Abstract
Despite wide use in clinical practice, acupuncture remains a controversial treatment for chronic pain. Our objective was to update an individual patient data meta-analysis to determine the effect size of acupuncture for four chronic pain conditions. We searched MEDLINE and the Cochrane Central Registry of Controlled Trials randomized trials published up until December 31, 2015. We included randomized trials of acupuncture needling versus either sham acupuncture or no acupuncture control for non-specific musculoskeletal pain, osteoarthritis, chronic headache, or shoulder pain. Trials were only included if allocation concealment was unambiguously determined to be adequate. Raw data were obtained from study authors and entered into an individual patient data meta-analysis. The main outcome measures were pain and function. An additional 13 trials were identified, with data received for a total of 20,827 patients from 39 trials. Acupuncture was superior to both sham and no acupuncture control for each pain condition (all p<0.001) with differences between groups close to 0.5 standard deviations (SD) for comparison with no acupuncture control and close to 0.2 SDs in comparison with sham. We also found clear evidence that the effects of acupuncture persist over time with only a small decrease, approximately 15%, in treatment effect at one year. In secondary analyses, we found no obvious association between trial outcome and characteristics of acupuncture treatment, but effect sizes of acupuncture were associated with the type of control group, with smaller effects sizes for sham controlled trials that used a penetrating needle for sham, and for trials that had high intensity of intervention in the control arm. We conclude that acupuncture is effective for the treatment of chronic pain, with treatment effects persisting over time. While factors in addition to the specific effects of needling at correct acupuncture point locations are important contributors to the treatment effect, decreases in pain following acupuncture cannot be explained solely in terms of placebo effects. Variations in the effect size of acupuncture in different trials are driven predominately by differences in treatments received by the control group rather than by differences in the characteristics of acupuncture treatment.
Keywords: Acupuncture, chronic pain, meta-analysis, osteoarthritis, back pain, neck pain, migraine, tension-type headaches, shoulder pain
Introduction
Acupuncture remains a controversial treatment for chronic pain, largely due to a provenance outside biomedicine. Traditional acupuncture theory invokes non-anatomical structures such as meridians and non-physiological processes such as the flow of qi energy. Although many contemporary practitioners do not rely on such concepts, there remains a dearth of data on how insertion of needles at specific points on the body could lead to long-term decreases in pain. Acupuncture undoubtedly has short-term physiological effects, several of which are relevant to pain7, 76, 119, but there is as yet no explanation as to how such effects could persist.
We previously reported an individual patient data meta-analysis of high-quality trials of acupuncture for chronic pain.92 Differences between acupuncture and control in trials without sham (placebo) control were both statistically and clinically significant. Acupuncture was significantly superior to sham control, suggesting that acupuncture effects are not solely explicable in terms of placebo, although these differences were relatively modest. We have separately reported secondary analyses examining whether characteristics of acupuncture treatment65 or control groups68 influence effect size, and whether the effects of acupuncture treatment persist over time69. Here we update our prior analyses now including studies published during the last 7 years.
Methods
The full protocol of the meta-analysis93 and the results of the first individual patient data meta-analysis including RCTs published up to November 200892 have been published. The literature search was repeated to identify eligible RCTs published between December 2008 and December 2015. Trials were considered eligible if they accrued patients with nonspecific back or neck pain, shoulder pain, chronic headache, or osteoarthritis; pain duration was at least 4 weeks for musculoskeletal disorders; at least one group received acupuncture needling and one group received either sham acupuncture or no acupuncture control; the primary endpoint was measured more than 4 weeks after the initial acupuncture treatment; and allocation concealment was determined unambiguously to be adequate. Principal investigators of eligible studies were asked to provide raw data. These raw data were used to replicate all analyses published in the original RCT publication to ensure data accuracy. Each trial was reanalyzed by analysis of covariance with the standardized primary endpoint (scores divided by pooled standard deviation) as the dependent variable, and the baseline measure of the primary endpoint and variables used to stratify randomization as covariates. The primary outcome for each study was that identified by the responding author of each study. The effect sizes for each study were then entered into a meta-analysis using the metan command in Stata (version 13, StataCorp, College Station, TX). Both fixed effects and random effects estimates were calculated. Fixed effects weights were calculated using inverse-variance weighting, and random effects weights were calculated using the DerSimonian and Laird method. We pre-specified that meta-analyses would be conducted separately for comparisons of acupuncture vs. sham and acupuncture vs. no acupuncture control, and within each pain type, and the hypothesis test would be based on the fixed effects analysis. In the original paper, trials for which individual patient data were not available were included as a sensitivity analysis; in this update, we include summary data for these trials in the main meta-analysis and exclude them as a sensitivity analysis.
As secondary analyses, we examined whether characteristics of acupuncture treatment modified treatment effects. Both trial-level and patient-level analyses were performed. For trial-level analyses, we used random-effects meta-regression to test the effect of each characteristic on the main effect estimate using the Stata command metareg. For patient-level analyses, we created a linear regression as for the main analysis of effect size, but included the characteristic and an interaction term between the characteristic and treatment allocation. The coefficient was then entered into a meta-analysis. In both analyses, random effects estimates and 95% confidence intervals were reported; p values are based on the fixed effects analysis. We also analyzed the effect of acupuncture relative to different types of sham acupuncture and different types of no acupuncture control group. Three comparisons of sham acupuncture were investigated: penetrating needle vs both non-penetrating needle and non-needle sham; non-penetrating needle vs non-needle sham; and the use of true acupuncture points vs non-acupuncture points among trials using non-penetrating or non-needle sham. For sham arms using penetrating needles, there was also a comparison done between the use of deep needle penetration and shallow needle penetration. We entered the effect size and standard error for each trial into a meta-regression along with the type of sham acupuncture used in that trial. For this analysis, smaller effect sizes indicate a smaller difference in effect between verum acupuncture and sham acupuncture, implying that the type of sham acupuncture used is more active and therefore more similar to verum acupuncture. For the analysis of acupuncture effect relative to no acupuncture control group, we used meta-regression to compare the effects of trials using no acupuncture control groups characterized as high intensity, usual care, or low intensity. We also repeated our prior analyses exploring possible effects of publication bias and exploring difference between sham acupuncture and no treatment.
Results
Systematic Review
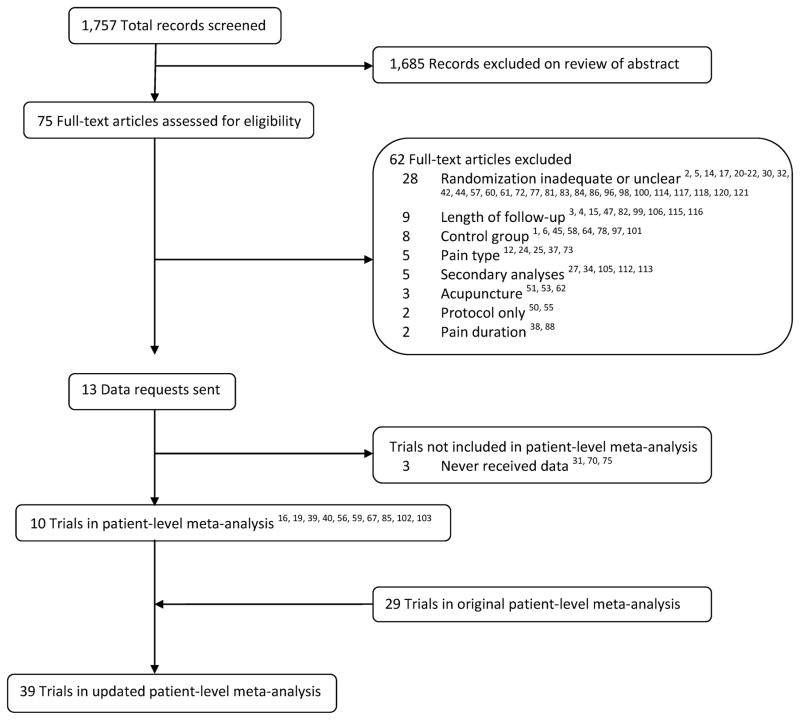
Our systematic review93 was updated to include trials published after November 2008 and before December 31, 2015. We identified 75 additional RCTs, of which 13 were eligible (Figure 1). These 13 studies include four trials19, 56, 75, 85 included as summary data only in a sensitivity analysis in our first report.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Data Extraction and Quality Assessment
Individual patient data for 2,905 patients were received from 10 of these 13 studies and included patients from the United States, Australia, China, Germany and the UK. For one of the three studies for which we did not receive data, the statisticians involved in the RCT failed to respond to repeated enquiries despite approval for data sharing being obtained from the principal investigator. For the other two studies, the trial authors were contacted and invited to participate but we received no further response. These three studies were included in the analysis as summary data only using the published estimates of effect size.31, 70, 75 Two trials from the original systematic review for which data were not received were also included as summary data in these analyses.23, 74
A total of 20,827 patients were included in the total 39 trials (Table 1). The trials comprised 25 comparisons with 16,041 patients of acupuncture and no acupuncture control, and 26 comparisons with 7,237 patients of acupuncture and sham acupuncture control. Of the trials on musculoskeletal pain, most had an eligibility criterion of a minimum 3 or 6 months pain duration. Amongst those for which individual patient data on chronicity were available, the median duration was 4 years (quartiles: 1.1 years, 10 years). There were two trials for which the time period between first symptom and evaluation of outcome could theoretically have been less than three months based on eligibility criteria and timing of assessment. For Irnich et al., the duration of disease was “4–52 weeks” for 19% of patients and longer than one year for the remainder.41 In the case of Kleinhenz et al., no data were provided on chronicity, however, the indication was rotator cuff tendinitis, which is rarely treated in the acute phase.52 We conclude that all but a trivial proportion of patients included in the analysis would have met the conventional definition of chronic pain, that is, pain lasting at least 3 to 6 months. Six sham RCTs were determined to have an intermediate likelihood of bias from unblinding.13, 26, 41, 49, 59, 103 In one trial, two types of sham acupuncture were used, although only one type (non-needle sham acupuncture) was found to have an intermediate likelihood of bias from unblinding.103 One trial (Hinman et al.) was determined to have a sham acupuncture arm with a high likelihood of bias from unblinding.39 This trial was excluded from the main analyses comparing acupuncture to sham acupuncture, but a sensitivity analysis including this trial was performed. None of the 10 new trials included in this analysis had dropout rates of higher than 25%.
Table 1.
Characteristics of included studies
| Indication (n=44) | Pain Type | Control Group | Primary Outcome Measure | Time Point |
|---|---|---|---|---|
| Chronic headache (n=9) | Migraine (n=3)26, 59, 63, tension-type headache (n=3)23, 28, 71, both31, 43, 95 (n=3) | Sham control (n=5)26, 28, 59, 63, 71 No acupuncture control (n=7); ancillary care (n=2)23, 31; usual care (n=4)43, 63, 71, 95; guideline care (n=1)26 |
Severity score (n=2)23, 95; days with headache (n=3)28, 43, 71; days with migraine (n=2)26, 59; days with moderate-to-severe pain (n=1)63; Migraine Disability Assessment (MIDAS) (n=1)31 | 1 mo (n=1)23 2 mo (n=1)31 3 mo (n=3)43, 63, 71 4 mo (n=1)59 6 mo (n=2)26, 28 12 mo (n=1)95 |
| Nonspecific musculoskeletal pain (back and neck) (n=18) | Back (n=12)11, 13, 18, 19, 36, 40, 48, 49, 74, 87, 102, 111; neck (n=6)41, 67, 79, 91, 104, 109 | Sham control (n=10)11, 13, 19, 36, 41, 48, 49, 74, 91, 104; No acupuncture control (n=12); Ancillary care (n=3)40, 74, 102; usual care (n=7)11, 19, 67, 79, 87, 109, 111; non-specific advice (n=1)18; guideline care (n=1)36 |
VAS (n=7)11, 13, 41, 49, 74, 91, 104; Roland Morris Disability Questionnaire (n=3)18, 19, 48; Northwick Park Neck Pain Questionnaire (n=2)67, 79; SF-36 Bodily pain (n=2)87, 102; Hannover Functional Questionnaire (n=1)111; Von Korff pain score (n=1)36; Oswestry Disability Index (n=1)40 | 1 mo (n=4)41, 49, 91, 104 2 mo (n=3)11, 18, 19 3 mo (n=5)48, 74, 79, 109, 111 4 mo (n=1)102 6 mo (n=2)36, 40 8 mo (n=1)13 12 mo (n=1)67 24 mo (n=1)87 |
| Osteoarthritis (n=13) | Sham control (n=10)8, 16, 33, 39, 70, 80, 85, 89, 103, 108 No acupuncture control (n=10); ancillary care (n=3)33, 70, 80; usual care (n=5)39, 56, 85, 108, 110; nonspecific advice (n=2)8, 107 |
WOMAC (n=5)16, 56, 70, 108, 110; WOMAC Pain subscore (n=4)8, 33, 80, 89; Oxford Knee score questionnaire (n=1)107; VAS103 (n=1); knee pain (0–10) (n=1)39; Joint-specific Multidimensional Assessment of Pain (n=1)85 | 1 mo (n=1)103 2 mo (n=3)70, 107, 108 3 mo (n=6)16, 39, 56, 85, 89, 110 6 mo (n=3)8, 33, 80 |
|
| Shoulder pain (n=4) | Sham control (n=4)35, 52, 75, 90 No-acupuncture control (n=1); ancillary care (n=1)75 |
Constant-Murley score (n=2)52, 90; VAS (n=2)35, 75 | 1 mo (n=2)52, 90 6 mo (n=2)35, 75 |
Meta-analysis
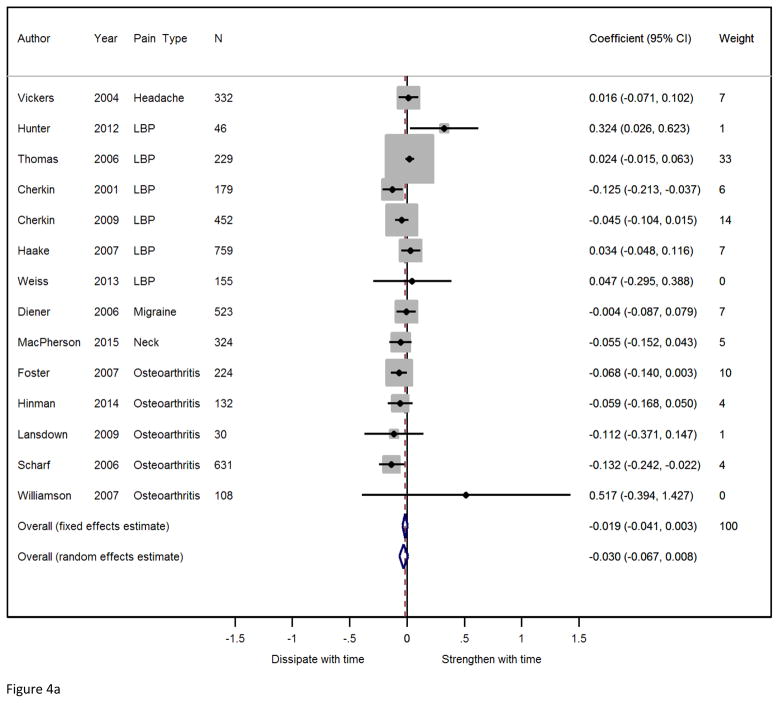
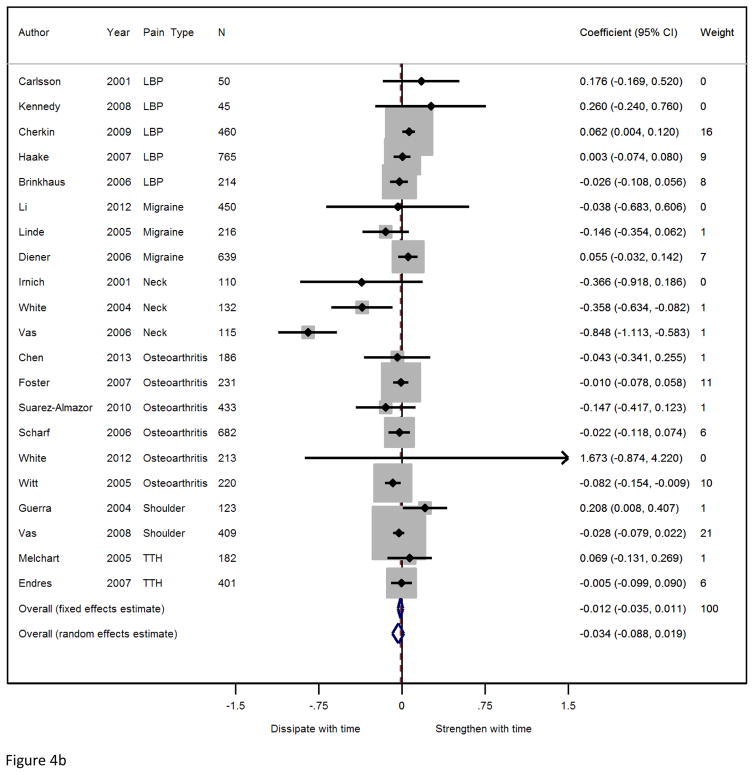
Forest plots for acupuncture against sham acupuncture and against no acupuncture control are shown separately for each of the 4 pain conditions in Figure 2 and Figure 3. Fixed effects weights are reported in Figures 2 and 3; forest plots with random effects weights reported are presented in Figures S1 and S2 of the supplementary materials. Meta-analytic statistics are shown in Table 2. Consistent with the results of the originally published meta-analysis, acupuncture is found to be statistically superior to control for all analyses (p < 0.001). Effect sizes in the updated analyses are similar to those in the original analyses, with effect sizes changing by 0.02 or less for most comparisons. Effect sizes are close to 0.5 in comparison to no acupuncture control and 0.2 for comparisons with sham. To illustrate these effect sizes in more clinically applicable terms, if baseline pain score in a typical RCT was 60 on a scale of 0–100, with a standard deviation of 25, follow-up scores might be 43 in a no acupuncture control group, 35 in a sham acupuncture group, and 30 among true acupuncture patients. If response were defined as a pain reduction of 50% or more, response rates would be approximately 30%, 42.5% and 50%, respectively. Also in keeping with the original analyses, significant heterogeneity was found in 5 out of 7 comparisons. Significant heterogeneity remained for sham-controlled musculoskeletal pain and osteoarthritis (p=0.001 and p<0.001, respectively) even after excluding the outlying Vas et al. trials. There was also significant heterogeneity for all indications in the comparison of acupuncture with no acupuncture control. Heterogeneity is further explored below (“Modifiers of Trial Outcome”).
Figure 2.
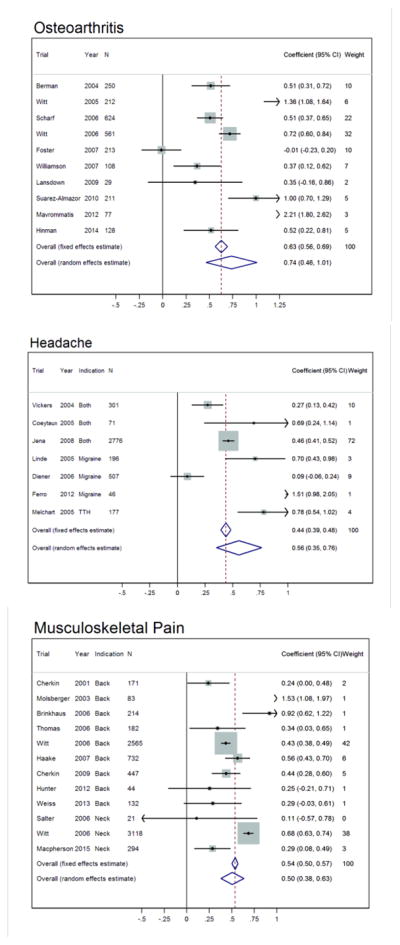
Forest plots for the comparison of acupuncture with no-acupuncture control. There were fewer than 3 trials for shoulder pain, so no meta-analyses were performed. Weights reported are fixed-effects weights calculated using inverse-variance weighting.
Figure 3.
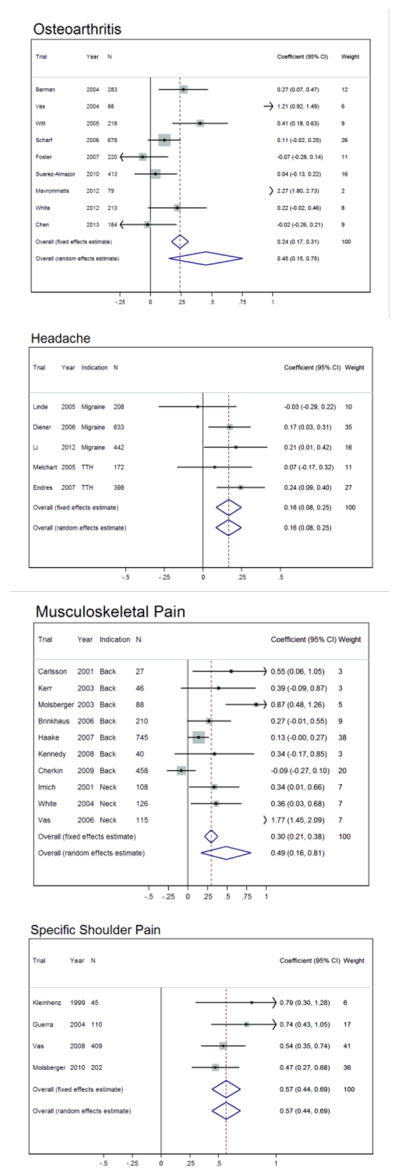
Forest plots for the comparison of true and sham acupuncture. Weights reported are fixed-effects weights calculated using inverse-variance weighting.
Table 2.
Primary Analyses, N=44 trials. Acupuncture is superior to control at p<0.001 except where indicated
| Sham | No acupuncture control | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Analysis | Indication | No. of studies |
FE (95% CI) | Heterogeneity p-value |
RE (95% CI) | No. of studies |
FE (95% CI) | Heterogeneity p-value |
RE (95% CI) |
| Main Analysis | Non-specific musculoskeletal pain | 10 | 0.30 (0.21, 0.38) | p<0.001 | 0.49 (0.16, 0.81) | 12 | 0.54 (0.50, 0.57) | p<0.001 | 0.50 (0.38, 0.63) |
| Osteoarthritis | 9 | 0.24 (0.17, 0.31) | p<0.001 | 0.45 (0.15, 0.75) | 10 | 0.63 (0.56, 0.69) | p<0.001 | 0.74 (0.46, 1.01) | |
| Chronic headache | 5 | 0.16 (0.08, 0.25) | p=0.4 | 0.16 (0.08, 0.25) | 7 | 0.44 (0.39, 0.48) | p<0.001 | 0.56 (0.35, 0.76) | |
| Shoulder | 4 | 0.57 (0.44, 0.69) | p=0.4 | 0.57 (0.44, 0.69) | 0 | No trials | |||
| Exclusion of Vas trials | Non-specific musculoskeletal pain | 9 | 0.19 (0.11, 0.28) | p=0.001 | 0.31 (0.13, 0.48) | ||||
| Osteoarthritis | 8 | 0.18 (0.10, 0.25) | p<0.001 | 0.35 (0.07, 0.62) | |||||
| Shoulder | 3 | 0.58 (0.42, 0.74) | p=0.2 | 0.61 (0.40, 0.81) | |||||
| Separate pain types | Back pain | 7 | 0.17 (0.07, 0.26) | p<0.001 | 0.30 (0.08, 0.52) | 9 | 0.46 (0.41, 0.50) | p<0.001 | 0.52 (0.37, 0.67) |
| Neck pain | 3 | 0.83 (0.64, 1.01) | p<0.001 | 0.82 (−0.11, 1.75) | |||||
| Excluding trials with summary data only | Non-specific musculoskeletal pain | 9 | 0.27 (0.19, 0.35) | p<0.001 | 0.44 (0.11, 0.78) | 11 | 0.53 (0.50, 0.56) | p<0.001 | 0.45 (0.33, 0.57) |
| Osteoarthritis | 8 | 0.19 (0.12, 0.26) | p<0.001 | 0.26 (0.04, 0.48) | 9 | 0.59 (0.52, 0.65) | p<0.001 | 0.59 (0.37, 0.82) | |
| Chronic headache | 5 | 0.43 (0.38, 0.47) | p<0.001 | 0.44 (0.24, 0.64) | |||||
| Shoulder | 3 | 0.62 (0.46, 0.77) | p=0.4 | 0.62 (0.46, 0.77) | |||||
| Excluding trials with possible bias due to blinding | Non-specific musculoskeletal pain | 7 | 0.28 (0.19, 0.37) | p<0.001 | 0.51 (0.09, 0.93) | ||||
| Osteoarthritis | 9 | 0.23 (0.16, 0.31) | p<0.001 | 0.44 (0.13, 0.75) | |||||
| Chronic headache* | 3 | 0.15 (0.03, 0.26) | p=0.15 | 0.12 (−0.05, 0.29) | |||||
| Including trials with high likelihood of bias due to blinding | Osteoarthritis | 10 | 0.23 (0.17, 0.30) | p<0.001 | 0.42 (0.14, 0.70) | ||||
| Multiple imputation | Non-specific musculoskeletal pain | 10 | 0.29 (0.21, 0.37) | p<0.001 | 0.49 (0.16, 0.81) | 12 | 0.54 (0.50, 0.57) | p<0.001 | 0.51 (0.38, 0.63) |
| Osteoarthritis | 9 | 0.24 (0.17, 0.31) | p<0.001 | 0.45 (0.15, 0.75) | 10 | 0.63 (0.57, 0.70) | p<0.001 | 0.74 (0.46, 1.01) | |
| Chronic headache | 5 | 0.17 (0.08, 0.25) | p=0.4 | 0.17 (0.08, 0.25) | 7 | 0.44 (0.40, 0.49) | p<0.001 | 0.55 (0.35, 0.75) | |
| Shoulder | 4 | 0.56 (0.44, 0.69) | p=0.4 | 0.56 (0.44, 0.69) | |||||
| Excluding trials where both acupuncture and control groups received additional treatments | Non-specific musculoskeletal pain | 10 | 0.54 (0.51, 0.57) | p<0.001 | 0.54 (0.40, 0.67) | ||||
| Osteoarthritis | 4 | 0.21 (0.11, 0.31) | p=0.081 | 0.22 (0.07, 0.38) | 7 | 0.70 (0.62, 0.78) | p<0.001 | 0.70 (0.47, 0.93) | |
| Chronic headache | 5 | 0.43 (0.38, 0.47) | p<0.001 | 0.44 (0.24, 0.64) | |||||
| Shoulder | 3 | 0.58 (0.42, 0.74) | p=0.2 | 0.61 (0.40, 0.81) | |||||
p=0.015
Sensitivity Analyses
Prespecified sensitivity analyses are also shown in Table 2. The exclusion of the RCTs by Vas et al.89–91 repeats our prior finding that the effect sizes for comparison with sham are similar for musculoskeletal pain, osteoarthritis and chronic headache. However, there are now sufficient trials for a meta-analysis of shoulder pain trials without inclusion of Vas et al.90 and the effect size for this indication is clearly much greater. There is also a large effect size for sham controlled neck pain trials when these are analyzed separately from back pain. Most other sensitivity analyses had little impact on the main findings. Analyses incorporating assessment of patient blinding, missing data or trials without individual patient data, all had very similar results to the primary analysis. As the primary outcome included in the analysis was the outcome specified by the trial authors, we also performed a sensitivity analysis restricted to a single endpoint (pain intensity) at a fixed follow-up time (2 – 3 months after randomization). Results were again very similar apart from sham-controlled trials of musculoskeletal pain (Table 3), where effect size decreased from 0.30 to 0.13, but this appears to be attributable to there being only 5 out of 11 trials that measured pain intensity at 2–3 months, and the trials excluded happened to be those with the larger effect sizes.
Table 3.
Sensitivity analyses including only pain endpoints measured between 2 and 3 months after randomization.
| Sham | No acupuncture control | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Analysis | Indication | No. of studies |
FE (95% CI) | Heterogeneity p-value |
RE (95% CI) | No. of studies |
FE (95% CI) | Heterogeneity p-value |
RE (95% CI) |
| Main Analysis | Non-specific musculoskeletal pain | 5 | 0.13 (0.01, 0.25) | p=0.005 | 0.23 (−0.03, 0.49) | 9 | 0.60 (0.56, 0.64) | p<0.0001 | 0.47 (0.34, 0.61) |
| Osteoarthritis | 7 | 0.31 (0.23, 0.39) | p<0.0001 | 0.69 (0.24, 1.14) | 9 | 0.73 (0.66, 0.80) | p<0.0001 | 0.88 (0.61, 1.15) | |
| Chronic headache | 5 | 0.14 (0.06, 0.22) | p=0.4 | 0.14 (0.06, 0.22) | 7 | 0.43 (0.38, 0.47) | p<0.0001 | 0.45 (0.27, 0.63) | |
| Shoulder | 2 | No meta-analysis | |||||||
We combined all trials into one meta-analysis for all indications to assess the possible effect of publication bias. As in the original analyses, we found some evidence that smaller studies had larger effect sizes for the sham comparison (p=0.024), but not for the no acupuncture comparisons (p=0.75). No significant asymmetry was seen after excluding the Vas trials and shoulder pain trials from the sham comparison (N=21, p=0.13), and also when excluding any trials with fewer than 100 patients (N=21, p=0.069). We found that the difference between acupuncture and control would become non-significant only if there were 51 and >100 unpublished trials with 100 patients and effect sizes in favor of control of 0.25 SD for sham and no acupuncture control respectively.
We also repeated our exploratory analysis comparing sham control with no acupuncture control. In a meta-analysis of 12 RCTs that had both sham and no acupuncture control arms, the effect sizes for sham were 0.39 (95% CI 0.33, 0.45) and 0.45 (95% CI 0.29, 0.61) for fixed and random effects, respectively (p<0.0001 for tests of both effect and heterogeneity).
Modifiers of trial outcome
In addition to updating the primary analyses, we also updated previously published analyses on how characteristics of the acupuncture and control interventions influence trial outcomes. Trial-level and patient-level characteristics are found in Tables 4 and 5, respectively.
Table 4.
Trial-level acupuncture characteristics, N=39. Counts for point prescription sum to 40 because one trial had two acupuncture groups, with each group receiving acupuncture based on a different point prescription.
| Style of Acupuncture | |
| Combination of traditional Chinese and Western | 9 (23%) |
| Traditional Chinese techniques | 23 (59%) |
| Western | 7 (18%) |
| Point Prescription | |
| Fixed needle formula | 9 (23%) |
| Flexible formula | 18 (45%) |
| Individualized | 13 (33%) |
| Location of needles | |
| Both Local and Distal Points | 37 (95%) |
| Distal Points Only | 2 (5.1%) |
| Electrical stimulation allowed | 11 (28%) |
| Manual stimulation allowed | 36 (92%) |
| Moxibustion allowed | 6 (15%) |
| Other Adjunctive Therapies Allowed | 8 (21%) |
| De Qi attempted (N=35) | 33 (94%) |
| Acupuncture-specific patient practitioner interactions | 16 (40%) |
| Minimum years of experience required | |
| No requirement specified (0 years) | 14 (36%) |
| 6 months to 2 years | 7 (18%) |
| 3–4 years | 13 (33%) |
| 5–9 years | 3 (7.7%) |
| 10 years | 2 (5.1%) |
| Maximum number of sessions | |
| 1–5 | 3 (7.7%) |
| 6–10 | 19 (49%) |
| 11–15 | 12 (31%) |
| 16–20 | 1 (2.6%) |
| 21–25 | 2 (5.1%) |
| 26–30 | 2 (5.1%) |
| Frequency of sessions (mean number of sessions per week) | |
| 0.88 | 1 (2.6%) |
| 1 | 19 (49%) |
| 1.43 | 1 (2.6%) |
| 1.5 | 7 (18%) |
| 1.67 | 1 (2.6%) |
| 2 | 9 (23%) |
| 5 | 1 (2.6%) |
| Mean duration of sessions, rounded to whole numbers (N=34) | |
| 15–19 minutes | 1 (2.9%) |
| 20–24 minutes | 11 (32%) |
| 25–29 minutes | 6 (18%) |
| 30+ minutes | 16 (47%) |
| Mean number of needles used (N=33) | |
| 1–4 | 3 (9.1%) |
| 5–9 | 11 (33%) |
| 10–14 | 12 (36%) |
| 15–20 | 7 (21%) |
Table 5.
Patient-level acupuncture characteristics, n=20,827.
| Number of Sessions | |
| 0 | 441 (2.1%) |
| 1–5 | 515 (2.5%) |
| 6–10 | 8003 (38%) |
| 11–15 | 2065 (10%) |
| 16–20 | 40 (0.2%) |
| 21–30 | 15 (<0.1%) |
| Missing | 1989 (10%) |
| Not reported | 7759 (37%) |
| Average Session Duration | |
| 2–15 | 163 (0.8%) |
| 15–30 | 2668 (13%) |
| 31–45 | 377 (1.8%) |
| 46–60 | 25 (0.1%) |
| 60+ | 1 (<0.1%) |
| Missing | 896 (4.3%) |
| Not reported | 16697 (80%) |
| Average Number of Needles | |
| 2–5 | 22 (0.1%) |
| 6–10 | 910 (4.4%) |
| 11–15 | 762 (3.7%) |
| 16–20 | 825 (4.0%) |
| 21–25 | 199 (1.0%) |
| 26+ | 30 (0.1%) |
| Missing | 1621 (7.8%) |
| Not reported | 16458 (79%) |
| Age of Physician/Acupuncturist | |
| 30–35 | 298 (1.4%) |
| 36–40 | 2119 (10%) |
| 41–45 | 2630 (13%) |
| 46–50 | 2407 (12%) |
| 51–55 | 1701 (8.2%) |
| 56–60 | 872 (4.2%) |
| 60+ | 303 (1.5%) |
| Missing | 368 (1.8%) |
| Not reported | 10129 (49%) |
| Physician/Acupuncturist Sex | |
| Female | 3626 (17%) |
| Male | 7002 (34%) |
| Missing | 70 (0.3%) |
| Not reported | 10129 (49%) |
Acupuncture Characteristics Analysis
We updated previously reported analyses examining whether characteristics of acupuncture treatment modified the effect of acupuncture relative to control. These analyses include both trial-level analysis, based on characteristics described in the study protocol, and patient-level analyses, based on data related to the individual patient. The results are shown in Table 6. We did not find any obvious association between trial outcome and characteristics such as the style of acupuncture (Traditional or Western), use of fixed versus individualized point selection or the use of electrical stimulation. The only clear finding was a dose-response effect to number of acupuncture treatments in trials with a no acupuncture control group (increase in effect size of 0.10 per five sessions, 95% CI −0.01, 0.21, p=0.001).
Table 6.
Results of univariate meta-regression analyses for the effect of acupuncture characteristics on acupuncture effect. β is an estimate of the change in the effect of acupuncture in terms of standardized difference compared to controls for each characteristic; a positive β indicates a larger effect of acupuncture compared to controls for trials. N is number of trials. The number of patients in the analysis and number of patients in included trials are given in parentheses where applicable.
| Sham acupuncture | No acupuncture control | |||||||
|---|---|---|---|---|---|---|---|---|
| N | β | 95% CI | p value | N | β | 95% CI | p value | |
| Style of acupuncture | 25 | 25 | ||||||
| Some TCM vs. Western only | −0.00 | −0.49, 0.48 | >0.9 | 0.10 | −0.55, 0.74 | 0.8 | ||
| TCM only vs. some Western | 0.02 | −0.38, 0.42 | 0.9 | −0.07 | −0.42, 0.28 | 0.7 | ||
| Point prescription | 25 | 25 | ||||||
| Fixed needle formula | Ref. | 0.6 | Ref. | 0.075 | ||||
| Flexible formula | 0.20 | −0.21, 0.60 | 0.01 | −0.45, 0.46 | ||||
| Fully individualized | −0.01 | −0.75, 0.73 | −0.34 | −0.79, 0.10 | ||||
| Electrical stimulation allowed | 25 | 0.32 | −0.11, 0.75 | 0.14 | 25 | −0.12 | −0.50, 0.26 | 0.5 |
| Manual stimulation allowed | 25 | 0.26 | −0.42, 0.95 | 0.5 | 25 | −0.38 | −0.99, 0.23 | 0.2 |
| Moxibustion allowed | No trials allowed | 25 | −0.32 | −0.71, 0.06 | 0.10 | |||
| Other adjunctive treatment allowed | 25 | −0.04 | −1.00, 0.92 | 0.9 | 25 | −0.22 | −0.59, 0.16 | 0.3 |
| De qi attempted | 25 | 0.29 | −0.67, 1.24 | 0.6 | 21 | 0.74 | −0.04, 1.52 | 0.063 |
| Acupuncture-specific patient practitioner interactions allowed | 25 | −0.03 | −0.50, 0.44 | 0.9 | 25 | −0.05 | −0.38, 0.28 | 0.8 |
| Minimum experience required (years) | 25 | 0.04 | −0.05, 0.13 | 0.4 | 25 | 0.05 | −0.03, 0.12 | 0.2 |
| Maximum number of sessions (per 5 sessions) | 25 | −0.01 | −0.23, 0.22 | 0.9 | 25 | 0.01 | −0.12, 0.14 | 0.9 |
| Patient-level analysis | 5 (1317/1377) | 0.09 | −0.31, 0.48 | 0.7 | 5 (8036/10157) | 0.10 | −0.01, 0.21 | 0.001 |
| Patient-level analysis, including Hinman trial | 6 (1421/1517) | −0.03 | −0.36, −0.30 | 0.9 | ||||
| Frequency of sessions (per week) | 25 | −0.06 | −0.29, 0.18 | 0.6 | 25 | 0.21 | −0.22, 0.64 | 0.3 |
| Duration of sessions (per 5 minutes) | 25 | 0.06 | −0.13, 0.25 | 0.5 | 20 | −0.06 | −0.25, 0.13 | 0.5 |
| Patient-level analysis | 6 (2863/2969) | 0.01 | −0.08, 0.09 | 0.9 | ||||
| Number of needles used (per 5 needles) | 25 | 0.05 | −0.17, 0.27 | 0.6 | 19 | 0.16 | −0.05, 0.38 | 0.13 |
| Patient-level analysis | 5 (2232/2317) | 0.04 | −0.08, 0.16 | 0.5 | ||||
| Age of practitioner (per 5 years) | ||||||||
| Patient-level analysis | 6 (9127/10550) | −0.01 | −0.04, 0.02 | 0.5 | ||||
| Male practitioner | ||||||||
| Patient-level analysis | 6 (9384/10550) | −0.07 | −0.16, 0.02 | 0.084 | ||||
Sham Acupuncture Control Analysis
We also updated a previously published analysis looking at the effects of acupuncture relative to different types of sham acupuncture and no acupuncture control groups. Differences in effect between acupuncture and the different sham acupuncture groups are found in Table 7. The largest difference in effect between acupuncture and sham acupuncture was seen in trials using non-penetrating needles, while the smallest difference was seen in trials using needle penetration. Significant differences were found between trials using penetrating needle sham and those trials that used non-penetrating or non-needle sham (difference in SD −0.30, 95% CI −0.60, −0.00, p=0.047), although this result was sensitive to the exclusion of the outlying Vas trials (difference in SD −0.07, 95% CI −0.24, 0.10, p=0.4, Table 8), two of which used non-penetrating controls.
Table 7.
Differences in effect size (in SD) between acupuncture and sham acupuncture groups (N=25) and between acupuncture and no acupuncture control groups (N=24). Total number of sham acupuncture-controlled trials sums to 26 because one trial had two different types of sham acupuncture control.
| Sham Acupuncture | |||
|---|---|---|---|
| Type of Control Group | N | Effect Size (95% CI) | p value |
| Penetrating needle sham | 11 | 0.17 (0.11, 0.22) | <0.0001 |
| Excluding B blinding grades | 9 | 0.16 (0.09, 0.24) | <0.0001 |
| Non-penetrating needle and non-needle sham | 15 | 0.48 (0.22, 0.74) | 0.0003 |
| Excluding B blinding grades | 11 | 0.51 (0.16, 0.86) | 0.004 |
| Including Hinman trial | 16 | 0.46 (0.21, 0.70) | 0.0003 |
| Excluding Vas trials | 12 | 0.27 (0.10, 0.44) | 0.002 |
| Non-penetrating needle sham | 10 | 0.52 (0.14, 0.91) | 0.007 |
| Excluding Vas trials | 7 | 0.22 (−0.05, 0.49) | 0.11 |
| Non-needle sham | 5 | 0.37 (0.21, 0.52) | <0.0001 |
| Including Hinman trial | 6 | 0.32 (0.18, 0.46) | <0.0001 |
| True acupuncture points (no penetrating needle sham) | 12 | 0.48 (0.15, 0.80) | 0.004 |
| Excluding B blinding grades | 10 | 0.51 (0.12, 0.89) | 0.010 |
| Including Hinman trial | 13 | 0.45 (0.15, 0.75) | 0.003 |
| Excluding Vas trials | 10 | 0.25 (0.06, 0.44) | 0.011 |
| Non-acupuncture points (no penetrating needle sham) | 3 | 0.52 (0.35, 0.69) | <0.0001 |
| Excluding Vas trials | 2 | 0.47 (0.13, 0.81) | 0.007 |
| No Acupuncture Control | |||
| Type of Control Group | N | Effect Size (95% CI) | p value |
| High intensity | 5 | 0.34 (0.11, 0.57) | 0.003 |
| Usual care and low intensity | 19 | 0.56 (0.43, 0.69) | <0.0001 |
| Usual care | 17 | 0.50 (0.40, 0.60) | <0.0001 |
| Low intensity | 2 | 1.14 (0.71, 1.58) | <0.0001 |
Table 8.
Differences in effect size between different types of control group. A negative effect size indicates that there is a smaller difference in effect between acupuncture and control for group 1 than for group 2, that is, the effect of control group 1 is more similar to verum acupuncture than the effect of control group 2.
| Sham Acupuncture | |||
|---|---|---|---|
| Group 1 | Group 2 | Effect Size (95% CI) | p value |
| Penetrating needle sham | Non-penetrating and non-needle sham | −0.30 (−0.60, −0.00) | 0.047 |
| Excluding B blinding grades | −0.33 (−0.72, 0.05) | 0.088 | |
| Including Hinman trial | −0.28 (−0.57, 0.01) | 0.061 | |
| Excluding Vas trials | −0.07 (−0.24, 0.10) | 0.4 | |
| Non-penetrating needle sham | Non-needle sham | 0.13 (−0.44, 0.70) | 0.6 |
| Including Hinman trial | 0.18 (−0.34, 0.70) | 0.5 | |
| Excluding Vas trials | −0.18 (−0.52, 0.17) | 0.3 | |
| True acupuncture points, excluding penetrating needle sham | Non-acupuncture points, excluding penetrating needle sham | −0.02 (−0.70, 0.66) | 0.9 |
| Including Hinman trial | −0.05 (−0.71, 0.61) | 0.9 | |
| Excluding Vas trials | −0.22 (−0.75, 0.30) | 0.4 | |
| No Acupuncture Controls | |||
| Group 1 | Group 2 | Effect Size (95% CI) | p value |
| High intensity | Usual care and low intensity | −0.23 (−0.50, 0.05) | 0.11 |
| High intensity | Low intensity | −0.81 (−1.26, −0.36) | 0.0004 |
| Usual care | Low intensity | −0.65 (−0.98, −0.31) | 0.0002 |
No Acupuncture Control Analysis
In addition to updating the analysis comparing types of sham acupuncture control, we also updated the analysis comparing types of no acupuncture control. We updated the categorization of no acupuncture control groups, and categorized trials as having a high intensity, usual care, or low intensity control group. In a “high intensity” control group, patients received a specified course of protocol-guided treatment. For instance, the UK APEX trial by Foster et al.33 is considered a high intensity control because patients were randomized to receive a course of individualized, supervised physical therapy plus acupuncture vs. physical therapy alone. In a trial with “usual care” control, patients are able to access whatever care they might reasonably receive outside of the study. As an example, in the UK NHS study, patients were randomized to “use” vs. “avoid” acupuncture and could receive whatever other treatments were offered to them.95 A control group was defined as “low intensity” if patients were not allowed to receive certain treatments that might otherwise be available. For instance, the Acupuncture Randomized Trials for low back pain and osteoarthritis limited treatment of pain in the control group to oral nonsteroidal anti-inflammatory drugs, excluding other types of treatment, such as steroids and other classes of analgesics.11, 108 Trials were assessed and assigned a control group type by three collaborators, with disagreements resolved by consensus. One trial was excluded from this analysis as there was a reasonable argument that it involved active control, prespecified to be excluded.26 Differences in effect between acupuncture and no acupuncture control groups are presented in Table 7. Significant differences were found between acupuncture and control for all types of no acupuncture control group. Notably, however, in trials that had high intensity control groups, acupuncture had smaller effect sizes compared to those with low intensity controls groups (difference −0.81, 95% CI −1.26, −0.36, p=0.0004); similarly in trials with usual care control acupuncture had smaller effect sizes than trials with a low intensity control group (difference in SD −0.65, 95% CI −0.98, −0.31, p=0.0002, Table 8).
Time Course of Acupuncture Effects Analysis
We updated a previously published analysis assessing change in the effects of acupuncture over time relative to sham acupuncture and no acupuncture control69. Number of weeks of acupuncture treatment and the time points used in this analysis are reported in Table 9. A total of 14 trials and 4,124 patients were included in the analysis of acupuncture vs no acupuncture control. The fixed-effects estimate for the between-group comparison of acupuncture vs no acupuncture controls showed a decrease in the effect size of acupuncture of 0.019 SD per 3 months (95% CI −0.041, 0.003, p=0.096, p=0.011 for heterogeneity, Figure 4a). Given a difference between acupuncture and no acupuncture control of around 0.5 SD, this is equivalent to about a 15% decrease in acupuncture effect relative to control at 1 year after randomization, which was usually between 9 and 10 months after the end of treatment. In the analysis of acupuncture vs sham acupuncture, a total of 21 trials and 6,276 patients were included. There was a non-significant decrease of 0.012 SD per 3 months in acupuncture relative to sham acupuncture (95% CI −0.035, 0.011, p=0.3, Figure 4b), about a 25% decrease in acupuncture effect at 1 year after randomization. Significant heterogeneity among trials was seen (p<0.0001). The previous analysis found that the decrease in effect of acupuncture relative to sham was driven by the decrease in neck pain trials (a decrease of 0.587 SD per 3 months, 95% CI −0.767, −0.406, p<0.0001). We also analyzed the change in acupuncture relative to sham excluding these trials and found a non-significant decrease of −0.003 SD per 3 months (95% CI −0.026, 0.020, p=0.8) with no significant heterogeneity among trials (p=0.12). Hence almost all the decrease in acupuncture effects in this analysis seems attributable to neck pain.
Table 9.
Trials with sham and no acupuncture control and time points assessed after the end of treatment
| Sham Acupuncture | No acupuncture control | ||||||
|---|---|---|---|---|---|---|---|
| Trial Name | Pain Condition | Average Length of Treatment | Time Points after End of Treatment | Included in meta-analysis | Control patients offered acupuncture treatment (Crossover) | Time Points after End of Treatment | Included in meta-analysis |
| Carlsson 200113 | Low Back Pain | 8 weeks | Weeks 5 and 18 | Yes | |||
| Chen 201316 | Osteoarthritis | 12 weeks | End of treatment and week 14 | Yes | |||
| Endres 200728 | Headache | 6 weeks | End of treatment and weeks 7 and 20 | Yes | |||
| Guerra de Hoyos 200435 | Shoulder | 8 weeks | Weeks 5 and 18 | Yes | |||
| Irnich 200141 | Neck | 3 weeks | Weeks 1 and 10 | Yes | |||
| Kennedy 200848 | Low Back Pain | 5 weeks | End of treatment and week 7 | Yes | |||
| Kerr 200349 | Low Back Pain | 6 weeks | None | No | |||
| Kleinhenz 199952 | Shoulder | 4 weeks | End of treatment | No | |||
| Li 201259 | Migraine | 4 weeks | End of treatment and week 4 | Yes | |||
| Vas 200489 | Osteoarthritis | 12 weeks | Week 1 | No | |||
| Vas 200691 | Neck | 3 weeks | Weeks 1 and 25 | Yes | |||
| Vas 200890 | Shoulder | 3 weeks | Weeks 1 and 10 | Yes | |||
| White 2004104 | Neck | 4 weeks | End of treatment and weeks 1 through 8 | Yes | |||
| White 2012103 | Osteoarthritis | 4 weeks | End of treatment and week 1 | Yes | |||
| Berman 20048 | Osteoarthritis | 26 weeks | End of treatment | No | No | End of treatment | No |
| Brinkhaus 200611 | Low Back Pain | 8 weeks | End of treatment and weeks 18 and 44 | Yes | At 8 weeks | End of treatment | No |
| Cherkin 200919 | Low Back Pain | 7 weeks | Weeks 1, 19 and 45 | Yes | No | Weeks 1, 19 and 45 | Yes |
| Diener 200626 | Migraine | 6 weeks | End of treatment and weeks 7 and 20 | Yes | No | End of treatment and weeks 7 and 20 | Yes |
| Foster 200733 | Osteoarthritis | 3 weeks | Weeks 3, 23 and 49 | Yes | No | Weeks 3, 23 and 49 | Yes |
| Haake 200736 | Low Back Pain | 6 weeks | End of treatment and weeks 7 and 20 | Yes | No | End of treatment and weeks 7 and 20 | Yes |
| Linde 200563 | Migraine | 8 weeks | End of treatment and weeks 4 and 16 | Yes | At 12 weeks | Week 4 | No |
| Melchart 200571 | Headache | 8 weeks | End of treatment and weeks 4 and 16 | Yes | At 12 weeks | Week 4 | No |
| Scharf 200680 | Osteoarthritis | 6 weeks | Weeks 7 and 20 | Yes | No | Weeks 7 and 20 | Yes |
| Suarez-Almazor 201085 | Osteoarthritis | 6 weeks | End of treatment and week 7 | Yes | No | Week 7 | No |
| Witt 2005108 | Osteoarthritis | 8 weeks | End of treatment and weeks 18 and 44 | Yes | At 8 weeks | End of treatment | No |
| Cherkin 200118 | Low Back Pain | 10 weeks | No | End of treatment and week 42 | Yes | ||
| Hinman 201439 | Osteoarthritis | 12 weeks | No | End of treatment and week 40 | Yes | ||
| Hunter 201240 | Low Back Pain | 6 weeks | No | Weeks 2, 7 and 20 | Yes | ||
| Jena 200843 | Headache | 12 weeks | At 12 weeks | All measurements after crossover | No | ||
| Lansdown 200956 | Osteoarthritis | 10 weeks | No | Weeks 3 and 42 | Yes | ||
| MacPherson 201567 | Neck | 16 weeks | No | Weeks 10 and 36 | Yes | ||
| Thomas 200687 | Low Back Pain | 12 weeks | No | Weeks 1, 40 and 92 | Yes | ||
| Salter 200679 | Neck | 12 weeks | No | Week 1 | No | ||
| Vickers 200495 | Headache | 6 weeks | No | Weeks 1 and 40 | Yes | ||
| Weiss 2013102 | Low Back Pain | 4 weeks | No | End of treatment and week 13 | Yes | ||
| Williamson 2007107 | Osteoarthritis | 6 weeks | No | Weeks 1 and 6 | Yes | ||
| Witt 2006109 | Neck | 12 weeks | At 12 weeks | All measurements after crossover | No | ||
| Witt 2006110 | Osteoarthritis | 12 weeks | At 12 weeks | All measurements after crossover | No | ||
| Witt ARC 2006111 | Low Back Pain | 12 weeks | At 12 weeks | All measurements after crossover | No | ||
Figure 4.
Forest plot showing the difference in pain change scores between acupuncture and no acupuncture control groups (a) and between acupuncture and sham acupuncture groups (b) over time. A coefficient of 0.01 means that the difference between acupuncture and control increases by 0.01 standard deviations for each 3 months following the end of treatment.
As a sensitivity analysis, we repeated the analyses including only trials that found a significant difference between acupuncture and control, as trials that showed no difference between groups cannot show a reduction in acupuncture effects over time. Nine trials with 2,997 patients were included in this analysis for the comparison between acupuncture and no acupuncture controls. A smaller and still non-significant decrease in the effect of acupuncture was found (−0.008 SD per 3 months, 95% CI −0.034, 0.018, p=0.5) and heterogeneity between trials was reduced (p=0.082). None of the newly included trials showed a significant effect of acupuncture vs sham and so this analysis of sham-controlled trials with a significant effect contains the same 7 trials and 1,450 patients and has the same results as reported in the original publication (−0.049 SD per 3 months, 95% CI −0.086, −0.013, p=0.008, heterogeneity p<0.0001).
Discussion
We updated an individual patient data meta-analysis of high-quality trials of acupuncture for chronic pain with seven additional years of data. An additional 10 studies were included with nearly 3,000 patients. In total, our analyses include 39 studies and 20,827 patients. The results confirm and strengthen prior key findings that acupuncture has a clinically relevant effect compared to no acupuncture control. Moreover, we confirmed that, although the effects of acupuncture are not completely explicable in terms of placebo effects, factors other than the specific effects of needling at correct acupuncture point locations are important contributors to acupuncture treatment benefit. Effects of acupuncture appear to persist over at least a 12 month period.
Heterogeneity continues to be an obvious aspect of our findings, with the results of trials varying by more than would be expected by chance. We have presented data that heterogeneity is predominately driven by differences between control groups rather than by differences between acupuncture treatment characteristics. We did not find any obvious differences between the results of trials depending on treatment characteristics such as style of acupuncture, duration of treatment sessions or training of acupuncturists. By contrast, we found evidence that effect sizes of acupuncture were smaller for sham-controlled trials with penetrating needles and for no acupuncture control trials where patients received high intensity care (e.g. a trial of acupuncture plus physical therapy vs. physical therapy alone). In some cases, heterogeneity was also driven by a set of outlying trials with large effect sizes. We have presented these analyses with and without the outlying trials to provide all necessary information for interpreting these results and drawing conclusions.
Another novel finding is the higher than average effects of acupuncture on upper body musculoskeletal pain. We now have sufficient data to conduct a meta-analysis for neck pain and for shoulder pain, even after exclusion of outlying trials. The effect sizes versus sham, 0.57 for shoulder and 0.83 for neck pain, were much larger than seen for low back pain, osteoarthritis and headache, although we also saw evidence that treatment benefits did not persist for neck pain.
Since publication of our results, there has been no substantive critique of our methodology in the peer-reviewed literature. The main issue under discussion seems to be whether the effect size of acupuncture is clinically relevant94, specifically, whether clinical relevance is determined by the comparison with no acupuncture control or by comparison with sham. We have previously argued in favor of the former, on the grounds that the clinical decision made by a referring clinician in discussion with their patient is not between acupuncture and sham but between acupuncture and no acupuncture. Our argument is given the context of the excellent safety profile of acupuncture66, evidence that the non-specific effects of acupuncture are particular to acupuncture and are not easily reproduced46, 54 and evidence provided here and elsewhere9 that some interventions used as sham acupuncture may be physiologically active.
It is also illustrative to compare our results to those of other interventions routinely used in clinical practice. For instance, in one meta-analysis of non-steroidal anti-inflammatory drugs (NSAIDs) for osteoarthritis of the knee, the effect size for NSAIDs vs placebo for trials that did not preselect NSAID responders was 0.23;10 for chronic low back pain, the effect size for NSAIDs is < 0.2029.
We find several implications for research. In terms of the methodology of subsequent acupuncture trials for chronic pain, we find that the balance of evidence is to give a higher dose of acupuncture in terms of a greater number of treatments in trials without sham control. Although the nature of the control group in trials will naturally be driven by the research question, investigators should be aware of the evidence that control arms that incorporate a relatively intense level of intervention, such as when acupuncture is added into an intensive rehabilitation regimen, tend to lead to smaller effect sizes, as do sham controls that involve needle penetration. Further research is warranted on whether acupuncture is particularly effective for upper body musculoskeletal pain. An associated hypothesis is whether there are subtypes of other chronic pain indications that have differential response to acupuncture. It would naturally be ideal to know before referring a patient for treatment whether, say, the type of back pain they are experiencing is one that would be amenable to treatment with acupuncture. We will also repeat our prior call for research on how best to incorporate acupuncture into the multidisciplinary care of chronic pain patients.
In terms of implications for clinical practice, we have confirmed that acupuncture has a clinically relevant, persistent effect on chronic pain that is not completely explained by placebo effects. Referral for a course of acupuncture treatment is therefore a reasonable option for a patient with chronic pain.
Supplementary Material
Highlights.
Acupuncture has a clinically relevant effect on chronic pain that persists over time
The effect of acupuncture cannot be explained only by placebo effects
Factors in addition to the specific effects of needling are important contributors
Referral for acupuncture treatment is a reasonable option for chronic pain patients
Perspective.
Acupuncture is effective for the treatment of chronic musculosketal, headache and osteoarthritis pain. Treatment effects of acupuncture persist over time and cannot be explained solely in terms of placebo effects. Referral for a course of acupuncture treatment is a reasonable option for a patient with chronic pain.
Acupuncture Trialists’ Collaboration Members
Claire Allen, BA, Evidence Aid, Oxford, United Kingdom.
Brian Berman, MD, University of Maryland School of Medicine and Center for Integrative Medicine, College Park, Maryland.
Benno Brinkhaus, MD, Institute for Social Medicine, Epidemiology and Health Economics, Charité University Medical Center, Berlin, Germany.
Remy Coeytaux, MD, PhD, Department of Community and Family Medicine, Duke University, Durham, North Carolina.
Hans-Christoph Diener, MD, PhD, Department of Neurology, University of Duisburg-Essen, Germany.
Heinz G. Endres, MD, Ruhr–University Bochum, Bochum, Germany.
Nadine E. Foster, DPhil, BSc(Hons), Arthritis Research UK Primary Care Centre, Research Institute of Primary Care and Health Sciences, Keele University, Newcastle-under-Lyme, Staffordshire, England.
Michael Haake, MD, PhD, Department of Orthopedics and Traumatology, SLK Hospitals, Heilbronn, Germany.
Rana S. Hinman, PhD, University of Melbourne, Melbourne, Australia.
Dominik Irnich, MD, Multidisciplinary Pain Centre, Department of Anesthesiology, Ludwig-Maximilians-Universität München (LMU Munich), Germany.
Wayne B. Jonas, MD, Samueli Institute, Alexandria, Virginia.
Kai Kronfeld, PhD, Interdisciplinary Centre for Clinical Trials (IZKS Mainz), University Medical Centre Mainz, Mainz, Germany.
Lixing Lao, PhD, University of Maryland and Center for Integrative Medicine, College Park, Maryland.
George Lewith, MD, FRCP, Primary Care and Population Sciences, Faculty of Medicine, University of Southampton, Southampton, England.
Klaus Linde, MD, Institute of General Practice, Technical University Munich, Munich, Germany.
Hugh MacPherson, PhD, Professor of Acupuncture Research, Department of Health Sciences, University of York, York, England.
Eric Manheimer, MS, Center for Integrative Medicine, University of Maryland School of Medicine, College Park, Maryland.
Dieter Melchart, MD, PhD, Competence Centre for Complementary Medicine and Naturopathy, Technical University Munich, Munich, Germany.
Albrecht Molsberger, MD, PhD, German Acupuncture Research Group, Duesseldorf, Germany.
Karen J. Sherman, PhD, MPH, Group Health Research Institute, Seattle, Washington.
Maria Suarez-Almazor, MD, PhD, MD Anderson Cancer Center, Houston, Texas.
Hans Trampisch, PhD, Department of Medical Statistics and Epidemiology, Ruhr–University Bochum, Germany.
Jorge Vas, MD, PhD, Pain Treatment Unit, Dos Hermanas Primary Care Health Center (Andalusia Public Health System), Dos Hermanas, Spain.
Andrew J. Vickers (collaboration chair), DPhil, Memorial Sloan Kettering Cancer Center, New York, New York Peter White, PhD, School of Health Sciences, University of Southampton, England.
Lyn Williamson, MD, MA (Oxon), MRCGP, FRCP, Great Western Hospital, Swindon, UK.
Stefan N. Willich, MD, MPH, MBA, Institute for Social Medicine, Epidemiology and Health Economics, Charité University Medical Center, Berlin, Germany.
Claudia M. Witt, MD, MBA, Institute for Complementary and Integrative Medicine, University of Zurich and University Hospital Zurich, Zurich, Switzerland; Institute for Social Medicine, Epidemiology and Health Economics, Charite-Universitätsmedizin, Berlin, Germany; Center for Integrative Medicine, University of Maryland School of Medicine, Baltimore, Maryland.
Footnotes
Authors’ contributions
The study was conceived by AV, GL, CW and KL. AV was responsible for the overall study design; EV for the systematic review; GL and HM with respect to acupuncture analyses; CW, NF, KS and KL with respect to clinical trial methodology and meta-analysis. Statistical analyses were conducted by EV. The first draft of the manuscript was written by AV and EV. All authors gave comments on early drafts and approved the final version of the manuscript. AV had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. GL died between completion of the first draft of the manuscript and submission to this journal.
Disclosures
An ethics statement was not required for this work. The authors declare that they have no competing interests. The Acupuncture Trialists’ Collaboration is funded by an R21 (AT004189I and an R01 (AT006794) from the National Center for Complementary and Alternative Medicine (NCCAM) at the National Institutes of Health (NIH) to Dr. Vickers) and by a grant from the Samueli Institute. Dr. MacPherson’s work on this project was funded in part by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research scheme (RP-PG-0707-10186). Prof. Foster, an NIHR Senior Investigator, was supported through an NIHR Research Professorship (RP-011-015). The views expressed in this publication are those of the author(s) and not necessarily those of the NCCAM, NHS, NIHR or the Department of Health in England. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Andrew J. Vickers, Memorial Sloan Kettering Cancer Center, New York, NY.
Emily A. Vertosick, Memorial Sloan Kettering Cancer Center, New York, NY.
George Lewith, University of Southampton, Southampton, UK.
Hugh MacPherson, University of York, York, UK.
Nadine E. Foster, Keele University, Newcastle-under-Lyme, UK.
Karen J. Sherman, Group Health Research Institute, Seattle, WA.
Dominik Irnich, Ludwig-Maximilians-Universität München (LMU Munich), Munich, Germany.
Claudia M. Witt, University of Zurich and University Hospital Zurich, Zurich, Switzerland; Charite-Universitätsmedizin, Berlin, Germany; University of Maryland School of Medicine, Baltimore, Maryland.
Klaus Linde, Technical University Munich, Germany.
References
- 1.Ahn CB, Lee SJ, Lee JC, Fossion JP, Sant’Ana A. A clinical pilot study comparing traditional acupuncture to combined acupuncture for treating headache, trigeminal neuralgia and retro-auricular pain in facial palsy. Journal of acupuncture and meridian studies. 2011;4:29–43. doi: 10.1016/S2005-2901(11)60005-8. [DOI] [PubMed] [Google Scholar]
- 2.Ahsin S, Saleem S, Bhatti AM, Iles RK, Aslam M. Clinical and endocrinological changes after electro-acupuncture treatment in patients with osteoarthritis of the knee. Pain. 2009;147:60–66. doi: 10.1016/j.pain.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Allais G, Romoli M, Rolando S, Airola G, Castagnoli Gabellari I, Allais R, Benedetto C. Ear acupuncture in the treatment of migraine attacks: a randomized trial on the efficacy of appropriate versus inappropriate acupoints. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2011;32(Suppl 1):S173–175. doi: 10.1007/s10072-011-0525-4. [DOI] [PubMed] [Google Scholar]
- 4.Allam H, Mohammed NH. The Role of Scalp Acupuncture for Relieving the Chronic Pain of Degenerative Osteoarthritis: A Pilot Study of Egyptian Women. Medical acupuncture. 2013;25:216–220. doi: 10.1089/acu.2012.0892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aranha MF, Muller CE, Gaviao MB. Pain intensity and cervical range of motion in women with myofascial pain treated with acupuncture and electroacupuncture: a double-blinded, randomized clinical trial. Brazilian journal of physical therapy. 2014;0:0. doi: 10.1590/bjpt-rbf.2014.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ashraf A, Zarei F, Hadianfard MJ, Kazemi B, Mohammadi S, Naseri M, Nasseri A, Khodadadi M, Sayadi M. Comparison the effect of lateral wedge insole and acupuncture in medial compartment knee osteoarthritis: a randomized controlled trial. The Knee. 2014;21:439–444. doi: 10.1016/j.knee.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Baeumler PI, Fleckenstein J, Takayama S, Simang M, Seki T, Irnich D. Effects of acupuncture on sensory perception: a systematic review and meta-analysis. PloS one. 2014;9:e113731. doi: 10.1371/journal.pone.0113731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AM, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004;141:901–910. doi: 10.7326/0003-4819-141-12-200412210-00006. [DOI] [PubMed] [Google Scholar]
- 9.Birch S. A review and analysis of placebo treatments, placebo effects, and placebo controls in trials of medical procedures when sham is not inert. J Altern Complement Med. 2006;12:303–310. doi: 10.1089/acm.2006.12.303. [DOI] [PubMed] [Google Scholar]
- 10.Bjordal JM, Ljunggren AE, Klovning A, Slordal L. Non-steroidal anti-inflammatory drugs, including cyclo-oxygenase-2 inhibitors, in osteoarthritic knee pain: meta-analysis of randomised placebo controlled trials. BMJ. 2004;329:1317. doi: 10.1136/bmj.38273.626655.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brinkhaus B, Witt CM, Jena S, Linde K, Streng A, Wagenpfeil S, Irnich D, Walther HU, Melchart D, Willich SN. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med. 2006;166:450–457. doi: 10.1001/archinte.166.4.450. [DOI] [PubMed] [Google Scholar]
- 12.Cameron ID, Wang E, Sindhusake D. A randomized trial comparing acupuncture and simulated acupuncture for subacute and chronic whiplash. Spine (Phila Pa 1976) 2011;36:E1659–1665. doi: 10.1097/BRS.0b013e31821bf674. [DOI] [PubMed] [Google Scholar]
- 13.Carlsson CP, Sjolund BH. Acupuncture for chronic low back pain: a randomized placebo-controlled study with long-term follow-up. Clin J Pain. 2001;17:296–305. doi: 10.1097/00002508-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Chassot M, Dussan-Sarria JA, Sehn FC, Deitos A, de Souza A, Vercelino R, Torres IL, Fregni F, Caumo W. Electroacupuncture analgesia is associated with increased serum brain-derived neurotrophic factor in chronic tension-type headache: a randomized, sham controlled, crossover trial. BMC complementary and alternative medicine. 2015;15:144. doi: 10.1186/s12906-015-0664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen CC, Yang CC, Hu CC, Shih HN, Chang YH, Hsieh PH. Acupuncture for pain relief after total knee arthroplasty: a randomized controlled trial. Regional anesthesia and pain medicine. 2015;40:31–36. doi: 10.1097/AAP.0000000000000138. [DOI] [PubMed] [Google Scholar]
- 16.Chen LX, Mao JJ, Fernandes S, Galantino ML, Guo W, Lariccia P, Teal VL, Bowman MA, Schumacher HR, Farrar JT. Integrating acupuncture with exercise-based physical therapy for knee osteoarthritis: a randomized controlled trial. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 2013;19:308–316. doi: 10.1097/RHU.0b013e3182a21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen X, Spaeth RB, Freeman SG, Scarborough DM, Hashmi JA, Wey HY, Egorova N, Vangel M, Mao J, Wasan AD, Edwards RR, Gollub RL, Kong J. The modulation effect of longitudinal acupuncture on resting state functional connectivity in knee osteoarthritis patients. Molecular pain. 2015;11:67. doi: 10.1186/s12990-015-0071-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cherkin DC, Eisenberg D, Sherman KJ, Barlow W, Kaptchuk TJ, Street J, Deyo RA. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med. 2001;161:1081–1088. doi: 10.1001/archinte.161.8.1081. [DOI] [PubMed] [Google Scholar]
- 19.Cherkin DC, Sherman KJ, Avins AL, Erro JH, Ichikawa L, Barlow WE, Delaney K, Hawkes R, Hamilton L, Pressman A, Khalsa PS, Deyo RA. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169:858–866. doi: 10.1001/archinternmed.2009.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho JH, Nam DH, Kim KT, Lee JH. Acupuncture with non-steroidal anti-inflammatory drugs (NSAIDs) versus acupuncture or NSAIDs alone for the treatment of chronic neck pain: an assessor-blinded randomised controlled pilot study. Acupunct Med. 2014;32:17–23. doi: 10.1136/acupmed-2013-010410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho YJ, Song YK, Cha YY, Shin BC, Shin IH, Park HJ, Lee HS, Kim KW, Cho JH, Chung WS, Lee JH, Song MY. Acupuncture for chronic low back pain: a multicenter, randomized, patient-assessor blind, sham-controlled clinical trial. Spine (Phila Pa 1976) 2013;38:549–557. doi: 10.1097/BRS.0b013e318275e601. [DOI] [PubMed] [Google Scholar]
- 22.Chou LW, Hsieh YL, Chen HS, Hong CZ, Kao MJ, Han TI. Remote therapeutic effectiveness of acupuncture in treating myofascial trigger point of the upper trapezius muscle. American journal of physical medicine & rehabilitation/Association of Academic Physiatrists. 2011;90:1036–1049. doi: 10.1097/PHM.0b013e3182328875. [DOI] [PubMed] [Google Scholar]
- 23.Coeytaux RR, Kaufman JS, Kaptchuk TJ, Chen W, Miller WC, Callahan LF, Mann JD. A randomized, controlled trial of acupuncture for chronic daily headache. Headache. 2005;45:1113–1123. doi: 10.1111/j.1526-4610.2005.00235.x. [DOI] [PubMed] [Google Scholar]
- 24.D’Alessandro E, de Brito C, Cecatto R, Saul M, Atta JA, Lin CA. Evaluation of acupuncture for cancer symptoms in a cancer institute in Brazil. Acupunct Med. 2013;31:23–26. doi: 10.1136/acupmed-2012-010206. [DOI] [PubMed] [Google Scholar]
- 25.De Kooning M, Tobbackx Y, Meeus M, Wauters L, Ickmans K, De Vilder P, Roose J, Verhaeghe T, Nijs J. Acupuncture-Analgesia Following a Single Treatment Session in Chronic Whiplash is Unrelated to Autonomic Nervous System Changes: A Randomized Cross-over Trial. Pain physician. 2015;18:527–536. [PubMed] [Google Scholar]
- 26.Diener HC, Kronfeld K, Boewing G, Lungenhausen M, Maier C, Molsberger A, Tegenthoff M, Trampisch HJ, Zenz M, Meinert R. Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomised controlled clinical trial. Lancet Neurol. 2006;5:310–316. doi: 10.1016/S1474-4422(06)70382-9. [DOI] [PubMed] [Google Scholar]
- 27.Egorova N, Gollub RL, Kong J. Repeated verum but not placebo acupuncture normalizes connectivity in brain regions dysregulated in chronic pain. NeuroImage Clinical. 2015;9:430–435. doi: 10.1016/j.nicl.2015.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Endres HG, Bowing G, Diener HC, Lange S, Maier C, Molsberger A, Zenz M, Vickers AJ, Tegenthoff M. Acupuncture for tension-type headache: a multicentre, sham-controlled, patient-and observer-blinded, randomised trial. J Headache Pain. 2007;8:306–314. doi: 10.1007/s10194-007-0416-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Enthoven WT, Roelofs PD, Deyo RA, van Tulder MW, Koes BW. Non-steroidal anti-inflammatory drugs for chronic low back pain. Cochrane Database Syst Rev. 2016;2:CD012087. doi: 10.1002/14651858.CD012087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Facco E, Liguori A, Petti F, Fauci AJ, Cavallin F, Zanette G. Acupuncture versus valproic acid in the prophylaxis of migraine without aura: a prospective controlled study. Minerva anestesiologica. 2013;79:634–642. [PubMed] [Google Scholar]
- 31.Ferro EC, Biagini AP, da Silva IE, Silva ML, Silva JR. The combined effect of acupuncture and Tanacetum parthenium on quality of life in women with headache: randomised study. Acupunct Med. 2012;30:252–257. doi: 10.1136/acupmed-2012-010195. [DOI] [PubMed] [Google Scholar]
- 32.Foroughipour M, Golchian AR, Kalhor M, Akhlaghi S, Farzadfard MT, Azizi H. A sham-controlled trial of acupuncture as an adjunct in migraine prophylaxis. Acupunct Med. 2014;32:12–16. doi: 10.1136/acupmed-2013-010362. [DOI] [PubMed] [Google Scholar]
- 33.Foster NE, Thomas E, Barlas P, Hill JC, Young J, Mason E, Hay EM. Acupuncture as an adjunct to exercise based physiotherapy for osteoarthritis of the knee: randomised controlled trial. Bmj. 2007;335:436. doi: 10.1136/bmj.39280.509803.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grotle M. Traditional Chinese acupuncture was not superior to sham acupuncture for knee osteoarthritis but delivering treatment with high expectations of improvement was superior to delivering treatment with neutral expectations. Journal of physiotherapy. 2011;57:56. doi: 10.1016/S1836-9553(11)70009-1. [DOI] [PubMed] [Google Scholar]
- 35.Guerra de Hoyos JA, del Andres Martin MC, Bassas y Baena de Leon E, Vigara Lopez M, Molina Lopez T, Verdugo Morilla FA, Gonzalez Moreno MJ. Randomised trial of long term effect of acupuncture for shoulder pain. Pain. 2004;112:289–298. doi: 10.1016/j.pain.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 36.Haake M, Muller HH, Schade-Brittinger C, Basler HD, Schafer H, Maier C, Endres HG, Trampisch HJ, Molsberger A. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167:1892–1898. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- 37.Hansson Y, Carlsson C, Olsson E. Intramuscular and periosteal acupuncture in patients suffering from chronic musculoskeletal pain - a controlled trial. Acupunct Med. 2008;26:214–223. doi: 10.1136/aim.26.4.214. [DOI] [PubMed] [Google Scholar]
- 38.Hasegawa TM, Baptista AS, de Souza MC, Yoshizumi AM, Natour J. Acupuncture for acute non-specific low back pain: a randomised, controlled, double-blind, placebo trial. Acupunct Med. 2014;32:109–115. doi: 10.1136/acupmed-2013-010333. [DOI] [PubMed] [Google Scholar]
- 39.Hinman RS, McCrory P, Pirotta M, Relf I, Forbes A, Crossley KM, Williamson E, Kyriakides M, Novy K, Metcalf BR, Harris A, Reddy P, Conaghan PG, Bennell KL. Acupuncture for chronic knee pain: a randomized clinical trial. Jama. 2014;312:1313–1322. doi: 10.1001/jama.2014.12660. [DOI] [PubMed] [Google Scholar]
- 40.Hunter RF, McDonough SM, Bradbury I, Liddle SD, Walsh DM, Dhamija S, Glasgow P, Gormley G, McCann SM, Park J, Hurley DA, Delitto A, Baxter GD. Exercise and Auricular Acupuncture for Chronic Low-back Pain: A Feasibility Randomized-controlled Trial. Clin J Pain. 2012;28:259–267. doi: 10.1097/AJP.0b013e3182274018. [DOI] [PubMed] [Google Scholar]
- 41.Irnich D, Behrens N, Molzen H, Konig A, Gleditsch J, Krauss M, Natalis M, Senn E, Beyer A, Schops P. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. Bmj. 2001;322:1574–1578. doi: 10.1136/bmj.322.7302.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Itoh K, Saito S, Sahara S, Naitoh Y, Imai K, Kitakoji H. Randomized trial of trigger point acupuncture treatment for chronic shoulder pain: a preliminary study. Journal of acupuncture and meridian studies. 2014;7:59–64. doi: 10.1016/j.jams.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 43.Jena S, Witt CM, Brinkhaus B, Wegscheider K, Willich SN. Acupuncture in patients with headache. Cephalalgia. 2008;28:969–979. doi: 10.1111/j.1468-2982.2008.01640.x. [DOI] [PubMed] [Google Scholar]
- 44.Ji L, Wang H, Cao Y, Yan P, Jin X, Nie P, Wang C, Li R, Zhang C, Yang M, Yang J. Sharp-Hook Acupuncture (Feng Gou Zhen) for Patients with Periarthritis of Shoulder: A Randomized Controlled Trial. Evid Based Complement Alternat Med. 2015;2015:312309. doi: 10.1155/2015/312309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Johansson K, Bergstrom A, Schroder K, Foldevi M. Subacromial corticosteroid injection or acupuncture with home exercises when treating patients with subacromial impingement in primary care--a randomized clinical trial. Family practice. 2011;28:355–365. doi: 10.1093/fampra/cmq119. [DOI] [PubMed] [Google Scholar]
- 46.Kaptchuk TJ, Stason WB, Davis RB, Legedza AR, Schnyer RN, Kerr CE, Stone DA, Nam BH, Kirsch I, Goldman RH. Sham device v inert pill: randomised controlled trial of two placebo treatments. BMJ. 2006;332:391–397. doi: 10.1136/bmj.38726.603310.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Karner M, Brazkiewicz F, Remppis A, Fischer J, Gerlach O, Stremmel W, Subramanian SV, Greten HJ. Objectifying specific and nonspecific effects of acupuncture: a double-blinded randomised trial in osteoarthritis of the knee. Evid Based Complement Alternat Med. 2013;2013:427265. doi: 10.1155/2013/427265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kennedy S, Baxter GD, Kerr DP, Bradbury I, Park J, McDonough SM. Acupuncture for acute non-specific low back pain: a pilot randomised non-penetrating sham controlled trial. Complement Ther Med. 2008;16:139–146. doi: 10.1016/j.ctim.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 49.Kerr DP, Walsh DM, Baxter D. Acupuncture in the management of chronic low back pain: a blinded randomized controlled trial. Clin J Pain. 2003;19:364–370. doi: 10.1097/00002508-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 50.Kim EJ, Lim CY, Lee EY, Lee SD, Kim KS. Comparing the effects of individualized, standard, sham and no acupuncture in the treatment of knee osteoarthritis: a multicenter randomized controlled trial. Trials. 2013;14:129. doi: 10.1186/1745-6215-14-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim JI, Kim TH, Lee MS, Kang JW, Kim KH, Choi JY, Kang KW, Kim AR, Shin MS, Jung SY, Choi SM. Evaluation of wet-cupping therapy for persistent non-specific low back pain: a randomised, waiting-list controlled, open-label, parallel-group pilot trial. Trials. 2011;12:146. doi: 10.1186/1745-6215-12-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kleinhenz J, Streitberger K, Windeler J, Gussbacher A, Mavridis G, Martin E. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain. 1999;83:235–241. doi: 10.1016/s0304-3959(99)00107-4. [DOI] [PubMed] [Google Scholar]
- 53.Koh PS, Seo BK, Cho NS, Park HS, Park DS, Baek YH. Clinical effectiveness of bee venom acupuncture and physiotherapy in the treatment of adhesive capsulitis: a randomized controlled trial. Journal of shoulder and elbow surgery/American Shoulder and Elbow Surgeons … [et al.] 2013;22:1053–1062. doi: 10.1016/j.jse.2012.10.045. [DOI] [PubMed] [Google Scholar]
- 54.Kong J, Spaeth R, Cook A, Kirsch I, Claggett B, Vangel M, Gollub RL, Smoller JW, Kaptchuk TJ. Are all placebo effects equal? Placebo pills, sham acupuncture, cue conditioning and their association. PloS one. 2013;8:e67485. doi: 10.1371/journal.pone.0067485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lan L, Gao Y, Zeng F, Qin W, Dong M, Liu M, Guo T, Liang F. A central analgesic mechanism of acupuncture for migraine: An ongoing functional MRI study. Neural regeneration research. 2013;8:2649–2655. doi: 10.3969/j.issn.1673-5374.2013.28.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lansdown H, Howard K, Brealey S, MacPherson H. Acupuncture for pain and osteoarthritis of the knee: a pilot study for an open parallel-arm randomised controlled trial. BMC Musculoskelet Disord. 2009;10:130. doi: 10.1186/1471-2474-10-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lathia AT, Jung SM, Chen LX. Efficacy of acupuncture as a treatment for chronic shoulder pain. J Altern Complement Med. 2009;15:613–618. doi: 10.1089/acm.2008.0272. [DOI] [PubMed] [Google Scholar]
- 58.Li N, Tian F, Wang C, Yu P, Zhou X, Wen Q, Qiao X, Huang L. Therapeutic effect of acupuncture and massage for shoulder-hand syndrome in hemiplegia patients: a clinical two-center randomized controlled trial. Journal of traditional Chinese medicine = Chung i tsa chih ying wen pan/sponsored by All-China Association of Traditional Chinese Medicine, Academy of Traditional Chinese Medicine. 2012;32:343–349. doi: 10.1016/s0254-6272(13)60035-7. [DOI] [PubMed] [Google Scholar]
- 59.Li Y, Zheng H, Witt CM, Roll S, Yu SG, Yan J, Sun GJ, Zhao L, Huang WJ, Chang XR, Zhang HX, Wang DJ, Lan L, Zou R, Liang FR. Acupuncture for migraine prophylaxis: a randomized controlled trial. Cmaj. 2012;184:401–410. doi: 10.1503/cmaj.110551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liang Z, Zhu X, Yang X, Fu W, Lu A. Assessment of a traditional acupuncture therapy for chronic neck pain: a pilot randomised controlled study. Complement Ther Med. 2011;19(Suppl 1):S26–32. doi: 10.1016/j.ctim.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 61.Lin ML, Lin MH, Fen JJ, Lin WT, Lin CW, Chen PQ. A comparison between pulsed radiofrequency and electro-acupuncture for relieving pain in patients with chronic low back pain. Acupuncture & electro-therapeutics research. 2010;35:133–146. doi: 10.3727/036012910803860940. [DOI] [PubMed] [Google Scholar]
- 62.Lin ML, Wu HC, Hsieh YH, Su CT, Shih YS, Lin CW, Wu JH. Evaluation of the effect of laser acupuncture and cupping with ryodoraku and visual analog scale on low back pain. Evid Based Complement Alternat Med. 2012;2012:521612. doi: 10.1155/2012/521612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Linde K, Streng A, Jurgens S, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes MG, Weidenhammer W, Willich SN, Melchart D. Acupuncture for patients with migraine: a randomized controlled trial. Jama. 2005;293:2118–2125. doi: 10.1001/jama.293.17.2118. [DOI] [PubMed] [Google Scholar]
- 64.Ma C, Wu S, Li G, Xiao X, Mai M, Yan T. Comparison of miniscalpel-needle release, acupuncture needling, and stretching exercise to trigger point in myofascial pain syndrome. Clin J Pain. 2010;26:251–257. doi: 10.1097/AJP.0b013e3181b8cdc8. [DOI] [PubMed] [Google Scholar]
- 65.MacPherson H, Maschino AC, Lewith G, Foster NE, Witt CM, Vickers AJ. Characteristics of acupuncture treatment associated with outcome: an individual patient meta-analysis of 17,922 patients with chronic pain in randomised controlled trials. PloS one. 2013;8:e77438. doi: 10.1371/journal.pone.0077438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Macpherson H, Scullion A, Thomas KJ, Walters S. Patient reports of adverse events associated with acupuncture treatment: a prospective national survey. Quality & safety in health care. 2004;13:349–355. doi: 10.1136/qshc.2003.009134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.MacPherson H, Tilbrook H, Richmond S, Woodman J, Ballard K, Atkin K, Bland M, Eldred J, Essex H, Hewitt C, Hopton A, Keding A, Lansdown H, Parrott S, Torgerson D, Wenham A, Watt I. Alexander Technique Lessons or Acupuncture Sessions for Persons With Chronic Neck Pain: A Randomized Trial. Ann Intern Med. 2015;163:653–662. doi: 10.7326/M15-0667. [DOI] [PubMed] [Google Scholar]
- 68.MacPherson H, Vertosick E, Lewith G, Linde K, Sherman KJ, Witt CM, Vickers AJ. Influence of control group on effect size in trials of acupuncture for chronic pain: a secondary analysis of an individual patient data meta-analysis. PloS one. 2014;9:e93739. doi: 10.1371/journal.pone.0093739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.MacPherson H, Vertosick EA, Foster NE, Lewith G, Linde K, Sherman KJ, Witt CM, Vickers AJ Acupuncture Trialists C. The persistence of the effects of acupuncture after a course of treatment: A meta-analysis of patients with chronic pain. Pain. 2016 doi: 10.1097/j.pain.0000000000000747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mavrommatis CI, Argyra E, Vadalouka A, Vasilakos DG. Acupuncture as an adjunctive therapy to pharmacological treatment in patients with chronic pain due to osteoarthritis of the knee: a 3-armed, randomized, placebo-controlled trial. Pain. 2012;153:1720–1726. doi: 10.1016/j.pain.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 71.Melchart D, Streng A, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes M, Hummelsberger J, Irnich D, Weidenhammer W, Willich SN, Linde K. Acupuncture in patients with tension-type headache: randomised controlled trial. Bmj. 2005;331:376–382. doi: 10.1136/bmj.38512.405440.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Miller E, Maimon Y, Rosenblatt Y, Mendler A, Hasner A, Barad A, Amir H, Dekel S, Lev-Ari S. Delayed Effect of Acupuncture Treatment in OA of the Knee: A Blinded, Randomized, Controlled Trial. Evid Based Complement Alternat Med. 2011;2011:792975. doi: 10.1093/ecam/nen080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Miyazaki S, Hagihara A, Kanda R, Mukaino Y, Nobutomo K. Applicability of press needles to a double-blind trial: a randomized, double-blind, placebo-controlled trial. Clin J Pain. 2009;25:438–444. doi: 10.1097/AJP.0b013e318193a6e1. [DOI] [PubMed] [Google Scholar]
- 74.Molsberger AF, Mau J, Pawelec DB, Winkler J. Does acupuncture improve the orthopedic management of chronic low back pain--a randomized, blinded, controlled trial with 3 months follow up. Pain. 2002;99:579–587. doi: 10.1016/S0304-3959(02)00269-5. [DOI] [PubMed] [Google Scholar]
- 75.Molsberger AF, Schneider T, Gotthardt H, Drabik A. German Randomized Acupuncture Trial for chronic shoulder pain (GRASP) - a pragmatic, controlled, patient-blinded, multi-centre trial in an outpatient care environment. Pain. 2010;151:146–154. doi: 10.1016/j.pain.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 76.Peets JM, Pomeranz B. CXBK mice deficient in opiate receptors show poor electroacupuncture analgesia. Nature. 1978;273:675–676. doi: 10.1038/273675a0. [DOI] [PubMed] [Google Scholar]
- 77.Sahin N, Ozcan E, Sezen K, Karatas O, Issever H. Efficacy of acupunture in patients with chronic neck pain--a randomised, sham controlled trial. Acupuncture & electro-therapeutics research. 2010;35:17–27. doi: 10.3727/036012910803860959. [DOI] [PubMed] [Google Scholar]
- 78.Saleki M, Ahadi T, Razi M, Raeisi GR, Forough B, Ali MK. Comparison of the effects of acupuncture and isometric exercises on symptom of knee osteoarthritis. International journal of preventive medicine. 2013;4:S73–77. [PMC free article] [PubMed] [Google Scholar]
- 79.Salter GC, Roman M, Bland MJ, MacPherson H. Acupuncture for chronic neck pain: a pilot for a randomised controlled trial. BMC Musculoskelet Disord. 2006;7:99. doi: 10.1186/1471-2474-7-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Scharf HP, Mansmann U, Streitberger K, Witte S, Kramer J, Maier C, Trampisch HJ, Victor N. Acupuncture and knee osteoarthritis: a three-armed randomized trial. Ann Intern Med. 2006;145:12–20. doi: 10.7326/0003-4819-145-1-200607040-00005. [DOI] [PubMed] [Google Scholar]
- 81.Shankar N, Thakur M, Tandon OP, Saxena AK, Arora S, Bhattacharya N. Autonomic status and pain profile in patients of chronic low back pain and following electro acupuncture therapy: a randomized control trial. Indian journal of physiology and pharmacology. 2011;55:25–36. [PubMed] [Google Scholar]
- 82.Silva AC, Biasotto-Gonzalez DA, Dos Santos DM, Melo NC, Gomes CA, Amorim CF, Politti F. Evaluation of the Immediate Effect of Auricular Acupuncture on Pain and Electromyographic Activity of the Upper Trapezius Muscle in Patients with Nonspecific Neck Pain: A Randomized, Single-Blinded, Sham-Controlled, Crossover Study. Evid Based Complement Alternat Med. 2015;2015:523851. doi: 10.1155/2015/523851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Soderberg EI, Carlsson JY, Stener-Victorin E, Dahlof C. Subjective well-being in patients with chronic tension-type headache: effect of acupuncture, physical training, and relaxation training. Clin J Pain. 2011;27:448–456. doi: 10.1097/AJP.0b013e318208c8fe. [DOI] [PubMed] [Google Scholar]
- 84.Spaeth RB, Camhi S, Hashmi JA, Vangel M, Wasan AD, Edwards RR, Gollub RL, Kong J. A longitudinal study of the reliability of acupuncture deqi sensations in knee osteoarthritis. Evid Based Complement Alternat Med. 2013;2013:204259. doi: 10.1155/2013/204259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Suarez-Almazor ME, Looney C, Liu Y, Cox V, Pietz K, Marcus DM, Street RL., Jr A randomized controlled trial of acupuncture for osteoarthritis of the knee: effects of patient-provider communication. Arthritis Care Res (Hoboken) 2010;62:1229–1236. doi: 10.1002/acr.20225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sun MY, Hsieh CL, Cheng YY, Hung HC, Li TC, Yen SM, Huang IS. The therapeutic effects of acupuncture on patients with chronic neck myofascial pain syndrome: a single-blind randomized controlled trial. Am J Chin Med. 2010;38:849–859. doi: 10.1142/S0192415X10008299. [DOI] [PubMed] [Google Scholar]
- 87.Thomas KJ, MacPherson H, Thorpe L, Brazier J, Fitter M, Campbell MJ, Roman M, Walters SJ, Nicholl J. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. Bmj. 2006;333:623. doi: 10.1136/bmj.38878.907361.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vas J, Aranda JM, Modesto M, Benitez-Parejo N, Herrera A, Martinez-Barquin DM, Aguilar I, Sanchez-Araujo M, Rivas-Ruiz F. Acupuncture in patients with acute low back pain: a multicentre randomised controlled clinical trial. Pain. 2012;153:1883–1889. doi: 10.1016/j.pain.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 89.Vas J, Mendez C, Perea-Milla E, Vega E, Panadero MD, Leon JM, Borge MA, Gaspar O, Sanchez-Rodriguez F, Aguilar I, Jurado R. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. Bmj. 2004;329:1216. doi: 10.1136/bmj.38238.601447.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Vas J, Ortega C, Olmo V, Perez-Fernandez F, Hernandez L, Medina I, Seminario JM, Herrera A, Luna F, Perea-Milla E, Mendez C, Madrazo F, Jimenez C, Ruiz MA, Aguilar I. Single-point acupuncture and physiotherapy for the treatment of painful shoulder: a multicentre randomized controlled trial. Rheumatology (Oxford) 2008;47:887–893. doi: 10.1093/rheumatology/ken040. [DOI] [PubMed] [Google Scholar]
- 91.Vas J, Perea-Milla E, Mendez C, Sanchez Navarro C, Leon Rubio JM, Brioso M, Garcia Obrero I. Efficacy and safety of acupuncture for chronic uncomplicated neck pain: a randomised controlled study. Pain. 2006;126:245–255. doi: 10.1016/j.pain.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 92.Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, Foster NE, Sherman KJ, Witt CM, Linde K. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444–1453. doi: 10.1001/archinternmed.2012.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vickers AJ, Cronin AM, Maschino AC, Lewith G, Macpherson H, Victor N, Sherman KJ, Witt C, Linde K. Individual patient data meta-analysis of acupuncture for chronic pain: protocol of the Acupuncture Trialists’ Collaboration. Trials. 2010;11:90. doi: 10.1186/1745-6215-11-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vickers AJ, Maschino AC, Lewith G, MacPherson H, Sherman KJ, Witt CM Acupuncture Trialists C. Responses to the Acupuncture Trialists’ Collaboration individual patient data meta-analysis. Acupunct Med. 2013;31:98–100. doi: 10.1136/acupmed-2013-010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, Fisher P, Van Haselen R. Acupuncture for chronic headache in primary care: large, pragmatic, randomised trial. Bmj. 2004;328:744. doi: 10.1136/bmj.38029.421863.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wallasch TM, Weinschuetz T, Mueller B, Kropp P. Cerebrovascular response in migraineurs during prophylactic treatment with acupuncture: a randomized controlled trial. J Altern Complement Med. 2012;18:777–783. doi: 10.1089/acm.2011.0308. [DOI] [PubMed] [Google Scholar]
- 97.Wand BM, Abbaszadeh S, Smith AJ, Catley MJ, Moseley GL. Acupuncture applied as a sensory discrimination training tool decreases movement-related pain in patients with chronic low back pain more than acupuncture alone: a randomised cross-over experiment. British journal of sports medicine. 2013;47:1085–1089. doi: 10.1136/bjsports-2013-092949. [DOI] [PubMed] [Google Scholar]
- 98.Wang LP, Zhang XZ, Guo J, Liu HL, Zhang Y, Liu CZ, Yi JH, Wang LP, Zhao JP, Li SS. Efficacy of acupuncture for migraine prophylaxis: a single-blinded, double-dummy, randomized controlled trial. Pain. 2011;152:1864–1871. doi: 10.1016/j.pain.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 99.Wang LP, Zhang XZ, Guo J, Liu HL, Zhang Y, Liu CZ, Yi JH, Wang LP, Zhao JP, Li SS. Efficacy of acupuncture for acute migraine attack: a multicenter single blinded, randomized controlled trial. Pain medicine (Malden, Mass) 2012;13:623–630. doi: 10.1111/j.1526-4637.2012.01376.x. [DOI] [PubMed] [Google Scholar]
- 100.Wang Y, Xue CC. Acupuncture for Frequent Migraine: A Randomized, Patient/Assessor Blinded, Controlled Trial with One-Year Follow-Up. 2015;2015:920353. doi: 10.1155/2015/920353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Weiner DK, Moore CG, Morone NE, Lee ES, Kent Kwoh C. Efficacy of periosteal stimulation for chronic pain associated with advanced knee osteoarthritis: a randomized, controlled clinical trial. Clin Ther. 2013;35:1703–1720.e1705. doi: 10.1016/j.clinthera.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 102.Weiss J, Quante S, Xue F, Muche R, Reuss-Borst M. Effectiveness and acceptance of acupuncture in patients with chronic low back pain: results of a prospective, randomized, controlled trial. J Altern Complement Med. 2013;19:935–941. doi: 10.1089/acm.2012.0338. [DOI] [PubMed] [Google Scholar]
- 103.White P, Bishop FL, Prescott P, Scott C, Little P, Lewith G. Practice, practitioner, or placebo? A multifactorial, mixed-methods randomized controlled trial of acupuncture. Pain. 2012;153:455–462. doi: 10.1016/j.pain.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 104.White P, Lewith G, Prescott P, Conway J. Acupuncture versus placebo for the treatment of chronic mechanical neck pain: a randomized, controlled trial. Ann Intern Med. 2004;141:911–919. doi: 10.7326/0003-4819-141-12-200412210-00007. [DOI] [PubMed] [Google Scholar]
- 105.Whitehurst DG, Bryan S, Hay EM, Thomas E, Young J, Foster NE. Cost-effectiveness of acupuncture care as an adjunct to exercise-based physical therapy for osteoarthritis of the knee. Physical therapy. 2011;91:630–641. doi: 10.2522/ptj.20100239. [DOI] [PubMed] [Google Scholar]
- 106.Wilke J, Vogt L, Niederer D, Hubscher M, Rothmayr J, Ivkovic D, Rickert M, Banzer W. Short-term effects of acupuncture and stretching on myofascial trigger point pain of the neck: a blinded, placebo-controlled RCT. Complement Ther Med. 2014;22:835–841. doi: 10.1016/j.ctim.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 107.Williamson L, Wyatt MR, Yein K, Melton JT. Severe knee osteoarthritis: a randomized controlled trial of acupuncture, physiotherapy (supervised exercise) and standard management for patients awaiting knee replacement. Rheumatology (Oxford) 2007;46:1445–1449. doi: 10.1093/rheumatology/kem119. [DOI] [PubMed] [Google Scholar]
- 108.Witt C, Brinkhaus B, Jena S, Linde K, Streng A, Wagenpfeil S, Hummelsberger J, Walther HU, Melchart D, Willich SN. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005;366:136–143. doi: 10.1016/S0140-6736(05)66871-7. [DOI] [PubMed] [Google Scholar]
- 109.Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture for patients with chronic neck pain. Pain. 2006 doi: 10.1016/j.pain.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 110.Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture in patients with osteoarthritis of the knee or hip: a randomized, controlled trial with an additional nonrandomized arm. Arthritis Rheum. 2006;54:3485–3493. doi: 10.1002/art.22154. [DOI] [PubMed] [Google Scholar]
- 111.Witt CM, Jena S, Selim D, Brinkhaus B, Reinhold T, Wruck K, Liecker B, Linde K, Wegscheider K, Willich SN. Pragmatic Randomized Trial Evaluating the Clinical and Economic Effectiveness of Acupuncture for Chronic Low Back Pain. Am J Epidemiol. 2006;164:487–496. doi: 10.1093/aje/kwj224. [DOI] [PubMed] [Google Scholar]
- 112.Witt CM, Schutzler L, Ludtke R, Wegscheider K, Willich SN. Patient characteristics and variation in treatment outcomes: which patients benefit most from acupuncture for chronic pain? Clin J Pain. 2011;27:550–555. doi: 10.1097/AJP.0b013e31820dfbf5. [DOI] [PubMed] [Google Scholar]
- 113.Yang CP, Chang MH, Li TC, Hsieh CL, Hwang KL, Chang HH. Predicting prognostic factors in a randomized controlled trial of acupuncture versus topiramate treatment in patients with chronic migraine. Clin J Pain. 2013;29:982–987. doi: 10.1097/AJP.0b013e31827eb511. [DOI] [PubMed] [Google Scholar]
- 114.Yang CP, Chang MH, Liu PE, Li TC, Hsieh CL, Hwang KL, Chang HH. Acupuncture versus topiramate in chronic migraine prophylaxis: a randomized clinical trial. Cephalalgia. 2011;31:1510–1521. doi: 10.1177/0333102411420585. [DOI] [PubMed] [Google Scholar]
- 115.Yang J, Zeng F, Feng Y, Fang L, Qin W, Liu X, Song W, Xie H, Chen J, Liang F. A PET-CT study on the specificity of acupoints through acupuncture treatment in migraine patients. BMC complementary and alternative medicine. 2012;12:123. doi: 10.1186/1472-6882-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yang M, Yang J, Zeng F, Liu P, Lai Z, Deng S, Fang L, Song W, Xie H, Liang F. Electroacupuncture stimulation at sub-specific acupoint and non-acupoint induced distinct brain glucose metabolism change in migraineurs: a PET-CT study. Journal of translational medicine. 2014;12:351. doi: 10.1186/s12967-014-0351-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yun M, Shao Y, Zhang Y, He S, Xiong N, Zhang J, Guo M, Liu D, Luo Y, Guo L, Yan J. Hegu acupuncture for chronic low-back pain: a randomized controlled trial. J Altern Complement Med. 2012;18:130–136. doi: 10.1089/acm.2010.0779. [DOI] [PubMed] [Google Scholar]
- 118.Zhang SP, Chiu TT, Chiu SN. Long-term efficacy of electroacupuncture for chronic neck pain: a randomised controlled trial. Hong Kong medical journal = Xianggang yi xue za zhi/Hong Kong Academy of Medicine. 2013;19(Suppl 9):36–39. [PubMed] [Google Scholar]
- 119.Zhang WT, Jin Z, Cui GH, Zhang KL, Zhang L, Zeng YW, Luo F, Chen AC, Han JS. Relations between brain network activation and analgesic effect induced by low vs. high frequency electrical acupoint stimulation in different subjects: a functional magnetic resonance imaging study. Brain Res. 2003;982:168–178. doi: 10.1016/s0006-8993(03)02983-4. [DOI] [PubMed] [Google Scholar]
- 120.Zhao H, Nie W, Sun Y, Li S, Yang S, Meng F, Zhang L, Wang F, Huang S. Warm Needling Therapy and Acupuncture at Meridian-Sinew Sites Based on the Meridian-Sinew Theory: Hemiplegic Shoulder Pain. Evid Based Complement Alternat Med. 2015;2015:694973. doi: 10.1155/2015/694973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhao L, Liu J, Zhang F, Dong X, Peng Y, Qin W, Wu F, Li Y, Yuan K, von Deneen KM, Gong Q, Tang Z, Liang F. Effects of long-term acupuncture treatment on resting-state brain activity in migraine patients: a randomized controlled trial on active acupoints and inactive acupoints. PloS one. 2014;9:e99538. doi: 10.1371/journal.pone.0099538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.