Abstract
Background
Autoimmune subepidermal bullous dermatoses have similar clinical features to those of a spectrum of immune reactants at the dermoepidermal junction (DEJ). It is difficult to obtain a precise diagnosis without an immunofluorescence assay because of their similar clinical presentations. The aim of this study was to describe the cellular cutaneous infiltration among autoimmune subepidermal bullous dermatoses.
Materials and methods
This retrospective analysis was conducted at a hospital in Riyadh, Saudi Arabia using biopsy-based data collected from 65 patients.
Results
Spongiotic changes, neutrophils, and lymphocyte infiltrations in the epidermis differed among the subepidermal bullous diseases. The DEJ showed a difference in the extent of neutrophil infiltration. The dermis showed differences in perivascular lymphocytic infiltration, neutrophilic infiltration, eosinophilic infiltration, and dermal edema.
Conclusion
The dermal and DEJ showed most of the histopathologic changes in subepidermal autoimmune bullous dermatoses.
Keywords: bullous pemphigoid, dermatitis herpetiformis, Saudi Arabia, subepidermal autoimmune bullous disorders, pemphigoid gestationis
Introduction
Autoimmune subepidermal bullous diseases are a heterogeneous group of disorders. They encompass many specific disorders, including the bullous pemphigoid (BP), pemphigoid gestationis (PG), linear IgA bullous dermatosis (LAD), dermatitis herpetiformis (DH), epidermolysis bullosa acquisita (EBA), bullous lupus erythematosus (BLE), lichen planus pemphigoides (LPP), and bullous vasculitis (BV).
Immunofluorescence techniques, direct and indirect, and enzyme-linked immunosorbent assay have a crucial role in diagnosis, but determining the types of inflammatory cell infiltrate is still of great value for differentiating between these disorders.1 Numerous inflammatory cells (neutrophils, eosinophils, lymphocytes, and plasma cells) have been identified in the upper dermis of patients with these disorders.2–5 We performed a detailed histopathologic study of a series of patients with these diseases to identify certain histopathologic features that might help to describe them.
Materials and methods
We conducted a retrospective study using biopsy-based data collected at a hospital in Riyadh, Saudi Arabia. This study was approved by the Institutional Ethical Review Board, College of Medicine, King Saud University. Patients’ consent to review their medical records was not required by the Institutional Review Board due to being retrospective in nature and related to histopathology. We assured the confidentiality of all patients.
We utilized histopathologic laboratory reports to identify all patients diagnosed with subepidermal bulbous dermatosis. We examined all biopsies collected between 1997 and 2016 (65 cases). All cases were examined by the dermatology clinic, and histopathologic findings and direct immunofluorescence assays were performed. All the original pathology reports were reviewed and evaluated by a dermatopathologist.
A histopathologic analysis of the biopsies was carried out based on the epidermal, subepidermal, and dermal changes. The presence or absence of acanthosis, para-keratosis, spongiosis, and dermal edema was noted. We also identified the presence of inflammatory cells, including lymphocytes, plasma cells, histiocytes, neutrophils, eosinophils, fibrin, and mast cells. Data were collected and stored in a spreadsheet using Microsoft Excel 2010®. Data management and coding were also performed in Excel. The data were analyzed using SPSS® version 21.0 (IBM Corporation, Armonk, NY, USA). A descriptive analysis was performed using categorical variables presented in the form of frequencies and percentages.
Results
A total of 65 cases of autoimmune subepidermal bullous diseases were diagnosed based on the histopathologic features and direct immunofluorescence assay on skin biopsies. The most common cause was BP (38%), followed by PG (34%), LAD (6%), BLE (6%), EBA (6%), DH (5%), LPP (3%), and BV (2%). The histopathologic features of the different diseases are enumerated and shown in Tables 1–3 and Figures 1–7, respectively.
Table 1.
Epidermal changes observed for the different diagnoses
| Characteristics | BP (n=25), n (%) | PG (n=22), n (%) | LAD (n=4), n (%) | BLE (n=4), n (%) | EBA (n=4), n (%) | DH (n=3), n (%) | LPP (n=2), n (%) | BV (n=1), n (%) |
|---|---|---|---|---|---|---|---|---|
| Acanthosis | ||||||||
| Positive (n=5) | 3 (12.0) | 1 (4.5) | 0 (0.0) | 0 (0.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Negative (n=60) | 22 (88.0) | 21 (95.5) | 4 (100) | 4 (100) | 3 (75.0) | 3 (100) | 2 (100) | 1 (100) |
| Parakeratosis | ||||||||
| Positive (n=8) | 2 (8.0) | 5 (22.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (33.3) | 0 (0.0) | 0 (0.0) |
| Negative (n=57) | 23 (92.0) | 17 (77.3) | 4 (100) | 4 (100) | 4 (100) | 2 (66.7) | 2 (100) | 1 (100) |
| Spongiosis | ||||||||
| Positive (n=24) | 5 (20.0) | 16 (72.7) | 0 (0.0) | 1 (25.0) | 0 (0.0) | 2 (66.7) | 0 (0.0) | 0 (0.0) |
| Negative (n=41) | 20 (80.0) | 6 (27.3) | 4 (100) | 3 (75.0) | 4 (100) | 1 (33.3) | 2 (100) | 1 (100) |
| Eosinophils | ||||||||
| Positive (n=7) | 2 (8.0) | 5 (22.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Negative (n=58) | 23 (92.0) | 17 (77.3) | 4 (100) | 4 (100) | 4 (100) | 3 (100) | 2 (100) | 1 (100) |
| Neutrophils | ||||||||
| Positive (n=2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (25.0) | 0 (0.0) | 1 (33.3) | 0 (0.0) | 0 (0.0) |
| Negative (n=63) | 25 (100) | 22 (100) | 4 (100) | 3 (75.0) | 4 (100) | 2 (66.7) | 2 (100) | 1 (100) |
| Lymphocytes | ||||||||
| Positive (n=1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Negative (n=64) | 25 (100) | 22 (100) | 4 (100) | 3 (75.0) | 4 (100) | 3 (100) | 2 (100) | 1 (100) |
Abbreviations: BLE, bullous lupus erythematosus; BP, bullous pemphigoid; BV, bullous vasculitis; DH, dermatitis herpetiformis; EBA, epidermolysis bullosa acquisita; LAD, linear IgA bullous dermatosis; LPP, lichen planus pemphigoides; PG, pemphigoid gestationis.
Table 2.
Dermo-epidermal junction alterations observed for the different diagnoses
| Characteristics | BP (n=25), n (%) | PG (n=22), n (%) | LAD (n=4), n (%) | BLE (n=4), n (%) | EBA (n=4), n (%) | DH (n=3), n (%) | LPP (n=2), n (%) | BV (n=1), n (%) |
|---|---|---|---|---|---|---|---|---|
| Eosinophils | ||||||||
| Positive (n=26) | 10 (40.0) | 12 (54.5) | 2(50.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 0 (0.0) |
| Negative (n=39) | 15 (60.0) | 10 (45.5) | 2(50.0) | 3 (75.0) | 4 (100) | 3 (100) | 1 (50.0) | 1 (100) |
| Neutrophils | ||||||||
| Positive (n=16) | 4 (16.0) | 0 (0.0) | 4 (100) | 2 (50.0) | 4 (100) | 1 (33.3) | 0 (0.0) | 1 (100) |
| Negative (n=49) | 21 (84.0) | 22 (100) | 0 (0.0) | 2 (50.0) | 0 (0.0) | 2 (66.7) | 2 (100) | 0 (0.0) |
| Lymphocytes | ||||||||
| Positive (n=3) | 2 (8.0) | 0 (0.0) | 0 (0.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Negative (n=62) | 23 (92.0) | 22 (100) | 4 (100) | 3 (75.0) | 4 (100) | 3 (100) | 2 (100) | 1 (100) |
| Fibrin | ||||||||
| Positive (n=6) | 3 (12.0) | 0 (0.0) | 0 (0.0) | 1 (25.0) | 1 (25.0) | 0 (0.0) | 1 (50.0) | 0 (0.0) |
| Negative (n=59) | 22 (88.0) | 22 (100) | 4 (100) | 3 (75.0) | 3 (75.0) | 3 (100) | 1 (50.0) | 1 (100) |
Abbreviations: BLE, bullous lupus erythematosus; BP, bullous pemphigoid; BV, bullous vasculitis; DH, dermatitis herpetiformis; EBA, epidermolysis bullosa acquisita; LAD, linear IgA bullous dermatosis; LPP, lichen planus pemphigoides; PG, pemphigoid gestationis.
Table 3.
A comparison of the dermal changes among the different diagnoses
| Characteristics | BP (n=25), n (%) | PG (n=22), n (%) | LAD (n=4), n (%) | BLE (n=4), n (%) | EBA (n=4), n (%) | DH (n=3), n (%) | LPP (n=2), n (%) | BV (n=1), n (%) |
|---|---|---|---|---|---|---|---|---|
| Perivascular lymphocytes | ||||||||
| Positive (n=40) | 8 (32.0) | 22 (100) | 2 (50.0) | 1 (25.0) | 3 (75.0) | 2 (66.7) | 2 (100) | 0 (0.0) |
| Negative (n=25) | 17 (68.0) | 0 (0.0) | 2 (50.0) | 3 (75.0) | 1 (25.0) | 1 (33.3) | 0 (0.0) | 1 (100) |
| Plasma cells | ||||||||
| Positive (n=4) | 2 (8.0) | 1 (4.5) | 1 (25.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Negative (n=61) | 23 (92.0) | 21 (95.5) | 3 (75.0) | 4 (100) | 4 (100) | 3 (100) | 2 (100) | 1 (100) |
| Histiocytes | ||||||||
| Positive (n=14) | 3 (12.0) | 8 (36.4) | 1 (25.0) | 0 (0.0) | 2 (50.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Negative (n=51) | 22 (88.0) | 14 (63.6) | 3 (75.0) | 4 (100) | 2 (50.0) | 3 (100) | 2 (100) | 1 (100) |
| Mast cells | ||||||||
| Positive (n=3) | 0 (0.0) | 3 (13.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Negative (n=19) | 25 (100) | 19 (86.4) | 4 (100) | 4 (100) | 4 (100) | 3 (100) | 2 (100) | 1 (100) |
| Neutrophils | ||||||||
| Positive (n=24) | 3 (12.0) | 6 (27.3) | 4 (100) | 4 (100) | 3 (75.0) | 3 (100) | 0 (0.0) | 1 (100) |
| Negative (n=41) | 22 (88.0) | 16 (72.7) | 0 (0.0) | 0 (0.0) | 1 (25.0) | 0 (0.0) | 2 (100) | 0 (0.0) |
| Eosinophils | ||||||||
| Positive (n=51) | 20 (80.0) | 21 (95.5) | 2 (50.0) | 1 (25.0) | 3 (75.0) | 2 (66.7) | 2 (100) | 0 (0.0) |
| Negative (n=14) | 5 (20.0) | 1 (4.5) | 2 (50.0) | 3 (75.0) | 1 (25.0) | 1 (33.3) | 0 (0.0) | 1 (100) |
| Dermal edema | ||||||||
| Positive (n=35) | 7 (28.0) | 22 (100) | 4 (100) | 2 (50.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Negative (n=30) | 18 (72.0) | 0 (0.0) | 0 (0.0) | 2 (50.0) | 4 (100) | 3 (100) | 2 (100) | 1 (100) |
Abbreviations: BLE, bullous lupus erythematosus; BP, bullous pemphigoid; BV, bullous vasculitis; DH, dermatitis herpetiformis; EBA, epidermolysis bullosa acquisita; LAD, linear IgA bullous dermatosis; LPP, lichen planus pemphigoides; PG, pemphigoid gestationis.
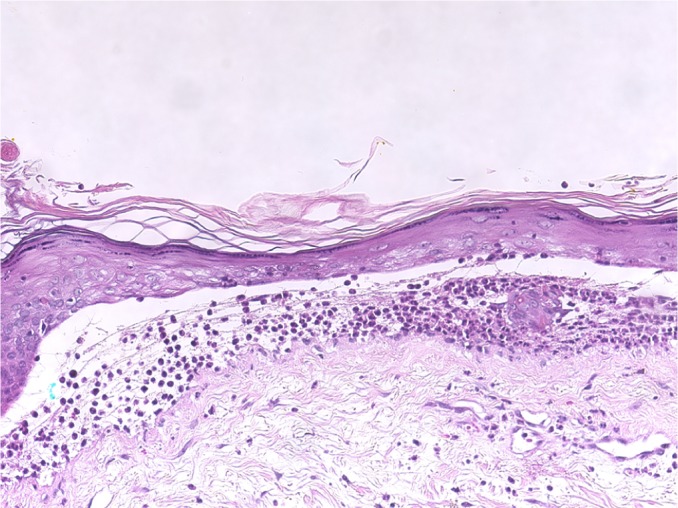
Figure 1.
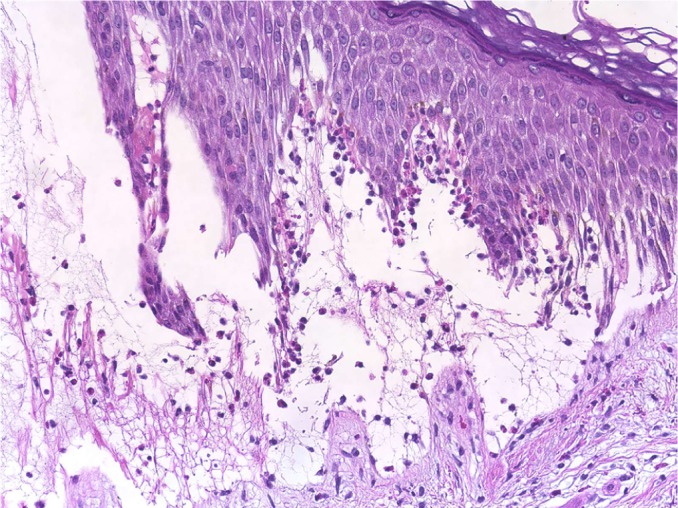
Bullous pemphigoid.
Note: Subepidermal blister with an accumulation of eosinophils consistent with bullous pemphigoid (H/E stain, original magnification 200×).
Abbreviation: H/E, Haemotoxylin and Eosin.
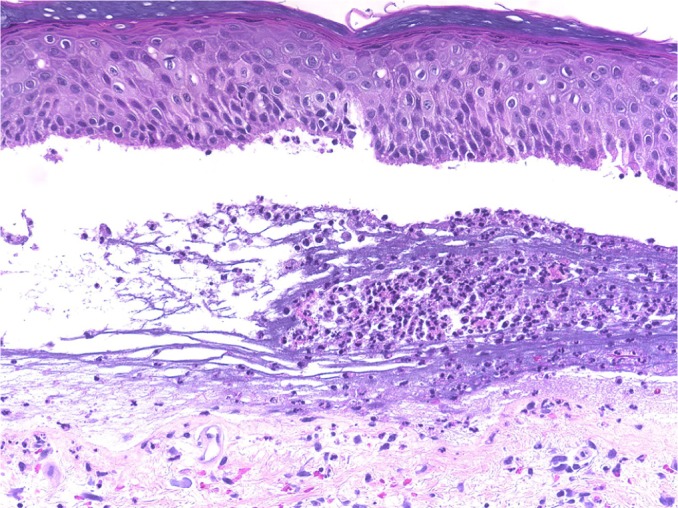
Figure 2.
Linear IgA bullous dermatosis.
Notes: Subepidermal cleft formation with neutrophils combatable with linear IgA bullous dermatosis (H/E stain, original magnification 400×).
Abbreviation: H/E, Haemotoxylin and Eosin.
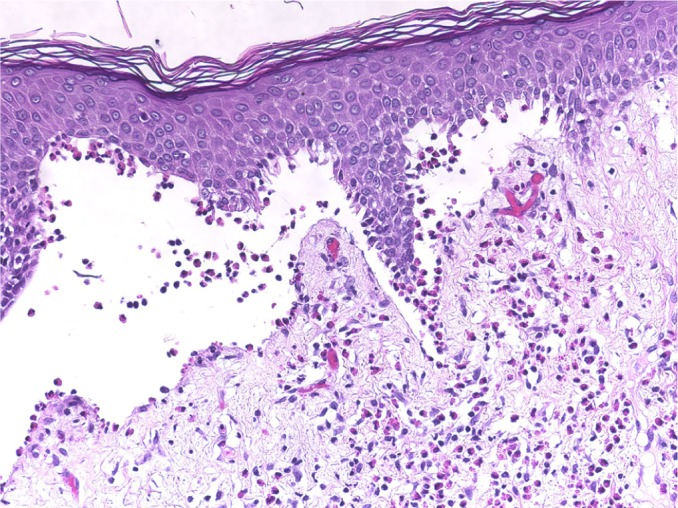
Figure 3.
Bullous vasculitis.
Notes: Neutrophilic infiltration of the small dermal blood vessels coupled with karyorrhexis and fibrinoid necrosis. A subepidermal cleft containing neutrophils is also noted (H/E stain, original magnification 200×).
Abbreviation: H/E, Haemotoxylin and Eosin.
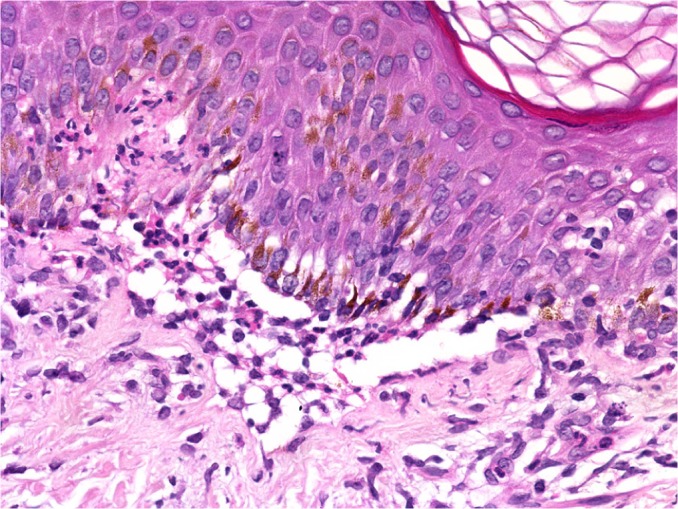
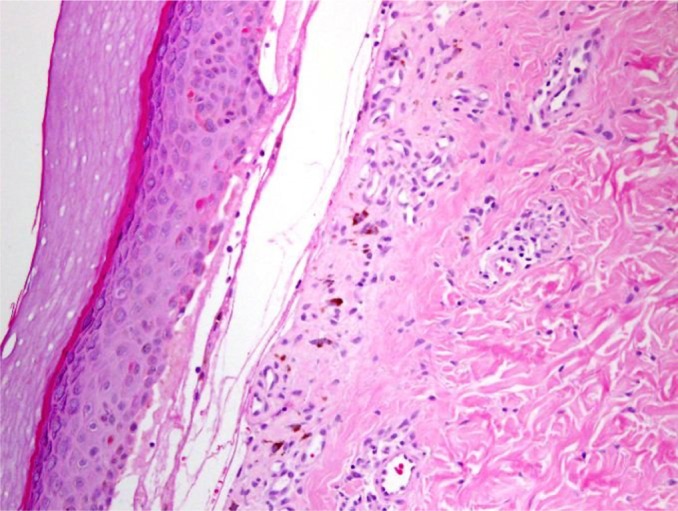
Figure 4.
Dermatitis herpetiformis.
Note: Subepidermal small cleft formation with a collection of neutrophils and eosinophils in the papillary dermis characteristic of dermatitis herpetiformis (H/E stain, original magnification 200×).
Abbreviation: H/E, Haemotoxylin and Eosin.
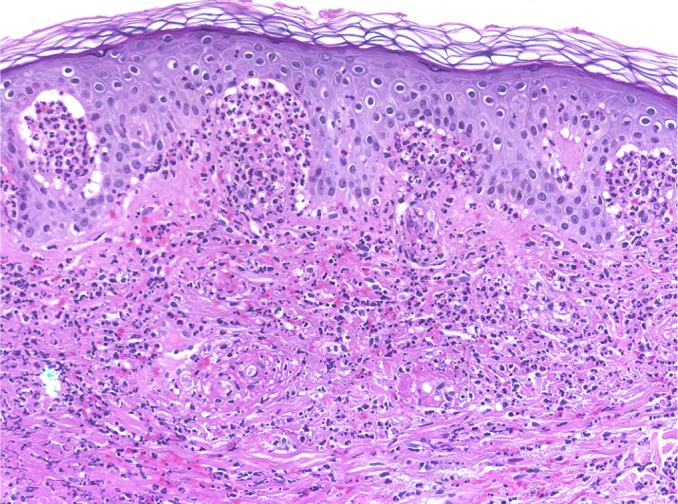
Figure 5.
Bullous lupus erythematosus.
Note: A subepidermal blister with neutrophils consistent with acute lupus erythematosus (H/E stain, original magnification 200×).
Abbreviation: H/E, Haemotoxylin and Eosin.
Figure 6.
Epidermolysis bullosa acquisita.
Note: A subepidermal blister with neutrophils similar to those found in acute lupus erythematosus (H/E stain, original magnification 200×).
Abbreviation: H/E, Haemotoxylin and Eosin.
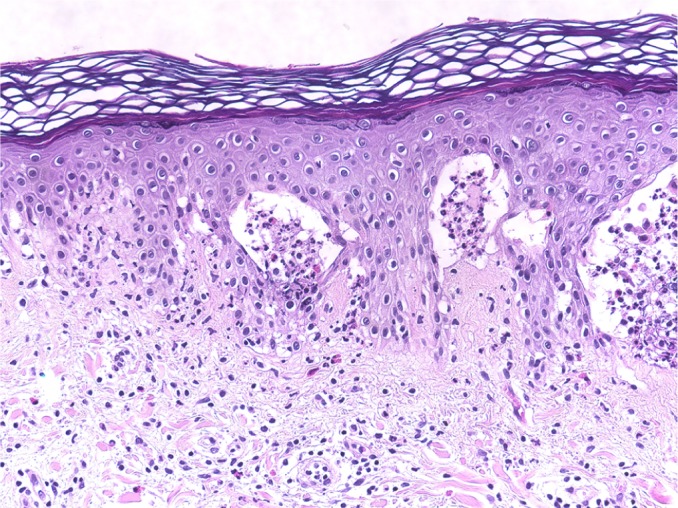
Figure 7.
Pemphigoid gestationis.
Note: A subepidermal blister with many dermal eosinophils consistent with pemphigoid gestationis (H/E stain, original magnification 200×).
Abbreviation: H/E, Haemotoxylin and Eosin.
The frequencies of each histopathologic finding were investigated for all types of autoimmune subepidermal bullous diseases. Overall, the most significant histopathologic changes were found in the dermal and dermoepidermal junction (DEJ).
Table 1 lists the epidermal changes. Acanthosis was more evident in BP and EBA (12.0% and 25.0% of cases, respectively), and parakeratosis was observed in BP, PG, and DH (8.0% 22.7%, and 33.3%, respectively). Epidermal spongiosis was significantly present in both PG and DH (72.0% and 66.7%, respectively). No significant epidermal inflammatory cell infiltration apart from eosinophilic infiltration (eosinophilic spongiosis) in BP and PG (8.0% and 22.7%, respectively) and neutrophil and lymphocyte infiltration in BLE (25.0%) was noted.
Table 2 lists the changes at the DEJ. The LAD, EBA, and BV contained significantly higher levels of neutrophil infiltration of nearly 100%, and 50.0% of BLE had neutrophils tagging the DEJ. Only 16.0% of BP had neutrophil infiltration along the DEJ. On the other hand, eosinophils significantly tagged the DEJ in BP, PG, LAD, and LPP (40.0%, 54.5%, 50.0%, and 50.0%, respectively). These results support the theory that these cells play a major role in the pathogenesis of bulla formation. No significant lymphocytic infiltrations along the DEJ were noted compared with other inflammatory cells. Fibrin was deposited in bullous dermatosis, which has the tendency to form scar-like BLE or EBA.
Table 3 lists the dermal changes. Perivascular lymphocytic infiltrates were significantly found in PG (100%), LPP (100%), EBA (75%), DH (66.7%), LAD (50.0%), BP (32%), and BLE (25%). A significant number of neutrophils were positively correlated with LAD (100%), BLE (100%), EBA (75%), DH (100%), and BV (100%). Eosinophils were highly infiltrated in BP (80%), PG (95.5%), EBA (75%), DH (66.7%), and LPP (100%), but they were present in only 50% of the LAD cases. However, they were less frequently observed in BLE or not found in BV. Dermal edema correlated significantly with PG (100%), LAD (100%), and BLE (50%); only 28% of BP had dermal edema. Plasma cells, histiocytes, and mast cells did not exhibit any significant differences.
Discussion
The diagnosis of subepidermal autoimmune bullous dermatoses is complex, and there is considerable clinical and histologic overlap between these diseases that necessitates more complicated assays to reach a definite diagnosis.6–8 At present, the diagnosis of autoimmune bullous disorders is based on immunologic and molecular findings rather than a clinical- or histopathologic-based diagnosis alone. Indirect immunofluorescence, immunoblotting, and immune electron microscopy may have great value in such diagnoses, but these technologies are available only in advanced research laboratories.8,9
In this study, 72% of the patients were in the pemphigoid group, which was consistent with the findings of international studies.10 Although it is difficult to give a precise estimate of the disease incidence of other subepidermal autoimmune bullous dermatoses because of their rarity, an annual incidence rate ranging from 0.26 to 0.67 cases per million people per year has been reported for LAD, BLE, and EBA.11–14 The incidence of DH ranges from 11.5 to 39.2 cases per 100,000 people.15,16 Bullous lesions are very rare in vasculitis, and they reflect the severity of inflammation.17,18 In Henoch–Schönlein purpura, the incidence of bullous lesions among patients was roughly 19%.19 As in other studies, our data indicated how rare these diseases are; their prevalence in our study ranged between 2% and 6%.
All subepidermal autoimmune bullous dermatoses exhibit nonspecific histopathologic changes in the epidermis. Epidermal changes in PG are not rare. A recent study showed increased Toll-like receptor 4 expression in the basal and suprabasal layers of BP lesions,20 and thickening of the epidermis and hyperkeratosis have been described in a BP model.21 The epidermis displays edema and focal eosinophilic spongiosis in PG.22 In our study, we found statistically significant eosinophilic spongiosis changes in 72.7% of the cases of PG; such changes were observed in only 20.0% of cases of BP (Table 1). Epidermal changes in LAD were rare and not statistically significant, although mild acanthosis has been reported in some cases.23 In our patients, we did not observe any significant epidermal changes (Table 1). Other studies have reported epidermal atrophy in BLE and extensive necrosis of the epidermis.24,25 We found epidermal spongiosis in 25.0% of our patients (Table 1). The histopathology of EBA depends on whether the presentation is an inflammatory or noninflammatory variant. Eosinophilic spongiosis has been reported in the inflammatory type.26 Although the epidermis of DH sometimes exhibits neutrophilic accumulation,27 the primary histopathologic changes are in the papillary dermis. LPP is characterized by the development of classical lichen planus lesions as well as tense bullae over lichenoid lesions and the de novo formation of these features in the uninvolved skin.28,29 The histopathologic features of LPP typically depend on the site of biopsy (from the bullous lesion on the top of lichenoid lesions or from the de novo bullous lesions). The epidermal changes in a bullous lesion on the top of lichenoid lesions will show features that are indistinguishable from classical lichen planus, and a de novo lesion may show eosinophilic spongiosis without features associated with lichen planus.29–33 The epidermal features of vasculitis appear to depend on the underlying disease, type, and severity of inflammatory cell infiltrations, and they may reveal variations in the extent of spongiosis, neutrophils, or eosinophils.34–36
The changes in the DEJ are the primary pathology in autoimmune subepidermal bullous diseases. The distribution and density of the inflammatory cells are very helpful for differentiating between these bullous eruptions. The separation of the DEJ in the pemphigoid groups depends on the accumulation of inflammatory cells, especially eosinophils, neutrophils, and their mediators.37,38 A linear arrangement of eosinophils and neutrophils along the DEJ is not uncommon in the pemphigoid group, especially in PG.39 We have noted a moderate-to-rich eosinophilic cell infiltration and tagging of eosinophils along the basal layer, which was observed in 54.5% and 40.0% of PG and BP patients, respectively (Table 2; Figures 1 and 7). Infiltration of neutrophils into the DEJ was noted in 16% of BP patients, 8% of whom had lymphocytes (Table 2). On the other hand, LAD is associated with a linear arrangement of neutrophils along the basal layer.39,40 We observed neutrophils at the DEJ in 100% of our patients, and these neutrophils were mixed with eosinophils in 50.0% of cases (Table 2; Figure 2). However, the presence of eosinophils may lead to a diagnostic confusion between LAD and BP.41 Primary histopathologic changes in BLE occurred in the DEJ and dermis, which included acute inflammation, interface change, intense leukocytoclastic hydropic basal degeneration, mucin deposition, and neutrophilic microabscesses at DEJ.24,42,43 Neutrophils were the dominant cellular infiltrates in the DEJ in our patients. However, lymphocytic and eosinophilic infiltrates were also present in 25% of cases (Table 2; Figure 5). The initial changes observed in EBA are around the DEJ and it is associated with neutropilic infiltration.44 One hundred percent of the specimens in our study exhibited neutrophilic infiltration around the DEJ, which was associated with fibrin deposition in 25% of these cases (Table 2; Figure 6).
The primary histopathologic changes of DH are in the papillary dermis. Piérard microabscesses are the characteristic histopathology changes in the papillary dermis, and this condition is characterized by neutrophilic accumulation. Occasionally, eosinophils occur in the early stage of DH. Furthermore, inflammatory perivascular infiltrates commonly occur, especially in the superficial and medial dermis. Late stages may show fibrin deposition, neutrophil fragments, and edema.45–49 In our study, only 33.3% of specimens exhibited neutrophils at the DEJ and the absence of eosinophils (Table 2). The changes in the DEJ in LPP may reflect the clinical types. The primary changes in a bullous lesion on the top of a lichenoid lesion are liquefactive degeneration of basal keratinocytes with a few civatte bodies. On the other hand, similar changes in the classical cases of BP typically occur in the de novo lesion.29–33 In our cases, biopsies were taken from de novo bullous lesions and showed almost normal epidermis and scattered basal cell necrotic keratinocytes (Figure 8).
Figure 8.
Lichen planus pemphigoides.
Notes: A subepidermal blister associated with orthokeratosis and scattered necrotic keratinocytes (H/E stain, original magnification 200×).
Abbreviation: H/E, Haemotoxylin and Eosin.
Cellular dermal infiltrations typically depend on the stage and severity of the lesions. Early prevesicular lesions of BP often display a significant number of eosinophils and dermal edema of the upper and middle dermis with both superficial and deep perivascular lymphohistiocytic infiltration. On the other hand, inflammatory cells, such as neutrophils, lymphocytes, and mast cells, may be present in the upper dermis of lesions.50–54 We characterized general dermal infiltration patterns in the pemphigoid group, and 80%–95% of the biopsies consistently revealed that eosinophils were the predominant dermal inflammatory infiltrate. Furthermore, nearly all of the specimens consistently exhibited perivascular lymphohistiocytic infiltration. The other inflammatory cells that were noted in the histologic specimens included neutrophils (12%–27%), plasma cells (5%–8%), and mast cells (13%, only in PG). Papillary edema was a constant feature in PG, and it occurred in 100% of the cases. In contrast, the occurrence rate was only 28% in BP cases. Cellular dermal infiltrations of LAD were mostly superficial and involved dermal infiltration by the neutrophils with papillary neutrophilic microabscesses and leukocytoclasia.40,55 Histopathology is useful for differentiating between LAD and IgA pemphigoid.56 Our patients exhibited mild neutrophilic and eosinophilic infiltration in the upper dermis, although neutrophilic infiltration was a constant feature in our patients at the DEJ. We also noted a mild perivascular lymphohistiocytic infiltration (Table 3).
Cellular dermal infiltration in BLE mostly involved constant neutrophilic infiltration, papillary edema, and papillary microabscesses. However, lymphocytic infiltration, mild dermal fibrosis, and mucin have also been reported.24–27 Our results revealed significant neutrophilic infiltrations in 100% of our patients and eosinophilic infiltrations in 25% of our patients, as well as mild dermal edema in 50% of cases (Table 3).
Cellular dermal infiltration in EBA can exhibit little inflammatory infiltration within the dermis, especially around the vessels, follicles, and in the interstitium in classical EBA. On the other end of the spectrum, rich neutrophilic infiltrations can be mixed with variable numbers of eosinophils and mononuclear cells in other types of EBA associated with variable fibrosis.44,57,58 Most of our patients had mixed inflammatory cell infiltrations, including neutrophils, eosinophils, incident histiocytes, and perivascular lymphocytic infiltrations (Table 3). The analysis of the cellular dermal infiltration of DH showed that 100% of our patients displayed the presence of neutrophils, 66.7% had eosinophils, and 66.7% had perivascular lymphocytes (Table 3; Figure 4).
Cellular dermal infiltrations in LPP correlated with the type of lesion from which the biopsy was obtained. The primary histopathologic features in a bullous lesion on the top of a lichenoid lesion were band-like lymphocytes beneath the DEJ, perivascular lymphocytic infiltrations, and scattered eosinophils. In contrast, dermal changes in de novo bullous lesions mostly exhibited dominant eosinophilic infiltrations with few perivascular lymphocytic infiltrations.29–33 All of our patients showed eosinophilic infiltrations with perivascular lymphocytic infiltrations and fibrin around the cleft (Table 3). Neutrophilic or eosinophilic infiltrations are the most common inflammatory cells associated with perivascular infiltrations, extravasated red blood cells, nuclear dust, and fibrinoid necrosis.34–36 Our patients exhibited dense neutrophilic infiltrations in the upper dermis associated with perivascular neutrophils, red blood cell extravasations, and fibrinoid necrosis.
Conclusion
The most significant histopathologic changes in subepidermal autoimmune bullous dermatoses were found in the dermal and DEJ. Eosinophil-rich infiltrates are characteristic of the pemphigoid group, and neutrophil-rich infiltrates are observed in LAD, DH, and BLE. EBA typically exhibits a cell-poor subepidermal bulla, and the inflammatory type of EBA reveals mixed neutrophilic and eosinophilic infiltrates.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Saxe N, Kahn LB. Subepidermal bullous disease. A correlated clinicopathologic study of 51 cases. J Cutan Pathol. 1976;3(2):88–94. doi: 10.1111/j.1600-0560.1976.tb00851.x. [DOI] [PubMed] [Google Scholar]
- 2.Verdolini R, Cerio R. Autoimmune subepidermal bullous skin diseases: The impact of recent findings for the dermatopathologist. Virchows Arch. 2003;443(2):184–193. doi: 10.1007/s00428-003-0776-4. [DOI] [PubMed] [Google Scholar]
- 3.Kolanko E, Bickle K, Keehn C, Glass LF. Subepidermal blistering disorders: a clinical and histopathologic review. Semin Cutan Med Surg. 2004;23(1):10–18. doi: 10.1016/s1085-5629(03)00083-x. [DOI] [PubMed] [Google Scholar]
- 4.Hussein MR, Ali FM, Omar AE. Immunohistological analysis of immune cells in blistering skin lesions. J Clin Pathol. 2007;60(1):62–71. doi: 10.1136/jcp.2006.037010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnadas MA, Gonzalez MJ, Planaguma M, et al. Clinical, histopathologic, and therapeutic aspects of subepidermal autoimmune bullous diseases with IgG on the floor of salt-split skin. Int J Dermatol. 2001;40(4):268–272. doi: 10.1046/j.1365-4362.2001.01188.x. [DOI] [PubMed] [Google Scholar]
- 6.Wojnarowska F, Venning VA. Immunobullous diseases. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook’s Textbook of Dermatology. 8th ed. Oxford: Blackwell; 2010. pp. 1–62. [Google Scholar]
- 7.Arundhathi S, Ragunatha S, Mahadeva KC. A cross-sectional study of clinical, histopathological and direct immunofluorescence spectrum of vesiculobullous disorders. J Clin Diagn Res. 2013;7(12):2788–2792. doi: 10.7860/JCDR/2013/7019.3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt E, Zillikens D. Modern diagnosis of autoimmune blistering skin diseases. Autoimmun Rev. 2010;10(2):84–89. doi: 10.1016/j.autrev.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 9.Minz RW, Chhabra S, Singh S, Radotra BD, Kumar B. Direct immunofluorescence of skin biopsy: perspective of an immunopathologist. Indian J Dermatol Venereol Leprol. 2010;76(2):150–157. doi: 10.4103/0378-6323.60561. [DOI] [PubMed] [Google Scholar]
- 10.Jain S, Basavaraj V, Vimala MG. Utility of direct immunofluorescence studies in subclassification of autoimmune subepidermal bullous diseases: A 2-year study in a tertiary care hospital. Turk Patoloji Derg. 2016;32(2):91–98. doi: 10.5146/tjpath.2015.01345. [DOI] [PubMed] [Google Scholar]
- 11.Lings K, Bygum A. Linear IgA bullous dermatosis: a retrospective study of 23 patients in Denmark. Acta Derm Venereol. 2015;95(4):466–471. doi: 10.2340/00015555-1990. [DOI] [PubMed] [Google Scholar]
- 12.Gammon WR, Briggaman RA. Bullous eruption of systemic lupus erythematosus. In: Wojnarowska F, Briggaman RA, editors. Management of Blistering Diseases. London: Chapman and Hall Ltd; 1990. pp. 263–275. [Google Scholar]
- 13.Iranzo P, Herrero-González JE, Mascaró-Galy JM, Suárez-Fernández R, España A. Epidermolysis bullosa acquisita: a retrospective analysis of 12 patients evaluated in four tertiary hospitals in Spain. Br J Dermatol. 2014;171(5):1022–1030. doi: 10.1111/bjd.13144. [DOI] [PubMed] [Google Scholar]
- 14.Woodley DT, Burgeson RE, Lunstrum G, Bruckner-Tuderman L, Reese MJ, Briggaman RA. The epidermolysis bullosa acquisita antigen is the globular carboxyl terminus of type VII procollagen. J Clin Invest. 1988;81(3):683–687. doi: 10.1172/JCI113373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mobacken H, Kastrup W, Nilsson LA. Incidence and prevalence of dermatitis herpetiformis in Sweden. Arch Derm Venereol. 1984;64(2):400–404. [PubMed] [Google Scholar]
- 16.Gawkrodger DJ, Blackwell JN, Gilmour HM, Rifkind EA, Heading RC, Barnetson RS. Dermatitis herpetiformis diagnosis, diet, and demography. Gut. 1984;25(2):151–157. doi: 10.1136/gut.25.2.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ishii Y, Takizawa T, Arakawa H, et al. Hemorrhagic bullous lesions in Henoch-Schönlein purpura. Pediatr Int. 2005;47(1):694–697. doi: 10.1111/j.1442-200x.2005.02133.x. [DOI] [PubMed] [Google Scholar]
- 18.Kobayashi T, Sakuraoka K, Iwatmoto M, Kurihara S. A case of anaphylactoid purpura with multiple blister formation: possible pathophysiological role of gelatinase (MMP-9) Dermatology. 1998;197(1):62–64. doi: 10.1159/000017959. [DOI] [PubMed] [Google Scholar]
- 19.Poterucha TJ, Wetter DA, Gibson LE, Camilleri MJ, Lohse CM. Histopathology and correlates of systemic disease in adult Henoch-Schönlein purpura: a retrospective study of microscopic and clinical findings in 68 patients at Mayo Clinic. J Am Acad Dermatol. 2013;68(3):420–424. doi: 10.1016/j.jaad.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 20.Sun XK, Chen JF, Shen H. Immunohistochemical study of toll-like receptors 2, 4, and 9 expressions in pemphigus and bullous pemphigoid lesions. Arch Dermatol Res. 2016;308(6):429–436. doi: 10.1007/s00403-016-1656-5. [DOI] [PubMed] [Google Scholar]
- 21.Hirose M, Recke A, Beckmann T, et al. Repetitive immunization breaks tolerance to type XVII collagen and leads to bullous pemphigoid in mice. J Immunol. 2011;187(3):1176–1183. doi: 10.4049/jimmunol.1100596. [DOI] [PubMed] [Google Scholar]
- 22.Shimanovich I, Bröcker EB, Zillikens D. Pemphigoid gestationis: new insights into the pathogenesis lead to novel diagnostic tools. BJOG. 2002;109(9):970–976. doi: 10.1111/j.1471-0528.2002.01016.x. [DOI] [PubMed] [Google Scholar]
- 23.Joseph TI, Sathyan P, Goma Kumar KU. Linear IgA dermatosis adult variant with oral manifestation: a rare case report. J Oral Maxillofac Pathol. 2015;19(1):83–87. doi: 10.4103/0973-029X.157207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Merklen-Djafri C, Bessis D, Frances C, et al. Blisters and loss of epidermis in patients with lupus erythematosus: a clinicopathological study of 22 patients. Medicine (Baltimore) 2015;94(46):e2102. doi: 10.1097/MD.0000000000002102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ting W, Stone MS, Racila D, Scofield RH, Sontheimer RD. Toxic epidermal necrolysis-like acute cutaneous lupus erythematosus and the spectrum of the acute syndrome of apoptotic panepidermolysis (ASAP): a case report, concept review, and proposal for new classification of lupus erythematosus vesiculobullous skin lesions. Lupus. 2004;13(12):941–950. doi: 10.1191/0961203304lu2037sa. [DOI] [PubMed] [Google Scholar]
- 26.Barreiro-Capurro A, Mascaró-Galy JM, Iranzo P. Estudio retrospectivo de las características clínicas, histológicas e inmunológicas en una serie de 9 pacientes con epidermólisis ampollosa adquirida [Retrospective study of the clinical, histologic, and immunologic features of epidermolysis bullosa acquisita in 9 patients] Actas Dermosifiliogr. 2013;104(10):904–914. doi: 10.1016/j.ad.2013.05.005. Spanish. [DOI] [PubMed] [Google Scholar]
- 27.Faure M. Dermatitis herpetiformis. Semin Dermatol. 1988;7(1):123–129. [PubMed] [Google Scholar]
- 28.Zaraa I, Mahfoudh A, Sellami MK, et al. Lichen planus pemphigoides: four new cases and a review of the literature. Int J Dermatol. 2013;52(4):406–412. doi: 10.1111/j.1365-4632.2012.05693.x. [DOI] [PubMed] [Google Scholar]
- 29.Davis AL, Bhogal BS, Whitehead P, et al. Lichen planus pemphigoides: Its relationship to bullous pemphigoid. Br J Dermatol. 1991;125(3):263–271. doi: 10.1111/j.1365-2133.1991.tb14753.x. [DOI] [PubMed] [Google Scholar]
- 30.Willesteed E, Bhogal BS, Das AK, Wojnarowska F, Black MM, McKee PH. Lichen planus pemphigoides: a clinicopathological study of nine cases. Histopathology. 1991;19(2):147–154. doi: 10.1111/j.1365-2559.1991.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 31.Ghosh A, Vora VN, Dave JN, Shah SV, Cardosco BJ. Lichen planus pemphigoides. Indian J Dermatol Venereol Leprol. 1997;63(1):68. [PubMed] [Google Scholar]
- 32.Gawkrodger DJ, Stavropoulos PG, McLaren KM, Buxton PK. Bullous lichen planus and lichen planus pemphigoides-Clinicopathological comparisons. Clin Exp Dermatol. 1989;14(2):150–153. doi: 10.1111/j.1365-2230.1989.tb00914.x. [DOI] [PubMed] [Google Scholar]
- 33.Mora RG, Nesbitt LT, Jr, Brantley JB. Lichen planus pemphigoides: Clinical and immunofluorescent findings in four cases. J Am Acad Dermatol. 1983;8(3):331–336. doi: 10.1016/s0190-9622(83)70035-6. [DOI] [PubMed] [Google Scholar]
- 34.Poterucha TJ, Wetter DA, Gibson LE, Camilleri MJ, Lohse CM. Histopathology and correlates of systemic disease in adult Henoch-Schönlein purpura: a retrospective study of microscopic and clinical findings in 68 patients at Mayo Clinic. J Am Acad Dermatol. 2013;68(3):420–424. doi: 10.1016/j.jaad.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 35.Gulati G, Siv J, Ware AE. Bullous skin lesions in an adult male: a diagnostic dilemma. Am J Case Rep. 2015;16:215–219. doi: 10.12659/AJCR.893218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ishibashi M, Kudo S, Yamamoto K, Shimai N, Chen KR. Churg-Strauss syndrome with coexistence of eosinophilic vasculitis, granulomatous phlebitis and granulomatous dermatitis in bullous pemphigoid-like blisters. J Cutan Pathol. 2011;38(3):290–294. doi: 10.1111/j.1600-0560.2010.01513.x. [DOI] [PubMed] [Google Scholar]
- 37.Borrego L, Maynard B, Peterson EA, et al. Deposition of eosinophil granule proteins precedes blister formation in bullous pemphigoid. Comparison with neutrophil and mast cell granule proteins. Am J Pathol. 1996;148(3):897–909. [PMC free article] [PubMed] [Google Scholar]
- 38.Stanley JR. Cell adhesion molecules as targets of autoantibodies in pemphigus and pemphigoid, bullous diseases due to defective epidermal cell adhesion. Adv Immunol. 1993;53:291–326. doi: 10.1016/s0065-2776(08)60503-9. [DOI] [PubMed] [Google Scholar]
- 39.Andrachuk L, Ghazarian D, Siddha S, Al Habeeb A. Linear arrangement of neutrophils along the basal layer in bullous pemphigoid: a unique histological finding. Am J Dermatopathol. 2012;34(2):192–193. doi: 10.1097/DAD.0b013e318222f951. [DOI] [PubMed] [Google Scholar]
- 40.Smith SB, Harrist TJ, Murphy GF, et al. Linear IgA bullous dermatosis v dermatitis herpetiformis. Quantitative measurements of dermoepidermal alterations. Arch Dermatol. 1984;120(3):324–328. [PubMed] [Google Scholar]
- 41.Tsai IC, Chu CY, Chen HJ, Wang LF, Chiu HC. Linear IgA bullous dermatosis: a clinical study of 16 cases at National Taiwan University Hospital. Dermatol Sinica. 2010;28(1):21–26. [Google Scholar]
- 42.Pennys NS, Wiley HE., 3rd Herpetiform blisters in systemic lupus erythematosus. Arch Dermatol. 1979;155(12):1427–1428. [PubMed] [Google Scholar]
- 43.Olansky AJ, Briggaman RA, Gammon WR, Kelly TF, Sams WM., Jr Bullous systemic lupus erythematosus. J Am Acad Dermatol. 1982;7(1):511–520. doi: 10.1016/s0190-9622(82)70134-3. [DOI] [PubMed] [Google Scholar]
- 44.Gupta R, Woodley DT, Chen M. Epidermolysis bullosa acquisita. Clin Dermatol. 2012;30(1):60–69. doi: 10.1016/j.clindermatol.2011.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Faure M. Dermatitis herpetiformis. Semin Dermatol. 1988;7:123–129. [PubMed] [Google Scholar]
- 46.Smith JB, Taylor TB, Zone JJ. The site of blister formation in dermatitis herpetiformis is within the lamina lucida. J Am Acad Dermatol. 1992;27(2 Pt 1):209–213. doi: 10.1016/0190-9622(92)70172-c. [DOI] [PubMed] [Google Scholar]
- 47.Clarindo MV, Possebon AT, Soligo EM, Uyeda H, Ruaro RT, Empinotti JC. Dermatitis herpetiformis: pathophysiology, clinical presentation, diagnosis and treatment. An Bras Dermatol. 2014;89(6):865–875. doi: 10.1590/abd1806-4841.20142966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Imber MJ, Kibbi AG, Mihm MC., Jr Dermatitis herpetiformis: Histopathologic findings. Clin Dermatol. 1991;9(3):289–293. doi: 10.1016/0738-081x(91)90020-l. [DOI] [PubMed] [Google Scholar]
- 49.Caproni M, Antiga E, Melani L, Fabbri P, Italian Group for Cutaneous Immunopathology Guidelines for the diagnosis and treatment of dermatitis herpetiformis. J Eur Acad Dermatol Venereol. 2009;23(6):633–638. doi: 10.1111/j.1468-3083.2009.03188.x. [DOI] [PubMed] [Google Scholar]
- 50.Nishioka K, Hashimoto K, Katayama I, Sarashi C, Kubo T, Sano S. Eosinophilic spongiosis in bullous pemphigoid. Arch Dermatol. 1984;120(9):1166–1168. [PubMed] [Google Scholar]
- 51.Natio K, Morioka S, Ikeda S, Ogawa H. Experimental bullous pemphigoid in guinea pigs: The role of pemphigoid antibodies, complement, and migrating cells. J Invest Dermatol. 1984;82(3):227–230. doi: 10.1111/1523-1747.ep12260057. [DOI] [PubMed] [Google Scholar]
- 52.Wintroub BU, Mihm MC, Jr, Goetzl EJ, Soter NA, Austen KF. Morphologic and functional evidence for release of mast-cell products in bullous pemphigoid. N Engl J Med. 1978;298(8):417–421. doi: 10.1056/NEJM197802232980803. [DOI] [PubMed] [Google Scholar]
- 53.Dvorak AM, Mihm MC, Jr, Osage JE, Kwan TH, Austen KF, Wintroub BU. Bullous pemphigoid, and ultrastructural study of the inflammatory response: Eosinophil, basophil and mast cell granule changes in multiple biopsies from one patient. J Invest Dermatol. 1982;78(2):91–101. doi: 10.1111/1523-1747.ep12505711. [DOI] [PubMed] [Google Scholar]
- 54.Yaoita H, Gullino M, Katz SI. Herpes gestationis. Ultrastructure and ultrastructural localization of in vivo-bound complement. J Invest Dermatol. 1976;66(6):383–388. doi: 10.1111/1523-1747.ep12483011. [DOI] [PubMed] [Google Scholar]
- 55.Blenkinsopp WK, Haffenden GP, Fry L, Leonard JN. Histology of linear IgA disease, dermatitis herpetiformis, and bullous pemphigoid. Am J Dermatopathol. 1983;5(6):547–554. doi: 10.1097/00000372-198312000-00005. [DOI] [PubMed] [Google Scholar]
- 56.Horváth B, Niedermeier A, Podstawa E, et al. IgA autoantibodies in the pemphigoids and linear IgA bullous dermatosis. Exp Dermatol. 2010;19(7):648–653. doi: 10.1111/j.1600-0625.2010.01080.x. [DOI] [PubMed] [Google Scholar]
- 57.De Jong MC, Bruins S, Heeres K, et al. Bullous pemphigoid and epidermolysis bullosa acquisita: differentiation by fluorescence overlay antigen mapping. Arch Dermatol. 1996;132(2):151–157. doi: 10.1001/archderm.132.2.151. [DOI] [PubMed] [Google Scholar]
- 58.Kazama T, Yamamoto Y, Hashimoto T, Komai A, Ito M. Application of confocal laser scanning microscopy to differential diagnosis of bullous pemphigoid and epidermolysis bullosa acquisita. Br J Dermatol. 1998;138(4):593–601. doi: 10.1046/j.1365-2133.1998.02167.x. [DOI] [PubMed] [Google Scholar]


