Highlights
-
•
Nodular Fasciitis, also known as infiltrative or pseudosarcomatous fasciitis, is a benign soft tissue tumour of fibroblastic/myofibroblastic differentiation.
-
•
Magnetic Resonance Imaging was done and showed an irregular mass in the right axilla in the muscular- subcutaneous plane measuring 10.8 × 8.8 × 12 cm.
-
•
Positive staining with alpha smooth muscle actin(SMA) is a feature of nodular fasciitis suggesting a myofibroblastic differentiation and less possibility of a sarcoma.
-
•
Treatment options include, observation, as spontaneous regression has been reported, intra-lesional steroid or wide local excision.
-
•
Magnetic Resonance Imaging along with histopathology and immunohistochemistry are key to diagnosis.
Keywords: Nodular fasciitis, Magnetic resonance imaging, Magnetic resonance angiogram, Muscular-subcutaneous plane, Histopathological, Case report
Abstract
Introduction
Nodular Fasciitis, also known as infiltrative or pseudosarcomatous fasciitis, is a benign soft tissue tumour of fibroblastic/myofibroblastic differentiation, that was first described in 1955 by Konwaler et al.
Presentation of case
This is a case report of a 27-year old male with complaints of a swelling in the right axilla for 2 and ½ years measuring 12 cm × 10 cm. Chest X-Ray was normal. Magnetic Resonance Imaging of the right arm and chest showed an irregular mass in the axilla in the muscular-subcutaneous plane measuring 10.8 cm × 8.8 cm × 12 cm, with no neural involvement. Magnetic Resonance Angiogram showed feeders from the branches of the Right Subclavian and Right Axillary Artery and venous drainage into the Right Subclavian Vein. USG guided biopsy was done which showed benign spindle cell neoplasm. Patient underwent wide local excision under general anesthesia. The specimen was sent for histopathological examination which showed histological and immunohistochemical features in favour of Nodular Fasciitis.
Discussion
Most nodular fasciitis lesions are solitary and occur in adults 20–40 years of age. Nodular fasciitis affects both men and women with equal frequency. Differential diagnosis of nodular fasciitis includes, fibrosarcoma, fibroma, fibrous histiocytoma, and desmoids and histopathology and immunohistochemistry play a key role in identifying the condition.
Conclusion
Owing to the size, location and findings of the Magnetic Resonance Angiogram we initially suspected a Soft Tissue Sarcoma, but to our surprise, on further investigation the mass was revealed to be Nodular Fasciitis.
1. Introduction
Nodular Fasciitis, also known as infiltrative or pseudosarcomatous fasciitis, is a benign soft tissue tumour of fibroblastic/myofibroblastic differentiation, that was first described in 1955 by Konwaler et al. [1]. The lesion often comes to clinical attention when the patient presents with a rapidly growing, occasionally painful, palpable soft tissue mass [[2], [3]]. Although nodular fasciitis is well accepted as a self-limited reactive process and not a true neoplasm, its precise etiology is unknown [4]. Most lesions are solitary and occur in adults 20–40 years of age [[5], [6], [7]]. Nodular fasciitis affects both men and women with equal frequency. It is found most commonly in the forearm (27%–29%), back or chest wall (15%–18%), and upper arm (12%) [[5], [6], [7]]. Patients may develop paresthesia if the mass exerts pressure on a peripheral nerve. Making a correct diagnosis of nodular fasciitis is important because of its striking resemblance to a soft tissue sarcoma. Magnetic Resonance Imaging and histopathological examination, along with the clinical features, are the key to diagnosis. This case was managed in an academic setting. I hereby declare that my work has been reported in line with the SCARE criteria [17].
2. Case presentation
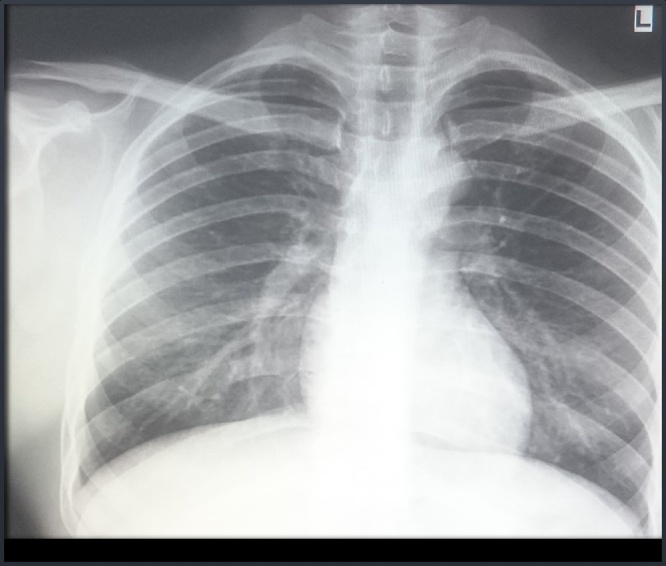
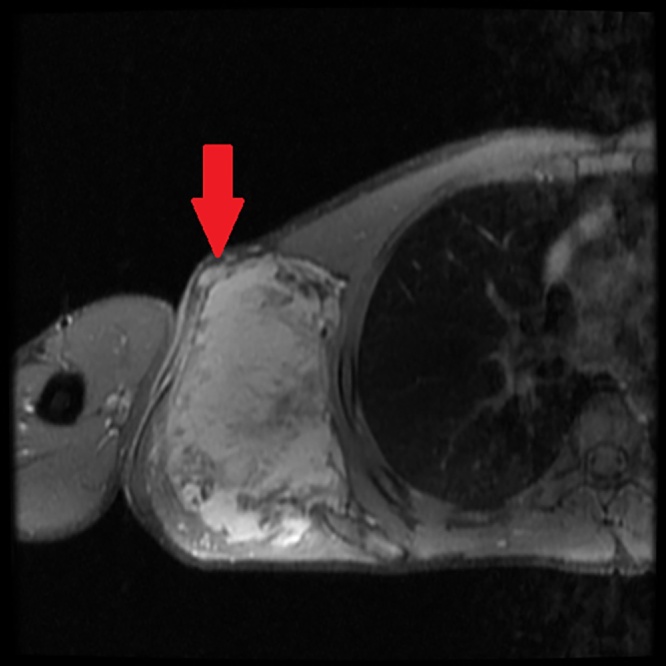
A 27-year-old male came to our hospital with complaints of a swelling in the right axilla for 2 and ½ years. It was insidious in onset and progressive in nature. The patient denied any history of pain, trauma, fever or weight loss. On examination, the swelling measured 12 cm × 10 cm, extending to the lateral border of the right scapula posteriorly, to the chest wall medially, to the apex of the axilla superiorly and to the 6th intercostal space inferiorly (Fig. 1). There was no warmth or tenderness noted. Skin over the swelling was normal and the surface was nodular. Dilated blood vessels were present over the surface of the swelling (Fig. 2). There were no visible pulsations, no discharge and no scars or sinuses. Movement of the shoulder joint was normal. The swelling was hard in consistency and not mobile. There were no palpable axillary or cervical lymph nodes. Baseline blood investigations were normal. Chest X-ray was normal and showed no osteolytic lesions of the right ribs or scapula (Fig. 3). Magnetic Resonance Imaging was done and showed an irregular mass in the right axilla in the muscular- subcutaneous plane measuring 10.8 × 8.8 × 12 cm. This mass was attached to the lateral border of scapula (Fig. 4) and displaced the subscapularis anteriorly. The infraspinatus, teres minor and teres major muscles were displaced posteriorly (Fig. 5). The lesion appeared iso to hyperintense to muscle on T1 and heterogeneously hyperintense on T2-weighted images. Multiple scattered areas of hemorrhage were noted within. The neurovascular bundle was seen displaced cranially. The lesion abutted the median, radial, ulnar nerves and axillary vessels in few sections. The lesion abutted the serratus anterior on the medial aspect.
Fig. 1.
Pre-operative image of the swelling.
Fig. 2.
Pre-operative image of the swelling showing vascularity.
Fig. 3.
Chest X-Ray showing no osteolytic lesions.
Fig. 4.
MRI showing an irregular mass in the musculo-subcutaneous plane.
Fig. 5.
MRI showing an irregular mass displacing infraspinatus, teres minor, and teres major muscles posteriorly. Multiple, scattered areas of hemorrhage noted within.
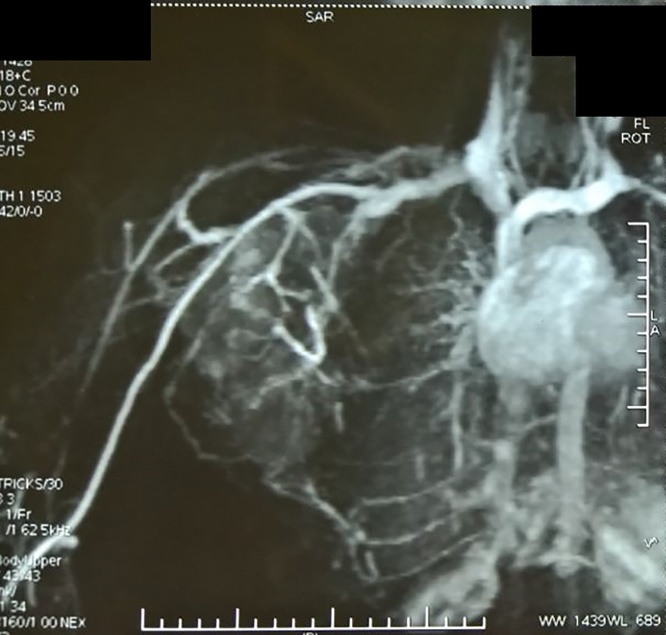
Magnetic Resonance Angiogram showed feeders from the branches of right subclavian and axillary arteries and venous drainage into the right subclavian vein (Fig. 6).
Fig. 6.
Magnetic Resonance Angiogram showing feeders.
Ultrasound guided biopsy was done which showed benign spindle cell neoplasm possibly of fibrous origin with moderate to abundant collagen and no evidence of cytological atypia/increased mitosis or necrosis.
Patient underwent Wide Local Excision under General Anesthesia (Fig. 7). Intra-operatively, the tumour was found to be adherent to the scapula posteriorly and to the latissmus dorsi laterally. It abutted the axillary vessels and nerves cranially. The tumour was completely excised (Fig. 8) and sent for histopathology. Histopathological examination showed a well circumscribed, encapsulated spindle cell lesion. The cells were arranged in irregular bundles and fascicles along with a small amount of mature collagen. These cells appeared to be plump, immature myofibroblasts and fibroblasts. Periphery of the lesion showed muscle giant cells, mitosis 2/10HPF. There was no evidence of necrosis. Immunohistochemistry showed that the tumour cells were positive for Vimentin, focally positive for Smooth Muscle Actin(SMA) and negative for S100 and CD34. Ki67 labelling index was less than 1%. Post-operative period was uneventful. The patient had full range of movement of the right shoulder. The wound was healthy and the drain was removed on post-operative day 6. The skin staplers were removed on post-operative day 10.
Fig. 7.
Intra-operative image of the tumour.
Fig. 8.
Post-operative image of the specimen after wide local excision.
3. Discussion
Nodular fasciitis, with characteristic pseudosarcomatous features, is considered a benign, reactive fibroblastic growth [1]. Most lesions are solitary and occur in adults 20–40 years of age [[5], [6], [7]]. Nodular fasciitis affects both men and women with equal frequency. It is found most commonly in the forearm (27%–29%), back or chest wall (15%–18%), and upper arm (12%) [[5], [6], [7]]. Pathologically nodular fasciitis is an unencapsulated lesion that is typically well demarcated from the surrounding uninvolved tissue but may be focally infiltrative [8]. Although most cases of nodular fasciitis are centered in the fascia, they can also be dermal, subcutaneous, deep-fascial, intermuscular, intramuscular, and intravascular [[9], [10], [11], [12]].
Nodular fasciitis is often misdiagnosed as a soft tissue sarcoma, which is the most important pathological differential diagnosis of this condition. Plaza et al. [13] reported that 2/3rd of their cases had been misdiagnosed as sarcoma. Histopathological examination and Magnetic Resonance Imaging is the key to diagnosis of nodular fasciitis. Cytological diagnosis can be very challenging, but immunohistochemistry helps in giving an accurate diagnosis. The histological findings are similar to those observed in sarcoma but are differentiated by plump, immature looking fibroblasts, in short irregular bundles and fascicles. Positive staining with alpha smooth muscle actin(SMA) is a feature of nodular fasciitis (as noted in our case), suggesting a myofibroblastic differentiation and less possibility of a sarcoma. Desmin, which is positive in various soft tissue sarcomas is often negative in nodular fasciitis.
On Magnetic Resonance Imaging, nodular fasciitis has been described as inhomogeneous, hypointense to muscle on T1-weighted images, and hyperintense to fat on T2-weighted images, with variable enhancement [[2], [9], [14], [15]].
Differential diagnosis of nodular fasciitis includes, fibrosarcoma, fibroma, fibrous histiocytoma, and desmoids and histopathology and immunohistochemistry play a key role in identifying the condition.
Treatment options include, observation, as spontaneous regression has been reported [16], intra-lesional steroid or wide local excision (as done in our case). Recurrence after excision is very rare.
4. Conclusion
There is a need for awareness of nodular fasciitis as it is often misdiagnosed as a sarcoma due to is rapid growth, rich cellularity, high mitotic activity and poorly circumscribed nature. Large lesions, like in our case, are often mistaken for a malignant lesion and further investigation is needed to prove the benign nature of the disease. Magnetic Resonance Imaging along with histopathology and immunohistochemistry are needed to overcome the challenges of making a diagnosis of nodular fasciitis. Close clinical follow-up is mandatory in all cases.
Conflicts of interest
None.
Funding
None.
Ethical approval
Ethical approval has been exempted by our institution since it is a Single Case Report.
Consent
Consent obtained in the usual manner.
Author contribution
Vatsal Khanna – Writing the paper, Data collection.
Manikandan Rajan – Study concept.
Trishya Reddy – Data collection.
Naveen Alexander – Data interpretation.
Parmasivam Surendran – Final editing.
Guarantor
Dr. Parmasivam Surendran.
Dr. Naveen Alexander.
Contributor Information
Vatsal Khanna, Email: vatsal_khanna@yahoo.com.
Manikandan Rajan, Email: doctorrs28@gmail.com.
Trishya Reddy, Email: reddy92@gmail.com.
Naveen Alexander, Email: naveenalexander@yahoo.co.in.
Parmasivam Surendran, Email: drsuru@yahoo.com.
References
- 1.Konwaler B.E., Keasbey L., Kaplan L. Subcutaneous pseudosarcomatous fibromatosis (fasciitis) Am. J. Clin. Pathol. 1955;25:241–252. doi: 10.1093/ajcp/25.3.241. [DOI] [PubMed] [Google Scholar]
- 2.Nikolaidis P., Gabriel H.A., Lamba A.R., Chan N.G. Sonographic appearance of nodular fasciitis. J. Ultrasound Med. 2006;25:281–285. doi: 10.7863/jum.2006.25.2.281. [DOI] [PubMed] [Google Scholar]
- 3.Bernstein K.E., Lattes R. Nodular (pseudosarcomatous) fasciitis, a nonrecurrent lesion: clinicopathologic study of 134 cases. Cancer. 1982;49:1668–1678. doi: 10.1002/1097-0142(19820415)49:8<1668::aid-cncr2820490823>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 4.Shimizu S., Hashimoto H., Enjoji M. Nodular fasciitis: an analysis of 250 patients. Pathology. 1984;16(April (2)):161–166. doi: 10.3109/00313028409059097. (PubMed) [DOI] [PubMed] [Google Scholar]
- 5.Bernstein K.E., Lattes R. Nodular (pseudosarcomatous) fasciitis, a nonrecurrent lesion: clinicopathologic study of 134 cases. Cancer. 1982;49(April (8)):1668–1678. doi: 10.1002/1097-0142(19820415)49:8<1668::aid-cncr2820490823>3.0.co;2-9. (PubMed) [DOI] [PubMed] [Google Scholar]
- 6.Brimhall C.L., Segura A.D., McTigue M.K., Esterly N.B. Nodular fasciitis on the palm of a child. Arch. Dermatol. 1989;125(October (10)):1441–1442. doi: 10.1001/archderm.125.10.1441. (PubMed) [DOI] [PubMed] [Google Scholar]
- 7.Stout A.P. Pseudosarcomatous fasciitis in children. Cancer. 1961;14(November–December):1216–1222. doi: 10.1002/1097-0142(196111/12)14:6<1216::aid-cncr2820140611>3.0.co;2-w. (PubMed) [DOI] [PubMed] [Google Scholar]
- 8.Tomita S., Thompson K., Carver T., Vazquez W.D. Nodular fasciitis: a sarcomatous impersonator. J. Pediatr. Surg. 2009;44(5):e17–e19. doi: 10.1016/j.jpedsurg.2009.01.047. (PubMed) [DOI] [PubMed] [Google Scholar]
- 9.Dinauer P.A., Brixey C.J., Moncur J.T., Fanburg-Smith J.C., Murphey M.D. Pathologic and MR imaging features of benign fibrous soft-tissue tumors in adults. Radiographics. 2007;27:173–187. doi: 10.1148/rg.271065065. [DOI] [PubMed] [Google Scholar]
- 10.Coyle J., White L.M., Dickson B., Ferguson P., Wunder J., Naraghi A. MRI characteristics of nodular fasciitis of the musculoskeletal system. Skeletal Radiol. 2013;42:975–982. doi: 10.1007/s00256-013-1620-9. [DOI] [PubMed] [Google Scholar]
- 11.Gelfand J.M., Mirza N., Kantor J. Nodular fasciitis. Arch. Dermatol. 2001;137:719–721. [PubMed] [Google Scholar]
- 12.Bancroft L.W., Peterson J.J., Kransdorf M.J., Nomikos G.C., Murphey M.D. Soft tissue tumors of the lower extremities. Radiol. Clin. North Am. 2002;40:991–1011. doi: 10.1016/s0033-8389(02)00033-7. [DOI] [PubMed] [Google Scholar]
- 13.Plaza J.A., Mayerson J., Wakely P.E., Jr. Nodular Fasciitis of the hand: a potential diagnostic pitfall in fine-needle aspiration cytopathology. Am. J. Clin. Pathol. 2005;123:388–393. doi: 10.1309/PWD0-HB51-1L3V-R56W. (PubMed) [DOI] [PubMed] [Google Scholar]
- 14.Kransdorf M.J. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJR Am. J. Roentgenol. 1995;164:395–402. doi: 10.2214/ajr.164.2.7839977. [DOI] [PubMed] [Google Scholar]
- 15.Leung L.Y., Shu S.J., Chan A.C., Chan M.K., Chan C.H. Nodular fasciitis: MRI appearance and literature review. Skeletal Radiol. 2002;31:9–13. doi: 10.1007/s002560100411. [DOI] [PubMed] [Google Scholar]
- 16.Mardi K., Sharma J., Kaur H. Nodular fasciitis of the hand – a potential diagnostic pitfall in fine needle aspiration cytology. J. Cytol. 2007;24(4):197. [Google Scholar]
- 17.R.A. Agha, A.J. Fowler, A. Saetta, I. Barai, S. Rajmohan, D.P. Orgill, the SCARE Group, The SCARE statement: consensus-based surgical case report guidelines, Int. J. Surg. [DOI] [PubMed]