Highlights
-
•
Gastrointestinal Stromal Tumours are a rare tumour of mesenchymal origin, and these tumours tend to be discovered incidentally.
-
•
Here, we discuss the case of a 57-year-old woman who underwent an emergency laporotomy for worsening occult GI bleed.
-
•
A 9.1 cm GIST was resected from her distal ileum
-
•
This occured on a background of two prior presentations of melena over a ten year period.
-
•
We suggest GIST should be considered as a possible differential in cases of gastrointestinal bleed, where other more common causes have been ruled out.
Keywords: Gastrointestinal stromal tumours, Melena, Case report
Abstract
Introduction
Gastrointestinal Stromal Tumors (GISTs) are a rare slow growing malignancy, accounting for less than 1% of all gastrointestinal (GI) tract tumors. These tumors are usually discovered incidentally by endoscopy, surgery or radiology. However on occasions they may present with significant symptoms including GI blood loss. This case report discusses an atypical presentation of a GIST in a 57-year-old female.
Case presentation
A 57-year-old woman presented to the emergency department following one episode of melena. This occurred on a background of two previous presentations with melena over a 10-year period. She had a preceding surgery for a Meckel’s Diverticulum. She was admitted for monitoring and investigation. An emergency upper endoscopy showed no upper gastrointestinal pathology to account for the bleeding. Her condition deteriorated with development of hypovolemic shock, requiring blood transfusion. An urgent CT angiogram identified a large mass in the distal ileum. The patient underwent an emergency laparotomy, where a 9.1 cm tumor located on the distal one-third of the ileum was resected. Histopathology confirmed the mass was a GIST. The patient had a successful post-operative period and subsequent treatment with Imatinib.
Discussion
The majority of GISTs are found incidentally. This case report describes an unusual presentation of a GIST in which the tumor bled into the intestinal lumen causing significant melena and life threatening hemorrhage.
Conclusion
We conclude that GIST should be considered as a possible differential in rare cases of GI bleeding where more common causes have been ruled out.
1. Introduction
Gastrointestinal Stromal Tumors (GISTs) are a rare slow growing malignancy, accounting for less than 1% of all gastrointestinal (GI) tract tumours [1]. However they are the most common tumor of mesenchymal origin in the GI tract [2]. GIST typically presents in patients in their sixties [3]. These tumors are usually discovered incidentally by endoscopy, surgery or radiology [4], but may on occasions be symptomatic. They are principally found in the stomach and small intestine. Very rarely they are found in extracolonic sites but they been reported in the mesentery and omentum. Tumor size dictates symptoms; with evidence suggesting the average size of tumor is 2.7 cm when asymptomatic and 8.1 cm when symptomatic [3]. Naturally larger lesions are more readily identified on radiological imaging. Symptoms tend to be non-specific but may include abdominal pain, intestinal obstruction, nausea, anorexia, weight loss and fever [5]. GIST may give rise to a chronic intraluminal GI bleed and thus the patient present with symptoms of malaise and anaemia. On rare occasions they may erode into the gastrointestinal tract or rupture cause catastrophic, life threatening intraperitoneal bleed [5].
Here we describe an unusual case of an extremely large GIST presenting with recurrent episodes of melena in a 57-year-old woman. This work has been reported in line with SCARE guidelines [6].
2. Case presentation
A 57-year-old woman self-presented to the emergency department with a significant gastrointestinal bleed. She had two similar admissions over the preceding ten years.
The patient described nausea, cramping and urgency, followed by the passage of a large volume of black tarry stool. There were no associated concerning symptoms in the months prior to current presentation. She denied abdominal pain, weight loss or change in bowel habit.
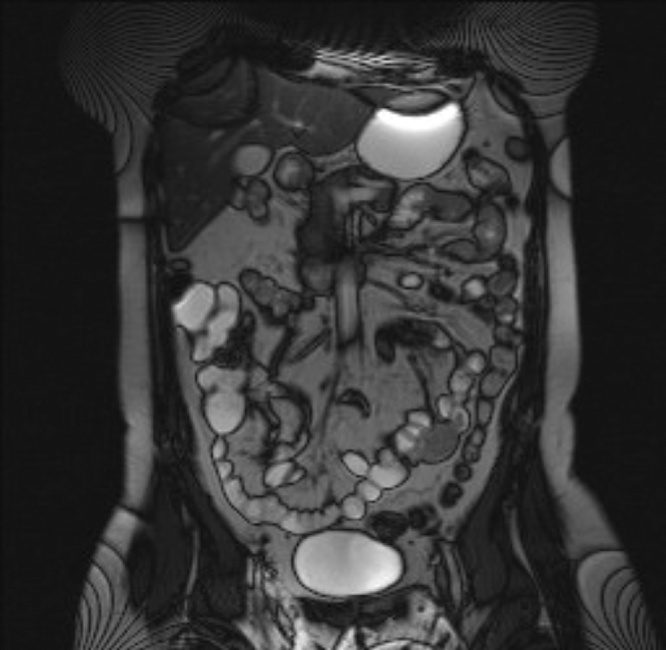
Of note, this patient had 2 previous admissions for melena in 2005 and 2011. Preceding upper endoscopies were normal with no pathology within stomach or duodenum to account for the melena. During her admission in 2005 she underwent a colonoscopy and polypectomy. On the same admission, an MRI small bowel follow through reported a 3 cm small bowel lesion (Fig. 1) suggestive of a Meckel’s diverticulum as a preceding isotope scan was positive for uptake in this region. She therefore underwent an appendectomy with excision of a Meckel’s diverticulum, which was confirmed on histology. In 2011 she represented with similar symptoms. An oesophago-gastro-duodenoscopy (OGD) and colonoscopy at that time were normal. Her haemoglobin remained within the normal range, and she was discharged. No abdominal imaging was performed. The presumptive diagnosis at this time point was angiodysplasia. We discussed a referral to another institute for a capsule endoscopy if symptoms recurred.
Fig. 1.
A coronal view of the patient’s abdomen on MRI-small bowel followthrough, showing a 3 cm lesion in the left lower quadrant.
This patient’s past medical history was significant for hypertension and hypothyroidism. Regular medications include telmisartan and levothyroxine. She had no known drug allergies. Her family history was significant for colorectal cancer; her brother was diagnosed aged 60 years old and her mother was diagnosed aged 82 years old. She was a non-smoker with an intake of 30 units of alcohol per week.
On initial presentation during this acute admission the patient was haemodynamically stable. Her abdomen was soft and non-tender. A stool sample was black in colour and was positive for occult blood. She was admitted for monitoring and investigation. Her haemoglobin on admission was 12 g/dl An emergency upper endoscopy showed no upper gastrointestinal pathology to account for the bleeding. Her condition subsequently deteriorated with development of hypovolemic shock, requiring blood transfusion. An urgent CT angiogram was requested to determine if identifiable source for bleeding. This showed a large mass in the distal bowel (Fig. 2).
Fig. 2.
An axial view of the patient’s pelvis on CT scan, showing a large lesion centrally communicating with the bowel.
The patient was considered too unstable to proceed with a minimally invasive approach. She underwent an urgent laparotomy, where a large mass was discovered on the surface of the distal third of the small bowel. The tumour, adjacent ileum and its mesentery were resected and a side-to-side anastomosis hand sewn anastomosis was performed in two layers. The 9.1 cm mass (Fig. 3) was sent to histopathology for diagnosis.
Fig. 3.
Large mass (9.1 cm), located on the distal one-third of the ileum, was resected along with adjacent ileum and corresponding mesentery.
This patient was monitored post-operatively. She experienced 2 episodes of melena post-operatively, and required 2 further units of red cells and transexamic acid. The haematology team was therefore involved in post-operative care. She was investigated for Von Willebrand’s Disease and the condition was ruled out. The post-operative melena was thought to be from residual blood sitting in the gastrointestinal tract. Over the following days everything stabilized, her hemoglobin remained stable and stool color returned to normal.
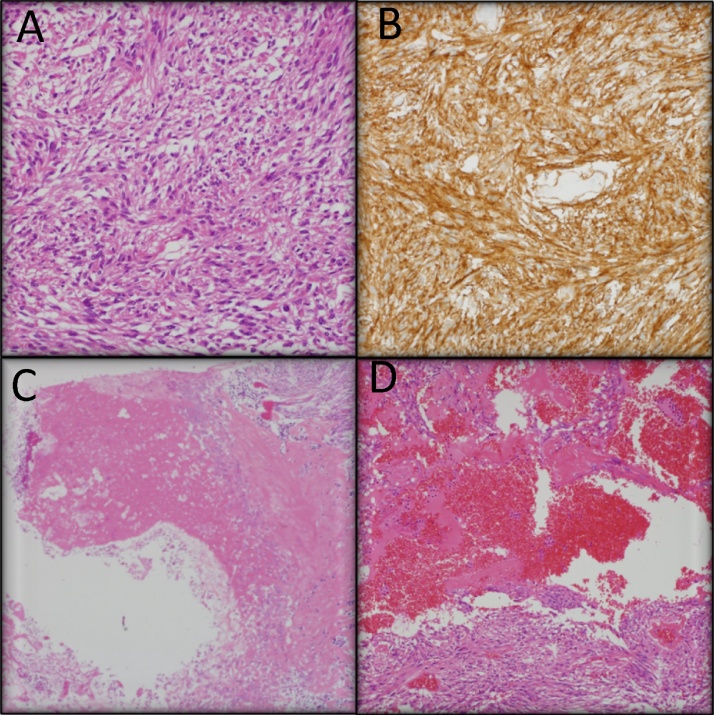
Histopathology confirmed the spindle cell nature of the resected lesion (Fig. 4A) and, along with positive staining with cKIT (Fig. 4B) and DOG1, confirmed this lesion was GIST in nature. Given the tumour size (9.1 cm), location (ileal) and mitotic count (<5 per 50 high power fields), this GIST was categorized as moderate risk [7]. Additionally, at the enteric luminal surface of the lesion there was significant mucosal ulceration (Fig. 4C) and deep to this the tumour was highly vascular (Fig. 4D), which would have accounted for her presentation with a significant gastrointestinal bleed. It was also found to have a KIT exon 11 mutation. The patient was followed up by medical oncology. Given the size and moderate risk associated with the GIST she was commenced on Imatinib therapy by the oncology team.
Fig. 4.
Histopathology results of the resected lesion. The tumour is confirmed GIST, given the spindle fibre arrangement of the lesion (A), and the fact that it is C-kit positive (B). Mucosal ulceration of the lesion (C) was also apparent, with a highly vascularised area deep to the mucosa (D);accounting for the intraluminal bleeding of this tumour.
In summary, this is a 57-year-old lady who presented to the emergency department with a significant gastrointestinal bleed. She presented with ongoing melena and haemodynamic changes necessitating transfusion. Following a normal OGD, a CT angiogram confirmed an intra-abdominal mass necessitating an emergency laparotomy. During this procedure, a large mass was visualized on the distal third of the ileum. This tumour was resected along with the adjacent ileum and mesentery. Histopathology confirmed the mass was GIST in origin and of moderate risk.
3. Discussion
We present the case of a 57-year-old woman who presented with a life threatening gastrointestinal bleed that was found to be secondary to a large 9.1 cm GIST found in the distal third of the ileum eroding onto the luminal surface. Notably, this lady presented with melena on two previous occasions over a ten-year period. GIST typically present with non-specific symptoms such as abdominal discomfort, anorexia, weight loss and fatigue [5]. In this case, the cause of melena was the large sized tumour resulting in pressure necrosis on the mucosa with subsequent ulceration and bleeding. This highlights a rare yet important cause of melena. Given the preceding Meckels diverticular resection the presumption on subsequent admissions was that her melena was secondary to angiodysplasia. However, in hindsight our impression is the lesion initially identified in 2005 on an MRI scan was incidental to the Meckels and represented a second pathology. Thus it was left in-situ at the initial surgery and not considered in the differential diagnosis subsequently. A capsule endoscopy if performed may potentially have identified the GIST at an early stage. Thus in patients who have obscure GIT bleeding in which endoscopy and colonoscopy have not identified a source capsule endoscopy should be considered.
A technical point in the above case is that following the small bowel resection we elected to perform the anastomosis using a hand-sewn technique as a stapled anastomosis is less haemostatic and there is the potential to bleed from a staple line. We wished to reduce this potential scenario in a patient who was unstable at the time of surgery, already had significant blood loss and potential for a coagulation disorder.
Another important point to note in this case report is that the source of bleeding was the distal ileum. Often when a patient presents with melena we associate this with pathology proximal to the ligament of Treitz; as defines an upper GI bleed. However, the above case highlights that it may also be secondary to distal small bowel pathology.
We conclude that GIST should be considered as a possible differential in rare cases of GI bleeding where more common causes have been ruled out. It also highlights the importance of considering differential diagnoses in patients who represent with ongoing symptoms despite a presumed preceding diagnosis.
Conflicts of interest
The authors confirm no conflicts of interest or biases.
Funding
No study sponsors.
Ethical approval
Granted by the ethics committee Galway University Hospital.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Grainne Mulkerrin – writing the paper, corresponding author.
Ms Niamh Hogan – selection of radiological images, editing.
Dr Margaret Sheehan – selection of histopathological images, editing.
Mr Myles Joyce – proposed case report, selection of images of gross pathology, selection of radiological images, editing.
Guarantor
Mr Myles Joyce.
References
- 1.Rubin B., Heinrich M., Corless C. Gastrointestinal stromal tumour. Lancet. 2007;369(9574):1731–1741. doi: 10.1016/S0140-6736(07)60780-6. [DOI] [PubMed] [Google Scholar]
- 2.Steigen S., Eide T. Gastrointestinal stromal tumors (GISTs): a review. APMIS. 2009;117(2):73–86. doi: 10.1111/j.1600-0463.2008.00020.x. [DOI] [PubMed] [Google Scholar]
- 3.Nilsson B., Bümming P., Meis-Kindblom J., Odén A., Dortok A., Gustavsson B. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era. Cancer. 2005;103(4):821–829. doi: 10.1002/cncr.20862. [DOI] [PubMed] [Google Scholar]
- 4.Søreide K., Sandvik O., Søreide J., Giljaca V., Jureckova A., Bulusu V. Global epidemiology of gastrointestinal stromal tumours (GIST): a systematic review of population-based cohort studies. Cancer Epidemiol. 2016;40:39–46. doi: 10.1016/j.canep.2015.10.031. [DOI] [PubMed] [Google Scholar]
- 5.Zhao Xiaohui. Changjun yue gastrointestinal stromal tumour. J. Gastrointest. Oncol. 2012;3(September (3)):189–208. doi: 10.3978/j.issn.2078-6891.2012.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34(October):180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Miettinen M. Lasota Gastrointestinal stromal tumors: pathology and prognosis at different sites. J. Semin. Diagn. Pathol. 2006;23(2):70–83. doi: 10.1053/j.semdp.2006.09.001. [DOI] [PubMed] [Google Scholar]