Abstract
Objectives
Lung disease is a leading cause of disability and death among older adults. We examine whether personality traits are associated with lung function and shortness of breath (dyspnea) in a national cohort with and without chronic obstructive pulmonary disease (COPD).
Method
Participants (N = 12,670) from the Health and Retirement Study were tested for peak expiratory flow (PEF) and completed measures of personality, health behaviors, and a medical history.
Results
High neuroticism and low extraversion, openness, agreeableness, and conscientiousness were associated with lower PEF, and higher likelihood of COPD and dyspnea. Conscientiousness had the strongest and most consistent associations, including lower risk of PEF less than 80% of the predicted value (OR = 0.67; 0.62–0.73) and dyspnea (OR = 0.52; 0.47–0.57). Although attenuated, the associations remained significant when accounting for smoking, physical activity, and chronic diseases including cardiovascular and psychiatric disorders. The associations between personality and PEF or dyspnea were similar among those with or without COPD, suggesting that psychological links to lung function are not disease dependent. In longitudinal analyses, high neuroticism (β = −0.019) and low conscientiousness (β = 0.027) predicted steeper declines in PEF.
Discussion
A vulnerable personality profile is common among individuals with limited lung function and COPD, predicts shortness of breath and worsening lung function.
Keywords: Chronic obstructive pulmonary disease, Conscientiousness, Lung function, Peak expiratory flow, Personality, Shortness of breath
Chronic bronchitis and emphysema are progressive and debilitating respiratory conditions that tend to co-occur and are referred to as chronic obstructive pulmonary disease (COPD). COPD is a chronic inflammatory lung disease characterized by airflow limitation and presents with shortness of breath (dyspnea), production of mucus, and chronic cough. COPD is often underdiagnosed (Bednarek, Maciejewski, Wozniak, Kuca, & Zielinski, 2008; Mannino, Gagnon, Petty, & Lydick, 2000), but the prevalence of COPD is about 8% according to international estimates (Halbert et al., 2006) and is especially common among older adults. Indeed, COPD has been labeled a disease of accelerated lung aging (Ito & Barnes, 2009). Lung disease is associated with high risk of hospitalization, considerable economic burden, lower quality of life, and it is a major cause of disability and mortality (Lopez et al., 2006; Suissa, Dell’Aniello, & Ernst, 2012; Vestbo et al., 2013). COPD is the third leading cause of death in the United States and Europe (Hoyert & Xu, 2012). About 80% of COPD deaths are due to tobacco smoking (DHHS, 2014).
Psychological factors are likely to have an impact on lung functioning and contribute to the etiology and prognosis associated with COPD. Anxiety and depression, for example, are prevalent comorbidities in COPD and are associated with worse quality of life and health outcomes for patients with lung disease (Maurer et al., 2008). Little is known, however, about whether more enduring behavioral, cognitive, and emotional dispositions assessed by personality questionnaires are associated with lung functioning. A few studies have examined the association between personality and COPD with mixed results (Goodwin & Friedman, 2006; Weston, Hill, & Jackson, 2014), but these studies have not considered measures of lung function or symptoms.
Most personality traits are captured by five broad dimensions: neuroticism, extraversion, openness, agreeableness, and conscientiousness (McCrae & John, 1992). These traits, and in particular low conscientiousness and high neuroticism, have been associated with physical inactivity, morbidity, and mortality (Chapman, Roberts, Lyness, & Duberstein, 2012; Hampson, 2012; Kern & Friedman, 2008; Stephan, Sutin, & Terracciano, 2014; Weston et al., 2014). Given the links between personality and cigarette smoking (Terracciano & Costa, 2004), chronic inflammation (Luchetti, Barkley, Stephan, Terracciano, & Sutin, 2014), and age-related diseases (Sutin, Zonderman, Ferrucci, & Terracciano, 2013), personality traits are likely to be related to COPD and may predict dyspnea and poor and worsening lung function among older adults. Besides COPD, poor lung functioning and shortness of breath are common in other conditions, such as asthma and congestive heart failure.
Even among healthy older adults, lung function gradually declines with age. Limited lung function can have a significant negative impact on mobility, activities of daily living, and quality of life (Roberts & Mapel, 2012). Poor lung function may also increase the risk of mild cognitive impairment (DeCarlo et al., 2015). In addition to COPD, it is thus of interest to examine the psychological correlates of lung function. Furthermore, it is of interest to examine the role of personality in shortness of breath or dyspnea, a patient-centered outcome and an emblematic symptom of poor lung function and COPD.
Using data from the Health and Retirement Study (HRS), a population-based cohort of older adults, this study sought to (a) characterize the personality profile of older adults reporting COPD, (b) test the concurrent and prospective associations of personality traits with lung function as measured by peak expiratory flow (PEF) in older adults with and without COPD, and (c) examine the potential role of personality in dyspnea with and without accounting for PEF, COPD, and other comorbidities.
Method
Participants
Participants were drawn from the Health and Retirement Study (HRS), a nationally representative longitudinal study of Americans aged 50 years and older. The HRS data are available for public download at http://hrsonline.isr.umich.edu/. Starting in 2006, HRS implemented a face-to-face interview that included a psychosocial questionnaire with a measure of personality traits. Half of the HRS participants completed the interview in 2006; the other half completed it in 2008. Across 2006 and 2008, the sample with complete data on personality and PEF included 12,670 participants. Table 1 shows descriptive statistics for the sample. Of the 12,670 individuals with complete data at baseline, 9,362 participants were assessed again for PEF at the 2010–2012 follow-up interviews. The individuals who were not assessed at follow-up did not differ on sex, race, or ethnicity from those who were assessed at follow-up (p > .05) but were older, had fewer years of education, worse PEF, and scored higher on neuroticism and lower on the other personality traits (p < .05).
Table 1.
Descriptive Statistics of the Study Participants in the Overall Sample and by COPD
| Total | No COPD | COPD | ||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Age | 68.07 | 10.40 | 67.89 | 10.47 | 69.59 | 9.62 |
| Female, n (%) | 7,555 | 60% | 6,727 | 59% | 828 | 62% |
| African American, n (%) | 1,564 | 12% | 1,422 | 13% | 142 | 11% |
| Hispanic, n (%) | 1,018 | 8% | 951 | 8% | 67 | 5% |
| Education | 12.80 | 4.46 | 12.86 | 4.31 | 12.32 | 5.54 |
| Height | 65.22 | 3.96 | 65.25 | 3.96 | 64.95 | 3.93 |
| Weight | 178.68 | 42.47 | 178.37 | 41.92 | 181.29 | 46.81 |
| BMI | 29.46 | 6.30 | 29.37 | 6.15 | 30.20 | 7.37 |
| Current smokers, n (%) | 1,626 | 13% | 1,295 | 11% | 331 | 25% |
| Ever smokers, n (%) | 6,546 | 52% | 5,585 | 49% | 961 | 73% |
| Moderate physical activity | 3.19 | 1.32 | 3.24 | 1.29 | 2.76 | 1.45 |
| Neuroticism | 2.05 | 0.61 | 2.04 | 0.61 | 2.18 | 0.66 |
| Extraversion | 3.20 | 0.55 | 3.21 | 0.55 | 3.13 | 0.55 |
| Openness | 2.94 | 0.55 | 2.94 | 0.55 | 2.89 | 0.54 |
| Agreeableness | 3.53 | 0.47 | 3.54 | 0.47 | 3.52 | 0.48 |
| Conscientiousness | 3.36 | 0.47 | 3.37 | 0.47 | 3.27 | 0.50 |
| Dyspnea, n (%) | 1,920 | 16% | 1,223 | 11% | 697 | 56% |
| PEF baseline | 357.52 | 132.00 | 366.97 | 130.58 | 276.69 | 115.45 |
| PEF baseline < 80%, n (%) | 3,445 | 27% | 2,694 | 24% | 751 | 57% |
| PEF follow-up | 360.57 | 134.65 | 368.28 | 133.06 | 283.60 | 126.02 |
Notes. BMI = body mass index; COPD = chronic obstructive pulmonary disease; PEF = peak expiratory flow.
Total N = 12,670; No COPD n = 11,345; COPD n = 1,325.
Personality
Personality was assessed using the Midlife Development Inventory (MIDI; Lachman, 2001). Participants were asked how much 25 adjectives described themselves on a scale ranging from 1 (not at all) to 4 (a lot). The adjectives measuring neuroticism were moody, worrying, nervous, and calm (reverse coded); the items for extraversion were outgoing, friendly, lively, active, and talkative; the items for openness were creative, imaginative, intelligent, curious, broadminded, sophisticated, and adventurous; the items for agreeableness were helpful, warm, caring, softhearted, and sympathetic; the items for conscientiousness were organized, responsible, hardworking, and careless (reverse coded).
Peak Expiratory Flow
The PEF lung test was performed as part of a battery of physical measurements using a Mini-Wright peak flow meter (Clement Clarke International Ltd., Harlow, U.K.) and a disposable mouthpiece. The interviewer instructions were as follows: “Next I’m going to ask you to perform a simple measurement that will measure how fast you can expel air from your lungs. It is important that you blow as hard and as fast as you can. I would like you to perform the measurement three times. When we are ready to begin, I’ll ask you to stand up. Take as deep a breath as possible. Open your mouth and close your lips firmly around the outside of the mouthpiece, and then blow as hard and as fast as you can into the mouthpiece. Like this … ” The trained interviewer then demonstrated the measurement and asked whether the respondent understood the instruction and whether it would be safe to perform the test. Three measurements were taken 30 seconds apart, with the maximum value used as the respondent’s PEF in the analyses.
As in previous studies (Jackson & Hubbard, 2003; Roberts & Mapel, 2012), we examined the clinical cutoff of PEF less than 80% of the predicted value based on sex, age, height, race, and ethnicity. As described in a previous study (Roberts & Mapel, 2012), the equations to estimate the PEF predicted values were based on regression coefficients obtained in a HRS subsample with no history of smoking, COPD, or reports of breathing problems. The equation for the predicted PEF in women was as follows: 350.7 + (−4.3 * age) + (4.2 * height) + (−26 * Hispanic American) + (−27.8 * African American). The equation for the predicted PEF in men was as follows: 320.9 + (−5.6 * age) + (7.9 * height) + (−39.7 * Hispanic American) + (−65.9 * African American). We used these equations to compute a predicted PEF value for each participant. The measured PEF was divided by the predicted PEF to obtain the percentage of the predicted PEF, with scores less than 80% of the predicted PEF indicating low PEF value.
COPD and Shortness of Breath
Physician-diagnosed COPD was recorded from answers to the question: Has a doctor ever told you that you have chronic lung disease such as chronic bronchitis or emphysema? In 2008, participants were asked whether they had persistent or troublesome “Shortness of breath while awake?” (0 = No, 1 = Yes).
Covariates
Age (in years), sex, educational level (in years), race (1 = African American, 0 = others), and ethnicity (1 = Hispanic, 0 = others) were included as demographic covariates in the analyses. In predicting PEF, height was used as a covariate because PEF is higher in taller individuals (Roberts & Mapel, 2012). Physical activity, current and ever cigarette smoking, and body mass index (BMI; kg/m2) were used as covariates as they are related to both personality traits and lung function. For physical activity, participants were asked “how often do you take part in sports or activities that are moderately energetic, such as gardening, cleaning the car, walking at a moderate pace, dancing, floor or stretching exercises” using a scale ranging from 1 (hardly ever or never) to 4 (more than once a week). Similar to the COPD assessment, participants were asked whether a physician has ever told them that they have stroke, heart disease, hypertension, diabetes, cancer, arthritis, and psychiatric disorders (0 = No, 1 = Yes).
Statistical Analyses
To test whether the group with COPD differed from those who did not report COPD on the personality traits, we conducted a multivariate analysis of covariance controlling for demographic variables (age, sex, race, ethnicity, and education), cigarette smoking, physical activity, and BMI. We examined the association between personality and lung function using linear regression to predict PEF as a continuous measure and logistic regression to predict PEF less than 80% of the predicted value. Basic regression models controlled for demographics and height. Given that PEF less than 80% of the predicted value was derived from sex, age, height, race, and ethnicity, those variables were not included as covariates in the analyses predicting PEF less than 80% (the pattern of results was similar when including those demographic covariates). Fully adjusted models controlled for cigarette smoking, physical activity, BMI, COPD, stroke, heart disease, hypertension, diabetes, cancer, arthritis, and psychiatric disorders. Analyses were conducted separately for each trait and also with all traits simultaneously in the same model. We examined whether the association between personality and PEF differed by COPD status by testing interactions between each trait and COPD. We used logistic regression to predict dyspnea. Additional analyses examined whether personality traits at baseline predicted change in PEF from baseline to follow-up. Furthermore, the longitudinal analyses examined the association of personality with risk of incident PEF less than 80% at follow-up among those with PEF more than 80% at baseline. The analyses were conducted using SPSS statistical software. Significance was set at p less than .01 (two tailed).
Results
As reported in Table 1, the 12,670 participants had a mean age of 68 years, 60% were women, 12% were African American, and 8% were Hispanic. About 52% were ever smokers and 13% were current smokers. About 27% of the sample had a PEF below the 80% of the predicted value. About 10% (n = 1,325) reported being told by a physician they had COPD, and the COPD group was more likely to have worse lung function, to be current and former smokers, older, male, not Hispanic, less active, with lower education, and higher BMI compared with those who did not report COPD (Table 1).
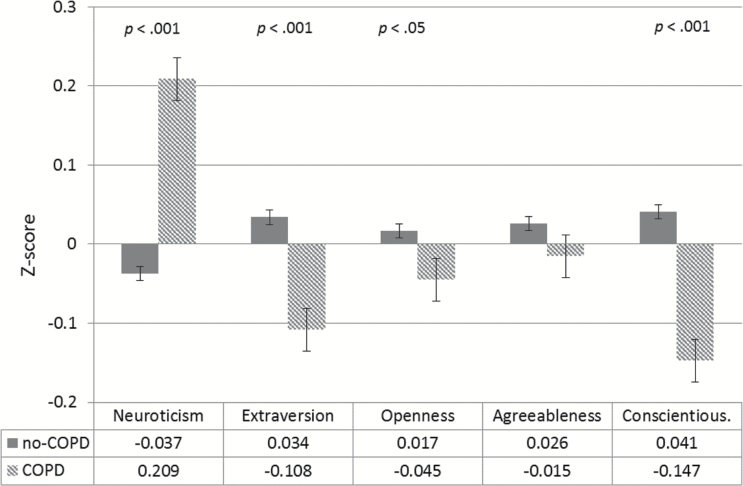
Individuals with COPD had higher scores on neuroticism and lower scores on extraversion, openness, and conscientiousness compared with those who did not report COPD (Table 1). The differences between the two groups remained significant after accounting for basic demographic variables, and Figure 1 illustrates that the effects are about d = 0.2 for neuroticism and conscientiousness. Except for openness, the associations remained significant even when accounting for cigarette smoking, physical activity, and BMI.
Figure 1.
Multivariate analysis of variance with age, sex, education, race, and ethnicity included as covariates. COPD = chronic obstructive pulmonary disease; COPD n = 1,325 and no COPD n = 11,345.
Personality Associations With PEF and PEF less than 80% of the Predicted Value
In linear regression analyses controlling for age, sex, education, race, ethnicity, and height, all five factors were significant predictors of PEF (Model 1, Table 2). All five factors remained significant predictors of PEF in the regression analysis that further adjusted for ever and current smoking, physical activity, BMI, COPD, stroke, heart disease, hypertension, diabetes, cancer, arthritis, and psychiatric disorders (Model 2, Table 2). Comparisons of the βs from Model 1 that included the demographics to the fully adjusted Model 2 indicate that smoking, physical activity, BMI, and disease accounted for about 50% of the association between personality and PEF. When all five factors were entered simultaneously in the fully adjusted regression model, higher openness and higher conscientiousness remained significant predictors of better PEF (Model 3, Table 2).
Table 2.
Results of Regression Analyses With Personality Traits Predicting PEF and PEF <80% of the Predicted Value
| PEF (β) | PEF < 80% (OR) | |||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| Neuroticism | −0.069* | −0.033* | −0.021* | 1.22 (1.14–1.30)* | 1.08 (1.01–1.16) | 1.03 (0.96–1.11) |
| Extraversion | 0.05* | 0.025* | −0.012 | 0.81 (0.75–0.87)* | 0.91 (0.85–0.99) | 1.09 (0.98–1.21) |
| Openness | 0.074* | 0.057* | 0.052* | 0.76 (0.71–0.82)* | 0.80 (0.74–0.86)* | 0.83 (0.75–0.91)* |
| Agreeableness | 0.034* | 0.022* | −0.006 | 0.84 (0.77–0.91)* | 0.88 (0.80–0.96)* | 1.00 (0.89–1.12) |
| Conscientiousness | 0.073* | 0.043* | 0.023* | 0.67 (0.62–0.73)* | 0.77 (0.70–0.84)* | 0.82 (0.74–0.91)* |
Notes. BMI = body mass index; COPD = chronic obstructive pulmonary disease; OR = odds ratio; PEF = peak expiratory flow.
Model 1 adjusted for age, sex, education, race, ethnicity, and height. For PEF < 80%, age, sex, race, ethnicity, and height were not included as covariates given that the prediction equations for PEF < 80% is based on these variables. Model 2 includes Model 1 covariates and ever and current smoking, moderate physical activity, BMI, COPD, stroke, heart disease, hypertension, diabetes, cancer, arthritis, and psychiatric disorders. Model 3 includes Model 2 covariates and all five factors in the same model. βs are from linear regressions predicting continuous PEF; OR from logistic regressions predicting PEF < 80% of the predicted value.
*p < .01.
Logistic regression indicated that 1 SD lower scores on neuroticism or higher scores on the other four traits were associated with about 20% to almost 50% (for conscientiousness) reduced risk of PEF less than 80% of the predicted value. The associations were attenuated but remained significant for openness and conscientiousness when adjusting for smoking, physical activity, BMI, disease, and the other personality traits (Table 2).
Personality and PEF by COPD Status
To examine whether the association between personality traits and lung function differed between those with and without COPD, we tested the interaction between each trait and COPD status in the fully adjusted regression models. None of the interactions were significant, indicating that the association between personality traits and PEF did not differ by COPD status. Follow-up analyses controlling for demographic variables further confirmed that among those with COPD (n = 1,325), all five factors were related to PEF. When all five factors were entered simultaneously, openness (β = 0.11) and conscientiousness (β = 0.07) were significant predictors.
Personality and Change in PEF Over the 4-Year Follow-up
We examined whether personality traits predicted change in PEF over the 4-year follow-up, from the 2006–2008 baseline assessment to the 2010–2012 follow-up assessment (n = 9,362). In addition to the five personality factors and covariates (age, sex, education, race, ethnicity, and height), PEF at baseline was included in the analyses as a predictor of PEF at follow-up. Worsening of PEF over the 4-year interval was predicted by higher scores on neuroticism (β = −0.019; p = .002) and lower scores on conscientiousness (β = .027, p < .001). In additional analyses, we tested whether personality traits were associated with increased risk of PEF less than 80% at follow-up among those with PEF more than 80% at baseline. This analysis included n = 7,183 participants with normal PEF at baseline, of whom 810 (11%) performed below the 80% of the predicted value at follow-up. We found that conscientiousness was associated with reduced risk of incident PEF less than 80% of the predicted value (OR = 0.67, 95% confidence interval [CI] = 0.57–0.79), and there were marginal associations with neuroticism (OR = 1.12, 95% CI = 1.00–1.27) and agreeableness (OR = 0.82, 95% CI = 0.71–0.96).
Personality and Dyspnea
Next, we examined to what extent personality traits predict shortness of breath (dyspnea) beyond what can be explained by lung capacity and physical and mental health. In logistic regressions that accounted for demographic variables, all five personality traits were predictors of dyspnea (Table 3). Of note, the probability of reporting dyspnea roughly doubled for each standard deviation higher score on neuroticism and lower score on extraversion or conscientiousness. All five factors remained significant predictors when further adjusted for lung function (PEF), ever and current smoking, physical activity, BMI, and disease. Except for openness, the other four traits were still significant predictors when entered simultaneously in the fully adjusted regression model.
Table 3.
Results of Regression Analyses With Personality Traits Predicting Shortness of Breath
| OR | |||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| Neuroticism | 1.87 (1.72−2.03)* | 1.52 (1.38–1.67)* | 1.39 (1.26–1.53)* |
| Extraversion | 0.56 (0.51–0.61)* | 0.66 (0.60–0.73)* | 0.71 (0.62–0.81)* |
| Openness | 0.71 (0.65–0.78)* | 0.75 (0.68–0.83)* | 0.98 (0.86–1.12) |
| Agreeableness | 0.77 (0.69–0.85)* | 0.80 (0.71–0.91)* | 1.21 (1.03–1.41)* |
| Conscientiousness | 0.52 (0.47–0.57)* | 0.67 (0.60–0.75)* | 0.79 (0.69–0.90)* |
Notes. BMI = body mass index; COPD = chronic obstructive pulmonary disease; OR = odds ratio; PEF = peak expiratory flow.
Model 1 adjusted for age, sex, education, race, and ethnicity. Model 2 includes Model 1 covariates and lung function (PEF), ever and current smoking, moderate physical activity, BMI, COPD, stroke, heart disease, hypertension, diabetes, cancer, arthritis, and psychiatric disorders. Model 3 includes Model 2 covariates and all five factors simultaneously entered in the same model.
*p < .01.
To examine whether personality predicted dyspnea among patients with lung disease, we tested the interaction between each trait and COPD status in the above fully adjusted model and repeated the analyses in the group with COPD. None of the interactions were significant, suggesting that personality predicts symptoms of dyspnea similarly for those with and without COPD. In the subsample with COPD, with the exception of openness, personality traits were associated with the reporting of dyspnea in a fully adjusted model with all factors entered simultaneously. Similar results were obtained in the subsample with PEF less than 80% of the predicted value (results not shown).
Discussion
With data from a large national sample of older adults, this study found that personality traits are associated with lung function (PEF), lung disease (COPD), and the associated symptomatology (dyspnea). In particular, older adults with higher neuroticism and lower conscientiousness were more likely to have lower PEF and a steeper PEF decline over time, to have COPD, and to suffer from dyspnea. The findings contribute to the aging, personality and health literature. The pattern of associations was consistent across the self-report measures and the performance-based biomarker. Furthermore, the associations between personality traits and PEF or dyspnea were similar among those with or without COPD, suggesting that the association between personality traits and lung function is not disease dependent (i.e., the observed pattern of association is unlikely to be caused by the disease or the COPD ascertainment method). The associations were attenuated but remained significant when accounting for potential mediators and confounders, such as cigarette smoking, physical activity, BMI, and several chronic diseases. Conscientiousness had the strongest and most consistent associations.
The significant differences in both neuroticism and conscientiousness between those with and without COPD are consistent with a large literature that links these personality traits to chronic diseases among older adults (Chapman et al., 2012; Goodwin & Friedman, 2006; Hampson, 2012; Jokela, Pulkki-Råback, Elovainio, & Kivimäki, 2014; Luchetti, Terracciano, Stephan, & Sutin, 2015; Sutin et al., 2013; Terracciano et al., 2014; Weston et al., 2014). COPD is mainly caused by tobacco smoking (DHHS, 2014), and similar to COPD, smokers tend to score higher on neuroticism and lower on conscientiousness (Malouff, Thorsteinsson, & Schutte, 2006; Terracciano & Costa, 2004; Terracciano, Löckenhoff, Zonderman, Ferrucci, & Costa, 2008; Turiano, Whiteman, Hampson, Roberts, & Mroczek, 2012). Of interest, there is longitudinal evidence that higher neuroticism and lower conscientiousness in children and adolescents predict cigarette smoking into adulthood (Cherry & Kiernan, 1976; Hampson, Goldberg, Vogt, & Dubanoski, 2006; Harakeh, Scholte, de Vries, & Engels, 2006; Kubicka, Matejcek, Dytrych, & Roth, 2001; Munafò & Black, 2007), which suggests that by increasing risk of smoking, personality may be a risk factor for the eventual development of COPD. For neuroticism, however, there is also evidence that being a smoker has a negative effect on mood and increases anxiety and depression (Jamal, Willem Van der Does, Cuijpers, & Penninx, 2012; Johnson et al., 2000; Parrott, 1998), whereas quitting smoking is associated with reduced depression, anxiety, and stress (Taylor et al., 2014). Thus, our findings and previous studies suggest that although personality traits are likely to contribute to the etiology of COPD, cigarette smoking and lung disease may also be associated with change in personality (Jokela, Hakulinen, Singh-Manoux, & Kivimäki, 2014; Sutin et al., 2013).
Our study also found that irrespective of COPD status, personality predicted concurrent PEF and change in PEF over time. For example, 1 SD higher score on conscientiousness was associated with about a 50% reduced risk of PEF less than 80% of the predicted value. This finding is noteworthy for several reasons. First, among those with COPD, it suggests that personality traits have clinical relevance because neuroticism and conscientiousness predict (a) the current level of PEF performance and (b) the rate of decline in lung function. Second, similar to anxiety and depression (Maurer et al., 2008; von Leupoldt, Taube, Lehmann, Fritzsche, & Magnussen, 2011), personality traits can aid in detecting individuals with worse functioning and symptomatology and those with worse prognosis in terms of accelerated functional decline. Third, personality traits are also related to treatment adherence (Axelsson, Brink, Lundgren, & Lötvall, 2011), and thus personality may help to identify patients who need greater surveillance. Finally, similar to psychiatric conditions, individuals who score higher on neuroticism can benefit from psychotherapy, medications such as antidepressants and anxiolytics, or other interventions (Costa, Bagby, Herbst, & McCrae, 2005; Tang et al., 2009). One advantage of assessing personality over psychiatric diagnoses is that conditions such as anxiety disorder affect a relatively small proportion of the population, whereas personality assessments characterize the entire population.
The performance-based PEF findings also corroborate the results based on the self-reported measure of COPD and the reporting of dyspnea. This convergence is reassuring because COPD is underdiagnosed (Bednarek et al., 2008) and the response to questions on physician-diagnosed COPD tend to have low sensitivity (Murgia et al., 2014). According to a report from the Centers for Disease Control and Prevention (CDC, 2002), about 10 million Americans reported physician-diagnosed COPD in 2000, but about 24 million were estimated to have spirometry-based evidence of impaired lung function, according to data from the National Health and Nutrition Examination Survey (NHANES; Mannino et al., 2000). The reporting and diagnosis of COPD is further complicated by its considerable overlap with asthma (Zeki, Schivo, Chan, Albertson, & Louie, 2011). Responses to questions related to diseases are also subject to potential recall biases, and individuals who score higher on neuroticism are more likely to report more symptoms, to be hypochondriacs, and thus more likely to be diagnosed (Costa & McCrae, 1987). Despite a range of potential biases and limitations, a consistent pattern of results emerged across self-reports and a performance-based biomarker. The PEF results are also broadly consistent with data from the Baltimore Longitudinal Study of Aging that found that lower neuroticism and higher extraversion, openness, and conscientiousness were associated with greater aerobic capacity at maximal sustained walking speed (Terracciano et al., 2013). Similarly, in the Health, Aging, and Body Composition study, older adults who scored higher on conscientiousness maintained a faster gait speed over a 3-year follow-up (Tolea et al., 2012). Thus, across different assessment paradigms, there is consistent evidence that personality traits are associated with older adults’ cardiorespiratory fitness.
Shortness of breath is not simply a function of lung capacity, physical health, or psychiatric conditions. There is no perfect correspondence between the level of airflow limitation and the reports of symptoms (Agusti et al., 2010). Personality may explain some of the variability in the clinical manifestation of COPD. Indeed, our findings indicate that personality was associated with shortness of breath among those with and without COPD. These associations are in part explained by personality links with health behaviors (e.g., tobacco smoking) and objective health status (e.g., PEF), and indeed the association was attenuated when including these variables in the model. Personality traits are also related to other influential factors, from the individual’s lifestyle (Stephan, Boiché, Canada, & Terracciano, 2014) to adherence to medications and other medical treatments (Axelsson et al., 2011). But even after accounting for demographic factors, cigarette smoking, lung function, heart disease, and psychiatric and other medical conditions, personality traits remained significant predictors of dyspnea. Of clinical relevance, personality was a significant predictor also in the subgroup with poor lung function (PEF < 80% of the predicted value).
Limitations of this study are mainly the brief assessment of the study variables. However, the large HRS sample size compensates for some of the inaccuracy due to the simpler measurement methods. In particular, spirometry is the gold standard to assess lung function, but it is more time consuming and expensive than the simple PEF test. Although not interchangeable, PEF and spirometry-assessed FEV1 (forced expiratory volume in 1 second) are highly correlated (e.g., r = .87 in 300 COPD patients; Pothirat et al., 2015). Further, PEF less than 80% of the predicted value identifies more than 90% of COPD patients and 100% of those with moderate-to-severe COPD (Jackson & Hubbard, 2003). Similarly, detailed personality questionnaires could provide a more reliable and in-depth assessment, but those are generally more time consuming. The MIDI has weak convergent and discriminant validity, and especially the agreeableness scale is far from optimal. More detailed questionnaires could provide data on the facets that compose each of the five factors that may increase the predictive power of personality (Paunonen & Ashton, 2001; Terracciano et al., 2014). Another limitation was the attrition of participants who were older, with limited lung function, lower education, and a more vulnerable personality. Despite such loss of follow-up of participants who were most at-risk, the longitudinal analyses indicated that neuroticism and conscientiousness were associated with worsening lung function.
Despite the limitations, this study clearly indicates that major dimensions of personality, and, in particular neuroticism and conscientiousness, are consistent predictors of lung function and disease among older adults. The associations are evident in the full national sample and in the subgroup with COPD. Thus, the study points to the personality characteristics of those with COPD and suboptimal peak flow performance and supports the notion of reciprocal relations between psychological dispositions and lung function. Similar to psychiatric comorbidities, personality traits can identify individuals at greater risk and with worse prognosis, which has translational utility for the care of older adults.
Funding
HRS is supported by the National Institute on Aging (NIA U01AG009740). For this article, the authors received no specific grant from any funding agency, commercial or not-for-profit sectors.
References
- Agusti A. Calverley P. M. Celli B. Coxson H. O. Edwards L. D. Lomas D. A., … Vestbo J; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) investigators. (2010). Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respiratory Research, 11, 122. doi:10.1186/1465-9921-11-12220831787 [Google Scholar]
- Axelsson M., Brink E., Lundgren J., Lötvall J. (2011). The influence of personality traits on reported adherence to medication in individuals with chronic disease: An epidemiological study in West Sweden. PLoS One, 6, e18241. doi:10.1371/journal.pone.0018241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bednarek M., Maciejewski J., Wozniak M., Kuca P., Zielinski J. (2008). Prevalence, severity and underdiagnosis of COPD in the primary care setting. Thorax, 63, 402–407. doi:10.1136/thx.2007.085456 [DOI] [PubMed] [Google Scholar]
- CDC. (2002). Chronic Obstructive Pulmonary Disease Surveillance—United States, 1971–2000. Morbidity and Mortality Weekly Report, 51, 1–16. [PubMed] [Google Scholar]
- Chapman B. P. Roberts B. Lyness J., & Duberstein P. (2012). Personality and physician-assessed illness burden in older primary care patients over 4 years. The American Journal of Geriatric Psychiatry, 21, 737–746. doi:10.1016/j.jagp.2012.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherry N., Kiernan K. (1976). Personality scores and smoking behaviour. A longitudinal study. British Journal of Preventive & Social Medicine, 30, 123–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa P. T., Jr., Bagby R. M., Herbst J. H., McCrae R. R. (2005). Personality self-reports are concurrently reliable and valid during acute depressive episodes. Journal of Affective Disorders, 89, 45–55. doi:10.1016/j.jad.2005.06.010 [DOI] [PubMed] [Google Scholar]
- Costa P. T. Jr., & McCrae R. R (1987). Neuroticism, somatic complaints, and disease: Is the bark worse than the bite? Journal of Personality, 55, 299–316. [DOI] [PubMed] [Google Scholar]
- DeCarlo C. A. MacDonald S. W. Vergote D. Jhamandas J. Westaway D., & Dixon R. A (2015). Vascular health and genetic risk affect mild cognitive impairment status and 4-year stability: Evidence from the Victoria Longitudinal Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. doi:10.1093/geronb/gbv043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DHHS (2014). The Health Consequences of Smoking–50 Years of Progress: A Report of the Surgeon General. [Google Scholar]
- Goodwin R. D., Friedman H. S. (2006). Health status and the five-factor personality traits in a nationally representative sample. Journal of Health Psychology, 11, 643–654. doi:10.1177/1359105306066610 [DOI] [PubMed] [Google Scholar]
- Halbert R. J., Natoli J. L., Gano A., Badamgarav E., Buist A. S., Mannino D. M. (2006). Global burden of COPD: Systematic review and meta-analysis. The European Respiratory Journal, 28, 523–532. doi:10.1183/09031936.06.00124605 [DOI] [PubMed] [Google Scholar]
- Hampson S. E. (2012). Personality processes: Mechanisms by which personality traits “get outside the skin.” Annual Review of Psychology, 63, 315–339. doi:10.1146/annurev-psych-120710-100419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson S. E., Goldberg L. R., Vogt T. M., Dubanoski J. P. (2006). Forty years on: Teachers’ assessments of children’s personality traits predict self-reported health behaviors and outcomes at midlife. Health Psychology, 25, 57–64. doi:10.1037/0278-6133.25.1.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harakeh Z., Scholte R. H., de Vries H., Engels R. C. (2006). Association between personality and adolescent smoking. Addictive Behaviors, 31, 232–245. doi:10.1016/j.addbeh.2005.05.003 [DOI] [PubMed] [Google Scholar]
- Hoyert D. L., & Xu J. Q (2012). Deaths: Preliminary data for 2011. The National Vital Statistics Report. Hyattsville, MD: Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- HRS. (2006, 2008, 2010, and 2012). Core public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740).
- Ito K., Barnes P. J. (2009). COPD as a disease of accelerated lung aging. Chest, 135, 173–180. doi:10.1378/chest.08-1419 [DOI] [PubMed] [Google Scholar]
- Jackson H., Hubbard R. (2003). Detecting chronic obstructive pulmonary disease using peak flow rate: Cross sectional survey. British Medical Journal, 327, 653–654. doi:10.1136/bmj.327.7416.653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal M., Willem Van der Does A. J., Cuijpers P., Penninx B. W. (2012). Association of smoking and nicotine dependence with severity and course of symptoms in patients with depressive or anxiety disorder. Drug and Alcohol Dependence, 126, 138–146. doi:10.1016/j.drugalcdep.2012.05.001 [DOI] [PubMed] [Google Scholar]
- Johnson J. G., Cohen P., Pine D. S., Klein D. F., Kasen S., Brook J. S. (2000). Association between cigarette smoking and anxiety disorders during adolescence and early adulthood. Journal of the American Medical Association, 284, 2348–2351. [DOI] [PubMed] [Google Scholar]
- Jokela M., Hakulinen C., Singh-Manoux A., Kivimäki M. (2014). Personality change associated with chronic diseases: Pooled analysis of four prospective cohort studies. Psychological Medicine, 44, 2629–2640. doi:10.1017/S0033291714000257 [DOI] [PubMed] [Google Scholar]
- Jokela M., Pulkki-Råback L., Elovainio M., Kivimäki M. (2014). Personality traits as risk factors for stroke and coronary heart disease mortality: Pooled analysis of three cohort studies. Journal of Behavioral Medicine, 37, 881–889. doi:10.1007/s10865-013-9548-z [DOI] [PubMed] [Google Scholar]
- Kern M. L., Friedman H. S. (2008). Do conscientious individuals live longer? A quantitative review. Health Psychology, 27, 505–512. doi:10.1037/0278-6133.27.5.505 [DOI] [PubMed] [Google Scholar]
- Kubicka L. Matejcek Z. Dytrych Z., & Roth Z (2001). IQ and personality traits assessed in childhood as predictors of drinking and smoking behaviour in middle-aged adults: A 24-year follow-up study. Addiction, 96, 1615–1628. [DOI] [PubMed] [Google Scholar]
- Lachman M. E. (Ed.). (2001). Handbook of midlife development. New York, NY: Wiley. [Google Scholar]
- Lopez A. D. Shibuya K. Rao C. Mathers C. D. Hansell A. L. Held L. S. … Buist S (2006). Chronic obstructive pulmonary disease: Current burden and future projections. The European Respiratory Journal, 27, 397–412. doi:10.1183/09031936.06.00025805 [DOI] [PubMed] [Google Scholar]
- Luchetti M., Barkley J. M., Stephan Y., Terracciano A., Sutin A. R. (2014). Five-factor model personality traits and inflammatory markers: New data and a meta-analysis. Psychoneuroendcocrinology, 50, 181–193. doi:10.1016/j.psyneuen.2014.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchetti M. Terracciano A. Stephan Y., & Sutin A. R (2015). Personality and cognitive decline in older adults: Data from a longitudinal sample and meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. doi:10.1093/geronb/gbu184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malouff J. M., Thorsteinsson E. B., Schutte N. S. (2006). The five-factor model of personality and smoking: A meta-analysis. Journal of Drug Education, 36, 47–58. [DOI] [PubMed] [Google Scholar]
- Mannino D. M., Gagnon R. C., Petty T. L., Lydick E. (2000). Obstructive lung disease and low lung function in adults in the United States: Data from the National Health and Nutrition Examination Survey, 1988–1994. Archives of Internal Medicine, 160, 1683–1689. [DOI] [PubMed] [Google Scholar]
- Maurer J. Rebbapragada V. Borson S. Goldstein R. Kunik M. E. Yohannes A. M., … Depression in, C. (2008). Anxiety and depression in COPD: Current understanding, unanswered questions, and research needs. Chest, 134(4 Suppl), 43S–56S. doi:10.1378/chest.08-0342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae R. R., John O. P. (1992). An introduction to the five-factor model and its applications. Journal of Personality, 60, 175–215. [DOI] [PubMed] [Google Scholar]
- Munafò M. R., Black S. (2007). Personality and smoking status: A longitudinal analysis. Nicotine & Tobacco Research, 9, 397–404. doi:10.1080/14622200701188869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murgia N., Brisman J., Claesson A., Muzi G., Olin A. C., Torén K. (2014). Validity of a questionnaire-based diagnosis of chronic obstructive pulmonary disease in a general population-based study. BMC Pulmonary Medicine, 14, 49. doi:10.1186/1471-2466-14-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrott A. C. (1998). Nesbitt’s Paradox resolved? Stress and arousal modulation during cigarette smoking. Addiction, 93, 27–39. [DOI] [PubMed] [Google Scholar]
- Paunonen S. V., Ashton M. C. (2001). Big five factors and facets and the prediction of behavior. Journal of Personality and Social Psychology, 81, 524–539. [PubMed] [Google Scholar]
- Pothirat C. Chaiwong W. Phetsuk N. Liwsrisakun C. Bumroongkit C. Deesomchok A., … Limsukon A (2015). Peak expiratory flow rate as a surrogate for forced expiratory volume in 1 second in COPD severity classification in Thailand. International Journal of Chronic Obstructive Pulmonary Disease, 10, 1213–1218. doi:10.2147/COPD.S85166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts M. H., Mapel D. W. (2012). Limited lung function: Impact of reduced peak expiratory flow on health status, health-care utilization, and expected survival in older adults. American Journal of Epidemiology, 176, 127–134. doi:10.1093/aje/kwr503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan Y., Boiché J., Canada B., Terracciano A. (2014). Association of personality with physical, social, and mental activities across the lifespan: Findings from US and French samples. British Journal of Psychology, 105, 564–580. doi:10.1111/bjop.12056 [DOI] [PubMed] [Google Scholar]
- Stephan Y. Sutin A. R., & Terracciano A (2014). Physical activity and personality development across adulthood and old age: Evidence from two longitudinal studies. Journal of Research in Personality, 49, 1–7. [Google Scholar]
- Suissa S. Dell’Aniello S., & Ernst P (2012). Long-term natural history of chronic obstructive pulmonary disease: Severe exacerbations and mortality. Thorax, 67, 957–963. doi:10.1136/thoraxjnl-2011–201518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin A. R., Zonderman A. B., Ferrucci L., Terracciano A. (2013). Personality traits and chronic disease: Implications for adult personality development. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 68, 912–920. doi:10.1093/geronb/gbt036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang T. Z., DeRubeis R. J., Hollon S. D., Amsterdam J., Shelton R., Schalet B. (2009). Personality change during depression treatment: A placebo-controlled trial. Archives of General Psychiatry, 66, 1322–1330. doi:10.1001/archgenpsychiatry.2009.166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor G. McNeill A. Girling A. Farley A. Lindson-Hawley N., & Aveyard P (2014). Change in mental health after smoking cessation: Systematic review and meta-analysis. British Medical Journal, 348, g1151. doi:10.1136/bmj.g1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A., Costa P. T., Jr (2004). Smoking and the Five-Factor Model of personality. Addiction, 99, 472–481. doi:10.1111/j.1360-0443.2004.00687.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A., Löckenhoff C. E., Zonderman A. B., Ferrucci L., Costa P. T., Jr (2008). Personality predictors of longevity: Activity, emotional stability, and conscientiousness. Psychosomatic Medicine, 70, 621–627. doi:10.1097/PSY.0b013e31817b9371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A., Schrack J. A., Sutin A. R., Chan W., Simonsick E. M., Ferrucci L. (2013). Personality, metabolic rate and aerobic capacity. PLoS One, 8, e54746. doi:10.1371/journal.pone.0054746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A., Sutin A. R., An Y., O’Brien R. J., Ferrucci L., Zonderman A. B., Resnick S. M. (2014). Personality and risk of Alzheimer’s disease: New data and meta-analysis. Alzheimer’s & Dementia, 10, 179–186. doi:10.1016/j.jalz.2013.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolea M. I., Costa P. T., Terracciano A., Ferrucci L., Faulkner K., Coday M. M. C., Study B. C. (2012). Associations of openness and conscientiousness with walking speed decline: Findings from the health, aging, and body composition study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 705–711. doi:10.1093/geronb/gbs030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano N. A. Whiteman S. D. Hampson S. E. Roberts B. W., & Mroczek D. K (2012). Personality and substance use in midlife: Conscientiousness as a moderator and the effects of trait change. Journal of Research in Personality, 46, 295–305. doi:10.1016/j.jrp.2012.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vestbo J. Hurd S. S. Agustí A. G. Jones P. W. Vogelmeier C. Anzueto A., … Rodriguez-Roisin R. (2013). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine, 187, 347–365. doi:10.1164/rccm.201204-0596PP [DOI] [PubMed] [Google Scholar]
- von Leupoldt A., Taube K., Lehmann K., Fritzsche A., Magnussen H. (2011). The impact of anxiety and depression on outcomes of pulmonary rehabilitation in patients with COPD. Chest, 140, 730–736. doi:10.1378/chest.10-2917 [DOI] [PubMed] [Google Scholar]
- Weston S. J. Hill P. L., & Jackson J. J (2014). Personality traits predict the onset of disease. Social Psychological and Personality Science, 1–9. doi:0.1177/1948550614553248 [Google Scholar]
- Zeki A. A., Schivo M., Chan A., Albertson T. E., Louie S. (2011). The asthma-COPD overlap syndrome: A common clinical problem in the elderly. Journal of Allergy, 2011, 861926. doi:10.1155/2011/861926 [DOI] [PMC free article] [PubMed] [Google Scholar]