Abstract
Purpose
The purpose of this study was to determine the validity and reliability of the Polish version of the Questionnaire for Health-Related Resource Use in an Elderly Population [Fragebogen zur Inanspruchnahme medizinischer und nicht-medizinischer Versorgungsleistungen im Alter (FIMA)].
Patients and methods
This was a cross-sectional study conducted in a rehabilitation care unit in Poland between January and June of 2017. Sixty-one patients aged ≥65 years who had been admitted to the unit were enrolled into the study. Each participant was evaluated twice: once within 48 hours of admission (T1) and once after 2 weeks (T2).
Results
The translated instrument was understood by most respondents in a selected population and it maintained a reading and comprehension level that was accessible by most respondents, even of a low education level. With the aid of the prevalence-adjusted bias-adjusted kappa (PABAK) and intraclass correlation coefficient (ICC), 100% test–retest reliability for 10 out of the 12 questions that were subjected to analysis was indicated. The most frequent health-related resource uses were appointments at the general practitioner (90.2%) and orthopedist (54.1%), medication (93.4%), and the necessity to have glasses as supportive equipment (70.5%).
Conclusion
The Polish FIMA demonstrated very good test–retest reliability, good validity, and ease of use for elderly people. Further investigation is required. In the future, the routine use of this instrument could be encouraged to assess the use and demand for medical and nonmedical services among the elderly.
Keywords: assessment, geriatrics, quality of care, care coordination, decision-making
Introduction
In the next few decades, the populations of all EU countries are expected to age rapidly.1 This could have a major impact on the health care sector.2 Economic evaluations have become increasingly integrated with demographic trends.3 These data can provide unbiased estimates for the calculation of cost-effectiveness to suggest decisions on the effective and efficient use of health care resources.4,5 For example, in the UK, the National Institute for Health Research’s Health Technology Assessment (HTA) program is involved in funding research, including clinical trials, to investigate the clinical relevance and cost-effectiveness of a range of health technologies (eg, medicines, devices, procedures, and screening) used to promote health, prevent and treat diseases, and improve rehabilitation and long-term care.4 The use of questionnaires based on patient recall was found to be the most variable aspect of the HTA trials studied.
There are no universally recognized methods for economic data collection in HTA-funded trials, although a wide variety of techniques are recognized and used. These methods include patient self-reports (using questionnaires, interviews, and diary cards), use of routinely available data (eg, medical records and general practitioner [GP] records), and use of expert panels. Each method has its advantages and disadvantages.4,6 The use of questionnaires based on patient recall was found to be the most variable aspect of the HTA trials studied.7 In addition, data obtained through patient surveys can be linked with other social and medical patient data.4
In Poland, health-related resources are not routinely assessed due to a lack of available standardized instruments. Fragebogen zur Inanspruchnahme medizinischer und nicht-medizinischer Versorgungsleistungen im Alter (FIMA), the Questionnaire for Health-Related Resource Use in an Elderly Population, was developed in Germany by Seidl et al8 and is the first standardized, generic questionnaire for the older population, which collects the health-related resource use, designed to ensure comparability of medical and nonmedical care services across studies.
The German FIMA instrument is a self-administered questionnaire, which assesses nine features and contains 28 questions altogether: questions 1–18 refer directly to the use of medical and nonmedical services by the elderly, whereas questions 19–28 concern the sociodemographic characteristics of the person surveyed as well as an assessment of questionnaire difficulty and time spent completing it. A pilot study of the original FIMA version indicated good agreement between self-reported health-related quality of life and the use of nursing and home care resources (phi coefficient values between 0.52 and 0.58).8
The objective of this study was to determine the validity and reliability of the Polish version of FIMA. The aim of the validation was to produce a translated version in a foreign language, which is conceptually equivalent to the original version, as well as being clear and easy to understand.
Participants and methods
Participants and procedures
This cross-sectional study was approved by the Bioethics Committee of the Wroclaw Medical University in Poland (KB-419/2017).
A well-trained physician informed and obtained consent from the participants. A total of 61 elderly people, 65 years of age and older, who had been admitted within the previous 48 hours to a 42-bed rehabilitation unit at the District Saint Hedvig Hospital in Trzebnica in Poland, were recruited. Patients were excluded if they had a severe visual or auditory impairment, a life-threatening condition, or a poor command of Polish or if they were unwilling to participate. No individuals with cognitive impairments were included in this study. Each participant was evaluated twice: the first time within 48 hours of admission (T1) and the second time 2 weeks after admission (T2). All participants provided written informed consent. Before screening for health-related resource use, using the Polish version of the FIMA, each participant was assessed using the EQ-5D 3 level version (EQ-5D-3L) questionnaire to determine their health-related quality of life. EQ-5D-3L was introduced in 1990 by the EuroQol Group and comprises the following five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.9 Each dimension has three levels: no problems, some problems, and extreme problems. Participants were asked to indicate their health state by ticking the box next to the most appropriate statement in each of the five dimensions. Due to the lack of recognized instruments that assess the demand for medical and nonmedical services among the elderly, a questionnaire related to the quality of life was chosen.
In the Polish version of the questionnaire, the area of insurance was excluded (questions 17 and 18), due to the presence of only one insurer and lack of division of patients insured by the state and by private companies. Table 1 gives an overview of the requested services, quantities, units, and periods. The nursing and home care services were assessed separately in terms of formal and informal care. Inpatient stays were classified as psychiatric or nonpsychiatric due to different assessment rates.
Table 1.
FIMA: cost categories, variables, units, and time periods
| Cost category | Variable | Unit | Period |
|---|---|---|---|
| Ambulatory health care | GP, internist, internist with specialty (eg, cardiologist, gastroenterologist, nephrologist, diabetologist, gynecologist, surgeon, orthopedist, neurologist, dermatologist, ophthalmologist, urologist, dentist, psychotherapist), ambulatory stays at hospital, others | Number of appointments (including collection of prescriptions and home visits) | 3 months |
| Remedies | Physiotherapy (kinesiotherapy, massage, physical therapy), ergotherapy, medical pedicure, osteopathy | Number of appointments | 3 months |
| Nursing and home care services | Ambulatory community care, private nursing care, informal care (family, friends, and so on), short-term care | Number of days in a week/number of days in a month/number of hours and minutes a day | 3 months |
| Medicines | Name of drug, packaging size | Daily/weekly/monthly/yearly dosage | 7 days |
| Rehabilitation | Ambulatory and stationary stays | Number of days | 12 months |
| Stays in hospital (ambulatory and stationary) | Outpatient clinics, stationary stays (including stays at the psychiatric hospital) | Number of days | 12 months |
| Auxiliary equipment | Walking frame, glasses, hearing device, dental prosthesis, breathing apparatus, wheelchair, hygiene pads, bath seat, others | Ownership and usage | Currently and in the past 12 months |
| Relocations | Necessity to change the place of residence | Yes or no | 12 months |
| Form of residence | Private household, shelter flat, residential care, others | Yes or no | 12 months |
Abbreviations: FIMA, Fragebogen zur Inanspruchnahme medizinischer und nicht-medizinischer Versorgungsleistungen im Alter [Questionnaire for Health-Related Resource Use in an Elderly Population]; GP, general practitioner.
Development of the Polish version of the FIMA
The Polish version of the FIMA was developed following the “Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcome Measures”.10
The validation process for the FIMA involved a team, with scientific background and with requisite training and experience in the medical and social sciences, assembled by the investigator.
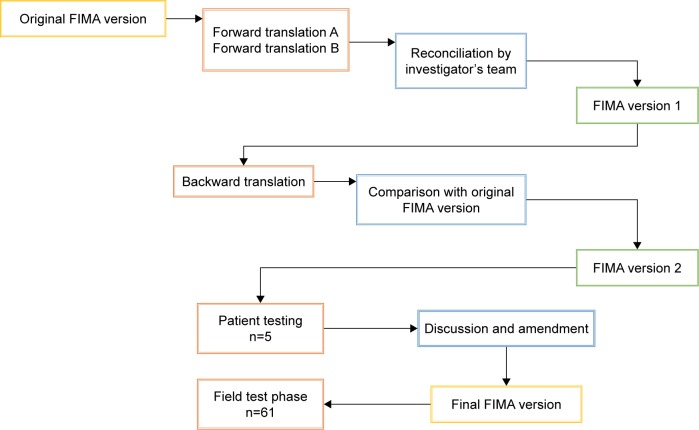
The validation of the FIMA questionnaire consisted of six steps (an algorithm is given in Figure 1):
Forward translation (passage from the source German language to Polish) by two local professional translators (named A and B in Figure 1), native target language speakers who were fluent in the source language.
Backward translation (translation of the first-reconciled forward version of the questionnaire back into the source German language) by a local professional translator, a native speaker of German who was fluent in the target language, with no access to the original German version of the questionnaire, finished with a comparison of the backward version with the original source version.
Feasibility study. The second version of the FIMA questionnaire (obtained after Step 2) was tested on a panel of five respondents. The test was performed using face-to-face interviews to inquire whether the patient had any difficulty in understanding the questionnaire and to check the patient’s interpretation of all items.
Proofreading by a native target language speaker and finalization. Both the translators and the investigator’s team reached a consensus after comparing and adapting the instrument so that the meaning would correspond to Polish culture.
The field test phase involved administration of the translated FIMA questionnaire to the target language population (61 elderly people at admission to the rehabilitation ward).
Statistical analyses of the data.
Figure 1.
Algorithm of the FIMA validation process.
Note: A and B represent the two local professional translators.
Abbreviation: FIMA, Fragebogen zur Inanspruchnahme medizinischer und nicht-medizinischer Versorgungsleistungen im Alter [Questionnaire for Health-Related Resource Use in an Elderly Population].
Statistical analysis
All statistical analyses were carried out with R for Windows (version 3.4.1).11 Demographic variables, as well as the use of the FIMA resource categories, are presented as mean ± SD and percentage. Cost categories, variables, units, and time periods of the FIMA are presented as frequency. Results were considered statistically significant at p<0.05.
For the assessment of test–retest reliability, patients completed the FIMA questionnaire for the second time 2 weeks later. Prevalence-adjusted bias-adjusted kappa (PABAK) and intraclass correlation coefficient (ICC) for each independent question were used to investigate the consistency between the two measurements. Values >0.4 were regarded as satisfactory.12 Internal reliability was assessed for the measurement points T1 and T2 with the use of logistic regression analyses. External validation was estimated by using the relationship between FIMA and a previously validated instrument, ie, correlation with the results of the assessment of psychophysical well-being (EQ-5D-3L scale) with the use of Yule’s Q coefficient was conducted.13
Results
Participant characteristics
Over a 6-month period, 70 participants were enrolled in the study. Seven were excluded due to their unwillingness to participate. Two patients were discharged before an assessment could take place. Figure 2 shows the details of the study in flowchart format. A total of 61 (mean age =73.7 years, SD =5.9 years) patients completed the study. The majority of the examined patients were female (75.4%, n=46), and most had graduated with postsecondary education (54.1%, n=33). Of the total patients surveyed, 55.7% (n=34) were married. All the people included in the study lived in their own households and were insured. Detailed sociodemographic data, as well as FIMA difficulty and completion time, are presented in Table 2. EQ-5D-3L scale results are presented in Table 3.
Figure 2.
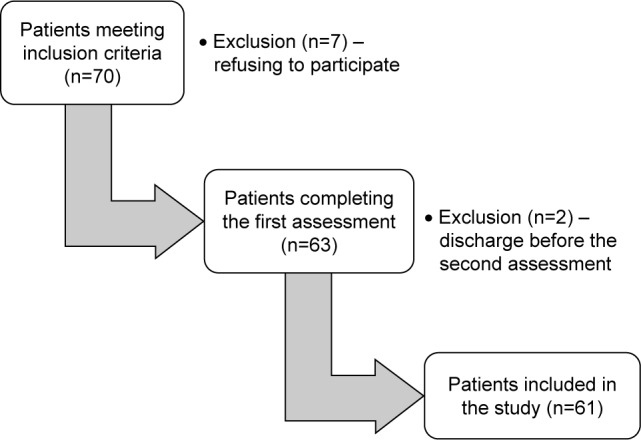
Study participant selection process.
Table 2.
Participant characteristics, FIMA completion time, and difficulty
| Characteristics | Participants (n=61) |
|---|---|
| Gender, n (%) | |
| Male | 15 (24.6) |
| Female | 46 (75.4) |
| Age, years, mean ± SD | 73.7±5.9 |
| Marital status, n (%) | |
| Married | 34 (55.7) |
| Widowed | 22 (36.1) |
| Divorced | 5 (8.2) |
| Level of qualification, n (%) | |
| University | 11 (18.0) |
| Postsecondary | 33 (54.1) |
| Vocational | 11 (18.0) |
| Primary | 6 (9.8) |
| FIMA completion time, mean ± SD | 15.6±7.3 |
| Minimum–maximum, minutes | 10–30 |
| FIMA difficulty, n (%) | |
| Alone | 57 (93.4) |
| With help | 4 (6.6) |
| Very easy | 18 (29.5) |
| Easy | 37 (60.7) |
| Difficult | 6 (9.8) |
Abbreviation: FIMA, Fragebogen zur Inanspruchnahme medizinischer und nicht-medizinischer Versorgungsleistungen im Alter [Questionnaire for Health-Related Resource Use in an Elderly Population].
Table 3.
EQ-5D-3L scale results
| Result | EQ-5D-3L1 (mobility), n (%) |
EQ-5D-3L2 (self-care), n (%) |
EQ-5D-3L3 (usual activities), n (%) |
EQ-5D-3L4 (pain/discomfort), n (%) |
EQ-5D-3L5 (anxiety/depression), n (%) |
|---|---|---|---|---|---|
| No problems | 32 (52.5) | 49 (80.3) | 31 (50.8) | 8 (13.1) | 34 (55.7) |
| Some problems | 29 (47.5) | 11 (18.0) | 28 (45.9) | 45 (73.8) | 25 (41.0) |
| Extreme problems | 0 (0) | 1 (1.7) | 2 (3.3) | 8 (13.1) | 2 (3.3) |
Abbreviation: EQ-5D-3L, three-level version of the EuroQol five-dimensional questionnaire.
Validity and reliability of the Polish FIMA
The minimum and maximum time taken to complete the Polish FIMA were 10 minutes and 30 minutes, respectively (mean =15.6 minutes; SD =7.3 minutes). The vast majority, 93.4% (n=57) of participants, completed the questionnaire alone, and 90.2% (n=55) rated the difficulty level as easy to very easy.
Test–retest reliability
The analysis of test–retest reliability included questions FIMA1–FIMA17 because the remaining questions concerned descriptive properties of the group. Five of the questions in the questionnaire were not considered (FIMA6, 13, 15, 16, and 17) because all the patients in T2 answered them in the same way; therefore, it was impossible to calculate the variance. With the aid of PABAK and ICC, 100% test–retest reliability for 10 out of the 12 questions subjected to analysis was obtained. There was indication for variability of answers in a separate measurement for the questions FIMA1 (PABAK =0.97 and ICC =0.66) and FIMA10 (PABAK =0.97 and ICC =0.97), signifying good and very good test–retest reliability, respectively (Table 4).
Table 4.
Test–retest reliability of the Polish version of the FIMA questionnaire
| Factors | Test–retest, PABAK, and ICC
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FIMA1 | FIMA2 | FIMA3 | FIMA4 | FIMA5 | FIMA7 | FIMA8 | FIMA9 | FIMA10 | FIMA11 | FIMA12 | FIMA14 | |
| Prevalence index | −0.95 | 0.41 | 0.90 | 0.97 | 0.25 | 0.93 | 0.67 | −0.87 | 0.10 | 0.80 | 0.05 | −0.90 |
| PABAK | 0.97 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0.97 | 1 | 1 | 1 |
| ICC | 0.66 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0.97 | 1 | 1 | 1 |
Abbreviations: FIMA, Fragebogen zur Inanspruchnahme medizinischer und nicht-medizinischer Versorgungsleistungen im Alter [Questionnaire for Health-Related Resource Use in an Elderly Population]; ICC, intraclass correlation; PABAK, prevalence-adjusted bias-adjusted kappa.
Internal reliability
Logistic regression analysis between the two FIMA measurements (T1 and T2) did not yield any significant values.
Theoretical and external validation
Two questions on the FIMA questionnaire, namely, FIMA5 and FIMA12, were characterized by the highest theoretical validity (FIMA5: T1 correlation =0.78 and T2 correlation =0.81; FIMA12: T1 correlation =0.76 and T2 correlation =0.75), indicating – at the same time – large variation in the answers given by respondents in these areas. The results of theoretical validity as well as those of Yule’s Q coefficient for the restriction of quality of life and the claimed resource use in the FIMA questions for T1 and T2 are shown in Table 5. Full, very good, or good compliance with all the EQ-5D-3L questions was obtained for the following FIMA questions: FIMA1, 3, 4, 5, and 7. The results for FIMA questions 6, 13, 15, 16, and 17 are not presented because all the participants answered them in the same way; therefore, it was impossible to calculate the variance.
Table 5.
Theoretical and external validation of the Polish version of the FIMA questionnaire
| Theoretical validity, Pearson’s correlation
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FIMA1 | FIMA2 | FIMA3 | FIMA4 | FIMA5 | FIMA7 | FIMA8 | FIMA9 | FIMA10 | FIMA11 | FIMA12 | FIMA14 | |
| T1 | 0.14 | 0.29 | 0.11 | 0.31 | 0.78 | 0.34 | 0.14 | 0.34 | −0.04 | 0.20 | 0.76 | 0.19 |
| p-value | 0.28 | 0.02 | 0.41 | 0.01 | <0.001 | 0.007 | 0.28 | 0.007 | 0.74 | 0.13 | <0.001 | 0.15 |
| T2 | −0.02 | 0.31 | 0.07 | 0.29 | 0.81 | 0.37 | 0.09 | 0.34 | −0.03 | 0.20 | 0.75 | 0.18 |
| p-value | 0.86 | 0.01 | 0.59 | 0.02 | <0.001 | 0.003 | 0.50 | 0.008 | 0.85 | 0.13 | <0.001 | 0.17 |
|
| ||||||||||||
|
External validity, Yule’s Q coefficient
|
||||||||||||
| FIMA1 | FIMA2 | FIMA3 | FIMA4 | FIMA5 | FIMA7 | FIMA8 | FIMA9 | FIMA10 | FIMA11 | FIMA12 | FIMA14 | |
|
| ||||||||||||
| T1 EQ1 (mobility) | −0.50 | 0.37 | 0.51 | 1 | 0.86 | 1 | −0.18 | 0.49 | −0.30 | −0.32 | 0.61 | 0.30 |
| T1 EQ2 (self-care) | 1 | −0.42 | 0.81 | 1 | 0.87 | 0.63 | 0.33 | 1 | −0.52 | −0.11 | 0.26 | 1 |
| T1 EQ3 (usual activities) | −1 | 0.18 | 0.56 | 1 | 0.69 | 1 | −0.22 | −0.02 | −0.35 | −0.35 | 0.23 | 0.33 |
| T1 EQ4 (pain/discomfort) | −1 | −0.21 | 1 | 1 | 0.53 | −0.76 | 0.18 | −1 | 0.20 | −0.82 | −0.59 | −1 |
| T1 EQ5 (anxiety/depression) | −0.52 | 0.16 | 1 | 1 | 0.50 | 0.52 | 0.14 | −0.12 | −0.19 | −0.25 | −0.11 | 0.24 |
| T2 EQ1 (mobility) | −1 | 0.37 | 0.51 | 1 | 0.86 | 1 | −0.18 | 0.49 | −0.30 | −0.32 | 0.61 | 0.30 |
| T2 EQ2 (self-care) | 1 | −0.42 | 0.81 | 1 | 0.87 | 0.63 | 0.33 | 1 | −0.52 | −0.11 | 0.26 | 1 |
| T2 EQ3 (usual activities) | −1 | 0.18 | 0.56 | 1 | 0.69 | 1 | −0.22 | −0.01 | −0.35 | −0.35 | 0.23 | 0.33 |
| T2 EQ4 (pain/discomfort) | −1 | −0.21 | 1 | 1 | 0.54 | −0.76 | 0.18 | −1 | 0.20 | −0.82 | −0.59 | −1 |
| T2 EQ5 (anxiety/depression) | 1 | 0.16 | 1 | 1 | 0.50 | 0.53 | 0.14 | −0.12 | −0.19 | −0.25 | −0.11 | 0.24 |
Notes: T1, participant evaluation within 48 hours of admission; T2, participant evaluation 2 weeks after admission.
Abbreviations: EQ, EuroQol; FIMA, Fragebogen zur Inanspruchnahme medizinischer und nicht-medizinischer Versorgungsleistungen im Alter [Questionnaire for Health-Related Resource Use in an Elderly Population].
The Polish pilot study of the FIMA
The usage data on the respective resource categories is listed in Table 6. The most frequent health-related resource uses were as follows: appointments with the GP (90.2%) and orthopedist (54.1%), medication (93.4%), and necessity to have an optical aid as supportive equipment (70.5%). It is notable that the mean number of drugs taken daily among the surveyed seniors amounted to as many as 6.2.
Table 6.
Use of the FIMA resource categories at T1
| Resource categories | Positive results
|
All patients
|
||||
|---|---|---|---|---|---|---|
| n | Mean | SD | % | Mean | SD | |
| FIMA1 | ||||||
| Ambulatory appointments with a physician (3 months) | ||||||
| GP | 55 | 2.44 | 1.26 | 90.2 | 2.20 | 1.40 |
| Internist | 19 | 1.90 | 1.24 | 31.1 | 0.59 | 1.12 |
| Gynecologist | 24 | 1 | 0 | 39.3 | 0.39 | 0.49 |
| Surgeon | 10 | 1.50 | 0.71 | 16.4 | 0.25 | 0.62 |
| Orthopedist | 33 | 1.42 | 0.71 | 54.1 | 0.77 | 0.88 |
| Neurologist | 13 | 1.31 | 0.48 | 21.3 | 0.28 | 0.58 |
| Dermatologist | 5 | 1.60 | 0.89 | 8.2 | 0.13 | 0.50 |
| Ophthalmologist | 19 | 1.47 | 1.17 | 31.1 | 0.46 | 0.94 |
| Urologist | 1 | 1 | – | 1.6 | 0.02 | 0.13 |
| Dentist | 10 | 1.90 | 1.52 | 16.4 | 0.31 | 0.92 |
| Psychologist | 3 | 1.67 | 1.16 | 4.9 | 0.08 | 0.42 |
| Stay at accident and emergency department | 8 | 1.25 | 0.46 | 13.1 | 0.16 | 0.45 |
| Any other specialist | 1 | 1 | – | 1.6 | 0.02 | 0.13 |
| FIMA2 | ||||||
| Ambulatory appointments with therapists (3 months) | ||||||
| Physiotherapist | 17 | 7.94 | 5.48 | 27.9 | 2.21 | 4.57 |
| Ergotherapist | 1 | 1 | – | 1.6 | 0.02 | 0.13 |
| Medical pedicure | 2 | 1 | 0 | 3.3 | 0.03 | 0.18 |
| FIMA3 | ||||||
| Help of a community nurse/social worker (3 months, average number of visits per month) | 3 | 3.83 | 5.35 | 4.9 | 0.19 | 1.29 |
| FIMA4 | ||||||
| Use of paid care services (3 months, average number of visits per month) | 1 | 30 | – | 1.6 | 0.49 | 3.84 |
| FIMA5 | ||||||
| Use of informal help (3 months, average number of visits per month) | 23 | 21.30 | 11.00 | 37.7 | 8.03 | 12.36 |
| FIMA6 | ||||||
| Use of day residential care (3 months, average number of days) | 0 | – | – | 0.0 | 0 | 0 |
| FIMA7 | ||||||
| Use of short-term care (3 months, average number of days) | 2 | 21.5 | 12.02 | 3.3 | 0.71 | 4.16 |
| FIMA8 | ||||||
| Use of care benefits (type of benefits), in Polish zlotys (PLN) per month | 10 | 294.7 | 216.89 | 16.4 | 48.31 | 138.41 |
| FIMA9 | ||||||
| Number of drugs taken | 57 | 6.2 | 3.30 | 93.4 | 5.77 | 3.52 |
| FIMA10 | ||||||
| Use of stationary rehabilitation (12 months, average number of days/year) | 28 | 18.89 | 8.91 | 45.9 | 8.67 | 11.22 |
| FIMA11 | ||||||
| Undergone ambulatory operations (12 months, average number of operations) | 6 | 1.5 | 0.84 | 9.8 | 0.15 | 0.51 |
| FIMA12 | ||||||
| Stationary stays at hospital wards (12 months, average number of stays/days) | 29 | 1.45/10.86 | 0.7361/6.00 | 47.5 | 0.69/5.16 | 0.89/6.83 |
| FIMA13 | ||||||
| Stationary stays at the psychiatric ward (12 months, average number of stays/days) | 0 | – | – | 0.0 | – | – |
| FIMA14 | ||||||
| Auxiliary equipment | ||||||
| Rotator | 10 | 1.80 | 0.42 | 16.4 | 0.30 | 0.69 |
| Wheelchair | 2 | 2 | 0 | 3.3 | 0.07 | 0.36 |
| Crutches | 24 | 1.50 | 0.51 | 39.3 | 0.59 | 0.80 |
| Bath seat | 6 | 1.33 | 0.52 | 9.8 | 0.13 | 0.43 |
| Glasses | 43 | 1.05 | 0.21 | 70.5 | 0.74 | 0.51 |
| Hearing device | 7 | 1 | 0 | 11.5 | 0.12 | 0.32 |
| Dental prosthesis | 43 | 1.09 | 0.29 | 70.5 | 0.77 | 0.56 |
| Breathing apparatus | 0 | – | – | 0.0 | 0 | 0 |
| Compression stockings | 3 | 1.33 | 0.58 | 4.9 | 0.07 | 0.31 |
| Hygiene pads | 10 | 1 | 0 | 16.4 | 0.16 | 0.37 |
| Others | 6 | 1.33 | 0.52 | 9.8 | 0.13 | 0.43 |
| FIMA15 | ||||||
| Form of residence (12 months) | ||||||
| Private household | 61 | – | – | 100 | – | – |
| Shelter flat | 0 | – | – | 0 | – | – |
| Residential care | 0 | – | – | 0 | – | – |
| Others | 0 | – | – | 0 | – | – |
| FIMA16 | ||||||
| Relocations (12 months) | ||||||
| No | 61 | – | – | 100 | – | – |
| FIMA17 | ||||||
| Health insurance | ||||||
| Yes | 61 | – | – | 100 | – | – |
Note: T1 indicates the participant evaluation within 48 hours of admission.
Abbreviations: FIMA, Fragebogen zur Inanspruchnahme medizinischer und nicht-medizinischer Versorgungsleistungen im Alter [Questionnaire for Health-Related Resource Use in an Elderly Population]; GP, general practitioner.
Discussion
This study aimed to assess the psychometric properties of the FIMA questionnaire, using a sample of Polish elderly people. To our knowledge, no other validated instruments are available in Poland to assess patients’ demand for medical and nonmedical services. This study demonstrated that the Polish version of the FIMA has high theoretical and external validation. The answers to particular FIMA questions are characterized by very good or good test–retest reliability. The result of the test–retest reliability with a 2-week interval was outstanding for the majority of the studied questions (100% compliance), whereas for two of them (FIMA1 – physician, and FIMA10 – stationary rehabilitation), the result was satisfactory.
FIMA was understood by most respondents in the selected population (mean time taken to complete it was 15.6 minutes) and had a reading and comprehension level that was appropriate for most respondents, even those with a low education level. The vast majority, 93.4% of participants, completed the questionnaire alone, and 90.2% rated the difficulty level as easy to very easy. Similar results are shown in the original German FIMA version: the questionnaire took an average of 21 minutes to complete, three-quarters of respondents completed it without any help, and 90% rated the difficulty level as easy or even very simple.8
The regression analysis did not give any valuable information because some FIMA answers were often highly prevalent. The extent of particular FIMA responses turned out to be too small, so there were no sufficient data for the opposite answers. The authors are considering using sums for future analysis for some FIMA questions (eg, FIMA1 – physician). It is worth wondering whether the FIMA questions in the current form are not too general. The authors also suggest that a study should be conducted on a larger number of elderly people.
In order to assess the external validation of the test, a comparison of the results of the FIMA questionnaire with the instrument of acknowledged validity for testing the EQ-5D-3L quality of life was made, after which their common variance was calculated. Individual items of the four FIMA questions (FIMA1 – physician, FIMA3 – community nurse/social worker, FIMA4 – paid care service, FIMA5 – informal help, and FIMA7 – short-term care) had Yule’s Q coefficients >0.5, which means that these questions have high levels of external validation. Similar results were obtained by Seidl et al8 in a pilot study of the original FIMA version, where good agreement between self-reported health-related quality of life and the use of nursing and home care resources were indicated (FIMA3 – community nurse/social worker; and FIMA5 – informal help; phi coefficient values: between 0.52 and 0.58). However, one should take into consideration certain limitations, which are the consequence of the assessment of the validity of the FIMA questionnaire with reference to the EQ-5D-3L scale. Not each of the domains described with the use of EQ-5D-3L will be reflected in particular areas of services that are studied with the FIMA. This fact is especially important in the case of formulation of hypotheses related to theoretical foundations as far as potential relationships between particular EQ-5D-3L domains and FIMA areas are concerned. Therefore, it is difficult to unambiguously assess whether the remaining areas studied by FIMA, ie, those which according to the statistical analysis obtained low levels, eg, the ambulatory appointments with therapists that patients avail themselves of (FIMA2) and use of care benefits (FIMA8), are characterized by poor external validation.
This study does have some limitations. The foremost weakness of the study is a relatively small sample size, which, given the questionnaire structure, may produce unreliable results concerning the studied reliability in the FIMA validation process. Moreover, the questionnaire was administered in a rehabilitation ward. It is possible that administering the FIMA under different conditions or in other regions in Poland (eg, eastern and western contexts regarding attitudes toward aging and care of elderly people) would have yielded different results. Thus, there is a need for further research with the use of this instrument on a larger and more heterogeneous population of older people.
In addition, there was no standard FIMA instrument with which to estimate concurrent validity. A certain weakness of the presented work may be the lack of recognized instruments that assess the demand for medical and nonmedical services among the elderly and the lack of a possibility to refer the presented results to the validation results of other language versions of FIMA.
This study is a starting point for other researchers to use the FIMA and to compare the results obtained between various subpopulations of elderly people in Poland.
Conclusion
There is currently no other instrument in Poland which would make it possible to identify the demand for medical and nonmedical services among the elderly. Findings of this study indicate that the FIMA questionnaire is a good self-reporting measure and could be used without the presence of an interviewer (ie, online surveys).
The use of this instrument by gerontologists, nurses, caregivers, health-care educators, politicians, and researchers could improve their knowledge and understanding of the demand for medical and nonmedical services among the elderly, which could result in enhanced patient satisfaction with their care.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Christensen K, Doblhammer G, Rau R, Vaupel JW. Aging populations: the challenges ahead. Lancet. 2009;374(9696):1196–1208. doi: 10.1016/S0140-6736(09)61460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knickman JR, Snell EK. The 2030 problem: caring for aging baby boomers. Health Serv Res. 2002;37(4):849–884. doi: 10.1034/j.1600-0560.2002.56.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dallmeyer S, Wicker P, Breuer C. How an aging society affects the economic costs of inactivity in Germany: empirical evidence and projections. Eur Rev Aging Phys Act. 2017;14:18. doi: 10.1186/s11556-017-0187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ridyard CH, Hughes DA. Methods for the collection of resource use data within clinical trials: a systematic review of studies funded by the UK Health Technology Assessment program. Value Health. 2010;13(8):867–872. doi: 10.1111/j.1524-4733.2010.00788.x. [DOI] [PubMed] [Google Scholar]
- 5.Bankhead CR, Bukach C, Webster P, Stewart-Brown S, Munafo M, Austoker J, webpage on the Internet . IHR Health Technology Assessment Programme: Executive Summaries. Southampton, UK: IHR Journals Library; 2003. [Accessed March 24, 2018]. The impact of screening on future health-promoting behaviours and health beliefs: a systematic review. Available from: https://www.ncbi.nlm.nih.gov/books/NBK62283/ [DOI] [PubMed] [Google Scholar]
- 6.Saczyński JS, McManus DD, Goldberg RJ. Commonly utilized data collection approaches in clinical research. Am J Med. 2013;126(11):946–950. doi: 10.1016/j.amjmed.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Petrou S, Gray A. Economic evaluation alongside randomised controlled trials: design, conduct, analysis, and reporting. BMJ. 2011;342:d1548. doi: 10.1136/bmj.d1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seidl H, Bowles D, Bock J-O, et al. FIMA – Fragebogen zur Erhebung von Gesundheitsleistungen im Alter: Entwicklung und Pilotstudie. Das Gesundheitswes. 2015;77(1):46–52. doi: 10.1055/s-0034-1372618. [DOI] [PubMed] [Google Scholar]
- 9.Szende A, Janssen B, Cabases J. Self-Reported Population Health: An International Perspective Based on EQ-5D. Dordrecht, Heidelberg, New York, London: SpringerOpen; 2014. [PubMed] [Google Scholar]
- 10.Wild D, Grove A, Martin M, et al. ISPOR Task Force for Translation and Cultural Adaptation Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005;8(2):94–104. doi: 10.1111/j.1524-4733.2005.04054.x. [DOI] [PubMed] [Google Scholar]
- 11.R Core Team . R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 12.Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–290. [Google Scholar]
- 13.Warrens MJ. On association coefficients for 2×2 tables and properties that do not depend on the marginal distributions. Psychometrika. 2008;73(4):777–789. doi: 10.1007/s11336-008-9070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]