Abstract
Objectives
Prior research emphasizes the importance of the residential neighborhood context during later life but little attention has been afforded to other areas that older adults encounter as they move beyond their residential environments for daily activities and social interactions. This study examines the predominance of the residential context within older adults’ everyday lives.
Method
We provided 60 older adults in four New York City neighborhoods with iPhones, which captured Global Positioning Systems (GPS) locations at 5-min intervals over 1 week (n = 55,561) and 17 ecological momentary assessments (EMAs) over 4 days (n = 757) to assess real-time activities.
Results
Older adults in our sample spent nearly 40% of their time outside of their residential tracts and they visited 28 other tracts, on average. Exercising, shopping, socializing, and social activities were especially likely to take place outside of residential tracts. Differences in residential and nonresidential poverty exposure vary across gender, race/ethnicity, education, car ownership, and residential areas.
Discussion
Measuring activity space, rather than relying on residential tracts, allows examination of the social environments that are relevant for older adults’ everyday lives. Variation in characteristics of activity spaces may be an underexplored source of differences in health and well-being during later life.
Keywords: Methods, Neighborhood, Social environment, Urban sociology
An unprecedented number of older adults are “aging in place,” or residing independently in the communities where they spent the bulk of their adult lives. Later life changes such as retirement, bereavement, and the development of functional impairments and chronic illness render many of these individuals particularly vulnerable to—and dependent upon—their social environments (see Cagney & York Cornwell, 2010; Robert & Li, 2001). Prior research suggests that neighborhood characteristics shape recovery from illness (Wen & Christakis, 2005), adaption to functional limitations (Beard et al., 2009), physical activity (Mendes de Leon et al., 2009), the ability to complete daily tasks (Michael, Green, & Farquhar, 2006), and continued independent living (Cannuscio, Block, & Kawachi, 2003).
This line of research is predominantly focused on the residential neighborhood, driven by an underlying assumption that residential areas are the only contexts—or the most important contexts—shaping health and well-being (Chaix, 2009; Cummins, 2007; Diez-Roux, 2007; Matthews & Yang, 2013). Some scholars have suggested that focusing on the residential neighborhood is particularly appropriate when studying older adults, as age-related changes may reduce the geographic range of activities, increasingly anchoring daily life to the local, residential area (Inagami, Cohen, & Finch, 2007; Pearce et al., 2009). However, this has not been directly tested. An important alternative possibility is that retirement may bring greater flexibility in structuring daily life and that older adults may move beyond their local neighborhood to access services, organizations, and amenities, as well as for social contact and participation in social activities (Cagney, Browning, Jackson, & Soller, 2013).
Focusing on residential neighborhoods therefore risks misspecification of older adults’ social environments and overlooks exposures to physical and structural characteristics of nonresidential areas that may be relevant for health and well-being (Jones & Pebley, 2014; Matthews & Yang, 2013; Perchoux, Chaix, Cummins, & Kestens, 2013). For example, concentrated socioeconomic disadvantage in the residential neighborhood has been associated with negative physical and mental health outcomes (Robert, 1998; Ross, 2000; Wen, Browning, & Cagney, 2003) and with restricted network size and network interaction among older adults (York Cornwell & Behler, 2015). However, recent work among adults in Los Angeles suggests that exposure to socioeconomically disadvantaged areas outside of the residential context also contributes to individual outcomes (Sharp, Denney, & Kimbro, 2015) and may condition the association between residential neighborhood disadvantage and poor health (Inagami et al., 2007). Unfortunately, scholars have not fully considered the relevance of nonresidential neighborhood contexts for health, social connectedness, and well-being. Doing so requires taking a close look at where individuals go during their daily lives.
In this article, we present new data from a study using smartphone-based location tracking to identify older adults’ “activity spaces”—or the locations of routine activities in everyday life (Golledge & Stimson, 1997). Activity spaces include, but are not limited to, individuals’ residential neighborhoods. Instead of assuming that the residential neighborhood circumscribes older adults’ daily lives, we identify relevant social spaces based on where older adults actually spend their time. To do this, we equipped 60 older adults in four New York City neighborhoods with iPhones. The iPhones were used to capture respondents’ GPS locations in 5-min intervals over 7 days (n = 55,561 observations) and to administer 17 ecological momentary assessments (EMAs) across four of those days (n = 757 observations). This article details the method and presents descriptive findings regarding the span of older adults’ activity spaces, the relevance of their residential neighborhoods in daily life, and their exposure to socioeconomic disadvantage inside and outside of their residential contexts. Our results point to the need for greater conceptual and empirical consideration of social environments that extend beyond older adults’ residential neighborhoods.
Identifying The Social Contexts of Everyday Life
Conventional approaches to the study of neighborhood effects on individual outcomes are not only limited by their focus on residential contexts but they also typically rely on administratively defined spatial units (e.g., census tracts) as proxies for the residential context (Feng, Glass, Curriero, Stewart, & Schwartz, 2010). A recent review of research on place and health in later life found, for example, that 73% of studies use administrative boundaries to define older adults’ residential neighborhoods (Yen, Michael, & Perdue, 2009). Using census tracts as proxies for residential neighborhoods has a number of practical advantages. Tracts were determined in part by natural boundaries such as major streets and with the goal of encompassing residents who are relatively homogeneous with regard to socioeconomic status. In addition, administrative data collected or aggregated at the tract level (e.g., poverty rates) are often indicative of physical and social characteristics of the surrounding area (Diez-Roux, 2007). However, contextual effects operationalized with residential tracts in multilevel models tend to be rather small and account for only a modest portion of variation in individual outcomes (Diez Roux et al., 2001; Oakes, 2004; Pickett & Pearl, 2001). Weak associations between residential tract characteristics and health outcomes may reflect heterogeneity in individuals’ exposure to the residential tract and their access and exposure to other areas (Spielman & Yoo 2009).
The consideration of activity spaces—a concept stemming from research in geography—provides an alternative to the focus on residential neighborhoods (Golledge & Stimson, 1997). Activity spaces encompass the social environments that individuals encounter during their routine activities in everyday life including, but not limited to, their residential neighborhoods. The span and characteristics of activity spaces may be shaped by individuals’ health, physical function, socioeconomic resources, and social connectedness (Jones & Pebley, 2014; Kwan, 1999). Residential neighborhood contexts, adjoining areas, and the availability of transportation may also affect the span and shape of individuals’ activity spaces (Rainham, McDowell, Krewski, & Sawada, 2010). Thus, while some older adults are largely reliant on local resources, others may regularly travel to more distant locations to attend church, visit family members, and shop for groceries.
Recent technological advances in real-time location tracking provide an opportunity to map the relevant social spaces of daily life from the ground up (Wan & Lin, 2013, 2016; Zenk et al., 2011). Such data allow us to examine the extent to which the residential context is representative of the social contexts where individuals spend their time. To illustrate, we use data from a smartphone-based pilot study of older adults to compare, on three different dimensions, the residential and nonresidential contexts of older adults’ everyday lives.
First, we assess the extent to which daily activities take individuals beyond their residential neighborhoods (or, as often operationalized, their residential tracts), both spatially and temporally. How large is the geographic span of activity space, compared to the residential tract? And, how much time do older adults spend inside and outside of their residential tracts? Second, we consider the types of activities that older adults typically complete inside and outside of their residential tracts. This provides insight into the extent to which residential tract is the primary site for particular activities such as socializing, exercising, shopping, and accessing health care. Finally, we examine similarities between nonresidential tracts in older adults’ activity spaces and their residential tracts, with a comparison of tract-level rates of poverty. These analyses are intended to highlight the types of questions and patterns that can be explored using smartphone-based data collection and the extent to which nonresidential locations may be relevant for older adults’ health and well-being.
Data
We use data from the Real-time Neighborhoods and Social Life Study (RNSLS), a smartphone-based study of older adults in New York City. Respondents were recruited for this study through convenience sampling at senior centers in each of four neighborhood areas: East Harlem, Gramercy Park, North Bedford-Stuyvesant, and South Bedford-Stuyvesant. These four sites were chosen to maximize racial/ethnic, socioeconomic, and geographic diversity in the sample. The senior centers tend to draw older adults who live nearby for social events, educational seminars, health check-ups, and meals.
In total, 60 individuals over the age of 55 completed the study during October–November 2014. As shown in Table 1, there were between 13 and 17 respondents per site. The sample is not representative of community-residing older adults in New York City but it is diverse. Data captured via a paper-and-pencil survey at the beginning of the study show that more than 50% of the respondents identified as Black, non-Hispanic and nearly 25 percent are of Hispanic origin. About 30% of the respondents have a college degree but respondents are predominantly low-income, with more than 40% reporting annual incomes below $20,000. Most respondents are women and only about a quarter of them own a car. More than half of the respondents have lived in their current neighborhood for more than 30 years.
Table 1.
Characteristics of Respondents in the RNSLS (n = 60)
| % | N | |
|---|---|---|
| Age | ||
| 55–64 | 21.67 | 13 |
| 65–74 | 53.33 | 32 |
| 75 and over | 25.00 | 15 |
| Gender | ||
| Male | 31.67 | 19 |
| Female | 68.33 | 41 |
| Racial/ethnic background | ||
| Black, non-Hispanic | 53.33 | 32 |
| Hispanic | 26.67 | 16 |
| White, non-Hispanic and other | 20.00 | 12 |
| Education | ||
| Some college or less | 70.18 | 40 |
| College degree or more | 29.82 | 17 |
| Income | ||
| Less than $20,000 | 41.67 | 25 |
| $20,000 and higher | 43.33 | 26 |
| Missing information on income | 15.00 | 9 |
| Owns car | 25.00 | 15 |
| Years of residence in current neighborhood | ||
| Fewer than 5 | 15.00 | 9 |
| 5–9 | 16.67 | 10 |
| 10–30 | 36.67 | 22 |
| More than 30 | 31.67 | 19 |
| Poverty rate in residential tract | ||
| 5–9.9% | 8.33 | 5 |
| 10–19.9% | 21.67 | 13 |
| 20–29.9% | 43.33 | 26 |
| 30–34.9% | 21.67 | 13 |
| 35%+ | 5.00 | 3 |
| Senior Center Site | ||
| East Harlem | 23.33 | 14 |
| Gramercy Park | 21.67 | 13 |
| North Bedford-Stuyvesant | 28.33 | 17 |
| South Bedford-Stuyvesant | 26.67 | 16 |
Note: RNSLS = Real-time Neighborhoods and Social Life Study.
The study began with an introductory training session on the first Monday of the study week. The training was designed and conducted in collaboration with Older Adults Technology Services (OATS), a nonprofit organization in New York City. During the training session, each respondent was provided with an iPhone 5c to carry for 7 days. The use of a smartphone enables GPS-tracking with intermittent collection of ecological momentary assessments (EMAs). GPS tracking and EMAs are described in more detail below.
GPS Tracking
Respondents’ activity spaces were assessed via GPS locations captured by the Find My iPhone application. Each iPhone was assigned an Apple ID that was unique to the respondent, but not personally identifiable. An algorithm written specifically for this study queried Find My iPhone for the location of each respondent’s phone in 5-min intervals throughout the study period.
Smartphone-based data collection and transmission requires careful attention to issues of data security and maintenance of respondent privacy. Location data were transmitted from the iPhones to a password-protected server in a locked room via Apple’s iCloud service. iCloud uses 128-bit AES encryption to protect the data from unauthorized access while it is being transmitted. An additional advantage of using the Find My iPhone application is that it could be used to lock the iPhone or erase all data on the iPhone should it be lost or stolen, although this did not occur during the study period.
Studies using GPS trackers rather than smartphones are able to capture locations in very short time intervals such as every 1 or 5 s (e.g., Wan & Lin, 2013, 2016; Zenk et al., 2011). We use 5-min intervals to minimize drain on the iPhone’s battery and insure that it could operate for at least 2 days without recharging. Although respondents were instructed to charge their iPhones every night, pretesting indicated that some respondents forget or are unable to do this each night. The 5-min intervals allow us to identify most locations where respondents spend their time but they likely exclude some areas that respondents briefly pass through, thereby underestimating the range of areas to which older adults are exposed.
Respondent locations were captured from 9:00 a.m. to 9:00 p.m., beginning 30 min after the conclusion of the introductory training session on Monday. Observations captured 30 min prior to a 2-hr training session held on Wednesday until 30 min after the training session are dropped from the data in order to reduce the impact of study participation on the observed locations. In all, 98.85% of location queries (n = 55,973) resulted in the receipt of valid GPS coordinates. The 55,561 valid GPS locations have a median accuracy radius of 10 m (about 0.01 miles) and a mean radius of 32.7 m. Overall, 61.4% of observations had an accuracy radius of 10 m or less. Each of the GPS points was located within its corresponding census tract (based on 2010 tract boundaries) using ArcGIS. Supplementary analyses limited to GPS locations with accuracies of 10 m or less (n = 34,106) provide substantively similar results to those that we present here.
Ecological Momentary Assessment (EMA) Collection
EMAs are research tools characterized by the repeated collection of individuals’ current or recent experiences and behaviors in real-world environments (Stone and Shiffman, 1994). EMAs traditionally rely on participants’ self-reports of their activities, surroundings, and subjective states—akin to short, momentary surveys. Early EMA studies often used paper diaries completed at specified times or when the respondent was notified by a pager or beeper. Compared to these approaches, smartphone-based EMA collection allows greater flexibility in EMA timing and reduces recall bias, response errors, and nonresponse (Trull and Ebner-Priemer, 2009). Several recent studies point to the feasibility of implementing smartphone-based EMA collection among older adults, including racial minorities (Fritz, Tarrif, Saleh, & Cutchin, 2017) and those with cognitive challenges (Ramsey, Wetherell, Depp, Dixon, & Lenze, 2016).
EMAs were collected on the iPhone using Survey Swipe, a commercially available application for mobile survey research developed by Survey Analytics (www.surveyswipe.com). EMA questions appeared as text on the iPhone screen inside the Survey Swipe application and respondents answered them using the touchscreen interface. When the respondent completed an EMA, his or her responses were securely transmitted to Survey Analytics; no EMA data were stored on the iPhone. The Survey Analytics database for this project was password-protected and located behind a firewall using CheckPoint VPN-1 security.
Respondents were asked to complete 17 EMAs during the study period. The EMAs began Wednesday evening, following a training session focusing on the completion of EMAs. Then, EMAs were sent during four time windows—morning, early afternoon, late afternoon, and evening—on the subsequent Thursday, Friday, Saturday, and Sunday. The collection of four EMAs over the course of each day aimed to capture respondents during a variety of activities but it is not comprehensive. Data from the EMAs provides a systematic sample of respondents’ locations, experiences, and activities at particular moments in time over the course of four days.
Respondents were informed of the time windows but they were not told exactly what time the EMAs would be requested. When it was time to take an EMA, respondents were “pinged” via a text message from the RNSLS staff stating, “Please complete your [morning/early afternoon/late afternoon/evening] survey now.” Immediately after the text-message ping, the survey was made available in Survey Swipe and a banner notification on respondents’ lock screens announced that a new survey had been made available.
The EMAs included 23 items asking respondents to provide real-time reports about where they are, whom they are with, what they are doing, and how they feel, including happiness, anger, loneliness, and symptoms of distress such as pain, fatigue, and perceived stress. These data allow examination of how locations, activities, and experiences correspond with real-time fluctuations in health and well-being. For this article, we focus on respondents’ reports of their activities.
Respondents were encouraged to complete EMAs as soon as they were pinged. On average, the EMAs required 4.6 min to complete. In all, 98.7% of EMAs were completed before the close of the time window. Because EMAs are intended to capture real-time activities and experiences, we restrict analysis to the 757 EMAs that were received within 20 min of the ping. This generates a response rate of 75.2%.
Measures
Span of Activity Space
Using the GPS point data, we generate two measures that summarize the size or range of older adults’ activity spaces. First, as a basic measure of mobility, we calculate the respondent’s average distance away from home, based on all GPS observations. Second, we calculate the standard deviation ellipse, which is a Euclidean measure commonly used in geographic research. The ellipse is a spatial unit that includes approximately 68% of the respondent’s observed locations, centered on the mean center of respondent’s observed locations (see Sherman, Spencer, Preisser, Gesler, & Arcury, 2005). Each respondent’s ellipse and its total area in square miles was calculated in ArcGIS. Ellipse size provides a general indicator of the span of respondents’ activity spaces, but it is important to note that ellipses typically include large regions that are not actually encountered by respondents. Identification of ellipses may therefore more useful for population health research assessing access to resources rather than for assessment of exposure to local conditions. For example, fresh food stores included within an older adult’s standard deviation ellipse should be accessible to him, since they fall within the spatial area of about two-thirds of his observed locations; older adults with more fresh food stores within their ellipses can be considered as having greater access to fresh food within their activity spaces.
We also use three measures to assess the extent to which activity spaces are contained within the respondent’s residential tract. We use tracts as the geographic unit here, since most prior research considering neighborhood effects on health operationalizes the neighborhood as the residential census tract (Yen et al., 2009). We calculate the proportion of GPS locations that are outside of the respondent’s residential tract, the total number of unique tracts that the respondent visited, and the number of tracts in which the respondent stayed for at least 10 min (i.e., had at least three consecutive observations) during the study period.
Residential and Nonresidential Activities
In each EMA, respondents were asked to indicate any or all activities they are doing. We combine the activities into nine categories: (a) personal care (grooming, sleeping); (b) receiving health care; (c) housekeeping or household tasks; (d) shopping or running errands; (e) eating or drinking; (f) walking or exercising; (g) relaxing, leisure, and reading; (h) socializing; and (i) participating in social activities (including group participation, volunteering, and religious participation). We use this information, coupled with GPS location at the time that the EMA was submitted, to examine how often respondents reported each activity inside and outside of their residential tracts.
Exposure to Poverty
As a basic assessment of how activity spaces differ from residential contexts, we compare respondents’ exposure to poverty within their residential tracts and the nonresidential tracts of their activity spaces. Tract-level poverty is based on the percentage of households in the tract with incomes below poverty, from the 2009 to 2013 American Community Survey (ACS). For each GPS location, we assign the tract-level poverty rate within its corresponding tract. We calculate the mean poverty rate in nonresidential tracts as the average of the tract poverty levels across all observations in which the respondent was outside of his or her tract. Our measure of nonresidential poverty exposure is therefore weighted by the amount of time the respondent spent in each tract.
Results
We are interested in the extent to which older adults move beyond their residential tracts as they complete everyday activities. Descriptive statistics presented in Table 2 provide empirical measures of respondents’ exposure to spaces outside of their residential tracts during the study period. First, note that activity spaces vary considerably in size. Respondents were located, on average, about 0.71 miles from their residence. But the distribution of distances from the respondent’s residence is right-skewed, with two respondents having average distances above 4 miles and one with an average distance of more than 10 miles. The average area within the standard deviation ellipse, which encompasses about two-thirds of each respondent’s locations, is 4.54 square miles. By comparison, respondents’ residential tracts have an average area of 0.07 square miles. About 87% of the respondents (n = 52) had standard deviation ellipse areas that were larger than their residential tract areas.
Table 2.
Summary Statistics for Measures of Activity Space in the RNSLS Sample (n = 60)
| Mean | SD | Q1 | Median | Q3 | |
|---|---|---|---|---|---|
| Size of activity space and residential tract | |||||
| Average distance from home (mi) | 0.71 | 1.49 | 0.15 | 0.36 | 0.61 |
| Standard deviation ellipse area (mi2) | 4.54 | 16.04 | 0.24 | 0.94 | 2.35 |
| Residential tract area (mi2) | 0.07 | 0.04 | 0.06 | 0.06 | 0.07 |
| Exposure to nonresidential tracts | |||||
| GPS observations outside residential tract (%) | 38.81 | 25.86 | 17.06 | 33.99 | 51.92 |
| Tracts visited | 28.10 | 19.20 | 16.00 | 23.50 | 35.50 |
| Tracts visited for at least 10 min | 9.35 | 4.94 | 6.00 | 9.00 | 12.00 |
Note: GPS = Global Positioning Systems; RNSLS = Real-time Neighborhoods and Social Life Study.
Next, we consider the predominance of residential tracts within respondents’ activity spaces. About 39% of GPS observations located respondents outside of their residential tracts. Notably, more than 25% of the respondents spent more than half of their time outside of their residential tract. The SD of 25.86% points reveals considerable heterogeneity in the relevance of the residential tract as a context for everyday activities.
During the study week, respondents visited an average of about 28 different tracts, including their own residential tract. About a quarter of the respondents visited more than 35 tracts, while about 15% of the respondents visited fewer than 10 tracts. The 5-min intervals in GPS collection likely overlook locations that respondents visited only briefly, making this a conservative estimate of the range of exposure to nonresidential tracts.
Nevertheless, many of the tracts that respondents visited were observed only once—meaning that the respondent spent less than 5 min in the tract, perhaps because they were traveling through a tract en route to another location. Passing through tracts, even if only briefly, may allow access to resources located there (e.g., health care, fresh foods, social services). However, the short time there may limit their relevance for everyday life and their exposure-related effects on health. Thus, we also consider the number of tracts in which the respondent had at least three consecutive observations—likely indicating that the respondent was exposed to the tract for at least 10 min. On average, respondents stayed for at least 10 min in 9.35 different tracts.
Variation in Activity Space Characteristics
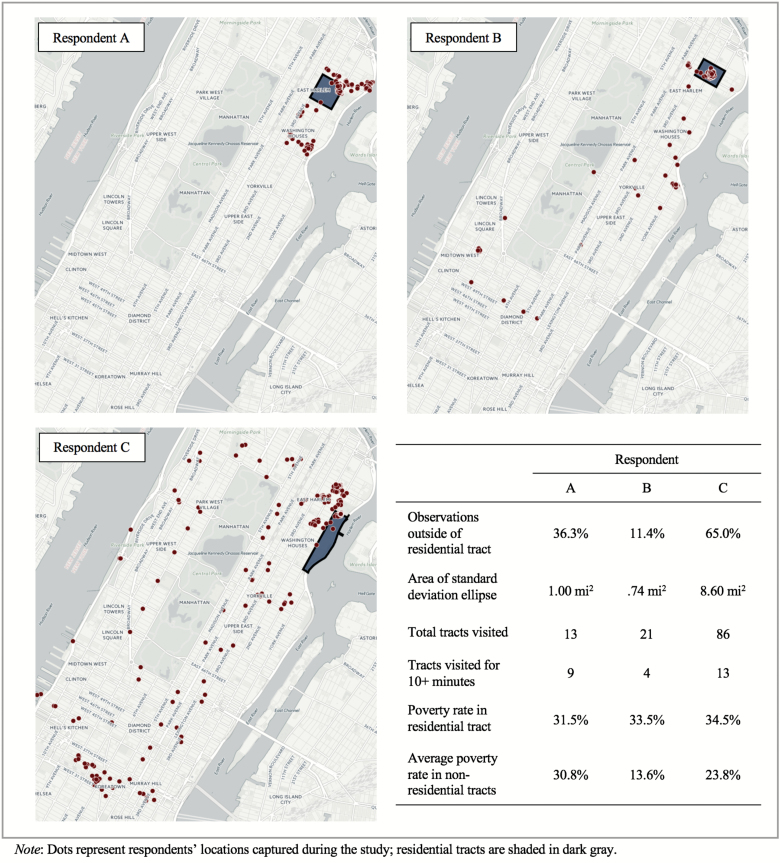
To illustrate how the span and characteristics of activity spaces vary across individuals, we take a closer look at three residents of East Harlem. The maps in Figure 1 plot each respondent’s activity space locations, with his or her residential tract shaded in dark gray. As shown, A’s activity space is tightly clustered around her residential tract while B traverses a wider range of locations. Thus, B visits more tracts than A, but because B spends less time (and therefore has fewer observations) in these tracts, his ellipse covers less total area. In contrast, C spends much more time outside of her residential tract and travels much further, which is reflected in the high count of total tracts visited (86) and the large geographic area of her activity space (8.60 square miles).
Figure 1.
Activity space characteristics of three respondents from East Harlem.
Table 3 examines variation in activity spaces across respondent characteristics and their neighborhoods. We do not find any significant differences in ellipse area across respondent characteristics or across sites but a few trends are worth noting. First, the oldest old respondents seem to have more constrained activity spaces than the younger groups, although the difference is not statistically significant. We also observe trends in which activity spaces are larger among more advantaged social groups, including whites, those with a college degree, and car owners—but large standard deviations within these groups also indicate greater heterogeneity in the span of their activity spaces. The same is true for residents of Gramercy Park and those who reside in relatively low poverty areas (having 10%–19.9% poverty).
Table 3.
Measures of Relevance of the Residential Area, by Respondent Characteristics
| Mean SD ellipse area (SD)a | Locations outside of residential tract (%)a | Mean number of tracts visited for 10+ min (SD)b | |
|---|---|---|---|
| Overall | 4.54 (16.09) | 38.81 | 9.35 (4.94) |
| Age | |||
| 55–64 | 3.35 (6.82) | 42.64 | 8.92 (3.25) |
| 65–74 | 3.03 (3.97) | 39.32 | 10.22 (5.60) |
| 75 and over | 1.18 (2.05) | 34.39 | 7.87 (4.49) |
| Gender | |||
| Male | 4.87 (6.53) | 37.50 | 10.74 (6.29) |
| Female | 4.38 (18.99) | 39.41 | 8.71 (4.11) |
| Racial/ethnic background | |||
| Black, non-Hispanic | 3.20 (5.36) | 38.71 | 9.47 (5.49) |
| Hispanic | 1.33 (2.13) | 38.81 | 8.00† (3.67) |
| White, non-Hispanic | 12.39 (34.73) | 39.08 | 10.83 (4.75) |
| Education | |||
| Less than college degree | 2.15 (3.34) | 40.13 | 8.83 (5.17) |
| College degree or more | 10.88 (29.36) | 38.53 | 10.71 (4.45) |
| Income | |||
| Less than $20,000 | 1.92 (2.91) | 44.59 | 8.56 (3.65) |
| $20,000 and higher | 3.31 (5.50) | 35.13 | 9.96 (5.63) |
| Car ownership | |||
| No | 1.98 (3.04) | 39.53 | 8.80 (4.77) |
| Yes | 12.22 (31.17) | 36.64 | 11.00 (5.25) |
| Senior Center Site | |||
| East Harlem | 1.37 (2.20) | 32.87 | 7.57 (3.74) |
| Gramercy Park | 12.05 (33.37) | 41.63 | 11.54* (6.54) |
| North Bedford-Stuyvesant | 3.90 (6.40) | 45.09 | 9.59 (4.36) |
| South Bedford-Stuyvesant | 1.89 (2.78) | 35.04 | 8.88 (4.69) |
| Poverty rate in residential tract | |||
| 5–9.9% | 2.06 (3.43) | 41.63 | 9.40 (6.66) |
| 10–19.9% | 12.30 (33.33) | 37.71 | 10.38 (5.92) |
| 20–29.9% | 3.02 (5.38) | 39.77 | 9.04 (4.54) |
| 30%+ | 1.49 (2.04) | 37.25 | 9.00 (4.53) |
Note: aSymbols indicate statistically significant difference from italicized group, based on bivariate OLS regression models predicting the proportion of locations outside of the residential tract. bSymbols indicate statistically significant difference from italicized group, based on bivariate negative binomial regression models predicting the number of tracts visited.
† p < .10. *p < .05. (two-tailed tests, compared to italicized group).
The largest gaps in the proportion of time spent outside of the residential tract are observed across age groups, with the oldest old spending about 34% of their time outside of the residential tract compared to nearly 43% of time among the youngest old in this sample (but the difference is not significant). The proportion of time spent outside of the residential tract does not significantly differ across other respondent characteristics, or across sites. However, trends suggest that respondents with less education and lower incomes spend more time outside of their residential tracts than their higher status counterparts.
Finally, we consider the number of tracts in which respondents stayed for more than 10 min. Men, those with a college degree, and car owners stayed in more tracts than their counterparts, but the differences are not significant. The only significant differences are found within race/ethnicity and sites. Hispanic respondents stayed in fewer tracts than White respondents (p = .067) and residents of East Harlem stayed in fewer tracts than residents of Gramercy Park (p < .05). Because most White respondents reside in Gramercy Park and most Hispanic respondents reside in East Harlem, it is not clear whether these patterns are attributable to racial/ethnic differences in activity space patterns or to differential spatial distributions of resources and amenities surrounding their residential neighborhoods.
Activities in Nonresidential Environments
We use data from the EMAs to examine how particular types of activities are associated with exposure to areas outside of older adults’ own residential tracts. As shown in Table 4, of the 757 valid EMAs, about 27.1% found the respondent at a location outside of his or her census tract. This is lower than the overall rate of nonresidential tract locations in the GPS data (38.8%), which may reflect that respondents were more likely to respond to EMAs within the 20-min time window when they were inside their residential areas. It is also worth noting that, in about 89.6% of the observations within the respondent’s residential tract, the respondent reported being at home.
Table 4.
EMA Observations and Activities Within Residential and Nonresidential Tracts (n = 757)
| Inside residential tract (%) | Outside residential tracta (%) | N | |
|---|---|---|---|
| All EMA observations | 72.92 | 27.08 | 757 |
| By activities reported | |||
| Housework or household tasks | 99.41 | 0.59 | 169 |
| Personal care | 94.00 | 6.00 | 200 |
| Leisure or relaxing | 81.30 | 18.70 | 353 |
| Eating | 73.30 | 26.70 | 221 |
| Receiving health care | 63.16 | 36.84 | 19 |
| Social activities | 57.22 | 42.78 | 194 |
| Socializing | 56.67 | 43.33 | 210 |
| Walking or exercising | 55.56 | 44.44 | 81 |
| Shopping or errands | 43.84 | 56.16 | 73 |
Note: EMA = Ecological momentary assessment.
Table 4 shows that housework, personal care, leisure activities, and eating were most likely to occur inside respondents’ residential tracts—with a large share of these taking place at home. About two-thirds of the observations in which respondents were receiving health care found them in their residential tracts but this is based on only 19 observations. Other activities are more evenly split across residential and nonresidential tracts. In more than 40% of the observations where respondents reported taking part in social activities, socializing, or exercising, they were outside of their residential tracts. And, in over half of the observations during which respondents were shopping (56.2%), they were located outside of their residential tracts.
Residential and Nonresidential Exposure to Poverty
Finally, we consider the extent to which characteristics of nonresidential tracts in respondents’ activity spaces are similar to those of their residential tracts. For this, we focus on exposure to poverty. Returning to the comparisons of East Harlem respondents in Figure 1, we observe striking differences in exposure to poverty, even within older adults who reside in the same neighborhood area. Respondent A’s nonresidential poverty exposure is similar to the poverty level in her residential tract (30.8% compared to 31.5%, respectively). Both B and C are exposed to lower poverty levels in nonresidential tracts. The difference in residential and nonresidential poverty rates is largest for B (19.9% points) but B spends much less time in nonresidential tracts than does C.
Table 5 examines variation in residential and nonresidential exposure to poverty across respondent characteristics. Nearly all of the groups in this sample had lower average exposure to poverty in nonresidential tracts compared to their residential tracts. The only exception is observed among residents of North Bedford-Stuyvesant, which may stem from the extremely high-poverty areas surrounding this neighborhood.
Table 5.
Poverty in Residential and Nonresidential Tracts, by Respondent Characteristics
| Mean poverty level in residential tract (SD)a | Exposure-weighted poverty level in nonresidential tracts (SD)b | Within-group difference between nonresidential and residential povertyc | |
|---|---|---|---|
| Overall | 23.31 (9.12) | 19.96 (7.30) | −3.35** |
| Age | |||
| 55–64 | 28.01 (9.31) | 22.29 (6.11) | −5.72† |
| 65–74 | 22.21† (8.53) | 19.71 (7.70) | −2.50 |
| 75 and over | 21.52† (8.38) | 18.46 (7.30) | −3.06 |
| Gender | |||
| Male | 21.52 (8.38) | 19.79 (7.58) | −1.73 |
| Female | 24.13 (9.42) | 20.03 (7.26) | −4.10** |
| Racial/Ethnic Background | |||
| Black, non-Hispanic | 22.59† (6.80) | 20.14** (6.98) | −2.45 |
| Hispanic | 29.37** (8.97) | 23.75*** (7.74) | −5.62* |
| White, non-Hispanic | 17.13 (10.46) | 14.41 (3.41) | −2.72 |
| Education | |||
| Less than college degree | 23.65 (8.07) | 21.87 (7.42) | −1.78 |
| College degree or more | 22.67 (11.59) | 15.45*** (4.75) | −7.22* |
| Income | |||
| Less than $20,000 | 25.69* (8.47) | 22.69* (6.84) | −3.00† |
| $20,000 and higher | 20.31 (9.05) | 17.63 (6.90) | −2.68 |
| Car ownership | |||
| No | 22.85 (9.93) | 20.50 (7.70) | −2.35 |
| Yes | 24.67 (6.16) | 18.32 (5.84) | −6.35*** |
| Senior Center Site | |||
| East Harlem | 32.47 (2.07) | 24.31 (6.37) | −8.16*** |
| Gramercy Park | 15.28*** (11.34) | 14.69** (8.53) | −0.59 |
| North Bedford-Stuyvesant | 23.50*** (2.41) | 25.02 (3.45) | 1.52 |
| South Bedford-Stuyvesant | 21.60*** (8.76) | 15.04*** (2.61) | −6.56** |
Note: aSymbols denote statistically significant differences compared to the italicized group, from bivariate OLS regressions of poverty rates in residential tracts. bSymbols denote statistically significant differences compared to the italicized group, from bivariate OLS regressions of poverty rates in nonresidential tracts. cSymbols denote statistically significant differences in residential and nonresidential poverty levels within the same group, based on paired-sample t-tests with df = n-1.
† p < .10. *p < .05. **p < .01. ***p < .001 (two-tailed tests).
Black and Hispanic respondents, and those with lower incomes, tend to live in higher poverty tracts than White and higher-income respondents. Similar patterns are observed for nonresidential poverty exposure. Black and Hispanic respondents are exposed to higher levels of nonresidential-tract poverty (20.1% and 23.8% poverty, respectively) compared to Whites (14.4% poverty). Those with lower incomes and lower levels of education are also exposed to greater poverty in their nonresidential areas.
Importantly, there is notable variation across groups in the magnitude of the differences between residential and nonresidential poverty exposure. As shown in the right-most column, the exposure-weighted poverty level in nonresidential tracts is more than 3% points lower than respondents’ residential tract poverty levels, on average. However, the difference between nonresidential and residential poverty levels is particularly large among Hispanic respondents (with a gap of 5.6% points), those with college degrees (7.2% points), and car owners (6.4% points). These findings suggest that social resources shape the extent to which older adults are exposed to less disadvantaged areas. Lower rates of nonresidential-tract poverty are also observed among residents of East Harlem and South Bedford-Stuyvesant, which may reflect that these areas are surrounded by less socioeconomic disadvantage than Gramercy Park or North Bedford-Stuyvesant.
Discussion
The purpose of this article is to present data from a smartphone-based study using GPS tracking and EMAs to describe the activity spaces of older adults. Contrary to the assumption that older adults are tightly tethered to their local, residential environments (e.g., Inagami et al., 2007; Pearce et al., 2009), we find that the vast majority of respondents in our sample have activity spaces that are larger in geographic size than their residential tracts. During the study week, respondents spent nearly 40% of their time outside of their residential tracts and spent at least 10 min in more than nine tracts, on average. Strikingly, more than a quarter of the sample spent more than half of their time outside of their residential tracts. This suggests that residential neighborhoods, typically operationalized as the residential census tract, do not capture all of the social environments of older adults’ everyday lives. Measuring activity space allows us to account for nonresidential exposures and conditions that may be relevant for health and well-being.
We also find that characteristics of activity spaces vary across individuals and groups. Importantly, we find some (nonsignificant) evidence that participants with lower levels of education and income spend more time outside of their tracts. But these groups had smaller activity space areas and visited fewer tracts than their higher status counterparts. More research is needed to explore how individuals’ socioeconomic status and their local area shape their exposure to other areas that pose health risks or provide health-promoting resources such as fresh foods or green spaces (see Jones & Pebley, 2014; Zenk et al., 2011).
Data from the EMAs shed some light on the kinds of activities that may pull older adults outside of their residential neighborhoods. We find four activities that took place outside of older adults’ residential tracts more than 40% of the times they were observed: shopping, exercising, socializing, and participating in social groups or activities. This is noteworthy because physical and social activities are often emphasized in programs promoting older adults’ health and social engagement. Further research should consider the implications of the proximity of these activities to older adults’ residential neighborhoods.
Finally, we compared structural characteristics of residential and nonresidential tracts by examining poverty rates. Poverty rates in nonresidential tracts tend to be lower than those in residential tracts but we observe substantial variation across groups in the extent of the difference between residential and nonresidential poverty exposure. Hispanic older adults, those with college degrees, and those who own cars spend time in nonresidential areas that have particularly low poverty compared to their residential tracts. This suggests that poverty within one’s residential tract may not be a good proxy for overall exposure to poverty. We urge more research on how exposure to nonresidential poverty may contribute to socioeconomic and racial/ethnic disparities in health and aging.
Methodological Limitations and Future Directions
This is the first study, of which we are aware, that uses smartphone-based GPS tracking and EMA collection to identify and characterize the activity spaces of older adults. Several limitations are worth noting. First, the small, nonprobabilistic sample constrains our ability to generalize from the findings to the broader population of older adults in the United States. The patterns we observe may be unique to the dense, urban context of New York City. Census tracts in the city are relatively small, which may increase exposure to nonresidential tracts. Low rates of car ownership and reliance on walking and public transportation may also shape mobility within this sample. While the clustering of respondents in residential neighborhoods allows us to observe some differences in activity patterns across residential areas, it also introduces the potential for autocorrelation within sample clusters. Larger clustered samples would enable the use of more advanced statistical approaches, such as multilevel regression models, for evaluation of the individual- and neighborhood-level variation in activity spaces.
Smartphone-based research on activity spaces generates more precise measures of activity space than survey-based approaches that ask respondents to report a handful of common destinations (e.g., grocery shopping, health care, attending religious services) (see, e.g., Jones & Pebley, 2014). However, the relatively short period of data collection in this study (7 days for GPS and 4 days for EMA collection) may overlook locations that are important to respondents but visited less frequently such as on a biweekly or monthly schedule. The short period of data collection may also be more susceptible to the influence of exogenous factors. Unseasonably warm weather during the weeks of this study, for example, may have increased older adults’ mobility around the city.
Five-minute intervals for GPS collection, intended to reduce battery drain, may have also caused us to overlook some locations, leading to underestimation of the range or span of older adults’ activity spaces. More frequent observations (e.g., 15- to 75-s intervals) would increase precision and allow us to glean additional information such as types of activities (e.g., walking, traveling via car, bus, or other means) from the GPS observations (Wan & Lin, 2013, 2016). The nature and duration of exposure to particular contexts may condition their effects on health.
More frequent EMA collection could have provided data on additional locations and activities but EMA frequency must be balanced against the risks of respondent burnout and nonresponse. A recent study suggests that older adults will participate in up to 7 EMAs per day for a week without significant increases in nonresponse (Fritz et al., 2017) but this may vary by the length and complexity of the EMAs. Further research should explore event-based EMAs that are deployed based on a variable of interest, such as the respondent’s location outside of the residential tract, physical activity, or participation in a particular activity such as socializing.
Smartphone-based research methods also pose some general challenges in implementation and administration. One is the nontrivial cost of providing smartphones and/or data plans for respondents. Smartphone-based data collection also requires technological expertise around the development of protocols for extracting accurate location data, and for securely transmitting, storing, and managing the data. Survey apps are making it easier to collect EMAs via smartphones, but these may need to be modified for research purposes or for specific populations, such as seniors with cognitive or functional impairments (see, e.g., Ramsey et al., 2016). Many older adults’ lack of familiarity with smartphones increases the need for training and technical assistance, but we found that it also heightened respondents’ interest in the study.
While the costs and challenges of smartphone-based data collection create hurdles for widespread implementation, this method could also be considered as a way to augment more traditional survey or observational designs. For example, smartphone-based data collection focused within a subset or clustered sample of respondents could identify those for whom the neighborhood is a less appropriate proxy for daily exposures. At the same time, investment in larger studies collecting longitudinal data on activity spaces, along with changes in health and social connectedness, could provide fresh insight into how social environmental conditions shape later-life trajectories of health and well-being.
Funding
This work was supported by the National Institute on Aging (grant number 1R01 AG050605-01A1); the Cornell Institute for Social Sciences (ISS); and the Cornell Population Center (CPC).
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
We are grateful for comments on earlier versions of this work from Chris Browning, Benjamin Cornwell, Kendra Bischoff, Steven Alvarado, Matt Hall, Anna Haskins, Laura Tach, and Dan Lichter. This project benefitted from research assistance provided by Alex Currit, Alex Glazebrook, George Berry, and Jessica Hajdukiewicz. Data collection for this project was funded through grants from the Cornell Institute for Social Sciences (ISS) and the Cornell Population Center (CPC).
References
- Beard J. R. Blaney S. Cerda M. Frye V. Lovasi G. S. Ompad D., … Vlahov D (2009). Neighborhood characteristics and disability in older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64B, 252–257. doi:10.1093/geronb/gbn018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagney K. A. Browning C. R. Jackson A. L., & Soller B (2013). Networks, neighborhoods, and institutions: An integrated ‘activity space’ approach for research on aging. In L., Waite (Ed.), New directions in the sociology of aging (pp. 151–174). Washington, DC: National Academies Press. [Google Scholar]
- Cagney K. A., York Cornwell E. (2010). Neighborhoods and health in later life: The intersection of biology and community. Annual Review of Gerontology and Geriatrics, 30, 323–348. doi:10.1891/0198-8794.30.323 [Google Scholar]
- Cannuscio C., Block J., Kawachi I. (2003). Social capital and successful aging: The role of senior housing. Annals of Internal Medicine, 139, 395–399. doi: 10.7326/0003-4819-139-5_Part_2-200309021-00003 [DOI] [PubMed] [Google Scholar]
- Chaix B. (2009). Geographic life environments and coronary heart disease: A literature review. Transportation Research Part C, 17, 285–297. doi:10.1016/j.healthplace.2013.01.003 [DOI] [PubMed] [Google Scholar]
- Cummins S. (2007). Commentary: investigating neighbourhood effects on health–avoiding the ‘local trap’. International Journal of Epidemiology, 36, 355–357. doi:10.1093/ije/dym033 [DOI] [PubMed] [Google Scholar]
- Diez Roux A. V. Merkin S. S. Arnett D. Chambless L. Massing M. Nieto F. J., … Watson R. L (2001). Neighborhood of residence and incidence of coronary heart disease. The New England Journal of Medicine, 345, 99–106. doi:10.1056/NEJM200107123450205 [DOI] [PubMed] [Google Scholar]
- Diez-Roux A. V. (2007). Neighborhoods and health: Where are we and where do we go from here?” Revue D’epidemiologie et de Sante Publique, 55, 13–21. doi:10.1016/j.respe.2006.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng J., Glass T. A., Curriero F. C., Stewart W. F., Schwartz B. S. (2010). The built environment and obesity: A systematic review of the epidemiologic evidence. Health & Place, 16, 175–190. doi:10.1016/j.healthplace.2009.09.008 [DOI] [PubMed] [Google Scholar]
- Fritz H. Tarrif W. Saleh D.J., & Cutchin M.P (2017). Using a smartphone-based ecological momentary assessment protocol with community-dwelling older African Americans. Journals of Gerontology: Social Sciences. doi:10.1093/geronb/gbw166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golledge R. G., & Stimson R. J (1997). Spatial behavior: A geographic perspective. New York: Guilford Press. [Google Scholar]
- Hufford M. R. (2007). Special methodological challenges and opportunities in ecological momentary assessment. In A. A. Stone S. Shiffman A. A. Atienza, & L. Nebeling, (Eds.), The science of real-time data capture: Self-reports in health research (pp. 54–75). Oxford: Oxford University Press. [Google Scholar]
- Inagami S., Cohen D. A., Finch B. K. (2007). Non-residential neighborhood exposures suppress neighborhood effects on self-rated health. Social Science & Medicine (1982), 65, 1779–1791. doi:10.1016/j.socscimed.2007.05.051 [DOI] [PubMed] [Google Scholar]
- Jones M., Pebley A. R. (2014). Redefining neighborhoods using common destinations: Social characteristics of activity spaces and home census tracts compared. Demography, 51, 727–752. doi:10.1007/s13524-014-0283-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan M. -P. (1999). Gender and individual access to urban opportunities: A study using space-time measures. Professional Geographer, 51, 210–227. doi:10.1111/0033-0124.00158 [Google Scholar]
- Matthews S. A., Yang T. C. (2013). Spatial polygamy and contextual exposures (SPACEs): Promoting activity space approaches in research on place and health. The American Behavioral Scientist, 57, 1057–1081. doi:10.1177/0002764213487345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes de Leon C. F. Cagney K. A. Bienias J. L. Barnes L. L., Skarupski K. A. Scherr P. A., & Evans D. A (2009). Neighborhood social cohesion and disorder in relation to walking in community-dwelling older adults: A multi-level analysis. Journal of Aging and Health, 21, 155–171. doi:10.1177/0898264308328650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael Y. L., Green M. K., Farquhar S. A. (2006). Neighborhood design and active aging. Health & Place, 12, 734–740. doi:10.1016/j.healthplace.2005.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakes J. M. (2004). The (mis)estimation of neighborhood effects: Causal inference for a practicable social epidemiology. Social Science & Medicine (1982), 58, 1929–1952. doi:10.1016/j.socscimed.2003.08.004 [DOI] [PubMed] [Google Scholar]
- Pearce A., Kirk C., Cummins S., Collins M., Elliman D., Connolly A. M., Law C. (2009). Gaining children’s perspectives: A multiple method approach to explore environmental influences on healthy eating and physical activity. Health & Place, 15, 614–621. doi:10.1016/j.healthplace.2008.10.007 [DOI] [PubMed] [Google Scholar]
- Perchoux C., Chaix B., Cummins S., Kestens Y. (2013). Conceptualization and measurement of environmental exposure in epidemiology: Accounting for activity space related to daily mobility. Health & Place, 21, 86–93. doi:10.1016/j.healthplace.2013.01.005 [DOI] [PubMed] [Google Scholar]
- Pickett K. E., Pearl M. (2001). Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. Journal of Epidemiology and Community Health, 55, 111–122. doi:10.1136/jech.55.2.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rainham D., McDowell I., Krewski D., Sawada M. (2010). Conceptualizing the healthscape: Contributions of time geography, location technologies and spatial ecology to place and health research. Social Science & Medicine (1982), 70, 668–676. doi:10.1016/j.socscimed.2009.10.035 [DOI] [PubMed] [Google Scholar]
- Ramsey A. T., Wetherell J. L., Depp C., Dixon D., Lenze E. (2016). Feasibility and acceptability of smartphone assessment in older adults with cognitive and emotional difficulties. Journal of Technology in Human Services, 34, 209–223. doi:10.1080/15228835.2016.1170649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert S. A. (1998). Community-level socioeconomic status effects on adult health. Journal of Health and Social Behavior, 39, 18–37. doi:10.2307/2676387 [PubMed] [Google Scholar]
- Robert S. A., Li L. W. 2001. Age variation in the relationship between community socioeconomic status and adult health. Research on Aging, 23, 233–258. doi:10.1177/0164027501232005 [Google Scholar]
- Ross C.E. (2000). Neighborhood disadvantage and adult depression. Journal of Health and Social Behavior, 41, 177–187. doi:10.2307/2676304 [PubMed] [Google Scholar]
- Sharp G., Denney J. T., Kimbro R. T. (2015). Multiple contexts of exposure: Activity spaces, residential neighborhoods, and self-rated health. Social Science & Medicine (1982), 146, 204–213. doi:10.1016/j.socscimed.2015.10.040 [DOI] [PubMed] [Google Scholar]
- Sherman J. E., Spencer J., Preisser J. S., Gesler W. M., Arcury T. A. (2005). A suite of methods for representing activity space in a healthcare accessibility study. International Journal of Health Geographics, 4, 24. doi:10.1186/1476-072X-4-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielman S. E., Yoo E. H. (2009). The spatial dimensions of neighborhood effects. Social Science & Medicine (1982), 68, 1098–1105. doi:10.1016/j.socscimed.2008.12.048 [DOI] [PubMed] [Google Scholar]
- Stone A. A., Shiffman S. (1994). Ecological momentary assessment in behavioral medicine. Annals of Behavioral Medicine, 24, 236–243. doi:10.1207/S15324796ABM2403_09 [Google Scholar]
- Trull T. J., & Ebner-Priemer U. W (2009). Using experience sampling methods/ecological momentary assessment (ESM/EMA) in clinical assessment and clinical research: Introduction to the special section. Psychological Assessment, 21, 457–462. doi:10.1037/a0017653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan N., & Lin G (2013). Life-space characterization from cellular telephone collected GPS data. Computers, Environment and Urban Systems, 39, 63–70. doi:10.1016/j.compenvurbsys.2013.01.003 [Google Scholar]
- Wan N., & Lin G (2016). Classifying human activity patterns from smartphone collected GPS data: A fuzzy classification and aggregation approach. Transactions in GIS, 20, 869–86. doi:10.1111/tgis.12181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M., Browning C. R., Cagney K. A. (2003). Poverty, affluence, and income inequality: Neighborhood economic structure and its implications for health. Social Science & Medicine, 57, 843–860. doi:10.1016/S0277-9536(02)00457-4 [DOI] [PubMed] [Google Scholar]
- Wen M., Christakis N. A. (2005). Neighborhood effects on posthospitalization mortality: A population-based cohort study of the elderly in Chicago. Health Services Research, 40, 1108–1127. doi:10.1111/j.1475-6773.2005.00398.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen I. H., Michael Y. L., Perdue L. (2009). Neighborhood environment in studies of health of older adults: A systematic review. American Journal of Preventive Medicine, 37, 455–463. doi:10.1016/j.amepre.2009.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- York Cornwell E., Behler R. L. (2015). Urbanism, neighborhood context, and social networks. City & Community, 14, 311–335. doi:10.1111/cico.12124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk S. N. Schulz A. J. Matthews S. A. Odoms-Young A. Wilbur J. Wegrzyn L., … Stokes C (2011). Activity space environment and dietary and physical activity behaviors: A pilot study. Health & Place, 17, 1150–1161. doi:10.1016/j.healthplace.2011.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]