Pain control can be maintained in Japanese cancer patients switching from morphine to hydromorphone at conversion ratios of both 1:5 and 1:8.
Keywords: hydromorphone, morphine, cancer pain, opioid switching, conversion ratio, efficacy ratio
Abstract
Objective
To confirm the morphine to hydromorphone conversion ratio for hydromorphone (DS-7113b) immediate-release tablets in cancer patients who achieved pain control with oral morphine.
Methods
This was a multicenter, active-controlled, randomized, double-blind, parallel-group, comparative study (July 2013 to December 2014) at 39 Japanese sites. Seventy-one patients (aged >20 years) who had achieved pain control with morphine 60 mg/day and 90 mg/day were randomly allocated 1:1 to hydromorphone immediate-release tablets at a dose converted at a hydromorphone:morphine ratio of 1:5 or 1:8, respectively, and treated for up to 5 days. The efficacy was evaluated as the pain control ratio.
Results
The pain control ratio in the full analysis set was 83.3% (25/30) in the conversion ratio 1:5 group and 95.0% (38/40) in the conversion ratio 1:8 group, and both groups demonstrated highly successful pain control. The incidence of adverse events was 46.7% (14/30) in the conversion ratio 1:5 group and 58.5% (24/41) in the 1:8 group; the difference was not clinically relevant. Frequently observed adverse events (incidence ≥5%) were nausea, vomiting, diarrhea, somnolence and dyspnea.
Conclusions
A high pain control ratio was maintained by a switch at either conversion ratio, and no notable difference was observed in the incidence of adverse events. A switch from morphine to hydromorphone is effective at a dose converted at ratios of 1:5 and 1:8.
Introduction
The ‘three-step ladder for cancer pain relief’ from the World Health Organization Guidelines recommends the use of Step 3 opioid analgesics for moderate to severe pain (1), as they are the most effective for relieving cancer pain and can provide successful pain control (2). Morphine, oxycodone, and fentanyl are currently used in Japan as Step 3 opioid analgesics (3).
The selective μ-opioid receptor agonist analgesic hydromorphone is currently used clinically in 45 countries and regions in the world (4); however, despite being a standard alternative for morphine (5–8), hydromorphone has not been developed for use in Japan. The metabolites of hydromorphone are inactive (9), so it could potentially be used for patients with renal impairment who cannot tolerate morphine, and its approval in Japan would increase the treatment options for pain relief.
There is no fixed opioid dose for cancer pain relief. The appropriate dose for each patient is considered to be that which produces a successful analgesic effect with tolerable adverse drug reactions. The converted dose is customarily calculated at the time of opioid switching for each opioid based on its conversion ratio from morphine, the standard drug. This is because of a lack of guidelines for established doses for other opioids. As shown in Tables 1 and 2, several conversion ratios of morphine to hydromorphone have been reported and range between 2.7- and 8-fold (10), so a definite ratio has not been established. A ratio of ~1:5 has been reported in many papers (6,11–16), while a conversion ratio of 1:8 (or 1:7.5) reportedly decreases the exposure (1,7,17,18). We therefore conducted a study in Japanese cancer patients to confirm the morphine to hydromorphone conversion ratio for hydromorphone immediate-release tablets and to confirm pain control by opioid switching using these two typical conversion ratios.
Table 1.
Conversion ratios in various textbooks/guidelines
| Text/guideline | Morphine | Hydromorphone | Conversion ratio | Year of publication |
|---|---|---|---|---|
| Principles of Analgesic use in the Treatment of Acute Pain and Cancer Pain (26) | 30 mg | 7.5 mg | 1:4a | 2008 |
| Bonica’s Management of Pain (27) | 30 mg | 7.5 mg | 1:4a | 2010 |
| 60 mg | 6–8 mg | 1:3.75–5a | ||
| Oxford Textbook of Palliative Medicine 4th edition (10) | – | – | 1:7.5 | 2010 |
| 20–60 mgc | 7.5 mg | 1:2.7–8a | ||
| Opioid Therapy in the 21st Century (28) | 30 mg | 7.5 mg | 1:4a | 2013 |
| Palliative Care Formulary 5th edition (11) | 1 mg | 4–5 mg (5–7.5 mg)b | 1:5 | 2014 |
| WHO Cancer Pain Relief 2nd edition (1) | – | – | ≈8-fold | 1996 |
| ESMO: Management of cancer pain (7) | 1 mg | 7.5 mg | 1:7.5 | 2011d |
| EAPC: Use of Opioid Analgesics in the Treatment of Cancer Pain (6) | 1 mg | 5 mg | 1:5 | 2012 |
| NCCN: Adult Cancer Pain (8) | 30 mg | 7.5 mg | 1:4 | 2016 |
aConversion ratio converted by the actual dose.
bThe values in the parentheses are the conversion ratios reported by the pharmaceutical company, with the content excerpted directly from the footnotes of the guidelines.
cExtensive survey data suggest that the relative potency of intramuscular:oral or subcutaneous:oral morphine of 1:6 changes to 1:2–3 with chronic dosing.
dThe latest edition, issued in 2012, includes no information on conversion ratio.
Table 2.
Conversion ratios reported by clinical studies and observational studies
| Author(s) | Study design | Number of subjects | Conversion ratio | Journal | Year of publication |
|---|---|---|---|---|---|
| Bruera E (12) | Retrospective | 733 | 1:5.33a | Cancer | 1996 |
| Lawlor P (13) | Retrospective | 207 | 1:5.76a | Pain | 1997 |
| Moriarty M (17) | Blinded, crossover | 100 | 1:7.5 | J Clin Res | 1999 |
| Palangio M (14) | Multicenter, joint, open-label | 445 | 1:5 | J Pain Symptom Manage | 2002 |
| Weinstein SM (18) | Multicenter, joint, open-label | 343 | 1:8 | Clin Ther | 2006 |
| Wirz S (16) | Prospective observational | 50 | 1:5 | Clin J Pain | 2006 |
| Wallace M (15) | Multicenter, joint, open-label | 148 | 1:5 | J Int Med Res | 2008 |
aConversion ratio converted by the actual dose.
Patients and methods
This study was conducted from July 2013 to December 2014 as a multicenter, active-controlled, randomized, double-blind, parallel-group comparison study, enrolling 71 patients at 39 sites in Japan (participating sites are listed in Supplemental File 1). The study was approved by the Institutional Review Board of each study site and was conducted in accordance with the ethical principles of the Declaration of Helsinki and Good Clinical Practice. Written informed consent was obtained from all subjects prior to study participation.
Participants
The study participants were cancer patients over 20 years of age receiving opioid analgesics for pain relief in whom pain control was achieved with regular administration of oral morphine either at 60 mg/day or 90 mg/day for at least 3 days before enrollment. Pain control was defined as patients reporting a pain intensity score of 0 (none) or 1 (mild) and administered rescue medication no more than twice daily. Exclusion criteria included patients for whom morphine is contraindicated or relatively contraindicated, patients receiving treatment with a monoamine oxidase inhibitor within 14 days of registration, patients participating in another clinical trial within 28 days of registration, and patients with serious hepatic, renal or respiratory disorders of Common Terminology Criteria for Adverse Events Grade 3.
Study design
Patients that had achieved pain control by administration of morphine were randomly allocated 1:1 to hydromorphone immediate-release tablets (DS-7113b; Daiichi Sankyo, Tokyo, Japan) at a conversion ratio of either 1:5 or 1:8. The study drug was provided by Daiichi Sankyo Co., Ltd. The computer-generated random allocation sequence was provided by Bell Medical Solutions Inc. (Tokyo, Japan), and was stratified according to the daily morphine dose prior to beginning the study (60 or 90 mg/day). A double-dummy method was employed for blinding, and subjects in the conversion ratio 1:5 group received 12 mg/day of hydromorphone when their oral morphine dose was 60 mg/day during the pre-treatment observation period, and hydromorphone 18 mg/day when their oral morphine dose was 90 mg/day. Similarly, the subjects in the conversion ratio 1:8 group received hydromorphone 7.5 mg/day (oral morphine dose at 60 mg/day during the pre-treatment observation period) or 12 mg/day (oral morphine dose at 90 mg/day during the pre-treatment observation period). The dose of study drug was to remain unchanged and the study was discontinued as ‘pain control not maintained’ if a dose increase or decrease was required. The study drug was administered if pain control was maintained, or for 5 days, whichever was shorter. The study drug was orally administered six times daily in both groups with two tablets of the active drug with or without additional placebo tablets to maintain blinding, as one dose, but administration of two doses before retiring was allowed in cases where midnight administration would be difficult. Treatment was switched to appropriate analgesics after achieving pain control or completion of study drug administration, and the post-study observation was conducted.
Every day from baseline to treatment completion (or discontinuation), patients evaluated their mean pain severity over the previous 24 h using a 4-step pain intensity scale [‘0, none’, ‘1, mild’, ‘2, moderate’, ‘3, severe’], and visual analog scale (VAS) and recorded their score in a diary once daily at a predetermined time. Sleep was evaluated on a 4-point scale: 0 = very unsatisfactory or did not sleep at all; 1 = markedly unsatisfactory; 2 = slightly unsatisfactory; 3 = satisfactory.
Oral morphine hydrochloride solution was used as rescue medication when additional analgesia was required because of breakthrough pain. However, the following were prohibited throughout the study: co-administration of a monoamine oxidase inhibitor, opioid analgesics other than rescue medication, and narcotic antagonists. Similarly, new administration of systemic non-opioid analgesics, supplementary analgesics, bisphosphonates, anti-RANKL antibody preparations and changes in dosage and administration were prohibited. New initiation of radiotherapy, nerve block, percutaneous vertebroplasty, surgery, or cancer chemotherapy or immunotherapy was also prohibited.
Outcomes
The primary efficacy endpoint was the pain control ratio. The criteria for pain control were satisfaction for 2 days in all of the following items: study treatment continued at the same dose; pain intensity either ‘0, none’ or ‘1, mild’; and administration of rescue medication twice daily or less.
Secondary efficacy endpoints were changes in VAS and sleep evaluation on each evaluation day, number of days required to achieve pain control, and use of rescue medication. Sleep evaluation was performed immediately prior to study drug administration, each day during the study, 2 days after the study, and if/when patients discontinued. Safety endpoints were adverse events, laboratory data, vital signs and 12-lead electrocardiogram (ECG).
Statistical analysis
The sample size was calculated based on the assumptions that the pain control ratio would be 90% for the 1:5 group and 80% for the 1:8 group. The target sample size was determined with reference to previous clinical studies of oxycodone in Japan. Based on these results, the pain control ratio was estimated to be 85–90% in patients that were switched with an appropriate conversion ratio. If the pain control ratio in the conversion ratio 1:5 group was also between 85% and 90%, it was estimated that the pain control ratio would be 10–20% lower in the conversion ratio 1:8 group. This was examined using 100,000 Monte Carlo simulations; therefore, 35 subjects in each group were required to achieve a probability of >80% for obtaining a difference of ≥10% when the difference in the true pain control ratio was 20%, and for obtaining a difference of ≥0% when the difference in the true pain control ratio was 10%. On this basis, 35 patients in each group were required to achieve a >80% pain control ratio that would be used to detect the difference of the point estimates between groups (conversion ratio 1:5 group > conversion ratio 1:8 group).
In the efficacy analysis, the full analysis set (FAS) based on the intention-to-treat principle was defined as the primary analysis set. The primary analysis was to calculate the pain control ratio and its 95% confidence interval (CI) for each group. Fisher’s exact test was used to compare the pain control ratio between groups, and the difference in the pain control ratio (conversion ratio 1:5 group − conversion ratio 1:8 group) and its 95% CI (two-sided, normal approximation) were calculated. The number of days required to achieve pain control in each group was calculated.
As secondary analyses, summary statistics were calculated for the change in VAS scores at treatment completion/discontinuation from baseline. Analysis of covariance (ANCOVA) was also conducted using the baseline VAS scores as a covariate, and difference in the least square means (conversion ratio 1:5 group − conversion ratio 1:8 group) and its 95% confidence interval (two-sided), and corresponding P value were calculated. As sleep data analyses, the Wilcoxon rank-sum test was used to compare groups at completion of treatment/discontinuation. SAS System Release 9.2 (SAS Inc., Cary, NC, USA) was used for statistical analysis.
Results
Patients and treatment exposure
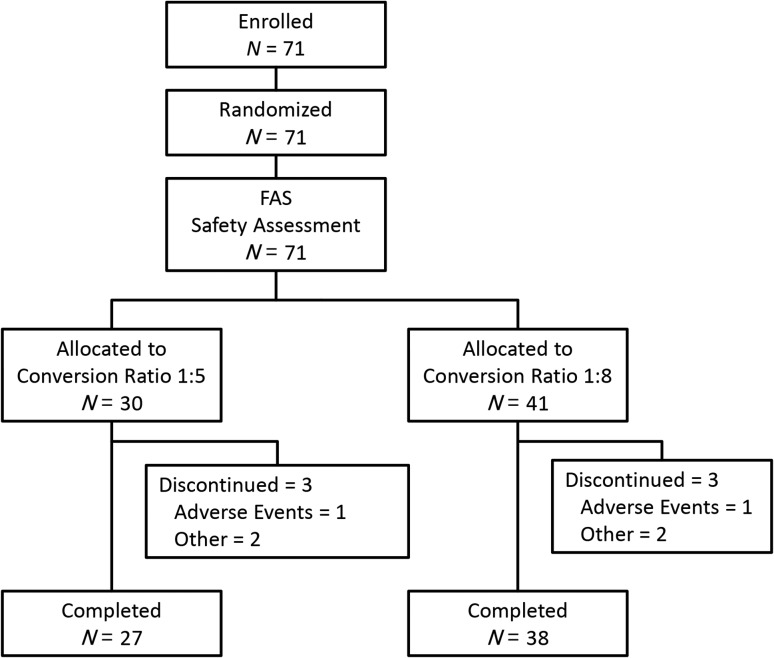
Figure 1 shows patient disposition. Enrolled patients were randomly allocated—30 to the conversion ratio 1:5 group and 41 to the conversion ratio 1:8 group—and all received the study drug. Of these, 27 in the conversion ratio 1:5 group and 38 in the conversion ratio 1:8 group completed the study. Although random allocation was performed following correct procedures, this imbalance in the number of patients between groups occurred by chance. Three subjects in each group discontinued the study, and the main reasons for study discontinuation were adverse events and withdrawal of consent.
Figure 1.
Patient disposition.
A total of 70 subjects were included in the FAS after excluding one subject in the conversion ratio 1:8 group for whom evaluable efficacy data were not available. Table 3 shows the demographics of the FAS. Approximately 85% of the conversion ratio 1:5 group was male compared with 60% of the conversion ratio 1:8 group. Subjects with a pain intensity score of 1 accounted for ~55% of the 1:5 and 70% of the 1:8 groups. No significant intergroup difference was observed for other items. Almost 80% of the subjects received the oral morphine dose of 60 mg/day and ~20% received the dose of 90 mg/day.
Table 3.
Baseline demographic and clinical characteristics
| Conversion ratio 1:5 group N = 30 | Conversion ratio 1:8 group N = 40 | ||
|---|---|---|---|
| Age (years) | Mean ± SD | 65.2 ± 11.22 | 66.1 ± 9.10 |
| Sex, n (%) | M | 26 (86.7) | 25 (62.5) |
| F | 4 (13.3) | 15 (37.5) | |
| Body weight (kg) | Mean ± SD | 53.23 ± 10.319 | 51.61 ± 9.065 |
| BMI (kg/m2) | Mean ± SD | 19.93 ± 3.339a | 20.01 ± 2.859 |
| Underlying tumor type, n (%) | Head and neck | 0 (0.0) | 1 (2.5) |
| Lung | 15 (50.0) | 21 (52.5) | |
| Breast | 3 (10.0) | 5 (12.5) | |
| Gastrointestinal | 10 (33.3) | 4 (10.0) | |
| Liver/gallbladder/pancreatic | 0 (0.0) | 1 (2.5) | |
| Urinary/reproductive organs | 1 (3.3) | 5 (12.5) | |
| Other | 1 (3.3) | 3 (7.5) | |
| ECOG PS, n (%) | 0 | 6 (20.0) | 13 (32.5) |
| 1 | 13 (43.3) | 20 (50.0) | |
| 2 | 6 (20.0) | 6 (15.0) | |
| 3 | 5 (16.7) | 1 (2.5) | |
| 4 | 0 (0.0) | 0 (0.0) | |
| VAS score (mm) | Mean ± SD | 15.3 ± 12.61 | 14.0 ± 10.48 |
| Pain intensity, n (%) | 0. None (not painful) | 13 (43.3) | 12 (30.0) |
| 1. Mild (somewhat painful) | 17 (56.7) | 28 (70.0) | |
| 2. Moderate (painful) | 0 (0.0) | 0 (0.0) | |
| 3. Severe (very painful) | 0 (0.0) | 0 (0.0) | |
| Pre-study oral morphine dose, n (%) | 60 mg/day | 24 (80.0) | 33 (82.5) |
| 90 mg/day | 6 (20.0) | 7 (17.5) |
BMI, body mass index; ECOG PS, Eastern Cooperative Oncology Group Performance Status; SD, standard deviation; VAS, visual analog scale.
Efficacy
The pain control ratio in the FAS was 83.3% (25/30) in the conversion ratio 1:5 group and 95.0% (38/40) in the conversion ratio 1:8 group, with a high pain control ratio maintained in both groups (Table 4). The intergroup difference in the pain control ratio (95% CI) was −11.7% (−26.6 to 3.3), which was not statistically significant (Fisher’s exact test: P = 0.1298). Pain control was not maintained in seven subjects (conversion ratio 1:5 group: 5, conversion ratio 1:8 group: 2). This was owing to non-response in three subjects (conversion ratio 1:5 group: 2; conversion ratio 1:8 group: 1), discontinuation due to onset of adverse drug reactions in two subjects (one patient in each group), withdrawal of consent by one subject (1:5 group), and non-achievement due to deviation from pain evaluation window in one subject (1:5 group).
Table 4.
Successful pain control ratio (FAS)
| N | Successful pain control n (%, achievement ratio) | 95% CI | Intergroup differencea | 95% CI for intergroup difference | P valueb | |
|---|---|---|---|---|---|---|
| Conversion ratio 1:5 group | 30 | 25 (83.3) | (65.3–94.4) | −11.7 | (−26.6–3.3) | 0.1298 |
| Conversion ratio 1:8 group | 40 | 38 (95.0) | (83.1–99.4) |
aConversion ratio 1:5 group − conversion ratio 1:8 group.
bFisher’s exact method.
CI, confidence interval; FAS, full analysis set.
Table 5 shows the number of days required for achieving pain control in each group in the FAS. Pain control was maintained on Day 2 in >80% of the subjects in both groups.
Table 5.
Number of days required for achievement of pain control (FAS)
| n (%) | Conversion ratio 1:5 group (N = 30) | Conversion ratio 1:8 group (N = 40) |
|---|---|---|
| Number of achievers | 25 (83.3) | 38 (95.0) |
| Day 2 | 24 (80.0) | 37 (92.5) |
| Day 3 | 0 | 1 (2.5) |
| Day 4 | 1 (3.3) | 0 |
| Day 5 | 0 | 0 |
| Number of non-achievers | 5 (16.7) | 2 (5.0) |
FAS, full analysis set.
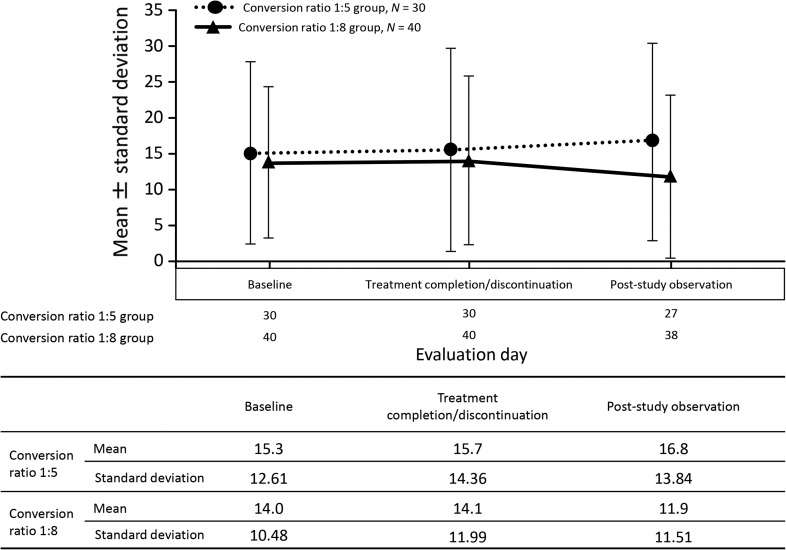
Table 6 shows the results of the ANCOVA of the magnitude of change in VAS score at treatment completion/discontinuation in the FAS. Figure 2 shows a transition diagram of VAS score in the FAS.
Table 6.
ANCOVA of the change in VAS score (treatment completion/discontinuation) (FAS)
| Conversion ratio 1:5 group (N = 30) | Conversion ratio 1:8 group (N = 40) | |
|---|---|---|
| Mean ± standard deviation | 0.4 ± 10.47 | 0.2 ± 7.73 |
| Minimum | −20 | −12 |
| Median | 0.0 | 0.0 |
| Maximum | 47 | 37 |
| Least square mean | 0.6 | 0.1 |
| Difference in least square meana | 0.5 | |
| 95% confidence interval | (−3.8–4.8) | |
| P value | 0.8287 |
aConversion ratio 1:5 group − conversion ratio 1:8 group.
ANCOVA, analysis of covariance; FAS, full analysis set.
Figure 2.
Changes in visual analog scale scores in the full analysis set (FAS).
The mean (±standard deviation) magnitude of change in VAS score at treatment completion/discontinuation in the FAS was 0.4 ± 10.47 mm in the conversion ratio 1:5 group and 0.2 ± 7.73 mm in the conversion ratio 1:8 group, showing little change in VAS score from baseline in either group. The difference in least square mean (95% CI) was 0.5 mm (−3.8 to 4.8), which was not statistically significant and indicated no intergroup difference (ANCOVA: P = 0.8287). VAS score did not increase after switching from morphine to hydromorphone in either group, and pain remained favorably controlled at completion/discontinuation of hydromorphone therapy.
Tabulation of daily use of rescue medication in the FAS showed that the frequency of use was 0 or once in more than 80% of the subjects in both groups on each observation day up to Day 3. The mean frequency of daily use of rescue medication after the start of administration on Day 1 up to Day 3 was less than once in both groups, and the frequency of use of rescue medication was not greatly increased compared with baseline use of oral morphine hydrochloride solution.
Table 7 shows the cross-frequency table of sleep assessment in the FAS at treatment completion/discontinuation. More than 70% of the subjects in both groups were assessed as either ‘2, slightly unsatisfactory’ or ‘3, satisfactory’, and no subject was assessed as aggravated compared with baseline. A comparison of sleep quality assessments between groups revealed no significant difference in the score at treatment completion/discontinuation (Wilcoxon’s rank-sum test: P = 0.7303).
Table 7.
Analysis of sleep quality assessment (cross-frequency table)
| Baseline | Treatment completion/discontinuation | Total n (%) | P valuea | P valueb | ||||
|---|---|---|---|---|---|---|---|---|
| 0. Very unsatisfactory or did not sleep at all | 1. Markedly unsatisfactory | 2. Slightly unsatisfactory | 3. Satisfactory | |||||
| Conversion ratio 1:5 group (N = 30) | 0. Very unsatisfactory or did not sleep at all | 0 | 1 | 0 | 0 | 1 (3.3) | 0.3667 | 0.7303 |
| 1. Markedly unsatisfactory | 0 | 3 | 3 | 2 | 8 (26.7) | |||
| 2. Slightly unsatisfactory | 0 | 4 | 8 | 1 | 13 (43.3) | |||
| 3. Satisfactory | 0 | 0 | 1 | 7 | 8 (26.7) | |||
| Total n (%) | 0 (0.0) | 8 (26.7) | 12 (40.0) | 10 (33.3) | 30 | |||
| Conversion ratio 1:8 group (N = 40) | 0. Very unsatisfactory or did not sleep at all | 0 | 0 | 0 | 0 | 0 (0.0) | 0.2657 | |
| 1. Markedly unsatisfactory | 0 | 0 | 1 | 0 | 1 (2.5) | |||
| 2. Slightly unsatisfactory | 1 | 4 | 17 | 5 | 27 (67.5) | |||
| 3. Satisfactory | 0 | 0 | 6 | 6 | 12 (30.0) | |||
| Total n (%) | 1 (2.5) | 4 (10.0) | 24 (60.0) | 11 (27.5) | 40 | |||
aWilcoxon’s signed rank test.
bWilcoxon’s rank-sum test.
Safety and tolerability
All 71 randomized subjects who received the study drug (30 in the conversion ratio 1:5 group and 41 in the conversion ratio 1:8 group) were included in the safety analysis. The incidence of adverse events was 46.7% (14/30) in the conversion ratio 1:5 group and 58.5% (24/41) in the conversion ratio 1:8 group, showing no significant intergroup difference. Frequently observed adverse events (incidence of ≥5%, Table 8) were nausea, vomiting, diarrhea, somnolence and dyspnea.
Table 8.
Adverse events with incidence ≥5%
| SOC PT | Conversion ratio 1:5 group N = 30 | Conversion ratio 1:8 group N = 41 |
|---|---|---|
| Number of subjects who developed adverse events (%) | 14 (46.7) | 24 (58.5) |
| Nausea | 2 (6.7) | 6 (14.6) |
| Vomiting | 2 (6.7) | 3 (7.3) |
| Somnolence | 3 (10.0) | 2 (4.9) |
| Diarrhea | 0 (0.0) | 4 (9.8) |
| Dyspnea | 2 (6.7) | 0 (0.0) |
SOC, system organ class; PT, preferred term.
The incidence of serious adverse events was 10.0% (3/30) in the conversion ratio 1:5 group and 9.8% (4/41) in the conversion ratio 1:8 group, showing no significant intergroup difference. Of these, events judged to be causally related to the study drug were observed in one subject (stupor) in the conversion ratio 1:5 group and three subjects (enterocolitis, ileus and nausea in one subject each) in the conversion ratio 1:8 group. All patients had recovered by the study completion.
There were no notable changes in laboratory data or vital signs, and evaluation of 12-lead ECG did not show clinically problematic QT prolongation.
Discussion
This study investigated the efficacy and safety of switching from morphine to hydromorphone immediate-release tablets at the conversion ratio of 1:5 or 1:8 in cancer patients with adequate pain control with oral morphine at 60 or 90 mg/day. The pain control ratio in the FAS, the primary efficacy endpoint, was 83.3% (25/30) in the conversion ratio 1:5 group and 95.0% (38/40) in the conversion ratio 1:8 group. The point estimate of the pain control ratio was higher in the 1:8 group than that in the 1:5 group. While no statistically significant difference was observed, these results did not support our initial hypothesis (of a higher pain control ratio in the 1:5 group than in the 1:8 group), but demonstrated high pain control ratios in both groups. No intergroup difference was observed in the incidence of adverse events, and the results did not greatly differ from those of previous reports (19,20).
The subjects in this study were randomized at a 1:1 ratio but 41 and 30 patients were allocated to the conversion ratio 1:8 and 1:5 groups, respectively. The imbalance in the allocated number of subjects would not affect evaluation of efficacy and safety because the random allocation was conducted according to the correct procedures. The imbalance in the number of subjects occurred by chance.
Although indexes of efficacy are not the same because they are also used for patients with non-cancer pain, the pain control ratio ranged between 50% and 84% in reports that evaluated pain control at the time of opioid switching (21–24). The pain control ratios (83.3% and 95.0% in the conversion ratio 1:5 and 1:8 groups, respectively) in this study were comparable to those in the above reports, and efficacy was confirmed to be clinically unproblematic. Both groups showed high pain control after switching to hydromorphone in VAS scores as the secondary endpoint and no intergroup difference was observed.
Prior to clinical use in Japan, the conversion ratios versus morphine ranged widely from 2.7- to 8-fold, so a more appropriate conversion ratio had to be confirmed. Based on the dose conversion ratios of 1:5 for the currently marketed hydromorphone products Exalgo (19) and Jurnista (20), 1:7.5 for Palladone (25), and ~1:8 recommended in the WHO guidelines (1), we investigated two groups with conversion ratios of 1:5 and 1:8 in this study. Some reports investigated the conversion ratio at switching, whereas others investigated the conversion ratio based on the final dose and the subsequent dose adjustment period. We evaluated pain control at the time of switching for the purpose of confirming information for safely conducting opioid switching. The results in both groups in our study showed that opioid switching was not clinically problematic, so the conversion ratio of hydromorphone from morphine was determined in the range of 1:5 and 1:8, and effective and safe switching was considered possible by calculating the converted dose. These findings indicate that the conversion ratio from morphine falls in the range of 1:5–1:8, suggesting that the conversion ratio to hydromorphone is not fixed to a specific value but can vary within a certain range. This range is consistent with any conversion ratios (1:5 for Exalgo, Jurnista, etc. and 1:7.5 for Palladone) calculated based on the converted doses listed in the package inserts of currently marketed hydromorphone formulations. However, the optimal dose after switching should be determined at the time of actual opioid switching and should include considerations of the reasons for switching and patients’ conditions, rather than by a mere numerical conversion using the conversion ratio.
This study has some limitations. First, our data do not apply to patients requiring opioid switching in a clinical situation, because the subjects in our study had achieved pain control with morphine and had no safety problems. Second, the study was designed to switch the total morphine dose to hydromorphone only in patients receiving daily morphine doses of 60 or 90 mg, and switching at high doses exceeding morphine 90 mg/day and stepwise switching were not investigated. Finally, the study was completed by confirming successful pain control after switching, and the relationship with the optimal dose after switching, including subsequent titration, was not investigated.
Conclusions
Successful pain control was maintained when switching from morphine to hydromorphone with a conversion ratio of 1:5 or 1:8 in Japanese cancer patients who had achieved pain control with oral morphine, with no significant difference between groups. No intergroup difference was observed in the incidence of adverse events or serious adverse events. A conversion ratio between 1:5 and 1:8 is considered clinically appropriate for a switch from morphine to hydromorphone for pain control in cancer patients.
Supplementary Material
Acknowledgements
The authors thank all of the investigators at the participating centers for their contributions to this study (this information is available in Supplementary Data File 1). Supplemental Files: 1 (Microsoft Word document list of participating centers and institutes)
Supplementary data
Supplementary data are available at Japanese Journal of Clinical Oncology online.
Funding
This work was supported by Daiichi Sankyo Company, which paid for all expenses related to preparation of this report and study implementation.
Conflict of interest statement
Yoji Saito was involved in this study as a medical specialist. Satoru Tsuneto and Etsuko Aruga were involved in this study as safety evaluation advisors. Satoshi Inoue, Takeshi Ogata, and Mitsutoshi Uemori are employees of Daiichi Sankyo Co., Ltd. Yoji Saito, Satoru Tsuneto and Etsuko Aruga has received personal fees from Daiichi Sankyo Co., Ltd.
Abbreviations
ANCOVA, analysis of covariance; BMI, body mass index; CI, confidence interval; ECG, electrocardiogram; ECOG PS, Eastern Cooperative Oncology Group performance status; FAS, full analysis set; PPS, per-protocol set; PT, preferred term; SOC, system organ class; SD, standard deviation; VAS, visual analog scale.
References
- 1. World Health Organization Cancer Pain Relief: With a Guide to Opioid Availability. 2nd edn Geneva: World Health Organization, 1996; http://apps.who.int/iris/bitstream/10665/37896/1/9241544821.pdf. [Google Scholar]
- 2. Zech DF, Grond S, Lynch J, et al. Validation of World Health Organization Guidelines for cancer pain relief: a 10-year prospective study. Pain 1995;63:65–76. [DOI] [PubMed] [Google Scholar]
- 3. Hastie BA, Gilson AM, Maurer MA, Cleary JF. An examination of global and regional opioid consumption trends 1980––011. J Pain Palliat Care Pharmacother 2014;28:259–75. [DOI] [PubMed] [Google Scholar]
- 4. International Narcotics Control Board REPORT 2013. Available from: http://www.incb.org/documents/Narcotic-Drugs/Technical-Publications/2013/Part_4_tables_EFS.pdf.
- 5. Hanks GW, Conno F, Cherny N, et al. Morphine and alternative opioids in cancer pain: the EAPC recommendations. Br J Cancer 2001;84:587–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Caraceni A, Hanks G, Kaasa S, et al. Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol 2012;13:e58–68. [DOI] [PubMed] [Google Scholar]
- 7. Ripamonti CI, Santini D, Maranzano E, et al. ESMO Guidelines Working Group Management of cancer pain: ESMO Clinical Practice Guidelines. Ann Oncol 2012;23:vii139–54. [DOI] [PubMed] [Google Scholar]
- 8. National Comprehensive Cancer Network Adult cancer pain. Version 2. 2012. Available from: http://www.nccn.org/professionals/physician_gls/pdf/pain.pdf.
- 9. Johnson SJ. Opioid safety in patients with renal or hepatic dysfunction. Pain Treatment Topics. 2007. Nov. Available at: http://paincommunity.org/blog/wp-content/uploads/Opioids-Renal-Hepatic-Dysfunction.pdf (22 August 2016, date last accessed).
- 10. Hanks G, Cherny NL, Christakis NA, et al., editors. Oxford Textbook of Palliative Medicine. 4th edn Oxford: Oxford University Press, 2010. [Google Scholar]
- 11. Twycross R, Wilcock A, Howard P, editors. Palliative Care Formulary. 5th edn Nottingham: Palliativecare.com Ltd, 2014. [Google Scholar]
- 12. Bruera E, Pereira J, Watanabe S. Opioid rotation in patients with cancer pain. A retrospective comparison of dose ratios between methadone, hydromorphone, and morphine. Cancer 1996;78:852–7. [DOI] [PubMed] [Google Scholar]
- 13. Lawlor P, Turner K, Hanson J, Bruera E. Dose ratio between morphine and hydromorphone in patients with cancer pain: a retrospective study. Pain 1997;72:79–85. [DOI] [PubMed] [Google Scholar]
- 14. Palangio M, Northfelt DW, Portenoy RK, et al. Dose conversion and titration with a novel, once-daily, OROS osmotic technology, extended-release hydromorphone formulation in the treatment of chronic malignant or nonmalignant pain. J Pain Symptom Manage 2002;23:355–68. [DOI] [PubMed] [Google Scholar]
- 15. Wallace M, Rauck RL, Moulin D, et al. Conversion from standard opioid therapy to once-daily oral extended-release hydromorphone in patients with chronic cancer pain. J Int Med Res 2008;36:343–52. [DOI] [PubMed] [Google Scholar]
- 16. Wirz S, Wartenberg HC, Elsen C, et al. Managing cancer pain and symptoms of outpatients by rotation to sustained-release hydromorphone: a prospective clinical trial. Clin J Pain 2006;22:770–5. [DOI] [PubMed] [Google Scholar]
- 17. Moriarty M, McDonald CJ, Miller AJ. A randomized crossover comparison of controlled release hydromorphone tablets with controlled release morphine tablets in patients with cancer pain. J Clin Res 1999;2:1–8. [Google Scholar]
- 18. Weinstein SM, Shi M, Buckley BJ, Kwarcinski MA. Multicenter, open-label, prospective evaluation of the conversion from previous opioid analgesics to extended-release hydromorphone administered every 24 hours to patients with persistent moderate to severe pain. Clin Ther 2006;28:86–98. [DOI] [PubMed] [Google Scholar]
- 19. Mallinckrodt Brand Pharmaceuticals EXALGO® (hydromorphone HCl) extended-release tablets. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/021217s009lbl.pdf.
- 20. JANSSEN-CILAG Pty Ltd Jurnista® Prolonged Release Tablets. Product Information. Available from: http://www.janssen.com/australia/sites/www_janssen_com_australia/files/product/pdf/jurnista_pi.pdf.
- 21. Mercadante S, Bruera E. Opioid switching: a systematic and critical review. Cancer Treat Rev 2006;32:304–15. [DOI] [PubMed] [Google Scholar]
- 22. Narabayashi M, Saijo Y, Takenoshita S, et al. Advisory Committee for Oxycodone Study. Opioid rotation from oral morphine to oral oxycodone in cancer patients with intolerable adverse effects: an open-label trial. Jpn J Clin Oncol 2008;38:296–304. [DOI] [PubMed] [Google Scholar]
- 23. Riley J, Ross JR, Rutter D, et al. No pain relief from morphine? Individual variation in sensitivity to morphine and the need to switch to an alternative opioid in cancer patients. Support Care Cancer 2006;14:56–64. [DOI] [PubMed] [Google Scholar]
- 24. Dale O, Moksnes K, Kaasa S. European Palliative Care Research Collaborative pain guidelines: opioid switching to improve analgesia or reduce side effects. A systematic review. Palliat Med 2011;25:494–503. [DOI] [PubMed] [Google Scholar]
- 25. Napp Pharmaceuticals Limited Palladone capsules. Available from: http://www.medicines.org.uk/emc/document.aspx?documentid=1227&docType=SPC (22 August 2016, date last accessed).
- 26. American Pain Society Principles of Analgesic Use in the Treatment of Acute Pain and Cancer Pain. 6th edn Glenview, IL: American Pain Society, 2008. [Google Scholar]
- 27. Fishman SM, Ballantyne JC, Rathmell JP, editors. Bonica’s Management of Pain. 4th edn Philadelphia: Lippincott, Williams and Wilkins, 2010. [Google Scholar]
- 28. Fallon M, Cherny NI, Hanks G. Opioid analgesic therapy In: Smith HS, editor. Opioid Therapy in the 21st Century. 2nd edn New York: Oxford University Press, 2014;661–98. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.