Abstract
Background
Although much research has been conducted on the determinants of HIV risk behavior among people who inject drugs (PWID), the influence of the neighborhood context on high-risk injection behavior remains understudied. To address this gap in the literature, we measured associations between neighborhood socioeconomic disadvantage and high-risk injection behavior, and determined whether these associations were modified by drug-related police activity and syringe exchange program (SEP) accessibility.
Methods
Our sample was comprised of 484 pharmacy-recruited PWID in New York City. Measures of neighborhood socioeconomic disadvantage were created using data from the 2006–2010 American Community Survey. Associations with high-risk injection behavior were estimated using multivariable Poisson regression. Effect modification by drug-related police activity and SEP accessibility was assessed by entering cross-product terms into adjusted models of high-risk injection behavior.
Results
Neighborhood socioeconomic disadvantage was associated with decreased receptive syringe sharing and unsterile syringe use. In neighborhoods with high drug-related police activity, associations between neighborhood disadvantage and unsterile syringe use were attenuated to the null. In neighborhoods with high SEP accessibility, neighborhood disadvantage was associated with decreased acquisition of syringes from an unsafe source.
Conclusions
PWID in disadvantaged neighborhoods reported safer injection behaviors than their counterparts in neighborhoods that were relatively better off. The contrasting patterns of effect modification by SEP accessibility and drug-related police activity support the use of harm reduction approaches over law enforcement-based strategies for the control of blood borne virus transmission among PWID in disadvantaged urban areas.
Keywords: people who inject drugs (PWID), injection drug use, HIV risk behavior, neighborhood context, receptive syringe sharing
1. Introduction
High-risk injection behaviors, such as syringe sharing and syringe reuse, facilitate the spread of HIV, HCV, and other infections among people who inject drugs (PWID) (Normand et al., 1995; Villano et al., 1997). Research on the determinants of high-risk injection behavior has traditionally concentrated on factors operating at the individual level. However, more recent work suggests that these behaviors are shaped not only by individual-level factors, but also by the environment in which they occur (Bluthenthal et al., 2007; Cooper et al., 2011; Genereux et al., 2010; Hutchinson et al., 2000; Latkin et al., 2005; Rockwell et al., 1999; Schilling et al., 2004). Several authors have written conceptual papers describing how HIV risk is influenced by contextual factors, but the paradigm most often cited is that proposed by Rhodes and colleagues in their writings on the risk environment (Galea et al., 2003; Poundstone et al., 2004; Rhodes et al., 2005). According to this paradigm, the risk environment is the space in which physical, social, political, and economic factors exogenous to the individual interact to shape the transmission of blood borne viruses (BBVs) among PWID.
One element of the risk environment that remains understudied in the context of high-risk injection behavior is neighborhood socioeconomic disadvantage. A review of the literature suggests that neighborhood disadvantage may influence high-risk injection behavior through a variety of pathways. For example, disadvantaged neighborhoods may exhibit higher levels of neighborhood social disorder than those that are relatively better off. Neighborhood social disorder may, in turn, impose psychological distress on PWID (Latkin and Curry, 2003), making them more likely to engage in unsafe injection behaviors (Latkin et al., 2005). Similarly, disadvantaged neighborhoods may also have larger populations of PWID, allowing injectors to form larger, denser injection networks. Both network size and network density have been shown to be associated with syringe sharing (De et al., 2007), potentially increasing the likelihood of high-risk injection behavior in poor areas. Although many hypotheses link neighborhood disadvantage to more unsafe injection practices, it is important to note that this exposure may also be protective. HIV prevention interventions like syringe exchange programs (SEPs) may be more common in disadvantaged neighborhoods where drug activity is traditionally higher. These interventions may promote safer injection behaviors in poor areas by increasing sterile syringe access and educating PWID on the risks of syringe sharing (Gibson et al., 2001).
To date, at least two studies have investigated associations between neighborhood disadvantage and high-risk injection behavior, each yielding different results. The first, conducted among PWID in the San Francisco Bay area, found that census tract-level measures of socioeconomic disadvantage were not associated with receptive syringe sharing (Bluthenthal et al., 2007). Conversely, the second found that neighborhood-level measures of poverty were associated with high-risk injection behavior among inner-city PWID in Montreal, Canada (Genereux et al., 2010). Interestingly, the associations detected in the Montreal-based study for neighborhood poverty and neighborhood educational attainment were in opposite directions. Both poverty and higher educational attainment were linked to more high-risk injection behavior. Together, these results offer conflicting perspectives as to whether neighborhood disadvantage influences injection practices, and if so, how.
In addition to emphasizing the role of contextual factors on individual-level behavior among PWID, the risk environment paradigm also emphasizes the interplay of these factors in shaping outcomes (Rhodes et al., 2005). With this in mind, it is helpful to examine how neighborhood socioeconomic disadvantage operates in the context of other area-level influences on high-risk injection behavior. Previous research has identified two area-level characteristics that warrant consideration: syringe exchange program (SEP) accessibility and drug-related police activity. Studies have shown that the proximity of injectors’ residences to SEP sites is associated with decreased syringe sharing (Cooper et al., 2011; Gindi et al., 2009; Hutchinson et al., 2000; Rockwell et al., 1999; Williams and Metzger, 2010), while drug-related police activity has been linked to increased high-risk injection behavior (Bluthenthal et al., 1999a; Bluthenthal et al., 1999b).
To better understand the role of the neighborhood environment in the etiology of high-risk injection behavior in PWID, we examined associations between common measures of neighborhood socioeconomic disadvantage and high-risk injection behavior among a sample of PWID in New York City. In addition, we examined whether these associations were modified by SEP accessibility and drug-related police activity.
2. Methods
2.1 Subjects and Setting
The current analyses use data from the Pharmacists as Resources Making Links to Community Services (PHARM-Link) study, which has been described elsewhere (Rivera et al., 2010). Briefly, the PHARM-Link study is a pharmacy-randomized intervention trial conducted among pharmacies participating in New York State’s Expanded Syringe Access Program (ESAP) – a program permitting the sale of non-prescription syringes to PWID. The purpose of the PHARM-Link study was to evaluate the impact of pharmacy-delivered referrals to health and social services on outcomes among pharmacy staff and PWID. ESAP-registered pharmacies in high drug activity neighborhoods in Brooklyn, Queens, Manhattan, and the Bronx were invited to participate. A total of 55 pharmacies were randomized to intervention and primary control arms. Intervention pharmacies offered PWID referrals to health and social services via print materials and a drug user-specific web resource guide, while primary control pharmacies offered only standard syringe sales services. PWID were recruited into PHARM-Link when visiting study pharmacies to purchase nonprescription syringes. During syringe transactions with PWID, pharmacy staff were trained to discreetly describe the PHARM-Link study and to offer a study appointment with research staff within one week of the pharmacy visit. PWID who were at least 18 years of age were eligible to participate. At the study appointment, research staff obtained informed consent and invited participants to complete a 45-minute Audio Computer Assisted Self Interview (ACASI) that ascertained data on a variety of topics, including socio-demographic characteristics, drug use history, HIV risk behaviors, syringe access and disposal practices, and history of access to medical and social services. Participants were compensated with $20 and a round-trip Metrocard for completion of the survey. Baseline data collection was conducted between March 2009 and October 2010. Participants who completed baseline surveys were invited to complete follow-up surveys at 3 months. The PHARM-Link study was approved by the institutional review boards at the New York Academy of Medicine and Columbia University. The current analyses are restricted to data collected at the baseline time point from participants who reported injection of illicit drugs in the three months prior to interview. Analyses include PWID recruited in both the intervention and primary control pharmacies.
2.2 Individual-Level Measures
2.2.1 High-Risk Injection Behaviors
The dependent variables in this analysis were the following high-risk injection behaviors: unsterile syringe use, receptive syringe sharing, and the acquisition of syringes from unsafe sources (Table 1). Unsterile syringe use includes both receptive syringe sharing and injectors’ reuse of their own syringes. This behavior was measured using the following item: “In the past three months, how often did you use a syringe that you were absolutely sure had not been used by anyone, not even yourself?” Participants were asked to respond to this item on a 6-point Likert scale ranging from “Never” to “Always.” Responses were dichotomized so that participants who endorsed any option other than “Always” were considered to have engaged in unsterile syringe use. Similarly, receptive syringe sharing was measured using the following item: “In the past three months, how often did you use a syringe that you knew someone had used before you?” Participants were asked to respond to this item on a 6-point Likert scale ranging from “Never” to “Always.” Responses were dichotomized so that participants who endorsed any option other than “Never” were considered to have engaged in receptive syringe sharing. Finally, to assess the acquisition of syringes from unsafe sources, participants were asked to report the frequency with which they obtained syringes from friends, relatives, syringe dealers, and shooting galleries in the past three months, using a 7-point Likert scale ranging from “Never” to “Everyday.” Responses were dichotomized so that participants who reported any frequency except “Never” for obtaining syringes from any of these sources were categorized as having used an unsafe syringe source.
Table 1.
Summary of key variables included in analyses
| Variable | Data Source | Operationalization |
|---|---|---|
| Individual-level Measures | ||
| High-risk injection behaviorsa | ||
| Receptive syringe sharing | PHARM-Link Survey | Any use of a syringe that the participant knew had been used by someone else in the past 3 months |
| Unsterile syringe use | PHARM-Link Survey | Any use of a syringe that was potentially non-sterile in the past 3 months |
| Use of unsafe syringe source | PHARM-Link Survey | Any acquisition of a syringe from a friend, relative, syringe dealer, or shooting gallery in the past 3 months |
| Neighborhood-level Measures | ||
| Neighborhood socioeconomic disadvantageb | ||
| % poverty | American Community Survey | Percent of neighborhood residents whose income in the past 12 months is below the poverty level |
| % public assistance | American Community Survey | Percent of neighborhood residents receiving public assistance |
| % low education | American Community Survey | Percent of neighborhood residents greater than 25 years of age without a high school diploma |
| % unemployed | American Community Survey | Percent of neighborhood residents greater than 16 years of age who are unemployed |
| % residential instability | American Community Survey | Percent of neighborhood residents living in a different house than 1 year ago |
| Neighborhood deprivation index | American Community Survey | Index calculated using the following neighborhood-level characteristics: percent of residents living in poverty, percent receiving public assistance, percent unemployed, and percent of households that are female-headed |
| Syringe exchange program accessibilityc | NYS Department of Health | Log of distance from the participant's street intersection to the nearest SEP in meters |
| Drug-related police activityc | NYS Division of Criminal Justice Services | Number of drug-related arrests per 1000 adult residents in the community district |
High-risk injection behaviors were the main dependent variables in this analysis and were entered into models in dichotomous form.
Measures of neighborhood socioeconomic disadvantage were the main independent variables in this analysis and were entered into models in continuous form.
Syringe exchange program accessibility and drug-related police activity were used as effect modifiers in this analysis and were entered into models in continuous form.
2.2.2 Individual-Level Covariates
On the basis of previous research regarding injection risk behavior among PWID, the following individual-level covariates were evaluated as potential confounders of associations between neighborhood socioeconomic disadvantage and high-risk injection behavior: age (continuous), gender (male/female), race (black/Latino/white or other), education (high school graduate or GED/less than high school), income (continuous), PHARM-Link randomization group (intervention/primary control), homelessness in the past 6 months (yes/no), sexual orientation (gay, lesbian, or bisexual/heterosexual), HIV status (positive/negative or unknown), and injection frequency (daily/less than daily).
2.3 Neighborhood-Level Measures
2.3.1 Neighborhood Socioeconomic Disadvantage
Participants’ neighborhoods were defined using data collected on the PHARM-Link survey. Each participant was asked to report the street intersection “where you spend most of your time.” Street intersections falling within New York City boundaries were geocoded in ArcGIS 10.1, and circular buffers with radii of 0.5 km were drawn around each intersect ion to approximate neighborhoods. A 0.5 km-buffer, corresponding to a 10-minute walking distance, has generally been accepted as a reasonable approximation of the size of the local area to which the average neighborhood resident is exposed (Cooper et al., 2009; Genereux et al., 2010; Rockwell et al., 1999).
Indicators of neighborhood socioeconomic disadvantage were created using the buffers in conjunction with census tract-level data from the 2006–2010 American Community Survey 5-year estimates. The American Community Survey (ACS) is a nationwide, continuous survey administered by the US Census Bureau to collect data on the demographic, housing, social, and economic characteristics of the US population (US Census Bureau, 2013). Because the area within each buffer included parts of multiple census tracts, census-tract level data from the ACS were used in combination with the area of the census tract parts within each buffer to calculate an area-weighted mean for each socioeconomic indicator. These area-weighted means were used as measures of neighborhood disadvantage for each individual in the analysis.
The following neighborhood-level factors were considered as exposures of interest: percent of residents living in poverty, percent receiving public assistance, percent with low education, percent >16 years of age unemployed, percent residential instability, and an index of neighborhood deprivation (Table 1). The neighborhood deprivation index was calculated using four census tract-level characteristics abstracted from the 2006–2010 ACS: percent of residents living in poverty, percent receiving public assistance, percent >16 years of age unemployed, and percent of households that are female-headed. These variables were standardized to the study sample using Z-scores and summed to calculate an index score. Indices similar to this one have been used in a variety of studies to measure neighborhood socioeconomic disadvantage (Boardman et al., 2001; Jacobson, 2006).
2.3.2 Syringe Exchange Program Accessibility
As a measure of SEP accessibility, distances were calculated from street intersections reported by PHARM-Link participants to the nearest authorized SEP site (Table 1). A list of authorized SEP sites operating in New York City in February 2010 was obtained from the New York State Department of Health. A total of 40 SEP sites were geocoded in ArcGIS 10.1, and distances from street intersections to the nearest SEP site were calculated along the street network in meters. Distances were log-transformed for inclusion in statistical analyses.
2.3.3 Drug-Related Police Activity
As a measure of the intensity of drug-related police activity, the number of drug-related arrests per 1000 adult residents was calculated within community districts (42 named neighborhood units within New York City) (Table 1). Data on the number of drug-related arrests occurring among adults in New York City police precincts in 2010 were obtained from the New York State Division of Criminal Justice Services. Arrests were included if the most serious charge was a misdemeanor or felony offense for the possession, sale, or use of illicit drugs, drug paraphernalia, or a controlled substance. Precinct-level arrest rates per 1000 adult residents were calculated by dividing the number of drug-related arrests within each precinct by the precinct population ≥ 16 years of age and multiplying by 1000. Area-weighted means were used to aggregate precinct-level arrest rates to the community district level.
2.4 Analytic Sample
A total of 592 participants completed the PHARM-Link survey. Of these, 61 reported insufficient data for geocoding (10.3%), 54 were missing data on one or more individual-level covariates (9.1%), and 1 was missing data on high-risk injection behavior (0.2%). Our final analytic sample contained 484 participants, or 81.7% of the original sample. Participants included in the analysis sample were recruited from 32 pharmacies, with each pharmacy recruiting a median of 11.5 participants. Participants excluded for missing data were similar to the analytic sample with two exceptions. Excluded participants were younger than those included in the analysis and more likely to report their sexual orientation as gay, lesbian, or bisexual.
2.5 Statistical Analysis
Associations between neighborhood socioeconomic disadvantage and high-risk injection behavior were measured using Poisson regression with robust error variance. These models were chosen instead of logistic regression due to the high prevalence of the outcomes in our analytic sample (23%–49%). Because odds ratios do not approximate risk ratios in the setting of common outcomes, Poisson regression was used to estimate risk ratios directly (Spiegelman and Hertzmark, 2005).
Unadjusted associations were estimated between all measures of neighborhood socioeconomic disadvantage and high-risk injection behavior. In adjusted analyses, each measure of neighborhood socioeconomic disadvantage was entered into a separate model with each indicator of high-risk injection behavior. Individual-level covariates were chosen for inclusion in adjusted analyses using the following strategy. All analyses were controlled for age, gender, race, education, and income. Any remaining individual-level covariates that were associated with a high-risk injection behavior at the p<0.10 level in bivariable analyses were also included in adjusted models. The additional covariates included in final models were homelessness, sexual orientation, and injection frequency. PHARM-Link randomization group was not associated with any high-risk injection behavior, and therefore, was not included in final models.
Log of distance to the nearest SEP and drug-related arrest rates were evaluated as potential modifiers of associations between neighborhood socioeconomic disadvantage and high-risk injection behavior. Effect modification was assessed by entering cross-product terms for measures of neighborhood disadvantage and effect modifiers into adjusted models of high-risk injection behavior. Both log of distance to the nearest SEP and drug-related arrest rates were entered into models in continuous form. All analyses were conducted in SAS 9.3.
3. Results
3.1 Sample Characteristics
Table 2 describes individual-level characteristics of PHARM-Link participants included in this analysis. Characteristics are given for the full sample and stratified by neighborhood socioeconomic disadvantage, where high and low groups were created by dichotomizing the neighborhood deprivation index at the median. Participants were 73.1% male with a mean age of 43.5 years. Individuals from low disadvantage neighborhoods were more likely to report both receptive syringe sharing (26.5% vs. 18.6%) and unsterile syringe use (52.1% vs. 46.3%) in the past three months, whereas use of any unsafe syringe source was nearly equal across low and high disadvantage groups (27.7% vs. 27.3%).
Table 2.
Descriptive characteristics of PHARM-Link study participants by level of neighborhood socioeconomic disadvantage (N=484)
| Characteristic | Total (N=484) |
Low neighborhood disadvantagea (N=242) |
High neighborhood disadvantagea (N=242) |
p-valueb | |
|---|---|---|---|---|---|
| No. (%) or Mean (SD) | |||||
| Age | 43.5 (9.3) | 43.9 (9.9) | 43.1 (8.7) | 0.38 | |
| Male | 354 (73.1%) | 178 (73.6%) | 176 (72.7%) | 0.84 | |
| Race/ethnicity | <.0001c | ||||
| Hispanic/Latino (regardless of race) | 251 (51.9%) | 85 (35.1%) | 166 (68.6%) | ||
| Non-Hispanic Black | 129 (26.7%) | 82 (33.9%) | 47 (19.4%) | ||
| Non-Hispanic White and other | 104 (21.5%) | 75 (31.0%) | 29 (12.0%) | ||
| Less than high school diploma/GED | 179 (37.0%) | 86 (35.5%) | 93 (38.4%) | 0.51 | |
| Income in the past year | 8951 (10412) | 9556 (11219) | 8347 (9522) | 0.20 | |
| Homeless in the past 6 months | 162 (33.5%) | 88 (36.4%) | 74 (30.6%) | 0.18 | |
| Gay, lesbian, or bisexual | 52 (10.7%) | 28 (11.6%) | 24 (9.9%) | 0.56 | |
| Injected daily in the past 3 months | 167 (34.5%) | 77 (31.8%) | 90 (37.2%) | 0.21 | |
| HIV positive | 63 (13.0%) | 16 (6.6%) | 47 (19.6%) | <.0001c | |
| PHARM-Link intervention group | 225 (46.5%) | 130 (53.7%) | 95 (39.3%) | 0.0014c | |
| High-risk injection behaviors (in the past 3 months) | |||||
| Receptive syringe sharing | 109 (22.5%) | 64 (26.5%) | 45 (18.6%) | 0.04c | |
| Unsterile syringe use | 238 (49.2%) | 126 (52.1%) | 112 (46.3%) | 0.20 | |
| Use of unsafe syringe source | 133 (27.5%) | 67 (27.7%) | 66 (27.3%) | 0.92 | |
Low and high neighborhood disadvantage groups were created by dichotomizing the neighborhood deprivation index at the median. Low neighborhood disadvantage is defined as a neighborhood deprivation index below the median (< 0.3), and high neighborhood disadvantage is at or above the median (≥ 0.3).
p-value for comparison of low and high neighborhood disadvantage groups. p-values are from t-tests for continuous variables and Chi-square tests for categorical variables.
p < 0.05
Table 3 describes measures of neighborhood socioeconomic disadvantage, SEP accessibility, and drug-related police activity for participants in the analytic sample. As described above, each of these measures was created using the street intersection at which participants reported spending most of their time. Street intersections were reported in Manhattan, Bronx, Brooklyn, and Queens. The range of socioeconomic disadvantage represented by neighborhoods surrounding these intersections was relatively wide. The proportion of residents living in poverty, for example, ranged from less than 10% to greater than 50% in the analysis sample. More than half of the study sample reported street intersections located within one kilometer of a SEP. Street intersections also tended to lie within community districts whose drug-related arrests rates were higher than the New York City average.
Table 3.
Characteristics of geographic areas surrounding street intersections reported by PHARM-Link study participants (N=484)
| Characteristic | Mean (SD) |
Minimum | 25th percentile |
50th percentile |
75th percentile |
Maximum | |
|---|---|---|---|---|---|---|---|
| Neighborhood socioeconomic disadvantage | |||||||
| % poverty | 31.3 (10.0) | 4.0 | 26.2 | 30.3 | 40.0 | 50.7 | |
| % public assistance | 8.0 (3.9) | 0.2 | 5.4 | 7.4 | 11.3 | 15.5 | |
| % low education | 30.9 (12.0) | 1.8 | 21.4 | 33.3 | 40.7 | 51.0 | |
| % unemployed | 12.7 (4.2) | 3.4 | 9.7 | 12.8 | 15.6 | 21.5 | |
| % residential instability | 12.7 (4.9) | 3.9 | 9.4 | 11.8 | 14.8 | 32.6 | |
| Neighborhood deprivation index | 0.1 (3.7) | −9.2 | −2.1 | 0.3 | 2.7 | 7.3 | |
| Distance to the nearest SEP (m) | 1161 (1153) | 5 | 413 | 861 | 1423 | 8233 | |
| Log of distance to the nearest SEP | 6.7 (1.0) | 1.6 | 6.0 | 6.8 | 7.3 | 9.0 | |
| Drug-related arrests per 1000 adults | 34.9 (16.6) | 1.1 | 26.7 | 38.2 | 49.0 | 64.6 | |
3.2 Neighborhood Socioeconomic Disadvantage and High-Risk Injection Behavior
Table 4 presents both unadjusted and adjusted associations between measures of neighborhood socioeconomic disadvantage and high-risk injection behavior in the past three months. In unadjusted models, the percentage of residents receiving public assistance, percentage unemployed, and neighborhood deprivation index were each independently associated with decreased receptive syringe sharing. After the addition of individual-level covariates, these associations remained statistically significant.
Table 4.
Unadjusted and adjusted associations between indicators of neighborhood socioeconomic disadvantage and high-risk injection behavior among PHARM-Link study participants (N=484)
| Receptive syringe sharing | Unsterile syringe use | Use of unsafe syringe source | ||||
|---|---|---|---|---|---|---|
| Unadjusted RR (95% CI) |
Adjusted RR (95% CI) |
Unadjusted RR (95% CI) |
Adjusted RR (95% CI) |
Unadjusted RR (95% CI) |
Adjusted RR (95% CI) |
|
| % poverty | 0.86 (0.73, 1.02) | 0.84 (0.70, 1.01) | 0.93 (0.85, 1.01) | 0.91 (0.83, 1.00) | 0.97 (0.85, 1.11) | 0.98 (0.84, 1.14) |
| % public assistance | 0.60 (0.40, 0.90)a | 0.56 (0.36, 0.88)a | 0.81 (0.65, 1.02) | 0.78 (0.61, 1.00) | 0.88 (0.62, 1.25) | 0.91 (0.63, 1.32) |
| % low education | 0.89 (0.78, 1.02) | 0.87 (0.75, 1.00) | 0.94 (0.87, 1.01) | 0.92 (0.85, 0.98)a | 0.98 (0.87, 1.11) | 0.99 (0.86, 1.13) |
| % unemployed | 0.62 (0.41, 0.93)a | 0.56 (0.37, 0.86)a | 0.81 (0.65, 1.01) | 0.79 (0.63, 0.99)a | 0.84 (0.60, 1.17) | 0.77 (0.53, 1.10) |
| % residential instability | 0.98 (0.69, 1.41) | 0.96 (0.67, 1.38) | 1.01 (0.84, 1.22) | 1.02 (0.85, 1.23) | 0.96 (0.70, 1.32) | 0.94 (0.69, 1.29) |
| Neighborhood deprivation index | 0.82 (0.69, 0.98)a | 0.79 (0.65, 0.96)a | 0.91 (0.83, 1.01) | 0.89 (0.81, 0.99)a | 0.94 (0.81, 1.09) | 0.93 (0.79, 1.10) |
p < 0.05
Note: Values shown are risk ratios and 95% confidence intervals for 10% increases (e.g., 10% to 20%) in indicators of neighborhood socioeconomic disadvantage, with the exception of neighborhood deprivation index. For neighborhood deprivation index, risk ratios were estimated for 4-unit increases. Adjusted models were controlled for the following individual-level confounders: age, gender, race, education, income, homelessness, sexual orientation, and injection frequency.
Although measures of neighborhood socioeconomic disadvantage were not significantly associated with unsterile syringe use in unadjusted models, the percentage of residents with low education, percentage unemployed, and neighborhood deprivation index were all associated with decreased unsterile syringe use in adjusted models.
No statistically significant associations were identified between measures of neighborhood socioeconomic disadvantage and the use of unsafe syringe sources.
3.3 Effect Modification by SEP Accessibility and Drug-Related Police Activity
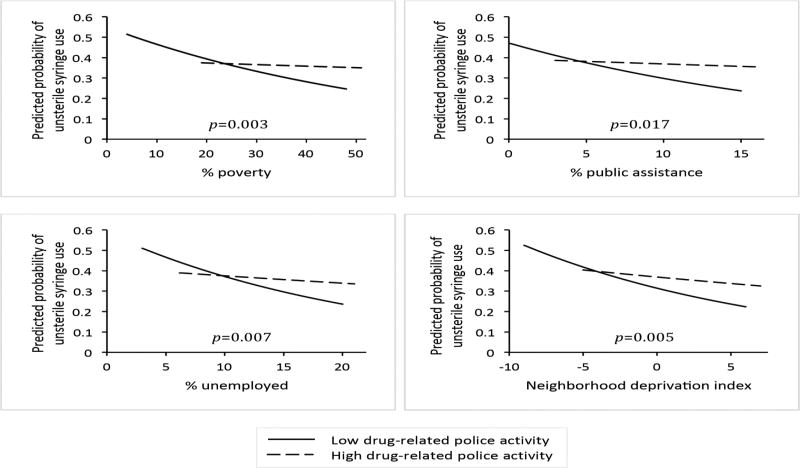
Effect modification was detected between measures of neighborhood socioeconomic disadvantage and drug-related police activity in models of unsterile syringe use. When drug-related arrest rates were low (25th percentile), the percentage of residents living in poverty was associated with less unsterile syringe use (RR=0.85 per 10% increase in percent poverty). However, when drug-related arrest rates were high (75th percentile), the protective influence of percentage in poverty was attenuated, and its association with unsterile syringe use was essentially null (RR=0.98). The interaction between percentage of residents in poverty and drug-related arrests was statistically significant (p=0.0034). As shown in Figure 1, similar patterns were observed for the percentage receiving public assistance, percentage unemployed, and neighborhood deprivation index.
Figure 1.
Effect modification of associations between indicators of neighborhood socioeconomic disadvantage and unsterile syringe use by drug-related police activity. Predicted probabilities of unsterile syringe use were estimated when drug-related arrest rates per 1000 adults were fixed at the 25th percentile (low drug-related police activity) and the 75th percentile (high drug-related police activity). Models were adjusted for the following individual-level confounders: age, gender, race, education, income, homelessness, sexual orientation, and injection frequency. Interaction p-values are from significance tests of cross-product terms entered into adjusted models.
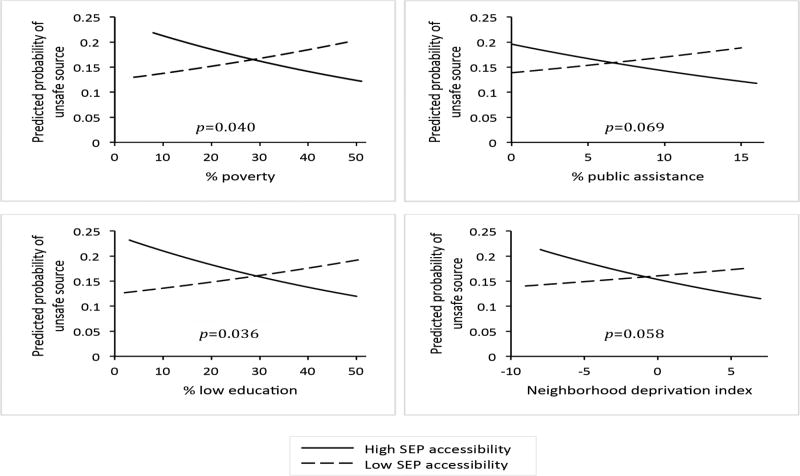
SEP accessibility was also identified as a modifier of associations between measures of neighborhood socioeconomic disadvantage and use of unsafe syringe sources. When distance to the nearest SEP was low (25th percentile), the percentage of residents living in poverty was associated with less use of unsafe syringe sources (RR=0.87 per 10% increase in percent poverty). Conversely, when distance to the nearest SEP was high (75th percentile), the association changed direction, and the percentage of residents in poverty was associated with increased use of unsafe syringe sources (RR=1.10). The cross-product term for percentage of residents in poverty and distance to the nearest SEP was statistically significant (p=0.0409). Similar patterns were observed for percentage receiving public assistance, percentage with low education, and neighborhood deprivation index, although not all interactions reached statistical significance (Figure 2).
Figure 2.
Effect modification of associations between indicators of neighborhood socioeconomic disadvantage and the use of unsafe syringe sources by SEP accessibility. Predicted probabilities of the use of unsafe syringe sources were estimated when distance to the nearest SEP was fixed at the 25th percentile (high SEP accessibility) and the 75th percentile (low SEP accessibility). Models were adjusted for the following individual-level confounders: age, gender, race, education, income, homelessness, sexual orientation, and injection frequency. Interaction p-values are from significance tests of cross-product terms entered into adjusted models.
4. Discussion
In this sample of urban PWID in New York City, neighborhood socioeconomic disadvantage was associated with safer injection behaviors. PWID in disadvantaged areas had a lower risk of receptive syringe sharing and unsterile syringe use than their counterparts in neighborhoods that were relatively better off. Interestingly, the direction of these associations was contrary to what we and other authors would predict (Buchanan et al., 2003; Galea et al., 2003). Hypotheses regarding the influence of neighborhood disadvantage on health commonly associate poverty with poorer health outcomes and riskier behaviors. However, our results suggest the opposite in the context of high-risk injection behavior, inviting future work to explore how socioeconomically disadvantaged areas may decrease injection risk among PWID.
The inverse association we observed between neighborhood disadvantage and high-risk injection behavior may be explained by several potential mechanisms. As described in the introduction, PWID in disadvantaged neighborhoods may have greater access to sterile syringes from SEPs than their counterparts in less disadvantaged neighborhoods. As a result, they may be less likely to engage in high-risk behaviors like syringe sharing and unsterile syringe use (Gibson et al., 2001). Alternatively, our results may be explained by injection drug use-related stigma. Because injection drug use is likely more common in disadvantaged neighborhoods, the stigma associated with this behavior may be lower in poor neighborhoods than in those that are relatively better off. As a result, PWID in poor neighborhoods may face fewer barriers to accessing sterile syringes from SEPs and pharmacies. Increased syringe access may subsequently lead to safer injection behaviors. Consistent with these hypotheses, at least two studies have found that drug use-related stigma is associated with riskier injection practices (Latkin et al., 2010; Rivera et al., 2014). Finally, neighborhood disadvantage may be linked to decreased receptive syringe sharing and unsterile syringe use by differences in HIV risk perception. PWID in poor areas with higher prevalences of HIV may perceive a greater risk of HIV transmission associated with syringe sharing than those in less disadvantaged neighborhoods that have been less affected by the HIV epidemic. For this reason, PWID in poor areas may be less likely to engage in high-risk injection behavior. This pathway is a plausible explanation of our results as the prevalence of HIV among participants in high disadvantage neighborhoods was nearly three times that in low disadvantage neighborhoods (19.6% vs. 6.6%) (Table 2).
Our analyses also found that the inverse association between neighborhood disadvantage and unsterile syringe use was attenuated by drug-related police activity. Of note, the associations between neighborhood disadvantage and receptive syringe sharing were not modified by drug-related arrest rates, indicating that modification effects on unsterile syringe use were attributable to increased reuse of injectors’ own syringes. Together, these results suggest that drug-related police activity is a barrier to sterile syringe access among PWID. Injectors who are deterred from acquiring new syringes at SEPs or pharmacies by a fear of police encounters may compensate for decreased syringe access by reusing their own injection equipment. These findings are not surprising, given the wealth of research linking drug-related police activity to decreases in SEP attendance and increases in high-risk injection behavior (Beletsky et al., 2014; Bluthenthal et al., 1999a; Bluthenthal et al., 1997; Bluthenthal et al., 1999b; Davis et al., 2005; Small et al., 2006).
Effect modification was also detected between neighborhood socioeconomic disadvantage and distance to the nearest SEP in models of the use of unsafe syringe sources (Figure 2). Among PWID who spent time close to an SEP site, neighborhood disadvantage was associated with decreased use of unsafe syringe sources. However, as distance to the nearest SEP site increased, neighborhood disadvantage became associated with increased use of unsafe syringe sources. This result is consistent with previous work linking SEP proximity to increased SEP participation and highlights the importance of SEPs as alternatives to unsafe syringe sources in disadvantaged neighborhoods (Gindi et al., 2009; Rockwell et al., 1999; Williams and Metzger, 2010).
The findings from this study should be considered in light of a number of limitations. First, our data are cross-sectional, which prevents us from establishing the temporality and causality of relations between neighborhood socioeconomic disadvantage and high-risk injection behavior. This is a common limitation of analyses investigating neighborhood-level characteristics due to the difficulty of studying neighborhoods longitudinally. Second, self-reported data were used to create measures of high-risk injection behavior. Although this approach introduces the possibility of bias, previous studies have shown that self-reported measures of injection risk behavior are accurate and reliable (Darke, 1998). Third, the findings from our study may have limited external validity. Participants in our sample were recruited while purchasing syringes from pharmacies, which suggests that they may engage in fewer high-risk injection behaviors than PWID in the general population who do not use safe syringe sources. In addition, our study was conducted in New York City, where syringe availability is high and HIV prevention services are extensive in comparison to other parts of the US. Taken together, these circumstances indicate that the findings from our analyses are not broadly generalizable. However, the sale of non-prescription syringes has been legalized in several states, creating new populations of pharmacy-using PWID across the country. Understanding the influence of neighborhood context on patterns of risk behavior in this group will continue to be important. Furthermore, as harm reduction approaches to addressing injection drug use become more commonplace, populations of PWID in urban areas will more closely resemble those in New York City.
In this study, we sought to explore how one aspect of the neighborhood context – socioeconomic disadvantage – may influence high-risk injection behavior. Our results highlight the importance of the risk environment in shaping injection behavior and BBV transmission among PWID. Additional studies are needed to investigate how aspects of the risk environment and their interplay influence individual-level behavior. A better understanding of these relations will be instrumental in designing policy interventions geared toward eliminating BBV transmission among PWID.
Highlights.
Neighborhood disadvantage was associated with safer injection behaviors.
Police activity attenuated the protective influence of neighborhood disadvantage.
Syringe exchange program (SEP) access modified associations between disadvantage and injection risk behavior.
Acknowledgments
Role of Funding Source
This study was funded by the National Institute on Drug Abuse (R01DA022144). Gina S. Lovasi was also funded by a generous gift from Dana and David Dornsife to the Drexel University Dornsife School of Public Health and a K-01 grant from the National Institute of Child Health and Human Development (G.S.L., grant K01HD067390). These funding entities had no further role in the design of this study; in the collection, analysis and interpretation of data; in the writing of this manuscript; or in the decision to submit this paper for publication.
The authors thank study participants for their time and research staff for their data collection efforts.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Jennifer DeCuir designed the study, analyzed the data, interpreted the results, and wrote the manuscript. Gina S. Lovasi contributed to the design of the analysis plan. Crystal Fuller Lewis supervised the data collection. All authors contributed to subsequent drafts and approved the final manuscript.
Conflict of Interest
The authors declare no conflict of interest.
References
- Beletsky L, Heller D, Jenness SM, Neaigus A, Gelpi-Acosta C, Hagan H. Syringe access, syringe sharing, and police encounters among people who inject drugs in New York City: A community-level perspective. Int. J. Drug Policy. 2014;25:105–111. doi: 10.1016/j.drugpo.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Do DP, Finch B, Martinez A, Edlin BR, Kral AH. Community characteristics associated with HIV risk among injection drug users in the San Francisco Bay Area: A multilevel analysis. J. Urban Health. 2007;84:653–666. doi: 10.1007/s11524-007-9213-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Kral AH, Erringer EA, Edlin BR. Drug paraphernalia laws and injection-related infectious disease risk among injectors. J. Drug Issues. 1999a;29:1–16. [Google Scholar]
- Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: A look at Oakland and San Francisco. Med. Anthropol. 1997;18:61–83. doi: 10.1080/01459740.1997.9966150. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Lorvick J, Kral A, Erringer E, Kahn J. Collateral damage in the war on drugs: HIV risk behaviors among injection drug users. Int. J. Drug Policy. 1999b;10:25–38. [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. J. Health Soc. Behav. 2001;42:151–165. [PubMed] [Google Scholar]
- Buchanan D, Shaw S, Teng W, Hiser P, Singer M. Neighborhood differences in patterns of syringe access, use, and discard among injection drug users: Implications for HIV outreach and prevention education. J. Urban Health. 2003;80:438–454. doi: 10.1093/jurban/jtg050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Bossak B, Tempalski B, Des Jarlais DC, Friedman SR. Geographic approaches to quantifying the risk environment: Drug-related law enforcement and access to syringe exchange programmes. Int. J. Drug Policy. 2009;20:217–226. doi: 10.1016/j.drugpo.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Des Jarlais DC, Ross Z, Tempalski B, Bossak B, Friedman SR. Spatial access to syringe exchange programs and pharmacies selling over-the-counter syringes as predictors of drug injectors' use of sterile syringes. Am. J. Public Health. 2011;101:1118–1125. doi: 10.2105/AJPH.2009.184580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: A review. Drug Alcohol Depend. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Davis CS, Burris S, Kraut-Becher J, Lynch KG, Metzger D. Effects of an intensive street-level police intervention on syringe exchange program use in Philadelphia, PA. Am. J. Public Health. 2005;95:233–236. doi: 10.2105/AJPH.2003.033563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De P, Cox J, Boivin J-F, Platt RW, Jolly AM. The importance of social networks in their association to drug equipment sharing among injection drug users: A review. Addiction. 2007;102:1730–1739. doi: 10.1111/j.1360-0443.2007.01936.x. [DOI] [PubMed] [Google Scholar]
- Galea S, Ahern J, Vlahov D. Contextual determinants of drug use risk behavior: A theoretic framework. J. Urban Health. 2003;80:iii50–iii58. doi: 10.1093/jurban/jtg082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genereux M, Bruneau J, Daniel M. Association between neighbourhood socioeconomic characteristics and high-risk injection behaviour amongst injection drug users living in inner and other city areas in Montreal, Canada. Int. J. Drug Policy. 2010;21:49–55. doi: 10.1016/j.drugpo.2009.01.004. [DOI] [PubMed] [Google Scholar]
- Gibson DR, Flynn NM, Perales D. Effectiveness of syringe exchange programs in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS. 2001;15:1329–1341. doi: 10.1097/00002030-200107270-00002. [DOI] [PubMed] [Google Scholar]
- Gindi RM, Rucker MG, Serio-Chapman CE, Sherman SG. Utilization patterns and correlates of retention among clients of the needle exchange program in Baltimore, Maryland. Drug Alcohol Depend. 2009;103:93–98. doi: 10.1016/j.drugalcdep.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson SJ, Taylor A, Goldberg DJ, Gruer L. Factors associated with injecting risk behaviour among serial community-wide samples of injecting drug users in Glasgow 1990–94: Implications for control and prevention of blood-borne viruses. Addiction. 2000;95:931–940. doi: 10.1046/j.1360-0443.2000.9569319.x. [DOI] [PubMed] [Google Scholar]
- Jacobson JO. Do drug treatment facilities increase clients' exposure to potential neighborhood-level triggers for relapse? A small-area assessment of a large, public treatment system. J. Urban Health. 2006;83:150–161. doi: 10.1007/s11524-005-9013-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C, Srikrishnan AK, Yang C, Johnson S, Solomon SS, Kumar S, Celentano DD, Solomon S. The relationship between drug use stigma and HIV injection risk behaviors among injection drug users in Chennai, India. Drug Alcohol Depend. 2010;110:221–227. doi: 10.1016/j.drugalcdep.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Curry AD. Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. J. Health Soc. Behav. 2003;44:34–44. [PubMed] [Google Scholar]
- Latkin CA, Williams CT, Wang J, Curry AD. Neighborhood social disorder as a determinant of drug injection behaviors: a structural equation modeling approach. Health Psychol. 2005;24:96–100. doi: 10.1037/0278-6133.24.1.96. [DOI] [PubMed] [Google Scholar]
- Normand J, Vlahov D, Moses L. Preventing HIV transmission: The role of sterile needles and bleach. Washington DC: 1995. [PubMed] [Google Scholar]
- Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol. Rev. 2004;26:22–35. doi: 10.1093/epirev/mxh005. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc. Sci. Med. 2005;61:1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- Rivera AV, Blaney S, Crawford ND, White K, Stern RJ, Amesty S, Fuller C. Individual- and neighborhood-level factors associated with nonprescription counseling in pharmacies participating in the New York State Expanded Syringe Access Program. J. Am. Pharm. Assoc. 2010;50:580–587. doi: 10.1331/JAPhA.2010.09202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera AV, DeCuir J, Crawford ND, Amesty S, Lewis CF. Internalized stigma and sterile syringe use among people who inject drugs in New York City, 2010–2012. Drug Alcohol Depend. 2014;144:259–264. doi: 10.1016/j.drugalcdep.2014.09.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockwell R, Des Jarlais DC, Friedman SR, Perlis TE, Paone D. Geographic proximity, policy and utilization of syringe exchange programmes. AIDS Care. 1999;11:437–442. doi: 10.1080/09540129947811. [DOI] [PubMed] [Google Scholar]
- Schilling RF, Fontdevila J, Fernando D, El-Bassel N, Monterroso E. Proximity to needle exchange programs and HIV-related risk behavior among injection drug users in Harlem. Eval. Program Plann. 2004;27:25–33. [Google Scholar]
- Small W, Kerr T, Charette J, Schechter MT, Spittal PM. Impacts of intensified police activity on injection drug users: Evidence from an ethnographic investigation. Int. J. Drug Policy. 2006;17:85–95. [Google Scholar]
- Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am. J. Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. American Community Survey: Information guide 2013 [Google Scholar]
- Villano SA, Vlahov D, Nelson KE, Lyles CM, Cohn S, Thomas DL. Incidence and risk factors for hepatitis C among injection drug users in Baltimore, Maryland. J. Clin. Microbiol. 1997;35:3274–3277. doi: 10.1128/jcm.35.12.3274-3277.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CT, Metzger DS. Race and distance effects on regular syringe exchange program use and injection risks: a geobehavioral analysis. Am. J. Public Health. 2010;100:1068–1074. doi: 10.2105/AJPH.2008.158337. [DOI] [PMC free article] [PubMed] [Google Scholar]