Abstract
We investigated extramedullary disease in newly diagnosed multiple myeloma patients and its impact on outcome following first-line autologous stem cell transplantation. We identified 3744 adult myeloma patients who received up-front single (n=3391) or tandem transplantation (n=353) between 2005 and 2014 with available data on extramedullary involvement at diagnosis. The overall incidence of extramedullary disease was 18.2% (n=682) and increased per year from 6.5% (2005) to 23.7% (2014). Paraskeletal involvement was found in 543 (14.5%) and extramedullary organ involvement in 139 (3.7%). More patients with extramedullary organ involvement had multiple involved sites (≥2; P<0.001). In a comparison of patients with single sites with patients without the disease, up-front transplantation resulted in at least similar 3-year progression-free survival (paraskeletal: P=0.86, and extramedullary organ: P=0.88). In single paraskeletal involvement, this translated less clearly into worse 3-year overall survival (P=0.07) while single organ involvement was significantly worse (P=0.001). Multiple organ sites were associated with worse outcome (P<0.001 and P=0.01). First-line treatment with tandem compared with single transplantation resulted in similar survival in patients with extramedullary disease at diagnosis (P=0.13 for both).
Introduction
Multiple myeloma (MM) accounts for approximately 2% of all new cancer cases and 13% of hematologic cancers with an age-adjusted incidence of 6 per 100,000 per year in the USA and Europe.1 Autologous stem cell transplantation (ASCT) and the development of new agents have considerably increased the median survival of MM patients.2 The disease is characterized by a clonal proliferation of malignant plasma cells with a strong dependence on the bone marrow (BM) microenvironment.3
However, in some MM patients, myeloma cells escape the BM, resulting in extramedullary disease (EMD), which can be further characterized by two different types of involvement: 1) paraskeletal (PS), consisting of masses that arose from bone lesions; and 2) extramedullary organ involvement (EM), resulting from hematogenous spread into different organs, skin and lymph nodes.4,5 At the time of MM diagnosis, the incidence of EM involvement in observational studies ranges from 1.7% to 4.5 using a baseline staging that includes whole-body magnetic resonance imaging (MRI) or positron emission tomography- computed tomography (PET-CT).6 Paraskeletal involvement is more frequent and varies from 7% to 34.2% due to different definitions and access of sensitive imaging techniques.7–10 Rates are also considered to be higher at relapse or after surgery.11,12 Several studies reported that EMD was associated with shorter survival rates, and thus considered EMD as a high-risk feature. However, the evidence of the effect of EMD at diagnosis is limited due to small populations, heterogenous patient or intervention selection, and relapse settings.13–16 Therefore, very limited data are available to assess the role of EMD at diagnosis of MM patients after up-front ASCT. This lack of evidence is striking, since ASCT is standard therapy in first- line therapy in eligible patients.17,18
Therefore, the objective of this study was to determine the demographic and clinical characteristics of EMD in MM patients at diagnosis and to evaluate its impact on outcome after up-front ASCT as first-line therapy. For this purpose, we analyzed 3744 patients with or without EMD at diagnosis after up-front single or tandem ASCT who had been reported to the European Society for Blood and Marrow Transplantation (EBMT) registry between 2005 and 2014.
Methods
Study design and data collection
We included adult patients with MM who had available data on extramedullary involvement at time of diagnosis who received an up-front single ASCT within 12 months of diagnosis or a tandem ASCT within six months from first ASCT as first- line therapy and who had been reported to the EBMT registry between January 2005 and December 2014. Patients were considered eligible for analysis if there were full data available on extramedullary involvement (yes or no) at time of diagnosis, its location, and the number of sites. This study was performed in accordance with the principles of the Declaration of Helsinki and was approved by the Chronic Malignancies Working Party of the EBMT. The EBMT is a non-profit, scientific society representing more than 600 transplant centers, mainly in Europe. Data are entered, managed, and maintained in a central database with internet access. Audits are routinely performed to determine the accuracy of the data. Data on extramedullary involvement were extracted from the database using Med-B forms. Patients whose transplant data are reported provided informed consent to use the information for research purposes and data are anonymized.
Definitions and statistical analysis
The primary end point was 3-year progression-free survival (PFS), which was defined as the time from ASCT to disease progression or death from any cause. The secondary end points were 3-year overall survival (OS), non-relapse mortality (NRM) and response. Overall survival was defined as the time from ASCT to death from any cause or last follow up. Non-relapse mortality was defined as death without evidence of relapse or progression, with relapse or progression as competing events. Remission, progression and relapse were defined according to standard EBMT criteria.19
On the basis of type of extramedullary involvement, we defined three groups of myeloma patients: 1) without EMD (MM group); 2) with paraskeletal (PS group); and 3) extramedullary organ involvement (EM group). In addition, we determined and analyzed the impact of the number of involved sites as one or multiple (≥ 2) sites. Disease stage at diagnosis was determined according to the International Staging System (ISS; I-III),20 Salmon and Durie stages I, II or III, and also according to renal function A or B.21 Performance status at ASCT was assessed with the Karnofsky score (≤80 indicating poor and >80 good status).22 Categorical variables were compared with the use of the Fisher’s exact test or the χ2 test. Continuous variables were analyzed using the Kruskal-Wallis test for independent samples.
Survival probabilities were estimated by the Kaplan-Meier method,23 and the Log-Rank test was used for univariate comparison. Median follow up was calculated according to the reverse Kaplan-Meier method.24 Outcomes were artificially censored at three years. We used cumulative incidence analysis to assess NRM, and labeled death from relapse as a competing event.25,26 The proportional hazards assumption was verified using graphical methods. Scaled Schoenfeld27 residuals and graphical checks proposed by Klein and Moeschberger28 were performed to find evidence of violations. To minimize the effect of selection bias, we used a landmark analysis at six months whenever single and tandem ASCT were compared.
To assess the multivariate effect of factors on each end point, we used the Cox proportional hazards model to estimate hazard ratios (HR).29 Only complete cases were included in the analysis. All tests were two-sided, with the type I error rate fixed at a=0.05. All analyses were performed using the statistical software R, v.3.1.0 (R Foundation for Statistical Computing, Vienna, Austria) and SPSS Statistics 23 (SPSS, IBM Corp, Armonk, NY, USA).
Results
Incidence and sites
Among the 3744 patients identified in the registry, 14.5% (n=543) had paraskeletal involvement (PS group) and 3.7% (n=139) extramedullary organ involvement (EM group), while 81.8% (n=3062) had no EMD (MM group). Between 2005 and 2014, the EMD incidence per year increased from 6.5% to 23.7%.
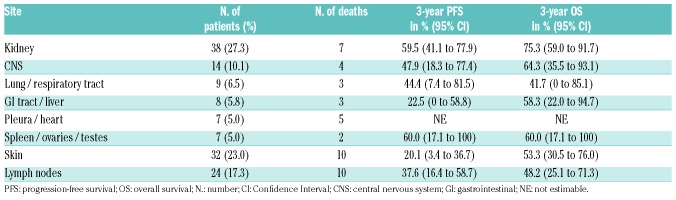
Within the EM group, the involved sites were: kidney (27.3%, n=38), skin (23.0%, n=32), lymph nodes (17.3%, n=24), central nervous system (CNS; 10.1%, n=14), lung and respiratory tract (6.5%, n=9), gastrointestinal tract (GI) and liver (5.8%, n=8), pleura and heart (5.0%, n=7), and spleen, ovaries and testes (5.0%, n=7). Most patients with EMD (93.5%, n=639) presented with one involved site (PS1 and EM1), 5.7% (n=36) had two sites, 0.7% (n=5) had three sites, while four and five sites were present in 0.1% (n=1) of patients, respectively. Notably, within the PS group, all 19 patients with multiple (≥2) sites had only additional paraskeletal involvement (PS2), while further involvement in all 24 EM patients was also restricted to other organs (EM2).
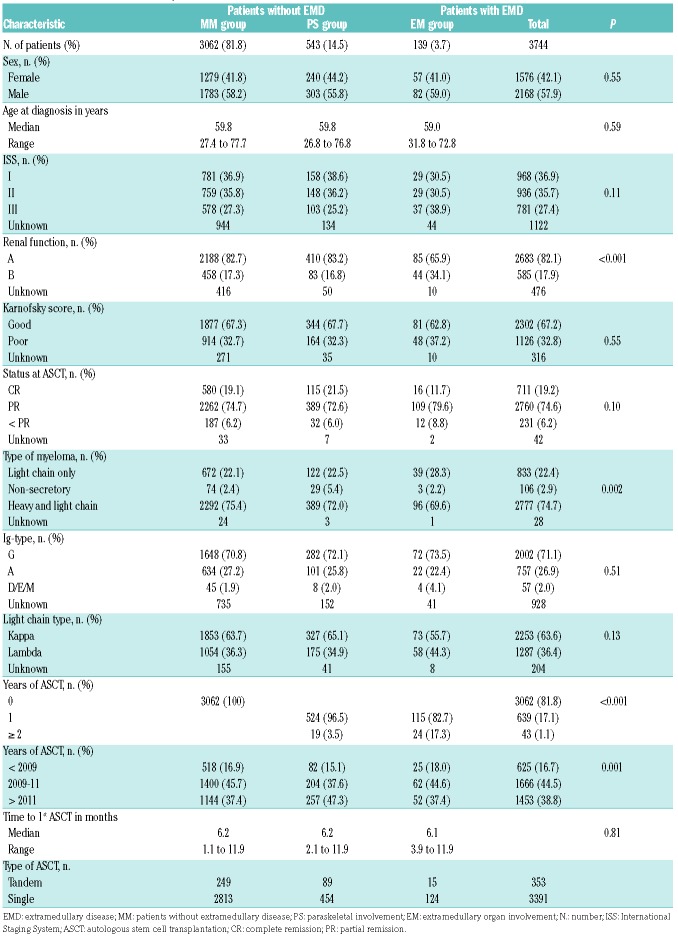
Patients’ and disease characteristics
Median age at diagnosis was 59.8 years in both MM and PS, and 59.0 years in EM patients (P=0.59). In all groups there were more males (57.9%) than females (42.1%). More EM patients (34.1%) had worse renal function (stage B) in comparison to PS (16.8%) and MM patients (17.3%; P<0.001). Patients with EM involvement (28.3%) were more likely to have light chain disease compared to PS (22.5%) and MM patients (22.1%; P=0.002). More detailed patients’ characteristics are listed in Table 1.
Table 1.
Patients’, disease and transplantation characteristics.
Transplantation characteristics and responses
The source of stem cells for all patients was peripheral blood. A total of 3391 patients underwent up-front single ASCT and 353 patients up-front tandem ASCT; there was no difference in time to first ASCT between the two groups (P=0.81). Complete remission (CR) before the first ASCT was reported in 21.5% PS, 11.7% EM and 19.1% MM patients; partial remission (PR) was achieved by 72.6% PS, 79.6% EM and 74.7% MM patients (P=0.1) (Table 1). After ASCT, complete response was achieved by 41.6% PS, 36.1% EM and 43.9% MM patients, while 54.0% PS, 51.9% EM and 49.8% MM patients showed partial response (P=0.001).
EMD and survival
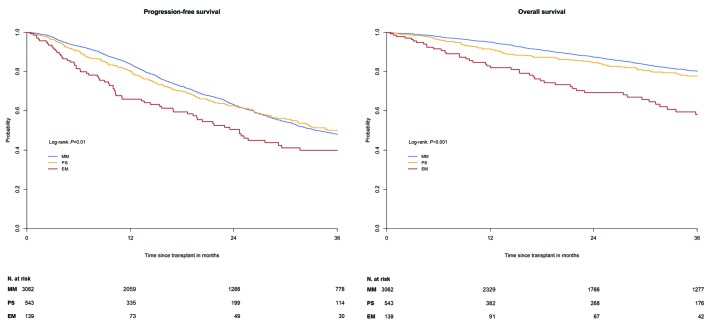
Median follow up was 36.3 months (range: 1–118.9 months) after the date of ASCT. In the univariate analysis, the MM and PS groups showed similar 3-year PFS of 47.9% (95%CI: 45.8–50.1) versus 50.0% (95%CI: 44.6–55.3; P=0.78) and similar 3-year OS of 80.1% (95%CI: 78.4–81.8) versus 77.7% (95%CI: 73.3–82.1; P=0.09) (Figure 1A and B). In contrast, EM patients had a significantly worse 3-year PFS of 39.9% (95%CI: 30.3–49.5) in comparison to MM (P=0.001) and PS patients (P=0.007), and a significantly worse 3-year OS of 58.0% (95%CI: 48.1–67.9) compared to MM and PS patients (P<0.001, respectively). Within the EM group, 3-year PFS differed according to involved organs: kidney (59.5%), skin (20.1%), lymph nodes (37.6%), CNS (47.9%), lung/respiratory tract (44.4%), GI/liver (22.5%), and spleen, ovaries and testes (60.0%) (Table 2).
Figure 1.
Progression-free survival (A) and overall survival (B) with numbers at risk of myeloma patients following up-front autologous stem cell transplantation according to presence of involvement. MM: no extramedullary disease; PS: paraskeletal involvement; EM: extramedullary organ involvement; N: number.
Table 2.
Involved sites in extramedullary organ involvement (EM) group and survival after autologous stem cell transplantation (ASCT).
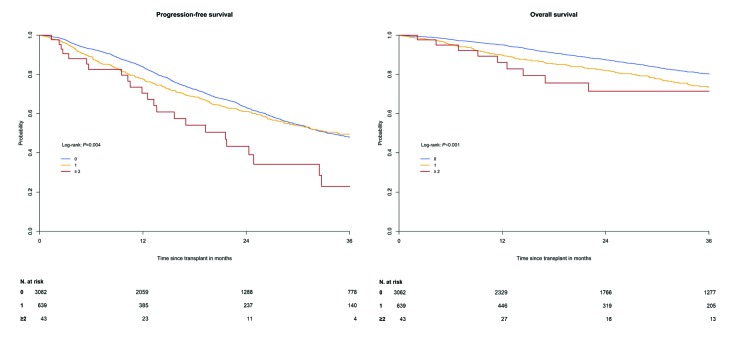
Comparing the MM group without EMD to those with EMD, one involved site resulted in a similar 3-year PFS of 49.4% (95%CI: 44.6–54.3; P=0.36) while multiple involved sites showed a worse PFS of 22.7% (95%CI: 5.2–40.2; P=0.001) (Figure 2A). Both one and multiple involved sites showed worse 3-year OS rates of 73.5% (95%CI: 69.2–77.7; P<0.001) and 71.4% (95%CI: 55.1–87.7; P=0.05) in comparison to patients without EMD (80.1%) (Figure 2B).
Figure 2.
Progression-free survival (A) and overall survival (B) with numbers at risk of myeloma patients following up-front autologous stem cell transplantation according to number of involvements: 0, 1 and ≥ 2. N: number.
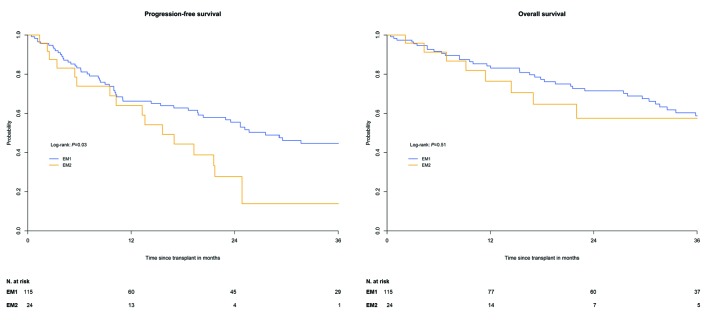
After stratification of EMD groups according to one versus multiple involved sites (PS1 vs. PS2, and EM1 vs. EM2), PS patients showed no significant difference in 3- year PFS of 50.5% (95%CI: 45.0–55.9%) versus 36.0% (95%CI: 5.2–66.8%; P=0.71), and OS of 77.2% (95%CI: 72.7–81.7%) versus 91.7% (95%CI: 76.0–100; P=0.27). In EM patients, this comparison resulted in a significantly worse 3-year PFS of multiple sites in the univariate analysis: 44.7% (95%CI: 34.1–55.3%) versus 13.9% (95%CI: 0–35.5%; P=0.03) (Figure 3A). In contrast, 3-year OS was 58.7% (95%CI: 47.9–69.5%) for EM1 versus 57.5% (95%CI: 34.2–80.8%; P=0.51) (Figure 3B).
Figure 3.
Progression-free survival (A) and overall survival (B) with numbers at risk of myeloma patients with extramedullary organ involvement following up-front autologous stem cell transplantation according to number of involvements: 1 and ≥ 2. EM: patients with extramedullary organ involvement; EM1: patients with one site of EM; EM2: patients with two or more sites of EM; N: number.
Tandem transplantation and survival
A landmark analysis was used to compare tandem and single ASCT, considering a total of 3139 patients who were alive at six months. In patients without EMD, the comparison of tandem versus single ASCT resulted in similar 3- year PFS, 53.8% (95%CI: 46.7–60.9) versus 51.3% (95%CI: 48.9–53.7; P=0.37), and similar 3-year OS: 84.7% (95%CI: 79.6–89.8) versus 81.6% (95%CI: 79.8–83.4; P=0.26).
Patients with EMD showed a 3-year PFS of 59.0% (95%CI: 46.3–71.8) after tandem versus 53.0% (95%CI: 47.5–58.6) after single (P=0.43) ASCT, while 3-year OS was 77.0% (95%CI: 66.1–87.9) versus 76.9% (95%CI: 72.4–81.4; P=0.91).
Within each EMD group, PS patients showed a similar 3- year PFS of 59.4% (95%CI: 45.3–73.6) after tandem versus 54.3% (95%CI: 48.0–60.5; P=0.44) after single ASCT and similar 3-year OS of 82.6% (95%CI: 72.3–92.8) versus 80.3% (95%CI: 75.6–85.1; P=0.88). Patients with EM involvement showed no significant difference in both 3- year PFS and OS after tandem versus single transplantation: 56.2% (95%CI: 27.2–85.3) versus 48.3% (95%CI: 36.6–60.1; P=0.98), and 52.0% (95%CI: 20.0–84.0) versus 64.9% (95%CI: 54.2–75.7; P=0.39).
Role of other factors on survival and causes of death
All patients in CR before first ASCT showed a significantly better 3-year PFS of 59.8% (95%CI: 55.3–64.3) compared to 30.7% (95%CI: 28.2–33.2) in PR and 24.7% (95%CI: 17.6–31.8; P<0.001) in less than PR. There was also a significant difference in 3-year OS, with patients in CR showing 83.6% (95%CI: 80.2–87.0) compared to 78.8% (95%CI: 76.9–80.6) in patients with PR and 27.8% (95%CI: 20.8–34.9) in patients with less than PR (P<0.001).
Other factors associated with worse PFS in patients with EMD were: older age (P=0.04), transplantation before 2011 (P=0.01), higher disease stage according to ISS (P=0.01) and Salmon and Durie (P=0.02), and lower remission status at transplantation (P<0.001). Factors associated with worse OS in EMD patients were: transplantation before 2011 (P=0.02), higher disease stage according to ISS (P=0.002) and Salmon and Durie (P=0.02), and lower remission status at transplantation (P<0.001).
Non-relapse mortality at three years occurred in 3.0% (95%CI: 2.0–4.0) of MM, 3.0% (95%CI: 2.0–5.0) of PS patients, and 7.0% (95%CI: 2.0–12.0) of EM patients (P=0.05). Main causes of death were relapse or progression (86.3%), infection (7.1%), secondary malignancy or post- transplant lymphoproliferative disorder (3.6%), organ damage or failure (1.8%), toxicity (0.4%), and unknown in 83 patients.
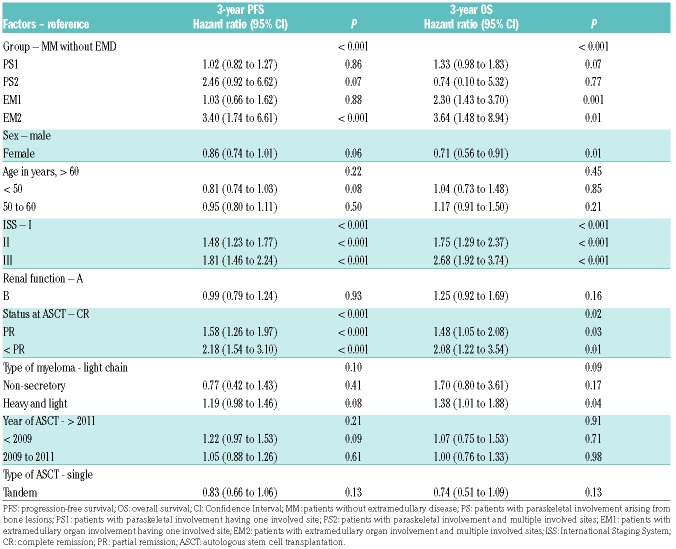
Multivariate analyses
A multivariable model was constructed to examine the effect of EMD on 3-year PFS and OS after adjusting for possible prognostic factors. All factors and covariates including corresponding references are listed in Table 3. To avoid linearly dependent covariates, we merged the disease group and the new variable of the number of involved sites into a 5-level variable consisting of patients without EMD (MM group) and patients with EMD according to number of involved sites (PS1, PS2, EM1 and EM2). Cox proportional hazards regression considering independent factors for worse PFS yielded significant results for EM2 with an HR of 3.40 (95%CI: 1.74–6.61; P<0.001). Interestingly, there was no difference in PFS in EM1 compared to MM with an HR of 1.03 (95%CI: 0.66–1.62; P=0.88). Comparison of PFS between PS and MM showed no difference for PS1, with an HR of 1.02 (95%CI: 0.83–1.27; P=0.86), and a less clear HR of 2.46 (95%CI: 0.92–6.62; P=0.07) for PS2.
Table 3.
Multivariate analysis.
In the OS analysis, EM1 and EM2 were associated with worse outcome, showing HRs of 2.30 (95%CI: 1.43–3.70; P=0.001) and 3.64 (95%CI: 1.48–8.94; P=0.01). The difference between patients with one site of PS involvement and those without EMD was less clear, with an HR of 1.33 (95%CI: 0.98–1.83; P=0.07), while PS2 resulted in a similar outcome with an HR of 0.74 (95%CI: 0.10–5.32; P=0.77).
Tandem ASCT showed similar 3-year PFS and OS compared to single ASCT, with HRs of 0.83 (95%CI: 0.66–1.06; P=0.13) and 0.74 (95%CI: 0.51–1.09; P=0.13). However, other factors made a significant contribution to an increased risk of worse outcome (Table 3). For PFS, these factors were: ISS stage II and III, PR and less than PR at ASCT. OS was significantly influenced by ISS stage II and III, male sex, PR and less than PR at ASCT, and the presence of heavy and light chains.
Discussion
Extramedullary disease in patients with MM is considered a poor prognostic factor. This EBMT registry study including 682 EMD patients identified an increase per year of EMD incidence at diagnosis from 2005 to 2014. We demonstrated that first-line ASCT resulted in at least similar 3-year PFS in patients with single sites of EMD compared to patients without EMD. Another finding, even though this was less clear, was that this translated into worse 3-year OS in single PS involvement while single sites of EM were significantly associated with worse outcome, which worsened still further when multiple sites of organs were involved. As far as treatment options for EMD at diagnosis are concerned, we found both first-line tandem and single ASCT resulted in similar 3-year PFS and OS.
Evidence on the role of EMD at diagnosis after first-line ASCT is still limited. A retrospective single center study30 of 27 patients concluded that ASCT might overcome poor prognosis at onset compared to patients without EMD, while another study showed extramedullary organ involvement in only 4 patients and that its impact on outcome could be under-estimated.5 A prospective study31 of patients in relapse with either soft-tissue or bone-related involvement at a single institution found that bone-related relapses were associated with better OS. However, treatments before diagnosis of extramedullary relapse significantly differed between groups. Since different types of involvement were reported, this variable was examined closely.
In our study, especially EM involvement in 139 MM patients was associated with lower rate of CR before and after ASCT, a higher frequency of ISS stage III, and worse renal function. Importantly, the impact of the number of involved sites on outcome in EMD at diagnosis had not previously been described. We found 20% of all EMD patients having multiple sites of involvement, which is in line with previous reports (16%).13 Notably, the location of further involvement was only paraskeletal in the PS group and was also restricted to other organs in the EM group.32
The use of radiation therapy might contribute to the difference in PFS and OS of patients with single sites of EMD compared to patients without EMD, because it is considered effective in reducing progression in patients with solitary osseous and extraosseous involvement,33,34 in particular because reports about the efficacy of novel agents in these cohorts at diagnosis are very limited. Some results would suggest an induction bortezomib-based regimen followed by high-dose melphalan/ASCT for patients with paraskeletal rather than extramedullary involvement.14,35–37 In a retrospective study38 investigating carfilzomib alone or in combination as salvage therapy in relapse, presence of extramedullary involvement resulted in shorter duration of response compared to absent EMD, suggesting limited treatment effect. Smaller reports on the possible impact of immunomodulatory drugs showed partial efficacy regarding response rates in EMD patients.10,39,40
Retrospective studies highlighted an extremely poor prognosis for CNS involvement with a median OS of less than six months.41,42 However, in addition to systemic anti- MM therapy, CNS irradiation and the use of novel combination therapies have been shown to improve the duration of response.42 With regard to these analyses outside transplantation settings, we investigated survival according to involved sites in EM patients, finding most of the patients had kidney, skin or lymph node involvement. After up-front ASCT, best outcomes were found in kidney and CNS involvement while skin and lymph node involvement showed worse outcome. Interestingly, our CNS cohort showed higher rates of OS compared to previous reports, which might be due to the selection of patients with CNS involvement at diagnosis, while most reports evaluated patients at later phases of the disease.41,42
A pooled analysis of prospective studies regarding transplantation strategies suggested the superiority of tandem ASCT in patients with poor prognostic features at diagnosis.4,43 Our landmark analyses of EMD patients who received either tandem or single ASCT as first-line therapy found no difference in PFS and OS. However, this analysis was conducted with the use of retrospective data and is, therefore, subject to the attendant limitations. Regression modeling and landmark analyses were performed as a means of controlling for differences between the patients, but such adjustment cannot account for all discrepancies in clinical and diagnostic characteristics between groups. The increasing incidence of EMD might be caused by a more frequent use of whole-body MRI or PET-CT in recent years. However, although recent evidence promotes the use of more sensitive imaging techniques,44 data are not routinely documented, and they are still not part of routine diagnostics and were thus not available in our study.45,46 A randomized trial is the only way to overcome these challenges and to assess the definite impact of EMD in newly diagnosed MM patients after ASCT.
In conclusion, this EBMT study identified an increase in incidence per year of EMD in newly diagnosed MM patients from 2005 to 2014. We revealed that first-line ASCT in patients with single sites of EMD (PS or EM) resulted in at least similar 3-year PFS compared to patients without EMD. Nevertheless, single EM involvement was associated with worse 3-year OS, which worsened still further when multiple sites of organs were involved.
Supplementary Material
Footnotes
Check the online version for the most updated information on this article, online supplements, and information on authorship & disclosures: www.haematologica.org/content/103/5890
References
- 1.National Cancer Institute. Surveillance epidemiology and end results program. SEER stat fact sheets: Myeloma. 2013; http://seer.cancer.gov/statfacts/html/mulmy.html [Last accessed 14 April 2017].
- 2.Kumar SK, Rajkumar SV, Dispenzieri A, et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood. 2008;111(5):2516–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palumbo A, Anderson K. Multiple myeloma. N Engl J Med. 2011; 364(11):1046–1060. [DOI] [PubMed] [Google Scholar]
- 4.Touzeau C, Moreau P. How I treat extramedullary myeloma. Blood. 2016; 127(8):971–976. [DOI] [PubMed] [Google Scholar]
- 5.Bladé J, Fernández de Larrea C, Rosiñol L, Cibeira MT, Jiménez R, Powles R. Soft-tissue plasmacytomas in multiple myeloma: incidence, mechanisms of extramedullary spread, and treatment approach. J Clin Oncol. 2011;29(28):3805–3812. [DOI] [PubMed] [Google Scholar]
- 6.Weinstock M, Aljawai Y, Morgan EA, et al. Incidence and clinical features of extramedullary multiple myeloma in patients who underwent stem cell transplantation. Br J Haematol. 2015;169(6):851–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cavo M, Terpos E, Nanni C, et al. Role of 18F-FDG PET/CT in the diagnosis and management of multiple myeloma and other plasma cell disorders: a consensus statement by the International Myeloma Working Group. Lancet Oncol. 2017;18(4):e206–e217. [DOI] [PubMed] [Google Scholar]
- 8.Bartel TB, Haessler J, Brown TL, et al. F18- fluorodeoxyglucose positron emission tomography in the context of other imaging techniques and prognostic factors in multiple myeloma. Blood. 2009; 114(10):2068–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Usmani SZ, Heuck C, Mitchell A, et al. Extramedullary disease portends poor prognosis in multiple myeloma and is overrepresented in high-risk disease even in the era of novel agents. Haematologica. 2012;97(11):4761–4767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Short KD, Rajkumar SV, Larson D, et al. Incidence of extramedullary disease in patients with multiple myeloma in the era of novel therapy and the activity of pomalidomide in extramedullary myeloma. Leukemia. 2011;25(6):906–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosiñol L, Fernández de Larrea C, Bladé J. Extramedullary myeloma spread triggered by surgical procedures: an emerging entity? Acta Haematol. 2014;132(1):36–38. [DOI] [PubMed] [Google Scholar]
- 12.Pérez-Simón JA, Sureda A, Fernández-Aviles F, et al. Reduced-intensity conditioning allogeneic transplantation is associated with a high incidence of extramedullary relapses in multiple myeloma patients. Leukemia. 2006;20(3):542–545. [DOI] [PubMed] [Google Scholar]
- 13.Varettoni M, Corso A, Pica G, Mangiacavalli S, Pascutto C, Lazzarino M. Incidence, presenting features and outcome of extramedullary disease in multiple myeloma: a longitudinal study on 1003 consecutive patients. Ann Oncol. 2010;21(2):325–330. [DOI] [PubMed] [Google Scholar]
- 14.Rosiñol L, Oriol A, Teruel AI, et al. Superiority of bortezomib, thalidomide, and dexamethasone (VTD) as induction pretransplantation therapy in multiple myeloma: a randomized phase 3 PETHEMA/GEMstudy. Blood. 2012;120(8):1589–1596. [DOI] [PubMed] [Google Scholar]
- 15.Usmani SZ, Rodriguez-Otero P, Bhutani M, Mateos MV, Miguel JS. Defining and treating high-risk myeloma. Leukemia. 2015;29(11):2119–2125. [DOI] [PubMed] [Google Scholar]
- 16.Sonneveld P, Avet-Loiseau H, Lonial S, et al. Treatment of multiple myeloma with high- risk cytogenetics: a consensus of the International Myeloma Working Group. Blood. 2016;127(24):2955–2962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cavo M, Rajkumar SV, Palumbo A, et al. International Myeloma Working Group consensus approach to the treatment of multiple myeloma patients who are candidates for autologous stem cell transplantation. Blood. 2011;117(23):6063–6073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bianchi G, Richardson PG, Anderson KC. Best Treatment Strategies in High-Risk Multiple Myeloma: Navigating a Gray Area. J Clin Oncol. 2014;32(20):2125–2132. [DOI] [PubMed] [Google Scholar]
- 19.Bladé J, Samson D, Reece D, et al. Criteria for evaluating disease response and progression in patients with multiple myeloma treated by high-dose therapy and haemopoietic stem cell transplantation. Myeloma Subcommittee of the EBMT. European Group for Blood and Marrow Transplant. Br J Haematol. 1998; 102(5):1115–1123. [DOI] [PubMed] [Google Scholar]
- 20.Greipp PR, San Miguel J, Durie BG, et al. International staging system for multiple myeloma. J Clin Oncol. 2005;23(15):3412–3420. [DOI] [PubMed] [Google Scholar]
- 21.Durie BG, Salmon SE. A clinical staging system for multiple myeloma. Correlation of measured myeloma cell mass with presenting clinical features, response to treatment, and survival. Cancer. 1975;36(3):842–854. [DOI] [PubMed] [Google Scholar]
- 22.Karnofsky DA, Abelmann WH, Craver LF, Burchenal JH. The Use of the Nitrogen Mustards in the Palliative Treatment of Carcinoma – with Particular Reference to Bronchogenic Carcinoma. Cancer. 1948;1(4):634–56. [Google Scholar]
- 23.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–481. [Google Scholar]
- 24.Schemper M, Smith TL. A note on quantifying follow-up in studies of failure time. Control Clin Trials. 1996;17(4):343–346. [DOI] [PubMed] [Google Scholar]
- 25.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. [Google Scholar]
- 26.Gray RJ. A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16(3):1141–1154. [Google Scholar]
- 27.Iacobelli S, EBMT Statistical Committee. Suggestions on the use of statistical methodologies in studies of the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant. 2013;48(Suppl 1):S1–37. [DOI] [PubMed] [Google Scholar]
- 28.Klein JP, Moeschberger ML. (eds): Survival Analysis: Techniques for Censored and Truncated Data, 2nd edn. Springer-Verlag: New York, USA, 2003. [Google Scholar]
- 29.Cox DR: Regression models and life tables. J R Stat Soc B. 1972;34(2):187–220. [Google Scholar]
- 30.Lee SE, Kim JH, Jeon YW, et al. Impact of extramedullary plasmacytomas on outcomes according to treatment approach in newly diagnosed symptomatic multiple myeloma. Ann Hematol. 2015; 94(3):445–452. [DOI] [PubMed] [Google Scholar]
- 31.Pour L, Sevcikova S, Greslikova H, et al. Soft-tissue extramedullary multiple myeloma prognosis is significantly worse in comparison to bone-related extramedullary relapse. Haematologica. 2014;99(2):360–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghobrial IM. Myeloma as a model for the process of metastasis: implications for therapy. Blood. 2012;120(1):20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu K, Yahalom J. Radiotherapy in the management of plasma cell tumors. Oncology (Williston Park). 2000;14(1):101–108. [PubMed] [Google Scholar]
- 34.Terpos E, Morgan G, Dimopoulos MA, et al. International Myeloma Working Group Recommendations for the Treatment of Multiple Myeloma–Related Bone Disease. J Clin Oncol. 2013;31(18):2347–2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paubelle E, Coppo P, Garderet L, et al. Complete remission with bortezomib on plasmocytomas in an end-stage patient with refractory multiple myeloma who failed all other therapies including hematopoietic stem cell transplantation: possible enhancement of graft-vs-tumor effect. Leukemia. 2005;19(9):1702–1704. [DOI] [PubMed] [Google Scholar]
- 36.Sonneveld P, Goldschmidt H, Rosiñol L, et al. Bortezomib-based versus nonbortezomib-based induction treatment before autologous stem-cell transplantation in patients with previously untreated multiple myeloma: a meta-analysis of phase III randomized, controlled trials. J Clin Oncol. 2013;31(26):3279–3287. [DOI] [PubMed] [Google Scholar]
- 37.Mateos MV, Oriol A, Matínez-López J, et al. Bortezomib, melphalan, and prednisone versus bortezomib, thalidomide, and prednisone as induction therapy followed by maintenance treatment with bortezomib and thalidomide versus bortezomib and prednisone in elderly patients with untreated multiple myeloma: a randomised trial. Lancet Oncol. 2010;11(10):934–941. [DOI] [PubMed] [Google Scholar]
- 38.Muchtar E, Gatt ME, Rouvio O, et al. Efficacy and safety of salvage therapy using Carfilzomib for relapsed or refractory multiple myeloma patients: a multicentre retrospective observational study. Br J Haematol. 2016;172(1):89–96. [DOI] [PubMed] [Google Scholar]
- 39.Calvo-Villas JM, Alegre A, Calle C, et al. Lenalidomide is effective for extramedullary disease in relapsed or refractory multiple myeloma. Eur J Haematol. 2011;87(3):281–284. [DOI] [PubMed] [Google Scholar]
- 40.Rosiñol L, Cibeira MT, Bladé J, et al. Extramedullary multiple myeloma escapes the effect of thalidomide. Haematologica. 2004;89(7):832–836. [PubMed] [Google Scholar]
- 41.Nieuwenhuizen L, Biesma DH. Central nervous system myelomatosis: review of the literature. Eur J Haematol. 2008;80(1):1–9. [DOI] [PubMed] [Google Scholar]
- 42.Chen CI, Masih-Khan E, Jiang H, et al. Central nervous system involvement with multiple myeloma: long term survival can be achieved with radiation, intrathecal chemotherapy, and immunomodulatory agents. Br J Haematol. 2013;162(4):483–488. [DOI] [PubMed] [Google Scholar]
- 43.Cavo M, Salwender H, Rosiñol L, et al. Double vs single autologous stem cell transplantation after bortezomib-based induction regimens for multiple myeloma: an integrated analysis of patient-level data from phase European III studies. Blood. 2013;122:767. [Google Scholar]
- 44.Moreau P, Attal M, Caillot D, et al. Prospective evaluation of magnetic resonance imaging and [18F] Fluorodeoxyglucose positron emission tomography-computed tomography at diagnosis and before Maintenance Therapy in Symptomatic Patients With Multiple Myeloma Included in the IFM/DFCI 2009 Trial: Results of the IMAJEM Study. J Clin Oncol. 2017; 35(25):2911–2918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328–346. [DOI] [PubMed] [Google Scholar]
- 46.Pawlyn C, Fowkes L, Otero S, et al. Whole- body diffusion-weighted MRI: a new gold standard for assessing disease burden in patients with multiple myeloma? Leukemia. 2016;30(6):1446–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.