Abstract
Objective:
Previous studies have found that positive self-perceptions of aging (SPA) are associated with longer survival; however, a biological mechanism was unknown. We examined whether C-reactive protein (CRP), a marker of cumulative stress-related inflammation, mediates the relationship between SPA and survival.
Method:
The SPA of participants aged 50 and older in the Health and Retirement Study (N = 4,149) were assessed at baseline. Inflammation was measured by the level of CRP 4 years later. Survival was followed for up to 6 years.
Results:
As hypothesized, CRP mediated the impact of SPA on survival. Following the steps of a mediation analysis, positive SPA at baseline predicted lower CRP after 4 years (β = −.29, p = .03) and longer survival in the 2 years following the CRP measurement (β = .20, p =.003); additionally, lower CRP predicted longer survival, after adjusting for positive SPA (β = −.02, p = .0001). All models adjusted for baseline age, CRP, health, sex, race, and education.
Discussion:
It was found that lower CRP partially mediates the relationship between positive SPA and longer survival. Hence, this study presents a novel pathway to explain the process by which positive SPA extend longevity.
Keywords: Aging, C-reactive protein, Inflammation, Longevity, Mechanism, Mortality, Self-perceptions of aging, Social cognition, Survival
Researchers on three continents have found that older individuals holding more-positive self-perceptions of aging (SPA) live longer than their same-aged peers holding more-negative SPA, even after adjusting for relevant health and demographic variables (e.g., Kotter-Grühn, Kleinspehn-Ammerlahn, Gerstorf, & Smith, 2009; Levy, Slade, Kunkel, & Kasl, 2002; Sargent-Cox, Anstey, & Luszcz, 2014; Westerhof et al., 2014). According to stereotype embodiment theory, and the research supporting it, SPA are assimilated from the surrounding culture and can influence outcomes by different routes, including a biological pathway (Levy, 2009; Levy, Slade, Murphy, & Gill, 2012). Yet, a biological mechanism that relates SPA to survival had not been examined. The goal of the present study was to explore whether inflammation, reflected by its marker, C-reactive protein (CRP), could act as such a mediator and, thereby, provide a survival advantage mechanism.
Two discrete fields of research suggest that inflammation is a likely mediator of the influence of SPA on survival. First, in an experiment, negative age beliefs amplified stress, whereas positive age beliefs acted as a shield against stress (Levy, Hausdorff, Hencke, & Wei, 2000). Insofar as older individuals tend to be frequently exposed to negative age beliefs, by such means as television programming and social media, this could lead to cumulative stress (Donlon, Ashman, & Levy, 2005; Levy, 2009; Levy, Chung, Bedford, & Navrazhina, 2014). Second, CRP reflects cumulative stress (Danese & McEwen, 2012; Gouin, Glaser, Malarkey, Beversdorf, & Kiecolt-Glaser, 2012). For example, those with post-traumatic stress disorder (PTSD) have significantly higher levels of CRP than those without PTSD (Spitzer, et al., 2009), and dementia caregivers have significantly higher CRP levels than non-caregivers—daily stressors mediated this relationship (Gouin et al., 2012). Further, numerous studies have shown that elevated CRP predicts reduced survival (e.g., Harris et al., 1999; Szewieczek et al., 2015). It is probable that this association is largely based on elevated inflammatory responses leading to vascular damage and coronary events (e.g., Black, Kushner, & Samols, 2004; Musunuru et al., 2008).
Thus, in the current study, we hypothesized that a lower level of inflammation, reflected by CRP, will mediate the relationship between positive SPA and longer survival.
Method
Participants
Data were obtained from the Health and Retirement Study (HRS), a nationally representative sample of individuals over the age of 50 in the United States, conducted by the Institute of Social Research at the University of Michigan. Our cohort consisted of 4,149 individuals followed across 6 years, comprising 28,711 person-years. Consistent with the older American population, the majority of the sample was White (83.4%) and female (60.4%). In 2008, the participants’ baseline age ranged from 50 to 99 (M = 68.15, SD = 8.83).
Measures
Self-perceptions of aging.
In 2008, the Attitudes Toward Own Aging subscale of the Philadelphia Geriatric Center Morale Scale, a reliable and valid measure (Lawton, 1975; Levy, Slade, et al., 2002; Liang & Bollen, 1983), was added to the HRS. It consists of the following items: (1) Things keep getting worse as I get older, (2) I have as much pep as I did last year, (3) The older I get, the more useless I feel, (4) I am as happy now as I was when I was younger, and (5) As I get older, things are better than I thought they would be. Thirteen individuals (<.01% of the sample) were dropped, because they had fewer than three responses to these items. The participants were asked to rate the statements on a 6-item scale ranging from strongly disagree to strongly agree; higher SPA scores meant more-positive views of their own aging. The scores were averaged across the 5 items, creating a final SPA score ranging from 1 to 6 that was used as a continuous variable in our models.
C-reactive Protein.
CRP levels were obtained from dried blood spots in 2008 and 2012. Dried blood spots, which were assayed at the University of Vermont using a standard protocol, are a valid way to assess CRP in large population-based studies (Crimmins et al., 2013; Williams & McDade, 2009). The HRS investigators applied weights to make the dried blood spots assay values equivalent to whole blood assay values gathered by the National Health and Nutrition Examination Survey (Crimmins et al., 2013). CRP is included as a continuous variable in the models.
Survival.
The outcome, survival, was examined for the 6 years following baseline—the period for which data were available at the time of analysis. Vital status was obtained by matching HRS participants to the mortality information provided by the National Death Index through 2014.
Covariates.
Models were adjusted for the baseline covariates of age, CRP, health, sex, race, and education, because all have been found to predict survival. Age and education were used as continuous variables. Health score was quantified by using the number of physician-diagnosed diseases (i.e., cancer, lung disease, heart disease, stroke, arthritis, diabetes, and hypertension).
Statistical Analyses
To examine whether lower level of inflammation, reflected by 2012 CRP, mediated the relationship between positive baseline SPA and survival, the three steps of the Kenny, Kashy, and Bolger (1998) mediation analysis were performed. The significance of this mediation was determined by calculating the joint probability that the effect of positive SPA on lower CRP and the effect of lower CRP on longer survival are both significant (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). All analyses used SAS 9.4 (SAS Institute, 2013, Cary, NC).
Results
As predicted, CRP mediated the relationship between positive SPA and longer survival. CRP fit the three criteria for a mediator (Kenny, Kashy, & Bolger, 1998). In line with the first criterion, baseline positive SPA predicted longer survival during the 2 years following assessment of CRP in 2012 in the unadjusted (β = .30, p < .0001) and adjusted models (β = .21, p = .003). SPA had a greater effect on survival than age, CRP, race, and education.
In line with the second mediation criterion, linear regressions revealed that positive SPA assessed in 2008 were predictive of lower CRP in 2012, in the unadjusted (β = −.49, SE = .12, p < .0001) and adjusted models (β = −.29, SE = .13, p = .03). The adjusted model included all the covariates as well as CRP in 2008.
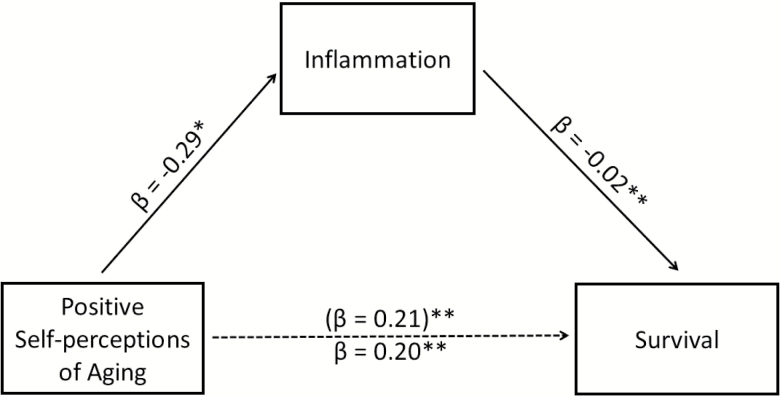
In line with the third mediation criterion, the presumed mediator, CRP assessed in 2012, affected the outcome of survival between 2012 and 2014, even after controlling for the direct path between baseline SPA and survival (unadjusted β = −.02, p < .0001; adjusted β = −.02, p ≤ .0001). As the survival advantage of SPA was attenuated but still significant after the addition of CRP to the model (unadjusted: β = .21, p <.003; adjusted: β = .20, p = .004), CRP fit the criterion of a partial mediator (see Figure 1). This mediation effect was significant at p < .0001, according to the causal step joint coefficient test (MacKinnon et al., 2002).
Figure 1.
Partial mediation of the association of positive SPA with survival by lower inflammation. In the mediation model, SPA were measured at baseline, inflammation was measured by the level of CRP 4 years later, and mortality was examined in the 2 years following the CRP measurement. The analyses adjusted for all covariates. The numbers in parentheses indicate the parameter estimate before inflammation was added to the model of SPA predicting mortality. *p < .05, **p < .01.
The contribution of positive SPA to survival, assessed across the 6 years, persisted when the sample was stratified by age, health, sex, race, and education; the first three variables were stratified at the sample median. When Cox proportional hazards models, adjusted for all covariates except the stratification variables, were performed, SPA were associated with survival advantage among those aged 50–69 and those 70 or above, those with fewer than two illnesses and those with two or more, males and females, races (White, Black, and other), and those with less than high school education and those with high school education or above.
Across the 6-year period, 13.0% of the positive SPA group died, in contrast to 25.4% of the negative SPA group. The SPA variable was stratified at its median in this analysis.
Discussion
The present study is the first to identify a biological mechanism in the association of positive SPA with longer survival. As expected, inflammation mediated the relationship between SPA and survival in a large national sample of older individuals. During the 6-year period, participants holding more-positive SPA were twice as likely to survive, compared with those holding more-negative SPA. It was also found that SPA predicted survival, regardless of age, health, sex, and race.
Two features of the mediation model support the assumed temporal order of the variables. First, we were able to examine them in the predicted longitudinal sequence, with SPA at baseline, CRP 4 years later, and survival measured during the 2-year period after CRP. Second, the mediation models were adjusted for relevant covariates, including baseline CRP.
Identifying a biological mechanism for SPA on survival has several potential benefits. For researchers, CRP, which can change in short intervals, could be used as an immediate and objective marker of SPA improvement when developing an intervention. For clinicians, it suggests a previously unrecognized etiology of high CRP levels that could be intervened upon in a noninvasive way by targeting negative SPA. For policymakers, it could provide an added incentive to implement public programs aimed at countering the societal sources that contribute to the negativity of SPA.
The findings of this study also demonstrate the benefit of combining social–psychological and biological approaches to aging research. With these approaches in tandem, we were able to explore the role of CRP in the survival advantage of assimilated positive age beliefs.
Funding
This work was supported by a grant to B. R. Levy from the National Institute on Aging (grant number R01AG032284). The Health and Retirement Study is supported by the National Institute on Aging (grant number NIA U01AG009740).
References
- Black S., Kushner I., Samols D. (2004). C-reactive protein. Journal of Biological Chemistry, 279, 48487–48490. doi:10.1074/jbc.R400025200 [DOI] [PubMed] [Google Scholar]
- Crimmins E., Faul J., Kim J., Guyer H., Langa K., Ofstedal M. B., Weir D. R. (2013). Documentation of biomarkers in the 2006 and 2008 Health and Retirement Study. Retrieved from http://hrsonline.isr.umich.edu/modules/meta/bio2008/desc/Biomarker2006and2008.pdf [Google Scholar]
- Danese A., McEwen B. S. (2012). Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiology & Behavior, 106, 29–39. doi:10.1016/j.physbeh.2011.08.019 [DOI] [PubMed] [Google Scholar]
- Donlon M. M., Ashman O., Levy B. R. (2005). Re-vision of older television characters: A stereotype-awareness intervention. Journal of Social Issues, 61, 307–319. doi:10.1111/j.1540-4560.2005.00407.x [Google Scholar]
- Gouin J. P., Glaser R., Malarkey W. B., Beversdorf D., Kiecolt-Glaser J. (2012). Chronic stress, daily stressors, and circulating inflammatory markers. Health Psychology, 31, 264–268. doi:10.1037/a0025536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris T. B. Ferrucci L. Tracy R. P. Corti M. C. Wacholder S. Ettinger W. H.,& Wallace R (1999). Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. The American Journal of Medicine, 106, 506–512. doi:10.1016/S0002-9343(99)00066-2 [DOI] [PubMed] [Google Scholar]
- Kenny D. A., Kashy D., Bolger N. (1998). Data analysis in social psychology. In D., Gilbert S., Fiske, G., Lindzey (Eds.), Handbook of social psychology (4th ed., pp. 233–265). New York, NY: McGraw-Hill. [Google Scholar]
- Kotter-Grühn D., Kleinspehn-Ammerlahn A., Gerstorf D., Smith J. (2009). Self-perceptions of aging predict mortality and change with approaching death: 16-Year longitudinal results from the Berlin Aging Study. Psychology and Aging, 24, 654–667. doi:10.1037/a0016510 [DOI] [PubMed] [Google Scholar]
- Lawton M. P. (1975). The Philadelphia Geriatric Center Morale Scale: A revision. Journal of Gerontology, 30, 85–89. doi:10.1093/geronj/30.1.85 [DOI] [PubMed] [Google Scholar]
- Levy B. R. (2008). Rigidity as a predictor of older persons’ aging stereotypes and aging self-perceptions of aging. Social Behavior and Personality, 36, 559–570. doi:10.2224/sbp.2008.36.4.559 [Google Scholar]
- Levy B. (2009). Stereotype embodiment: A psychosocial approach to aging. Current Directions in Psychological Science, 18, 332–336. doi:10.1111/j.1467-8721.2009.01662.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B. R., Chung P. H., Bedford T., Navrazhina K. (2014). Facebook as a site for negative age stereotypes. Gerontologist, 54, 172–176. doi:10.1093/geront/gns194 [DOI] [PubMed] [Google Scholar]
- Levy B. R., Slade M. D., Kunkel S. R., Kasl S. V. (2002). Longevity increased by positive self-perceptions of aging. Journal of Personality and Social Psychology, 83, 261–270. doi: http://dx.doi.org/10.1037/0022-3514.83.2.261 [DOI] [PubMed] [Google Scholar]
- Levy B. R., Hausdorff J. M., Hencke R., Wei J. Y. (2000). Reducing cardiovascular stress with positive self-stereotypes of aging. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 55, P205–P213. doi:10.1093/geronb/55.4.P205 [DOI] [PubMed] [Google Scholar]
- Levy B. R., Slade M. D., Murphy T. E., Gill T. M. (2012). Association between positive age stereotypes and recovery from disability in older persons. The Journal of the American Medical Association, 308, 1972–1973. doi:10.1001/jama.2012.14541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J., Bollen K. A. (1983). The structure of the Philadelphia Geriatric Center Morale Scale: A reinterpretation. Journal of Gerontology, 38, 181–189. doi:10.1093/geronj/38.2.181 [DOI] [PubMed] [Google Scholar]
- MacKinnon D. P., Lockwood C. M., Hoffman J. M., West S. G., Sheets V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. doi:10.1037/1082-989X.7.1.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musunuru K., Kral B. G., Blumenthal R. S., Fuster V. F., Campbell C. Y., Gluckman T. J., Mora S. (2008). The use of high-sensitivity assays for C-reactive protein in clinical practice. Nature Clinical Practice Cardiovascular Medicine, 5, 621–635. doi:10.1038/ncpcardio1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sargent-Cox K. A., Anstey K. J., Luszcz M. A. (2014). Longitudinal change of self-perceptions of aging and mortality. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69, 168–173. doi:10.1093/geronb/gbt005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J. Fisher G. Ryan L. Clarke P. House J. Weir D.,& The HRS Psychosocial Working Group. (2013). Psychosocial and Lifestyle Questionnaire 2006–2010 Documentation Report. Ann Arbor, MI: Survey Research Center, Institute of Social Research, University of Michigan. [Google Scholar]
- Spitzer C., Barnow S., Völzke H., John U., Freyberger H. J., Grabe H. J. (2009). Trauma, posttraumatic stress disorder, and physical illness: Findings from the general population. Psychosomatic Medicine, 71, 1012–1017. doi:10.1097/PSY.0b013e3181bc76b5 [DOI] [PubMed] [Google Scholar]
- Szewieczek J., Francuz T., Dulawa J., Legierska K., Hornik B., Włodarczyk I., Batko-Szwaczka A. (2015). Functional measures, inflammatory markers and endothelin-1 as predictors of 360-day survival in centenarians. Age, 37, 85. doi:10.1007/s11357-015-9822-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerhof G. J., Miche M., Brothers A. F., Barrett A. E., Diehl M., Montepare J. M., Wurm S. W. (2014). The influence of subjective aging on health and longevity: A meta-analysis of longitudinal data. Psychology and Aging, 29, 793–802. doi:10.1037/a0038016 [DOI] [PubMed] [Google Scholar]
- Williams S. R., McDade T. W. (2009). The use of dried blood spot sampling in the National Social Life, Health, and Aging Project. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64(Suppl. 1), i131–i136. doi:10.1093/geronb/gbn022 [DOI] [PMC free article] [PubMed] [Google Scholar]