Abstract
Post-Traumatic Stress Disorder (PTSD) commonly accompanies complex chronic pain, yet PTSD is often overlooked in chronic pain management. Using the 4-item Primary Care (PC)-PTSD screening tool, we evaluated the relationship between the number and type of PC-PTSD symptoms endorsed and a set of patient-reported outcomes, including: pain intensity and interference; function; mood; quality of life; and substance abuse risk in a consecutive sample of patients with chronic pain (n=4,402). Patients completed PainTracker™, a web-based patient-reported outcome tool that provides a multidimensional evaluation of chronic pain, as part of their intake evaluation at a specialty pain clinic in a community setting. Twenty-seven percent of the sample met PC-PTSD screening criteria for PTSD by endorsing three of the four symptom domains. Significant ordinal trends were observed between increasing number of PTSD symptoms and all outcomes evaluated. The occurrence of even one PTSD symptom was associated with overall poorer outcomes, suggesting that subsyndromal PTSD is clinically significant in the context of chronic pain. Among the four PTSD domains assessed, “numbness/detachment” was most strongly associated with negative pain outcomes by relative weight analysis. Results from this cross-sectional study suggest that a range of pain-related outcomes may be significantly related to co-morbid PTSD.
Perspective
We present evidence that PTSD symptoms are significantly related to a broad set of pain-related patient-reported outcomes. These findings highlight the need to evaluate for PTSD symptoms in patients with chronic pain, especially feelings of numbness or detachment from others, in order to improve understanding and management of chronic pain.
Keywords: post-traumatic stress disorder, PTSD symptoms, chronic pain, patient-reported outcomes
Introduction
Post-traumatic stress disorder (PTSD) commonly accompanies chronic pain. Population-based data from the National Comorbidity Survey suggest that prevalence of PTSD in patients with chronic pain is nearly four times that of the general population, controlling for sociodemographic characteristics.29 Estimates of PTSD in individuals with chronic pain range from 10% to 50%,3 depending on sample characteristics and the type of trauma experienced. Individuals with chronic pain and concurrent PTSD report increased pain intensity, more physical co-morbidities,32 and greater pain-related disability2 than those without PTSD.
The vast majority of research on the topic of PTSD and chronic pain has focused on a comparison of individuals with and without the full PTSD syndrome. However, PTSD is a multidimensional disorder37 that may not be fully captured by a binary “PTSD”/“No PTSD” classification. In addition to exposure to a traumatic event, DSM-V criteria for PTSD require that patients endorse multiple symptom domains (i.e., re-experiencing, avoidance, negative thoughts or feelings, arousal) that significantly interfere with daily functioning for more than one month. The observation that many symptomatic individuals do not fulfill all of these criteria stimulated the concept of partial or subsyndromal PTSD.39
Subsyndromal PTSD has been associated with a number of clinically meaningful outcomes, including: increased rates of lifetime mood disorders, substance use disorders, and attempted suicide;33,34 increased likelihood of physical diagnoses, including musculoskeletal disorders;17, 32 impaired social and occupational functional status;44, 50 and increased pain and pain interference among female veterans.4 In general, these studies found that individuals with subsyndromal PTSD had intermediate frequency or severity of most outcomes assessed compared to individuals with and without PTSD. It is therefore likely that subsyndromal PTSD may be similarly associated with negative outcomes in patients with chronic pain.
In addition to the number of PTSD symptoms, the type of PTSD symptoms may be important in patients with chronic pain. Multiple relationships among specific PTSD symptom domains and pain outcomes have been identified in previous studies. Hyperarousal has been associated with pain intensity, disability, and pain acceptance among chronic pain outpatients.10, 46 Emotional numbing and avoidance were associated with pain-related disability in homogenous samples of patients with chronic pain.11, 23, 28 Finally, avoidance predicted pain-related disability, and re-experiencing predicted pain-related distress in women with orofacial pain.13 These studies differed with respect to sample characteristics (i.e., sample size, pain diagnoses, etc.) and analytic methods used, precluding any real consensus regarding the relative importance of distinct PTSD symptom domains in chronic pain. The relationship between dimensions of trauma-related mental disorder (PTSD) and chronic pain outcomes therefore remains unclear. Thorough and systematic examination of the relationship between PTSD symptom domains and multi-dimensional chronic pain outcomes is needed to clarify the possible role of psychological trauma-focused therapies in chronic pain care.
The objectives of the current study were two-fold: (1) to evaluate the relationship between incremental increases in the number of PTSD symptom domains endorsed, spanning “subsyndromal“ (one and two symptoms) and “syndromal” (three and four symptoms), using the Primary Care-PTSD (PC-PTSD) screen for four prototypical PTSD symptom domains (intrusion, avoidance, hyperarousal, numbness/detachment) and (2) to determine the relative importance of specific PTSD symptom domains in terms of their relationship with pain-related outcomes in a large sample of treatment-seeking patients with chronic pain. A better understanding of the complex relationship between the symptoms of PTSD and the multi-dimensional experience of chronic pain is necessary in order to deliver and optimize comprehensive pain care for patients suffering from chronic pain.
Methods
Patients and Setting
Study participants (N=4,402) were consecutive, predominantly civilian, patients seeking care for various chronic pain conditions at the University of Washington Center for Pain Relief (UW CPR) between June of 2014 and October of 2017, who completed an initial PainTracker™ assessment. PainTracker™ is a web-based patient-reported outcome (PRO) measurement tool that was developed to facilitate comprehensive, multi-dimensional pain assessment and management to improve outcomes for patients with chronic pain, described below.40
Instruments
Basic demographic data was extracted from patients’ electronic medical records and merged with PainTracker™ data. The following measures were included in the PainTracker™ assessment.
PTSD Symptoms
The Primary Care-PTSD Screen (PC-PTSD)35 was used to evaluate the occurrence of PTSD symptoms. The PC-PTSD is a brief 4-item instrument developed by the Veteran’s Administration (VA) to screen for PTSD in primary care settings. It asks: “In your life, have you ever had any experience that was so frightening, horrible, or upsetting that, in the past month you…” This statement is followed by four items that broadly correspond to DSM-V diagnostic criteria: (1) intrusion (unwanted nightmares or thoughts about the experience); (2) avoidance (avoiding thoughts or situations that are reminders of the experience); (3) hyperarousal (“constantly on guard, watchful, or easily startled”), and (4) numbness or detachment (from others, activities, or surroundings). The PC-PTSD has been found to be superior to other PTSD screening tests, including the PTSD Checklist (PCL), with better sensitivity (85%) and specificity (82%) in a civilian primary care setting.18 The PC-PTSD was also found to perform similarly to the PCL in identifying PTSD risk among patients admitted to a trauma center20 and predicting PTSD among soldiers returning from combat.6
Pain and Interference
Pain and interference were evaluated using the 3-item Pain intensity and interference with Enjoyment of life and General activity (PEG).25 Pain Intensity was rated on an 11-point numeric rating scale (NRS), from 0 “no pain” to 10 “pain as bad as you can imagine.” For interference items, patients indicated how much pain interfered with enjoyment of life and with general activity from 0 “does not interfere” to 10 “completely interferes.” The PEG has established reliability and validity in a community and veteran populations with chronic pain and has shown similar responsiveness to improvement as the Brief Pain Inventory.24
Function
The Oswestry Disability Index (ODI)15 was used to evaluate pain-related functional disability. The ODI is a 10-item questionnaire that evaluates pain intensity and functional disability (e.g., personal care, lifting, walking, sleeping) associated with chronic low back pain. It is also a valuable outcome measure for other chronic pain conditions.16 It has established reliability and construct and discriminant validity.38, 48
Mood and Quality of Life
The Patient Health Questionnaire-9 (PHQ-9)26 The PHQ-9 is a 9-item questionnaire developed to screen for depression in the primary care setting. The items are based on DSM criteria for depressive disorders and has well-established validity and reliability.27 Patients are asked how often in the previous two weeks had they been bothered by these nine problems, such as “little interest or pleasure in doing things” or “feeling down, depressed, or hopeless” (0 “not at all”, 1 “several days”, 2 “more than half the days”, 3 “nearly every day”). Responses are summed to yield a total score and scores 10 or greater indicate a likely diagnosis of depression.
The Generalized Anxiety Disorder-7 (GAD-7)42 was used to evaluate the severity of symptoms of anxiety. The GAD-7 is a 7-item scale developed to screen for generalized anxiety disorder in the primary care setting. Similar to the PHQ-9 described above, patients are asked to indicate how often they have been bothered by the 7 problems, such as “feeling nervous, anxious, or on edge” or “becoming easily annoyed or irritable” (0 “not at all”, 1 “several days”, 2 “over half the days”, 3 “nearly every day”). Responses are summed to yield a total score, where higher scores indicate more severe anxiety. Total scores of 10 or higher indicate a likely diagnosis of GAD.42
The Patient Reported Outcome Measurement Information System (PROMIS) Global Health Short Form9 questionnaire was used to evaluate overall health-related quality of life (HRQOL). This reliable and valid scale is part of a National Institutes of Health initiative to standardize the collection of patient reported outcome measurement across studies and medical conditions.9 The scale consists of 10 items, spanning physical and mental health domains. Items are scored using a 5-point Likert scale from 1 to 5, where lower scores indicate poorer HRQOL.
Substance Abuse Risk
The Opioid Risk Tool49 was used to evaluate the risk of opioid misuse. The ORT evaluates the presence of risk factors associated with substance abuse, including personal and family history of substance abuse, sex, age (16–45 years), history of sexual abuse and select psychological disorders. The total number of risk factors correspond to low (0–3 risk factors), moderate (4–7 risk factors), and high (≥8 risk factors) risk for opioid misuse. Scores for certain items (e.g., history of preadolescent sexual abuse) are scored differentially for males and females. Higher scores denote greater risk for opioid misuse.
The Alcohol Use Disorders Identification Test-Consumption (AUDIT-C)8 was used to measure alcohol consumption. The AUDIT-C is a 3-item screening tool for risky drinking behavior, where total scores range from 0 – 12. Total scores ≥ 4 in men and ≥ 3 in women indicate hazardous drinking behavior. The AUDIT-C has shown similar efficiency as the 10-item AUDIT scale and has demonstrated good reliability and validity.14
Study Procedures
Consecutive new patients who attended the University of Washington (UW) Center for Pain Relief (CPR), between July of 2014 and June of 2016, completed a collection of pain-relevant patient-reported outcome questionnaires (PRO) using PainTracker.™ All new patients were asked to complete the online questionnaires within one week of their scheduled appointment. Given that the PTSD screen is only included in the baseline assessment, only baseline questionnaire data were analyzed for the purposes of the current study. This cross-sectional study is an examination of existing PainTracker™ PRO data from patients’ intake visits at UW CPR. The use of PainTracker™ data for research purposes was reviewed and approved by the Institutional Review Board at the University of Washington and a waiver of the requirement to obtain participant consent was obtained.
Data Analysis
Descriptive statistics and frequency distributions were calculated for sample characteristics. One-way analyses of variance (ANOVA) and Jonckheere-Terprstra tests (for ordered independent variable) for continuous variables and chi-square tests for categorical variables were used to evaluate for differences among patients with 0, 1, 2, 3, or 4 positive responses on the PC-PTSD. Posthoc Dunnett’s test and chi-square tests with Bonferroni corrections were conducted for continuous and categorical variables, respectively, to determine differences between patients with and without PTSD symptoms. A p-value of <0.05 was considered statistically significant. Data were analyzed using SPSS v.19 (IBM, Armonk, NY, USA). Adjustments were not made for missing data. The average completion rate across all outcome variables was 98.7% n=4,346), with completion rates ranging from 95.5% (n=4,205) to 99.7% (n=4,390).
Relative weight analysis (RWA),22 a technique most commonly used in business psychology and organizational research, was used to evaluate the relative contribution of specific PTSD symptom domains to the variance observed in pain and related outcomes. In brief, RWA applies an orthogonal transformation to predictor variables to overcome issues with multicollinearity and standard multiple regression analysis can be performed using transformed predictor variables.22, 45 Resultant beta weights are rescaled by combining them with standardized regression coefficients derived from regressing the original predictor variables on their orthogonal transformations.45 RWA thus captures the unique contribution of each predictor as well as its contribution in combination with other predictor variables.22 Specific PTSD symptom domains (i.e., intrusion, avoidance, hyperarousal, numbness/detachment) were entered as “predictor” variables and the various pain-related outcomes were entered in separate multiple regression models as independent criterion variables. Pairwise deletion was used to handle missing data and the recommended 10,000 bootstrap replications were applied to test for statistical significance at an alpha level of 0.05. Data were analyzed using the free, RWA web application (http://relativeimportance.davidson.edu/).45 De-identified data were uploaded to this interactive website and RWA code was executed in R, a free statistical software program (http://www.R-project.org/). R output raw and rescaled weights corresponding to the proportion of variance accounted for by each predictor and the “relative weight” of each predictor, respectively.45 Rescaled relative weights were interpreted as the percentage of predicted variance attributed to each predictor.
Results
Sample Characteristics
Table 1 describes the characteristics of the total sample. Online PainTracker™ completion rate was 71.3% for the study period. Patients were predominantly female (64.4%) and 48 years old, on average. The highest proportion of patients had private insurance (36.4%), followed by Medicaid (33.1%). On average, patients reported 1.4 ± 1.6 PTSD symptoms and 27.7% screened positive for PTSD (i.e., 3 of 4 PC-PTSD symptoms endorsed). Patients rated their pain intensity as 6.6 (SD=1.9) out of 10, on average, and 2,427 patients (57.5%) met or exceeded a cut-off of 7 for severe pain.
Table 1.
Demographic characteristics, PTSD, and pain intensity of the total sample (N=4,402).
| DEMOGRAPHICS
| |
|---|---|
| Sex - % Female (n) | 64.4 (2,834) |
|
| |
| Age, Mean (SD) | 48.3 (14.6);Range: 18–96 |
|
| |
| Payor Category, % (n) | |
| Private Insurance | 36.4 (1,484) |
| Medicaid | 33.1 (1,347) |
| Medicare | 24.0 (976) |
| Other (e.g., LNI/Charity/Tricare) | 6.6 (267) |
|
PC-PTSD | |
| PC-PTSD score, Mean (SD) | 1.4 (1.6);Range: 0–4 |
|
| |
| Positive screen for PTSD ≥3, %(n) | 27.7% (1,218) |
|
| |
| % (n) sample endorsed: | |
| Intrusion | 35.1 (1,554) |
| Avoidance | 34.9 (1,538) |
| Hyperarousal | 30.4 (1,340) |
| Numbness/detachment | 36.2 (1,595) |
|
PAIN INTENSITY | |
| Pain intensity (SD) | 6.6 (1.9) Range: 0–10 |
|
| |
| % with Severe Pain ≥ 7 (n) | 57.5% (2,427) |
Abbreviations: LNI = Labor & Industries; PC = Primary Care; PTSD = Post-traumatic Stress Disorder; SD = standard deviation; VA = Veterans Administration
Occurrence of PC-PTSD Symptoms and Pain-Related Outcomes
Table 2 describes the relationship between the number of PTSD symptoms and demographic and pain-related outcomes: 2,111 (48.0%) reported zero PTSD symptoms; 557 (12.7%) reported one PTSD symptom; 516 (11.7%) reported two PTSD symptoms, 444 (10.1%) reported three PTSD symptoms; and 774 (17.6%) reported all four PTSD symptoms.
Table 2.
Association between Number of PTSD Symptoms and Pain-related Outcome Measures (N=4,402).
| Number of PTSD Positive Answers | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| 0 48.0% (N=2,111) |
1 12.7% (N=557) |
2 11.7% (N=516) |
3 10.1% (N=444) |
4 17.6% (N=774) |
ANOVA or Chi-square/Jonckheer e-Terpstra p-values | |
|
| ||||||
| DEMOGRAPHICS | ||||||
|
| ||||||
| Sex, % female (n) | 62.0 (1,302) | 63.3 (349) | 67.0 (343)* | 67.7 (300)* | 70.1 (440)* | 0.001 |
|
| ||||||
| Age, Mean (SD) | 50.2 (15.2) | 49.9 (14.9) | 47.6 (14.2)* | 46.5 (13.4)* | 43.8 (12.2)* | <0.001/<0.001 |
|
| ||||||
| Payor category - % (n) | <0.001 | |||||
| Private insurance | 45.0 (890) | 32.3 (164)* | 31.5 (149)* | 28.1 (115)* | 23.5 (166)* | <0.001 |
| Medicaid | 25.2 (499) | 31.4 (159)* | 34.0 (161)* | 43.8 (179)* | 49.4 (349)* | <0.001 |
| Medicare | 24.8 (491) | 28.6 (145) | 27.9 (132) | 21.8 (89) | 16.8 (119)* | <0.001 |
| Other (e.g., LNI/Tricare) | 5.0 (98) | 7.7 (39) | 6.6 (31) | 6.4% (26) | 10.3 (73)* | <0.001 |
|
| ||||||
| PAIN & INTERFERENCE | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
|
| ||||||
| Pain intensity | 6.3 (1.9) | 6.5 (2.0) | 6.7 (1.8)* | 7.0 (1.7)* | 7.1 (1.7)* | <0.001/<0.001 |
|
| ||||||
| Pain interference with general activity | 6.6 (2.4) | 7.0 (2.3)* | 7.1 (2.1)* | 7.5 (2.1)* | 7.7 (2.1)* | <0.001/<0.001 |
|
| ||||||
| Pain interference with enjoyment of life | 6.6 (2.5) | 7.2 (2.4)* | 7.2 (2.3)* | 7.8 (2.2)* | 7.9 (2.1)* | <0.001/<0.001 |
|
| ||||||
| FUNCTION | ||||||
|
| ||||||
| ODI score | 43.0 (16.2) | 47.4 (16.3)* | 48.8 (15.7)* | 51.7 (15.1)* | 54.6 (15.1)* | 0<.001/0<.001 |
|
| ||||||
| MOOD, QOL, SATISFACTION | ||||||
|
| ||||||
| PHQ-9 score | 8.7 (5.7) | 11.9 (6.0)* | 12.7 (5.7)* | 14.8 (6.0)* | 16.6 (6.5)* | 0<.001/0<.001 |
|
| ||||||
| GAD-7 score | 4.5 (4.4) | 7.4 (5.0)* | 8.6 (5.0)* | 10.9 (5.4)* | 13.0 (5.8)* | <0.001/<0.001 |
|
| ||||||
| PROMIS global | 27.5 (4.8) | 26.3 (4.6)* | 25.7 (4.2)* | 25.3 (4.4)* | 24.7 (4.0)* | <0.001/0<.001 |
|
| ||||||
| SUBSTANCE ABUSE/MISUSE | ||||||
|
| ||||||
| ORT score | 2.5 (3.3) | 3.7 (4.1)* | 4.3 (4.1)* | 4.8 (4.6)* | 5.5 (4.9)* | <0.001/<0.001 |
|
| ||||||
| AUDIT-C score | 1.4 (1.6) | 1.2 (1.5)* | 1.1 (1.5)* | 1.1 (1.4)* | 1.0 (1.3)* | 0.002/<0.001 |
Abbreviations: AUDIT = Alcohol Use Disorders Identification Test; GAD = Generalized Anxiety Disorder; LNI = Labor & Industries; ODI = Oswestry Disability Index; ORT = Opioid Risk Tool; PHQ = Patient Health Questionnaire; PROMIS = Patient-Reported Outcomes Measurement Information System; PTSD = Post-traumatic Stress Disorder; QOL = quality of life; SD = standard deviation
As displayed in Table 2, significant Jonckheere-Terpstra tests for ordered independent variables were observed for all pain-related outcomes evaluated. In general, incremental increases in the number of PTSD symptoms was associated with increased pain intensity and interference, increased pain-related disability, increased depressive symptom and anxiety severity, and reduced HRQOL, as well as increased risk for opioid misuse (all p<0.001).
Compared to patients with no PTSD symptoms, patients who endorsed one or more PTSD symptom reported: greater pain interference (with general activity and enjoyment of life; greater pain-related functional disability; greater depression and anxiety symptoms; reduced HRQOL; increased risk for opioid misuse; and decreased alcohol use (all post-hoc multiple comparisons, p<0.05). Compared to patients with no PTSD symptoms, patients who endorsed two, three, or four PTSD symptoms also reported: increased pain intensity ratings (post-hoc multiple comparisons, p<0.01).
Relative Weight Analyses
Figure 1 displays the RWA findings. The relative weights of each PTSD symptom, expressed as the percent of predicted variance in the outcome attributed to each symptom domain, are displayed for each of the outcomes assessed. If each of the symptom domains contributed an equal proportion of variance, each of their respective weights would be ~25% (25% × 4 = 100%). As Figure 1 depicts, numbness or detachment was the only PTSD symptom that accounted for more than 25% variance for every outcome assessed. Raw and rescaled weights, including 95% confidence intervals, for each of the models evaluated are displayed in Supplemental Table 1. Supplemental Table 1 also indicates whether numbness or detachment accounted for significantly more of the predicted variance than the other PTSD symptoms. For pain interference with general activity, pain interference with enjoyment of life, pain-related disability (ODI score), depressive symptoms, anxiety, and HRQOL, numbness/detachment accounted for significantly more of the predicted variance than each of the other symptoms (i.e, intrusion, avoidance, hyperarousal). For pain intensity, numbness/detachment accounted for significantly more of the predicted variance than intrusion.
Figure 1.
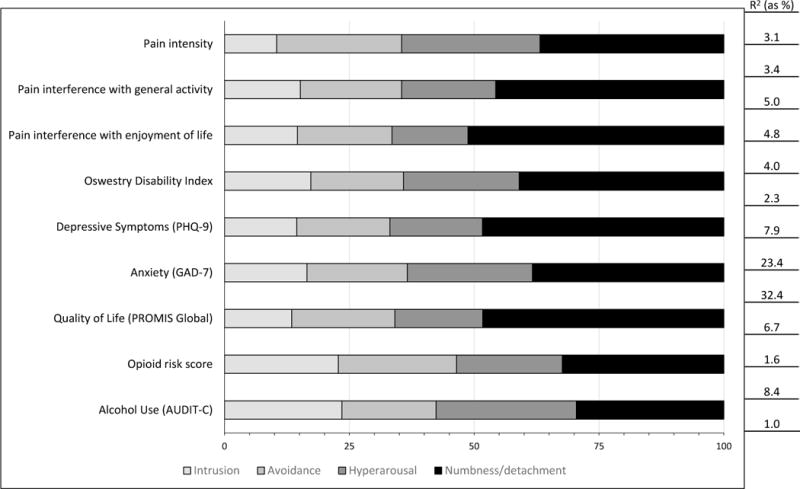
Results of the relative weight analysis (RWA). The relative weights of each PTSD symptom, expressed as the percent of predicted variance in the outcome attributed to each symptom domain, are displayed for each of the patient-reported outcomes assessed.
Discussion
This cross-sectional study of patients at a specialty pain center serving a predominantly civilian population documents the important relationship between PTSD symptoms and a broad array of pain-related outcomes. It also highlights the especially important role of the symptom, “numbness or detachment from others”, which accounted for a larger proportion of the predicted variance than the other PTSD symptom domains for most pain related outcomes assessed. This cross-sectional study cannot verify that PTSD symptoms are causing patients to experience worse pain-related outcomes, but it suggests that there is a strong relationship that should be studied with longitudinal data.
The proportion of patients screened positive for PTSD in this sample (27%) is consistent with previous reports.1, 2, 36 The finding that patients who screened positive for PTSD were younger, more likely to be women, and reported significantly worse pain, function, and mood outcomes, also corroborates previous findings,1, 2, 12, 19, 30, 31, 43 and provides additional confirmation of the importance of evaluating for PTSD symptoms in the setting of chronic pain. Patients with likely PTSD also reported lower alcohol use than patients without PTSD symptoms. This latter finding may be due to avoidance of an alcohol-related traumatic experience, medical comorbidities or medications that prohibit alcohol use, or avoidance due to a history of alcohol use disorder.
We observed a significant relationship between increases in the number of PTSD symptom domains endorsed and increases in the severity of all pain-related outcomes evaluated. Among this large, heterogeneous sample of patients with chronic pain, the occurrence of even one or two PTSD symptoms was associated with a host of negative outcomes. Compared to patients with no symptoms, patients who reported two PTSD symptoms reported higher pain intensity and pain interference, greater pain-related disability, more severe depressive and anxiety symptoms, poorer HRQOL, and greater risk of opioid misuse than those without PTSD symptoms. Even patients who endorsed only one PTSD symptom reported greater pain interference with general activity and enjoyment of life; greater pain-related functional disability; greater depression and anxiety symptoms; reduced HRQOL; increased risk for opioid misuse; and lower alcohol use. Of note, increased risk of opioid misuse may be, at least partially, explained by the fact that the ORT contains items related to a history of preadolescent sexual abuse and the occurrence of psychological disorders. Overall, even the experience of one PTSD symptom appears to incur significantly elevated risk for poorer pain-related outcomes. These findings suggest that subsyndromal PTSD is clinically meaningful in patients with chronic pain. The standard threshold for a positive PTSD screen using the PC-PTSD (i.e., endorsement of any three of four symptoms) may overlook a substantial proportion of patients (25%) who do not fulfill diagnostic criteria (i.e., one or two symptoms), yet still have significant pain-related impairment relative to patients with no PTSD symptoms. In fact, Prins et al. proposed a PC-PTSD cut-off score of 2 in circumstances where maximization of sensitivity is preferable.35 Given the substantial association between PTSD symptoms and the outcomes studied, patients with chronic pain who endorse even one PTSD symptoms may warrant closer evaluation.
Findings from the RWA indicated that emotional numbness or detachment from others had the largest contribution to the total variance in nearly all of the predicted outcomes. This finding provides additional support for recent modifications made to DSM-V criteria, which separate the DSM-IV PTSD grouping of avoidance and emotional numbing into two separate domains.5 Moreover, these findings are in line with previous investigations into the factor structure of PTSD symptoms that identified four distinct PTSD symptom domains (re-experiencing, avoidance, numbing, hyperarousal).3 Interestingly, among patients who reported only one PTSD symptom, nearly half (46.7%; n=260/557) endorsed numbness or detachment. In turn, these patients experienced overall worse-pain related outcomes (increased pain intensity, pain interference with general activity and enjoyment of life, pain-related disability, depressive symptoms, anxiety, and reduced HRQOL) compared to patients who reported only one of the other symptom domains (data not shown).
Existing theoretical models like the Shared Vulnerability3 and Mutual Maintenance41 models provide a valuable framework for conceptualizing the intricate relationship between chronic pain and PTSD. The Shared Vulnerability Model posits that a predisposing factor, such as anxiety sensitivity, underlies the development of and/or response to both chronic pain and PTSD.3 Anxiety sensitivity has also been proposed as a key predisposing factor in the diasthesis-stress model of chronic pain.47 The Mutual Maintenance Model proposes that elements of chronic pain impact the experience of PTSD and vice versa (e.g., anxiety sensitivity, avoidance), resulting in a negative cyclic relationship that exacerbates both conditions.41 Both models highlight the importance of anxiety sensitivity and avoidance or fear of pain as key mediators of the relationship between chronic pain and PTSD. However, neither model incorporates or accounts for emotional numbing or detachment.
In another study, emotional numbing, but not avoidance, was found to significantly predict pain-related disability 6- and 12-months following thoracotomy.23 Similarly, emotional numbing was associated with impaired functioning in patients injured in motor vehicle accidents.11 Moreover, emotional numbing and hyperarousal symptoms (not re-experiencing or avoidance) were significantly associated with pain intensity and disability among patients with chronic musculoskeletal pain, a relationship mediated by anxiety sensitivity, catastrophizing, and fear of pain.28 This relative importance of numbness/detachment in pain outcomes is notable given that opioid treatment of chronic pain in patients with PTSD appears to relieve mostly re-experiencing and hyperarousal symptoms.7 In contrast, opioids and benzodiazepines, may deepen numbing and detachment. Alternate interventions that target the numbness and detachment of PTSD are needed.
This study had important limitations. Because of the cross-sectional nature of the current study, the causal relationship between chronic pain and PTSD symptoms cannot be determined. However, in a longitudinal study of pain and PTSD associated with accidental injury, PTSD symptoms were found to significantly predict improvement in pain over time, but not the converse,21 suggesting that interventions that target PTSD symptoms may have an important impact on pain reduction. Follow-up studies will evaluate the subset of patients who continued their care at UW CPR to determine how pain outcomes and PTSD symptoms change over time.
In addition, time since the traumatic event and duration of chronic pain were not captured. Therefore, it is not known whether the pain experienced by the patients is a result of a traumatic event (e.g., motor vehicle accident, multiple failed surgeries, sexual abuse), or if pain preceded the traumatic event. Specific information related to dose of pain medication use was not collected; therefore, although the risk for opioid misuse was captured, the dose of opioids at the time of data collection is not known. Finally, the PC-PTSD is a relatively simple instrument, only capturing one or two symptoms from each PTSD symptom domain. Other symptoms not captured by the PC-PTSD screen, such as self-blame or destructive behavior, might also be associated with the experience of chronic pain. A revised PC-PTSD screen (PC-PTSD-5) was recently introduced to more comprehensively reflect DSM-V criteria for PTSD, including self-blame. Of note, 71.3% of patients seeking care at UW CPR completed the new patient PainTracker™ assessment during the observation period. Reasons for non-completion were not documented, therefore generalizability to all patients receiving care at specialty pain clinics is limited.
In summary, our screening study suggested that PTSD and subsyndromal PTSD are highly prevalent among patients with chronic pain (>50%) and are associated with significantly worse pain intensity and interference, function, mood, and HRQOL outcomes. Numbness or detachment as a result of trauma exposure appears to be the PTSD symptom most strongly associated with pain-related outcomes. This numbness and detachment warrants further investigation and may comprise an important target for interventions that improve both PTSD symptoms and pain.
Supplementary Material
Highlights.
PTSD symptoms are associated with multiple outcomes in patients with chronic pain
Even one PTSD symptom was associated with poorer pain-related outcomes overall
The PTSD symptom of numbness or detachment is particularly important
Subsyndromal PTSD and numbness or detachment are important in chronic pain
Acknowledgments
Disclosures
Funding sources include the National Institute of Nursing Research of the National Institutes of Health under award number K24 NR015340. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest to disclose.
References
- 1.Akerblom S, Perrin S, Rivano Fischer M, McCracken LM. The Impact of PTSD on Functioning in Patients Seeking Treatment for Chronic Pain and Validation of the Posttraumatic Diagnostic Scale. Int J Behav Med. 2017;24(2):249–259. doi: 10.1007/s12529-017-9641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andersen TE, Andersen LA, Andersen PG. Chronic pain patients with possible co-morbid post-traumatic stress disorder admitted to multidisciplinary pain rehabilitation-a 1-year cohort study. Eur J Psychotraumatol. 2014;5 doi: 10.3402/ejpt.v5.23235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47(10):930–7. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- 4.Asmundson GJ, Wright KD, Stein MB. Pain and PTSD symptoms in female veterans. Eur J Pain. 2004;8(4):345–50. doi: 10.1016/j.ejpain.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Association, A.P. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: 2013. Series: Diagnostic and statistical manual of mental disorders, (5th ed.) [Google Scholar]
- 6.Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. J Consult Clin Psychol. 2008;76(2):272–81. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- 7.Bremner JD, Southwick SM, Darnell A, Charney DS. Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am J Psychiatry. 1996;153(3):369–75. doi: 10.1176/ajp.153.3.369. [DOI] [PubMed] [Google Scholar]
- 8.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–95. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 9.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, Devellis R, DeWalt D, Fries JF, Gershon R, Hahn EA, Lai JS, Pilkonis P, Revicki D, Rose M, Weinfurt K, Hays R, P.C. Group The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cho SK, Heiby EM, McCracken LM, Moon DE, Lee JH. Daily functioning in chronic pain: study of structural relations with posttraumatic stress disorder symptoms, pain intensity, and pain avoidance. Korean J Pain. 2011;24(1):13–21. doi: 10.3344/kjp.2011.24.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clapp JD, Beck JG, Palyo SA, Grant DM. An examination of the synergy of pain and PTSD on quality of life: additive or multiplicative effects? Pain. 2008;138(2):301–9. doi: 10.1016/j.pain.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Creamer M, Burgess P, McFarlane AC. Post-traumatic stress disorder: findings from the Australian National Survey of Mental Health and Well-being. Psychol Med. 2001;31(7):1237–47. doi: 10.1017/s0033291701004287. [DOI] [PubMed] [Google Scholar]
- 13.Cyders MA, Burris JL, Carlson CR. Disaggregating the relationship between posttraumatic stress disorder symptom clusters and chronic orofacial pain: implications for the prediction of health outcomes with PTSD symptom clusters. Ann Behav Med. 2011;41(1):1–12. doi: 10.1007/s12160-010-9221-5. [DOI] [PubMed] [Google Scholar]
- 14.Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcoholism-Clinical and Experimental Research. 2005;29(5):844–854. doi: 10.1097/01.alc.0000164374.32229.a2. [DOI] [PubMed] [Google Scholar]
- 15.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–3. [PubMed] [Google Scholar]
- 16.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25(22):2940–52. doi: 10.1097/00007632-200011150-00017. discussion 2952. [DOI] [PubMed] [Google Scholar]
- 17.Fetzner MG, McMillan KA, Asmundson GJ. Similarities in specific physical health disorder prevalence among formerly deployed Canadian forces veterans with full and subsyndromal PTSD. Depress Anxiety. 2012;29(11):958–65. doi: 10.1002/da.21976. [DOI] [PubMed] [Google Scholar]
- 18.Freedy JR, Steenkamp MM, Magruder KM, Yeager DE, Zoller JS, Hueston WJ, Carek PJ. Post-traumatic stress disorder screening test performance in civilian primary care. Fam Pract. 2010;27(6):615–24. doi: 10.1093/fampra/cmq049. [DOI] [PubMed] [Google Scholar]
- 19.Geisser ME, Roth RS, Bachman JE, Eckert TA. The relationship between symptoms of post-traumatic stress disorder and pain, affective disturbance and disability among patients with accident and non-accident related pain. Pain. 1996;66(2–3):207–14. doi: 10.1016/0304-3959(96)03038-2. [DOI] [PubMed] [Google Scholar]
- 20.Hanley J, deRoon-Cassini T, Brasel K. Efficiency of a four-item posttraumatic stress disorder screen in trauma patients. J Trauma Acute Care Surg. 2013;75(4):722–7. doi: 10.1097/TA.0b013e3182a53a5f. [DOI] [PubMed] [Google Scholar]
- 21.Jenewein J, Wittmann L, Moergeli H, Creutzig J, Schnyder U. Mutual influence of posttraumatic stress disorder symptoms and chronic pain among injured accident survivors: a longitudinal study. J Trauma Stress. 2009;22(6):540–8. doi: 10.1002/jts.20453. [DOI] [PubMed] [Google Scholar]
- 22.Johnson JW. A Heuristic Method for Estimating the Relative Weight of Predictor Variables in Multiple Regression. Multivariate Behav Res. 2000;35(1):1–19. doi: 10.1207/S15327906MBR3501_1. [DOI] [PubMed] [Google Scholar]
- 23.Katz J, Asmundson GJ, McRae K, Halket E. Emotional numbing and pain intensity predict the development of pain disability up to one year after lateral thoracotomy. Eur J Pain. 2009;13(8):870–8. doi: 10.1016/j.ejpain.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 24.Krebs EE, Bair MJ, Damush TM, Tu W, Wu J, Kroenke K. Comparative responsiveness of pain outcome measures among primary care patients with musculoskeletal pain. Med Care. 2010;48(11):1007–14. doi: 10.1097/MLR.0b013e3181eaf835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krebs EE, Lorenz KA, Bair MJ, Damush TM, Wu J, Sutherland JM, Asch SM, Kroenke K. Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J Gen Intern Med. 2009;24(6):733–8. doi: 10.1007/s11606-009-0981-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JB. A new measure of depression severity: The PHQ-9. Journal of General Internal Medicine. 2000;15:78–78. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lopez-Martinez AE, Ramirez-Maestre C, Esteve R. An examination of the structural link between post-traumatic stress symptoms and chronic pain in the framework of fear-avoidance models. Eur J Pain. 2014;18(8):1129–38. doi: 10.1002/j.1532-2149.2014.00459.x. [DOI] [PubMed] [Google Scholar]
- 29.McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. 2003;106(1–2):127–33. doi: 10.1016/s0304-3959(03)00301-4. [DOI] [PubMed] [Google Scholar]
- 30.Morasco BJ, Lovejoy TI, Lu M, Turk DC, Lewis L, Dobscha SK. The relationship between PTSD and chronic pain: mediating role of coping strategies and depression. Pain. 2013;154(4):609–16. doi: 10.1016/j.pain.2013.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olff M. Sex and gender differences in post-traumatic stress disorder: an update. Eur J Psychotraumatol. 2017;8(sup4) [Google Scholar]
- 32.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Medical comorbidity of full and partial posttraumatic stress disorder in US adults: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom Med. 2011;73(8):697–707. doi: 10.1097/PSY.0b013e3182303775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25(3):456–65. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pietrzak RH, Schechter CB, Bromet EJ, Katz CL, Reissman DB, Ozbay F, Sharma V, Crane M, Harrison D, Herbert R, Levin SM, Luft BJ, Moline JM, Stellman JM, Udasin IG, Landrigan PJ, Southwick SM. The burden of full and subsyndromal posttraumatic stress disorder among police involved in the World Trade Center rescue and recovery effort. J Psychiatr Res. 2012;46(7):835–42. doi: 10.1016/j.jpsychires.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 35.Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, Sheikh JI. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry. 2003;9(1):9–14. [Google Scholar]
- 36.Roy-Byrne P, Smith WR, Goldberg J, Afari N, Buchwald D. Post-traumatic stress disorder among patients with chronic pain and chronic fatigue. Psychol Med. 2004;34(2):363–8. doi: 10.1017/s0033291703008894. [DOI] [PubMed] [Google Scholar]
- 37.Ruscio AM, Ruscio J, Keane TM. The latent structure of posttraumatic stress disorder: a taxometric investigation of reactions to extreme stress. J Abnorm Psychol. 2002;111(2):290–301. [PubMed] [Google Scholar]
- 38.Saltychev M, Mattie R, McCormick Z, Barlund E, Laimi K. Psychometric properties of the Oswestry Disability Index. Int J Rehabil Res. 2017 doi: 10.1097/MRR.0000000000000226. [DOI] [PubMed] [Google Scholar]
- 39.Schnurr PP. A guide to the literature on partial PTSD. PTSD Research Quarterly. 2014;25(1):1–8. [Google Scholar]
- 40.Schorn MM, Doorenbos AZ, Gordon D, Read-Williams P. Survey of Primary-Care Providers on Perceived Benefits of and Barriers to PainTracker. J Nurse Pract. 2014;10(10):781–786. doi: 10.1016/j.nurpra.2014.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin Psychol Rev. 2001;21(6):857–77. doi: 10.1016/s0272-7358(00)00071-4. [DOI] [PubMed] [Google Scholar]
- 42.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 43.Stalnacke BM, Ostman A. Post-traumatic stress in patients with injury-related chronic pain participating in a multimodal pain rehabilitation program. Neuropsychiatr Dis Treat. 2010;6:59–66. doi: 10.2147/ndt.s7985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry. 1997;154(8):1114–9. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- 45.Tonidandel S, LeBreton JM. RWA Web: A free, comprehensive, web-based, and user-friendly tool for relative weight analyses. J Bus Psyol. 2015;30(2):207–216. [Google Scholar]
- 46.Tsui P, Stein T, Sonty N. The relationship among PTSD symptoms, chronic pain acceptance and disability. J Pain. 2010;11:S58. [Google Scholar]
- 47.Turk DC. A diathesis-stress model of chronic pain and disability following traumatic injury. Pain Res Manag. 2002;7(1):9–19. doi: 10.1155/2002/252904. [DOI] [PubMed] [Google Scholar]
- 48.Vianin M. Psychometric properties and clinical usefulness of the Oswestry Disability Index. J Chiropr Med. 2008;7(4):161–3. doi: 10.1016/j.jcm.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 2005;6(6):432–42. doi: 10.1111/j.1526-4637.2005.00072.x. [DOI] [PubMed] [Google Scholar]
- 50.Zlotnick C, Franklin CL, Zimmerman M. Does “subthreshold” posttraumatic stress disorder have any clinical relevance? Compr Psychiatry. 2002;43(6):413–9. doi: 10.1053/comp.2002.35900. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


