Abstract
Objectives
Physical activity is a key health behavior that reduces disease risk, and yet most older adults are not very active. This study examined time-varying associations between physical activity and a recognized barrier, namely, precipitation. And it examined the moderating role of physical activity intentions and functional mobility on precipitation–physical activity associations.
Method
One hundred and twenty-six older adults (M age = 72 years; 64% women) from Metro Vancouver provided health and background information and wore triaxial accelerometers for up to 10 consecutive days. Daily weather information was collected from local weather stations.
Results
Multilevel models corroborate previous research by showing that older adults engaged in less physical activity on days with increased precipitation across four indices: activity counts, step counts, minutes of moderate to vigorous physical activity (MVPA), and bout-corrected minutes of MVPA. Older adults with strong physical activity intentions engaged in more physical activity overall. Physical activity intentions also modified the association between time-varying precipitation and activity counts and step counts, whereas functional mobility moderated the negative association between precipitation and activity counts and minutes of MVPA.
Discussion
Findings highlight the important role of time-varying influences on physical activity and how these associations are moderated by psychological and biological factors.
Keywords: Intention, Intra-individual variability, Physical activity, Weather
Physical activity is identified as one of the highest priorities for health promotion because it reduces the risk of many chronic diseases such as cardiovascular disease, stroke, Type 2 diabetes, cognitive decline, and it improves well-being (Almeida et al., 2014; Blair, 2009; Brassington, Hekler, Cohen, & King, 2012; Haskell et al., 2007; Nelson et al., 2007). Engaging in physical activity is relatively inexpensive compared with the health care costs of chronic disease; yet, more than half of North American older adults do not meet physical activity guidelines (Ashe, Miller, Eng, & Noreau, 2008; Brassington et al., 2012; Brown, Yore, Ham, & Macera, 2001). Physical activity does not have to occur in the form of structured exercise; engaging in physical activity as part of one’s daily life routines may be more sustainable than specific exercise regimens. The purpose of this study, therefore, was to target physical activity as captured by up to 10 days of accelerometer information, using a sample of 126 community-dwelling older adults from the Metro Vancouver, Canada area (M age = 72 years) who went about their typical daily life routines. We were especially interested in the day-to-day variability of physical activity and its association with a recognized barrier to physical activity—poor weather. We also examined how older adults with low, as compared with high, functional mobility are affected by inclement weather and whether their physical activity intentions would moderate time-varying weather–physical activity associations.
North American guidelines recommend that to achieve substantial health benefits older adults need to accumulate a minimum of 150 minutes of moderate to vigorous intensity physical activity (MVPA) per week in at least 10-minute bouts (Canadian Society for Exercise Physiology, 2012; U.S. Department of Health and Human Services, 2008). Physical activity is defined as bodily movement that involves skeletal muscles requiring energy expenditure (Caspersen, Powell, & Christenson, 1985). This definition of physical activity is intentionally broad; physical activity is not limited to structured exercise. Therefore, guidelines can be met by engaging in tasks where the primary purpose is something other than physical activity as long as they involve moderate to high intensity movement such as utilitarian walking, gardening, completing heavy household chores, or lifting and playing with grandchildren.
Previous research on physical activity demonstrates that the lion’s share of variability in this key health behavior is not associated with differences between persons but with time-varying situational characteristics (Dunton, Atienza, Castro, & King, 2009; Scholz, Keller, & Perren, 2009). This emphasizes the need to take physical activity research out of the lab and into older adults’ daily lives and to investigate how physical activity is impacted by time-varying circumstances such as the weather.
The weather is a prototypical example of a fluctuating circumstance that has clear ramifications for physical activity (Brandon, Gill, Speechley, Gilliland, & Jones, 2009; Dunn, Shaw, & Trousdale, 2012; Merchant, Dehghan, & Akhtar-Danesh, 2007; Tucker & Gilliland, 2007; Witham et al., 2014). Some weather conditions such as those leading to icy streets and sidewalks create barriers to physical activity, and they also increase falls and injury risks in older adults (Lord, Sherrington, Menz, & Close, 2007). Other weather conditions involving precipitation may be more unpleasant than dangerous, but they too reduce physical activity in older adults (Brandon et al., 2009; Feinglass et al., 2011; Klenk, Büchele, Rapp, Franke, & Peter, 2012). To examine associations between poor weather and physical activity, our study aimed to replicate and extend previous research regarding a negative association between daily physical activity and precipitation in adulthood (Feinglass et al., 2011). We specifically focused on precipitation because precipitation per se does not rule out most types of physical activities, but it makes them less enjoyable. Thus focusing on precipitation allowed us to examine the influences of a time-varying unpleasant circumstance on physical activity also taking into account potential moderators of the proposed negative physical activity–precipitation association to better understand what might be done to help older adults capitalize on good opportunities to be physically active in their daily lives.
Today’s older adults are generally of better health than past cohorts, but there is considerable variability in older adults’ health and in their motivation to be physically active (Baltes & Smith, 2003; Chipperfield, Newall, Chuchmach, Swift, & Haynes, 2008; Sarkin, Johnson, Prochaska, & Prochaska, 2001; Ziegelmann, Lippke, & Schwarzer, 2006a). The present study thus aimed to examine the role of one physical health and one psychological motivational factor in moderating the expected negative precipitation–physical activity association. We focused on functional mobility as a physical health measure because of its immediate relevance for physical activity engagement (Whitney, Lord, & Close, 2005). Functional mobility can be operationally defined as the speed with which an individual performs basic mobility tasks such as getting up, walking, turning, and sitting down that are necessary skills for going outside safely (Podsiadlo & Richardson, 1991; Whitney et al., 2005). We expected that older adults with high functional mobility would be better equipped to manage barriers to physical activity such as precipitation than older adults with low functional mobility.
Many psychological models of health behavior change are built on the idea that intentions are key predictors of behavior (Ajzen, 1991; Brassington et al., 2012; Rogers, 1983; Sheeran, 2002). There is substantial evidence to support this assumption. Previous research has shown that adults who have strong intentions to be physically active are more likely to come through than those with weak physical activity intentions and that adults are more physically active on days characterized by high as compared with low intention strength (Ajzen, 1991; Brassington et al., 2012; Conroy, Elavsky, Doerksen, & Maher, 2013; Rogers, 1983; Sheeran, 2002). Yet, translating intentions into behavior is not a simple task, and many individuals encounter barriers when trying to do so (Sheeran, 2002) including but not limited to precipitation (Witham et al., 2014). The present study therefore examined whether older adults with strong as compared with weaker physical activity intentions have higher overall levels of physical activity and also whether the predicted negative impact of precipitation on older adults’ physical activity is moderated by physical activity intention strength.
To explore varying interpretations of the anticipated associations between physical activity, precipitation, functional mobility, and physical activity intentions, we also collected data on individual characteristics such as age, gender, self-rated health, heritage, and seasonal effects (Benyamini, 2011; Conroy, Elavsky, Hyde, & Doerksen, 2011; Witham et al., 2014). In addition to recording the daily amount of precipitation, we also considered temperature and weekend versus weekday effects (Brandon et al., 2009; Conroy et al., 2011) in all analyses.
The purpose of this study was to replicate and extend previous evidence on time-varying associations between physical activity using accelerometer data and objectively measured precipitation in a sample of community-dwelling older adults. In addition, we also investigated potential moderators of the proposed negative precipitation–physical activity link. Specifically, we explored whether older adults with high functional mobility and strong physical activity intentions would be less negatively impacted by the effect of precipitation on physical activity than older adults with low functional mobility and week intentions.
Method
Participants
Participants were 142 community-dwelling older adults from Metro Vancouver, Canada. Participants were recruited through media advertisements and local community centers. Eligibility requirements were being 65 years or older, able to read newspaper sized print and to hear an alarm clock, able to speak and understand English, Cantonese, or Mandarin, free of any health conditions for which exercise is contraindicated, and free of any neurodegenerative disease or brain dysfunction.
Of those who consented to participate, three failed to complete the study. Another 11 participants did not provide usable data because of technical problems with the accelerometer unit or human error. Two further participants were excluded from analyses because of below normal functional mobility (Whitney et al., 2005). The remaining 126 older adults had an average age of 71.90 years (SD = 5.00; 64–93 years [one participant turned 65 years within the same calendar years as data collection took place but was still 64 years of age at time of study]; 64% women). The majority of them were retired (89%) and were of European or Asian heritage (62% European heritage; 36% Asian heritage; 1% other; and 1% missing). Close to half of the sample was married (49% married; 2% cohabiting; 18% divorced; 14% single; 14% widowed; and 3% other). Education ranged from less than 9 years of schooling to having earned a university degree, with the majority having had some university education (63%). On average, participants perceived their health to be good (M = 3.64; SD = .92; 1 = poor to 5 = excellent), but 21% reported having fallen over the previous 12 months. Each participant received a $100 honorarium for completing the study. The University of British Columbia’s Behavioral Research Ethics Board approved the study.
Procedure
With an average precipitation of 1,167.3mm/year, Vancouver is one of the rainiest cities of the world; almost twice as rainy as London, England (Climatemps, 2015). Data collection took place between May 2011 and September 2011, a time of year where there is no snow and ice on the ground.
The project started with a 3-hour Baseline session held in the Psychology Department of the University of British Columbia. In the course of this session, we used the instruments described below for collecting data on sociodemographic characteristics, physical activity intentions, and physical health. In addition, we used the Baseline session for instructing participants on the use of a hip-mounted triaxial accelerometer (ActiGraph GT3X, ActiGraph, Pensacola, FL). Participants then started a 10-day phase during which they completed daily diaries and wore the accelerometer. Finally, participants returned to the lab to deliver the equipment, to complete additional psychological measures, and to provide feedback on their experience. Participants rated the 10 days during which they participated as typical of their daily lives (M = 4.02; SD = 1.16; 1 [not at all typical of everyday life] to 5 [very much typical of everyday life]).
Measures
Physical Activity Intentions
At Baseline, participants rated their intentions to be physically active using five intention items that were adapted from previous research (Ziegelmann, Lippke, & Schwarzer, 2006b). The items specifically targeted physical activity and were not limited to exercise. The physical activity intention measure included intensity (e.g., “I intend to work up a sweat regularly.”), frequency (“I intend to be physically active several times a week.”), and duration (“I intend to engage in at least 150 minutes (2.5 hours) of moderate to vigorous physical activity a week, in bouts of 10 minutes or more.”) items. Agreement was rated on a five-point Likert scale: 1 (not at all true) to 5 (absolutely true). Averaged across all five items, our participants had an average physical activity intention rating of 4.27 (SD = .71). A Cronbach’s alpha of .80 in this sample indicates satisfactory internal consistency.
Functional Mobility
At Baseline, functional mobility was assessed with the Timed Up and Go test (TUG; Podsiadlo & Richardson, 1991). For the test, a participant is required to stand up from a sitting position without the use of hands, to walk at their usual walking speed for 3 m, and to turn around, walk back, and sit down again. On average, our sample needed 8.42 seconds to complete this test (SD = 1.66), which is within the range of normal mobility (Whitney et al., 2005). Note that high values indicate low functional mobility.
Physical Activity
Starting in the morning after the Baseline session, participants wore a preprogrammed triaxial accelerometer on an elastic waistband above their dominant hip for 10 consecutive days during waking hours. This accelerometer is commonly used in physical activity research (Gorman, Hanson, Yang, Khan, Liu-Ambrose, & Ashe, 2014). It continuously records accelerations ranging from 0.05 to 2g at a rate of 30 Hz along three axes, and it also provides step count information. The epoch length was set to 1 second. Participants were instructed not to wear the accelerometer for water-based activities, or when sleeping. Nonwear time was excluded before data analysis based on participants’ daily wear-time logs and also whenever there was an episode of more than 90 minutes of continuous zeros. Data analysis was restricted to days with at least 10 hours of wear time. These criteria left us with 1,178 accelerometer days, with a mean of 9.20 out of 10 possible accelerometer days per participant (SD = 1.44). The sample had average activity counts of 289.00 per minute (SD = 119.15), average step counts of 9.31 per minute (SD = 3.40), an average of 31.18 daily minutes of MVPA (SD = 22.73), and an average of 14.79 bout corrected daily minutes of MVPA (SD = 15.33; Freedson, Melanson, & Sirard 1998; MVPA ≥ 1952 accelerometer counts). A comparison between our sample and a normative sample of older adults from the United States indicates that our sample was more physically active (M = 7,772 steps per day versus M = 4,241 steps per day, respectively for our sample versus the U.S. sample; Tudor-Locke et al., 2013). More importantly, 70% of our sample failed to meet the 150 minutes of MVPA in at least 10-minute bouts per week that are recommended by current physical activity guidelines.
Weather Records
The daily temperature over the study period averaged 16.16°C (SD = 2.04), daily precipitation averaged 1.33mm (SD = 1.47), and the average for daylight hours was 15.26 (SD = 1.07). Objectively measured daily temperature, precipitation, and daylight information was retrieved online from Environment Canada at the Vancouver International Airport (Environment Canada, 2014).
Covariates
To examine the role of individual difference factors that are known to be associated with physical activity, we also included age, gender, heritage, self-rated health, daylight hours, temperature, accelerometer wear time, and a weekend versus weekday variable in our analyses.
Statistical Analysis
Hierarchical linear models were used to account for the nested data structure with days nested within individuals (HLM; Raudenbush, Bryk, Cheong, & Congdon, 2000). HLM allows for missing observations (Raudenbush et al., 2000). In a first step, we examined associations between concurrent precipitation, control variables, and physical activity using separate models for each physical activity index. In a second step, we then tested our main hypotheses by also including main and interaction effects for physical activity intentions and functional mobility. Again, separate models were conducted for each of the four physical activity indices. The multilevel models took the following form:
Level 1 variables were person centered and therefore reflect deviations from the respective individual’s mean with the exception of precipitation where the coefficient reflects deviations from 0mm of precipitation. The weekend versus weekday variable was dummy coded with “1” representing weekend days. Level 2 variables were grand-mean centered to allow comparisons across study participants with the exception of gender which was dummy coded with “1” representing women and heritage with “1” representing East Asian heritage. For reasons of parsimony, Level 2 slopes of control variables were treated as fixed. We also tested cross-level interactions between functional mobility and physical activity intentions on the precipitation–physical activity slope. These interactions did not reach statistical significance and are therefore not reported in the table.
Results
Table 1 shows the correlations between the central study variables. Of note, self-rated health, precipitation, and physical activity intentions were significantly correlated with all physical activity indices in the expected direction, whereas functional mobility was only associated with activity counts. The different physical activity indices were strongly correlated with each other.
Table 1.
Intercorrelations (N = 126)
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Age | −.06 | .12 | .05 | −.02 | −.14 | .12 | −.11 | −.14 | −.13 | −.16* |
| 2 | Gender | −.08 | −.12 | −.13 | −.15 | .19* | .07 | −.19* | −.12 | −.15 | |
| 3 | Self-rated health | −.28** | .40** | −.24** | −.16 | .09 | .31** | .27** | .26** | ||
| 4 | Functional mobility (high values = low functional mobility) | −.18* | .15 | .10 | −.12 | −.22** | −.17 | −.14 | |||
| 5 | Intentions | −.06 | −.01 | −.01 | .44** | .46** | .41** | ||||
| 6 | Mean temperature (°C) | −.40** | −.24** | .03 | .03 | .10 | |||||
| 7 | Mean precipitation (mm) | −.13 | −.21** | −.18* | −.17 | ||||||
| 8 | Mean daylight hours | .12 | .13 | .05 | |||||||
| 9 | Average daily activity counts per minute | .91** | .90** | ||||||||
| 10 | Average daily step counts per minute | .87** | |||||||||
| 11 | Average daily minutes of MVPA |
Notes. MVPA = moderate to vigorous physical activity.
*p < .05. **p < .01.
Associations Between Physical Activity, Precipitation, Functional Mobility, and Intentions
A preliminary analysis focused on the distribution of variability across persons and between days. The results showed that there was substantial day-to-day variability across all physical activity indices with about half of the variability originating at the day level (46% for activity counts, 55% for step counts, 55% for minutes of moderate to vigorous physical activity, and 66% for minutes of bout corrected moderate to vigorous physical activity) and the other half between persons. This finding indicates that a thorough understanding of the factors that shape physical activity in old age needs to take into account time-varying characteristics that distinguish one day from the next.
We then examined effects due to time-varying precipitation and several day-level variables (temperature, accelerometer wear time, and weekend effects) and person-specific control variables (age, gender, heritage, daylight hours, and self-rated health) on physical activity (Table 2, A Models). The results concerning day-level variables show that participants had lower average daily activity counts (−3.12, p < .01), had lower average daily step counts (−0.11, p < .01), and engaged in fewer minutes of MVPA (−.48, p < .01) on days with higher precipitation as compared with days with no precipitation. In addition, accelerometer wear time was positively associated with minutes of MVPA (−0.04, p < .01). Findings regarding person-level characteristics indicate that women had lower activity counts than men (−42.25, p < .05). Older age was negatively associated with average daily activity counts (−4.07, p < .05), average daily step counts (−0.11, p < .05), minutes of MVPA (−0.92, p < .01), and bout corrected minutes of MVPA (−0.59, p < .05). Self-rated health was negatively related with daily activity counts (−35.10, p < .01), daily step counts (−.99, p < .01), minutes of MVPA (−6.44, p < .01), and bout corrected minutes of MVPA (−4.98, p < .01). Heritage, daylight hours, daily temperature, and weekend versus weekdays were not related to physical activity in a statistically significant way.
Table 2.
Hierarchical Linear Models Predicting Physical Activity From Age, Gender, Heritage, Mean Daylight Hours, Subjective Health, Functional Mobility, Physical Activity Intentions, Daily Precipitation, Daily Temperature, Daily Weartime, and Social Calendar Using Full Maximum Likelihood Estimation (N = 126)
| Fixed effects | Average daily activity counts/min | Average daily step counts/min | Daily minutes of moderate to vigorous activity | Daily minutes of moderate to vigorous activity in bouts | ||||
|---|---|---|---|---|---|---|---|---|
| Model A | Model B | Model A | Model B | Model A | Model B | Model A | Model B | |
| Intercept | 211.96 | 195.82 | 3.51 | 2.71 | 33.67 | 27.43 | 15.76 | 8.49 |
| Gender | −42.25* | −36.48 | −0.76 | −0.50 | −6.16 | −4.62 | −3.17 | −1.54 |
| Age | −4.07* | −3.34* | −0.11* | −0.09 | −0.92** | −0.80* | −0.59* | −0.52* |
| Heritage | −1.36 | −6.47 | 0.62 | 0.51 | 0.79 | 0.17 | −1.58 | −1.84 |
| Daylight hours | 7.26 | 8.19 | 0.41 | 0.45 | 0.14 | 0.50 | 0.16 | 0.57 |
| Self-rated health | 35.10** | 13.91 | 0.99** | 0.38 | 6.44** | 2.90 | 4.98** | 2.87 |
| Functional mobility (high values = low functional mobility) | −9.35 | −0.12 | −0.82 | 0.29 | ||||
| Intentions | 60.57** | 2.01** | 11.12** | 8.25** | ||||
| Daily precipitation | −3.12** | −3.34** | −0.11** | −0.11** | −0.48** | −0.54** | −0.22 | −0.28* |
| Daily precipitation × Functional mobility | 0.83* | 0.02 | 0.25* | 0.18 | ||||
| Daily precipitation × Intentions | −1.33* | −0.05* | −0.13 | −0.14 | ||||
| Daily temperature | −0.98 | −1.05 | −0.05 | −0.06 | −0.56 | −0.60 | −0.92* | −0.96* |
| Daily wear time | −0.04 | −0.04 | −0.00 | −0.00 | 0.04** | 0.04** | 0.01 | 0.01 |
| Weekend | −2.50 | −2.35 | −0.05 | −0.04 | −1.14 | −1.12 | 0.95 | 0.95 |
| Random effects | ||||||||
| Residual | 1,0768.34 | 10,751.73 | 11.85 | 11.83 | 516.83 | 515.60 | 410.71 | 410.32 |
| Intercept | 11,065.97** | 9,238.86** | 9.15** | 7.39** | 393.48** | 337.94** | 199.56** | 168.45** |
| Slope | 5.28 | 3.87 | 0.00 | 0.00 | 0.01 | 0.01 | 0.16 | 0.14 |
| Deviance reduction | 21.44** | 23.70** | 18.93** | 17.85** | ||||
Notes. We also explored interactions between age and self-rated health on precipitation–physical activity slopes, which were not statistically significant over and above the reported findings. Additional analyses controlling for self-reported typicality of time in study did not reveal any statistically significant main or moderating effects of typicality on precipitation–physical activity associations for any of the four physical activity indices.
*p < .05. **p < .01.
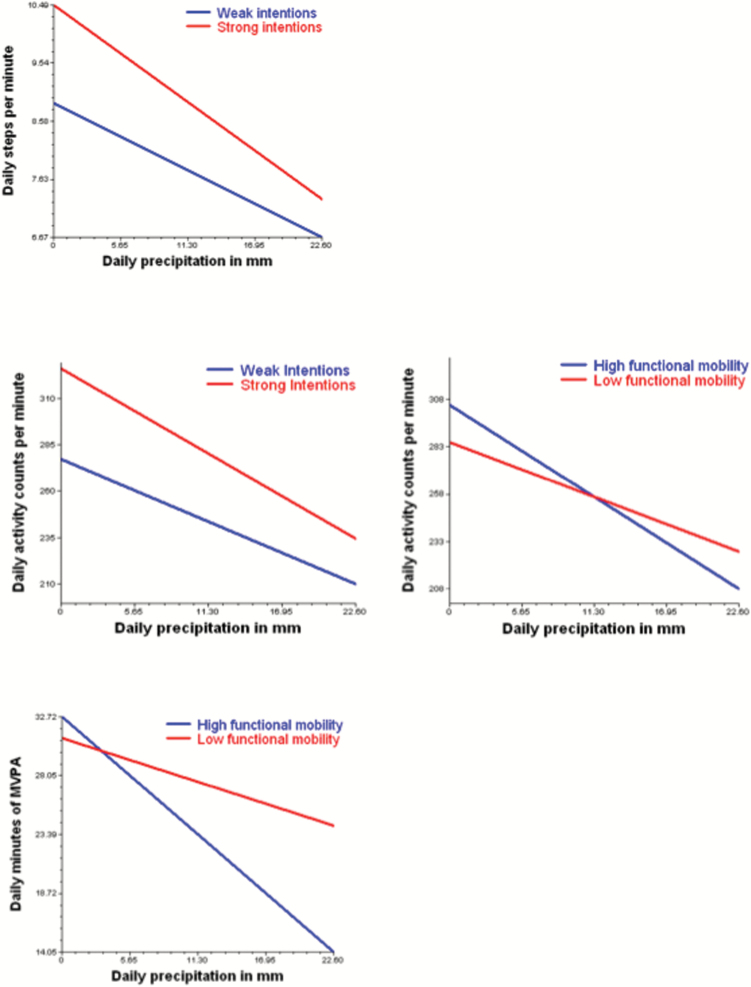
To test our main hypothesis, we next added functional mobility and physical activity intentions as main effects and cross-level interactions for functional mobility and physical activity intentions predicting the precipitation–physical activity slope (Table 2, B Models). There was no statistically significant main effect of functional mobility on any of the four physical activity indices. However, results revealed steeper precipitation–physical activity slopes for both activity counts (0.83, p < .05) and minutes of MVPA (0.25, p < .05) in individuals with high compared with low functional capacity. This means that older adults with high functional mobility compared with those with low functional mobility engaged in more physical activity on days without precipitation relative to days with precipitation. Furthermore, physical activity intentions were positively associated with overall levels of daily activity counts (60.57, p < .01), daily step counts (2.01, p < .01), minutes of MVPA (11.12, p < .01), and bout corrected minutes of MVPA (8.25, p < .01). The proposed moderating effect of physical activity intentions on precipitation–physical activity associations was evident for activity counts (−1.33, p < .05) and step counts (−.05, p < .05). The direction of this moderation implies that strong physical activity intentions were most effective under conditions of low precipitation. We further tested a three-way interaction between functional mobility and physical activity intentions on precipitation–physical activity slopes, which was not statistically significant and therefore not reported. The significant cross-level interactions of functional mobility, and physical activity intentions precipitation–physical activity slopes are illustrated in Figure 1A–D. Taken together, we found evidence for substantial daily life variability in physical activity with precipitation being one important source of such variability. Physical activity intentions were associated with higher overall physical activity engagement, and functional mobility and physical activity intentions both moderated the negative physical activity–precipitation associations.
Figure 1.
Intention and functional mobility moderate precipitation–physical activity associations. Weak intentions and low functional mobility scores are those that fall onto the 25th percentile (low functional mobility = high values on Timed Up and Go Test), and strong intentions and high functional mobility scores fall on the 75th percentile. These scores are depicted for illustrative purposes only; they were treated as continuous variables in the models.
Discussion
This study extends previous research on physical activity in older adults by investigating time-varying associations between objectively measured physical activity and precipitation as well as possible person-level moderators. Using up to 10 days of accelerometer information from a sample of 126 community-dwelling older adults and corresponding weather station information from Vancouver, Canada, we extended previously documented associations between physical activity and precipitation. In addition, our findings provide evidence that older adults with strong as compared to weak physical activity intentions engaged in more physical activity. Despite the fact that physical activity intentions and functional mobility moderated time-varying associations between daily precipitation and physical activity, having strong physical activity intentions and high functional mobility did not ward off the negative effect of precipitation on physical activity. We discuss our findings in the context of the health psychology and aging literature and suggest further steps to substantiate findings.
This study demonstrates the importance of taking physical activity research into the daily lives of older adults and shows the additional insights that may be gained when examining time-varying predictors of physical activity in old age. Specifically, we have demonstrated that about half of the variability in this key health behavior originates at the day level. In replicating previous research, we showed that increased precipitation was associated with concurrent reductions in physical activity (Brandon et al., 2009; Feinglass et al., 2011; Klenk et al., 2012). The fact that neither temperature nor daylight hours were associated with physical activity may be interpreted in the context of larger seasonal effects (Witham et al., 2014). In other words, it is conceivable that once temperature and daylight hours are within a certain range, they no longer restrict or extend older adult’s likelihood of engaging in physical activity. Furthermore, precipitation may have captured temperature information to the extent that increased precipitation goes along with reductions in temperature, which tends to be the case in temperate climate zones such as the Pacific North West. This may be different in other climate zones such as the subtropical weather that is characteristic of the Southern United States.
In addition to corroborating previous findings on precipitation–physical activity associations using objective weather information and accelerometer data (e.g., Witham et al., 2014), we also extended them by identifying one psychological (physical activity intentions) and one physical health (functional mobility) moderator. We find that in addition to a positive main effect of physical activity intentions on the overall amount of older adults’ physical activity (Renner, Spivak, Kwon & Schwarzer, 2007), physical activity intentions also moderated time-varying precipitation–physical activity associations. This relatively strong effect of a psychological relative to a physical health factor is important because physical activity intentions are potentially modifiable and can be targeted in health psychological interventions (Halbert, Crotty, Weller, Ahern, & Silagy, 2001). Although physical activity intentions moderated precipitation–activity count and precipitation–step count associations, the direction of this moderation was opposite to what we had expected. This counter intuitive finding may make more sense when recognizing that precipitation is the prototypical example of a low control obstacle to physical activity. Hence, although physical activity intentions have a significant main effect on the overall amount of physical activity in the present sample, it also needs to be recognized that this may be particularly true when older adults have more degrees of freedom—that is on days with little or no precipitation. In addition, it also needs to be recognized that the average precipitation over the study period was 1.33mm/day. Hence, there were enough precipitation-free days to make up for a low physical activity day spent inside.
Older adults with high as compared to low functional mobility also displayed more pronounced precipitation–physical activity slopes. This finding may be taken to indicate that older adults with high functional mobility are more responsive to changing contextual characteristics. For example, older adults with high functional mobility may be more likely to go on a brisk walk when there is no precipitation as compared to days with precipitation.
Limitations and Future Directions
We note several limitations that need to be addressed in future research. This project is based on a relatively active community-dwelling sample of older adults in the Metro Vancouver area with limited generalizability to rural communities. Vancouver offers a wide variety of physical activity promoting destinations and it has a relatively accessible public transportation system (Chaudhury, Mahmood, Michael, Campo, & Hay, 2012). It is conceivable that the present study underestimates the effects of precipitation, functional mobility, and intentions on physical activity given that it took place in an environment that is conducive to physical activity as compared with other environments (e.g., rural environments, large cities with recognized personal safety issues, or regions with a less moderate climate). We also note that older adults may not only differ in their performance-based functional mobility but also in the extent to which they perceive their mobility to be limited and that subjective mobility perceptions can also influence physical activity engagement over and above performance-based measures.
Our objective measurement of physical activity was a strength but accelerometry also has limitations (Pedišić & Bauman, 2015). For example, the accelerometers we used are not water proof and so we failed to capture any water-based activities. In addition, accelerometers do not accurately quantify intensity of movement associated with bike riding (Brandes, VAN Hees, Hannöver, & Brage, 2012). This could have underestimated the physical activity older adults engaged in, particularly so on days with precipitation when someone might use a stationary bike instead of going outside.
In addition, findings are based on a single assessment of intentions. Future extensions may involve time-varying reports of intention strength across days, which would allow comparisons between days with and without precipitation (Conroy et al., 2011; Hekler et al., 2012). Although we aimed to schedule participants during a typical week, which is mirrored by high post study typicality ratings, we cannot rule out that some participants travelled out of town for some of their time in the study, potentially compromising the fit between precipitation and physical activity data which depends on the extent to which participants engaged in physical activity in Vancouver versus some place else. Finally, although we managed to sample 10 days that older adults considered to be typical of their daily lives, we recognize that this study represents a snapshot of interrelated daily life processes that do not allow for causal inferences.
In conclusion, the present study points to negative associations between precipitation and physical activity in community-dwelling older adults as well as the moderating role of functional mobility and intentions. Those older adults with strong physical activity intentions not only engaged in more physical activity overall, but older adults with higher as compared with lower physical activity intentions and functional mobility were also better able to seize opportunities to be physically active.
Funding
This work was supported by a Canadian Institutes of Health Research (CIHR) Catalyst Grant to C. A. Hoppmann, M. C. Ashe, P. Graf, K. M. Khan, and J. P. Ziegelmann (102229-1).
Acknowledgment
C. A. Hoppmann gratefully acknowledges the support of the Michael Smith Foundation for Health Research (MSFHR) and the Canada Research Chairs program. M.C. Ashe acknowledges MSFHR and the CIHR for Career awards.
References
- Ajzen I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211. doi:10.1016/0749-5978(91)90020-T [Google Scholar]
- Almeida O. P., Khan K. M., Hankey G. J., Yeap B. B., Golledge J., Flicker L. (2014). 150 minutes of vigorous physical activity per week predicts survival and successful ageing: A population-based 11-year longitudinal study of 12 201 older Australian men. British Journal of Sports Medicine, 48, 220–225. doi:10.1136/bjsports-2013-092814 [DOI] [PubMed] [Google Scholar]
- Ashe M. C. Miller W. C. Eng J. J., & Noreau L (2008). Older adults, chronic disease and leisure-time physical activity. Gerontology, 55, 64–72. doi:10.1159/000141518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltes P. B., & Smith J (2003). New frontiers in the future of aging: From successful aging in the young old to the dilemmas of the fourth age. Gerontology, 49, 123–135. doi:10.1159/000067946 [DOI] [PubMed] [Google Scholar]
- Benyamini Y. (2011). Why does self-rated health predict mortality? An update on current knowledge and a research agenda for psychologists. Psychology & Health, 26, 1407–1413. doi:10.1080/08870446.2011.621703 [DOI] [PubMed] [Google Scholar]
- Blair S. N. (2009). Physical inactivity: The biggest public health problem of the 21st century. British Journal of Sports Medicine, 43, 1–2. [PubMed] [Google Scholar]
- Brandes M., VAN Hees V. T., Hannöver V., Brage S. (2012). Estimating energy expenditure from raw accelerometry in three types of locomotion. Medicine and Science in Sports and Exercise, 44, 2235–2242. doi:10.1249/MSS.0b013e318260402b [DOI] [PubMed] [Google Scholar]
- Brandon C. A. Gill D. P. Speechley M. Gilliland J., & Jones G. R (2009). Physical activity levels of older community dwelling adults are influenced by summer weather variables. Applied Physiology, Nutrition, and Metabolism, 34, 182–190. doi:10.1139/H09-004 [DOI] [PubMed] [Google Scholar]
- Brassington G. S. Hekler E. B. Cohen Z., & King A. C (2012). Health-enhancing physical activity. In A., Baum, T. A., Revenson (Eds.), Handbook of Health Psychology (pp. 353–374). Hoboken, NJ: Psychology Press. [Google Scholar]
- Brown D. R. Yore M. M. Ham S. A., & Macera C. A (2001). Physical activity among adults >or=50 yr with and without disabilities. Medicine and Science in Sports and Exercise, 37, 620–629. doi:10.1249/01.MSS.0000158189.17546.ED [DOI] [PubMed] [Google Scholar]
- Canadian Society for Exercise Physiology. (2012). Canadian physical activity guidelines, Canadian sedentary behavior guidelines, http://www.csep.ca/CMFiles/Guidelines/CSEP_Guidelines_Handbook.pdf
- Caspersen C. J. Powell K. E., & Christenson G. M (1985). Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Reports, 100, 126–131. [PMC free article] [PubMed] [Google Scholar]
- Chaudhury H. Mahmood A. Michael Y. L. Campo M., & Hay K (2012). The influence of neighborhood residential density, physical and social environments on older adults’ physical activity: An exploratory study in two metropolitan areas. Journal of Aging Studies, 26, 35–43. doi:10.1016/j.jaging.2011.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chipperfield J. G. Newall N. E. Chuchmach L. P. Swift A. U., & Haynes T. L (2008). Differential determinants of men’s and women’s everyday physical activity in later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 63B, S211–S218. doi:10.1093/geronb/63.4.S211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Climatemps (2015). Climate comparison table, http://www.vancouver.climatemps.com/vs/london.php
- Conroy, D. E., Elavsky, S., Doerksen, S. E., & Maher, J. P. (2013). A daily process analysis of intentions and physical activity in college students. Journal of Sport & Exercise Psychology, 35, 493–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy D. E., Elavsky S., Hyde A. L., Doerksen S. E. (2011). The dynamic nature of physical activity intentions: A within-person perspective on intention-behavior coupling. Journal of Sport & Exercise Psychology, 33, 807–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn R. A., Shaw W. D., Trousdale M. A. (2012). The effect of weather on walking behavior in older adults. Journal of Aging and Physical Activity, 20, 80–92. [DOI] [PubMed] [Google Scholar]
- Dunton G. Atienza A. A. Castro C. M., & King A. C (2009). Using ecological momentary assessment to examine antecedents and correlates of physical activity bouts in adults age 50+ years: A pilot study. Annals of Behavioral Medicine, 38, 249–255. doi:10.1007/s12160-009-9141-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Environment Canada (2014, February 12) Monthly Data Report for 2011 Retrieved from http://climate.weather.gc.ca/climateData/monthlydata_e.html?timeframe=3&Prov=BC%20%20&StationID=889&mlyRange=1937-01-01|2012-12-01&Year=2011&Month=4&Day=19.
- Feinglass J., Lee J., Semanik P., Song J., Dunlop D., Chang R. (2011). The effects of daily weather on accelerometer-measured physical activity. Journal of Physical Activity & Health, 8, 934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedson P. S. Melanson E., & Sirard J (1998). Calibration of the computer science and applications, inc. accelerometer. Medicine & Science in Sports & Exercise, 30, 777–781. doi:10.1097/00005768-199805000-00021 [DOI] [PubMed] [Google Scholar]
- Gorman E. Hanson H. M. Yang P. H. Khan K. M. Liu-Ambrose T. Y., & Ashe M. C (2014). Accelerometry analysis of physical activity and sedentary behavior in older adults: A systematic review and data analysis. European Review of Aging and Physical Activity, 11, 35–49. doi:10.1007/s11556-013-0132-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert J., Crotty M., Weller D., Ahern M., Silagy C.(2001). Primary care–based physical activity programs: Effectiveness in sedentary older patients with osteoarthritis symptoms. Arthritis Care & Research, 45, 228–234. doi:10.1002/1529-0131(200106)45:3<228::AID-ART253>3.0.CO;2-2 [DOI] [PubMed] [Google Scholar]
- Haskell W. L. Lee I. M. Pate R. R. Powell K. E. Blair S. N. Franklin B. A., … Bauman A (2007). Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Medicine and Science in Sports and Exercise, 39, 1423–1435. doi:10.1161/circulationaha.107.185649 [DOI] [PubMed] [Google Scholar]
- Hekler E. B., Buman M. P., Ahn D., Dunton G., Atienza A. A., King A. C. (2012). Are daily fluctuations in perceived environment associated with walking? Psychology & Health, 27, 1009–1020. doi:10.1080/08870446.2011.645213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klenk J. Büchele G. Rapp K. Franke S., & Peter R (2012). Walking on sunshine: Effect of weather conditions on physical activity in older people. Journal of Epidemiology and Community Health, 66, 474–476. doi:10.1136/jech.2010.128090 [DOI] [PubMed] [Google Scholar]
- Lord S. R. Sherrington C. Menz H. B., & Close J. C. T (2007). Falls of older people. Cambridge: Cambridge University Press; doi:10.1093/ageing/afm098 [Google Scholar]
- Merchant A. T., Dehghan M., Akhtar-Danesh N. (2007). Seasonal variation in leisure-time physical activity among Canadians. Canadian Journal of Public Health = Revue Canadienne de Santé Publique, 98, 203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson M. E. Rejeski W. J. Blair S. N. Duncan P. W. Judge J. O. King A. C., … Castaneda-Sceppa C (2007). Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Medicine & Science in Sports & Exercise, 39, 1435–1445. doi:10.1161/circulationaha.107.185650 [DOI] [PubMed] [Google Scholar]
- Pedišić Ž., Bauman A. (2015). Accelerometer-based measures in physical activity surveillance: Current practices and issues. British Journal Of Sports Medicine, 49, 219–223. doi:10.1136/bjsports-2013-093407 [DOI] [PubMed] [Google Scholar]
- Podsiadlo D., & Richardson S (1991). The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. Journal of The American Geriatrics Society, 39, 142–148. doi:10.1111/j.1532–5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- Raudenbush S. W. Bryk A. S. Cheong Y. F., & Congdon R (2000). HLM 5. Hierarchal linear and nonlinear modeling. Chicago, IL: Scientific Software International. [Google Scholar]
- Renner B., Spivak Y., Kwon S., Schwarzer R. (2007). Does age make a difference? Predicting physical activity of South Koreans. Psychology and Aging, 22, 482–493. doi:10.1037/0882-7974.22.3.482 [DOI] [PubMed] [Google Scholar]
- Rogers R. W. (1983). Cognitive and physiological processes in fear-based attitude change: A revised theory of protection motivation. In J., Cacioppo, R., Petty (Eds.), Social psycho-physiology: A sourcebook (pp. 153–176). New York, NY: Guilford Press. [Google Scholar]
- Sarkin J. A. Johnson S. S. Prochaska J. O., & Prochaska J. M (2001). Applying the transtheoretical model to regular moderate exercise in an overweight population: Validation of a stages of change measure. Preventive Medicine: An International Journal Devoted to Practice And Theory, 33, 462–469. doi:10.1006/pmed.2001.0916 [DOI] [PubMed] [Google Scholar]
- Scholz U. Keller R., & Perren S (2009). Predicting behavioral intentions and physical exercise: A test of the Health Action Process Approach at the intraperson level. Health Psychology, 28, 702–708. doi:10.1037/a0016088 [DOI] [PubMed] [Google Scholar]
- Sheeran P. (2002). Intention-behavior relations: A conceptual and empirical review. In W., Stroebe, M., Hewstone (Eds.), European Review of Social Psychology (Vol. 12, pp. 1–36). Chichester, UK: Wiley. [Google Scholar]
- Tudor-Locke C. Schuna J. M. Barreira T. V. Mire E. F. Broyles S. T. Katzmarzyk P. T., & Johnson W. D (2013). Normative steps/day values for older adults: NHANES 2005–2006. Journals of Gerontology: Medical Sciences, 68,1426–1432. [DOI] [PubMed] [Google Scholar]
- Tucker P., & Gilliland J (2007). The effect of season and weather on physical activity: A systematic review. Public Health, 121, 909–922. doi:10.1093/gerona/glt116 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2008). Physical activity guidelines for Americans. Atlanta, GA: Center for Disease Control. [Google Scholar]
- Witham M. D., Donnan P. T., Vadiveloo T., Sniehotta F. F., Crombie I. K., Feng Z., McMurdo M. E. (2014). Association of day length and weather conditions with physical activity levels in older community dwelling people. Plos ONE, 9, e85331 doi:10.1371/journal.pone.0085331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitney J. C., Lord S. R., Close J. C. (2005). Streamlining assessment and intervention in a falls clinic using the Timed Up and Go Test and Physiological Profile Assessments. Age and Ageing, 34, 567–571. doi:10.1093/ageing/afi178 [DOI] [PubMed] [Google Scholar]
- Ziegelmann J. P. Lippke S., & Schwarzer R (2006a). Adoption and maintenance of physical activity: Planning interventions in young, middle-aged, and older adults. Psychology & Health, 21, 145–163. doi:10.1080/1476832050018891 [DOI] [PubMed] [Google Scholar]
- Ziegelmann J. P. Lippke S., & Schwarzer R (2006b). Subjective residual life expectancy in health self-regulation. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 61B, P195–P201. doi:10.1093/geronb/61.4.P195 [DOI] [PubMed] [Google Scholar]