Abstract
AIM:
The purpose of the paper was to assess job demands, burnout, and teamwork in healthcare professionals (HPs) working in a general hospital that was analysed at two points in time with a time lag of three years.
METHODS:
Time 1 respondents (N = 325) were HPs who participated during the first wave of data collection (2011). Time 2 respondents (N = 197) were HPs from the same hospital who responded at Time 2 (2014). Job demands, burnout, and teamwork were measured with Hospital Experience Scale, Maslach Burnout Inventory, and Hospital Survey on Patient Safety Culture, respectively.
RESULTS:
Significantly higher scores of emotional exhaustion (21.03 vs. 15.37, t = 5.1, p < 0.001), depersonalization (4.48 vs. 2.75, t = 3.8, p < 0.001), as well as organizational (2.51 vs. 2.34, t = 2.38, p = 0.017), emotional (2.46 vs. 2.25, t = 3.68, p < 0.001), and cognitive (2.82 vs. 2.64, t = 2.68, p = 0.008) job demands were found at Time 2. Teamwork levels were similar at both points in time (Time 1 = 3.84 vs. Time 2 = 3.84, t = 0.043, p = 0.97).
CONCLUSION:
Actual longitudinal study revealed significantly higher mean values of emotional exhaustion and depersonalization in 2014 that could be explained by significantly increased job demands between analysed points in time.
Keywords: Job demands, Burnout, Teamwork, Longitudinal study, Healthcare professionals
Introduction
Burnout is most often analysed as a psychological syndrome, resulting from exposure to chronic emotional and interpersonal workplace stressors [1] [2] [3]. This syndrome is represented by three dimensions - emotional exhaustion (an overwhelming exhaustion, as well as feelings of being overextended by the demands of the job and depleted of one’s emotional and physical resources), depersonalization or cynicism (a negative, callous, or excessively detached response to various aspects of the job, as well as cynical response to the recipients of care), and reduced personal accomplishment (feelings of incompetence and a lack of achievement and productivity at work) [3]. Since reduced personal accomplishment correlates weakly with both emotional exhaustion and depersonalization and with detected burnout correlates [4] [5], recent studies focused mostly on emotional exhaustion and depersonalization [6] [7] [8].
It is clearly shown that workplace stress and burnout are important issues for a wide range of occupations. For example, the teaching profession is becoming more and more stressful due to increased responsibilities and demanding deadlines [9] [10] [11]. Healthcare professionals (HPs), while providing healthcare services to the patients, are exposed to different psychosocial hazards that originate from the workplace demands and conditions [12] [13]. These hazards are particularly detrimental when requirements of the work do not match the capabilities, resources or needs of the worker [14]. Hospital HPs in everyday practice is dealing with different physical (e.g., responsibility for too many patients, very fast work), social, emotional, cognitive, and organisational factors (job demands) that require prolonged physical and/or psychological (cognitive and emotional) efforts. Job demands are associated with certain physiological and/or psychological costs in workers (leading to overtaxing and emotional exhaustion) when the invested personal efforts are high [3] [6] [15] [16].
On the other hand, job resources represent those aspects of the job that reduce both job demands and changes in workers related to the job demands. Additionally, job resources help workers in achieving work goals; they stimulate personal growth, learning and development of employees [15]. Job resources are present at the organizational (e.g., good salary, job security) or interpersonal (e.g., teamwork, supervisor and co-worker support) level, at the specific job position (e.g., participation in decision making), and at the level of the task (e.g., autonomy, performance feedback) [16].
According to the job demands/resources model of stress (JD - R model), burnout develops through two types of psychological processes: demanding aspects of work (high job demands) resulting in overtaxing and exhaustion (energetic process); and lack of resources leading to withdrawal behaviour (depersonalization) and disengagement (motivational process) [6] [16]. When the organizational context is represented by adequate job resources, such as proper feedback, adequate supervisor and co-worker support, and appropriate teamwork, in employees could be detected high levels of job engagement as well as low levels of depersonalization. On the contrary, in the context of reduced job resources (e.g., inappropriate performance feedback, low salary, job insecurity, inadequate supervisory coaching and teamwork), job demands are particularly effective and detrimental [6] [16] [17].
Teamwork, as a particular job resource, is a specific cooperative process between team members that allows them to develop effective, mutual relationships in achieving team goals through sharing knowledge and skills [18] [19]. Teamwork is an extremely important resource in hospital settings, and HPs are coordinating their activities to deliver healthcare services to the patients that should be safe, effective, patient - centred, timely, efficient, and equitable [20]. Also, teamwork could protect workers from emotional exhaustion, depersonalization, and disengagement [15]. However, research in this field has demonstrated that teamwork had stronger effects on the relationship job engagement - job satisfaction than on the relationship job demands - burnout. Those findings support theoretical and empirical data about the existence of two psychological processes: 1. energetic process, in which job demands lead to poor health via burnout, and 2. motivational process, in which job resources result in higher job satisfaction via job engagement [15] [21] with job resources having weaker effect on the relationship job demands - burnout.
Despite numerous studies on burnout in HPs, either cross-sectional or longitudinal [22] [23] [24] [25] [26] [27], mainly analysing its predictors and consequences, to date there is poor pool of data in the region of South - East Europe (SEE) on changes in burnout levels over time. In this study we analysed HPs working in a general hospital in Skopje, Macedonia that is an educational base of the Faculty of Medicine in Skopje, providing health care to the general population at secondary and tertiary level.
The health care system in the Republic of Macedonia faces continuous reforms oriented towards improvement of safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity of patient care, as the key attributes of high quality health care [28] [29]. Within aforementioned reforms, followed by reorganisation of hospital settings, HPs from the study hospital are referring increased job demands (ex., significantly increased number of patients served, low salaries of HPs, complex administrative requirements, etc.) [28]. On the other hand, previous qualitative and quantitative studies [28] [29] [30] demonstrated protective workplace factors (job resources) within analysed hospital context (ex., appropriate working conditions, support from superiors and co-workers, teamwork, independence in decision - making, excellent interpersonal relationships, etc.). But, although hospital management continued to implement good organizational and management standards, high level of discipline, teamwork, good communication between team members, HPs working in this hospital still complain about the listed job demands.
The actual paper analyses the concepts of job demands, burnout, and teamwork taking into consideration the national context and specifics of the hospital in focus. The purpose of the present study was to assess job demands, burnout, and teamwork in HPs working in a general hospital that was analysed at two points in time with a time lag of three years.
Methods
The study was conducted in a general teaching hospital from Skopje, Macedonia, an educational base of the Faculty of Medicine. The most important criteria for selecting the hospital were to have stable management and to represent the most typical hospital organisational system, providing inpatient and outpatient (specialist healthcare with specialist diagnostics) health care and laboratory tests. The total number of employees in the hospital in 2011 was about 420, and it had about 500 beds. Before the research, ethical approval was obtained by the hospital’s ethics committee.
The research design included two cross-sectional studies. The hospital employees were studied at two points in time during hospital reorganisations that were conducted in line with country health care reforms. The reforms were followed by higher job demands in HPs, represented mainly by the increased workload, increased number of patients served, and complex administration procedures. The surveys were performed at two points in time (2011 and 2014) with a time lag of three years. On both occasions, the hard copies of the questionnaires together with a letter explaining the objectives of the study and assuring participants’ anonymity and confidentiality were distributed in envelopes to all HPs working in the Hospital. Questionnaires were returned anonymously in sealed envelopes to protect participants’ privacy. Participation in the study was voluntary.
Participants were HPs working in general hospital that was subject to analysis. Time 1 respondents (N = 325) were those who participated during the first wave of data collection (2011) and who had completed the questionnaires. Time 2 respondents (N = 197) were HPs from the same hospital who responded at Time 2 (2014) and who had also completed the questionnaires. Job demands, burnout, and teamwork were measured with Hospital Experience Scale, Maslach Burnout Inventory, and Hospital Survey on Patient Safety Culture, respectively.
Hospital Experience Scale (HES), which was constructed and developed for FP7 ORCAB Project (http://orcab.web.auth.gr/), was applied for the assessment of job demands within the actual study. The items were categorised into four subscales: physical workload (seven items, e.g., I am responsible for too many patients in hospital rounds), organisational (six items, e.g., The roles in my department are not clear/ambiguous), emotional (six items, e.g., I have to deal with verbally abusive patients) and cognitive (five items, e.g., I have to make decisions when I don’t have all the information I need) job demands. Participants indicated their level of agreement with the items on a 5 - point Likert scale (1 = never to 5 = always), and points for statements relating to each of the job demands types were averaged to derive the four types of job demands. The higher mean score means, the higher perceived level of particular job demands type.
Burnout was examined with the Maslach Burnout Inventory (MBI) [3]. Emotional exhaustion (nine items) and depersonalisation (five items) subscales were applied and measured using a 7 -point Likert scale (0 = never to 6 every day). Emotional exhaustion refers to the feelings of overwhelming exhaustion, lack of energy and depletion of emotional resources and the person feels used up. Depersonalization is the interpersonal dimension of burnout that refers to the feelings of frustration, anger, and cynicism. It is described as an excessively detached response to other people. Emotional exhaustion was assessed through items such as “I feel emotionally drained from my work” and “I feel burned out by my work”, and depersonalization with items such as “I feel I treat some patients as if they were impersonal objects”. Responses are added to form a score for each subscale, thus giving each participant scores for the two components of burnout. The higher the score in one dimension delineates the higher level of burnout.
Teamwork (four items, e.g., when one area in this unit gets busy, others help out) was measured with the Hospital Survey on Patient Safety Culture, developed by the US Agency for Healthcare Research and Quality (http://www.ahrq.gov/qual/patientsafetyculture/hospcult1.htm). Participants indicated the level of agreement with the items (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree) and the mean score was calculated. The higher mean score represents a higher level of perceived teamwork.
To keep participants’ anonymity and confidentiality, the questionnaires were returned anonymously in sealed envelopes and data were made completely anonymous before being analysed and published. Therefore, there was no possibility to follow one person from one point of time to the next. Afterwards, data were analysed as if they were independent.
Independent samples t-test was used to compare data obtained at two points in time (2011 and 2014). Pearson’s correlation coefficients were calculated to examine relationships between continuous variables (burnout dimensions, different types of job demands, and teamwork). P values < 0.05 were considered statistically significant, and the main results are given with 95% confidence intervals (CI). The Statistical Package for the Social Sciences (SPSS) statistics (Chicago USA 2011, version 20) was used for the statistical analyses.
Results
Completed surveys were returned by 325 HPs (70.2% females, 29.8% males) at Time 1. Participants had an average age of 38.12 (SD = 10.58) years, and they worked for an average of 130.55 (SD = 121.01) months at the same hospital and 105.18 (SD = 106.03) months within the same unit. They worked for an average of 42.14 (SD = 11.21) hours per week.
At Time 2, 197 HPs (79.9% females, 20.1% males) returned completed surveys. They had an average age of 42.36 (SD = 9.29) years, and they worked for an average of 157.3 (SD = 115.27) months at the same hospital and 115.25 (SD = 108.19) months within the same unit. They worked for an average of 43.73 (SD = 8.41) hours per week. Similar frequencies of participants were married or lived together with their partner and reported full - time contract as a type of employment at Time 1 and Time 2.
Means, standard deviations, internal consistency coefficients (i.e., Cronbach’s alphas), and correlation coefficients of analysed variables at Time 1 and Time 2 are presented in Table 1.
Table 1.
Means, standard deviations, internal consistency coefficients (i.e., Cronbach’s alphas), and correlation coefficients of variables in Time 1 and Time 2
| Variable | Mean | St. dev. | α | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|---|---|
| Time 1 | |||||||||
| 1. Emotional Exhaustion | 15.37 | 11.46 | 0.88 | / | |||||
| 2. Depersonalization | 2.75 | 4.3 | 0.75 | 0.623** | / | ||||
| 3. Job demands Physical demands | 3.29 | 0.67 | 0.71 | 0.283** | 0.146** | / | |||
| 4. Job demands Organizational demands | 2.34 | 0.77 | 0.78 | 0.229** | 0.21** | 0.431** | / | ||
| 5. Job demands Emotional demands | 2.25 | 0.61 | 0.75 | 0.285** | 0.263** | 0.367** | 0.58** | / | |
| 6. Job demands Cognitive demands | 2.64 | 0.71 | 0.71 | 0.27** | 0.161** | 0.422** | 0.502** | 0.449** | / |
| 7. Teamwork | 3.84 | 0.79 | 0.84 | -0.249** | -0.25** | -0.161** | -0.435** | -0.291** | -0.206** |
| Time 2 | |||||||||
| 1. Emotional Exhaustion | 21.03 | 12.78 | 0.91 | / | |||||
| 2. Depersonalization | 4.48 | 5.42 | 0.78 | 0.639** | / | ||||
| 3. Job demands Physical demands | 3.3 | 0.64 | 0.73 | 0.379** | 0.315** | / | |||
| 4. Job demands Organizational demands | 2.51 | 0.73 | 0.72 | 0.342** | 0.346** | 0.362** | / | ||
| 5. Job demands Emotional demands | 2.46 | 0.65 | 0.75 | 0.293** | 0.306** | 0.355** | 0.605** | / | |
| 6. Job demands Cognitive demands | 2.82 | 0.73 | 0.72 | 0.221** | 0.245** | 0.309** | 0.586** | 0.546** | / |
| 7. Teamwork | 3.84 | 0.86 | 0.91 | -0.182** | -0.173* | -0.163* | -0.28** | -0.172* | -0.23** |
** Correlation is significant at the 0.01 level (2 - tailed); * Correlation is significant at the 0.05 level (2 - tailed); Note. First row numbers (1 - 6) indicate the same respective; variables as shown in the first column (eg., 1. Emotional Exhaustion, 2. Depersonalization, 3. Job demands - Physical demands etc.)
The reliability of the scales at both Time 1 and Time 2 was above 0.7 which was adequate for further statistical analyses. Using bivariate analyses, we found significant positive correlations of burnout dimensions with all job demands types at both times. On the other hand, teamwork was negatively correlated with both burnout dimensions and all types of job demands at Time 1 and Time 2 (see Table 1). Figure 1 and Figure 2 show mean emotional exhaustion and depersonalization scores in 2011 and 2014.
Figure 1.
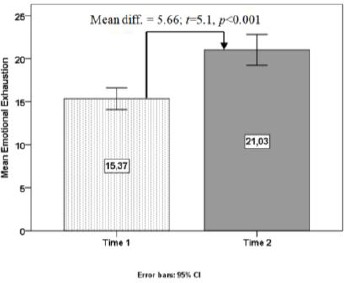
Mean emotional exhaustion scores in 2011 (Time 1) and 2014 (Time 2)
Figure 2.
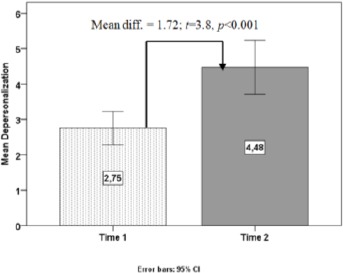
Mean depersonalization scores in 2011 (Time 1) and 2014 (Time 2)
Figure 1 and Figure 2 data demonstrate that significantly higher scores of emotional exhaustion (21.03 vs. 15.37, Mean diff. = 5.66, t = 5.1, p < 0.001) and depersonalization (4.48 vs. 2.75, Mean diff. = 1.72, t = 3.8, p < 0.001) were detected at Time 2 (2014).
Descriptive statistics of job demands and teamwork and differences between 2011 (Time 1) and 2014 (Time 2) are shown in Table 2.
Table 2.
Descriptive statistics of job demands and teamwork and differences between 2011 (Time 1) and 2014 (Time 2)
| Mean | SD | t | Mean diff. (95% CI) | p | ||
|---|---|---|---|---|---|---|
| Job demands - Physical demands | 2011 | 3.29 | 0.67 | -0.043 | 0.003 (-0.11, 0.12) | 0.965 |
| 2014 | 3.3 | 0.64 | ||||
| Job demands - Organizational demands | 2011 | 2.34 | 0.77 | -2.38 | -0.16 (-0.3, -0.03) | 0.017 |
| 2014 | 2.51 | 0.73 | ||||
| Job demands - Emotional demands | 2011 | 2.25 | 0.61 | -3.68 | -0.21 (-0.32, -0.1) | <0.001 |
| 2014 | 2.46 | 0.65 | ||||
| Job demands - Cognitive demands | 2011 | 2.64 | 0.71 | -2.68 | -0.17 (-0.3, -0.07) | 0.008 |
| 2014 | 2.82 | 0.73 | ||||
| Teamwork | 2011 | 3.84 | 0.79 | 0.043 | 0.003 (-0.14, 0.15) | 0.965 |
| 2014 | 3.84 | 0.86 |
The data obtained represent significantly higher scores of organizational (2.51 vs. 2.34, Mean diff. = 0.16, t = 2.38, p = 0.017), emotional (2.46 vs. 2.25, Mean diff. = 0.21, t = 3.68, p < 0.001), and cognitive (2.82 vs. 2.64, Mean diff. = 0.17, t = 2.68, p=0.008) job demands at Time 2. Despite aforementioned significant differences, teamwork levels were similar at both points in time (Time 1 = 3.84 vs. Time 2 = 3.84, Mean diff. = 0.003, t = 0.043, p = 0.97) (see Table 2).
Discussion
Emotional exhaustion (15.37) and depersonalization (2.75) mean scores in 2011 within the actual study were lower than it was found in previous studies analysing burnout in hospital HPs. For example, Vahey DC et al. registered an average score of emotional exhaustion - 24.3 and an average score of depersonalization - 7.4 in nurses from 40 units in 20 urban hospitals across the United States [31]. Similarly, low mean values of both burnout dimensions were also registered in HPs in other studies conducted in R. Macedonia [29][30][32][33]. In a study conducted in HPs from seven South and South - Eastern European countries, adopting a cross-national approach, Macedonian HPs demonstrated levels of emotional exhaustion (EE) and depersonalization (DP) in the lower end of the average EE and DP scores [34].
On the other hand, job demands in 2011 showed medium level (physical - 3.29, organisational - 2.34, emotional - 2.25, and cognitive - 2.64 job demands) with the relatively high level of perceived teamwork - 3.84. The average score of teamwork with the added value of the standard deviation - 0.79 becomes over 4.5, the level that demonstrates teamwork as a significant protective factor within analysed hospital, taking into consideration that teamwork is found to be one of the most important job resources, together with good interpersonal relationships, support from superiors, adequate feedback, and independence in decision making.
The implementation of JD - R Model within analysed hospital context in 2011, references to both medium level job demands and high level teamwork that could boost the compensatory efforts in HPs in order to maintain high level of performance (high job engagement) and to reduce physiological and psychological costs in HPs associated with their work efforts (low exhaustion and depersonalization) [16]. Indeed, job demands may lead to the depletion of energy (emotional exhaustion), but in our case job resources (e.g., high level of teamwork) with their protective and motivational potential have led to low levels of exhaustion and depersonalization. The protective function of teamwork was demonstrated elsewhere. Different studies have shown that teamwork predicted lower levels of burnout. The more that HPs experienced teamwork, the less they felt burnt out [15] [17] [32].
To our knowledge, similar studies analysing changes in burnout levels over time in the SEE Region are very rare. The present study was aimed to assess job demands, burnout, and teamwork in HPs, working in a general hospital, at two points in time (2011 and 2014). We have found that both burnout dimensions were positively correlated with all types of job demands, while teamwork was negatively correlated with burnout dimensions and job demands at both occasions (2011 and 2014). Similarly to our findings, studies have shown that HPs who perceive their job demands as reasonable and who have more support from colleagues (higher levels of teamwork) have higher levels of psychological well - being [35]. Additionally, equivalent results of bivariate analyses were also registered in other studies conducted in R. Macedonia [29] [30].
The actual study demonstrated that in 2014, the mean values of emotional exhaustion and depersonalization were significantly higher than in 2011. This increase in emotional exhaustion and depersonalization levels between 2011 and 2014 has to be explained in a hospital context where job demands also significantly increased between analysed points in time, while perceived teamwork levels remained relatively high and constant from 2011 until 2014. Namely, our data suggested that in HPs, in the period between 2011 and 2014, the feelings of more strict hierarchy in the hospital, ambiguous roles, and problematic communication have become more intense, they became more concerned about the negative influence of media on the work of HPs, together with an increase in emotional (e.g., emotional involvement in work, dealing with verbally abusive patients) and cognitive (e.g., inadequate feedback, time pressures) job demands.
According to the JD - R model, demanding aspects of work (high job demands) as well as involvement in jobs with chronic job demands (either work overload or emotional demands or others) exhaust employees’ mental and physical resources and may, therefore, lead to the depletion of energy [16]. It was scientifically proven that these job demands predict overtaxing and exhaustion in workers. Additionally, in Macedonian context, it was detected that ageing of HPs positively predicted both emotional exhaustion and depersonalization [30]. Having in mind this knowledge, we further performed bivariate analyses between burnout dimensions and age within the actual study. These analyses showed a positive correlation of both burnout dimensions with an age of HPs in either 2011 or 2014, meaning that the older HPs experienced more emotional exhaustion and depersonalization. Therefore, higher burnout scores in 2014 than in 2011 could be a result not only of higher job demands but also an effect of the ageing of HPs.
The other component of JD - R model, besides job demands, is job resources. Hospital context is, usually, characterised by one of the most important job resources, defined as teamwork. It is well established that teamwork could protect workers from emotional exhaustion, depersonalization, and disengagement [15]. Research has shown that teamwork demonstrated a buffering effect (i.e., increasing the teamwork would decrease either the effect of the job demands on burnout or the effect of age on burnout) [30].
Since the level of perceived teamwork was constantly high between 2011 and 2014 (over 4.5, together with the added value of the standard deviation), we expected that the high level of this job resource would boost the compensatory efforts in HPs to reduce exhaustion and depersonalization. However, the levels of burnout significantly increased from 2011 to 2014. These findings could be explained the results of mediation and moderation analyses showing that teamwork had stronger effects on the relationship job engagement - job satisfaction than on the relationship job demands - burnout [32]. In other words, in the analysed hospital context, teamwork has failed to decrease the effect of the job demands on burnout. Finally, this study again confirms the existence of two processes in the psychosocial functioning of workers: 1. Energetic process (job demands - burnout - poor health), and 2. Motivational process (job resources - job engagement - job satisfaction) [15] [21].
Findings of the actual study should be interpreted with caution as answering bias could rise because it is possible that more affected HPs tended to answer. Also, a “healthy worker effect” may have underestimated the levels of burnout. Additional limitations also include the fact that the analyses were based on self - reporting from questionnaires.
As a conclusion, this study shows differences in job demands and burnout in HPs working in a general hospital that was analysed at two points in time with a time lag of three years. In 2011, emotional exhaustion and average depersonalization scores were lower than it was found in previous studies analysing burnout in hospital HPs. On the other hand, job demands in 2011 showed medium level, while teamwork demonstrated relatively high level. The actual study revealed significantly higher mean values of emotional exhaustion and depersonalization in 2014 that could be explained by significantly increased job demands between analysed points in time. The perceived teamwork levels remained relatively high and constant from 2011 until 2014. Although, scientific data demonstrated that teamwork negatively predicted burnout and it can boost compensatory efforts in HPs to reduce exhaustion and depersonalise zation, this study supports the findings that teamwork had stronger effects on the relationship job engagement - job satisfaction than on the relationship job demands - burnout.
Obtained data can be used in the implementation of specific organisational interventions in the hospital setting through providing adequate JD - R interaction to prevent burnout in HPs. The interventions should be guided by the findings that job demands have a key role in the increase of exhaustion and depersonalization levels over time. The most importantly, this study highlights the importance of job demands in burnout development, even in the context when teamwork has constantly high levels. Specific strategies should be implemented in the hospital towards minimising competitiveness between colleagues, giving clear roles to workers, improvement of communication, giving adequate feedback about completed workplace tasks, and lowering time pressures. Further keeping the teamwork on high levels can be used towards the improvement of job engagement, job satisfaction, as well as good health and well - being in HPs since it has effects on the energetic and motivational psychosocial processes.
Physical job demands should not be overlooked since there level over time was constantly higher than the levels of other job demands. Reducing workload and time pressure through new employment as well as by purchasing new medical equipment and other supplies should be taken into account. Raising awareness in policymakers and key stakeholders should be strengthened. Finally, it should be stressed that providing adequate job demands-resources interaction can lead to the prevention of job burnout in HPs, as well as to improve the quality of care for the final consumers, or patients.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Maslach C, Leiter MP. The truth about burnout. San Francisco, CA: Jossey-Bass; 1997. PMid:9332965. [Google Scholar]
- 2.Leiter MP, Maslach C. Burnout and health. In: Baum A, Revenson T, Singer J, editors. Handbook of health psychology. Hillsdale, NJ: Lawrence Earlbaum; 2000. Retrieved from http://cord.acadiau.ca/publications.html . PMCid: PMC310941. [Google Scholar]
- 3.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. https://doi.org/10.1146/annurev.psych.52.1.397. PMid:11148311. [DOI] [PubMed] [Google Scholar]
- 4.Cordes C, Dougherty T. A review and integration of research on job burnout. Acad Manage Rev. 1993;18:621–659. [Google Scholar]
- 5.Kalliath TJ, O'Driscoll MP, Gillespie DE, Bluedom AC. A test of the Maslach Burnout Inventory in three samples of healthcare professionals. Work & Stress. 2000;14:35–50. https://doi.org/10.1080/026783700417212. [Google Scholar]
- 6.Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86:499–512. https://doi.org/10.1037/0021-9010.86.3.499. PMid:11419809. [PubMed] [Google Scholar]
- 7.Maslach C, Leiter MP. Early predictors of job burnout and engagement. J Appl Psychol. 2008;93:498–512. doi: 10.1037/0021-9010.93.3.498. https://doi.org/10.1037/0021-9010.93.3.498. PMid:18457483. [DOI] [PubMed] [Google Scholar]
- 8.Purvanova RK, Muros JP. Gender differences in burnout: A meta-analysis. J Vocat Behav. 2010;77:168–185. https://doi.org/10.1016/j.jvb.2010.04.006. [Google Scholar]
- 9.Hepburn A, Brown S. Teacher stress and management of accountability. Human Relations. 2001;54(6):691–715. https://doi.org/10.1177/0018726701546001. [Google Scholar]
- 10.Kyriacou C. Teacher stress and burnout: An international review. Educational Research. 1987;29:145–152. https://doi.org/10.1080/0013188870290207. [Google Scholar]
- 11.Cooper CL. Life at the Chalkface - Identifying and measuring teacher stress. Br J Educ Psychol. 1995;65(1):69–71. doi: 10.1111/j.2044-8279.1995.tb01131.x. https://doi.org/10.1111/j.2044-8279.1995.tb01131.x. PMid:7727268. [DOI] [PubMed] [Google Scholar]
- 12.International Labour Organization International Occupational Safety and Health Information Centre. Hazard datasheets on occupations (HDO) Geneva, Switzerland: International Labour Organization (ILO), International Occupational Safety and Health Information Centre (CIS); 2000. [Accessed August 22 2017]. http://www.ilo.org/ Page reviewed 2012. Page updated 2014. [Google Scholar]
- 13.National Institute for Occupational Safety and Health. CDC resources page. Centers for Disease Control and Prevention Web site. Healthcare workers. [Accessed August 22, 2017]. http://www.cdc.gov/niosh/topics/healthcare/ Page reviewed January 13 2017; Page updated May 14 2017.
- 14.National Institute for Occupational Safety and Health. Stress at work (DHHS [NIOSH] publication no. 99-101) Cincinnati, OH: National Institute for Occupational Safety and Health; 1999. [Google Scholar]
- 15.Schaufeli WB, Bakker AB. Job demands, job resources, and their relationship with burnout and engagement: a multi-sample study. J Organiz Behav. 2004;25:293–315. https://doi.org/10.1002/job.248. [Google Scholar]
- 16.Demerouti E, Bakker A. The Job demands-resources model: Challenges for future research. SA Journal of Industrial Psychology. 2011;37(2):1–9. https://doi.org/10.4102/sajip.v37i2.974. [Google Scholar]
- 17.Schaufeli WB, Bakker AB, Van Rhenen W. How changes in job demands and resources predict burnout, work engagement, and sickness absenteeism. J Organ Behav. 2009;30:893–917. https://doi.org/10.1002/job.595. [Google Scholar]
- 18.Scarnati JT. On becoming a team player. Team Performance Management: An International Journal. 2001;7(1/2):5–10. https://doi.org/10.1108/13527590110389501. [Google Scholar]
- 19.Harris PR, Harris KG. Managing effectively through teams. Team Performance Management: An International Journal. 1996;2(3):23–36. https://doi.org/10.1108/13527599610126247. [Google Scholar]
- 20.Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Serv Res. 2006;41(4 Pt 2):1576–1598. doi: 10.1111/j.1475-6773.2006.00566.x. https://doi.org/10.1111/j.1475-6773.2006.00566.x. PMid:16898980. PMCid: PMC1955345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schaufeli WB, Bakker AB. Werk en welbevinden: Naar een positieve benadering in de Arbeidsen Gezondheidspsychologie (Work and well-being: Towards a positive occupational health psychology) Gedrag & Organisatie. 2001;14:229–253. [Google Scholar]
- 22.Nordang K, Hall-Lord ML, Farup PG. Burnout in health-care professionals during reorganizations and downsizing. A cohort study in nurses. BMC Nursing. 2010;9:8. doi: 10.1186/1472-6955-9-8. https://doi.org/10.1186/1472-6955-9-8. PMid:20525338. PMCid: PMC2900247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McManus IC, Winder BC, Gordon D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet. 2002;359:2089–2090. doi: 10.1016/s0140-6736(02)08915-8. https://doi.org/10.1016/S0140-6736(02)08915-8. [DOI] [PubMed] [Google Scholar]
- 24.Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. 2007;13(5):482–488. doi: 10.1097/MCC.0b013e3282efd28a. https://doi.org/10.1097/MCC.0b013e3282efd28a. PMid:17762223. [DOI] [PubMed] [Google Scholar]
- 25.Innstrand ST, Langballe EM, Espnes GA, Falkum E, Aasland OG. Positive and negative work–family interaction and burnout: A longitudinal study of reciprocal relations. Work & Stress. 2008;22(1):1–15. https://doi.org/10.1080/02678370801975842. [Google Scholar]
- 26.Kim H, Ji J, Kao D. Burnout and Physical Health among Social Workers: A Three-Year Longitudinal Study. Social Work. 2011;56(3):258–268. doi: 10.1093/sw/56.3.258. https://doi.org/10.1093/sw/56.3.258. PMid:21848090. [DOI] [PubMed] [Google Scholar]
- 27.Rouleau D, Fournier P, Philibert A, Mbengue B, Dumont A. The effects of midwives'job satisfaction on burnout, intention to quit and turnover: a longitudinal study in Senegal. Hum Resour Health. 2012;10:9. doi: 10.1186/1478-4491-10-9. https://doi.org/10.1186/1478-4491-10-9. PMid:22546053. PMCid: PMC3444355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karadzinska-Bislimovska J, Basarovska V, Mijakoski D, Minov J, Stoleski S, Angeleska N, Atanasovska A. Linkages between workplace stressors and quality of care from health professionals'perspective - Macedonian experience. Br J Health Psychol. 2014;19(2):425–41. doi: 10.1111/bjhp.12040. https://doi.org/10.1111/bjhp.12040. PMid:23480487. [DOI] [PubMed] [Google Scholar]
- 29.Mijakoski D, Karadzinska-Bislimovska J, Basarovska V, Montgomery A, Panagopoulou E, Stoleski S, Minov J. Burnout, Engagement, and Organizational Culture: Differences between Physicians and Nurses. Open Access Maced J Med Sci. 2015;3(3):506–513. doi: 10.3889/oamjms.2015.091. https://doi.org/10.3889/oamjms.2015.091. PMid:27275279. PMCid: PMC4877848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mijakoski D, Karadzinska-Bislimovska J, Milosevic M, Mustajbegovic J, Stoleski S, Minov J. Differences in burnout, work demands and team work between Croatian and Macedonian hospital nurses. Cognition, Brain, Behavior. 2015;19(3):179–200. [Google Scholar]
- 31.Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Med Care. 2004;42(2):II57–II66. doi: 10.1097/01.mlr.0000109126.50398.5a. https://doi.org/10.1097/01.mlr.0000109126.50398.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mijakoski D, Karadzinska-Bislimovska J, Basarovska V, Minov J, Stoleski S, Angeleska N, Atanasovska A. Work demands-burnout and job engagement-job satisfaction relationships: teamwork as a mediator and moderator. Open Access Maced J Med Sci. 2015;3(1):176–183. doi: 10.3889/oamjms.2015.024. https://doi.org/10.3889/oamjms.2015.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mijakoski D, Karadzinska-Bislimovska J, Basarovska V, Stoleski S, Minov J. Burnout and work demands predict reduced job satisfaction in health professionals working in a surgery clinic. Open Access Maced J Med Sci. 2015;15(3(1)):166–173. doi: 10.3889/oamjms.2015.020. https://doi.org/10.3889/oamjms.2015.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alexandrova-Karamanova A, Todorova I, Montgomery A, et al. Burnout and health behaviors in health professionals from seven European countries. Int Arch Occup Environ Health. 2016;89(7):1059–1075. doi: 10.1007/s00420-016-1143-5. https://doi.org/10.1007/s00420-016-1143-5. PMid:27251338. [DOI] [PubMed] [Google Scholar]
- 35.Freeborn DK. Satisfaction, commitment, and psychological well-being among HMO physicians. West J Med. 2001;174(1):13–8. doi: 10.1136/ewjm.174.1.13. https://doi.org/10.1136/ewjm.174.1.13. PMid:11154654. PMCid: PMC1071220. [DOI] [PMC free article] [PubMed] [Google Scholar]


