Abstract
Despite decades of epidemiological research, it remains uncertain whether ionizing radiation can cause lymphomas. Most epidemiological studies of lymphoma risk following non-uniform exposure used dose to red bone marrow (RBM), constituting a small fraction of the lymphocytes, as a surrogate of dose to the lymphocytes. We developed a method to estimate dose to the lymphocytes using the reference distribution of lymphocytes throughout the body and Monte Carlo simulations of computational human phantoms. We applied our method to estimating lymphocyte doses for a pediatric CT patient cohort in the United Kingdom. Estimated dose to the RBM was greater than lymphocyte dose for most scan types (up to 2.6-fold higher, a 5-year-old brain scan) except abdomen scan (RBM dose was about half the lymphocyte dose, a 5-year-old abdomen scan). The lymphocyte dose in the UK cohort showed that T-spine and whole body scans delivered the highest lymphocyte doses (up to 22.4 mGy).
INTRODUCTION
Despite decades of epidemiological research, it remains uncertain whether ionizing radiation can cause lymphomas(1–5). Most of the previous epidemiological studies of lymphoma risk used radiation dose to red bone marrow (RBM) as a surrogate of radiation dose to lymphocytes, from which lymphomas derive. Because the RBM only constitutes a small fraction (3–7%)(6, 7) of the lymphocyte distribution throughout the body, it may be a relatively poor surrogate for exposure, which could have reduced the power of previous epidemiological studies of non-uniform exposures to detect a dose-response for lymphomas.
The lymphatic system is composed of lymphatic vessels, patches of lymphatic tissue, lymphatic organs, and isolated lymphocytes(7). Computational human phantoms simulating human anatomy coupled with Monte Carlo radiation transport techniques have made it possible to precisely estimate radiation dose delivered to some organs within the lymphatic system exposed to a variety of radiation source. However, it is still complex to derive dose to other remaining tissues. To our knowledge, no dosimetry methods for the lymphatic system have been reported to date.
In the current study, we developed a new method to estimate lymphocyte dose by using reference data for lymphocyte distribution throughout the body and Monte Carlo radiation transport in human anatomy represented by a series of computational human phantoms. We then applied the method to estimate lymphocyte dose for the pediatric and young adult patients who underwent computed tomography (CT) examinations in the United Kingdom.
MATERIALS AND METHODS
Lymphocyte dosimetry model
International Commission on Radiological Protection (ICRP) Publication 23(6) and 89(7) report the distribution of lymphocytes across four major tissue sites in human anatomy as a function of age as summarized in Table 1: RBM, lymphatic organs (spleen, lymph node, thymus and small intestine), blood and outside hematopoietic tissues (i.e. lymphocytes circulating throughout the body). Once radiation dose to each of the four components is estimated in any radiation exposure scenarios, lymphocyte dose can be derived through weighting dose to the four components by the distribution of lymphocytes in each component.
Table 1.
Distribution of lymphocyte (%) across the four components in children and adults (ICRP Publication 89(7)).
| Age | Mass (g) | Distribution of lymphocytes (%) | |||
|---|---|---|---|---|---|
| Red bone marrow | Blood | Lymphatic organsa | Outside hematopoietic tissues | ||
| Newborn | 150 | 5.0 | 0.3 | 16.0 | 78.7 |
| 1 year | 650 | 3.0 | 0.2 | 12.0 | 84.8 |
| 5 years | 650 | 3.0 | 0.2 | 12.0 | 84.8 |
| 10 years | 900 | 4.5 | 0.2 | 9.5 | 85.8 |
| 15 years | 1250 | 6.0 | 0.2 | 7.5 | 86.3 |
| Adult female | 1500 | 7.0 | 0.2 | 7.0 | 85.8 |
| Adult male | 1300 | 7.0 | 0.2 | 7.0 | 85.8 |
aLymphatic organs include spleen, lymph node, thymus and small intestine.
This approach requires computational human phantoms coupled with Monte Carlo radiation transport technique to estimate radiation dose delivered to specific organs in human anatomy. We adopted a series of computational human phantoms(8) representing newborn, 1-, 5-, 10-, 15-year old, and adult male and female reference individuals where the ICRP reference organ mass(7), the ICRP reference dimension of alimentary tract(9), and the reference elemental composition(7, 10) are incorporated. The anatomy of the male and female phantoms from newborn to 10-year old is identical except for the urinary bladder and the gender-specific organs such as gonads, uterus, and prostate. For Monte Carlo radiation transport, we used a general purpose Monte Carlo code, MCNPX Version 2.7(11).
First, dose to RBM can be estimated by using the skeletal anatomy models built in the computational human phantom series and Monte Carlo code. Radiation fluence (particle/m2) to spongiosa within each bone site is estimated through Monte Carlo method for computational phantoms and converted to absorbed dose (Gy) to RBM by multiplying them by pre-calculated dose coefficients called response function (Gy m2)(12). Dose to RBM calculated for different bone sites is then weighted by the distribution of RBM across bone sites(7) to estimate whole body RBM dose.
Dose to blood, the second component in the lymphocyte distribution (Table 1), can be derived by using organ doses computed from the computational human phantoms and reference blood distribution. ICRP Publication 89(7) provides the reference values for regional blood volumes for adult male and female across about 30 different organs and tissues. Once doses to the organs and tissues are calculated, the blood volume distribution data can be used for weighting the doses to derive average blood dose. We assumed that children have the same blood volume distribution as the reference adult data because ICRP Publication 89 only provides adult data.
Third, all lymphatic organs are available from computational human phantoms, including a lymph node model(13) that we previously published. The lymph nodes in the phantoms are distributed across the 16 cluster sites identified from the literature: extrathoracic, cervical, thoracic (upper and lower), breast (left and right), mesentery (left and right), axillary (left and right), cubital (left and right), inguinal (left and right) and popliteal (left and right). Dose to each organ and tissue including lymph nodes can be calculated from phantoms and weighted by organ volumes to obtain average lymphatic organ dose.
Finally, as a surrogate for lymphocytes circulating outside hematopoietic tissues, we used volume-weighted dose to all organs and tissues except for the lymphatic organs and skeleton.
Lymphocyte dose for the UK CT patients
We applied our lymphocyte dosimetry method to the UK CT retrospective epidemiological study(14). The cohort includes a total of 180 000 children and young adults who underwent CT scans in the UK between 1980 and 2002. The numerous CT scan types in the cohort were grouped into 15 different scan regions: brain, partial brain, facial bone, neck, chest, high-resolution CT, abdomen, pelvis, hip, cervical spine, thoracic spine, lumbosacral spine, shoulder, whole body and extremity. To estimate lymphocyte dose to the patient cohort, we first calculated dose coefficients, which convert CT scanner output (CTDIvol) to organ dose(15, 16), and then multiply them by a set of CTDIvol values(17) previously established from surveys(18, 19) conducted in the UK.
First, we calculated overall lymphocyte dose coefficients after estimating dose coefficients for the four tissue components in Table 1 for six age groups (newborn, 1, 5, 10, 15 years and adult) undergoing the 15 CT examinations by using an in-house CT organ dose calculator, National Cancer Institute dosimetry system for CT (NCICT)(15). NCICT is based on a comprehensive library of dose coefficients for 33 organs and tissues calculated from the computational phantom series coupled with Monte Carlo radiation transport code, MCNPX2.7(11). Dose to blood was derived from organ doses calculated by NCICT and weighted by the blood volume distribution as described in the previous section. Since NCICT does not provide lymph node dose, it was additionally calculated using Monte Carlo simulation of a reference CT scanner(20) coupled with the lymph node-implemented computational human phantom series(13).
Second, we multiplied the CTDIvol collected from two UK surveys(18, 19) by the lymphocyte dose coefficients for the 15 scan types as described in the following equation.
| (1) |
where is the dose to lymphocyte for a given age and gender of patients scanned for the scan type in the year , is the slice number where scanning starts, and is the slice number where scanning ends, is the dose coefficients for the patient of age and gender at the slice , and is the CTDIvol for the age of a patient, the scan type and in the year collected from the UK survey. Based on previous studies(21–23), we divided the period of the UK CT study (1980–2002) into two time periods, before and after 2001, assuming that CT scan protocols for adults were also used for children before 2001 and age-specific protocols began to be used since then. For the patients with ‘unknown’ scan type (no information on CT scan region was given), average doses weighted by the frequency of the other 15 CT scan types were used for the dose estimates(17).
RESULTS AND DISCUSSION
We tabulated dose coefficients (mGy/mGy) of the four major tissue sites and lymphocytes for three major scan types calculated using the protocol assumed to be used before 2001 (adult scan protocol was used for children) in Table 2. As expected from the distribution of lymphocytes across the four tissue sites in Table 1, the doses to outside hematopoietic tissues are overall similar to the lymphocyte doses for all ages except for newborns, for whom dose to outside hematopoietic tissues is 13% greater than lymphocyte dose for a brain scan, 10% smaller for a chest scan, and 17% smaller for an abdominal scan. The phantoms representing younger ages show greater lymphocyte dose coefficients than those for older ages. For example, the newborn phantom showed greater lymphocyte dose coefficients than the adult male phantom by a factor of 5.3, 2.7 and 2.5 times for brain, chest and abdomen scans, respectively. The chest scan delivers a higher dose to the lymphocytes compared with other scans when CTDIvol is fixed. In case of the adult male, the lymphocytes in chest scan receive about 8.4 times greater dose than brain scan.
Table 2.
Organ dose per unit CTDIvol (mGy/mGy) for the four major tissue sites and the lymphocyte in the pediatric and adult male and female phantoms simulated for brain, chest, and abdomen CT scans.
| Scan type | Organs and tissues | Age (year) and gender (M/F) of phantoms | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 00 MF | 01 MF | 05 MF | 10 MF | 15 F | 15 M | Adult F | Adult M | ||
| Brain scan | Red bone marrow | 0.30 | 0.35 | 0.30 | 0.16 | 0.10 | 0.11 | 0.05 | 0.05 |
| Blood | 0.10 | 0.11 | 0.08 | 0.05 | 0.04 | 0.04 | 0.04 | 0.03 | |
| Lymphatic organs | 0.03 | 0.02 | 0.02 | 0.01 | 0.01 | 0.01 | 0.01 | 0.01 | |
| Outside hematopoietic tissue | 0.20 | 0.18 | 0.12 | 0.07 | 0.05 | 0.05 | 0.05 | 0.03 | |
| Lymphocyte | 0.17 | 0.17 | 0.11 | 0.07 | 0.05 | 0.05 | 0.04 | 0.03 | |
| Chest scan | Red bone marrow | 0.84 | 0.69 | 0.39 | 0.40 | 0.35 | 0.35 | 0.39 | 0.31 |
| Blood | 1.10 | 0.86 | 0.69 | 0.63 | 0.52 | 0.53 | 0.47 | 0.45 | |
| Lymphatic organs | 1.04 | 0.72 | 0.44 | 0.35 | 0.32 | 0.27 | 0.21 | 0.21 | |
| Outside hematopoietic tissue | 0.67 | 0.39 | 0.36 | 0.38 | 0.29 | 0.37 | 0.26 | 0.28 | |
| Lymphocyte | 0.74 | 0.44 | 0.37 | 0.38 | 0.29 | 0.36 | 0.27 | 0.27 | |
| Abdomen scan | Red bone marrow | 0.47 | 0.33 | 0.23 | 0.26 | 0.27 | 0.23 | 0.25 | 0.22 |
| Blood | 0.81 | 0.53 | 0.54 | 0.44 | 0.41 | 0.37 | 0.32 | 0.35 | |
| Lymphatic organs | 1.36 | 1.00 | 1.00 | 1.07 | 0.88 | 0.73 | 0.81 | 0.67 | |
| Outside hematopoietic tissue | 0.59 | 0.32 | 0.38 | 0.34 | 0.25 | 0.27 | 0.21 | 0.26 | |
| Lymphocyte | 0.71 | 0.40 | 0.45 | 0.40 | 0.30 | 0.31 | 0.25 | 0.28 | |
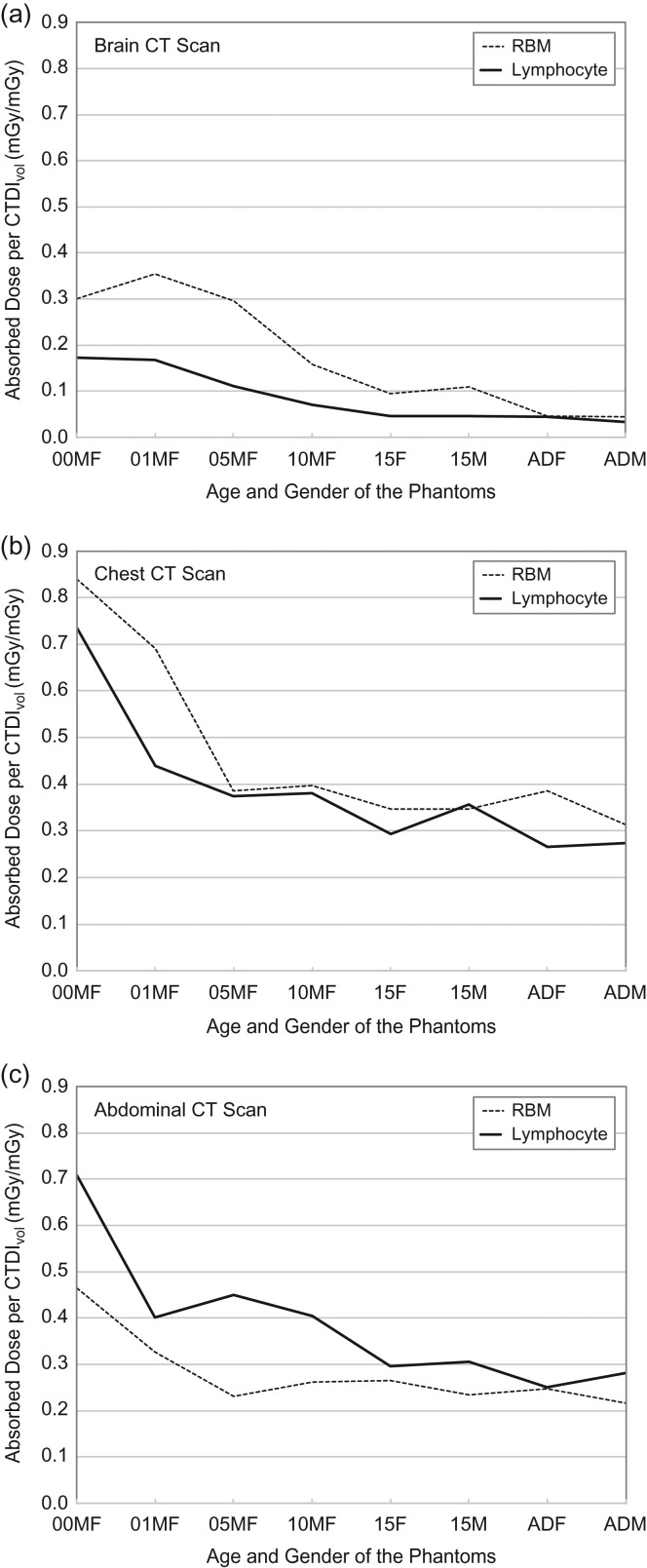
Figure 1 shows the comparison of age-dependent doses coefficients to the RBM, which is usually used as a surrogate for lymphocyte in epidemiological studies, versus overall lymphocyte dose for (a) brain, (b) chest and (c) abdomen scans. RBM dose coefficients overall overestimate lymphocyte dose coefficients except for abdomen scan. RBM dose coefficients are up to 2.6 (5-year old) and 1.6 (1-year old) times greater than lymphocyte dose in brain and chest scans, respectively. In contrast, RBM dose coefficients are about half the lymphocyte dose coefficients in the abdomen scan of 5-year-old phantoms.
Figure 1.
Comparison of age-dependent absorbed dose per CTDIvol (mGy/mGy) to red bone marrow (RBM) and lymphocyte in (a) brain, (b) chest and (c) abdominal CT scans.
Estimated age-dependent lymphocyte doses for the UK CT cohort are tabulated in Table 3 for the two time periods: before and after 2001. Lymphocyte doses (mGy) show different trends from the lymphocyte dose coefficients (Table 2) because the absolute dose was derived by multiplying the dose coefficients by the CTDIvol from the UK CT cohort. The lymphocyte doses from the newborn to 10-year old are identical between male and female because gender-specific organs (e.g. gonads and urinary bladder) contribute only 0.04% (male) and 0.02% (female)(7) of the blood dose, which again contributes to about 0.2% of the lymphocyte dose (Table 1). However, for both 15-year olds and adults, the male phantoms receive slightly greater dose than the female phantoms for torso CT scans because the volume ratio of muscle (more than 50% of the total body volume) is greater in the male phantoms than the female phantoms(7). T-spine and whole body scans deliver major lymphocyte doses, up to 22.4 mGy for newborns, which are followed by L-spine, abdomen, and chest scans that deliver 17.9, 12.7 and 12.5 mGy, respectively, in newborns before 2001. Similar to the trends in other organ doses that were reported by Kim et al.(17), the lymphocyte dose significantly decreased after 2001. The lymphocyte dose of newborn scanned for T-spine examinations decrease from 22.4 before 2001 to 5.9 mGy since 2001.
Table 3.
Lymphocyte dose (mGy) for the patients in the United Kingdom for different ages (newborn to 20 years old) and scan types in the two time periods (before and after 2001).
| Scan type | 0 MF | 1 MF | 5 MF | 10 MF | 15 F | 15 M | ADF | ADM |
|---|---|---|---|---|---|---|---|---|
| Before 2001 | ||||||||
| Brain | 8.9 | 8.6 | 5.7 | 3.6 | 2.4 | 2.4 | 2.3 | 1.7 |
| Partial brain | 4.7 | 5.5 | 4.4 | 2.7 | 1.9 | 1.9 | 1.9 | 1.4 |
| Facial bone | 8.7 | 7.0 | 5.1 | 3.5 | 2.5 | 2.9 | 2.6 | 2.3 |
| Neck | 7.1 | 7.1 | 5.4 | 4.3 | 3.0 | 3.5 | 3.4 | 2.9 |
| Chest | 12.5 | 7.5 | 6.4 | 6.5 | 5.0 | 6.1 | 4.5 | 4.7 |
| HRCT | 2.9 | 1.8 | 1.5 | 1.5 | 1.2 | 1.4 | 1.1 | 1.1 |
| Abdomen | 12.7 | 7.2 | 8.1 | 7.3 | 5.3 | 5.5 | 4.5 | 5.1 |
| Pelvis | 8.9 | 8.6 | 9.1 | 8.6 | 6.3 | 7.4 | 6.2 | 6.3 |
| Hip | 4.1 | 4.3 | 5.7 | 5.8 | 4.5 | 4.5 | 3.9 | 5.1 |
| C-spine | 4.3 | 5.5 | 4.2 | 3.6 | 2.5 | 3.2 | 2.9 | 2.5 |
| T-spine | 22.4 | 14.0 | 13.1 | 14.0 | 8.3 | 8.9 | 8.2 | 9.1 |
| L-spine | 17.9 | 11.3 | 14.0 | 13.0 | 10.5 | 12.3 | 9.0 | 9.6 |
| Shoulder | 7.4 | 5.4 | 5.8 | 7.0 | 5.7 | 6.3 | 4.7 | 4.3 |
| Whole body | 21.6 | 16.3 | 17.2 | 16.6 | 12.1 | 14.0 | 12.0 | 12.4 |
| Extremity | 7.0 | 5.2 | 10.1 | 9.9 | 9.6 | 10.5 | 9.1 | 9.5 |
| Unknown | 8.1 | 7.0 | 5.6 | 4.3 | 3.1 | 3.3 | 3.0 | 2.7 |
| After 2001 | ||||||||
| Brain | 4.3 | 4.2 | 3.8 | 3.1 | 2.6 | 2.6 | 2.5 | 1.8 |
| Partial brain | 1.9 | 2.2 | 2.4 | 1.9 | 1.7 | 1.7 | 1.7 | 1.2 |
| Facial bone | 3.9 | 3.2 | 3.2 | 2.8 | 2.5 | 2.9 | 2.6 | 2.3 |
| Neck | 1.3 | 1.4 | 1.0 | 1.0 | 0.5 | 0.6 | 1.2 | 1.0 |
| Chest | 4.1 | 2.4 | 2.1 | 2.7 | 1.4 | 1.8 | 2.7 | 2.7 |
| HRCT | 0.8 | 0.4 | 0.4 | 0.6 | 0.3 | 0.4 | 0.5 | 0.5 |
| Abdomen | 4.7 | 2.6 | 2.9 | 3.4 | 1.8 | 1.8 | 3.0 | 3.4 |
| Pelvis | 2.2 | 2.1 | 2.2 | 2.6 | 1.4 | 1.7 | 2.7 | 2.8 |
| Hip | 1.0 | 1.2 | 1.4 | 1.8 | 1.0 | 1.0 | 1.7 | 2.2 |
| C-spine | 1.2 | 1.5 | 1.2 | 1.3 | 0.6 | 0.8 | 1.4 | 1.2 |
| T-spine | 5.9 | 3.6 | 3.3 | 4.8 | 1.8 | 2.0 | 3.7 | 4.1 |
| L-spine | 4.6 | 2.8 | 3.5 | 4.1 | 2.4 | 2.8 | 4.0 | 4.2 |
| Shoulder | 1.4 | 1.0 | 1.1 | 1.6 | 1.0 | 1.1 | 1.6 | 1.5 |
| Whole body | 7.2 | 5.3 | 5.6 | 6.8 | 3.5 | 4.1 | 7.0 | 7.3 |
| Extremity | 1.9 | 1.4 | 2.8 | 3.5 | 2.3 | 2.5 | 4.3 | 4.5 |
| Unknown | 3.4 | 3.0 | 2.9 | 2.6 | 2.0 | 2.0 | 2.3 | 2.0 |
CONCLUSION
We developed a method to estimate dose to lymphocytes by using the reference distribution of lymphocytes throughout the body reported by the ICRP and Monte Carlo simulations of computational human phantoms. We applied the method to estimating lymphocyte doses for the UK CT patient cohort to enable evaluation of the association between lymphocyte doses and subsequent lymphoma risk. RBM dose coefficients are overall greater than lymphocyte dose for most scan types (up to 2.6 times for 5-year-old brain scan) except in the abdomen scan where RBM dose coefficients are about half the lymphocyte dose. The dosimetry method and lymphocyte dose coefficients can be used for other epidemiological investigations analyzing the risk of lymphoma following non-uniform exposures. Improved dosimetry is essential to help clarify whether lymphomas can be induced by ionizing radiation.
ACKNOWLEDGMENT
This study utilized the high-performance computational capabilities of the Biowulf computing system at the National Institutes of Health, Bethesda, MD (http://biowulf.nih.gov).
REFERENCES
- 1. Boice J. D. Jr et al.. Second cancers following radiation treatment for cervical cancer. An international collaboration among cancer registries. J. Natl. Cancer Inst. 74(5), 955 (1985). [PubMed] [Google Scholar]
- 2. Davis F. G., Boice J. D., Hrubec Z. and Monson R. R.. Cancer mortality in a radiation-exposed cohort of Massachusetts tuberculosis patients. Cancer Res. 49(21), 6130–6136 (1989). [PubMed] [Google Scholar]
- 3. Boice J. D., Morin M. M., Glass A. G., Friedman G. D., Stovall M., Hoover R. N. and Fraumeni J. F. Jr. Diagnostic X-ray procedures and risk of leukemia, lymphoma, and multiple myeloma. J. Am. Med. Assoc. 265(10), 1290–1294 (1991) doi:10.1001/jama.1991.03460100092031. [PubMed] [Google Scholar]
- 4. Leuraud K. et al.. Ionising radiation and risk of death from leukaemia and lymphoma in radiation-monitored workers (INWORKS): an international cohort study. Lancet Haematol. 2(7), e276–e281 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hsu W.-L. et al.. The incidence of leukemia, lymphoma and multiple myeloma among atomic bomb survivors: 1950–01. Radiat. Res. 179(3), 361–382 (2013) doi:10.1667/RR2892.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. ICRP.. Report on the task group on reference man. Ann. ICRP/ICRP Publication 23, 1–480 (1975). [DOI] [PubMed] [Google Scholar]
- 7. ICRP.. Basic anatomical and physiological data for use in radiological protection: reference values. Ann. ICRP 32(3–4), 1–277 (2002) ICRP publication 89. [PubMed] [Google Scholar]
- 8. Lee C., Lodwick D., Hurtado J., Pafundi D., Williams J. L. and Bolch W. E.. The UF family of reference hybrid phantoms for computational radiation dosimetry. Phys. Med. Biol. 55(2), 339–363 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. ICRP.. Human alimentary tract model for radiological protection. Ann. ICRP 36(1–2), 1–336 (2006) doi:10.1016/j.icrp.2006.03.004. ICRP Publication 100. [DOI] [PubMed] [Google Scholar]
- 10. ICRU.. Photon, Electron, Proton and Neutron Interaction Data for Body Tissues. Vol 46, Bethesda, MD: International Commission on Radiation Units and Measurements; ) (1992). [Google Scholar]
- 11. Pelowitz D. B. MCNPX User’s Manual Version 2.7.0 (Los Alamos National Laboratory; ) (2011). [Google Scholar]
- 12. Johnson P. B., Bahadori A. A., Eckerman K. F., Lee C. and Bolch W. E.. Response functions for computing absorbed dose to skeletal tissues from photon irradiation—an update. Phys. Med. Biol. 56, 2347 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lee C., Lamart S. and Moroz B. E.. Computational lymphatic node models in pediatric and adult hybrid phantoms for radiation dosimetry. Phys. Med. Biol. 58(5), N59–N82 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pearce M. S. et al.. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380(9840), 499–505 (2012) doi:10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lee C., Kim K. P., Bolch W. E., Moroz B. E. Folio Les. NCICT: a computational solution to estimate organ doses for pediatric and adult patients undergoing CT scans. J. Radiol. Prot. 35(4), 891–909 (2015) doi:10.1088/0952-4746/35/4/891. [DOI] [PubMed] [Google Scholar]
- 16. Bahadori A., Miglioretti D., Kruger R., Flynn M., Weinmann S., Smith-Bindman R. and Lee C.. Calculation of organ doses for a large number of patients undergoing CT examinations. Am. J. Roentgenol. 205(4), 827–833 (2015) doi:10.2214/AJR.14.14135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kim K. P., Berrington de Gonzalez A., Pearce M. S., Salotti J. A., Parker L., McHugh K., Craft A. W. and Lee C.. Development of a database of organ doses for paediatric and young adult CT scans in the United Kingdom. Radiat. Prot. Dosim. 150(4), 415–426 (2012) doi:10.1093/rpd/ncr429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shrimpton P. C., Hart D., Hillier M. C., Wall B. F., Le Heron J. C. and Faulkner K.. Survey of CT practice in the UK. Part 2: Dosimetric aspects. Natl. Radiol. Protect. Board 50, 165–172 (1991) doi:10.1016/S0969-8043(98)00024-4. [Google Scholar]
- 19. Shrimpton P. C., Hillier M. C., Lewis M. A. and Dunn M.. National survey of doses from CT in the UK: 2003. Br. J. Radiol. 79(948), 968–980 (2006) doi:10.1259/bjr/93277434. [DOI] [PubMed] [Google Scholar]
- 20. Lee C., Kim K. P., Long D. and Bolch W. E.. Organ doses for reference pediatric and adolescent patients undergoing computed tomography estimated by Monte Carlo simulation. Med. Phys. 39(4), 2129–2146 (2012) doi:10.1118/1.3693052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shrimpton P. C., Hillier M. C., Lewis M. A. and Dunn M.. Doses From Computed Tomography (CT) Examinations in the UK-2003 Review (Chilton: NRPB; ) pp. 1–93 (2005). [Google Scholar]
- 22. Galanski M., Nagel H. D. and Stamm G.. Paediatric CT exposure practice in the federal republic of germany: results of a nation-wide survey in 2005/06. 2005:56.
- 23. Hollingsworth C., Frush D. P., Cross M. and Lucaya J.. Helical CT of the body: a survey of techniques used for pediatric patients. Am. J. Roentgenol. 180(2), 401–406 (2003) doi:10.2214/ajr.180.2.1800401. [DOI] [PubMed] [Google Scholar]