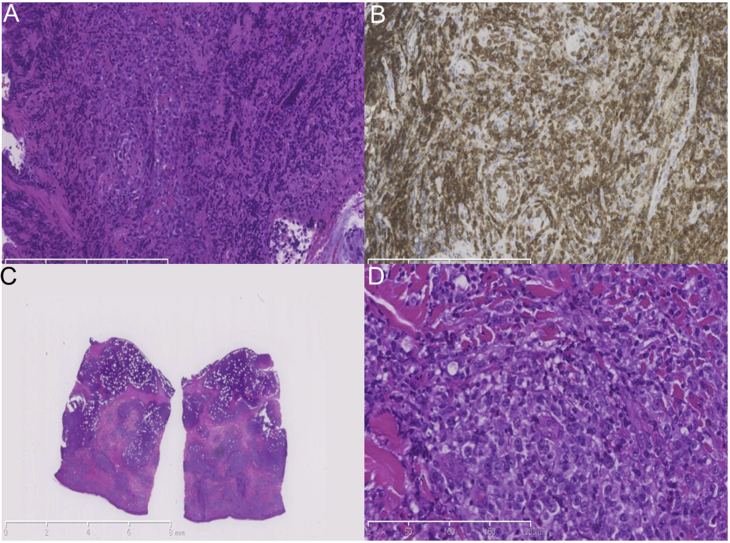
Fig. 5.
A and B are pathological findings of biopsied tissue from the mucosal lesion of the right B3 entrance (HE & CD3 staining). Submucosal invasion of medium-to large-sized atypical lymphocytes is shown. C and D are pathological findings of biopsied tissue from the subcutaneous nodule. Atypical lymphocyte infiltration similar to the bronchial lesion was found.
Fig. 6.
CT images showed the marked reduction in the right hilar mass and multiple lymphadenopathies after five cycles of chemotherapy.
3. Discussion
PTCL is a rare disease, and PTCL-NOS more frequently occurs in Japan and East Asian countries than in Western countries. It is reported that PTCL-NOS comprises 25.9% of T cell lymphomas [3]. To the best of our knowledge, there have been only two case reports describing PTCL-NOS patients with endobronchial lesion alone (reference 4 and 5), and the authors did not describe the difference of clinical characteristics between endobronchial lesion alone type and general type. Both of the two previous cases were not advanced stage and they were treated with chemotherapy with a good response [4,5]. (Table 1).
Table 1.
Literature Review of the case reports of PTCL-NOS with endobronchial lesion.
| Age (years old)/Gender | CT Findings | Stage | Treatment | Outcome |
|---|---|---|---|---|
| 81/M4) |
|
I E |
|
|
| 51/M5) |
|
IV |
|
|
| 68/M (This case) |
|
IV |
|
|
THP-COP therapy: pirarubicin, cyclophosphamide, vincristine, and prednisone.
CHOP therapy: cyclophosphamide, adriamycin, vincristine, and prednisolone.
CHASE therapy: cyclophosphamide, cytarabine, etoposide, and dexamethasone.
Generalized lymphadenopathy is the most common CT finding of PTCL-NOS. In patients with disseminated conditions, the imaging features are not distinguished from those in other subtypes of lymphoma in the disseminated state. Primary pulmonary non-Hodgkin lymphoma (NHL) has been reported to comprise 3.6% of extranodal lymphomas [6]. Only 0.05% of NHL autopsy cases have an airway lesion [7]. Previously reported cases of malignant lymphoma with airway lesions diagnosed by TBB are rare. Most of those cases are diffuse large B-cell lymphoma, pulmonary mucosa-associated lymphoid tissue lymphoma, and NK cell lymphoma. To the best of our knowledge, this is a rare case report of PTCL-NOS with an airway lesion that was diagnosed by a TBB in the English literature. The pathogenesis of an airway lesion of NHL is thought to be the following: 1) arising from the submucosal lymphoid tissue, 2) hematogenous or lymphogenous metastasis, or 3) invasion from adjacent lymph nodes. In our patient, the lesion of the right hilar lymph node might have invaded the right upper lobe bronchus. The tracheal lesion was thought to be hematogenous or lymphogenous metastasis.
Dyspnea, cough, wheeze, and hoarseness are primary symptoms of malignant lymphoma with an airway lesion. Hemoptysis is rare and very different from other intratracheal tumors, in which 66% of patients have blood-stained sputum and hemoptysis [8]. Our patient also did not have hemoptysis.
The 5- and 10-year survival rates of PTCL-NOS are 43.0% and 33.5%, respectively. The four main significant prognostic factors are age ≥60 years old, performance status (PS) 2 to 4, LDH elevation, and bone marrow invasion [9]. Furthermore, immunohistochemically, EBV and CCR4 positivity are poor prognosis factors [[10], [11], [12]]. Our patient had an Eastern Cooperative Oncology Group (ECOG) PS was 1 and CCR4 was positive. There are many case reports that tumor-only resection or regional radiotherapy was therapeutically effective for cases localized to an intratracheal lesion. Moreover, the efficacy of multimodality therapy including chemotherapy and radiation for severe airway stenosis has been reported. The present case was stage IV, and CHOP therapy was temporarily effective; however, the patient ultimately died due to septic shock after six courses of CHOP and three courses of CHASE therapy. This is the typical clinical course of PTCL-NOS. First-line chemotherapy was also effective in the two previously reported cases of PTCL-NOS with the endobronchial lesion, however, the details of the subsequent process are unknown (Table 1).
In summary, our patient's presentation was unique in that endobronchial lesions of PTCL-NOS caused atelectasis as the primary presentation. This case highlights the importance of including lymphoma in the differential diagnosis of an endobronchial lesion.
Conflicts of interest
None declared.
Funding
This work has been carried out without any grants or funds.
Consent
Witten informed consent was obtained.
Acknowledgments
We would like to express our gratitude to Dr. Masafumi Oya and Dr. Fumiyoshi Fushimi, who provided insightful comments and suggestions about the pathological findings.
References
- 1.Nakamura S., Ponzoni M., Campo E. Intravascular large B-cell lymphoma. In: Swerdlow S., Campo E., Harris N., editors. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press; Lyon: 2008. pp. 252–253. [Google Scholar]
- 2.Lee H.J., Im J.G., Goo J.M., Kim K.W., Choi B.I., Chang K.H. Peripheral T-cell lymphoma: spectrum of imaging findings with clinical and pathologic features. Radiographics. 2003;23:7–26. doi: 10.1148/rg.231025018. [DOI] [PubMed] [Google Scholar]
- 3.Vose J., Armitage J., Weisenburger D., International T-Cell Lymphoma Project International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J. Clin. Oncol. 2008 Sep 1;26:4124–4130. doi: 10.1200/JCO.2008.16.4558. [DOI] [PubMed] [Google Scholar]
- 4.Matsumoto S., Fujimoto N., Fuchimoto Y., Asano M., Yano T., Kishimoto T. Endobronchial T-cell lymphoma in a patient with chronic pyothorax. Respirol Case Rep. 2015 Jun;3:44–47. doi: 10.1002/rcr2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferrer G., Gutierrez G., Schwartz A.M., Delaney M.D. Peripheral t-cell lymphoma with endobronchial involvement. J. Bronchology Interv. Pulmonol. 2010;17:169–170. doi: 10.1097/LBR.0b013e3181da2a60. [DOI] [PubMed] [Google Scholar]
- 6.Solomonov A., Zuckerman T., Goralnik L., Ben-Arieh Y., Rowe J.M., Yigla M. Non-Hodgkin's lymphoma presenting as an endobronchial tumor: report of eight cases and literature review. Am. J. Hematol. 2008;83:416–419. doi: 10.1002/ajh.21112. [DOI] [PubMed] [Google Scholar]
- 7.Rosenberg Saul A., Diamond Henry D., Jaslowitz Bernard, Craver Lloyd F. Lymphosarcoma: a review of 1269 cases. Medicine. 1961;40:31–84. doi: 10.1097/00005792-196102000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Houston Hal E., Spencer Payne W., Harrison Edgar G., Jr., Olsen Arthur M. Primary cancers of the trachea. Arch. Surg. 1969;99:132–140. doi: 10.1001/archsurg.1969.01340140004002. [DOI] [PubMed] [Google Scholar]
- 9.Gallamini Andrea, Stelitano Caterina, Calvi Roberta, Bellei Monica, Mattei Daniele, Vitolo Umberto. Peripheral T-cell lymphoma unspecified (PTCL-U): a new prognostic model from a retrospective multicentric clinical study. Blood. 2004;103:2474–2479. doi: 10.1182/blood-2003-09-3080. [DOI] [PubMed] [Google Scholar]
- 10.Dupuis J., Emile J.F., Mounier N., Gisselbrecht C., Martin-Garcia N., Petrella T. Prognostic significance of Epstein-Barr virus in nodal peripheral T-cell lymphoma, unspecified: a Groupe d'Etude des Lymphomes de l'Adulte (GELA) study. Blood. 2006;108:4163–4169. doi: 10.1182/blood-2006-04-017632. [DOI] [PubMed] [Google Scholar]
- 11.Asano Naoko, Suzuki Ritsuro, Ohshima Koichi, Kagami Yoshitoyo, Ishida Fumihiro, Yoshino Tadashi. Linkage of expression of chemokine receptors (CXCR3 and CCR4) and cytotoxic molecules in peripheral T cell lymphoma, not otherwise specified and ALK-negative anaplastic large cell lymphoma. Int. J. Hematol. 2010;91:426–435. doi: 10.1007/s12185-010-0513-0. [DOI] [PubMed] [Google Scholar]
- 12.Ishida Takashi, Inagaki Hiroshi, Utsunomiya Atae, Takatsuka Yoshifusa, Komatsu Hirokazu, Iida Shinsuke. CXC chemokine receptor 3 and CC chemokine receptor 4 expression in t-cell and NK-cell lymphomas with special reference to clinicopathological significance for peripheral t-cell lymphoma, Unspecified. Clin. Canc. Res. 2004;10:5494–5500. doi: 10.1158/1078-0432.CCR-04-0371. [DOI] [PubMed] [Google Scholar]