Abstract
Objectives:
Bisexual older adults are a growing yet largely invisible, underserved, and understudied population. Utilizing the Health Equity Promotion Model, we examined hypothesized mechanisms accounting for health disparities between bisexual older adults and lesbian and gay older adults.
Method:
Based on data from Caring and Aging with Pride, the largest national survey of LGBT older adults, this study (N = 2,463) utilized structural equation modeling to investigate direct and indirect associations between sexual identity (bisexual vs. lesbian and gay) and health via sexual identity factors (identity disclosure and internalized stigma), social resources, and socioeconomic status (SES).
Results:
Bisexual older adults reported significantly poorer health compared with lesbian and gay older adults. Indirect effects involving sexual identity factors, social resources, and SES explained the association between bisexual identity and poorer health. A potentially protective pathway was also identified wherein bisexuals had larger social networks after adjusting for other factors.
Discussion:
Bisexual older adults face distinct challenges and health risks relative to other older adults, likely because of the accumulation of socioeconomic and psychosocial disadvantages across the life course. Interventions taking into account older bisexuals’ unique risk and protective factors may be helpful in reducing health inequities.
Keywords: Aging, Diversity, Health disparities, Inequities, SES, Sexual identity, Sexual orientation
Sexual minority adults are health disparate and underserved compared with heterosexuals, experiencing elevated psychological distress, poorer physical health, and reduced access to health care resources (Buchmueller & Carpenter, 2010; Conron, Mimiaga, & Landers, 2010). Much of the scientific literature has collapsed bisexuals with other sexual minorities for analytic purposes (Wallace, Cochran, Durazo, & Ford, 2011), implying the largely untested assumption that lesbian, gay, and bisexual adults share similar experiences and needs. Yet there is increasing evidence that bisexual adults experience significant mental and physical health disparities compared not only with heterosexuals but also with lesbians and gay men in both population-based (Fredriksen-Goldsen, Kim, Barkan, Balsam, & Mincer, 2010; Gorman, Denney, Dowdy, & Medeiros, 2015; Jorm, Korten, Rodgers, Jacomb, & Christensen, 2002; Veenstra, 2011) and community-based studies (Bostwick, Hughes, & Everett, 2015; Fredriksen-Goldsen et al., 2011; Koh & Ross, 2006). Thus, it is important to disaggregate these groups to fully understand their experiences, strengths, and risk factors.
Little of the research examining bisexuals’ unique risk factors and health outcomes has focused on bisexuals in older age, yet the historical and social contexts that influence well-being and resources over the life course are markedly different for today’s older and younger bisexuals. Today’s bisexual older adults came of age during a time when same-sex behavior was severely stigmatized and criminalized. At the same time, bisexual identities were largely invisible, including within lesbian and gay communities, limiting access to support and resources via those communities. It is possible that the accumulation of social and economic disadvantage across the life course culminates in persistent or increasing health disparities for bisexuals as they reach older age. Alternately, or in parallel due to mortality (Dupre, 2007), in the general population age has sometimes been found to act as a “leveler,” diminishing observable associations between resources and health (Herd, 2006; Robert et al., 2009). In the present study, we used an equity life course framework to investigate economic, psychological, and social risk and protective factors, with the goal of identifying modifiable mechanisms that contribute to health inequities in bisexual adults as they age.
Conceptual Framework
The Health Equity Promotion Model (Fredriksen-Goldsen et al., 2014), an integrative framework, was developed to identify structural, psychological, and social factors that are associated with mental and physical health, emphasizing life course development and the importance of historical context, and to investigate explanatory mechanisms that account for the health, aging, and well-being of lesbian, gay, bisexual, and transgender (LGBT) older adults. This model highlights the heterogeneity and intersectionality of social positions that result in unique networks of interconnected health-promoting and adverse processes. As a result, it can shed light on experiences that are common across different subgroups of LGBT people, as well as mechanisms of risk and resilience that may be more likely to operate in a particular subgroup such as bisexual older adults. The Health Equity Promotion Model is designed to move beyond simply identifying disparities toward ensuring LGBT people have the opportunity to reach their full health potential. Thus, in this study, it was used to inform empirically supported hypotheses about multiple pathways that not only explain variance in bisexual older adults’ health outcomes but also carry implications for both systemic and individual-level intervention.
Sexual identity factors
Two processes that are unique to sexual minority populations and have been associated with health are internalized stigma and disclosure of sexual identity. In studies with younger lesbian, gay, and bisexual (LGB) adults, internalized stigma (i.e., personal adoption of society’s negative attitudes toward sexual minorities) has been empirically linked to poorer mental and physical health (Meyer & Dean, 1998). It has been shown consistently across several studies with both probability and community samples that compared with lesbian and gay adults, bisexual adults experience greater levels of internalized stigma (Costa, Pereira, & Leal, 2013; Herek, Gillis, & Cogan, 2009). In addition, bisexual adults have been found in several community-based samples to have lower levels of identity disclosure compared with lesbians and gay men, and hence may be less visible than lesbians and gay men (Balsam & Mohr, 2007; Costa et al., 2013; Legate, Ryan, & Weinstein, 2012; Lewis, Derlega, Brown, Rose, & Henson, 2009), including among older adults (Fredriksen-Goldsen et al., 2011). Openness about sexual identity is often considered beneficial to sexual minority adults’ psychological well-being (Morris, Waldo, & Rothblum, 2001); at the same time, among bisexual adults, identity disclosure has sometimes been associated with more conflict about sexual orientation (Lewis et al., 2009) and poorer mental health (Koh & Ross, 2006). Among today’s bisexual older adults, it is not yet understood how societal shifts in the visibility and acceptability of bisexuality interplay with the cumulative effects of disclosure (or concealment) and internalized stigma.
Social resources
Existing studies document the importance of interconnecting social resources, such as social support, social network size, and connectedness to the LGBT community, in promoting health and well-being of sexual minorities (Kertzner, Meyer, Frost, & Stirratt, 2009; White & Cant, 2003), including sexual minority older adults (Grossman, D’Augelli, & Hershberger, 2000; Fredriksen-Goldsen, Emlet et al., 2013; Lyons, Pitts, & Grierson, 2013). Bisexual adults, compared with lesbians and gay men, have been found to have lower levels of family support and more negative pressure within their interpersonal relationships (Jorm et al., 2002) as well as lower levels of community connection and social integration (Balsam & Mohr, 2007; Hsieh, 2014). Greater identity stigma/concealment may account for some of this disparity in bisexuals’ social resources. For example, internalized stigma has been associated with lower relationship functioning, quality, and length (Mohr & Fassinger, 2006; Ross and Rosser, 1996). Bisexual older adults’ sense of belonging within LGBT communities may also be limited because of historically negative attitudes toward bisexuality among lesbians and gay men (Fredriksen-Goldsen, 2016; Friedman et al., 2014). Yet little is known about how these associations play out for older bisexuals, nor about how they may be influenced by age-related changes in the size and structure of social networks.
Socioeconomic resources
Despite playing a prominent role in a wide variety of life domains, including mental and physical health across the life course, socioeconomic status (SES) and its components (e.g., income) have long been overlooked in most LGBT health studies, most often treated as control covariates (Conron et al., 2010; Dilley, Simmons, Boysun, Pizacani, & Stark, 2010). Yet there is strong and conclusive evidence in the general population that SES is a primary social determinant of mental and physical health (Braveman, Cubbin, Egerter, Williams, & Pamuk, 2010; Williams, 1990). Several studies have also investigated the relationship between SES and mental and physical health among older adults in the general population, finding that lower SES is associated with poorer physical (Grundy & Holt, 2001; Grundy & Sloggett, 2003) and mental health (Norstrand, Glicksman, Lubben, & Kleban, 2012). Some evidence suggests that sexual minority adults have higher rates of poverty than heterosexual adults (Badgett, Durso, & Schneebaum, 2013), and unemployment and lower education level have been associated with poorer social well-being among LGB adults (Kertzner et al., 2009). To date, however, there is very limited information about potential differences in SES between bisexual older adults and lesbian and gay older adults. The few studies that have compared bisexual adults with lesbian and gay adults have found lower income levels (Fredriksen-Goldsen et al., 2010; Hsieh, 2014) and greater financial problems (Jorm et al., 2002; Klein & Dudley, 2014) among bisexuals, but how these differences interact with older age, and their associations with mental and physical health among bisexual older adults, has yet to be explored. Although it is possible that resources available to older adults (e.g., Medicare) may help level some disparities in economic resources, it is likely that the compounding effects of less wealth-building over the life course and decreasing likelihood of new education or income growth in older age result in persistent or increasing SES disparities in older age.
Mental and physical health
Each of the identified predictors—greater internalized stigma, lower identity disclosure, fewer social resources, and lower SES—has been associated with poorer psychological well-being and elevated psychological distress in sexual minority adults (Kertzner et al., 2009; Lewis, Derlega, Griffin, & Krowinski, 2003; Morris et al., 2001). Yet findings have been mixed regarding whether bisexual adults actually experience greater psychological distress compared with lesbians and gay men. While some studies have identified elevated levels of distress and mental health concerns for bisexual compared with lesbians and gay men (e.g., Bostwick et al., 2015; Fredriksen-Goldsen et al., 2010; Jorm et al., 2002; Koh & Ross, 2006; Rothblum & Factor, 2001), others have found no significant differences in average levels of distress between these subgroups (e.g., Balsam, Beauchaine, Mickey, & Rothblum, 2005; Lewis et al., 2009). The limited evidence available with bisexual older adults suggests that they may have poorer general mental health compared with lesbian and gay older adults (Fredriksen-Goldsen et al., 2011), but detailed explorations of factors associated with bisexual older adults’ mental health have not yet been conducted.
There is consistent evidence of physical health disparities between bisexual and other sexual minority adults. Compared with lesbians, bisexual women more frequently report poor general health and health-related quality of life, limited activities due to health, and adverse health behaviors such as smoking and excessive drinking (Fredriksen-Goldsen et al., 2010) and are more likely to have ever contracted a sexually transmitted infection (Bostwick et al., 2015). Other studies have found poorer self-rated health for both bisexual women and bisexual men compared with lesbians and gay men (Gorman et al., 2015; Veenstra, 2011); bisexual college students compared with gay and lesbian students report significantly higher levels of chronic pain, colds, and flu (Klein & Dudley, 2014). In one study of adults aged 50 and older, Fredriksen-Goldsen and colleagues (Fredriksen-Goldsen, Kim et al., 2013) reported that bisexual men compared with gay men were more likely to have a diagnosis of diabetes and less likely to have had an HIV test in a population-based sample from Washington State; bisexual older adults also reported higher levels of internalized stigma and identity concealment compared with lesbian and gay older adults, which were risk factors for poor general health and disability (Fredriksen-Goldsen, Emlet et al., 2013).
Present Study
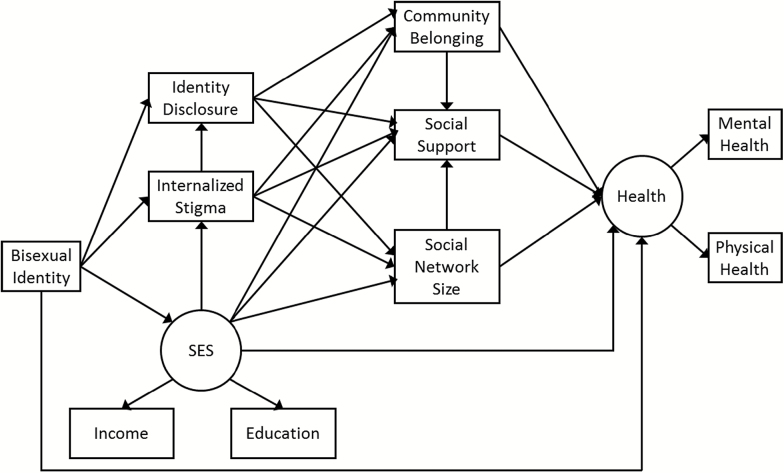
Based on the Health Equity Promotion Model and existing research, we tested three hypotheses in this study. First, we hypothesized that bisexual older adults would have poorer health compared with lesbians and gay men of similar age (Hypothesis 1). Next, we expected that bisexual older adults would show disadvantages in sexual identity factors (lower level of identity disclosure and elevated internalized stigma) and social resources (less positive sense of LGBT community belonging, smaller social network size, and lower level of social support) compared with lesbians and gay men of similar age and that these disadvantages would partially explain the association between bisexual identity and poorer health (Hypothesis 2). Finally, we hypothesized that bisexual older adults would show disadvantages in SES compared with lesbians and gay men of similar age and that this disadvantage would further explain the association between bisexual identity and poorer health (Hypothesis 3), both independently and by contributing to the disadvantages in Hypothesis 2. The full hypothesized model is shown in Figure 1.
Figure 1.
Hypothesized model.
Method
Caring and Aging with Pride is the first federally funded and largest study to date of sexual and gender minority older adults. In 2010, through community-based collaborations with 12 community agencies across the United States, 2,560 LGBT adults aged 50 years and older were surveyed. A complete description of the methods used in this study has been published (see Fredriksen-Goldsen, Emlet et al., 2013). This study selected those participants who identified as bisexual, lesbian, or gay, with a final sample of 2,463. The key domains assessed included sexual identity, other demographic and background characteristics, SES, sexual identity factors, social resources, and mental and physical health.
Measures
Background characteristics
Demographic and background characteristics included in the study were age (in years, ranging 50–95), gender (1: women, 2: men, and 3: other), and race/ethnicity (0: Hispanic, African American, Asian or Pacific Islander, or other person of color and 1: Non-Hispanic White). Sexual identity was measured by a single item: “Do you consider yourself to be: 1: Gay, 2: Lesbian, 3: Bisexual, 4: Heterosexual or straight, and 5: Other.” A binary variable was created: 0: lesbian or gay versus 1: bisexual. (Participants identifying as heterosexual or other were not included in this analysis.)
Sexual identity factors
Sexual identity factors measured in this study were internalized stigma and identity disclosure. Internalized stigma was assessed with a modified version of the Homosexual Stigma Scale (Herek, Cogan, Gillis, & Glunt, 1998; Liu, Feng, Rhodes, & Liu, 2009). Participants were asked to rate to what extent they agreed with five statements pertaining to their LGBT identity, such as “I feel that being lesbian, gay, bisexual or transgender is a personal shortcoming for me” and “I have tried to not be lesbian, gay, bisexual or transgender.” Summary scores were created by averaging across the items, ranging from 1 (strongly disagree) to 4 (strongly agree), with a higher score representing a greater level of internalized stigma (Cronbach’s α = .78). Identity disclosure was assessed with a modified version of the Outness Inventory scale (Mohr & Fassinger, 2000). Participants were asked to rank to what degree their sexual identity was known to 12 specific groups of people or individuals including family members, best friend, supervisor, neighbors, faith community, and primary physician. We computed summary scores by taking the weighted average across items to accommodate nonexistence of certain relationships. In other words, only items representing existing relationships were included in calculation of the summary scores. The summary scores ranged from 1 (definitely do not know) to 4 (definitely know) (Cronbach’s α = .92).
Social resources
Social resources included three components: social support, social network size, and positive sense of community belonging. To measure social support, we used the 4-item abbreviated Medical Outcomes Study Social Support Survey (Gjesfjeld, Greeno, & Kim, 2008; Sherbourne & Stewart, 1991) assessing the availability when needed of different types of support, such as “someone to turn to for suggestions about how to deal with a personal problem.” The summary score was the average across items ranging from 1 (never) to 4 (always) (Cronbach’s α = .85). Social network size was calculated by summing the reported number of people (e.g., friends, family members, colleagues, and neighbors) the participant interacted with in a typical month. Because the distribution of the summed scores was highly skewed with a few outliers, we recoded the scores by quartiles, with 1 indicating low 25% (small network) and 4 indicating high 25% (large network). We measured community belonging with two items, asking participants to indicate the extent of their positive feelings about belonging to LGBT communities. The average score ranging from 1 (strongly disagree) to 4 (strongly agree) was computed, with higher scores representing greater community belonging. The Spearman-Brown statistic was used for reliability = 0.95 (Eisinga, Grotenhuis, & Pelzer, 2013).
Socioeconomic status
Consistent with Grundy and Holt’s recommendation (2001), we included household resources and education in our measurement of SES. Although occupation is often included as a component of SES, in this sample the majority were retired or not employed. Household resources were assessed by asking participants to select their pre-tax household income level in 2009. The six income levels ranged from less than $20,000 to $75,000 or more. Level of education was measured by asking participants to indicate the highest grade completed, ranging from 1 (never attended school or only attended kindergarten) to 6 (4 years of college or more). Both of these variables were treated as continuous and used as observed indicators of a latent SES variable.
Health
Health was measured with the SF-8 Health Survey (Ware, Kosinski, Dewey, & Gandek, 2001), which includes 8 items regarding physical and mental health. The physical health subscale asks participants to rate their health during the past 4 weeks on four domains, including physical functioning, limitations due to physical problems, bodily pain, and general health. The mental health subscale also includes four domains: vitality, social functioning, mental health, and role limitations due to emotional problems. Each subscale yields a continuous summary score ranging from 0 to 100, with higher scores indicating better health (Cronbach’s α for physical health = .89; mental health = .86). These scores were used as observed indicators of a latent health variable.
Analyses
In preliminary analyses, we examined bivariate correlations and whether there were significant differences between bisexual versus lesbian and gay older adults on demographic and background characteristics as well as the variables included in our hypothesized model. Next, structural equation modeling (SEM) using full information maximum likelihood estimation with robust standard errors was conducted to test the hypothesized model with direct and indirect effects. We used a multistep model building approach to systematically examine our hypotheses: first, we computed a model with only the direct effect from bisexual identity to health; second, we added sexual identity factors and social resources as mediators; and finally, we added SES as an additional mediator to complete the hypothesized model (Figure 1). The fit of this full model was assessed with the Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), and the Standardized Root Mean Square Residual (SRMR). A series of systematic modifications consistent with the conceptual framework were implemented based on modification indices to produce the best-fitting final model (Figure 2). Based on the recommendations from Kenny (2014), the current study utilized cutoff points for good model fit as follows: RMSEA = 0.05, CFI = 0.9, TLI = 0.9, and SRMR = 0.08. Standardized coefficients for both latent and observed variables were reported to facilitate the interpretation of study results. For exploratory purposes, we also stratified the sample and ran the model separately by gender. All statistical analyses were conducted in Mplus 7.1 (Muthén & Muthén, 1998–2012).
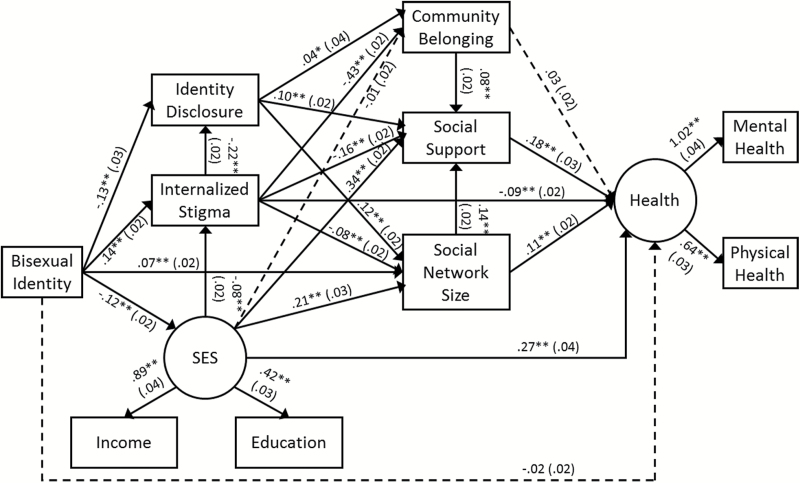
Figure 2.
Final fitted model. Dashed lines indicate nonsignificant pathways. RMSEA = .044 (90% CI .039–.049); CFI = .948; TLI = .907; SRMR = .029.
Results
Preliminary Analyses
In the sample, 174 participants identified as bisexual. On average, the sample was 66.7 years of age (SD = 8.9), with 36.2% identifying as women, 63.2% as men, and 0.6% as other. About 13.2% were people of color. Table 1 summarizes the demographic and background characteristics and descriptive statistics for the other key variables. Bisexual older adults reported poorer mental and physical health compared with lesbian and gay older adults.
Table 1.
Characteristics of Sample and Bivariate Analyses
| Overall | Bisexual | Lesbian/Gay | ||
|---|---|---|---|---|
| N = 2,463 | n = 174 | n = 2,289 | ||
| Mean or % (SD)a | Mean or % (SD)a | Mean or % (SD)a | p | |
| Demographic background | ||||
| Age | 66.73 (8.90) | 65.69 (9.40) | 66.81 (9.06) | .13 |
| Genderb | .00 | |||
| Female | 36.18 | 47.70 | 35.30 | |
| Male | 63.22 | 46.55 | 64.48 | |
| Other | 0.61 | 5.75 | 0.22 | |
| Race/Ethnicityc | .77 | |||
| Person of color | 13.15 | 13.87 | 13.09 | |
| Non-Hispanic White | 86.85 | 86.13 | 86.91 | |
| Sexual identity factors | ||||
| Internalized stigma | 1.46 (0.56) | 1.74 (0.67) | 1.44 (0.55) | .00 |
| Identity disclosure | 3.49 (0.62) | 3.14 (0.90) | 3.52 (0.60) | .00 |
| Social resources | ||||
| Community belonging | 3.42 (0.77) | 3.28 (0.81) | 3.44 (0.78) | .01 |
| Social network size | 2.50 (1.18) | 2.59 (1.27) | 2.50 (1.25) | .37 |
| Social support | 3.10 (0.75) | 2.91 (0.80) | 3.12 (0.78) | .00 |
| Socioeconomic status | ||||
| Educational level | 5.65 (0.66) | 5.57 (0.78) | 5.65 (0.66) | .19 |
| Income | 3.99 (1.93) | 3.27 (1.96) | 4.04 (1.96) | .00 |
| Health | ||||
| Physical—SF-8 Scaled Score | 69.99 (21.82) | 65.69 (20.07) | 70.32 (21.87) | .00 |
| Mental—SF-8 Scaled Score | 71.12 (20.33) | 65.41 (22.33) | 71.56 (20.11) | .00 |
Notes: aAll the standard deviations for continuous variables were calculated with 300 bootstrapped replications.
bBased on the result from Fisher exact test.
cBased on the result from chi-square test.
Table 2 presents the results of bivariate correlations among the variables in the study. Because race/ethnicity, gender, and age were significantly and highly correlated with many of the other variables in the model, we controlled for those variables in order to obtain better estimations. Moreover, although community belonging was not significantly associated with education level, all the other correlations were significant with moderate magnitudes, suggesting that SEM was an appropriate analytic approach.
Table 2.
Bivariate Correlations between Factors
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Bisexual | |||||||||||||
| (2) Non-Hispanic White | — | ||||||||||||
| (3) Gender: Male | — | .03 | |||||||||||
| (4) Gender: Other | — | −.24** | — | ||||||||||
| (5) Age | −.03 | .08** | .18** | −.04† | |||||||||
| (6) Internalized stigma | .14** | −.03 | .14** | .02 | .06** | ||||||||
| (7) Identity disclosure | −.15** | .03 | −.08** | −.03 | −.25** | −.24** | |||||||
| (8) Community belonging | −.05* | .02 | −.09** | −.01 | −.09** | −.44** | .16** | ||||||
| (9) Social support | −.07** | .08** | −.14** | −.01 | −.06** | −.27** | .22** | .21** | |||||
| (10) Social network size | .02 | .05* | −.10** | −.02 | −.09** | −.12** | .16** | .19** | .26** | ||||
| (11) Educational level | −.03 | .09** | −.05** | .00 | −.06** | −.04* | .11** | .01 | .15** | .14** | |||
| (12) Income | −.11** | .11** | −.03 | −.03 | −.17** | −.09** | .15** | .05* | .37** | .20** | .37** | ||
| (13) Mental health | −.08** | −.09** | .02 | −.03 | −.00 | −.19** | .06** | .14** | .35** | .23** | .17** | .29** | |
| (14) Physical health | −.05** | .05* | .08** | −.03 | −.11** | −.10** | .04* | .07** | .17** | .12** | .17** | .29** | .65** |
Notes: Factors (1)–(4) are binary and (5)–(14) are continuous. Correlation coefficients between a binary and a continuous variable are calculated with point-biserial correlation; correlation coefficients between two binary variables are calculated with tetrachoric correlation.
† p < .1. *p < .05. **p < .01.
Structural Equation Modeling
Model building
The first model we tested, which included only the direct effect from bisexual identity to health, showed that there was, as hypothesized (Hypothesis 1), a negative association between bisexual identity and health (standardized β = −.08, p < .001). The second model, which included sexual identity factors and social resources, indicated that all of the hypothesized paths were significant and in the expected direction; the direct effect from bisexual identity to health remained significant as well (standardized β = −.04, p = .03). Finally, in the full model adding SES as an additional mediator, the direct effect from bisexual identity to health was no longer significant (standardized β = −.02, p = .42), indicating that the mediating pathways fully explained the association between bisexual identity and health.
Final model
The full fitted model is presented in Figure 2. Fit indices suggested that the model fits the data well (RMSEA = .044, 90% CI: 0.039–0.049; CFI = .948; TLI = .907; SRMR = .029). Most of the hypothesized pathways were significant, with two exceptions: There was no association between SES and community belonging, or between community belonging and health. Moreover, additional direct relationships emerged between stigma and health (standardized β = −.09, SE = .02, p < .01) and between bisexual identity and social network size (standardized β = .07, SE = .02, p < .01).
Indirect effects, which address Hypotheses 2 and 3, are summarized in Table 3. Consistent with Hypothesis 2, bisexuals’ poorer health compared with lesbians and gay men was explained in part by significant indirect effects via combinations of sexual identity factors and social resources. One indirect effect involved only internalized stigma as an additional mediator: Bisexuals had higher internalized stigma, which predicted poorer health. Other indirect effects involved both identity disclosure and social resources as mediators (e.g., bisexuals had lower levels of identity disclosure, which predicted lower social support, which in turn predicted poorer health). Unexpectedly, a pair of protective social pathways involving social network size emerged (i.e., after adjusting for the other variables in the model, bisexual identity was associated with larger social network size, which in turn was associated with better health).
Table 3.
Significant Indirect Effects of Major Pathways Connecting Bisexual Identity to Health
| Major pathways | Number of effects | Examples | Total effect |
|---|---|---|---|
| Indirect effects showing risk via psychosocial processes | |||
| Internalized stigma | 1 | Bisexual → Internalized Stigma → Health | −.013** (.004) |
| One or more social resources | 4 | Bisexual → Internalized Stigma → Social Support → Health | −.006** (.002) |
| Internalized stigma | |||
| One or more social resources | 3 | Bisexual → Identity Disclosure → Social Support → Health | −.004** (.001) |
| Identity disclosure | |||
| One or more social resources | 3 | Bisexual → Internalized Stigma → Identity Disclosure → Social Network Size → Health | −.001** (.001) |
| Identity disclosure | |||
| Internalized stigma | |||
| Indirect effects showing protection via psychosocial processes | |||
| Social network size | 1 | Bisexual → Social Network Size → Health | .008** (.003) |
| Social support | 1 | Bisexual → Social Network Size → Social Support → Health | .002* (.001) |
| Social network size | |||
| Indirect effects showing risk via SES | |||
| SES | 1 | Bisexual → SES → Health | −.033** (.008) |
| Internalized stigma | 1 | Bisexual → SES → Internalized Stigma → Health | −.001* (.001) |
| SES | |||
| One or more social resources | 3 | Bisexual → SES → Social Support → Health | −.011** (.002) |
| SES | |||
| One or more social resources | 7 | Bisexual → SES → Internalized Stigma → Community Belonging → Social Support → Health | −.001** (.001) |
| Internalized stigma | |||
| SES |
Notes: All estimates are standardized. Only significant indirect effects are included in effect total.
SES = socioeconomic status.
A large cluster of indirect pathways involving SES were also significant, consistent with Hypothesis 3. One effect involved SES alone as a mediator: Bisexuals had lower SES, which in turn predicted poorer health. Other effects also involved internalized stigma, identity disclosure, social resources, or a combination of these variables (e.g., bisexuals’ lower SES predicted greater internalized stigma, which in turn predicted lower social support, which in turn predicted poorer health).
When we ran the model separately by gender, the findings for men were similar to the full sample (all directions and significances were identical). For women, we observed changes in four paths: one path became marginally significant (the path from SES to stigma, p = .07), whereas three others were no longer significant (bisexual to network size, p = .53; stigma to network size, p = .65; and network size to health, p = .15). All other pathways for women were identical in direction and significance to the full sample.
Discussion
In this study, one of the first to examine health disparities in bisexual older adults compared with lesbian and gay older adults, we used the Health Equity Promotion Model, an intersectional life course framework, to identify multiple potential mechanisms that influence the aging process in this largely invisible population. We found that bisexual older adults had poorer mental and physical health compared with lesbians and gay men of similar age (Hypothesis 1). We also found that they had higher levels of internalized stigma, lower levels of identity disclosure, and lower levels of some social resources (social support and community belonging) compared with lesbian and gay older adults and that these factors partially explained the association between bisexual identity and poorer health (Hypothesis 2). Finally, we found that bisexual older adults experienced disadvantages in SES, which further helped explain their poorer health (Hypothesis 3).
On the whole, our findings support the idea that the accumulation of disadvantage results in persistent health inequities for bisexuals in older age. The historical context of invisibility and rejection of bisexuality may limit access to resources across the life course, resulting by older age in more limited accumulation of wealth and health that supports optimal aging. It is important to note that this does not indicate these processes are completely unique to bisexual older adults; similar mechanisms may operate for some lesbian and gay older adults as well, contributing to the health disparities observed in previous studies between sexual minority older adults and heterosexuals of similar age. Our model highlights that identifying as bisexual, as opposed to lesbian or gay, confers additional risk for experiencing these adverse processes, with meaningful implications for health and aging.
Pathways involving sexual identity factors and social resources were highly predictive of differences in health outcomes. Compared with lesbian and gay older adults, bisexual older adults experienced greater stigma, less identity disclosure, less social support, and less community belonging. These findings indicate that disadvantages in social positions observed in working-age bisexuals also extend into older age. High levels of internalized stigma and identity concealment may be barriers to obtaining important social resources that contribute to health and well-being; for example, bisexual adults’ relative lack of acceptance into sexual minority communities may limit their access to support and specialized services within these communities. Furthermore, during the aging process, older adults’ social networks often shrink (Ajrouch, Blandon, & Antonucci, 2005) and they may become more dependent on other types of support services. Thus, bisexual adults may face dual mutually maintained challenges as they age: high need for social and health resources due to the accumulation of disadvantages over time, along with low access to the communities that may be best positioned to address these elevated needs.
Notably, SES was also a strong explanatory mechanism for the health disparities we observed in bisexual older adults, directly and indirectly explaining more of the variance in health outcomes than any other predictor we examined. Consistent with the Health Equity Promotion Model, these findings highlight the overwhelming importance of socioeconomic resources to health and well-being, which has been well established in other populations but largely neglected in research with sexual minorities and older populations. These findings also raise important questions about how bisexual adults come to be of low SES in middle and older age. It has been documented that bisexual individuals begin to experience a variety of disadvantages in their earlier years, including lower SES (Fredriksen-Goldsen et al., 2010; Hsieh, 2014). Moreover, in our sample, bisexual older adults had similar educational attainment but significantly lower income levels than their lesbian and gay peers, indicating that they may also experience more job insecurity or other barriers to reaching their full earning potential. The reasons for this remain to be investigated in future research; one possibility is that biases encountered at the workplace, which likely sustain high levels of internalized stigma, may interfere with career advancement. The effects of these and other disadvantages over a lifetime may render it difficult for individuals to escape poor socioeconomic conditions and increase the likelihood of mental and physical health disparities as they age. Thus, prevention and intervention programs for this population must both be accessible to the individuals at highest risk for adverse health outcomes (including those with limited resources) and, where possible, target the specific socioeconomic factors that are most detrimental.
Despite their disadvantages, bisexual older adults also displayed important resources that need to be recognized. In addition to adversity-oriented pathways that contributed to the disparities we observed, we also identified potential protective pathways involving social network size. The bivariate association between identifying as bisexual and network size was not significant. However, when disadvantages in identity-related factors and SES were partialed out, bisexual identity was associated with having a larger social network compared with lesbian and gay older adults. Social network size was positively associated with social support, which in turn was associated with better health outcomes. This finding suggests that promoting identity-related and socioeconomic resources could help bisexual older adults build social networks. At the same time, it is important to consider that bisexuals had lower levels of social support on average compared with lesbian and gay older adults, suggesting that perhaps they have social networks but receive lower quality of support from their social connections. This finding requires further study to fully understand, especially because we only see it after adjusting for other factors. Research has shown that bisexual older adults often have different life histories than lesbian and gay older adults (e.g., higher likelihood of opposite-sex marriage and parenthood), resulting in differing social relations and social network size and composition throughout adulthood that carries into older age (Fredriksen-Goldsen et al., in press; Goldsen et al., in press; Kim et al., in press). Protective pathways such as these may provide promising opportunities to develop tailored interventions for bisexual older adults focused on increasing resilience, building on individuals’ existing social resources and strengths, and promoting equity in health and well-being.
In the exploratory analyses of gender differences in pathways to health, we found that among women social network size may not be a key factor in determining health disparities between bisexual women and lesbians, although quality of network does account for such differences. Some previous studies have found that among women in general, larger social network size is associated with potentially greater burden (Antonucci, Ajrouch, & Birditt, 2014) given caregiving and other family responsibilities. Overall, it will be important to further investigate intersections between gender and sexual identities, which may be important considerations in the context of developing prevention and intervention strategies. Moreover, sexual identity can be fluid over the course of an individual’s life (Diamond, 2015), particularly among women, and thus future research examining sexual identity history in addition to current sexual identity may further illuminate pathways to health that differ by gender.
The findings from this study further our knowledge about older bisexuals’ health and aging in multiple ways. First, they suggest that bisexuals’ health disparities do not resolve with age, indicating that older bisexuals are an at-risk population that is likely difficult to reach, highlighting the need for targeted services. Additionally, we identified key elements of the Health Equity Promotion Model that contribute to bisexuals’ health inequities in older age, including SES which is often overlooked. And, importantly, we took a developmental approach to examining risk and resilience, examining pathways (i.e., indirect effects involving one or more intervening variables) across which bisexual older adults differentially accumulate health risk, rather than comparing single predictors between different sexual minority groups as previous research has done. This approach revealed that both adverse and health-promoting pathways contribute uniquely to health outcomes among bisexual older adults. These pathways, moreover, can intertwine with each other, suggesting that risk and protective factors on multiple levels interact with each other to collectively shape bisexual older adults’ mental and physical health and well-being.
These findings must be interpreted in light of the study’s limitations. First, because the study design was cross-sectional, inferences about causal relationships and directionality of associations are limited. Although the associations we hypothesized were derived from an empirically grounded model, we cannot conclude that the mechanisms we observed were causal. Second, as the sampling of participants was agency and community-based and our sample size of bisexual-identified participants was low relative to population estimates, the findings may not be generalizable to the larger population of bisexual older adults. The community-based agencies in this collaboration were serving LGBT adults and the bisexuals in this sample may have different needs and strengths than bisexuals being served in mainstream agencies.
Third, as health and well-being are multidimensional, some important predictors of bisexual older adult health were likely not captured by our study. The mediational pathways we modeled explained a modest proportion (22%) of the variance in health; thus, although the present study sheds light on important processes linking bisexual identity with health, other major influences on health were outside the scope of this study. Future research is needed to investigate additional factors, which may include, for example, healthcare access and utilization and health-promoting and risk behaviors among bisexuals. In addition, longitudinal research incorporating historical and ongoing experiences will undoubtedly contribute to a fuller understanding of how LGB older adults arrive at their health status in older age. For instance, sexual identity, attraction, and behavior may shift over an individual’s life, which may in turn profoundly influence social resources, health, and well-being. Furthermore, structural factors, such as anti-discrimination legislation, change over time and may also influence opportunities for good health.
Conclusion
Future longitudinal research will be immensely helpful in illuminating how health and aging processes differ for bisexual older adults compared with their lesbian and gay peers. Whereas a cross-sectional study can provide only a snapshot view of a population’s health, surveying the same participants repeatedly can provide information about factors such as illness incidence rates and trajectories over time of health and the factors that influence health and well-being. The present study laid the foundation for longitudinal research, which is currently underway, by identifying potential pathways of risk and resilience that contribute to the health of bisexual older adults. In the future, a better understanding of the processes by which bisexual older adults reach disadvantaged and optimal health statuses will support the development of interventions that are tailored to address the distinct needs of bisexuals as they age, which will be an important step forward to reducing this population’s health disparities.
Funding
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG026526 (Fredriksen-Goldsen, PI).
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. K. I. Fredriksen-Goldsen originated the study, synthesized the conceptualization, and led manuscript development. C. Shiu contributed to the development and conceptualization of the study and served as lead data analyst. A. E. B. Bryan conducted data analyses and participated in the writing and editing of the manuscript. J. Goldsen participated in the conceptualization, literature review, writing, and editing. H.-J. Kim contributed to the development and conceptualization of the study and interpretation of findings. All authors participated in the preparation of the manuscript.
References
- Ajrouch K. J. Blandon A. Y., & Antonucci T. C (2005). Social networks among men and women: The effects of age and socieconomic status. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, S311–S317. doi:10.1093/geronb/60.6.S311 [DOI] [PubMed] [Google Scholar]
- Antonucci T. C. Ajrouch K. J., & Birditt K. S (2014). The convoy model: explaining social relations from a multidisciplinary perspective. The Gerontologist, 54, 82–92. doi:10.1093/geront/gnt118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badgett M. V. L. Durso L. E., & Schneebaum A (2013). New patterns of poverty in the lesbian, gay, and bisexual community. Los Angeles, CA: The Williams Institute; Retrieved from http://williamsinstitute.law.ucla.edu/research/census-lgbt-demographics-studies/lgbt-poverty-update-june-2013/ [Google Scholar]
- Balsam K. F. Beauchaine T. P. Mickey R. M., & Rothblum E. D (2005). Mental health of lesbian, gay, bisexual, and heterosexual siblings: Effects of gender, sexual orientation, and family. Journal of Abnormal Psychology, 114, 471–476. doi:10.1037/0021-843X.114.3.471 [DOI] [PubMed] [Google Scholar]
- Balsam K. F., & Mohr J. J (2007). Adaptation to sexual orientation stigma: A comparison of bisexual and lesbian/gay adults. Journal of Counseling Psychology, 54, 306–319. doi:10.1037/0022-0167.54.3.306 [Google Scholar]
- Bostwick W. B. Hughes T. L., & Everett B (2015). Health behavior, status, and outcomes among a community-based sample of lesbian and bisexual women. LGBT Health, 2, 121–126. doi:10.1089/lgbt.2014.0074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P. A. Cubbin C. Egerter S. Williams D. R., & Pamuk E (2010). Socioeconomic disparities in health in the United States: What the patterns tell us. American Journal of Public Health, 100(Suppl. 1), S186–S196. doi:10.2105/AJPH.2009.166082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmueller T., & Carpenter C. S (2010). Disparities in health insurance coverage, access, and outcomes for individuals in same-sex versus different-sex relationships, 2000-2007. American Journal of Public Health, 100, 489–495. doi:10.2105/AJPH.2009.160804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conron K. J. Mimiaga M. J., & Landers S. J (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100, 1953–1960. doi:10.2105/AJPH.2009.174169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa P. A. Pereira H., & Leal I (2013). Internalized homonegativity, disclosure, and acceptance of sexual orientation in a sample of Portuguese gay and bisexual men, and lesbian and bisexual women. Journal of Bisexuality, 13, 229–244. doi:10.1080/15299716.2013.782481 [Google Scholar]
- Diamond L. M. (2015). Sexual fluidity. In Whelehan P., Bolin A. (Eds.), The International Encyclopedia of Human Sexuality (pp. 1115–1354). Hoboken, NJ: John Wiley & Sons. doi:10.1002/9781118896877.wbiehs452 [Google Scholar]
- Dilley J. A. Simmons K. W. Boysun M. J. Pizacani B. A., & Stark M. J (2010). Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific Northwest. American Journal of Public Health, 100, 460–467. doi:10.2105/AJPH.2007.130336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre M. E. (2007). Educational differences in age-related patterns of disease: Reconsidering the cumulative disadvantage and age-as-leveler hypotheses. Journal of Health and Social Behavior, 48, 1–15. doi:10.1177/002214650704800101 [DOI] [PubMed] [Google Scholar]
- Eisinga R. Grotenhuis M. t., & Pelzer B (2013). The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? International Journal of Public Health, 58, 637–642. doi:10.1007/s00038-012-0416-3 [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. (2016). The future of LGBT+ aging: A blueprint for action in services, policies and research. Generations, 40, 6–13. [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I., & Kim J.-H (in press). The science of conducting research with LGBT older adults - an introduction to Aging with Pride: National Health, Aging, Sexuality and Gender Study. The Gerontologist. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Emlet C. A. Kim H. J. Muraco A. Erosheva E. A. Goldsen J., & Hoy-Ellis C. P (2013). The physical and mental health of lesbian, gay male, and bisexual (LGB) older adults: The role of key health indicators and risk and protective factors. The Gerontologist, 53, 664–675. doi:10.1093/geront/gns123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Kim H. J. Barkan S. E. Balsam K. F., & Mincer S. L (2010). Disparities in health-related quality of life: A comparison of lesbians and bisexual women. American Journal of Public Health, 100, 2255–2261. doi:10.2105/AJPH.2009.177329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Kim H. J. Barkan S. E. Muraco A., & Hoy-Ellis C. P (2013). Health disparities among lesbian, gay, and bisexual older adults: Results from a population-based study. American Journal of Public Health, 103, 1802–1809. doi:10.2105/AJPH.2012.301110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Kim H.-J. Emlet C. A. Muraco A. Erosheva E. A. Hoy-Ellis C. P. Goldsen J., & Petry H (2011). The aging and health report: Disparities and resilience among lesbian, gay, bisexual, and transgender older adults. Seattle, WA: Institute for Multigenerational Health. [Google Scholar]
- Fredriksen-Goldsen K. I. Simoni J. M. Kim H. J. Lehavot K. Walters K. L. Yang J. , … Muraco A (2014). The health equity promotion model: Reconceptualization of lesbian, gay, bisexual, and transgender (LGBT) health disparities. The American Journal of Orthopsychiatry, 84, 653–663. doi:10.1037/ort0000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman M. R. Dodge B. Schick V. Herbenick D. Hubach R. D. Bowling J., . . . & Reece M (2014). From BIAS to bisexual health disparities: Attitudes toward bisexual men and women in the United States. LGBT Health, 1, 309–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsen J. Bryan A. E. B. Muraco A. Kim H.-J. Jen S., & Fredriksen-Goldsen K. I.(in press). Who says I do: The changing context of marriage and health and quality of life for older LGBT older adults. The Gerontologist. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman B. K. Denney J. T. Dowdy H., & Medeiros R. A (2015). A new piece of the puzzle: Sexual orientation, gender, and physical health status. Demography, 52, 1357–1382. doi:10.1007/s13524-015-0406-1 [DOI] [PubMed] [Google Scholar]
- Gjesfjeld C. Greeno C., & Kim K (2008). A confirmatory factor analysis of an abbreviated social support instrument: The MOS-SSS. Research on Social Work Practice, 18, 231–237. doi:10.1177/1049731507309830 [Google Scholar]
- Grossman A. H. D’Augelli A. R., & Hershberger S. L (2000). Social support networks of lesbian, gay, and bisexual adults 60 years of age and older. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 55, 171–179. doi:10.1093/geronb/55.3.p171 [DOI] [PubMed] [Google Scholar]
- Grundy E., & Holt G (2001). The socioeconomic status of older adults: How should we measure it in studies of health inequalities? Journal of Epidemiology and Community Health, 55, 895–904. doi:10.1136/jech.55.12.895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy E., & Sloggett A (2003). Health inequalities in the older population: The role of personal capital, social resources and socio-economic circumstances. Social Science & Medicine, 56, 935–947. doi:10.1016/s0277-9536(02)00093-x [DOI] [PubMed] [Google Scholar]
- Herd P. (2006). Do functional health inequalities decrease in old age? Educational status and functional decline among the 1931–1941 birth cohort. Research on Aging, 28, 375–392. doi:10.1177/0164027505285845 [Google Scholar]
- Herek G. M. Cogan J. C. Gillis J. R., & Glunt E. K (1998). Correlates of internalized homophobia in a community sample of lesbians and gay men. Journal of the Gay and Lesbian Medical Association, 2, 17–25. [Google Scholar]
- Herek G. M. Gillis J. R., & Cogan J. C (2009). Internalized stigma among sexual minority adults: Insights from a social psychological perspective. Journal of Counseling Psychology, 56, 32–43. doi:10.1037/a0014672 [Google Scholar]
- Hsieh N. (2014). Explaining the mental health disparity by sexual orientation: The importance of social resources. Society and Mental Health, 4, 129–146. doi:10.1177/2156869314524959 [Google Scholar]
- Jorm A. F. Korten A. E. Rodgers B. Jacomb P.A., & Christensen H (2002). Sexual orientation and mental health: Results from a community survey of young and middle-aged adults. British Journal of Psychiatry, 180, 423–427. doi:10.1192/bjp.180.5.423 [DOI] [PubMed] [Google Scholar]
- Kenny D. A. (2014). Measuring model fit. Retrieved from http://davidakenny.net/cm/fit.htm [Google Scholar]
- Kertzner R. M. Meyer I. H. Frost D. M., & Stirratt M. J (2009). Social and psychological well-being in lesbians, gay men, and bisexuals: The effects of race, gender, age, and sexual identity. The American Journal of Orthopsychiatry, 79, 500–510. doi:10.1037/a0016848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.-J. Fredriksen-Goldsen K. I. Bryan A. E. B., & Muraco A.(in press). Social network types and mental health among lesbian, gay, bisexual, and transgender (LGBT) older adults. The Gerontologist. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein N. A., & Dudley M. G (2014). Impediments to academic performance of bisexual college students. Journal of American College Health, 62, 399–406. doi:10.1080/07448481.2014.917653 [DOI] [PubMed] [Google Scholar]
- Koh A. S., & Ross L. K (2006). Mental health issues: A comparison of lesbian, bisexual and heterosexual women. Journal of Homosexuality, 51, 33–57. doi:10.1300/J082v51n01_03 [DOI] [PubMed] [Google Scholar]
- Legate N. Ryan R. M., & Weinstein N (2012). Is coming out always a “good thing”? Exploring the relations of autonomy support, outness, and wellness for lesbian, gay, and bisexual individuals. Social Psychological and Personality Science, 3, 145–152. doi:10.1177/1948550611411929 [Google Scholar]
- Lewis R. J. Derlega V. J. Brown D. Rose S., & Henson J. M (2009). Sexual minority stress, depressive symptoms, and sexual orientation conflict: Focus on the experiences of bisexuals. Journal of Social and Clinical Psychology, 28, 971–992. doi:10.1521/jscp.2009.28.8.971 [Google Scholar]
- Lewis R. J. Derlega V. J. Griffin J. L., & Krowinski A. C (2003). Stressors for gay men and lesbians: Life stress, gay-related stress, stigma consciousness, and depressive symptoms. Journal of Social and Clinical Psychology, 22, 716–729. doi:10.1521/jscp.22.6.716.22932 [Google Scholar]
- Liu H. Feng T. Rhodes A. G., & Liu H (2009). Assessment of the Chinese version of HIV and homosexuality related stigma scales. Sexually Transmitted Infections, 85, 65–69. doi:10.1136/sti.2008.032714 [DOI] [PubMed] [Google Scholar]
- Lyons A. Pitts M., & Grierson J (2013). Factors related to positive mental health in a stigmatized minority: An investigation of older gay men. Journal of Aging and Health, 25, 1159–1181. doi:10.1177/0898264313495562 [DOI] [PubMed] [Google Scholar]
- Meyer I. H., & Dean L (1998). Internalized homophobia, intimacy, and sexual behavior among gay and bisexual men. In Herek G. (Ed.), Psychological perspectives on lesbian and gay issues: Stigma and sexual orientation: Understanding prejudice against lesbians, gay men, and bisexuals (pp. 160–186). Thousand Oaks, CA: Sage Publications. doi:10.4135/9781452243818.n8 [Google Scholar]
- Mohr J. J., & Fassinger R. E (2000). Measuring dimensions of lesbian and gay male experience. Measurement and Evaluation in Counseling and Development, 33, 66–90. [Google Scholar]
- Mohr J. J., & Fassinger R. E (2006). Sexual orientation identity and romantic relationship quality in same-sex couples. Personality & Social Psychology Bulletin, 32, 1085–1099. doi:10.1177/0146167206288281 [DOI] [PubMed] [Google Scholar]
- Morris J. F. Waldo C. R., & Rothblum E. D (2001). A model of predictors and outcomes of outness among lesbian and bisexual women. American Journal of Orthopsychiatry, 71, 61–71. doi:10.1037//0002-9432.71.1.61 [DOI] [PubMed] [Google Scholar]
- Muthén L. K., & Muthén B. O (1998. –2012). Mplus User’s Guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Norstrand J. A. Glicksman A. Lubben J., & Kleban M (2012). The role of the social environment on physical and mental health of older adults. Journal of Housing for the Elderly, 26, 290–307. doi:10.1080/02763893.2012.651382 [Google Scholar]
- Robert S. A. Cherepanov D. Palta M. Dunham N. C. Feeny D., & Fryback D. G (2009). Socioeconomic status and age variations in health-related quality of life: Results from the national health measurement study. The Journals of Gerontology: Psychological Sciences and Social Sciences, 64, 378–289. doi:10.1093/geronb/gbp012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross M. W., & Rosser B. R (1996). Measurement and correlates of internalized homophobia: A factor analytic study. Journal of Clinical Psychology, 52, 15–21. doi:10.1002/(SICI)1097-4679(199601)52:1<15::AID-JCLP2>3.0.CO;2-V [DOI] [PubMed] [Google Scholar]
- Rothblum E. D., & Factor R (2001). Lesbians and their sisters as a control group: Demographic and mental health factors. Psychological Science, 12, 63–69. doi:10.1111/1467-9280.00311 [DOI] [PubMed] [Google Scholar]
- Sherbourne C. D., & Stewart A. L (1991). The MOS social support survey. Social Science & Medicine, 32, 705–714. doi:10.1016/0277-9536(91)90150-b [DOI] [PubMed] [Google Scholar]
- Veenstra G. (2011). Race, gender, class, and sexual orientation: intersecting axes of inequality and self-rated health in Canada. International Journal for Equity in Health, 10, 3. doi:10.1186/1475-9276-10-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J. E. Kosinski M. Dewey J. E., & Gandek B (2001). A manual for users of the SF-8 Health Survey. Lincoln, RI: Quality Metric Incorporated. [Google Scholar]
- Wallace S. P. Cochran S. D. Durazo E. M., & Ford C. L (2011). The health of aging lesbian, gay and bisexual adults in California. Policy Brief UCLA Center for Health Policy Research, PB2011-2, 1–8. [PMC free article] [PubMed] [Google Scholar]
- White L., & Cant B (2003). Social networks, social support, health and HIV‐positive gay men. Health and Social Care in the Community, 11, 329–334. doi:10.1046/j.1365- 2524.2003.00431.x [DOI] [PubMed] [Google Scholar]
- Williams D. R. (1990). Socioeconomic differentials in health: A review and redirection. Social Psychology Quarterly, 53, 81–99. doi:10.2307/2786672 [Google Scholar]