Highlights
-
•
Hepatic splenosis is a rare clinical occurrence.
-
•
Hepatic splenosis mimics neoplasia.
-
•
Focal hepatic lesions must be differentially diagnosed in patients whose spleens have been removed.
-
•
The diagnosis cannot be made until after surgical resection.
Keywords: Splenosis, Neoplasia, Liver, Splenectomy
Abstract
Introduction
Splenosis is defined as the heterotopic autoimplantation of splenic tissue following trauma to or surgery on the spleen.
Clinical case
We present a case of an asymptomatic 73-year-old male in whom hypervascular lesions were detected during routine exams. The patient reported a history of carotid artery surgery and cholecystectomy; he had a laparotomy incision from childhood but was unaware of the reason for it. The patient exhibited slightly elevated carcinoembryonic antigen (CEA) levels. Histopathology revealed intrahepatic heterotopic splenic parenchyma, with no evidence of neoplasia in either of the two lesions, the diameters of which were 1.5 cm and 3.6 cm. Patient received outpatient follow-up care for 24 months and experienced no complications.
Discussion
Our clinical, laboratory, and imaging exams failed to reveal the etiology of the lesion. Because the masses were hypervascular lesions, a percutaneous liver biopsy was not feasible.
Conclusion
Through this report, we emphasize the importance of considering intrahepatic splenosis as a remote possibility in patients with hepatic nodules who have a history of splenectomy.
1. Introduction
The term “splenosis” was first used by Buchbinder and Lopkoff in 1939, when they described a case of autoimplantation of splenic tissue in a woman with a suspected case of endometriosis [1]. Splenosis has been reported in 26% to 67% of patients with a history of splenic trauma or splenectomy [2]. It can also occur in the pleural cavity, pericardium, lung, subcutaneous tissue, and the brain, as well as on the abdominal wall. In the abdomen, it usually manifests as an asymptomatic mass discovered by chance [3].
Most of the reported cases occurred as a result of trauma or iatrogenesis involving the spleen during childhood. The average interval between the initial trauma or surgery and the onset of splenosis ranges from 5 months to 32 years and lasts an average of 10 years [4]. Our case report is in accordance with Consensus based Surgical Case Report (SCAREcriteria) [9].
2. Clinical case
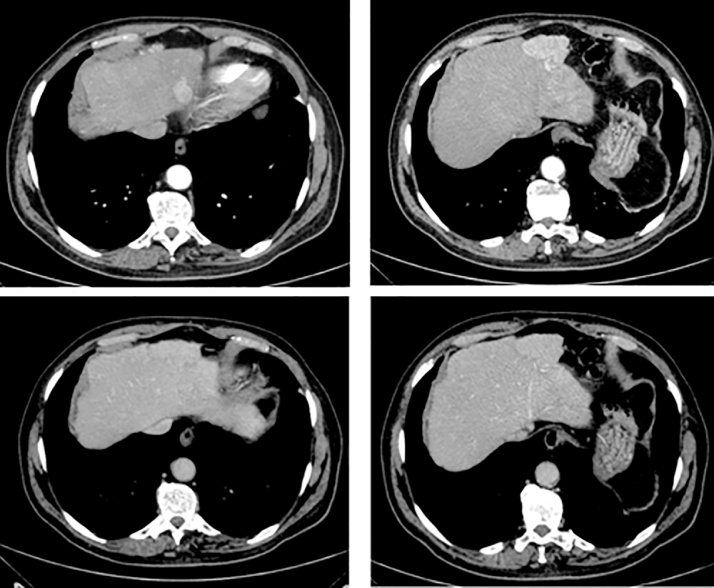
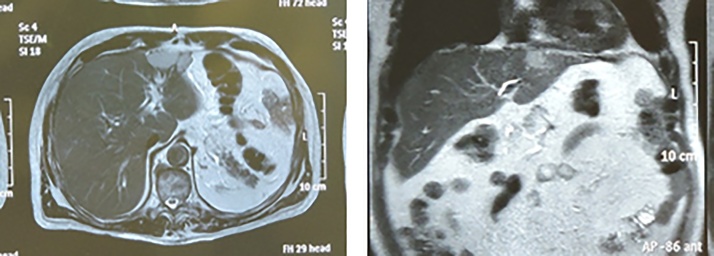
Male patient: 73 years of age; sought orthopedic care for lower back pain, at which point magnetic resonance imaging (MRI) of the spine was ordered. The MRI revealed tumors on the lumbar spine and the liver. The patient was referred to an oncologist and to a hepatobiliary and pancreatic surgeon for attempted treatment of the primary or secondary tumor on the liver; the patient reported no other issues. Patient reported no weight loss, diarrhea, or constipation. History of systemic arterial hypertension, nephropathy, carotid artery surgery, cholecystectomy and, a laparotomy in childhood for reasons unknown. He reported no smoking or drinking habits, nor any history of blood transfusions. The physical examination showed that the patient was in good overall health, eutrophic, and anicteric, with no pain in the abdomen, no palpable masses, and a supraumbilical transverse laparotomy scar on the midline. Exams were performed, and the findings were as follows: upper gastrointestinal endoscopy showed evidence of a prior gastrectomy with Billroth’s operation II; colonoscopy showed evidence of a prior resection of tubular adenomatous polyposis; abdominal ultrasound showed evidence of prior cholecystectomy and splenectomy, as well as two hepatic nodules in the left lobe that were 1.3 cm and 1.9 cm in diameter and one in the right lobe that was 0.7 cm in diameter; CT and MRI of the abdomen (Fig. 1, Fig. 2) also showed evidence of prior cholecystectomy and splenectomy, as well as a hepatic nodule in segment 2 that was 1.7 cm in diameter and one in segment 3 that was 4.9 cm in diameter, nodules which were suggestive of neoplasia; finally, the bone scintigraphy showed no lesions suggestive of secondary implants.
Fig. 1.
Computed Tomography (CT) of the abdomen.
Fig. 2.
MRI of the abdomen.
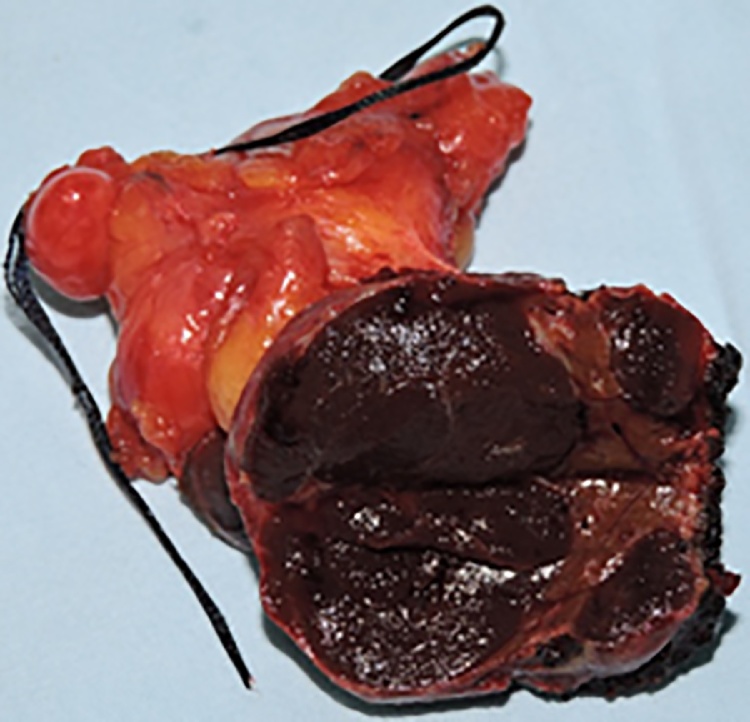
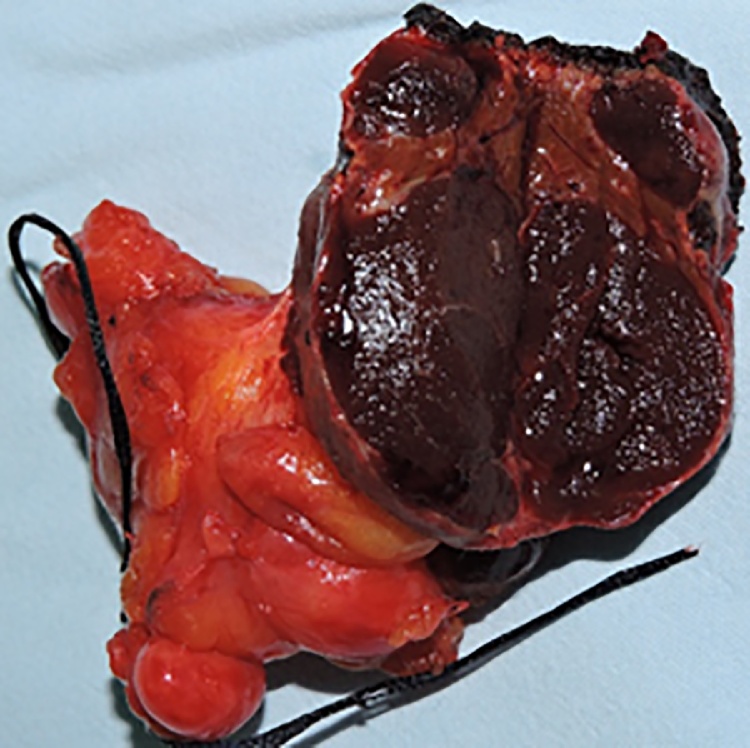
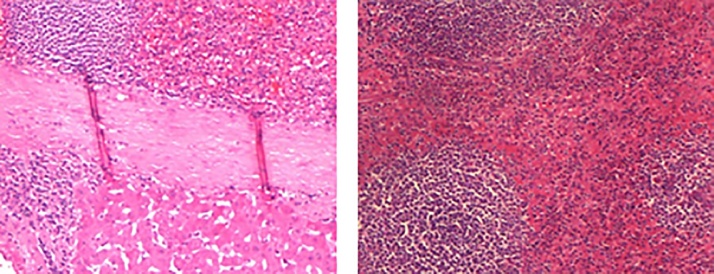
Tumor markers exams were requested and revealed normal alpha-fetoprotein and CA 19-9 levels; however, carcinoembryonic antigen (CEA) levels were slightly elevated. We therefore opted for surgical intervention after clinical evaluations of operative risk. A left lobectomy was performed, and the procedure resulted in no immediate postoperative complications. On the fourth postoperative day, the abdominal drain was removed and the patient was discharged from the hospital. During the outpatient follow-up period, the patient experienced a superficial infection of the surgical wound that was treated with antibiotic therapy; however, overall progression was favorable. Histopathology revealed intrahepatic heterotopic splenic parenchyma, with no evidence of neoplasia in either of the two lesions, the diameters of which were 1.5 cm and 3.6 cm (Fig. 3, Fig. 4, Fig. 5). The investigation by the oncologist was negative for primary cancer foci. In the case of his lumbar spine, the patient received treatment for chronic osteoarticular pain. Patient received outpatient follow-up care for 24 months and experienced no complications.
Fig. 3.
Macroscopy of the mass.
Fig. 4.
Macroscopy of the mass.
Fig. 5.
Microscopy of the mass.
3. Discussion
Splenosis is defined as a benign condition caused by the autoimplantation of splenic tissue exposed to circulation after trauma or iatrogenesis involving the spleen [5]. A possible mechanism is the hematogenous spread of splenic parenchyma, which generates intrahepatic nodules. Progenitor cells of erythrocytes of the spleen reach the liver through the portal vein and grow in response to tissue hypoxia [6].
Increases in the frequency of accidents resulting in abdominal trauma have made cases of splenosis more common. However, intrahepatic splenosis remains an extremely rare condition [2]. There are very few reports in the literature on the occurrence of intrahepatic splenosis. The existing descriptions are all of asymptomatic patients, as was the case with our patient.
Our clinical, laboratory, and imaging exams failed to reveal the etiology of the lesion. Because the masses were hypervascular lesions, a percutaneous liver biopsy was not feasible. Due to the uncertain diagnosis, we opted for surgical resection.
The most frequent sites of splenosis are, in descending order, the serous surface of the small intestine, the greater omentum, the parietal peritoneum, the large intestine, the small bowel mesentery, the lower portion of the diaphragm, and the thorax. Focal deposits outside the peritoneal cavity are rare [7].
Splenosis must be distinguished from accessory spleens. Implanted nodules have no hilum and are supplied by local arteries that penetrate the fibrous capsule. Accessory spleens, however, are located in regions close to the normal region of the spleen, in the area of the gastrosplenic and splenopancreatic ligaments; they also exhibit hlia, capsules, and their own irrigation [[6], [8]].
4. Conclusion
Through this report, we emphasize the importance of considering intrahepatic splenosis as a remote possibility in patients with hepatic nodules who have a history of splenectomy. It is important to take into account the patient’s clinical history and any complementary, non-conclusive exams when performing the histopathological diagnosis and deciding how to proceed.
Conflicts of interest
All authors declare no conflicts of interest relevant to this report.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
The study was approved by the Research Ethics Committee of the Faculdade Faceres − São Paulo (78153517.8.0000.8083) on 11/07/2017, under the number 2.369.042.
Consent
The participant agreeing to participate in the study were first informed of the research objectives and signed a Free and Informed Consent Form according to Resolution (Brazil) 466/12. Participant was assured that refusal to participate would not affect assessment in their disciplines. The information collected was used exclusively in research for academic purposes, and the confidentiality of the information was guaranteed
Author contribution
Gabriel Neves Saad Teles did the acquisition of data, analysis and interpretation of data and wrote the article, Paulo Eduardo Zerati Monteiro, did the surgery and collected cases’ outcomes and Raphael Raphe did the surgery, collected cases’ outcomes and did critically revised the manuscript; final version was approved by all authors.
Guarantor
Raphael Raphe
References
- 1.Buchbinder J.H., Lipkoff C.J. Splenosis, multiple peritoneal splenic implants following abdominal injury: a report of a case and review of the literature. Surgery. 1939;6:927–934. [Google Scholar]
- 2.Liu C., Liu J., Wang F. Intrahepatic splenosis mimicking liver câncer: report of a case and review of literature. Int. J. Clin. Exp. Pathol. 2015;8(1):1031–1035. [PMC free article] [PubMed] [Google Scholar]
- 3.Bresciani C., Ferreira N.R., Perez R.O., Jacob C.E., Zilberstein B., Cecconello I. Esplenose mimetizando GIST: Relato de caso e revisão da literatura. ABCD Arq. Bras. Cir. Dig. 2011;24(2):183–185. [Google Scholar]
- 4.Fremont R.D., Rice T.W. Splenosis a review. South. Med. J. 2007;100(6):589–593. doi: 10.1097/SMJ.0b013e318038d1f8. [DOI] [PubMed] [Google Scholar]
- 5.Dorota K., Peña A.S. Abdominal splenosis. Rev. Esp. Enferm. Dig. (Madrid) 2011;103(8):421–426. [PubMed] [Google Scholar]
- 6.Moreira R.C.L., Paula I.S., Silva M.M.Q., Bernardes B.R., Capanema H.X.M. Case report on splenosis: important differential diagnosis in patients whose spleens have been removed and who exhibit abdominal masses. Revista da Universidade Vale do Rio Verde, Três Corações. 2014;12(1):748–754. (Original Title in Portuguese: Relato de caso de esplenose: Diagnóstico diferencial importante em pacientes esplenectomizados apresentando massas abdominais) [Google Scholar]
- 7.González J.T., Artacho G.S., Solís I.M.R., Ruiz F.J.P., Ángel M. Intrahepatic splenosis as a differential diagnosis in focal liver lesions. Cir. Esp. 2014;92(10):688–698. doi: 10.1016/j.ciresp.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Kandil T.S., Sorogy M.E., Naiem Y., Elkashef W.F. Post-splenectomy splenosis presenting as hepatocellular carcinoma in the left lateral section of the liver: a case report. Int. J. Surg. Case Rep. 2014;5:877–878. doi: 10.1016/j.ijscr.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agha Riaz A., Fowler Alexander J., Saeta Alexander, Barai Ishani, Shivanchan Rajmohan, Orgill Dennis P. The SCARE statement: consensus-based surgicalcase report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]