Abstract
Introduction
Bosniak introduced a classification of renal cysts based on imaging characteristics. Cystic renal changes are categorized determining their risk of malignancy and further management. However, defining the malignancy of category III lesions still remains a challenge and our aim was to evaluate the features of malignancy in computed tomography within this category.
Material and methods
The Vilnius University Hospital Santariškių Klinikos information system was retrospectively searched for computed tomography examinations in which Bosniak category III lesions were reported. Data of genetic disorders and history of malignancy were collected. Longest diameter, location, shape, amount and location of calcification, contrast enhancement of Bosniak category III lesions were evaluated. The relation between collected data and malignancy was estimated.
RESULTS
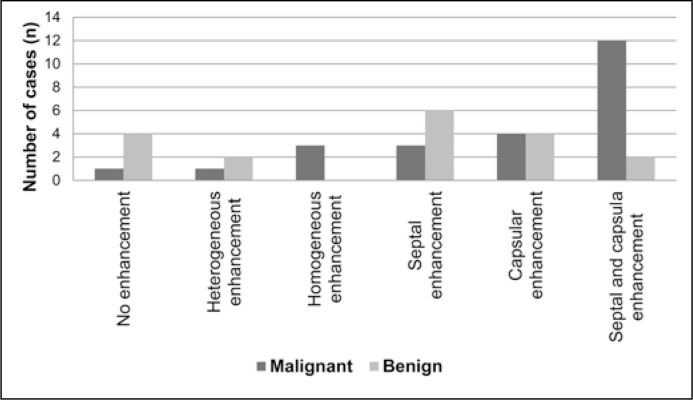
There were 73 patients with Bosniak category III lesions included and 43 cysts were surgically removed and histologically analyzed. Mean tumor size was significantly lower in malignant lesions. Mean enhancement in arterial and portovenous phase, change of mean enhancement in portovenous and native phases were significantly different between benign and malignant lesions. Significant differences in the contrast enhancement pattern was found: septa and capsular enhancement was detected in 28.6% (n = 12) of cases in malignant lesions, while only 4.8% (n = 2) benign lesions show the same enhancement pattern. Some other features showed tendencies to be more prevalent in malignant lesions, however, no significant differences were found.
Conclusions
The collected data and selected features do not allow us to reliably differentiate Bosniak category III cystic lesions as benign or malignant. Some of the criteria showed some tendencies, however, further studies are required to confirm these findings' potential.
Keywords: cancer, kidney, computed tomography, renal cell carcinoma, renal cyst, renal tumor, Bosniak, renal neoplasm
INTRODUCTION
As computed tomography (CT) gained a more important role in medical care, the CT image quality improved and the number of CT examinations performed increased, there has been an increase in the detection of renal cysts. Some of them appear as incidental findings and some are detected purposefully when searching for kidney pathology. However, in some cases renal cysts remain a challenge for radiologists and clinicians, when the decision whether the cyst is malignant or benign has to be made.
In 1986, Morton A. Bosniak introduced the Bosniak classification of renal cysts based on the imaging characteristics of contrast-enhanced CT. The main purpose of the classification was to divide cystic renal changes into categories, which would determine the risk of malignancy and further management. Initially, there were four categories in the classification. The Bosniak I and II category cystic lesions were considered benign and surgical intervention was not recommended. Cysts, that had some features of malignancy, were evaluated as Bosniak category III and IV lesions. These lesions were considered to require surgical removal.
As more experience was gained, some weaknesses of the classification were revealed. It was noticed that quite a lot of cysts that were classified as Bosniak category III lesions were benign after surgical removal and pathological examination. Then the classification was enriched with the category IIF, which includes cysts that are advised to be followed up in time. And only in the case of the appearance of additional worrisome features, the IIF category cyst should be reclassified to a category III and surgically removed. Despite the renewal of the classification system, there still exists the problem that approximately half of the Bosniak category III cystic lesions appear to be benign after surgery [1]. However, the possibility arises that there may be some undiscovered radiological features, allowing us to further differentiate Bosniak category III cystic lesions specifically as benign or malignant.
MATERIAL AND METHODS
Vilnius University Hospital Santariškių Klinikos electronical information system was retrospectively searched from April 19, 2007, through January 1, 2016, for all contrast enhanced computed tomography (CT) examinations in which the terms ‘Bosniak III’, ‘Bosniac III’, ‘Bosniaką III’, ‘Bosniakas III’ appeared in the radiologist's report. Patients were followed till March 1, 2016 for pathologic evaluation after Bosniak III cystic lesion surgical treatment. One computed tomography examination was not properly stored in the hospital's electronical information system and the patient was excluded from the study.
Bosniak classification used in the Vilnius University Hospital Santariškių Klinikos to evaluate renal cystic lesions was based on the criteria described in literature [2, 3].
Data of genetic disorders and history of malignancy were collected before or at the moment of the Bosniak category III cystic lesion discovery. If the Bosniak III lesion was detected and there was a suspicion of another malignancy in the CT examination, the patient's history was followed for pathologic approval until March 1, 2016. In the case of no pathologic results, no additional malignancy was considered to be present.
The longest diameter of Bosniak category III cystic renal lesions was measured in the axial plane.
Contrast enhancement was measured in 0.5 cm2 region of interest (ROI). One cystic lesion was smaller than 0.5 cm2 in size so the 0.2 cm2 ROI was selected for the case.
The difference of Hounsfield Units (HU) in unenhanced and contrast-enhanced images (arterial or portovenous phase) was measured to evaluate the cystic lesion enhancement. A threshold of 15 HU was chosen.
Several patterns of contrast enhancement were pointed out:
Septal enhancement;
Capsular enhancement;
Septal and capsular enhancement;
Heterogeneous enhancement – septal or capsular enhancement are not clearly visible, but there was irregular enhancement of the intracystic part of the lesion;
Homogeneous enhancement – cystic lesion with regular, diffuse enhancement.
The cystic lesion was classified as exophytic if more than 50% of the cyst extended beyond the natural surface of the kidney and as endophytic if less than 50% of the cyst extended beyond the natural surface of the kidney. There were no completely intraparenchymal cystic lesions identified in our study.
Cystic lesions were divided into two groups according to their shape: cystic lesions with defined shape (oval, round or polycyclic) and cystic lesions with irregular, undefined shape.
To determine the amount of calcification within each cystic lesion, a subjective grouping into four categories according to the Israel and Bosniak article [1] was used:
Minimal calcification – smooth, hairline-thin strands of calcification;
Mild calcification – calcification with some thickness and minimal nodularity;
Moderate calcification – calcification with further thickness and/or a grossly nodular appearance;
Severe calcification – grossly thickened, nodular, and extensive calcification.
The location of the calcifications was grouped into three categories: peripheral (or capsular) calcifications, intracystic (also septal) calcifications and both peripheral and intracystic calcifications.
Statistical analysis was performed with SPSS 22.0 software. Continuous variables were compared by using the Mann – Whitney U test as data were not normally distributed.
The homogeneity hypothesis for proportions from independent groups was assessed by using the Pearson χ2 and Fisher exact tests. A statistically significant result was indicated by a p-value less than 0.05.
RESULTS
Baseline characteristics of analyzed patients and surgically removed Bosniak category III lesions are shown in Table 1.
Table 1.
Baseline characteristics of analyzed patients and Bosniak category III lesions
| Baseline characteristics | |
|---|---|
| No. of patients | 73 |
| Median age (years) | 60.78 ±4.4 |
| Gender (% (n) male) | 60.3 (47) |
| No. of surgically removed lesions (%) | 43 (55) |
| Surgically removed lesions’ characteristics | |
| Median age (years) | 57.79 ±13.5 |
| Gender (% (n) male) | 55.8 (24) |
| Malignant (%) | 55.8% |
| Surgical Pathologic Findings | |
| Clear cell renal cell carcinoma [n (%)] | 18 (41.9) |
| Benign epithelial or fibrous cyst [n (%)] | 16 (37.2) |
| Papillary renal cell carcinoma [n (%)] | 6 (14.0) |
| Cystic nephroma [n (%)] | 2 (4.7) |
| Oncocytoma [n (%)] | 1 (2.3) |
| Fuhrman nuclear grade | |
| G1 [n (%)] | 9 (41) |
| G2 [n (%)] | 11 (50) |
| G3 [n (%)] | 2 (9) |
The mean age between the analyzed patients with malignant and benign cystic lesions did not significantly differ. However, the mean tumor size was significantly lower in malignant Bosniak category III cystic lesions.
Malignant cystic lesions were diagnosed for 23.3% (n = 10) women, while benign lesions presented in 20.9%. (n = 9) cases. There were 32.6% (n = 14) men with malignant cystic lesions and respectively 23.3% (n = 10) with benign lesions. However, there was no statistically significant association between the gender and malignancy of Bosniak category III cystic lesions revealed (p = 0.708).
History of other malignancy (or positive oncologic anamnesis) was recorded in less than half of the patients (39.5%; n = 17) at the moment of Bosniak category III cystic lesion detection. The data of types of malignancy are as follows: renal cancer was detected in 58.8% (n = 10), prostate cancer in 23.5% (n = 4), colorectal cancer in 11.8% (n = 2), pancreatic cancer in 5.9% (n = 1) of patients. There was no significant difference in malignancy of Bosniak category III cystic lesions in patients with and without history of malignancy, history of renal cancer or history of renal cancer among patients with positive oncologic anamnesis (Table 2).
Table 2.
Distribution of benign and malignant Bosniak category III lesions in patients with positive or negative oncologic anamnesis
| Benign [% (n)] | Malignant [% (n)] | P Value | |
|---|---|---|---|
| History of malignancy/ No history of malignancy | 11.6 (n = 5)/ 32.6 % (n = 14) | 27.9 % (n = 12)/ 27.9 % (n = 12) | p = 0.115 |
| History of renal cancer/ No history of cancer or history of non-renal malignancy | 7 % (n = 3)/ 37.2% (n = 16) | 16.3 % (n = 7)/ 39.5 % (n = 17) | p = 0.47 |
| History of renal cancer in patients with positive oncologic anamnesis/ History of non-renal malignancy in patients with positive oncologic anamnesis | 17.6 % (n = 3)/ 11.8 % (n = 2) | 41.2% (n = 7) /29.4% (n = 5) | p = 1.0 |
Two Bosniak category III lesions were identified for one patient with von Hippel-Lindau syndrome. Both cysts were surgically removed and appeared to be malignant after pathological evaluation. However, there was no statistical significance found between presence of von Hippel-Lindau syndrome and the malignancy of the Bosniak category III lesions (p = 0.495).
Nevertheless, mean enhancement in arterial and portovenous phase and the differences between mean enhancement in portovenous and the native phases were significantly different between benign and malignant cystic lesions (Table 3). More characteristics of enhancement and other analyzed features of the Bosniak category III lesions are presented in Table 3.
Table 3.
Characteristics of analyzed patients and Bosniak category III lesions
| Malignant | Benign | P Value | |
|---|---|---|---|
| Mean age ± standard deviation (SD) (years) | 56.96 ±15.8 | 59.94 ±9.3 | P = 0.835 |
| Mean tumor size ± SD (mm) | 33.71 ±17.9 | 44.61 ±16.7 | P = 0.031 |
| Exophytic/ Endophytic location [% (n)] | 35.7 (15)/ 21.4 (9) | 31 (13)/ 11.9(5) | P = 0.508 |
| Defined/ undefined shape [% (n)] | 26.2 (11)/ 31 (13) | 33.3 (14)/ 9.5 (4) | P = 0.057 |
| Calcified component/ No calcified component [% (n)] | 21.4 (9)/ 35.7 (15) | 19 (8)/ 23.8 (10) | P = 0.65 |
| Presence of septa/ No septa [% (n)] | 40.5 (17)/ 16.7 (7) | 28.6 (12)/ 14.3 (6) | P = 0.773 |
| Enhancement of Bosniak category III lesions | |||
| Contrast enhancing lesions/ No enhancement [% (n)] | 52.4 (22)/ 4.8 (2) | 28.6 (12)/ 14.3 (6) | P = 0.056 |
| Native phase ( Hounsfield Units (HU)) | 25.92 ±12.7 | 20.94 ±9.7 | P = 0.217 |
| Mean enhancement in arterial phase (HU) | 68.46 ±40.6 | 44.00 ±21.6 | P = 0.037 |
| Mean enhancement in portovenous phase (HU) | 57.42 ±29.6 | 38.28 ±17.9 | P = 0.017 |
| Mean arterial phase (HU) – Mean native phase (HU) | 42.54 ±36.2 | 23.06 ±19.7 | P = 0.069 |
| Mean portovenous phase (HU) – Mean native phase (HU) | 31.50 ±24.1 | 17.33 ±16.3 | P = 0.039 |
| Mean arterial phase (HU) – Mean portovenous phase (HU) | 11.04 ±17.7 | 5.72 ±7.2 | P = 0.647 |
Significant differences were also found depending on the contrast enhancement pattern (p = 0.01): septal and capsular enhancement was detected in 28.6% (n = 12) of cases in malignant Bosniak category III lesions, while only 4.8% (n = 2) benign lesions showed the same enhancement pattern. The whole distribution between patterns of contrast enhancement in malignant and benign lesions is shown in Figure 1.
Figure 1.
The distribution of contrast enhancement patterns in malignant and benign Bosniak category III lesions.
The amount and location of calcification in Bosniak category III lesions were not significantly different between malignant and benign lesions, even though moderate and severe amount of calcifications were only found in malignant cystic lesions (Table 4).
Table 4.
The amount and location of calcification in benign and malignant Bosniak category III lesions
| Amount of calcifications [% (n)] | Location of calcifications [% (n)] | ||||||
|---|---|---|---|---|---|---|---|
| Minimal | Mild | Moderate | Severe | Capsular | Intracystic | Peripheral + intracystic | |
| Malignant | 29.4 (5) | 5.9 (1) | 11.8 (2) | 5.9 (1) | 17.6 (3) | 17.6 (3) | 17.6 (3) |
| Benign | 17.3 (3) | 29.4 (5) | 0 (0) | 0 (0) | 11.8 (2) | 29.4 (5) | 5.9 (1) |
| P-value | P = 0.092 | P = 0.578 | |||||
DISCUSSION
Since Morton A. Bosniak introduced the Bosniak classification of renal cysts, it has been updated and renewed several times. However, the Bosniak category III lesions still remain a challenge for both radiologists and clinicians. The main concern is that approximately half of the Bosniak category III cystic lesions are benign, although surgical treatment is recommended in most of the cases [1].
The amount of studies that analyzed the usefulness of Bosniak classification in determination of malignancy is quite low and most of the studies available were performed retrospectively [4–8]. Moreover, most of the previous studies [4, 9, 10, 11] are not reliable enough due to the small amount of patients included, as the Bosniak category III cystic lesions are not common in clinical practice. In our study, a larger sample size may have given more specific results, although our sample size (n = 43) exceeded the number of patients in the majority of previous studies available.
Graumann et al. [12] selected studies that were performed until 2009 and more than 30 patients were included. The results showed that the newly introduced IIF category reduced the number of Bosniak category III cystic lesion classifications and unnecessary surgery. Moreover, the IIF category lesions were benign in all of the cases, which suggest the high reliability of this category.
In 2012, Smith et al. [1] analyzed 69 Bosniak category IIF and 144 Bosniak category III cystic lesions. Surgically removed lesions appeared to be malignant in 25% (4/16) of cases in category IIF and 54% (58/107) of cases in the category III. The study confirms that most of the Bosniak category IIF lesions are benign, even though the prevalence of malignancy is higher than in the Graumann et al. [12] selected studies.
Another study was performed by Weibl et al. [13] in 2014, which included 27 IIF category and 58 III category lesions. The 9 category IIF and 54 category III lesions were surgically removed. Malignancy appeared to be in 89% (8/9) of category IIF and in 69% (37/54) of category III lesions. Data showed the inappropriately high rate of malignancy in the category IIF lesions. The explanation of this result may be the decision to manage category IIF lesions surgically and not to reclassify the lesion into Bosniak category III when new worrisome features appeared in the computed tomography (CT) on follow-up.
However, the results also show that a great number of Bosniak category III cystic renal lesions are surgically removed despite their benignity and newly established category IIF.
The mean age of patients included in our study does not significantly differ from other author's data. The mean age of patients included in the O'Malley RL et al. study was 61 years [7], in the Smith et al. the mean age was 57 years [1] while in Weibl et al. the mean age was 59 years [13].
Bosniak category III lesions were found approximately twice as often in men as in women. Similar results were published in Weibl et al. study [13], where 60% of the patients were men.
Malignant Bosniak category III cystic lesions were identified in 55.8% of cases after surgical removal. Histologically, clear cell and papillary renal cell carcinoma (RCC) were the most prevalent malignant neoplasms and the minority of these lesions were classified as Fuhrman nuclear Grade 3. Our study shows very similar tendencies to the other authors' findings [1, 7, 13].
Smith et al. [1] study evaluated the association of the prevalence of malignancy in the Bosniak III lesions and these three factors: coexisting Bosniak III lesion, coexisting Bosniak IV lesion and/or solid mass, and a history of malignant renal neoplasm. All of the three factors were associated with a significantly higher percentage of malignancy in the Bosniak category III lesions. However, there was no significant difference between the malignancy rate and positive oncologic anamnesis found in our study.
According to literature and previous studies, the great majority of cystic renal neoplasms in patients with von Hippel-Lindau syndrome are malignant [1, 14, 15]. The malignancy rate was around 24–45% [15]. There was one patient in our study with von Hippel-Lindau syndrome, who had two Bosniak category III lesions detected on CT. Both of the lesions were proved to be malignant after surgical removal, however, no statistically significant dependency between von Hippel-Lindau syndrome and malignancy was detected.
One of the most important criteria used in differentiating renal lesions is the determination of enhancement. The latter is considered to be a sign of malignancy [2]. In our study, contrast enhancement was detected in malignant lesions more often than in benign, but the difference was not proved to be statistically significant. Nevertheless, the difference between mean enhancement in portovenous and native phases was significantly higher in patients with malignant Bosniak category III cystic lesions. This result may be influenced by papillary RCC, which usually shows a specific pattern of contrast enhancement as the lesion enhancement over time increases and usually no washout is seen [16]. It means that the value of enhancement detected in portovenous phase is higher than in the arterial phase and consequently, the difference between portovenous and native phases is also higher.
Our study found significant difference between the particular enhancement pattern (when both septa and capsule enhances) and the malignancy rate. To our knowledge no previous study has evaluated this characteristic of the lesion. Further studies will be needed to confirm or deny our findings.
Israel et al. [17] tried to determine the amount of calcifications in the Bosniak cystic lesions and associate it with malignancy. In summary, calcium per se can be seen either in benign or in malignant cystic lesions and the amount of calcifications can not specify the malignancy. Our study confirmed the Israel et al. [17] results, though moderate and severe amount of calcifications was only seen in malignant lesions.
There were some limitations of our study. Firstly, the results of the CT examinations were retrospectively collected and radiologists with different amounts of experience evaluated the obtained images. Secondly, the usage of the Bosniak classification of renal cystic lesions started on the 19th of April, 2007 in our hospital. Until the 31st of December, 2009, there were only five cases with Bosniak category III cystic lesions discovered. The vast majority of the cases were detected since 2010. Probably, some of the Bosniak category III lesions, found before 2010, are not included in our study, even if they satisfy the specified criteria. Radiologists may have used other terms to evaluate the malignancy rate of lesions before 2010 and the terminology may have differed from our selected keywords. Moreover, the CT protocol was not standardized in all patients and the quality of some of the images was quite poor. That is the reason why some of the characteristics evaluated on CT may be inaccurate.
Finally, the oncologic anamnesis was collected before the moment or at the moment of Bosniak category III cystic lesion detection. When other malignancy was suspected in the CT images, where Bosniak category III lesion was detected, the patient's history was followed for pathologic approval until March 1, 2016. If the approval was not confirmed, it was considered that no other malignancy was detected. Consequently, some of the cases with probable positive oncologic anamnesis were not included in the study, because histology results were presented after the 1st of March, 2016.
CONCLUSIONS
The collected data and selected features do not reliably differentiate Bosniak category III cystic lesions into benign or malignant. Some of the criteria (for example, pattern of contrast enhancement in septa and capsule, moderate or severe calcification, difference of the Hounsfield Unit (HU) between portovenous and native phases et.) show some tendencies; however, further studies are required to confirm these findings' potential.
In the near future, the Bosniak classification may be used not only in computed tomography, but also in other modalities, such as contrast-enhanced ultrasound or magnetic resonance imaging. However, previous studies [18–22] show controversial results and further research is required in order to prove the advantages of these methods.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Smith AD, Remer EM, Cox KL, et al. Bosniak category IIF and III cystic renal lesions: outcomes and associations. Radiology. 2012;262:152–160. doi: 10.1148/radiol.11110888. [DOI] [PubMed] [Google Scholar]
- 2.Israel GM, Bosniak MA. How I do it: evaluating renal masses. Radiology. 2005;236:441–450. doi: 10.1148/radiol.2362040218. [DOI] [PubMed] [Google Scholar]
- 3.Israel GM, Bosniak MA. An update of the Bosniak renal cyst classification system. Urology. 2005;66:484–488. doi: 10.1016/j.urology.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Harisinghani MG, Maher MM, Gervais DA, et al. Incidence of Malignancy in complex cystic renal masses (Bosniak category III): Should imaging-guided biopsy precede surgery? AJR Am J Roentgenol. 2003;180:755–758. doi: 10.2214/ajr.180.3.1800755. [DOI] [PubMed] [Google Scholar]
- 5.Koga S, Nishikido M, Inuzuka S, et al. An evaluation of Bosniak's radiological classification of cystic renal masses. BJU Int. 2001;86:607–609. doi: 10.1046/j.1464-410x.2000.00882.x. [DOI] [PubMed] [Google Scholar]
- 6.Warren KS, McFarlane J. The Bosniak classification of renal cystic masses. BJU Int. 2005;95:939–942. doi: 10.1111/j.1464-410X.2005.05442.x. [DOI] [PubMed] [Google Scholar]
- 7.O'Malley RL, Godoy G, Hecht EM, Stifelman MD, Taneja SS. Bosniak category IIF designation and surgery for complex renal cysts. J Urol. 2009;182:1091–1095. doi: 10.1016/j.juro.2009.05.046. [DOI] [PubMed] [Google Scholar]
- 8.Song C, Min GE, Song K, et al. Differential diagnosis of complex cystic renal mass using multiphase computerized tomography. J Urol. 2009;181:2446–2450. doi: 10.1016/j.juro.2009.01.111. [DOI] [PubMed] [Google Scholar]
- 9.Cloix P, Martin X, Pangaud C, et al. Surgical management of complex renal cysts: a series of 32 cases. J Urol. 1996;156:28–30. [PubMed] [Google Scholar]
- 10.Aronson S, Frazier HA, Baluch JD, Hartman DS, Christenson PJ. Cystic renal masses: usefulness of the Bosniak classification. Urol Radiol. 1991;13:83–90. doi: 10.1007/BF02924596. [DOI] [PubMed] [Google Scholar]
- 11.Wilson TE, Doelle EA, Cohan RH, Wojno K, Korobkin M. Cystic renal masses: a reevaluation of the usefulness of the Bosniak classification system. Acad Radiol. 1996;3:564–570. doi: 10.1016/s1076-6332(96)80221-2. [DOI] [PubMed] [Google Scholar]
- 12.Graumann O, Osther SS, Osther PJ. Characterization of complex renal cysts: a critical evaluation of the Bosniak classification. Scand J Urol Nephrol. 2011;45:84–90. doi: 10.3109/00365599.2010.533695. [DOI] [PubMed] [Google Scholar]
- 13.Weibl P, Hora M, Kollarik B, Shariat SF, Klatte T. Management, pathology and outcomes of Bosniak category IIF and III cystic renal lesions. World J Urol. 2015;33:295–300. doi: 10.1007/s00345-014-1301-x. [DOI] [PubMed] [Google Scholar]
- 14.Katabathina VS, Vinu-Nair S. Cross-sectional imaging spectrum of von Hippel-Lindau disease. J Transl Med Epidemiol. 2014;2:1021.. [Google Scholar]
- 15.Leung RS, Biswas SW, Duncan M, Rankin S. Imaging features of von Hippel–Lindau disease. Radiographics. 2008;28:65–79. doi: 10.1148/rg.281075052. [DOI] [PubMed] [Google Scholar]
- 16.Yang CW, Shen SH, Chang YH, et al. Are there useful ct features to differentiate renal cell carcinoma from lipid-poor renal angiomyolipoma? AJR Am J Roentgenol. 2013;201:1017–1028. doi: 10.2214/AJR.12.10204. [DOI] [PubMed] [Google Scholar]
- 17.Israel GM, Bosniak MA. Calcification in cystic renal masses: is it important in diagnosis? Radiology. 2003;226:47–52. doi: 10.1148/radiol.2261011704. [DOI] [PubMed] [Google Scholar]
- 18.Israel GM, Hindman NM, Bosniak MA. Evaluation of cystic renal masses: comparison of CT and MR Imaging by using the Bosniak classification system. Radiology. 2004;231:365–371. doi: 10.1148/radiol.2312031025. [DOI] [PubMed] [Google Scholar]
- 19.Ignee A, Schreiber D, Schuessler G, Wolff J, Dietrich CF. 0664: Contrast enhanced ultrasound in the characterisation of renal masses. Ultrasound in Med Biol. 2009;35:S91.. [Google Scholar]
- 20.Cokkinos DD, Antypa EG, Skilakaki M, Kriketou D, Tavernaraki E, Piperopoulos PN. Contrast enhanced ultrasound of the kidneys: what is it capable of? BioMed Res Int. 2013;2013:1–13. doi: 10.1155/2013/595873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Graumann O, Osther SS, Karstoft J, Hørlyck A, Osther PJ. Bosniak classification system: a prospective comparison of CT, contrast-enhanced US, and MR for categorizing complex renal cystic masses. Acta Radiol. 2016;57:1409–1417. doi: 10.1177/0284185115588124. [DOI] [PubMed] [Google Scholar]
- 22.Ragel M, Nedumaran A, Makowska-Webb J. Prospective comparison of use of contrast-enhanced ultrasound and contrast-enhanced computed tomography in the Bosniak classification of complex renal cysts. Ultrasound. 2016;24:6–16. doi: 10.1177/1742271X15626959. [DOI] [PMC free article] [PubMed] [Google Scholar]