Abstract
Recent guidelines concerning exercise for people with cancer provide evidence-based direction for exercise assessment and prescription for clinicians and their patients. Although the guidelines promote exercise integration into clinical care for people with cancer, they do not support strategies for bridging the guidelines with related resources or programs. Exercise program accessibility remains a challenge in implementing the guidelines, but that challenge might be mitigated with conceptual frameworks (“pathways”) that connect patients with exercise-related resources. In the present paper, we describe a pathway model and related resources that were developed by an expert panel of practitioners and researchers in the field of exercise and rehabilitation in oncology and that support the transition from health care practitioner to exercise programs or services for people with cancer. The model acknowledges the nuanced distinctions between research and exercise programming, as well as physical activity promotion, that, depending on the available programming in the local community or region, might influence practitioner use. Furthermore, the pathway identifies and provides examples of processes for referral, screening, medical clearance, and programming for people after a cancer diagnosis. The pathway supports the implementation of exercise guidelines and should serve as a model of enhanced care delivery to increase the health and well-being of people with cancer.
Keywords: Physical activity, exercise, rehabilitation, knowledge translation, care plans
INTRODUCTION
The safety and benefits of exercise after a cancer diagnosis are well documented. For cancer survivors, research has traditionally focused on the relationship between exercise and the various domains of quality of life. Recent surges in basic science describing antineoplastic properties of exercise have sought to explain the accumulating epidemiologic data that reveal cancer-specific survival advantages for individuals who are physically active compared with those who are not1,2. Collectively, the research into physical activity (pa) and exercise-related benefits for people with cancer is often called “convincing,” “compelling,” or “overwhelming” and has established the evidence base for pa or exercise endorsements and recommendations by oncology and exercise organizations alike2–4.
The American College of Sports Medicine’s exercise guidelines for people with cancer5 fundamentally resemble the World Health Organization’s pa guidelines for the healthy adult population6. The recommended weekly dose of moderate-to-vigorous exercise or pa is 150 minutes, with the specific caveats that “some physical activity is better than none” (p. 1410) and that “exercise prescriptions should be individualized according to a cancer survivor’s pre-treatment aerobic fitness, medical comorbidities, response to treatment, and the immediate or persistent negative effects of treatment that are experienced at any given time” (p. 1412)5.
The nuanced distinctions between pa and exercise are worth highlighting, given potential contextual differences in how their respective programming might be implemented into cancer care. Physical activity is defined as “any bodily movement produced by skeletal muscles that results in energy expenditure,” whereas exercise is defined as “a subset of pa that is planned, structured, and repetitive and has as a final or an intermediate objective the improvement or maintenance of physical fitness” (p. 126)7. In healthy people and in those with chronic disease, pa is recommended as a lifestyle behaviour for overall wellness and health promotion (the focus of the World Health Organization guidelines). In a clinical context, pa in the form of exercise plays a specific role in preparation for treatment (prehabilitation); in concurrent or adjuvant treatment to optimize health outcomes; in rehabilitation (inpatient or outpatient impairment-oriented exercise); and in ongoing health and wellness promotion in light of underlying morbidity (the focus of the American College of Sports Medicine guidelines).
To ensure safety and benefit, exercise prescriptions often must be tailored to accommodate the needs and capacity of the patient. Guideline implementation refers to “exercise” to denote purposeful engagement in structured pa by the cancer survivor in an effort to ameliorate current conditions and to protect against chronic and latent adverse effects. It should be noted that encouragement is given for a physically active lifestyle in addition to a structured exercise regimen.
Recent clinical practice guidelines from a regional cancer authority have further solidified the role of exercise in cancer care. The Cancer Care Ontario (cco) “exercise for people with cancer” guidelines8 contain additional evidence-based recommendations targeted toward health care practitioners (hcps):
■ The benefits of specific types of exercise
■ Recommendations for pre-exercise screening
■ Participant safety
■ Advice about models of exercise program delivery for patients throughout the cancer care continuum
The cco guidelines are directed toward hcps because of their point-of-care presence throughout the cancer journey, where they can support the promotion and facilitation of exercise.
Choosing the most appropriate hcp to discuss exercise with patients requires consideration, because hcps show some variability in terms of who is most able and likely to have an exercise conversation with a patient. Nyrop and colleagues9 found that, in 361 clinical encounters, 35% included hcp communication about pa or exercise and that, compared with other clinical specialists such as radiation and clinical oncologists, medical oncologists were most likely to discuss pa (55% of encounters vs. 20% of encounters). In a recent survey of oncology hcps, Nadler et al.10 found that nurses were most able to identify the cco guidelines (42%), followed by allied health staff (25%), physicians (24%), and radiation therapists (9%). Allied health staff felt the most able to encourage exercise and to identify when exercise was appropriate (63%), and 80% of all hcps agreed that exercise counselling should be a part of care. The top 3 strategies to promote exercise in oncology practice reported by respondents were more education for hcps (about indications, guidelines, referrals, and safety), educational handouts for the patient, and integration of a qualified exercise professional (qep) into the clinical team.
Despite the critical role of hcps in managing the broad spectrum of disease- and survivorship-related needs of cancer survivors, as well as a general acceptance that exercise is an effective therapeutic and supportive care strategy, engaging hcps to discuss exercise with their patients has been challenging. Common barriers to recommendations for exercise cited by oncology hcps include a lack of exercise-specific expertise; perceived patient indifference to exercise information or guidance; and likely most prominently, lack of time for exercise-related discussions amidst other clinical activity10–13. When exercise is discussed in interactions between hcps and cancer patients, the evidence suggests that such conversations only modestly affect pa and exercise behaviours. For example, of 15,000 patients treated for colorectal cancer in the U.K. National Health Service, 31% reported receiving pa advice, and they were subsequently only 5% more likely to meet pa guidelines14. In another recent study of more than 3300 cancer survivors, a hcp’s recommendation for pa was associated with a reduction of 8% in “inactive” patients and with an increase of 4% in the number of patients meeting the pa guidelines15. The authors of the latter study describe the interaction with hcps as a “window of opportunity” to increase the level of pa engagement by survivors; however, the strategy of simply making recommendations for pa apparently fails to adequately capitalize on the opportunity. Accordingly, strategies that are more directed might be necessary to effectively stimulate and support a greater proportion of cancer survivors to participate in exercise as a long-term adjuvant component of therapy. Evidence of the value of providing a recommendation and an outlet or resource for exercise compared with providing only the recommendation was seen in improved participation and patient outcomes in three recent trials in people with cancer16–18.
Consistent with the foregoing findings, the U.K. National Institute for Health and Care Excellence recommends that “policy makers fund exercise referral schemes for people who are sedentary or inactive and have existing health conditions (such as cancer) or other factors that put them at increased risk of ill health if: i) the scheme incorporates health-behaviour change principles that are contextualized to the patient; and ii) monitors and reports the scheme’s implementation and outcomes”19. The prevailing and complementary guidelines from the American College of Sports Medicine, cco, and the National Institute for Health and Care Excellence suggest that bridging the gap between sedentariness and exercise for people with chronic disease requires a more directed and systematic approach (“pathway”), including structured resources delivered or developed (or both) by qeps. Thus, a pathway to exercise as an adjuvant cancer therapy requires consideration of the facilitators and barriers already described, and specifically
■ incorporation of a team approach to exercise messaging and referrals that reduces the burden on the primary hcps in cancer care (namely, oncologists and oncology nurses);
■ local access to directed programming for cancer exercise and rehabilitation; and
■ self-management and behaviour change skills development or resources for long-term exercise or pa participation.
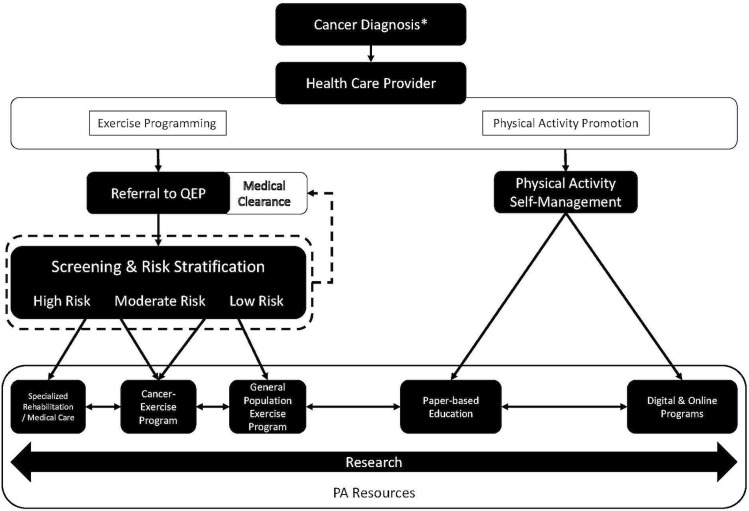
For the pathway to be effective, it requires further individualization to the complex personal, clinical, and environmental context of the patient so that it is safe, it addresses the patient’s needs and goals, and it can endure over the long term. It is with that lens that we present a patient pathway from an oncology-directed clinical setting to exercise programming or pa resources, or both (Figure 1). By providing a visual framework, the pathway can potentially support the implementation of exercise or pa guidelines that aim to improve patient outcomes.
FIGURE 1.
Cancer survivors can enter the pathway at any point after diagnosis. In addition, for those receiving palliative care or living with advanced cancer, the pathway could be instrumental for well-being and overall quality of life. QEP = qualified exercise professional; PA = physical activity.
THE PATHWAY
Pathway Background
The pathway is an exercise care-plan model intended to engage hcps and assist with providing care that includes appropriate and qualified exercise promotion and support for people with cancer. The pathway pertains to people diagnosed with cancer and their opportunities for improved physical, functional, and psychosocial well-being throughout the continuum of care—that is, not just at diagnosis. Specifically, the potential access points to the pathway can include before treatment (prehabilitation), during treatment, after treatment (at the short- and long-term survivorship time points alike), and in palliative care or life with advanced cancer.
The development of the pathway was a collaborative endeavour involving clinicians and scientists in the fields of cancer, exercise, and rehabilitation, plus members of cco’s Exercise for People with Cancer Guideline Working Group, who are involved in advancing exercise guidelines into practice. The pathway takes into account regional differences in accessibility to cancer exercise programs (for example, rural vs. urban), opportunities for “clinic to community” models of care, and the variability of health and well-being experienced by people with cancer. Ultimately, the pathway provides a model of shared responsibility for engaging patients in ways that improve their health through exercise and pa.
Pathway Steps
The HCP
In the pathway, “hcp” refers to a clinician responsible for managing health care throughout, or at any point during, the continuum of care after a cancer diagnosis. Increasing accessibility to exercise programs and pa resources for cancer survivors is the responsibility of the system and not any one hcp; thus, strategies that enable the entire care team to bridge the gap to exercise are needed. Creating the infrastructure or culture to support greater accessibility can be led by an oncologist (medical, surgical, radiation), a family physician, or other specialist receiving a referral in the cancer care setting, such as a cardiologist or physiatrist, depending on the setting, patient condition, timing of care, and physician aptitude for exercise or pa discussion and leadership. In addition, the hcp is not limited to the medical doctor, but can include nurses, psychologists, social workers, and members of the allied health care team who can provide the essential information or screening and can facilitate exercise or pa referrals. Ideally, the hcp can support the promotion of exercise during patient interactions and assess the context or opportunities for patient access to appropriate exercise resources, such as a referral to a qep, a cancer-exercise program, or available pa tools that can support self-management (for example, pamphlets, Web sites). The role of hcps in exercise promotion cannot be overstated: they represent the starting point for access to resources. That role is particularly crucial if patients have the opportunity to participate in a cancer-exercise program that requires referral or clearance to enrol.
It is worth highlighting that the qep might also be a hcp; however, for the purposes of the pathway, qeps are incorporated as “downstream” members of the team responsible for the delivery or development, or both,of resources and programming. Models and settings can vary, but cancertrained qeps play a central role in program delivery and are the resource within the comprehensive referral pathway for hcps. Similarly, hcps have reported being unaware of appropriate pa and exercise resources to which to refer their patients20,a, which might include the specific training and oncology expertise of qeps. A qep, such as a certified exercise physiologist or kinesiologist, requires at least an undergraduate degree in exercise or a related science and is recommended to have several hundred hours of clinical exercise physiology experience before being eligible to attempt licensing or certification exams. Beyond their general clinical exercise certifications, qeps working in oncology can further advance their expertise with courses that are specific to the physiology of exercise as it relates to cancer and the accompanying adaptations to fitness testing and training. Table i presents North American qep designations, training, and cancer-specific exercise credentials.
TABLE I.
Qualified exercise professionals (QEPs) appropriate to work with people with cancer: based credentials and oncology training in North America
| Credential | Prerequisites | Continuing education | Certification recognition | Liability insurance |
|---|---|---|---|---|
| QEP exercise certificationsa | ||||
| College of Kinesiologists of Ontario | ||||
| Registered Kinesiologist | ■ Qualifying theory exam | NAb | Ontario | Required |
| Canadian Society for Exercise Physiology | ||||
| Certified Exercise Physiologist | ■ Minimum of 100 hours of practical experience | Required | Canada | Required |
| ■ Qualifying theory exam | ||||
| ■ Qualifying practical exam | ||||
| American College of Sports Medicine | ||||
| Certified Clinical Exercise Physiologist | ■ Qualifying theory exam | Required | United States | Recommended |
| Registered Clinical Exercise Physiologist | ■ Post graduate degree in exercise science or related field | Required | United States | Recommended |
| ■ Qualifying theory exam | ||||
| Exercise Physiologist | ■ Qualifying theory exam | NA | United States | Recommended |
| American Council on Exercise | ||||
| Medical Exercise Specialist | ■ Minimum of 500 hours of practical experience | Required | United States | Recommended |
| ■ Qualifying theory exam | ||||
| Cancer-specific training and certificationc | ||||
| American College of Sports Medicine | ||||
| Cancer Exercise Trainer | ■ 500 Hours of experience training older adults or individuals with chronic condition | NA | United States | NA |
| ■ American College of Sports Medicine– or National Commission for Certifying Agencies–accredited health and fitness certification | ||||
| ■ Qualifying practical exam | ||||
| Wellspring Cancer Support Network | ||||
| CancerSmart Rehab Techniques | ■ Rehabilitation professional in the field of physiotherapy, kinesiology, exercise physiology, and occupational therapy | NA | Canada | NA |
| University of Northern Colorado | ||||
| Cancer Rehabilitation Institute | ||||
| Clinical Cancer Exercise Specialist | ■ Exercise physiologists, physical therapists, nurses, nurse practitioners, rehabilitation specialists, personal trainers, and other medical professionals | NA | United States | NA |
| Thrive Health Services | ■ QEP | Required | Canada | NA |
| American Council on Exercise | ||||
| Cancer Exercise Specialist | ■ National Commission for Certifying Agencies–accredited health and fitness certification | Required | United States | NA |
| ■ Completion of online module | ||||
| ■ Qualifying theory exam |
Certification describes the ability to screen and assess human movement and performance in individuals with or without chronic disease and to provide management or rehabilitation needs (or both) for physical conditioning or function. A bachelor’s degree in exercise physiology or a related field is the minimum requirement.
Requires annual professional self-assessment that can include continuing eduction in addition to other professional development activity.
Certification provides training in cancer-specific needs and considerations for screening, assessment, rehabilitation, and exercise conditioning for exercise physiologists, rehabilitation professionals, and health care providers.
Given the variability in program accessibility by region and community, the subsections that follow are divided into potential pathway options. For hcps and patients who have local access to directed programming for cancer exercise and rehabilitation, access to such resources can be achieved through the Exercise Programming option. In circumstances in which cancer-exercise programming is not accessible, patients could be directed to pa tools within the Physical Activity Promotion option. The two options are not mutually exclusive, but rather complementary; they can be implemented and adapted to the health care setting and patient preferences and circumstances.
Exercise Programming Option
Referral for Exercise:
In communities and centres in which cancer-exercise programming is available, referral or physician clearance is commonly required. The initiation of exercise can be expedited by the provision of medical clearance from the hcp at the time of referral; otherwise, patients would have to obtain clearance at a later time from their referring or family physician to proceed with exercise. Referrals to exercise programming should occur early in the cancer continuum (or at the earliest opportunity) to maximize the benefits of the exercise and to minimize the deleterious effects of cancer treatment. Examples of referrals can be found in the work by Kirkham et al.18 and Alberta Cancer Exercise (Table ii). Alternatively, cancer-exercise programs might have internal mechanisms for obtaining clearance (such as medical directors within the program to advise on exercise clearance and contraindications), and in some settings, patients might self-refer (that is, contact the program from a poster or brochure). Regardless of the method of program entry, cancer-exercise guidelines indicate that patients should be screened or assessed (or both) for exercise safety by a qep before initiating a structured exercise program5,8.
TABLE II.
Alberta Cancer Exercise physical activity screening form
| Patient label: | Tumour information: | ||
| Primary tumour type: | |||
| Metastasis: (identify location and organ) | |||
| Stage: □ 1 □ 2 □ 3 □ 4 | |||
| Treatment: (see “Additional comments” for more comment space if needed) | |||
|
Chemotherapy Type: Dates: Comments: |
Radiation Dates: Comments: |
Surgery (include side of body if applicable) Type: Date: |
Herceptin Dates: Hormone therapy Dates: |
| Current side effects (see “Additional comments” for more comment space if needed) | |||
| □ Cardiotoxicity | □ Neutropenia | □ Decreased range of motion | |
| □ Pulmonary function | □ Anemia | □ Bone or joint issues | |
| □ Fatigue | □ Thrombocytopenia | □ Lymphedema | |
| □ Bowel/bladder changes | □ Peripheral neuropathy | □ Skin changes | |
| Other: | |||
| Past medical history affecting exercise participation (see “Additional comments” for more comment space if needed) | |||
| □ Currently being treated for (besides cancer) | □ Medications | ||
| □ MSK injury | □ Surgery | ||
| Comorbidities (check all that apply) (see “Additional comments” for more comment space if needed) | |||
| Cardiac | Metabolic | Pulmonary | |
| □ Hypertension/hypotension | □ Diabetes | □ COPD | |
| □ Cardiovascular disease | □ Type 1 | □ Asthma | |
| □ Myocardial | □ Type 2 | □ Pulmonary hypertension | |
| □ Valve | □ Pulmonary embolism | ||
| □ Coronary artery disease | |||
| □ Arrhythmias | Musculoskeletal | Mental health | |
| □ Peripheral artery disease | □ Neuropathy (extremeties) | □ Anxiety/depression | |
| □ Previous stroke | □ Arthritis | □ Memory disorders | |
| □ DVT | □ Osteo | □ Cognitive disorder | |
| □ Pre-syncope/syncope | □ Rheumatoid | ||
| □ Fatigue | □ Osteopenia | Renal | |
| □ Osteoporosis | □ Renal disease | ||
| Comments (see “Additional comments” for more comment space if needed) | |||
| Physical activity clearance | |||
| □ No physical activity at this time | |||
| □ Under supervision of qualified exercise professional | □ With avoidance of | ||
| □ Unrestricted or progressive physical activity | |||
| Physician signature: | Stamp: | Date: | |
| Additional comments: | |||
Medical Screening and Risk Stratification for Exercise:
Connecting people with cancer to appropriate exercise programming requires the identification of precautions and contraindications so that programming is ensured to be safe. Brown and colleagues21 conducted a survey of medical, rehabilitation, cancer survivorship, and exercise professionals about health factors that could augment the risk of exercise participation after a cancer diagnosis. That survey resulted in the development of a 42-item risk screening checklist that allows for the addition of “other” health factors that could influence exercise safety21. Participants who answer yes to any of the items are required to seek medical clearance before initiating unsupervised moderate-to-vigorous exercise.
Other risk stratification tools can further delineate highand low-risk categories22,23. For example, Burr et al.22 and the U.S. National Comprehensive Cancer Network23 provide additional strata based on medical complexity and potential risk of adverse events associated with exercise. In the National Comprehensive Cancer Network risk stratification model, medical clearance is recommended for some moderate-risk patients and for all high-risk patients. Both tools facilitate an understanding of the risk associated with exercise and relevant adaptations to an exercise prescription; however, their use and interpretation come at the discretion of the clinicians and programs implementing them and might be superseded by clinical judgment with consideration for patient preferences and other contextual factors.
It is important to emphasize that patients who are identified to be at high risk or who fail the initial screening are not necessarily ineligible for exercise; rather, they require some combination of appropriate cautions, supervision, or additional clearance before initiating exercise. Although it is recommended that qeps conduct their own screening before providing an exercise program to a person with cancer, medical screening and risk stratification completed by the hcp supports a thorough examination of the medical history, contributes unique perspectives about the requirements for exercise prescription adaptation, and facilitates expedient participation in the exercise program with medical clearance. In some centres, program-specific screening and assessment models conducted by an oncology-trained qep or other hcp can be appropriate for admitting or referring patients to an exercise program, provided that the exercise is low-intensity (yoga, tai chi) or the program is overseen by a physician, or both.
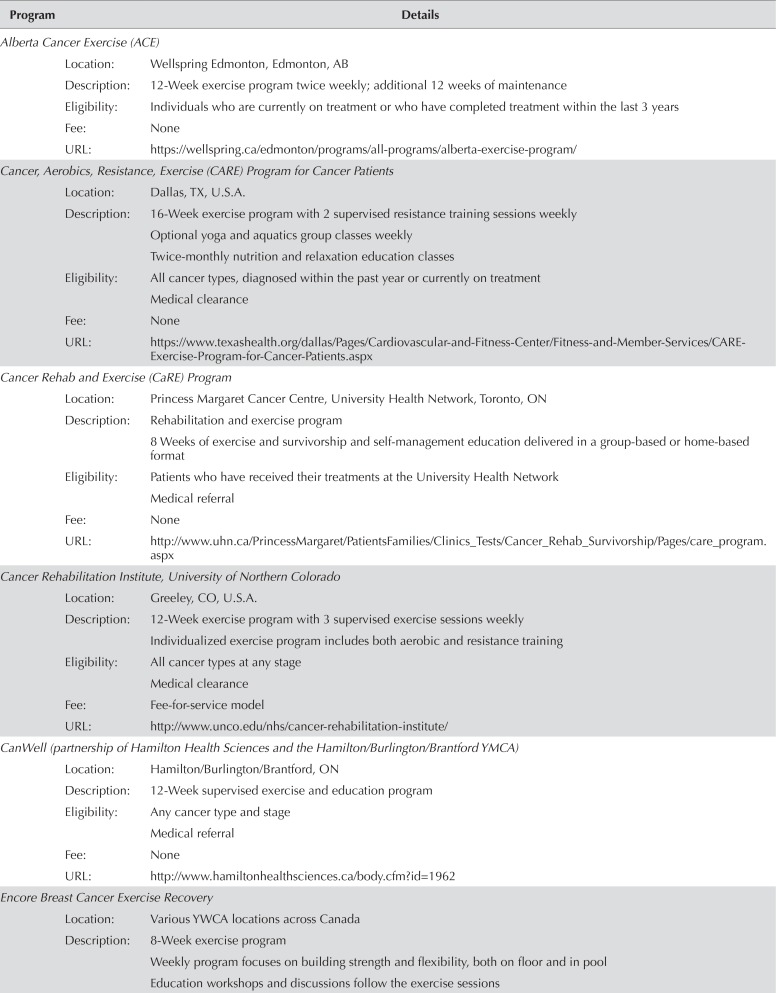
Rehabilitation and Exercise Programs:
Depending on the medical needs of the patient, directed exercise programming can be delivered in rehabilitation, cancer-exercise, or general-population exercise programs. For the low-risk patient, or for those who have received medical clearance to exercise, referral to an appropriate or qep-supervised general exercise program in community or public fitness facilities, or to a tailored home-based program, is recommended so that exercise can be performed on an ongoing basis with minimal barriers. Alternatively, some patients might benefit from exercise programming that is specific to those with a history of cancer, enhancing comfort, safety, and social support. Cancer-exercise programs can be delivered in a group, one-on-one, or in a home-based format and can encompass the variety of program models found in the community; however, such programs are specific to participants with a history of cancer and are delivered by qeps with oncology training and experience (see Table iii for examples of cancer-exercise programs in North America). Finally, some patients might require medical or inpatient- or outpatient-specific rehabilitation programs before or concurrent with general exercise. Because of the fluctuations in health that can occur throughout the cancer continuum, transitioning between public exercise programs, cancer-exercise programs, and specialized rehabilitation or medical care might be necessary. For example, a breast cancer patient might receive specific rehabilitation for range of motion in the shoulder while also participating in an exercise program designed to improve general fitness and functional capacity. After participation in the cancer-exercise program, the same patient could be encouraged to participate in a community-based exercise program at a local fitness facility that is more proximal to her home and that can support her ongoing exercise-related needs. Changes in medical status or physical capacity might necessitate returning to more directed cancer-exercise programming or to medical or rehabilitation services.
TABLE III.
Cancer and exercise programs in Canada and the United States.
| Program | Details | |
|---|---|---|
| Alberta Cancer Exercise (ACE) | ||
| Location: | Wellspring Edmonton, Edmonton, AB | |
| Description: | 12-Week exercise program twice weekly; additional 12 weeks of maintenance | |
| Eligibility: | Individuals who are currently on treatment or who have completed treatment within the last 3 years | |
| Fee: | None | |
| URL: | https://wellspring.ca/edmonton/programs/all-programs/alberta-exercise-program/ | |
| Cancer, Aerobics, Resistance, Exercise (CARE) Program for Cancer Patients | ||
| Location: | Dallas, TX, U.S.A. | |
| Description: | 16-Week exercise program with 2 supervised resistance training sessions weekly | |
| Optional yoga and aquatics group classes weekly | ||
| Twice-monthly nutrition and relaxation education classes | ||
| Eligibility: | All cancer types, diagnosed within the past year or currently on treatment | |
| Medical clearance | ||
| Fee: | None | |
| URL: | https://www.texashealth.org/dallas/Pages/Cardiovascular-and-Fitness-Center/Fitness-and-Member-Services/CARE-Exercise-Program-for-Cancer-Patients.aspx | |
| Cancer Rehab and Exercise (CaRE) Program | ||
| Location: | Princess Margaret Cancer Centre, University Health Network, Toronto, ON | |
| Description: | Rehabilitation and exercise program | |
| 8 Weeks of exercise and survivorship and self-management education delivered in a group-based or home-based format | ||
| Eligibility: | Patients who have received their treatments at the University Health Network | |
| Medical referral | ||
| Fee: | None | |
| URL: | http://www.uhn.ca/PrincessMargaret/PatientsFamilies/Clinics_Tests/Cancer_Rehab_Survivorship/Pages/care_program.aspx | |
| Cancer Rehabilitation Institute, University of Northern Colorado | ||
| Location: | Greeley, CO, U.S.A. | |
| Description: | 12-Week exercise program with 3 supervised exercise sessions weekly | |
| Individualized exercise program includes both aerobic and resistance training | ||
| Eligibility: | All cancer types at any stage | |
| Medical clearance | ||
| Fee: | Fee-for-service model | |
| URL: | http://www.unco.edu/nhs/cancer-rehabilitation-institute/ | |
| CanWell (partnership of Hamilton Health Sciences and the Hamilton/Burlington/Brantford YMCA) | ||
| Location: | Hamilton/Burlington/Brantford, ON | |
| Description: | 12-Week supervised exercise and education program | |
| Eligibility: | Any cancer type and stage | |
| Medical referral | ||
| Fee: | None | |
| URL: | http://www.hamiltonhealthsciences.ca/body.cfm?id=1962 | |
| Encore Breast Cancer Exercise Recovery | ||
| Location: | Various YWCA locations across Canada | |
| Description: | 8-Week exercise program | |
| Weekly program focuses on building strength and flexibility, both on floor and in pool | ||
| Education workshops and discussions follow the exercise sessions | ||
| Encore Breast Cancer Exercise Recovery continued | ||
| Eligibility: | Women with breast cancer at any stage of their lives | |
| Medical clearance | ||
| Fee: | None | |
| URL: | Multiple Web sites; contact the local YMCA for details | |
| FitSTEPS for Life | ||
| Location: | Cancer Foundation for Life, Tyler, TX, U.S.A. | |
| Description: | Evidence-based cancer rehabilitation for achieving and maintaining functional mobility and endurance | |
| Individualized exercise program, available as supervised or home-based | ||
| Eligibility: | All cancer types (diagnosis to posttreatment) | |
| Medical referral | ||
| Fee: | None | |
| URL: | http://www.cancerfoundationforlife.org/fitstepsforlife/ | |
| Health, Exercise, Active Living and Therapeutic Lifestyle (HEALTh) program | ||
| Location: | Toronto Rehabilitation Institute, University Health Network, Toronto, ON | |
| Description: | 6-Month program providing education, exercise, and peer support | |
| Eligibility: | Breast cancer | |
| Medical referral | ||
| Relevant clinical notes and recent blood work from referring doctor | ||
| Fee: | None | |
| URL: | http://www.uhn.ca/TorontoRehab/PatientsFamilies/Clinics_Tests/HEALTh | |
| LIVESTRONG at the YMCA | ||
| Location: | Various (an initiative of the LIVESTRONG Foundation, Austin, TX, U.S.A., in partnership with the YMCA) | |
| Description: | 12-Week physical activity program | |
| Eligibility: | All cancer types (after diagnosis) | |
| Medical clearance | ||
| Fee: | None or varies with location | |
| URL: | https://www.livestrong.org/what-we-do/program/livestrong-at-the-ymca | |
| MacWarriors Cancer Rehabilitation Service | ||
| Location: | McMaster University, Physical Activity Centre of Excellence, Hamilton, ON | |
| Description: | Physiotherapy and supervised exercise sessions | |
| Exercise prescription and individual treatment sessions, manual therapy, and exercise consultations | ||
| Eligibility: | Medical clearance | |
| Fee: | Fee-for-service model | |
| URL: | https://pace.mcmaster.ca/programs/mac-warriors-cancer-rehabilitation | |
| PEER: Pediatric Cancer Survivors Engaging in Exercise for Recovery | ||
| Location: | University of Calgary, Calgary, AB | |
| Description: | Individualized exercise programming tailored to the health status and fitness level of participants | |
| Eligibility: | Children and youth 4–18 years | |
| Fee: | None | |
| URL: | http://www.ucalgary.ca/healthandwellnesslab/programs/peer | |
| RENEW: Life After Cancer Treatment | ||
| Location: | Windsor Regional Hospital and Windsor Squash and Fitness, Windsor, ON | |
| Description: | Two-part program that includes | |
| ■ a 5-part education series, weekly. | ||
| ■ a supervised exercise program twice weekly for 8–10 weeks. | ||
| Eligibility: | Survivors who have completed active treatment | |
| Medical clearance | ||
| Fee: | Education sessions: none | |
| Exercise sessions: fee-for-service | ||
| URL: | http://www.wrh.on.ca/Site_Published/wrh_internet/RichText.aspx?Body.QueryId.Id=88604&LeftNav.QueryId.Categories=837#RENEWProg | |
| Strength and Stretch | ||
| Location: | Prostate Cancer Centre, Calgary, AB | |
| Description: | Weekly program designed for prostate cancer patients | |
| Eligibility: | Men with prostate cancer | |
| Fee: | Unclear | |
| URL: | http://www.prostatecancercentre.ca/our-programs/patient-services/#strength-and-stretch | |
| Thrive Program | ||
| Location: | University of Calgary, Health and Wellness Lab, Calgary, AB | |
| Description: | Fitness assessment and exercise prescription | |
| Follow-up appointments | ||
| Facilities made available for participants and their support persons | ||
| Eligibility: | Any cancer type and stage | |
| Fee: | Fee-for-service model | |
| URL: | https://www.ucalgary.ca/healthandwellnesslab/programs/thrive-program | |
| UCSF Cancer Exercise Counseling | ||
| Location: | University of California San Francisco, San Francisco, CA, U.S.A. | |
| Description: | One-on-one exercise counselling: tips and strategies for success and follow-up telephone calls | |
| Individualized, hour-long classes | ||
| Patients receive a written set of exercise recommendations and referral to group yoga and exercise classes | ||
| Eligibility: | Patients who are undergoing or who have completed treatment | |
| Screening appointment | ||
| Fee: | None | |
| URL: | https://www.ucsfhealth.org/services/cancer_exercise_counseling/index.html | |
| UW WELL-FIT | ||
| Location: | University of Waterloo, Kitchener–Waterloo, ON | |
| Description: | 12-Week supervised group-based exercise | |
| 1-Hour sessions, twice weekly | ||
| Eligibility: | Currently undergoing chemotherapy or radiation; starting hormonal therapy; or recently completed surgery as the only form of treatment | |
| Medical referral | ||
| Fee: | None | |
| URL: | https://uwaterloo.ca/uw-fitness/uw-well-fit | |
| Wellspring Cancer Exercise | ||
| Location: | Various, in AB and ON | |
| Description: | 20-Week supervised exercise program | |
| 1-Hour session, twice weekly | ||
| Eligibility: | Any cancer type and stage | |
| Medical referral | ||
| Fee: | None | |
| URL: | http://www.wellspring.ca (choose location and search programs) | |
| Winship at the Y | ||
| Location: | Emory University, Winship Cancer Institute, and various YMCA locations in Metro Atlanta, Atlanta, GA, U.S.A. | |
| Description: | One-on-one meetings with wellness coach once per month for 6 months | |
| Eligibility: | Survivors who have completed active treatment | |
| Medical clearance | ||
| Fee: | YMCA membership | |
| URL: | https://winshipcancer.emory.edu/patient-care/living-with-cancer/wellness-program.html | |
Description of the programs does not constitute endorsement by the authors. Programs are presented as examples of existing resources (accessed and verified on 15 March 2018).
Although most cancer-exercise programming is designed to be centre-based, it is worth noting that home-based programming can effectively expand the accessibility of facility-based programs while lessening common barriers to attendance such as travel distance, transportation cost, and time. Those features of the “home” or independent setting make it a preferable context for many people with cancer24–27. To ensure safety and to facilitate benefit in program models involving independent or home-based exercise (or both), these components are recommended:
■ Exercise screening and risk stratification (with medical clearance as necessary)
■ Appropriate instruction in exercise by a qep
■ Provision of resources to support exercise engagement (for example, manuals, log books; Web sites or apps; and basic exercise equipment such as resistance bands, stability ball)
■ Routine follow-ups with the qep, scheduled to ensure appropriate adjustment of the exercise prescription to accommodate changes in capacity, goals, or health status
Notably, the operationalization of “home-based” remains relatively ambiguous, because environmental factors vary considerably between homes, affecting amenability to exercise. Home-based exercise might therefore more aptly be called independent or un supervised exercise to encompass the various settings in which an individual with cancer could exercise away from the facility in which exercise is prescribed28. And despite patient preference and the convenience of home-based exercise programming, a recent comparison of home and facility-based exercise interventions in a systematic review and meta-analysis found greater benefits in physical functioning for facility-based programs29. Recent research has also found that, compared with exercising independently at-home, exercising in facility-based programs, especially those delivered in a group format, might expose participants to social factors that enhance the exercise experience and improve long-term adherence30.
Ultimately, exercise and pa programming must align with the context, preferences, and opportunities of the patient. Appropriate inquiry into medical, social, economic, and geographic factors will support program participation and success. Independent, unsupervised exercise programming provides a partial solution that reduces the need for infrastructure and personnel, but that might require some qep guidance and support throughout the experience to optimize patient engagement and benefits.
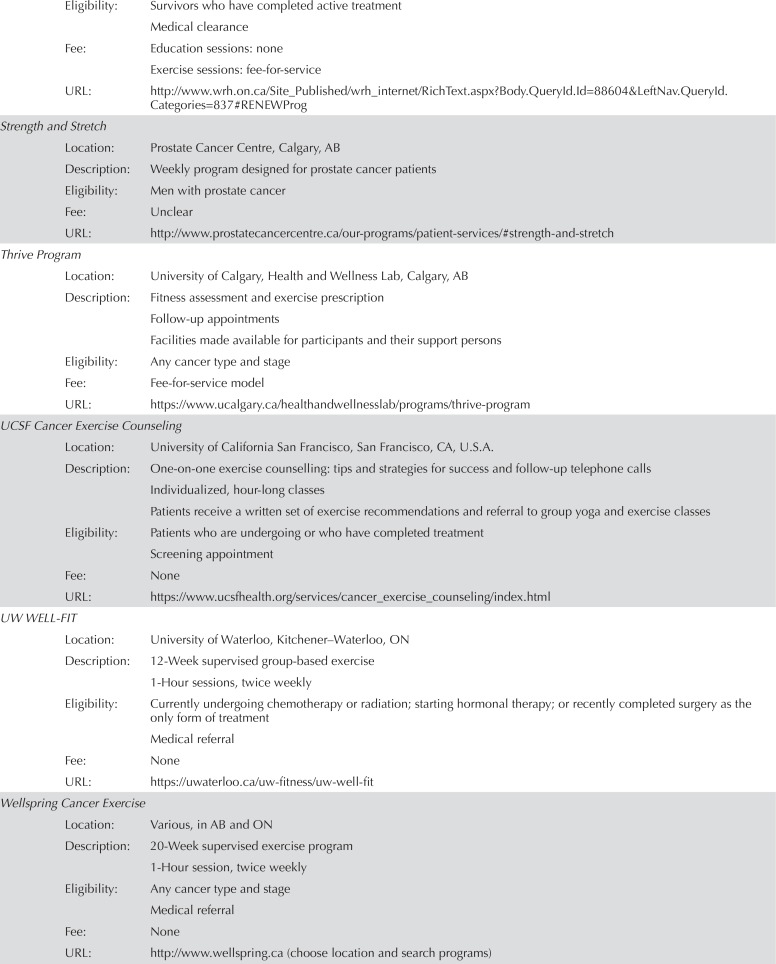
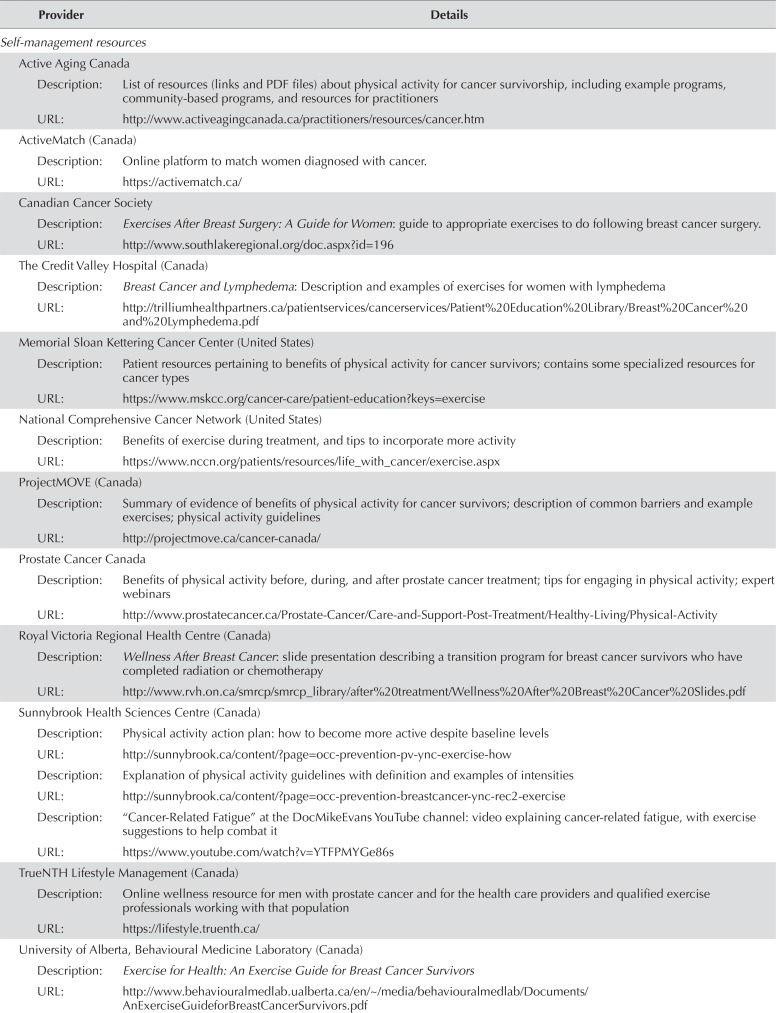
PA Promotion Option
PA Self-Management:
Structured exercise-related services delivered by appropriately trained qeps remain relatively scarce and are typically found in urban areas, proximal to major hospitals and universities. Given the broad catchment area of cancer centres, many patients travel significant distances for cancer care and are not reasonably able to participate in ongoing exercise programs based within such large, urban institutions. Strategies to improve accessibility to cancer-exercise services in regions that lack such services is a high priority. Without access to a cancer-specific exercise program or to an oncology-trained qep, a focus must be placed on providing self-management resources for cancer survivors that promote regular pa throughout the cancer care continuum.
If an individually prescribed, yet independent and unsupervised, option is not available, the most common approach for engaging patients to participate in regular pa is education. Education about the principles of pa, behaviour change techniques, and adherence strategies are the cornerstones of most resources to increase pa in people with cancer. Educational resources can range in scope, delivery method, and cost. Brochures and informational posters are likely the most simple and inexpensive approach to conveying basic information about pa for people with cancer, and they can be delivered broadly during patient visits with hcps. They are limited in that they cannot provide individualized information or feedback, and they remain static for the user—that is, they cannot be updated once received. They are thus inadequate for the delivery of detailed and tailored exercise recommendations. Nevertheless, they provide an entry-level opportunity to improve awareness of the benefits of pa after a cancer diagnosis, and they contribute to a culture shift in the direction of lifestyle medicine for improved patient outcomes within the clinical environment. Table iv provides North American examples of education and self-management resources relative to exercise and pa in cancer.
TABLE IV.
| Provider | Details |
|---|---|
| Self-management resources | |
| Active Aging Canada | |
| Description: | List of resources (links and PDF files) about physical activity for cancer survivorship, including example programs, |
| community-based programs, and resources for practitioners | |
| URL: | http://www.activeagingcanada.ca/practitioners/resources/cancer.htm |
| ActiveMatch (Canada) | |
| Description: | Online platform to match women diagnosed with cancer. |
| URL: | https://activematch.ca/ |
| Canadian Cancer Society | |
| Description: | Exercises After Breast Surgery: A Guide for Women: guide to appropriate exercises to do following breast cancer surgery. |
| URL: | http://www.southlakeregional.org/doc.aspx?id=196 |
| The Credit Valley Hospital (Canada) | |
| Description: | Breast Cancer and Lymphedema: Description and examples of exercises for women with lymphedema |
| URL: | http://trilliumhealthpartners.ca/patientservices/cancerservices/Patient%20Education%20Library/Breast%20Cancer%20and%20Lymphedema.pdf |
| Memorial Sloan Kettering Cancer Center (United States) | |
| Description: | Patient resources pertaining to benefits of physical activity for cancer survivors; contains some specialized resources for cancer types |
| URL: | https://www.mskcc.org/cancer-care/patient-education?keys=exercise |
| National Comprehensive Cancer Network (United States) | |
| Description: | Benefits of exercise during treatment, and tips to incorporate more activity |
| URL: | https://www.nccn.org/patients/resources/life_with_cancer/exercise.aspx |
| ProjectMOVE (Canada) | |
| Description: | Summary of evidence of benefits of physical activity for cancer survivors; description of common barriers and example exercises; physical activity guidelines |
| URL: | http://projectmove.ca/cancer-canada/ |
| Prostate Cancer Canada | |
| Description: | Benefits of physical activity before, during, and after prostate cancer treatment; tips for engaging in physical activity; expert webinars |
| URL: | http://www.prostatecancer.ca/Prostate-Cancer/Care-and-Support-Post-Treatment/Healthy-Living/Physical-Activity |
| Royal Victoria Regional Health Centre (Canada) | |
| Description: | Wellness After Breast Cancer: slide presentation describing a transition program for breast cancer survivors who have completed radiation or chemotherapy |
| URL: | http://www.rvh.on.ca/smrcp/smrcp_library/after%20treatment/Wellness%20After%20Breast%20Cancer%20Slides.pdf |
| Sunnybrook Health Sciences Centre (Canada) | |
| Description: | Physical activity action plan: how to become more active despite baseline levels |
| URL: | http://sunnybrook.ca/content/?page=occ-prevention-pv-ync-exercise-how |
| Description: | Explanation of physical activity guidelines with definition and examples of intensities |
| URL: | http://sunnybrook.ca/content/?page=occ-prevention-breastcancer-ync-rec2-exercise |
| Description: | Cancer-Related Fatigue” at the DocMikeEvans YouTube channel: video explaining cancer-related fatigue, with exercise suggestions to help combat it |
| URL: | https://www.youtube.com/watch?v=YTFPMYGe86s |
| TrueNTH Lifestyle Management (Canada) | |
| Description: | Online wellness resource for men with prostate cancer and for the health care providers and qualified exercise professionals working with that population |
| URL: | https://lifestyle.truenth.ca/ |
| University of Alberta, Behavioural Medicine Laboratory (Canada) | |
| Description: | Exercise for Health: An Exercise Guide for Breast Cancer Survivors |
| URL: | http://www.behaviouralmedlab.ualberta.ca/en/~/media/behaviouralmedlab/Documents/AnExerciseGuideforBreastCancerSurvivors.pdf |
| University Health Network (Canada) | |
| Description: | Functional Rehab After Breast Cancer Surgery: Exercises to use after surgery (lumpectomy, mastectomy, sentinel node biopsy, or axillary node dissection) |
| URL: | http://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Documents/Your_Functional_Rehabilitation_After_Breast_Surgery.pdf |
| Description: | Prevent and Reduce Stiffness Caused by Radiation Treatment: Discussion of the importance of exercises after treatment for head-and-neck cancers; how often and when to exercise; and safety considerations |
| URL: | http://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Documents/Prevent_and_reduce_stiffness_caused_by_radiation_treatment.pdf#search=exercise |
| Verywell (United States) | |
| Description: | Benefits of physical activity for lung cancer prevention and for survivorship; tips on how to become more active after a diagnosis |
| URL: | https://www.verywell.com/exercise-and-lung-cancer-2249235 |
| Winnipeg Regional Health Authority, Breast Health Centre (Canada) | |
| Description: | Exercises to Improve Mobility of the Arm and Shoulder After Breast Cancer Surgery |
| URL: | http://www.cancercare.mb.ca/resource/File/Breast_Cancer/Exercises_to_Improve_mobility_after_Surgery_bilingual_07.pdf |
| Education resources | |
| American Cancer Society (United States) | |
| Description: | Benefits of physical activity for cancer survivors, and the consequences of not engaging in physical activity |
| URL: | https://www.cancer.org/content/dam/cancer-org/cancer-control/en/booklets-flyers/physical-activity-and-cancer-fact-sheet.pdf |
| BreastCancer.org (United States) | |
| Description: | Summary of research evidence about physical activity for breast cancer patients from experts |
| URL: | http://www.breastcancer.org/tips/ask_expert/2006_01 |
| Canadian Cancer Society | |
| Description: | Benefits and considerations for physical activity for survivors during and after treatment |
| URL: | During treatment: http://www.cancer.ca/en/cancer-information/cancer-journey/living-with-cancer/physical-activity-during-cancer-treatment/?region=on |
| After treatment: http://www.cancer.ca/en/cancer-information/cancer-journey/life-after-cancer/your-wellness-plan/physical-activity-after-treatment/?region=on | |
| Cancer Care Ontario (Canada) | |
| Description | Overview of the benefits of exercise |
| Includes information about types of exercise and exercise safety | |
| Tips on how to get started with exercise, with emphasis on goal-setting and tracking exercises | |
| URL: | Exercise guide: https://www.cancercareontario.ca/en/system/files_force/derivative/ExerciseGuide-EN.pdf |
| Exercise tracking sheet: https://www.cancercareontario.ca/en/system/files_force/derivative/ExerciseToolkit-EN.pdf | |
| Juravinski Cancer Centre (Canada) | |
| Description: | “Is Pushing My Luck Enough Exercise?” |
| Slide presentation for providers: benefits of physical activity for cancer survivors and how to discuss physical activity with | |
| patients | |
| URL: | http://www.jcc.hhsc.ca/workfiles/LABC/Is%20pushing%20my%20luck%20enough%20exercise%20-%20Copy%20%282%29.pdf |
| MD Anderson Cancer Center (United States) | |
| Description: | Physical activity guidelines, examples of types of exercises, and tips on how to be more active |
| URL: | https://www.mdanderson.org/prevention-screening/manage-your-risk/physical-activity.html |
| National Cancer Institute (United States) | |
| Description: | Definition and benefits of physical activity; information on sedentary behaviour; relationship between physical activity and cancer from a research perspective |
| URL: | https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/physical-activity-fact-sheet |
The table presents information from programs in Canada and the United States and might not represent an exhaustive list of all available resources in both countries (accessed and verified on 15 March 2018).
Description of the programs does not constitute endorsement by the authors. Programs are presented to the user for consideration relative to their individual needs. Self-management resources help patients to guide their own exercise and physical activity behaviours. Education is targeted to health care providers to assist them in guiding their patients in exercise and physical activity behaviours.
Digital resources can educate users and provide an interactive, self-management experience throughout survivorship care and during pa and exercise specifically. Digital resources can be delivered using dvds, a usb drive, and more frequently, online. Apps and online services can include point-and-click access to information, secondary sources, algorithmic tailoring of exercise particulars to the specific needs of the user, online education, audio and videos to demonstrate exercises, and tracking tools for pa completion and related health outcomes (for example, fatigue, quality of life). Web-based platforms are also able to connect peers, promoting social support for pa and potentially linking to other commercially available wellness platforms such as wrist-worn activity trackers. Digital resources can also connect patients to pa and exercise resources in regions with growing access to programming. Table iv lists publicly available resources containing pa information for cancer survivors.
Participation in Research
Throughout the cancer continuum, opportunities for people with cancer to receive pa and exercise programming and support can come in research avenues. Before the development of exercise programs for people with cancer, study participation was likely a primary conduit for patients to access qeps and exercise services. The advancement of the field has pushed research questions beyond efficacy and toward mechanisms of benefit and strategies to optimize uptake and to promote long-term adherence. In addition, research is examining questions of effectiveness—the translation of exercise benefits in experimental designs into real-world settings. This latter research direction has sought to reduce barriers to participation and to improve the understanding of adherence to exercise and pa in people with cancer—efforts that have led to innovations and collaborations that stretch the geographic reach of the programs and the feasibility of the research. The next step is to move this important research into practice, implementing programs beyond the traditional academic and clinical settings into community health and fitness settings to improve overall accessibility and benefit. Participation in research includes rigorous assessment of study eligibility, often including medical screening or clearance and a detailed description of the assessment and interventions. Patients who might be interested in research could be directed to common trial registries, such as http://ClinicalTrials.gov.
SUMMARY
Recommendations for pa and tailored exercise after a cancer diagnosis have further stimulated discourse about how to best facilitate and support patients in achieving the related benefits. Exercise services and supports are diverse and respond to local needs and resources. However, most cancer survivors are either not aware of or not able to access the available resources. Exercise guidelines have shed light on the question of “what to do,” but little is known about how best to do it (that is, implementation). A major challenge to guideline implementation is a lack of direction about how to connect patients with relevant services and resources. In the present paper, we have articulated a pathway that bridges patients from interactions with their hcps to exercise and pa resources for people with cancer. The pathway acknowledges both the complexity of providing exercise services to people with cancer and the inherent challenges of exercise promotion and support in the medical system. To overcome those obstacles to exercise and pa engagement, the pathway encourages interprofessional communication and collaboration for the safe and effective delivery of resources aligned with the guidelines.
The pathway reflects the experiences of clinicians and researchers who have created, advised, or supported knowledge translation in cancer and exercise toward improved access to, and availability of, related services. The pathway summarizes approaches to resource implementation or dissemination as they are used within programs across Canada and by other authorities in cancer care and exercise physiology, with the intention of initiating programmatic, organizational, community, and broader discussions about improving the well-being of people with cancer through greater engagement in exercise and pa. Thus, the pathway is intended to be flexible and dynamic, providing a starting point for organizations, programs, and individual hcps to consider as they create a systematic approach to bridging the gap between the evidence of benefit related to exercise and the cancer patient population they serve.
Future work in moving evidence into practice must include an examination of how pathway resources affect exercise participation and pa levels, and the related health outcomes of people with cancer. Assessment of pathway costs (time and personnel required, resources utilized) in the clinical setting so as to tailor the pathway to unique needs is an important next step in moving our pa and exercise evidence into clinical practice. A pathway that is feasible and economically sustainable has the potential to significantly positively affect the cancer survivor’s journey.
ACKNOWLEDGMENTS
We acknowledge Cancer Care Ontario’s Clinical Advisory Group for their implementation of the Exercise for People with Cancer guidelines. Ms. Kaitlyn Kauffeldt is acknowledged for contributions related to the development of the pathway, the manuscript, and compilation of the supporting resources.
Footnotes
Fong A, Jones JM, Faulkner G, Sabiston CM. Oncology clinician experiences with physical activity counselling in breast cancer survivors: a qualitative analysis. Submitted.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Friedenreich CM, Neilson HK, Farris MS, Courneya KS. Physical activity and cancer outcomes: a precision medicine approach. Clin Cancer Res. 2016;122:4766–75. doi: 10.1158/1078-0432.CCR-16-0067. [DOI] [PubMed] [Google Scholar]
- 2.Cormie P, Zopf EM, Zhang X, Schmitz KH. The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects. Epidemiol Rev. 2017;39:1–22. doi: 10.1093/epirev/mxx007. [DOI] [PubMed] [Google Scholar]
- 3.Kimmel GT, Haas BK, Hermanns M. The role of exercise in cancer treatment: bridging the gap. Curr Sports Med Rep. 2014;13:246–52. doi: 10.1249/JSR.0000000000000068. [DOI] [PubMed] [Google Scholar]
- 4.Santa Mina D, Alibhai SM, Matthew AG, et al. Exercise in the clinical care for cancer: a call to action and program development description. Curr Oncol. 2012;19:e136–44. doi: 10.3747/co.19.912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmitz KH, Courneya KS, Matthews C, et al. on behalf of the American College of Sports Medicine American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42:1409–26. doi: 10.1249/MSS.0b013e3181e0c112. [Erratum in: Med Sci Sports Exerc 2011;43:195] [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO). Global Recommendations on Physical Activity for Health. Geneva, Switzerland: WHO; 2010. [PubMed] [Google Scholar]
- 7.Casperson CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–31. [PMC free article] [PubMed] [Google Scholar]
- 8.Segal R, Zwaal C, Green E, et al. on behalf of the Exercise for People with Cancer Guideline Development Group Exercise for people with cancer: a clinical practice guideline. Curr Oncol. 2017;24:40–6. doi: 10.3747/co.24.3376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nyrop KA, Deal AM, Williams GR, Guerard EJ, Pergolotti M, Muss HB. Physical activity communication between oncology providers and patients with early-stage breast, colon, or prostate cancer. Cancer. 2016;122:470–6. doi: 10.1002/cncr.29786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nadler M, Bainbridge D, Tomasone J, Cheifetz O, Juergens RA, Sussman J. Oncology care provider perspectives on exercise promotion in people with cancer: an examination of knowledge, practices, barriers, and facilitators. Support Care Cancer. 2017;25:2297–304. doi: 10.1007/s00520-017-3640-9. [DOI] [PubMed] [Google Scholar]
- 11.Karvinen KH, DuBose KD, Carney B, Allison RR. Promotion of physical activity among oncologists in the United States. J Support Oncol. 2010;8:35–41. [PubMed] [Google Scholar]
- 12.Karvinen KH, McGourty S, Parent T, Walker PR. Physical activity promotion among oncology nurses. Cancer Nurs. 2012;35:E41–8. doi: 10.1097/NCC.0b013e31822d9081. [DOI] [PubMed] [Google Scholar]
- 13.Jones LW, Courneya KS, Peddle C, Mackey JR. Oncologists’ opinions towards recommending exercise to patients with cancer: a Canadian national survey. Support Care Cancer. 2005;13:929–37. doi: 10.1007/s00520-005-0805-8. [DOI] [PubMed] [Google Scholar]
- 14.Fisher A, Williams K, Beeken R, Wardle J. Recall of physical activity advice was associated with higher levels of physical activity in colorectal cancer patients. BMJ Open. 2015;5:e006853. doi: 10.1136/bmjopen-2014-006853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tarasenko YN, Miller EA, Chen C, Schoenberg NE. Physical activity levels and counseling by health care providers in cancer survivors. Prev Med. 2017;99:211–17. doi: 10.1016/j.ypmed.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 16.Winters-Stone KM, Moe EL, Perry CK, et al. Enhancing an oncologist’s recommendation to exercise to manage fatigue levels in breast cancer patients: a randomized controlled trial. Support Care Cancer. 2017;26:905–12. doi: 10.1007/s00520-017-3909-z. [DOI] [PubMed] [Google Scholar]
- 17.Park JH, Lee J, Oh M, et al. The effect of oncologists’ exercise recommendations on the level of exercise and quality of life in survivors of breast and colorectal cancer: a randomized controlled trial. Cancer. 2015;121:2740–8. doi: 10.1002/cncr.29400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirkham AA, Van Patten CL, Gelmon KA, et al. Effectiveness of oncologist referred exercise and healthy eating programming as a part of supportive adjuvant care for early breast cancer. Oncologist. 2018;23:105–15. doi: 10.1634/theoncologist.2017-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.K. National Institute for Health and Care Excellence (nice). Physical Activity: Exercise Referral Schemes. London, UK: NICE; 2014. [Google Scholar]
- 20.O’Brien MW, Shields CA, Oh PI, Fowles JR. Health care provider confidence and exercise prescription practices of Exercise Is Medicine Canada workshop attendees. Appl Physiol Nutr Metab. 2017;42:384–90. doi: 10.1139/apnm-2016-0413. [DOI] [PubMed] [Google Scholar]
- 21.Brown JC, Ko EM, Schmitz KH. Development of a risk-screening tool for cancer survivors to participate in unsupervised moderate-to vigorous-intensity exercise: results from a survey study. PM R. 2015;7:113–22. doi: 10.1016/j.pmrj.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burr JF, Jones L, Shephard RJ. Physical activity for cancer patients. Can Fam Physician. 2012;58:970–3. [PMC free article] [PubMed] [Google Scholar]
- 23.Denlinger CS, Sanft T, Baker KS, et al. Survivorship, version 2.2017, nccn clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15:1140–63. doi: 10.6004/jnccn.2017.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karvinen KH, Courneya KS, Campbell KL, et al. Exercise preferences of endometrial cancer survivors: a population-based study. Cancer Nurs. 2006;29:259–65. doi: 10.1097/00002820-200607000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Karvinen KH, Courneya KS, Venner P, North S. Exercise programming and counseling preferences in bladder cancer survivors: a population-based study. J Cancer Surviv. 2007;1:27–34. doi: 10.1007/s11764-007-0010-5. [DOI] [PubMed] [Google Scholar]
- 26.Rogers LQ, Markwell SJ, Verhulst S, McAuley E, Courneya KS. Rural breast cancer survivors: exercise preferences and their determinants. Psychooncology. 2009;18:412–21. doi: 10.1002/pon.1497. [DOI] [PubMed] [Google Scholar]
- 27.Jones LW, Guill B, Keir ST, et al. Exercise interest and preferences among patients diagnosed with primary brain cancer. Support Care Cancer. 2007;15:47–55. doi: 10.1007/s00520-006-0096-8. [DOI] [PubMed] [Google Scholar]
- 28.Lopez C, Jones J, Alibhai SMH, Santa Mina D. What is the “home” in home-based exercise? The need to define independent exercise for survivors of cancer. J Clin Oncol. 2018;36:926–7. doi: 10.1200/JCO.2017.76.4365. [DOI] [PubMed] [Google Scholar]
- 29.Swartz MC, Lewis ZH, Lyons EJ, et al. Effect of home- and community-based physical activity interventions on physical function among cancer survivors: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2017;98:1652–65. doi: 10.1016/j.apmr.2017.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jackson C, Dowd AJ, Capozzi LC, Bridel W, Lau HY, Culos-Reed SN. Eur J Cancer Care (Engl) 2018. A turning point: head and neck cancer patients’ exercise preferences and barriers before and after participation in an exercise intervention. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]