Highlights
-
•
Mesenteric hematoma is a rare condition without specific symptoms.
-
•
Rivaroxaban is not affect to the value of PT or APTT.
-
•
It is difficult to diagnose mesenteric hematoma.
Abbreviations: PT, prothrombin time; PT-INR, prothrombin time-international normalized ratio; APTT, activated partial thromboplastin time; CT, computed tomography; IVR, interventional radiography; LCA, left colic artery; SRA, superior rectal artery; DOAC, direct oral anticoagulant
Keywords: Mesenteric hematoma, Sigmoid colon, Anticoagulation, Rivaroxaban
Abstract
Introduction
Mesenteric hematoma is a rare condition caused by bleeding localized in the mesenteric vascular tree. This is a first report of spontaneous mesenteric hematoma caused by rivaroxaban.
Presentation of case
The patient was a 71-year-old man who had taken rivaroxaban for paroxysmal atrial fibrillation. He had experienced abdominal pain and diarrhea for the prior 3 days. He had little melena and was referred to our institute. He presented with hypotension on arrival. Computed tomography (CT) revealed a 10 cm mass in the mesentery of the sigmoid colon with extravasation. Active bleeding from the sigmoid colic arteries was embolized with angiography on the day of admission. On the second day, we operated on the patient. We detected 200 mL of bloody ascites accumulated in the abdomen. The serosa of the sigmoid colon was ruptured along the tenia due to the compression of the hematoma in the mesentery. The sigmoid colon was resected and a descending colostomy was reconstructed. Operative and pathological findings did not reveal the cause of bleeding. We finally diagnosed the patient with spontaneous mesenteric hematoma associated with rivaroxaban.
Discussion
Previous reports of mesenteric hematoma with anticoagulant were associated with warfarin. Since rivaroxaban is not affect to the value of prothrombin time (PT) and activated partial thromboplastin time (APTT) and mesenteric hematoma presents non-specific symptoms, it is difficult to diagnose mesenteric hematoma in the patients taking rivaroxaban.
Conclusion
It is important to keep in mind that mesenteric hematoma is one of the critical complications in patients taking rivaroxaban.
1. Introduction
Mesenteric hematoma is a rare condition caused by localized bleeding in the mesenteric vascular tree of a bowel segment. It occurs as a direct result of abdominal trauma [1]. Non-traumatic mesenteric hematoma is associated with mesenteric vascular disease. Spontaneous mesenteric hematoma is diagnosed as a hematoma that does not satisfy these clinical or pathological features and is potentially associated with collagen diseases, anticoagulants, and other diseases such as Crohn’s disease [[2], [3]].
Here, we present a case of mesenteric hematoma in a patient who had been taking rivaroxaban, a direct inhibitor of Factor Xa. The cases of spontaneous mesenteric hematoma associated with anticoagulant previously reported were mainly caused by warfarin [[4], [5], [6], [7]]. To our knowledge, this case is first report of mesenteric hematoma associated with rivaroxaban. This work has been reported according to CARE guidelines 2016 [8].
1.1. Presentation of case
The patient was a 71-year-old man with paroxysmal atrial fibrillation. He had taken rivaroxaban for anticoagulation and had been experiencing diarrhea for the prior 3 days. He had no history of abdominal trauma. The practitioner initially diagnosed the patient with enterocolitis. However, he had melena and was referred to our institution. The patient showed lower abdominal swelling and slight rebound tenderness. Hematoma was not confirmed in the abdominal wall. The patient had no clinical symptoms of bowel obstruction. We could not confirm the presence of melena when he arrived at our hospital. His blood pressure was 67/47 mmHg, heart rate 96 bpm, and body temperature 38.4 °C. Initial blood examinations showed a hemoglobin level of 9.3 g/dL, white blood cell count of 13900/μL, platelet count of 143 × 103/μL, C-reactive protein level of 5.0 mg/dL, PT of 53.5%, PT- INR of 1.4, APTT of 47.6 s, and bleeding time of 4 min.
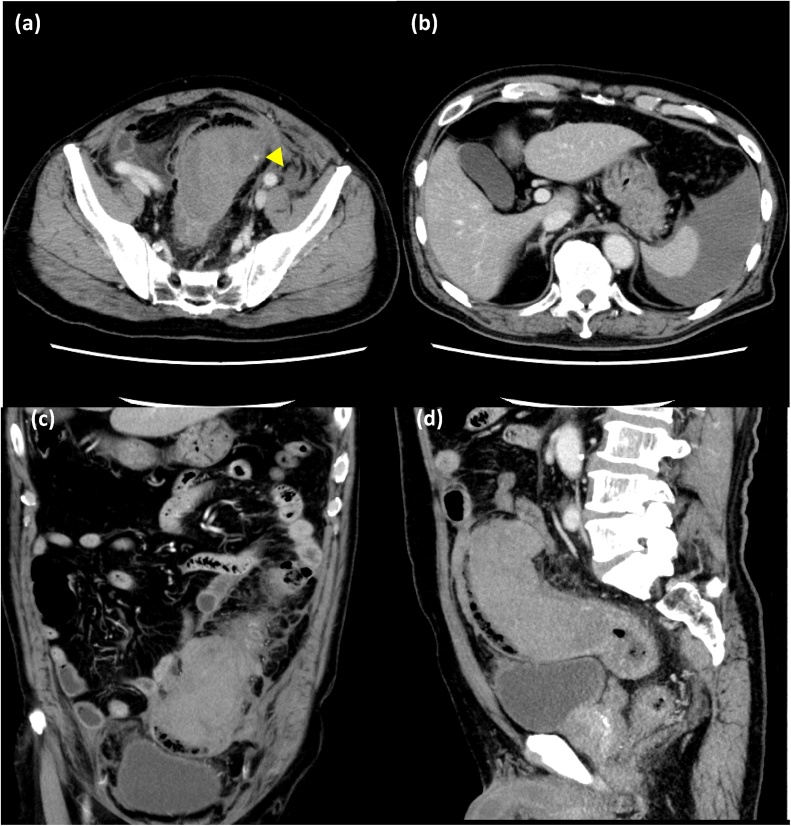
Contrast-enhanced CT showed a low-density round mass with a maximum diameter of 10 cm adjacent to the sigmoid colon. The lumen of the sigmoid colon became narrow due to the mass. Small extravasations were confirmed in the mass. Abdominal fluid was accumulated around the spleen and was still expanding (Fig. 1).
Fig. 1.
Computed tomography findings.
Computed tomography revealed a low-density mass close to the sigmoid colon, with a 10 cm diameter, and ascites accumulated around the spleen. Small extravasations were confirmed in the mass (arrows).
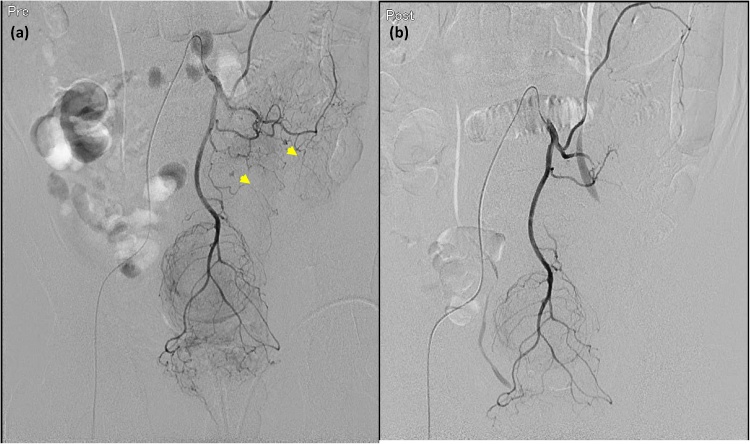
We initially diagnosed the patient with intraabdominal bleeding from the sigmoid arteries and obstruction of sigmoid colon due to the mass. Emergency IVR was performed on the day of admission. Sigmoid arteriography revealed small active bleeding, and embolization was performed in the sigmoid arteries while preserving the left colic artery (LCA) and superior rectal artery (SRA) (Fig. 2).
Fig. 2.
Interventional radiography findings.
Angiography from the inferior mesenteric artery revealed small extravasations in the region of the sigmoid colic arteries (arrows). The sigmoid colic arteries were embolized while preserving the left colic artery and superior rectal artery and the extravasations disappeared (b).
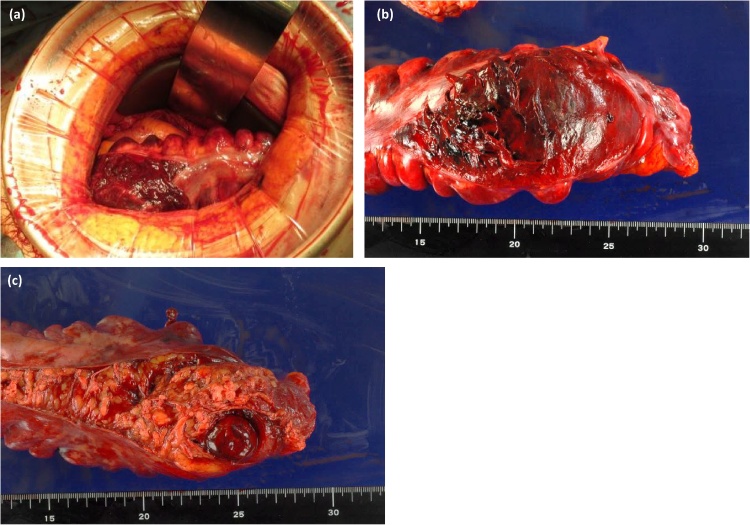
The operation was performed on the second hospital day. During surgery, 200 mL of bloody ascites were found in the abdomen. A 10 × 8 cm hematoma was located in the mesentery of the sigmoid colon. The sigmoid colon was compressed by the hematoma and the anterior serosa of the sigmoid colon was ruptured along the tenia. The bleeding from the ruptured serosa was halted (Fig. 3).
Fig. 3.
Intraoperative findings and specimens.
During surgery, 200 mL of bloody ascites were found to be accumulated in the abdomen. The serosa of the sigmoid colon was ruptured without active bleeding (a). The hematoma was localized in the mesentery of the sigmoid colon and the anterior serosa was ruptured due to the compression of the hematoma (b, c).
The mesentery of the sigmoid colon was resected close to the wall of the colon. Then, the sigmoid colon was resected while preserving the LCA and SRA since the marginal arteries of sigmoid colon were occluded with IVR. A descending colostomy was constructed. Anti-coagulation was re-started at post-operative day (POD) 1 and rivaroxaban was started at POD 3. The patient was discharged on postoperative day 16 with no significant complications.
The resected specimen indicated hematoma in the mesentery (Fig. 3b, c). The mucosa had collapsed partially and bleeding was found in the colon wall. The etiology of bleeding was not diagnosed by histopathological findings.
2. Discussion
Mesenteric hematoma is a rare clinical condition directly caused by abdominal trauma, including postoperative complications. Non-traumatic cases are associated with mesenteric vascular diseases such as aneurysm and vasculitis. Spontaneous mesenteric hematoma is diagnosed if these clinical or pathological findings are not confirmed. Spontaneous mesenteric hematoma is potentially caused by anti-coagulation therapy, connective tissue diseases such as Ehlers-Danlos syndrome, and other diseases including Crohn’s disease and incarcerated inguinal hernia [[2], [3]]. The responsible vessels are mostly the superior mesenteric arteries. Suzuki et al. published a review of 36 spontaneous mesenteric hematoma cases in Japan. The locations of the hematomas were the superior mesenteric artery (61%), inferior mesenteric artery (19%), and unknown origin (19%), respectively [9]. In the present case, angiography revealed active bleeding from the peripheral arteries of the sigmoid colic artery and no aneurysms in the responsible region. Pathological findings also suggested no significant lesions capable of causing mesenteric hematoma. We finally diagnosed the patient with spontaneous mesenteric hematoma in the sigmoid colon, which was potentially caused by anti-coagulation therapy.
Mesenteric hematoma presents with non-specific symptoms: abdominal pain, vomiting, abdominal masses, diarrhea, and melena. Increasing bleeding can lead to hypotension [[2], [9], [10]]. In the present case, the patient presented with diarrhea and melena. The hematoma compressed the sigmoid colon and occluded the lumen. The extension of the colon caused rupture of the serosa and mucosa. The patient then presented with melena and intraabdominal bleeding.
Mesenteric hematoma can be treated with non-operative methods if the hemorrhage can be controlled [10]. In contrast, in the present case, the patient had hypotension, intraabdominal bleeding, and bowel obstruction and underwent surgical resection of the intestine. Angiography is also useful for the diagnosis of the origin of bleeding and prevention or alleviation of hypotension.
In the present case, the patient used rivaroxaban for paroxysmal atrial fibrillation. Warfarin, a vitamin K antagonist, is available for the prevention of ischemic stroke in patients with atrial fibrillation. However, warfarin is affected by multiple foods, drug, and pharmacogenomic interactions and requires maintenance within therapeutic INR. In recent years, direct oral anticoagulants (DOACs), including apixaban, edoxaban, rivaroxaban, and dabigatran, have become available for anticoagulation therapy. The patient in this case used rivaroxaban, which was a direct inhibitor of Factor Xa. In the J-ROCET AF study, which evaluated the safety of rivaroxaban compared to warfarin in Japanese people, the rate of gastrointestinal bleeding in the rivaroxaban group (1.1%) tended to be lower than that in the warfarin group (2.3%). No cases of critical gastrointestinal or intraabdominal bleeding were reported [11]. Previous reports regarding mesenteric hematoma or intraluminal hematoma due to warfarin are scarce [[4], [5], [6], [7]]. On the other hand, mesenteric hematoma associated with rivaroxaban are not reported yet. In warfarin-associated mesenteric hematoma, INR values were higher than the therapeutic range in previous reports. However, since DOACs do not affect PT and APTT, it is difficult to diagnose mesenteric hematoma when patients taking DOAC experience non-specific abdominal symptoms. The patient in the present case was initially diagnosed with enterocolitis. Since he presented with hypotension and little melena, CT was performed and he was diagnosed with mesenteric hematoma. It is difficult but important to diagnose mesenteric hematoma before the patient presents with hypotension. Rivaroxaban is associated with fewer bleeding complications than warfarin. However, it is important to keep in mind that mesenteric hematoma is one of the critical complications in patients with non-specific abdominal symptoms who have been exposed to rivaroxaban.
3. Conclusion
Mesenteric hematoma is a rare clinical condition with non-specific symptoms and a potential critical complication in patients taking rivaroxaban. It is important to diagnose mesenteric hematoma before patients present with a severe clinical state, such as bowel obstruction or hypotension.
Conflict of interests
All authors declare that we have no conflict of interests.
Sources of funding
None.
Ethical approval
The ethical approval has been obtained in our institute.
Informed consent
We obtained the written consent for publication this report from the patient.
Author contribution
HK managed the patient and wrote this manuscript. BT, OS, and ST supported the operation and the treatment of the patient. OT helped in drafting the manuscript. FT totally supervised this case report. All authors read and approved the final manuscript.
Guarantor
Katsuhisa Hirano
Acknowledgement
None.
Contributor Information
Katsuhisa Hirano, Email: hrnkths@med.u-toyama.ac.jp.
Tadashi Bando, Email: bando@saiseikai-toyama.jp.
Soshi Osawa, Email: soshi74@yahoo.co.jp.
Tetsuro Shimizu, Email: shimitetsu@gmail.com.
Tomoyuki Okumura, Email: okumura@med.u-toyama.ac.jp.
Tsutomu Fujii, Email: fjt@med.u-toyama.ac.jp.
References
- 1.Kubota T., Mizokami K., Shimaguchi M., Katagiri H., Okumura K., Yoshikawa K., Sakamoto T. A occult transverse laceration with only mesenteric hematoma: no free air, no ascitic fluid, no bowel thickening in CT do not give us a guarantee in which surgically important bowel injury is absent. HSOA J. Emerg. Med. Trauma Surg. Care. 2016;3:015. [Google Scholar]
- 2.Kappikeri V.S., Akshay K., Vinayak I. Haematoma in the mesentery of terminal ileum and intramural haematoma of caecum, ascending colon with hemoperitoneum due to abdominal massage. RGUHS Med. Sci. 2017;7:38–39. [Google Scholar]
- 3.Shikata D., Nakagomi H., Takano A., Nakagomi T., Watanabe H., Maruyama M., Nakada H., Yamamoto A., Furuya K., Hada M., Miyasaka Y., Omata M., Oyama T. Report of a case with a spontaneous mesenteric hematoma that ruptured into the small intestine. Int. J. Surg. Case Rep. 2016;24:124–127. doi: 10.1016/j.ijscr.2016.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaiteerakij R., Treeprasertsuk S., Mahachai V., Kullavanijaya P. Anticoagulant-induced intramural intestinal hematoma: report of three cases and literature review. J. Med. Assoc. Thail. 2008;91:1285–1290. [PubMed] [Google Scholar]
- 5.Bekheit M., AlaaSallam M., Khafagy P.A., Corder R., Katri K. Non-traumatic intramural hematomas in patients on anticoagulant therapy: report of three cases and overview of the literature. Afr. J. Emerg. Med. 2014;4:e1–e4. [Google Scholar]
- 6.Ou Yang C.M., Hsiao T.F., Chou Y.H., Chang J.S., Chen T.H. Spontaneous intramural small-bowel hematoma due to a rare complication of warfarin therapy: report of two cases. J. Acute Med. 2014;4:45–48. [Google Scholar]
- 7.Moftah M., Cahill R., Johnston S. Spontaneous sublingual and intramural small-bowel hematoma in a patient on oral anticoagulation. Gastroenterol. Insights. 2012;4:73–75. [Google Scholar]
- 8.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., The SCARE Group S. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;(34):180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 9.Iwata T., Muto Y., Hokama A., Kurihara K., Sho Y., Miyagi M., Matayoshi M. Mesenteric hematoma of the sigmoid colon: a case report and a review of the literature in Japan. Rukyu Med. J. 1985;8(2):73–80. [Google Scholar]
- 10.Parker S.G., Thompson J.N. Spontaneous mesenteric hematoma; diagnosis and management. BMJ Case Rep. 2012;(August) doi: 10.1136/bcr-2012-006624. published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hori M., Matsumoto M., Tanahashi N., Momomura S., Uchiyama S., Goto S., Izumi T., Koretune Y., Kajikawa M., Kato M., Ueda H., Iwamoto K., Tajiri M. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation – the J-ROCKET AF study –. Circ. J. 2012;76:2014–2111. doi: 10.1253/circj.cj-13-1324. [DOI] [PubMed] [Google Scholar]