Abstract
The International Continence Society (ICS) committee has defined overactive bladder (OAB) as “a syndrome characterized by symptoms of urgency, with or without urgency incontinence, usually with increased daytime frequency and nocturia (increased night time urination). The term OAB can only be used if there is no proven infection or other obvious pathology”. Though the ICS gives no anatomical basis for OAB, it is suggested that the cause is from the detrusor itself. In this review, urodynamic evidence is presented that OAB in the female may be a prematurely activated but normal micturition reflex, as predicted by the Integral Theory. Anatomically, a trampoline analogy explains how loose ligaments prevent the vaginal stretching so important for support of the bladder base stretch receptors which control the reflex. Surgical cure of OAB by repair of loose cardinal/ uterosacral ligaments are an important proof that the origins of OAB are outside the bladder, laxity of the suspensory ligaments which in turn, inactivate the striated muscle vector forces which contract against them. This concept is not in in conflict with the definitions of the ICS. Rather it provides a causative anatomical background to the definitions.
Keywords: ligaments, urge incontinence, overactive bladder, surgical cure
INTRODUCTION
Standardization of terminology (definitions) of symptoms and conditions of the pelvic floor has been a raison d'etre of the International Continence Society (ICS) committees for more than 40 years [1, 2]. OAB has been defined as follows [2].
“Overactive bladder (OAB) is a syndrome characterized by symptoms of urgency, with or without urgency incontinence, usually with increased daytime frequency and nocturia (increased night time urination). The term OAB can only be used if there is no proven infection or other obvious pathology”.
Though etiology is sometimes suggested by the ICS [1, 2], generally, no specific anatomical basis is given for the majority of these definitions. The vast majority of bladder, bowel and pain conditions are considered as being incurable.
Messelink [3] commented on the importance of definitions and guidelines as follows:
“There can be no guidelines without definitions, and no definitions without understanding the item that is defined. The definitions and terminology we use reflect our present knowledge Definitions and terms are of utmost importance because they are the basis for the language we use”.
“Understanding the item” [3], clearly involves an understanding of normal anatomy and physiology of the pelvic floor, and how it can go wrong.
MATERIAL AND METHODS
This review is confined to “overactive bladder” (OAB) as defined by the ICS. The aim of this work is to review existing studies of anatomy, physiology and surgery relative to an anatomical basis for OAB and to discuss a way forward for cure. The 2013 ICS fact sheets [2] and 2002 publication [1] and recent CEJU publication by Liedl et al. [4] were chosen as reference points.
Evidence
ICS definition OAB symptoms consist of frequency, urgency/ urge incontinence, nocturia [2]. According to [2], “the symptoms of OAB are suggestive of detrusor (bladder muscle) overactivity”.
Analysis If what [2] states is correct, it would not be possible to cure OAB symptoms surgically. Yet cure rates of up to 90% for frequency and urgency have been published in patients following repair of cardinal/uterosacral ligaments [4–11].
Anatomical and physiological explanations for an anatomical origin of overactive bladder
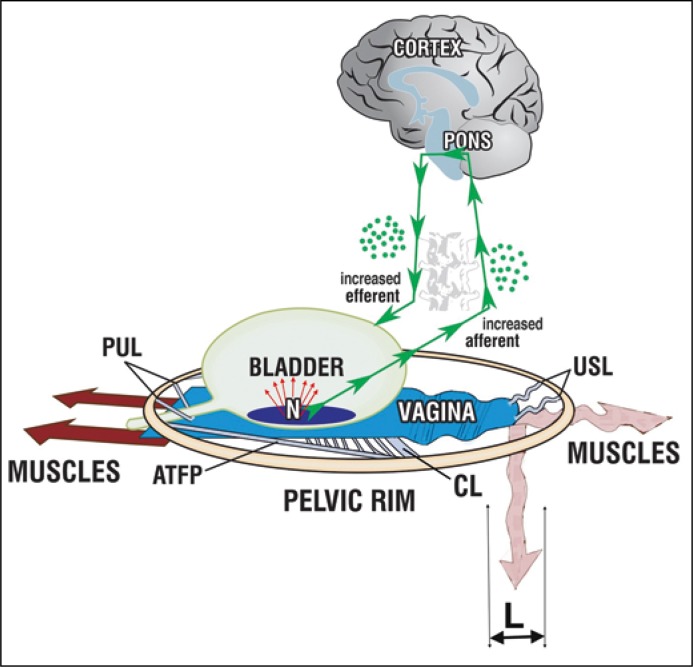
As part of the 1990 Integral Theory, frequency, urgency and nocturia were defined as being manifestations of a prematurely activated, but normal micturition reflex [12]. It was hypothesized that loose suspensory ligaments, pubourethral anteriorly and uterosacral posteriorly, weakened the musculoelastic stretching mechanism of the vagina which supported the bladder base stretch receptors 'N', Figure 1. In 1993, it was demonstrated that the events occurring in patients with DI (urodynamic “detrusor instability”), now 'DO', were identical with those occurring during micturition, first sensory urgency, then urethral relaxation, then detrusor contraction, then urine loss [13]. In a further study [14], in a small group of patients, it was possible to control urodynamic 'DI' by digital support of the bladder base. This would not be possible if the problem was in the detrusor itself [2]. This experiment also confirmed that the activator of the urodynamic DO were peripherally located stretch receptors, 'N', Figure 1.
Figure 1.
If the uterosacral ligaments (USL) lengthen say by 'L', USLs are unable to suspend the vagina adequately. The downward/backward muscle forces (arrows) weaken as a muscle requires a firm anchoring point to contract efficiently. The muscle forces (arrows) cannot stretch the vagina sufficiently to support the stretch receptors 'N'. 'N' fire off increased afferent impulses at a low bladder volume and this is perceived by the cortex as urgency. If the number of afferent signals is sufficient to activate the micturition reflex, the efferents are activated; the forward muscles relax; the backward muscles open out urethra; bladder contracts; the patient may uncontrollably lose urine (“urge incontinence”). PUL – pubourethral ligament, ATFP – arcus tendineus fascia pelvis, CL – cardinal ligament; USL – uterosacral ligament
Surgical evidence of the anatomical origin of overactive bladder
A recent study of 611 patients who had a TFS posterior sling repair for uterine/apical prolapse found a high co-occurrence of chronic pelvic pain, bowel symptoms and OAB symptoms [4]. The results following posterior TFS sling were 90% prolapse cure in 611 patients. Symptom incidence in these 611 patients (% Cure at 12 months in brackets) was: urge incontinence: n = 310 (85%); frequency: n = 317 (83%); nocturia: n = 254 (68%); chronic pelvic pain (CPP): n = 194 (77%); fecal incontinence: n = 93 (65%).
Though co-occurrence of CPP, bladder & bowel dysfunction was convincingly demonstrated by [4], it has been demonstrated that patients tend to complain of mainly one of these symptoms [15]. This phenomenon has been called the “Pescatori Iceberg” after Pescatori who first reported it. For example, in 198 patients who presented with CPP [15], 127 had frequency, 55 urge incontinence, 63 nocturia, 59 obstructive defecation, 66 USI, 44 residual urine, 68 bladder emptying symptoms, 56 fecal incontinence. It follows from this that any patient who has any type of uterine/apical prolapse is likely to have OAB symptoms and that these are potentially curable surgically.
The importance of competent posterior ligaments
Urge incontinence concerns the symptom “inability to hold on” [1, 2]. This begs the questions, “hold on to what”? Clearly inappropriate activation of the micturition reflex, which is the Integral Theory's definition of OAB, Figure 1. The role of uterosacral ligaments in OAB and fecal incontinence (FI) cure was discussed more comprehensively recently [16]; the posterior vectors (arrows), Figure 1, act to close and open both the urethra and anus [17] and both act against the uterosacral ligaments (USL) [18]. Therefore weakness in USL explains the co-incidence of OAB and FI symptoms [4] and how both are potentially curable by shortening and reinforcing USLs, as demonstrated [4]. As regards nocturia, a similar mechanism to Figure 1 holds. To visualize this, turn Figure 1 90 degrees. The patient is supine and the pelvic muscles are relaxed. As the bladder fills, it stretches downward by the force of gravity. Normally intact USLs support the volume of urine. If USLs are weak, as the volume of urine increases, the bladder base continues to descend. This stimulates the stretch receptors 'N' which in turn activate the micturition reflex. The patient is woken by an urge to pass urine.
Conclusions
The evidence for an external mechanism for causation of OAB and OAB as a prematurely activated micturition, but normal micturition reflex as described in this work is strong if not overwhelming. This concept is not in conflict with the definitions of the ICS. Rather it provides a causative anatomical background to the definitions.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Abrams P, Cardozo L, Fall M, et al. The standardization of terminology of lower urinary tract function: report from the standardization sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:179–183. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 2.ICS Fact Sheets A Background to Urinary and Faecal Incontinence Prepared by the Publications & Communications Committee. 2013. Jul, [Google Scholar]
- 3.Messelink B. Perspective - Chronic Pelvic Pain needs an integral approach. Pelviperineology. 2017;36:67–70. [Google Scholar]
- 4.Liedl B, Inoue H, Sekiguchi Y, et al. Is overactive bladder in the female surgically curable by ligament repair? Cent European J Urol. 2017;70:51–57. doi: 10.5173/ceju.2017.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neuman M, Lavy Y. Posterior intra-vaginal slingplasty for the treatment of vaginal apex prolapse: Medium-term results of 140 operations with a novel procedure. Eur J Obstet Gynecol Reprod Biol. 2008;140:230–233. doi: 10.1016/j.ejogrb.2006.07.035. [DOI] [PubMed] [Google Scholar]
- 6.Goeschen K. Posterior Fornix Syndrome: Comparison of original (2004) and modifed (2015) post-PIVS anatomic and symptomatic results: a personal journey. Pelviperineology. 2015;34:85–91. [Google Scholar]
- 7.Caliskan A, Goeschen K, Zumrutbas AE. Long term results of modifed posterior intravaginal slingplasty (P-IVS) in patients with pelvic organ prolapse. Pelviperineology. 2015;34:94–100. [Google Scholar]
- 8.Richardson P. Surgical cure of nocturia using 4 different methods based on strengthening the structural supports of the vaginal apex - a short review. Pelviperineology. 2015;34:92–93. [Google Scholar]
- 9.Petros PE. New ambulatory surgical methods using an anatomical classification of urinary dysfunction improve stress, urge, and abnormal emptying. Int J Urogynecology. 1997;5:270–278. doi: 10.1007/BF02765483. [DOI] [PubMed] [Google Scholar]
- 10.Inoue H, Kohata Y, Sekiguchi Y, Kusaka T, Fukuda T, Monnma M. The TFS minisling restores major pelvic organ prolapse and symptoms in aged Japanese women by repairing damaged suspensory ligament - 12-48 month data. Pelviperineology. 2015;34:79–83. [Google Scholar]
- 11.Haverfield M. Tissue fixation system (TFS) neoligament pelvic organ repair procedures -12 and 24 month results. Pelviperineology. 2015;34:70–74. [Google Scholar]
- 12.Petros PE, Ulmsten U. An Integral Theory of female urinary incontinence. Acta Obstet Gynecol Scand. 1990;153(Suppl):1–79. doi: 10.1111/j.1600-0412.1990.tb08027.x. [DOI] [PubMed] [Google Scholar]
- 13.Petros PE, Ulmsten U. Bladder instability in women: A premature activation of the micturition reflex. Neurourol Urodyn. 1993;12:235–239. doi: 10.1002/nau.1930120305. [DOI] [PubMed] [Google Scholar]
- 14.Petros PE. Detrusor instability and low compliance may represent different levels of disturbance in peripheral feedback ontrol of the micturition reflex. Neurourol Urodyn. 1999;18:81–91. doi: 10.1002/(sici)1520-6777(1999)18:2<81::aid-nau3>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 15.Goeschen K, Gold DM. Surgical cure of chronic pelvic pain, associated bladder & bowel symptoms by posterior sling in 198 patients validates the Pescatori Iceberg principle of pelvic symptom co-occurrence. Pelviperineology. 2017;36:84–88. [Google Scholar]
- 16.Petros P, Liedl B, Inoue H, Sekiguchi Y, et al. Is overactive bladder in the female surgically curable by ligament repair? (Letter to the Editor) Cent European J Urol. 2017;70:454. doi: 10.5173/ceju.2017.938. Referring to the paper: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petros PE, Bush MB. The same posterior muscle vectors act to open urethra and anus during micturition and defecation. Pelviperineology. 2017;36:35–36. [Google Scholar]
- 18.Liedl B, Bush M. Competent uterosacral ligaments are required for normal bladder evacuation - testing a hypothesis evolving from finite element studies on micturition mechanisms in the female. Pelviperineology. 2016;35:105–108. [Google Scholar]