Abstract
The hospital setting creates a high-stakes environment where patients’ lives depend on accurate tracking of health data. Despite recent work emphasizing the importance of patients’ engagement in their own health care, less is known about how patients track their health and care in the hospital. Through interviews and design probes, we investigated hospitalized patients’ tracking activity and analyzed our results using the stage-based personal informatics model. We used this model to understand how to support the tracking needs of hospitalized patients at each stage. In this paper, we discuss hospitalized patients’ needs for collaboratively tracking their health with their care team. We suggest future extensions of the stage-based model to accommodate collaborative tracking situations, such as hospitals, where data is collected, analyzed, and acted on by multiple people. Our findings uncover new directions for HCI research and highlight ways to support patients in tracking their care and improving patient safety.
Keywords: Health informatics, personal informatics, self-tracking, patient-clinician collaboration, hospital, patient engagement, patient safety
ACM Classification: J.3 Life and Medical Sciences, Health, Medical Information Systems, H.5.m. Information interfaces and presentation
INTRODUCTION
The hospital setting creates a high-stakes environment where patients’ lives depend on data. Traditionally clinicians are the only actors who collect, track, and reflect on data in the hospital. However, patients who are engaged with their care have both better care experiences [17] and better health outcomes [16] than disengaged patients. Most definitions of patient engagement emphasize patients’ awareness of their health status, understanding of their health care needs, or performance of particular behaviors (e.g. [15,18,21,40]). Thus, to engage with their individual care, patients must engage with information about their health status and treatment themselves, rather than relying on clinicians to track it for them. Recent work has demonstrated that patients in the hospital (inpatients) desire to stay informed about their care (e.g. [26,56]), but often lack the tools to fully engage with their health information and treatment. Their inability to access this information limits their participation in the care they receive [3,24,35].
Several barriers impact inpatients’ access to this information. Much of the information transfer in hospitals continues to be verbal [26], meaning patients’ access to information depends on their alertness and ability to recall what was said. Inpatients also frequently face challenges in obtaining specific details about their care like their daily schedule [26], or even who is coming into their room and when [38]. Given the high number of hospitalizations occurring each year in the United States—more than 34 million in 2014 [1]—it is urgent that researchers investigate how to design better tools to support patients in tracking their health and care information while in the hospital.
Many HCI researchers have studied the nature of health tracking and designed tools to support it. Much of this work concerns everyday health and wellness. For example, researchers have examined the use of novel or commercially available systems for daily activity and dietary tracking (e.g. [47]) and tracking of daily or weekly physical activity goals (e.g. [9]), and health tracking in the context of chronic disease management (e.g.[2,14,33]). In addition, models of personal informatics like the stage- based model [29] and lived informatics model [13] have primarily been developed for an everyday context.
However, the hospital environment differs substantially from the everyday context in which personal informatics has traditionally been studied. In the everyday context, people are largely in control of their own data and independently decide to set goals and track their personal progress towards them. In the hospital setting, patients surrender their bodies and health data to a host of doctors, nurses, technicians, and other health care providers whom they have likely never encountered before. With data locked in an electronic system that few have complete access to, patients have less access to their personal health data than they had with earlier paper-based systems [26]. In this vastly different context of control, how do personal informatics models hold up? How can we extend these models to apply in a context where the self that is being monitored might not be the self doing the monitoring?
To explore these questions, we conducted 30 interviews with hospitalized patients and caregivers (e.g. parents, spouses, and other informal helpers) and engaged them in speculative design exercises. We sought to understand how patients in the hospital envisioned their role in monitoring their own health status and what kinds of support they needed. We found that patients desired support for collaborative tracking of their health and care in conjunction with clinicians. In this paper, we:
Illustrate how patients envisioned collaborating with clinicians to track their health and care through all stages of tracking (collaborative tracking);
Discuss design implications for supporting patients in collaboratively tracking their health while in the hospital; and
Reflect on how the stage-based model should be extended to describe collaborative tracking fully.
RELATED WORK
Here we summarize related work on information needs in the inpatient setting. We discuss work on clinician-patient interactions over health tracking outside the hospital.
Information Needs in the Inpatient Setting
Studies have shown that patients in the hospital essentially “want to know everything” [3] about their health status and care in the hospital. However, existing information sources often do not meet their information needs [26,42]. Patients in the hospital get information about their care primarily from verbal encounters with clinicians and written notes on whiteboards. However, patients typically forget 40–80% of the information communicated in verbal encounters [27], and this information cannot be reviewed. At the same time, information on whiteboards is often not up to date [26,49] and only shows information that clinicians think patients ought to know, rather than information sought by patients themselves [26]. Compounding the problem, online information sources like patient portals that are frequently available outside the hospital are not always available in hospitals [20,25], even though patients find them valuable [25,41,58].
Researchers have begun to explore new ways to inform inpatients about their care [4,19,38,45,50,51,53,54,56], as well as to understand how patients and caregivers work together to exchange care-related information [23,39]. However, between receiving information and communicating about it lies a crucial step: tracking information. Valdez et al. recognize tracking as an important part of patient work [52], and researchers have begun to explore the potential of tracking support tools in this space (e.g. [57] and others reviewed in the discussion section). However, tracking remains a difficult task for patients in the hospital. Kendall et al., surveying patients’ and caregivers difficulties in tracking information in the hospital, found that members of both populations struggled with tracking changes in symptoms and questions for the care team [26]. Benham-Hutchins et al., looking at how patients with chronic illnesses kept track of health and care information both in and out of the hospital, found they relied on a mix of methods such as paper-based logs, memory, and electronic methods including “multiple patient portals,” computer and phone applications, and digital notes [3]. This scattershot approach to tracking implies a need for better tools to support patients and caregivers in tracking health and care in the hospital.
Health Tracking and Patient-Clinician Interactions
Most of the work about health tracking in HCI has been done outside the hospital, for wellness [7,9] or chronic conditions [2,14,33]. This tracking could be performed alone or in collaboration with family members [43]. Rather than summarizing here the extensive body of literature about health tracking in general, we focus on health tracking in settings where patients are regularly interacting with clinicians about their health tracking.
Researchers have found that patients collect data outside the clinic both to develop self-awareness and to collaborate with clinicians in shaping their care plan [59]. Some also collect it for curiosity [31,59]. At the same time, clinicians can find patient-generated data overwhelming, unreliable, and clinically irrelevant [59]. Patients may collect data on different topics from what clinicians would prescribe [46], in part because the tools they use are not designed flexibly enough to support customized goals [8]. Patients and clinicians may have misaligned goals, leading to frustration on both sides [8]. Patients and clinicians may also approach the analysis of data in different ways [32]. However, successful collaboration can be very rewarding: with the proper tools, discussing tracked data with clinician experts can increase patients’ understanding of their health data, lead to more productive reflection, improve the clinician-patient relationship, and ultimately increase patients’ ability to self-manage [34,44,48]. Clinicians and patients can collaborate over data to jointly interpret it in and engage in shared decision-making [37].
The design of the tracking tools themselves is very important. Chung et al. suggest that tracking tools be designed to more flexibly support collaboration and provide better visualizations [8], while West et al. suggest that tracking tools make it easier for clinicians to reason about the data they collect [55]. Schroeder et al. suggest that tools support exploration through flexibility and simplicity, and emphasize the generation of actionable insights [48].
This work represents a valuable starting point in understanding patient-clinician interactions over health tracking. However, thus far researchers have largely focused on data collected by patients or their family members. Although researchers have begun to explore better ways to present data provided to patients by health care organizations [22,60], much work remains to be done on how to support patient-provider collaboration in the hospital, where clinicians collect and control the bulk of patient data. Thus far, studies in this space have shown that hospitalized patients value the ability to ask their clinicians questions electronically [57], “triage” their inquiries [57], and set personalized health goals [10]. Studies of technology-mediated patient-clinician collaboration in the hospital [12] and after discharge [5] have shown improved outcomes as a result of this collaboration, underscoring the importance of properly supporting this collaboration. Research has further shown that hospitalized patients and clinicians place different values on specific types of information [6], highlighting the importance of understanding both parties’ needs for the design of tracking tools in the hospital. Because clinicians’ workflows in the hospital environment are complex and constrained, we begin by investigating patients’ perspectives: what process do hospitalized patients envision for collaboratively tracking with their clinicians, and what designs can support them in doing so?
METHODS
To explore how patients envision collaborating with clinicians to track their health and care, we interviewed 30 patients and caregivers in two urban hospitals in the United States. We conducted these interviews with a speculative design probe to understand what kinds of tools could best support patients’ health tracking needs. The design probe consisted of a series of “feature cards” (see Fig. 1 for examples). Each card depicted a hypothetical tool or function to support tracking of health status or care, or facilitate communication with clinicians. For example, one feature card showed a generic line graph representing test results with an area labeled “Doctor’s Notes” next to it; others contained features that would allow patients to take notes in various formats. During the interviews, participants described their thoughts about the feature, how it would or would not be valuable to them, and how they envisioned it working. Participants were encouraged to expand on each feature—including writing or drawing on it—to explain new ideas that the feature cards gave them.
Figure 1.
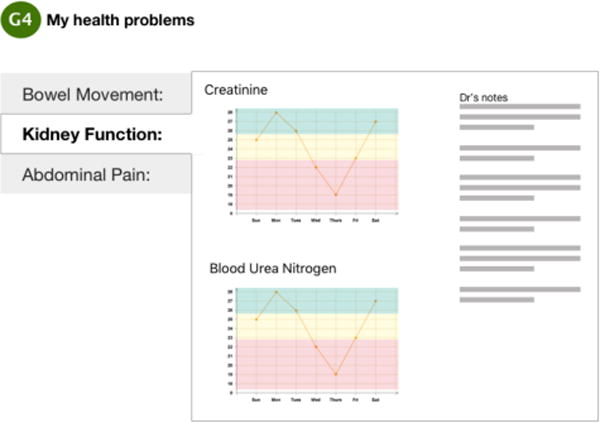
Example “feature card” showing generic graphs representing test results and doctors’ notes to the side.
The interviews lasted 30–60 minutes and were recorded, then transcribed. Members of the research team then analyzed the transcripts using an iterative, inductive coding process to identify different themes in the data. The project was approved by the researchers’ institutional review board.
Research Sites and Participants
Our research sites were Seattle Children’s Hospital and Virginia Mason Hospital (a tertiary care hospital for adults) in Seattle, WA, United States. We identify participants from Seattle Children’s Hospital with a Y (for youth) and participants from Virginia Mason Hospital with an A (for adults). From Seattle Children’s, we recruited 12 pediatric patients. Because caregivers play a critical role in pediatric settings and our goal in this study was to get a broad sample rather than to distinguish patients from caregivers, we recruited 3 adult caregiver participants (Y13, Y14, and Y15). Five of the pediatric patients also had caregivers present during the interview. Pediatric patient participants ranged in age from 7 to 17 (mean and median age 10.5). At Virginia Mason, we recruited 15 patients, who ranged in age from 18–75 (mean age 57.5, median 64). Across both groups, 15 participants were male and 15 female. Participants were recruited across services and conditions to get a broad sample of experience.
FINDINGS: COLLABORATIVE HEALTH TRACKING IN THE HOSPITAL
Our participants described a vision of health tracking in the hospital in which neither patients nor clinicians were solely responsible for health tracking. Instead, participants envisioned a world where patients and clinicians could collaboratively track the patient’s health. They described this vision in terms of both the tracking activities that they currently performed and the tracking activities that they wanted to perform. We illustrate participants’ vision of collaborative tracking in the hospital and present the findings by the 5 stages of the personal informatics model [29]: preparation, collection, integration, reflection, and action. We use this model, rather than the lived informatics model [13], because parts of the lived informatics model (e.g. selecting tools, lapsing) are rooted in the everyday tracking context, while the stage-based model’s process-oriented focus generalizes more easily to different contexts. For brevity and because most of our participants were patients rather than caregivers, we refer to them as “patients” rather than “patients and caregivers,” but include both patients and caregivers in that term.
Preparation stage
In the preparation stage, users decide what data to collect and how [29]. In the hospital, these decisions are traditionally made by clinicians, who decide which tests to order and which biometrics to track. However, in addition to the existing standard in which clinicians collect data about patients, our participants envisioned a collaborative process for determining what data to collect, in which clinicians could request that patients collect data, and patients could also decide for themselves which data to collect, as well as request that clinicians collect data on their behalf. Participants also wanted to track important metadata regarding data collection.
Collaboratively determining what data to track
Participants were happy to collect data about their health that had been requested by the care team. For instance, A05 had been asked by clinicians to record his urine output, and Y11 had checkboxes on the whiteboard in her room to mark how much water she drank. Participants also wanted to collect data about their health that clinicians were not already collecting. Often this data was about the patient’s symptoms. Participants described wanting tools to support their data collection. For example, Y06 took it upon himself to photograph his surgery scar and track its healing progress, for his own sake rather than because clinicians had asked him to. Y04 wanted to take photos of “a thing in my neck that’s been changing in size…. It would be nice if we could keep [a photographic record] somewhere….”. Clinicians had not requested that Y04 collect this data, but Y04 saw it as an important part of her health record. Moreover, she wanted to collect it to support discussion and collaboration between her and her care team.
In addition to data about themselves, participants thought it crucial to collect data from or about other people and processes in the hospital that were relevant to their care. One such data type was conversations with clinicians. Dialogue between patient and clinician was an important source of information about health status, but because it typically occurred verbally, participants were not able to retrieve the information later. As a result, some participants welcomed the idea of a notetaking tool or even an audiorecording of the conversation, like Y03, who said, “if I wanted to remember something, I’d just … go back over it and listen to it,” and A11, who said “Recordings would be [helpful] because [my caregiver] tends to forget like what the doctor said, even though she wrote it down.”
When it was inconvenient for participants to collect data themselves, they also wanted to be able to ask clinicians to collect data for them. A09, for example, wanted pictures of how his wound was healing, but instead of taking the photos himself, he wanted someone from the hospital to take those photographs for him. Other participants envisioned clinicians tracking information for them about hospital processes and care administration, like shift changes and the medication schedule. For instance, Y15 wanted to know “that Dr. [NAME] is here until 8 p.m. or 12 p.m …. That after 10 p.m. there is a handoff or something is going to happen.”
Collecting metadata about tracked data
In addition to health data, participants wanted important metadata about tracked data to also be collected and shared with them. In particular, participants were interested in metadata about information provenance and the timing of information availability. Regarding information provenance, Y13 saw her care team members as distinct individuals. When describing how she wanted to hear about what her doctors were thinking (which we return to in the reflection section), she emphasized wanting to know what each individual doctor was thinking, especially as they changed shifts: she wanted “to know one doctor’s thinking to the next … to keep track of that stuff.” Similarly, A09 wanted to have metadata about which doctor a given opinion came from, so that he could act based on that information: “… I know that urology thinks I’m doing fine, but why does everybody else think I’m not doing fine? That way I can ask additional questions.”
A14 explained how metadata about both information provenance and the timing of information availability would help her keep track of her progress at the hospital. She said that because of “the number of doctors or residents or interns coming in at different times and then the surgeon and the nurses and everything… it would be nice [if] you could just look it up on this date – Nurse Ratchet came in and told me …. A, B, and C ….” Although A14 was describing performing a reflective activity (reviewing data), her statement implied the necessity of collecting metadata about information provenance and timing of information availability, i.e. who said what when. A14 focused on metadata about the timing of information availability in the past, but some participants revealed that they needed real-time updates and even forecasts about when information would become available to support later stages. Y04 wanted updates about when lab results would come, analogous to package tracking. She was waiting on lab results and wanted to know when information is “coming out of the lab and when the information is coming to the hospital that you’re in.” In other words, Y04 felt that in order to keep track of her health, she also needed to keep track of hospital activities that were completely out of her control. Participants also frequently wanted to know when clinicians were coming to their rooms to give them updates, because clinician-patient patient conversations were one of the key ways in which participants received information about their care. Participants needed this metadata both to prepare themselves to engage with the information they would receive and to keep track of what was happening with their care. Y02, for example, wanted to know when the doctor was coming so that she could take steps independently to prepare herself for the clinical encounter: she wanted to “be ready and have a plan when the doctor comes and when you meet with them, to …. have questions ready.”
In sum, participants envisioned not just collecting data when clinicians asked them to, but also independently deciding what data they would collect as well as what data clinicians would gather about or on behalf of them. They identified types of metadata—e.g., information provenance and timing of information availability—that would support them in later stages of tracking.
Collection
In the collection stage, users actually collect the data, and must navigate the weaknesses of their collection tool and any inherent ambiguity in the data to gather data and get it into the tracking system [29]. Our participants did not have good tools to support them in tracking their health, so instead of describing how they used tools to collect data, participants described characteristics of tools that they thought might meet their needs. Participants needed tools that would allow them to assert their own voice and offer flexible options for joint data collection.
Asserting their voice
Participants required tools that would let them collect data in their own words rather than relying on clinicians’ language. For A09, using his own voice was essential for understanding. He preferred the notetaking feature card over the audiorecording card because notetaking let him “put it in my own terms versus what they’re saying might be in medical jargon that I don’t necessarily understand.” Y04 saw the ability to use her own words as a form of empowerment. She wanted to express her symptoms as she experienced them instead of struggling to find the right medical words, and explained that patients should be able to “….focus on just … talking about how they feel instead of trying to put it into words for their mom to write down.”
Flexible options for joint data collection
A few participants addressed the role of caregivers in data collection, but expressed opposing views. Y04 wanted a tool that would support patients in collecting data independently from and unaided by caregivers. Implying that caregivers could corrupt the record, she said, “…it’d be better to hear it from a kid what’s going on with them …. because their mom might add to it, whatever, because my mom adds to it.” Y04 furthermore wanted a private chat with her doctors that her mother could not access, “Like maybe something that you write down and then it goes away and just goes to your doctor. And you can’t find it on your – it’s just gone. … that would be really helpful, like if you want to let them know something, and not whoever’s in your room to know or whoever was using this to know.” By contrast, A06 depended on caregivers: she “wasn’t able to get photographs because … I’m flat on my back and I couldn’t even access my phone.” Note that both participants focused on the role of their caregiver rather than a clinician. No participants described wanting clinician help in recording data, nor did any participants want to maintain independent records of things clinicians were already tracking. We will return to this topic in the discussion.
Integration
Integration refers to bringing data that has been collected together so that it can reveal insights [29]. In collaborative tracking, integration means not just bringing different bits of data together, but bringing together data from different sources: from clinicians, patients, and caregivers. Our participants envisioned accessing clinicians’ data, granting them access to data they collected themselves, and having data from both sources conjoined to support reflection.
Accessing clinicians’ data
Participants wanted direct access to the same information their clinicians had. A05 wanted specifically to see laid out before him exactly what his doctors saw:
“I’ve had … tumors that are visible, but they never give me the visual record, they always just give me the pathology interpretation. So the pathologist has a picture in front of him or her that they’re describing…but they don’t ever show the image so you can never correlate what they’re [saying with] what’s in the image. …. for the doctor looking at it, they’re both reading and seeing, and so they’re getting a hell of a lot more information [than I am]. So if my chest X-ray actually came up along with the medical report that describes the findings, I would be a lot more interested in that.” —A05.
Other participants wanted tools that provided them information that clinicians might be expected to already know. For example, Y01 wanted to know not just what bacteria had caused his infection, but other information like how common it was and what cured it. Participants also wanted to understand the reasoning behind the care plan, which clinicians knew but did not always communicate to patients. For instance, Y04’s caregiver wanted to know during blood draws “[w]hat they’re checking in your blood. Are they checking white blood cell count? Are they checking platelets? Are they checking iron?” Y13, although a nurse herself, felt uncomfortable with her level of understanding of her child’s treatment, and wanted more information to “understand a little bit more as far as what they’re watching and stuff.… he’s on a certain medication that helps to potentiate one of the other medications, he doesn’t necessarily need it by itself … initially I didn’t have a clue as to why he was on it other than for just getting rid of fluid….” Y13 needed more detail about what function each medication served to understand the care plan she was looking at and to support reflective activities later on.
For their own purposes, participants wanted access to data tracked by clinicians about hospital processes and care administration, such as when shift change would happen and when medication would be administered. Access to this information would support participants in later-stage reflection on the care plan, to identify breaks in the care plan and the reasons for it. For instance, Y15 described how having access to information about the schedules and whereabouts of clinicians would enable her to notice if there was an irregularity in the care plan and to shape her actions in response: “…if I’m waiting for my nurse, if it is a time to give Albuterol to my daughter … I’d like to know where my nurse is, so that I know okay, she is attending someone critical, she’s on lunch, something like that.”
In general participants wanted to know everything their doctors knew, but a few participants wanted clinicians to act as gatekeepers of negative news. For example, Y01, afraid of getting bad news from his doctors, preferred no news to the chance of bad news. However, most participants, like A11, wanted to know everything, good or bad: “Let me know…if I got a month, do I have a year?”
Granting access to patient-collected data
In addition to wanting access to clinicians’ data, participants wanted clinicians to have real-time access to data patients could gather themselves. For example, the photos that Y04 wanted to take of her neck were something she wanted to “keep … archived in the app and go back and look at it and then like the doctor have access to it through their computers ….” A10 and Y14 wanted tools to be able to communicate symptoms to clinicians, either to immediately get information about whether the symptoms were normal (Y14) or because otherwise they could forget when they experienced specific symptoms (A10). A12 wanted a way to share information about herself with clinicians to streamline communication. Annoyed with having to repeating information about herself to clinicians again and again, she said, “…it should give you some centralized place … so you don’t have to continually do it over and over again….”
The ability to share their data with clinicians was important to participants both because it would give clinicians a more complete picture of their health and because it would enable them to intervene in their treatment when needed. A06 wanted to send a photographic record of how her foot’s condition was changing to send to clinicians because she felt that clinicians were not treating her correctly. As she put it, “The purpose on that was to get the photo to my doctor because they were not transmitting it at [neighborhood]. The nurses were not getting the information to my doctor ….”
Conjoining data to support reflection
Having access to both their own data and clinicians’ data was important to participants so that they could conjoin the two. Several participants commented positively along the lines of how “hav[ing] like everything on the same app …. would be cool” (A10). A05 spoke vehemently and at length about the benefits of a unified system that “mak[es] the information useful so that the patient can interact with it”. Others wanted to look at clinician-collected data about when medication was administered alongside patient-collected data about symptoms so that they could identify cause and effect patterns between medications and symptoms. We will discuss this in the reflection section.
With only a couple of exceptions around the delivery of bad news, participants desired to see the same data their clinicians see, and know the same things their clinicians knew. They also wanted the reverse: for clinicians to have instant access to patient-generated data about patients’ symptoms and needs. Furthermore, participants wanted to conjoin clinician-generated and patient-generated data to support reflection.
Reflection
Li et al. define the reflection stage as “when the user reflects on their personal information”. It includes both short- and long- term reflection, where short-term reflection informs the user about their current condition and long-term reflection uncovers patterns and trends over time [29]. In collaborative tracking in the hospital, reflection encompasses both patients reflecting on their data to make conclusions about their health themselves, and patients influencing clinicians’ reflections. Participants described a number of types of tools that could support them in independent reflection, including information about clinicians’ reflections and different types of contextualizing information. Additionally, some participants spoke about their desire to collaboratively reflect with clinicians.
Support for Independent Reflection
Participants discussed tracked health information with their clinicians face-to-face to understand their health status. During these conversations, clinicians would convey to patients their own reflections on the patient’s health. Participants wanted access to these reflections from clinicians, to reflect on themselves. Participants wanted this information as a supplement to, rather than a substitute for, conversations with clinicians. Our “feature cards” contained two options for conveying clinicians’ reflections: a card representing doctor’s notes, and a card depicting emojis reflecting clinicians’ attitudes about the patient’s health. Although participants had mixed reactions to the specific format represented by the cards, they were extremely interested in accessing the content of clinicians’ reflections because this information could support their own, independent reflective activities. A02 wanted to know “how [the doctor] feels about my overall – how I’m doing. Because he’s going to examine all my results and come to a conclusion.” A14 likewise wanted access to “what you’re [the doctor] thinking is happening here”. Y13 emphasized that having access to information about clinician reflections was important for independent reflection: as she said, “…people are busy, you know? It would be nice to just go look it up yourself and be done with it.” Y11 pointed out that forcing clinicians to enter information about their reflections in a tool might help her learn more than she would otherwise be able to find out through conversation with clinicians. One of the few participants who responded positively to the emojis, Y11 liked them because she felt that she could not trust her clinicians to be completely honest with her unless they were forced into a simple, emotive response. Worried that her doctors would not tell her the whole truth, she said, “I mean, the doctors always tell you like ‘oh, you’re doing great,’ but you never really get to see like what they mean by that, if they’re telling the truth or not…. I want their emotion.”
In addition to information about their clinicians’ reflections and conclusions, participants wanted information that would contextualize their health data and help them form their own conclusions. To contextualize their health data, participants wanted: (1) information to help them see the effects of the care plan, (2) benchmark ranges, (3) the patient’s own history, and (4) the projected trajectory of the patient’s care plan or hospital stay.
A couple participants wanted information that would help them see the effects of their care plan on their symptoms, to understand cause and effect. For instance, Y15 wanted to “know exactly what has happened last time I visited and what time admitted, what was the observation, what kind of medications we’re given on an hourly basis or something like that …. I can track, and if she’s talking longer time this time to recover, then I can match exactly how much time last time she took to recover.” Y15 wanted to reflect on the patient’s data herself, both to understand the patient’s current health status (short-term reflection) and to find trends and understand patterns of cause and effect (long-term reflection).
Participants also wanted to see benchmark ranges. A14 wanted to see “the margins that is best to be in for this particular lab that we had drawn”. Y14 thought the benchmark range as an interpretative aid was more important than the results themselves, saying that “it’s fine if you have charts” but that it was more important that patients “have some sort of an explanation that [anyone] can understand and not spend so much time reading the actual results.”
Several participants felt that their own history would be useful in contextualizing their results. For example, Y04 (quoted earlier) wanted precise records of how her health issue was changing over time, and A03 wanted “to know, it’s my body, how things are going through this treatment, lymphoma, and how’s the progress.”
Participants also wanted information about the trajectory of their care plan or hospital stay as a way to help them understand their health status. Y11 tracked her progress through her stay in context of how close she was to her discharge date. Y06’s caregiver understood the patient’s health status in terms of future care. She wanted results contextualized in terms of “at what points you’re going to need the transfusion so you can see oh, I’m getting close to like the red line … critical values so that you know they’re going to have to do something about it.” A14 similarly wanted a tool that would explain to her, “if you’re on the low side, this is what you could be expecting, or if you’re on the high side and how to go about correcting that.”
Collaborating with Clinicians in the Reflection Stage
Collaboration with clinicians in the reflection stage was also important to our participants. A12 stressed the importance of engaging in dialogue with clinicians, saying, “we have to be in charge of our own health, absolutely, but I also don’t want [clinicians] to abdicate what they’re responsible for, which is to keep me informed and make sure we’ve had this dialogue.” A couple of participants described how they proactively involve themselves as their clinicians formed impressions about their health and care. A09 felt that since each person is “responsible for your health ultimately,” it is their own responsibility to “give them [clinicians] the most information in an easy to understand way,” aiding not just with supplying information but with interpreting it for them. A09 felt that because clinicians’ communication was necessarily imperfect, he needed to “be his own advocate”. Discussing the “great variances in how people do things, and their interpretations of what heavy means and what light means,” he felt that he was the failsafe to make sure the proper amount of lidocaine was applied. Similarly, A14 made a point of listening in to nurse handoffs “because maybe I didn’t explain something right, and now I’m hearing how she’s presenting or he’s presenting, and then I can interject something”.
Our findings on the reflection stage suggest that patients desire tools that will support them in independently reflecting on and drawing conclusions about their health and care. However, participants also evinced desire to maintain a dialogue with clinicians and influence clinicians’ reflections on patients’ health data.
Action
Li et al. define the action stage as the time when people decide what to do about what they have learned through reflection. In some cases, action is about tracking progress towards goals, while in others it is about driving behaviour [29]. In the hospital, participants wanted to be able to track their progress towards goals and modify their behavior to reach those goals, as well as collaborate with clinicians to set the goals. Participants also wanted to collaborate with clinicians to make changes to their care plans based on their reflections on information about their health and care.
Tracking and collaborating over discharge goals
Several participants wanted to track progress towards their discharge goals, i.e., goals set by clinicians that describe what needs to happen for the patient to go home. Participants wanted to know about their discharge goals so that they could act to meet them. For example, A10 said, “It’s just helpful to know like … exactly what you have to … complete each day …. if I’m missing something, I want to make sure that I get it done ….” A14 lamented that her clinicians had not been clear about discharge goals with her. She knew her clinicians had been tracking her urine output, but did not know that she also had to reach a respiration goal. She said, “… if I knew about that in the very beginning, that this was something that you really have to work on and work on breathing into this tube, I could have been maybe on it a little bit earlier and not just dismiss it.”
Although most participants took discharge goals as fixed criteria set by clinicians, a couple saw them as something that both parties should have input on. Y06 said that “Sometimes we have to even convince our doctors” that they were ready for discharge. A13 likewise expressed agency over his goals and goal achievement, joking about his ability to meet his discharge goals on his own timetable.
Collaborating with clinicians to change the care plan
Monitoring their health and care allowed participants not just to keep tabs on their health, but also to modify their care plan. A07, keeping track of his different therapies and his leg pain, drew a conclusion about how to improve his pain and suggested a change to the care plan. After a day with several back to back therapy sessions, A07 noticed that his legs hurt. To improve his symptoms, he suggested that he should be given pain medication before his therapy session and that there should be a change to the therapy schedule for the next day: “…my suggestion was … a bit more spacing in between my therapies so I can recover, you know, and it wouldn’t have such a high impact.” Y13 used her knowledge of her child’s needs and the care plan to coordinate with clinicians to “customiz[e] [the care plan] for the day”. She described working with clinicians to change medication administration times so that her child could sleep uninterrupted. A14 wanted to weigh in on her positioning on the table while under anesthesia. After a procedure, she felt “tremendous pain across my upper back”. Her discussion with clinicians yielded the insight that this pain could have been due to her positioning on table as well as the anesthesia, and she valued the ability to give “input for the docs too, to say well, maybe we shouldn’t have had her upside down, that caused some problems,” so that in future this problem could be corrected. A09 similarly wanted to pass on to clinicians his evaluation of his care and the impact it had on him, so that clinicians could “improve or in some cases stop doing something that you find annoying or not helpful.” Similarly, Y03 described how a tool to communicate evaluations of the care team would have been useful to him and his caregiver on a past occasion. At that time, his father had realized that the clinicians’ assessments of the patient’s status contradicted the patient’s own description of his symptoms. He described how “the nurses kept saying I was faking my pain, and then [my father] kind of went off on them.” He believed that better electronic communication support could have helped his father manage the conflict and secure him proper pain management.
Because any change to the care plan had to be made in conjunction with clinicians, participants also needed to know who was who on the care team to direct their communication. For instance, A08 wanted to be able to communicate directly with the hospitalist, “Because the hospitalist is really the person that takes care of things … it all has to go through the main hospitalist anyway.” A05 also evaluated clinicians by role: he valued his hematologist but said, “… the other people that come in, the hospitalists and that sort of thing, really aren’t that interesting”.
In summary, participants demonstrated a desire not just to track their progress towards their goals, but in some cases to negotiate those goals. Participants also used their knowledge of their health, care plan, and care team to collaborate with clinicians to modify their care plans.
DISCUSSION
In this section, we reflect on the nature of collaborative tracking and discuss its implications for the stage-based model and for systems that support collaborative tracking. We then discuss implications of our findings for the design of patient-facing technologies in the hospital.
Adding collaboration to the stage-based model
One of our goals was to evaluate how well the stage-based model held up in the hospital context. We found that the model was overall robust to the change of context—our findings about health tracking neatly aligned themselves with Li et al.’s five stages, despite the shift in context to a short-term situation where the self being tracked (the patient) is not always in control of collecting, analyzing, reflecting, or acting on their data. Our findings suggest that people engaged in collaborative tracking go through the five stages in parallel with their collaborators. We discuss barriers that arise in only the collaborative tracking setting, and additional considerations—the definition of collaborators and the importance of process-oriented metadata—associated with collaborative tracking that the stage-based model in its current form does not account for.
Based on our findings, collaborative tracking looks like a mix of independent and collaborative work. To the maximum extent possible, our participants wanted to carry out tasks for each stage independently, then share the results with clinicians. Thus, in the collection stage, participants wanted to collect and contribute data but did not speak of needing clinician help. In the reflection stage, participants desired to reflect independently and form their own opinions to take action collaboratively with clinicians later on. Our participants also generally did not speak of maintaining an independent record of things that clinicians were already keeping track of.
Thus, in terms of the stage based model for collaborative tracking, collaborators go through the same stages in parallel, touching base with each other in each stage. But in those touchpoints new barriers can arise that, in accordance with the stage-based model, can cascade to impede tracking activities later on. One such barrier is conflict amongst tracking collaborators. When they come into conflict in one stage, further stages are impacted, such as when Y03’s father and the nurses disagreed about the patient’s health status, which then made it difficult for Y03’s father to take the action he thought necessary (getting more pain medication for Y03). Another such barrier is the potential for segregated knowledge. When knowledge is not shared among stakeholders the effects cascade, as when patients were unable to interpret their lab results (reflection) because they lacked access to contextualizing knowledge held by clinicians (integration).
Another consideration for modeling collaborative tracking is how the collaborators are defined. Chung et al. have already noted the need to extend the stage-based model to allow for the articulation of different roles in collaboration [8]. However, Chung et al.’s study took place in the context of pair-wise interactions between clinicians and patients, outside the hospital. Our study took place inside the hospital, where patients interact with a multitude of clinicians, and might additionally be accompanied by caregivers. In this type of multi-agent setting, a tracking collaborator could be a single person (e.g. the hospitalist), a group of people (e.g. the whole care team), or even a role filled by different people at different times (e.g. the nurse on shift). A system that supports collaborative tracking must allow different kinds of collaborators to connect with each other as needed: individuals should be able to connect to individuals, groups, or roles, etc. Furthermore, these different types of collaborators stand in different relationships to each other. For example, a patient may have a very different relationship with a caregiver than they do with a clinician. Understanding what these different relationships mean for how collaborative tracking activities are conducted is a fertile new area of research for HCI.
Collaborative tracking also highlights the importance not just of data collection, but of process-oriented metadata collection. As shown in our findings, people engaged in collaborative tracking need metadata about information provenance and the timing of information availability. Although not explicitly discussed by our participants, metadata about task assignment may also be important for supporting collaborative tracking. Metadata about information provenance is particularly important in settings where there are more than two people engaged in collaborative tracking. Collaborators touch base with each other throughout the tracking process. Without metadata about information provenance, this step cannot happen and later stages of tracking may be impossible. Metadata about the timing of information availability is necessary to inform people engaged in collaborative tracking about where their collaborators are in the process. Metadata about task assignment may also be necessary to inform collaborators about what information to expect and to make sure that collaborators are all on the same page about what data needs to be collected. Providing all three types of metadata will support people engaged in collaborative tracking in knowing what each collaborator is responsible for and where other collaborators are in their process.
Supporting inpatients in collaborative tracking
We applied the stage-based model to our findings to see if findings from other research in personal informatics can help us understand patients’ needs in the hospital setting. Because the stage-based model held up well in this new context, we derive recommendations for supporting inpatients in collaborative tracking based on the personal informatics literature. For example, findings that systems should be designed to allow for flexibility of data collection [8,31] and integration [31] can be applied to this context, as can lessons about the questions people ask in discovery-phase tracking [30]. Adding to this literature, our findings shed light on how systems can be designed to support hospitalized patients in collaboratively tracking their care. Participants desired an equal, collaborative role throughout every stage of the personal informatics model. They envisioned a collaborative medical record, forged and used collaboratively by patients and clinicians. Building on existing avenues for electronic patient-clinician communication, like the ability for patients to electronically ask questions [57] or communicate health goals [10], this transformed electronic health record would capture data from patients, caregivers, and clinicians to become a comprehensive record of the patient’s health and care from multiple perspectives. Importantly, this record must support, rather than replace, communication between patients and clinicians. Below we discuss how this record should support different stages of tracking.
To support preparation, such a record should support requests for data collection from each party to each other and transparent delegation of tasks. Highlighting the role of the patient in particular could facilitate their participation [3,28,36]. To support collection, the record should support multiple kinds of data formats (e.g. text, photos, or recordings), and give patients flexible options for joint data collection (e.g. with or without caregiver help). Patients should be able to communicate with clinicians independently of caregivers, but also to grant caregivers editing privileges as needed, in compliance with hospital policies and laws. To support integration, the record must be accessible to and editable by patients, clinicians, and caregivers. Because information provenance is such crucial metadata in collaborative tracking and in the hospital, all users should be able to distinguish whether information came from a particular clinician, the patient, or a caregiver.
Permission management must be granular enough to distinguish when data is editable by a user and when the user can only annotate or comment on the data. Patients should furthermore be able to opt out of seeing data they do not want to see without clinician mediation, like bad news that they would prefer to receive only face to face.
Reflection support requires the inclusion of contextualizing information and support for communication about data. Our findings uncovered several ways in which patients understand health data: by looking for cause and effect patterns, and by contextualizing health information against benchmarks, the patient’s personal history, and the patient’s care trajectory. Collaborative tracking systems should support all of the above means.
Regarding benchmarks, Zikmund-Fisher et al. demonstrated that visualizations of benchmark ranges for test results can help patients interpret data and distinguish near-normal from atypical results [60]. However, Wilcox et al. point out that clinicians sometimes object to the presentation of reference ranges because they are not appropriate in all cases [56]. One technique to resolve these conflicting needs is to provide reference ranges that can be turned on and off, modified, or otherwise annotated by clinicians as appropriate for individual patients. For instance, a clinician could leave an explicit comment or a visual indicator that the reference range may not apply to the patient. Allowing clinicians to show or hide individual chunks of content has been used in other contexts. For example, clinicians using OpenNotes—an approach to allow patients to see all notes about their care, rather than the typical subset—can decide whether or not to share individual notes with a patient, and the function has not produced a significant increase in clinician workload [11]. Nor is reflection support limited to test results—photographs of a surgical wound, for example, can be contextualized with past photographs to facilitate monitoring of progress. However, future research is needed to better understand how to communicate this information.
Finally, note that some of the collaborative tracking activities described in this paper are things that patients in theory already can do, but often don’t (such as audiorecording conversations with clinicians), or are features that were not received well by patients in other studies (e.g. the less favorable responses towards features like sharing notes with clinicians that promoted active engagement in [58]). Our findings reaffirm that patients need better tools to support them in collaboratively tracking their health while in the hospital. The discrepancy between the need for tracking support that we discovered and the cool reception of specific tracking tools suggests that HCI researchers must continue to explore this space to find the right designs and implementations to support hospitalized patients in actually performing collaborative tracking.
LIMITATIONS AND FUTURE WORK
Our broad sampling strategy, which enabled us to cut across conditions, was also a limitation: the strategy enabled us to cut across conditions, but also did not allow us to identify differences in tracking needs between patients with different conditions or provide deep insight into condition-specific tracking practices. Dykes et al. have demonstrated the potential of patient-clinician collaboration in the MICU [12], but it is unclear how well our findings on collaborative tracking apply in specific contexts, like mental health and trauma. More research is needed to understand how needs for collaborative tracking could change in different care contexts.
Our work focused on understanding patients’ needs for collaborative tracking. Because collaborative tracking is by definition about multiple agents, future work should also explore clinicians’ and caregivers’ needs and constraints in in this arena. Furthermore, our methods used simple, generic tracking prompts to elicit patient needs. Future work is needed to understand how to implement collaborative tracking systems given the large variety and amount of clinical data possible. Care must be taken to ensure that patients are not overwhelmed by the information they receive during their hospital stay. Rather than seeing collaborative tracking tools as sole information channels, they should be seen as a supplement to help patients be well informed when entering a dialogue with their clinicians.
CONCLUSION
Patients in the hospital want to keep track of their health, but lack the digital tools to collect, track, and reflect on all the data that is important to them. In this study, we investigated inpatient needs for tracking their health, and found that inpatients envision collaboratively tracking their health and care plan with their clinical team. We found their tracking process follows the stage-based model, but that collaborative tracking introduces new barriers to and requirements for successful tracking. We provided insights about designing collaborative tracking systems to help hospitalized patients manage their health and care, reflections on how collaborative tracking extends the stage-based model of personal informatics, and suggestions for new research directions. With better tools for collaborative tracking, patients in the hospital will be able to keep track of their health and care, increasing the potential for improved health outcomes and medical error prevention.
Acknowledgments
We thank our participants, Seattle Children’s Hospital, Virginia Mason Hospital, and members of the Patients as Safeguards research team, including Barry Aaronson, Kelsey Aiello, and Corey Brown. Thanks also to Jessica Pater for her feedback. This work was funded by the Agency for Healthcare Research and Quality (grant #1R01HS022894), with support from the NIH National Library of Medicine Biomedical and Health Informatics Training Grant at the University of Washington (grant #T15LM007442).
References
- 1.American Hospital Association. Fast Facts on US Hospitals. 2016 Retrieved from http://www.aha.org/research/rc/stat-studies/fast-facts.shtml.
- 2.Ayobi Amid, Marshall Paul, Cox Anna, Chen Yunan. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (CHI ‘17) ACM; 2017. Quantifying the body and caring for the mind: Understanding self-tracking in multiple sclerosis; pp. 6889–6901. http://doi.org/10.1145/3025453.3025869. [Google Scholar]
- 3.Benham-Hutchins Marge, Staggers Nancy, Mackert Michael, Johnson Alisha H, DeBronkart Dave. I want to know everything: A qualitative study of perspectives from patients with chronic diseases on sharing health information during hospitalization. BMC Health Services Reseasrch. 2017;17:529–538. doi: 10.1186/s12913-017-2487-6. http://doi.org/10.1186/s12913-017-2487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bickmore Timothy W, Pfeifer Laura M, Jack Brian W. Taking the time to care: empowering low health literacy hospital patients with virtual nurse agents. Proceedings of the 27th international conference on Human factors in computing systems - CHI 09. 2009:1265–1274. http://doi.org/10.1145/1518701.1518891.
- 5.Brennan Patricia Flatley, Casper Gail R, Burke Laura J, et al. Technology-enhanced practice for patients with chronic cardiac disease: home implementation and evaluation. Heart & Lung : The Journal of Critical Care. 2010;39(6 Suppl):S34–S46. doi: 10.1016/j.hrtlng.2010.09.003. http://doi.org/10.1016/j.hrtlng.2010.09.003.Technology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caligtan Christine A, Carroll Diane L, Hurley Ann C, Gersh-Zaremski Ronna, Dykes Patricia C. Bedside information technology to support patient-centered care. International Journal of Medical Informatics. 2012;81(7):442–451. doi: 10.1016/j.ijmedinf.2011.12.005. http://doi.org/10.1016/j.ijmedinf.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Chung Chia-Fang, Agapie Elena, Schroeder Jessica, Mishra Sonali, Fogarty James, Munson Sean A. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (CHI ‘17) ACM; 2017. When personal tracking becomes social: Examining the use of Instagram for healthy eating; pp. 1674–1687. http://doi.org/10.1145/3025453.3025747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung Chia-Fang, Dew Kristin, Cole Allison, et al. Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing (CSCW ‘16) ACM; 2016. Boundary negotiating artifacts in personal informatics: Patient-provider collaboration with Patient-generated data; pp. 770–786. http://doi.org/http://dx.doi.org/10.1145/2818048.2819926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Consolvo Sunny, Klasnja Predrag, McDonald David W, et al. Proceedings of the 10th international conference on Ubiquitous computing (UbiComp ‘08) ACM; 2008. Flowers or a Robot army?: Encouraging Awareness & Activity with Personal, Mobile Displays; pp. 54–63. http://doi.org/10.1145/1409635.1409644. [Google Scholar]
- 10.Dalal Anuj K, Dykes Patricia C, Collins Sarah, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: A preliminary evaluation. Journal of the American Medical Informatics Association. 2016;23:80–87. doi: 10.1093/jamia/ocv093. http://doi.org/10.1093/jamia/ocv093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delbanco Tom, Walker Jan, Bell Sigall K, et al. Inviting Patients to Read Their Doctors’ Notes: A Quasi-Experimental Study and a Look Ahead. Annals of Internal Medicine. 2012;157:461–70. doi: 10.7326/0003-4819-157-7-201210020-00002. http://doi.org/10.7326/0003-4819-157-7-201210020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dykes Patricia C, Rozenblum Ronen, Dalal Anuj, et al. Prospective evaluation of a multifaceted intervention to improve outcomes in intensive care. Critical Care Medicine. 2017;45(8):e806–e813. doi: 10.1097/CCM.0000000000002449. http://doi.org/10.1097/CCM.0000000000002449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Epstein Daniel A, Ping An, Fogarty James, Munson Sean A. A Lived Informatics Model of Personal Informatics. Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing - UbiComp ‘15. 2015:731–742. doi: 10.1145/2971648.2971656. http://doi.org/10.1145/2750858.2804250. [DOI] [PMC free article] [PubMed]
- 14.Felipe Sergio, Singh Aneesha, Bradley Caroline, Williams Amanda Cdec, Bianchi-berthouze Nadia. Roles for personal informatics in chronic pain. 9th International Conference on Pervasive Computing Technologies for Healthcare. 2015:161–168. http://doi.org/http://dx.doi.org/10.4108/icst.pervasivehealth.2015.259501.
- 15.Graffigna Guendalina, Barello Serena, Bonanomi Andrea, Lozza Edoardo. Measuring Patient Engagement: Development and Psychometric Properties of the Patient Health Engagement (PHE) Scale. Frontiers in Psychology. 2015 Mar;6:1–10. doi: 10.3389/fpsyg.2015.00274. http://doi.org/10.3389/fpsyg.2015.00274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When Patient Activation Levels Change, Health Outcomes And Costs Change, Too. Health Affairs. 2015;34:431–437. doi: 10.1377/hlthaff.2014.0452. http://doi.org/10.1377/hlthaff.2014.0452. [DOI] [PubMed] [Google Scholar]
- 17.Greene Jessica, Hibbard Judith H, Sacks Rebecca, Overton Valerie. When Seeing the Same Physician, Highly Activated Patients Have Better Care Experiences Than Less Activated Patients. Health Affairs. 2013;32:1299–1305. doi: 10.1377/hlthaff.2012.1409. http://doi.org/10.1377/hlthaff.2012.1409. [DOI] [PubMed] [Google Scholar]
- 18.Gruman Jessie, Rovner Margaret Holmes, French Molly E, et al. From Patient Education to Patient Engagement: Implications for the Field of Patient Education. Patient Education and Counseling. 2010;78(3):350–356. doi: 10.1016/j.pec.2010.02.002. http://doi.org/10.1016/j.pec.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Haldar Shefali, Mishra Sonali R, Khelifi Maher, Pollack Ari H, Pratt Wanda. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (CHI ‘17) ACM; 2017. Opportunities and design considerations for peer support in a hospital setting; pp. 867–879. http://doi.org/10.1145/3025453.3026040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.HealthIT.gov. What is a Patient Portal? 2015 Retrieved from https://www.healthit.gov/providers-professionals/faqs/what-patient-portal.
- 21.Hibbard Judith H, Stockard Jean, Mahoney Eldon R, Tusler Martin. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health services research. 2004;39:1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. http://doi.org/10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hong Matthew K, Feustel Clayton, Agnihotri Meeshu, Silverman Max, Simoneaux Stephen F, Wilcox Lauren. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (CHI ‘17) ACM; 2017. Supporting families in reviewing and communicating about radiology imaging studies; pp. 5245–5256. http://doi.org/10.1145/3025453.3025754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hong Matthew K, Wilcox Lauren, Machado Daniel, Olson Thomas A, Simoneaux Stephen F. Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems (CHI ‘16) ACM; 2016. Care Partnerships : Toward Technology to Support Teens ‘ Participation in Their Health Care; pp. 5337–5349. http://doi.org/10.1145/2858036.2858508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Irizarry Taya, Shoemake Jocelyn, Nilsen Marci Lee, Czaja Sara, Beach Scott, DeVito Dabbs Annette. Patient portals as a tool for health care engagement: A mixed-method study of older adults with varying levels of health literacy and prior patient portal use. Journal of Medical Internet Research. 2017;19(3):e99. doi: 10.2196/jmir.7099. http://doi.org/10.2196/jmir.7099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kelly Michelle M, Hoonakker Peter LT, Dean Shannon M. Using an Inpatient Portal to Engage Families in Pediatric Hospital Care. Journal of the American Medical Informatics Association. 2016;24(1):153–161. doi: 10.1093/jamia/ocw070. http://doi.org/10.1093/jamia/ocw070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kendall Logan, Mishra Sonali R, Pollack Ari, Aaronson Barry, Pratt Wanda. Making background work visible: Opportunities to address patient information needs in the hospital. AMIA Annual Symposium proceedings. 2015:1957–66. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26958295. [PMC free article] [PubMed]
- 27.Kessels Roy PC. Patients’ memory for medical information. Journal of the Royal Society of Medicine. 2003;96:219–22. doi: 10.1258/jrsm.96.5.219. http://doi.org/10.1258/jrsm.96.5.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Larsson Inga E, Sahlsten Monika JM, Segesten Kerstin, Plos Kaety AE. Patients’ perceptions of barriers for participation in nursing care. Scandinavian Journal of Caring Sciences. 2011;25(3):575–582. doi: 10.1111/j.1471-6712.2010.00866.x. http://doi.org/10.1111/j.1471-6712.2010.00866.x. [DOI] [PubMed] [Google Scholar]
- 29.Li Ian, Dey Anind, Forlizzi Jodi. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ‘10) ACM; 2010. A stage-based model of personal informatics systems; pp. 557–566. http://doi.org/10.1145/1753326.1753409. [Google Scholar]
- 30.Li Ian, Dey Anind, Forlizzi Jodi. Proceedings of the 13th international conference on Ubiquitous computing (UbiComp ‘11) ACM; 2011. Understanding my data, myself: Supporting self-reflection with ubicomp technologies; pp. 405–414. http://doi.org/10.1145/2030112.2030166. [Google Scholar]
- 31.MacLeod Haley, Tang Anthony, Carpendale Sheelagh. Personal informatics in chronic illness management. Proceedings of Graphics Interface 2013 (GI ‘13), Canadian Information Processing Society. 2013:149–156. Retrieved from http://hcitang.org/papers/2013-gi2013-personal-informatics.pdf.
- 32.Mamykina Lena, Levine Matthew E, Davidson Patricia G, Smaldone Arlene M, Elhadad Noemie, Albers David J. From personal informatics to personal analytics: Investigating how clinicians and patients reason about personal data generated with self-monitoring in diabetes. In: Patel Vimla L, Arocha Jose F, Ancker Jessica S., editors. Cognitive Informatics in Health and Biomedicine: Understanding and Modeling Health Behaviors. Springer International Publishing; 2017. pp. 301–313. http://doi.org/10.1007/978-3-319-51732-2. [Google Scholar]
- 33.Mamykina Lena, Miller Andrew D. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ‘10) ACM; 2010. Constructing identities through storytelling in diabetes management; pp. 1203–1212. http://doi.org/10.1145/1753326.1753507. [Google Scholar]
- 34.Mamykina Lena, Mynatt Elizabeth, Davidson Patricia, Greenblatt David. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ‘08) ACM; 2008. MAHI: Investigation of social scaffolding for reflective thinking in diabetes management; pp. 477–486. http://doi.org/10.1145/1357054.1357131. [Google Scholar]
- 35.Mann L. From “Silos” to seamless healthcare: Bringing hospitals and GPs back together again. Medical Journal of Australia. 2005;182(1):34–7. doi: 10.5694/j.1326-5377.2005.tb06552.x. [DOI] [PubMed] [Google Scholar]
- 36.McMurray Anne, Chaboyer Wendy, Wallis Marianne, Johnson Joanne, Gehrke Tanya. Patients’ perspectives of bedside nursing handover. Collegian. 2011;18:19–26. doi: 10.1016/j.colegn.2010.04.004. http://doi.org/10.1016/j.colegn.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 37.Mentis Helena M, Komlodi Anita, Schrader Katrina, et al. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (CHI ‘17) ACM; 2017. Crafting a view of self-tracking data in the clinical visit; pp. 5800–5812. http://doi.org/10.1145/3025453.3025589. [Google Scholar]
- 38.Miller Andrew D, Pollack Ari H, Pratt Wanda. Bursting the information bubble: Identifying opportunities for pediatric patient-centered technology. AMIA Annual Symposium Proceedings. 2016:894–903. [PMC free article] [PubMed] [Google Scholar]
- 39.Miller Andrew D, Mishra Sonali R, Kendall Logan, Haldar Shefali, Pollack Ari H, Pratt Wanda. Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing (CSCW ‘16) ACM; 2016. Partners in Care: Design Considerations for Caregivers and Patients During a Hospital Stay; pp. 756–769. http://doi.org/http://10.1145/2818048.2819983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mishra Sonali R, Haldar Shefali, Pollack Ari H, et al. Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems (CHI ‘16) ACM; 2016. “Not just a receiver”: Understanding patient behavior in the hospital environment; pp. 3103–3114. http://doi.org/10.1145/2858036.2858167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.O’Leary Kevin J, Lohman Mary E, Culver Eckford, Killarney Audrey, Smith G Randy, Liebovitz David M. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. Journal of the American Medical Informatics Association. 2016;23(1):159–165. doi: 10.1093/jamia/ocv058. http://doi.org/10.1093/jamia/ocv058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Young Park Sun, Chen Yunan. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (CHI ‘17) ACM; 2017. Patient strategies as active adaptation: Understanding patient behaviors during an emergency visit; pp. 880–892. http://doi.org/10.1145/3025453.3025978. [Google Scholar]
- 43.Pina Laura R, Sien Sang-Wha, Ward Teresa, et al. Proceedings of the 2017 ACM Conference on Computer Supported Cooperative Work and Social Computing (CSCW ‘17) ACM; 2017. From personal informatics to family informatics; pp. 2300–2315. http://doi.org/10.1145/2998181.2998362. [Google Scholar]
- 44.Piras Enrico Maria, Miele Francesco. Clinical self-tracking and monitoring technologies: Negotiations in the ICT-mediated patient–provider relationship. Health Sociology Review. 2017;26(1):38–53. http://doi.org/10.1080/14461242.2016.1212316. [Google Scholar]
- 45.Prey Jennifer E, Woollen Janet, Wilcox Lauren, et al. Patient Engagement in the Inpatient Setting: A Systematic Review. Journal of the American Medical Informatics Association. 2014;21:742–750. doi: 10.1136/amiajnl-2013-002141. http://doi.org/10.1136/amiajnl-2013-002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rajabiyazdi Fateme, Perin Charles, Vermeulen Jo, MacLeod Haley, Gromala Diane, Carpendale Sheelagh. Proceedings of Pervasive Computing Technologies for Healthcare, 2017. ACM; 2016. Differences that matter: In-clinic communication challenges; pp. 53–59. http://doi.org/10.1145/1235. [Google Scholar]
- 47.Rooksby John, Rost Mattias, Morrison Alistair, Chalmers Matthew Chalmers. Proceedings of the 32nd annual ACM conference on Human factors in computing systems (CHI ‘14) ACM; 2014. Personal Tracking as Lived Informatics; pp. 1163–1172. http://doi.org/10.1145/2556288.2557039. [Google Scholar]
- 48.Schroeder Jessica, Hoffswell Jane, Chung Chia-fang, Fogarty James, Munson Sean, Zia Jasmine. Proceedings of the 2017 ACM Conference on Computer Supported Cooperative Work and Social Computing (CSCW ‘17) ACM; 2017. Supporting patient-provider collaboration to identify individual triggers using food and symptom journals; pp. 1726–1739. http://doi.org/10.1145/2998181.2998276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sehgal Niraj L, Green Adrienne, Vidyarthi Arpana R, Blegen Mary A, Wachter Robert M. Patient whiteboards as a communication tool in the hospital setting: A survey of practices and recommendations. Journal of Hospital Medicine. 2010;5(4):234–239. doi: 10.1002/jhm.638. http://doi.org/10.1002/jhm.638. [DOI] [PubMed] [Google Scholar]
- 50.Skeels Meredith M, Unruh Kenton T, Powell Christopher, Pratt Wanda. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ‘10) ACM; 2010. Catalyzing Social Support for Breast Cancer Patients; pp. 173–182. http://doi.org/10.1145/1753326.1753353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Skeels Meredith, Tan Desney S. Proceedings of the 1st ACM International Health Informatics Symposium (IHI ‘10) ACM; 2010. Identifying Opportunities for Inpatient-Centric Technology; pp. 580–589. http://doi.org/http://doi.org/10.1145/1882992.1883087. [Google Scholar]
- 52.Valdez Rupa S, Holden Richard J, Novak Laurie L, Veinot Tiffany C. Transforming consumer health informatics through a patient work framework: connecting patients to context. Journal of the American Medical Informatics Association. 2015;22:2–10. doi: 10.1136/amiajnl-2014-002826. http://doi.org/10.1136/amiajnl-2014-002826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vardoulakis Laura Pfeifer, Karlson Amy, Morris Dan, Smith Greg, Gatewood Justin, Tan Desney. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ‘12) ACM; 2012. Using mobile phones to present medical information to hospital patients; p. 1411. http://doi.org/10.1145/2207676.2208601. [Google Scholar]
- 54.Vawdrey David K, Wilcox Lauren G, Collins Sarah A, et al. A Tablet Computer Application for Patients to Participate in Their Hospital Care. AMIA Annual Symposium proceedings. 2011:1428–35. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3243172&tool=pmcentrez&rendertype=abstract. [PMC free article] [PubMed]
- 55.West Peter, Giordano Richard, Van Kleek Max, Shadbolt Nigel. Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems (CHI ‘16) ACM; 2016. The quantified patient in the doctor’s office: Challenges & opportunities; pp. 3066–3078. http://doi.org/10.1145/2858036.2858445. [Google Scholar]
- 56.Wilcox Lauren, Morris Dan, Tan Desney, Gatewood Justin. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ‘10) ACM; 2010. Designing Patient-Centric Information Displays for Hospitals; pp. 2123–2132. http://doi.org/10.1145/1753326.1753650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wilcox Lauren, Woollen Janet, Prey Jennifer, et al. Interactive tools for inpatient medication tracking: A multi-phase study with cardiothoracic surgery patients. Journal of the American Medical Informatics Association. 2016;23:144–158. doi: 10.1093/jamia/ocv160. http://doi.org/10.1093/jamia/ocv160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Woollen Janet, Prey Jennifer, Wilcox Lauren, et al. Patient Experiences Using an Inpatient Personal Health Record. Applied Clinical Informatics. 2016;7:446–460. doi: 10.4338/ACI-2015-10-RA-0130. http://doi.org/10.4338/ACI-2015-10-RA-0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhu Haining, Colgan Joanna, Reddy Madhu, Choe Eun Kyoung. Sharing patient-generated data in clinical practices: An interview study. AMIA Annual Symposium proceedings. 2017:1303–1312. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/28269928%5Cn http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC5333267. [PMC free article] [PubMed]
- 60.Zikmund-Fisher Brian J, Scherer Aaron M, Witteman Holly O, et al. Graphics help patients distinguish between urgent and non-urgent deviations in laboratory test results. Journal of the American Medical Informatics Association. 2017;24(3):520–528. doi: 10.1093/jamia/ocw169. http://doi.org/10.1093/jamia/ocw169. [DOI] [PMC free article] [PubMed] [Google Scholar]


