Highlights
-
•
We present a case of Idiopathic scrotal calcinosis, rare benign tumor.
-
•
Controversy concerning the origin of ICS remains, whether the nodules are the result of dystrophic calcification of preexistent epidermal inclusion cysts or if they have emerged de novo.
-
•
Idiopathic scrotal calcinosis can be sexually invalidating.
-
•
Golden standard in surgical excision.
Keywords: Idiopathic scrotal calcinosis, Case report, Epidermal inclusion cyst
Abstract
Introduction
Idiopathic scrotal calcinosis is a rare benign condition which presents with asymptomatic multiple nodules on the scrotal skin.
Presentation of case
Our patient, a 64-year-old Indian male with Fitzpatrick skin type 4, presented with multiple nodules, which were completely surgically excised with no complications. Histological examination reveals extensive intradermal deposition of calcium surrounded by histiocytes and without cystic structure.
Discussion
Numerous theories about the pathogenesis have been proposed and the evidence presented suggests this is a continuum.
Conclusion
The nature of idiopathic scrotal calcinosis is still unknown and it is up to debate whether the term “idiopathic” is appropriate for the condition.
1. Introduction
Idiopathic scrotal calcinosis (ISC) is a rare benign condition, characterized by multiple intradermal monomorphic nodules on the scrotum without the presence of any underlying systemic metabolic disease [[1], [2], [3]] e.g. scleroderma and dermatomyositis [[4], [5]]. To the authors knowledge only 86 individual publications of ISC have been described in the PubMed. The condition was first described by Lewinski in 1883 [6].
ISC often presents in the third decade of life. The condition may progress over several years before the patient consults a medical professional [[1], [3]], due to the indolent and painless nature of these tumors on the scrotum.
The typical appearance includes rock-hard white nodules on the scrotal skin. Even though most of the cases are asymptomatic and patients often seek medical advice for cosmetic reasons, some complain with pruritus, soreness and white-chalky exudate from the nodules accompanied with secondary infection of the skin [[1], [2], [7]].
Differential diagnoses include epidermal inclusion cysts, steatocystoma, lipoma, angiokeratoma, solitary neurofibroma, genital leiomyoma, scleroderma especially in patients with CREST syndrome (Calcinosis cutis, Raynaud phenomena, Esophageal dysfunction, Sclerodactyly and Teleangiectasia), dermatomyositis especially the juvenile subtype, pilomatricoma and scabies in nodular variant [[1], [3], [8], [9], [10], [11]].
Epidermal inclusion cysts appear as non-tender, firm dome-shaped skin-colored nodules sometimes with a dilated central pore and surrounding scarring, some authors suggest these can develop into ICS over time [12]. Steatocystomas in contrast to ICS are characterized by skin-colored soft nodules ranging 1–3 cm in diameter. Fordyce angiokeratomas are often darker then ICS with red to purple, 2–5 mm in diameter papules with surrounding erythema of the scrotal skin. Solitary genital leiomyomas arise from the dartoic muscle tissue and appear as single or multiple firm and non-tender pink to red-brown papules, they appear deeper in the tissue then ICS. In particular one should consider CREST as a relevant differential diagnosis because calcinosis cutis is seen in 25–40% [5] of the cases predilected to fingers and pressure points. It presents clinically as rock-hard nodules that may exude white chalky material similar to ICS. In dermatomyositis 30% of the adult cases and 70% [11] of the cases with juvenile dermatomyositis represent with subcutaneous yellow-white nodules, plaques and ulceration. Unlike ICS the typical locations include knees and elbows.
The golden standard for treatment is an elliptical excision of the nodule above dartos fascia, as the nodules are localized within the dermis. Primary closure of the wound is often achievable because of the skin laxity [[7], [14]].
The final diagnosis of ISC is made by excisional biopsy and histopathologic evaluation, which reveals the presence of calcified deposits of varying size in the dermis that may be surrounded by histiocytes and inflammatory giant cell reaction. Partial epithelial lining around the calcified deposits may be visible in some cases. This is a distinctive form of epidermal inclusion cysts because of the epithelial lining [13]. This case is reported in line with the SCARE criteria [14].
2. Case
A 64-year-old Indian male with Fitzpatrick skin type 4 was referred to the plastic surgery department from a local dermatologist with 5 scrotal nodules. The lesions had gradually increased in size during the last 2 decades without causing any symptoms or discomfort besides cosmetic reasons. There was no relevant history of previous or actual medical condition. Laboratory examination including serum calcium, phosphorus, thyroid hormone, creatinine, urea, sodium, potassium and alkaline phosphatase levels showed no abnormality.
Physical examination (Fig. 1) revealed 5 prominent flesh/white colored firm and non-tender nodules within the scrotal skin that measured up to 10 mm in diameter. There were no areas of ulceration, discharge or infection. The remaining skin was without any remarks.
Fig 1.
Firm flesh-colored nodules within the scrotal dermis before and after surgery.
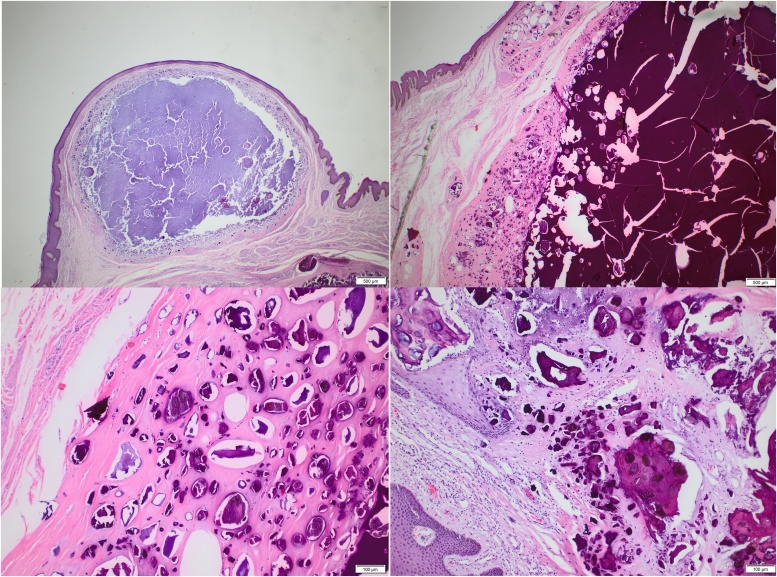
Excisional biopsy of 1 nodule was done for microscopic examination. The histopathological evaluation revealed the presence of calcium deposits with periinflammation and without cyst walls representative of the diagnosis ISC (Fig. 2).
Fig. 2.
Upper left. Hematoxylin and eosin stain (HE) of complete nodule. Upper right: HE stain revealed numerous amorphous calcified areas within the dermis. Lower left: Close look at calcified deposits. Lower right: Resection shows epidermis, dermis and subcutis. Epidermis shows hyperplastic epithelium with basal hyperpigmentation. In the underlying dermis and subcutis, numerous size variant of calcified deposits. There are no epithelial or melanocytic changes. No evidence of malignancy.
The remaining nodules were excised subsequently. The postoperative course was uneventful and there was no observed recurrence after a 6-month follow-up period.
3. Discussion
The pathogenesis of ISC remains unclear and numerous theories have been proposed [1]. Controversy concerning the origin of ICS remains, whether the nodules are the result of dystrophic calcification of preexistent epidermal inclusion cysts or if they have emerged de novo without any triggering metabolic condition, infiltration of foreign body material or induced by trauma.
Shapiro et al. [13] proposed the idiopathic nature of the condition after histopathologic evaluation of 14 cases with ISC that demonstrated no cyst wall structure. Other studies have subsequently supported this hypothesis [[1], [16], [17]].
In contrast some studies found evidence of epithelial lining. Swinehart et al. [12] examined 3 cases with scrotal epidermoid cysts in varying stages of inflammation appearing concurrently with scrotal calcinosis. Although coincidental calcinosis formation and epidermoid cyst formation could not be excluded, the authors postulated that ISC might represent inflammation associated with dystrophic calcification, which destroys the cyst walls. Song et al. [18] found cyst wall structure in various stages of inflammation with calcification in 51 nodules from the same case. Shah et al. [2] found cyst walls in 14 out of 20 cases.
Dubey et al. [3] evaluated 100 cases with ISC, in which 53% of the cases revealed inflamed cysts containing calcific material with an intact cyst wall structure and 11% with a partial cyst wall structure.
No cyst wall formation was observed in our case, which is similar to other reported cases. This could be a result of most patients undergoing surgery several years after the initial presentation. Thus only the calcified deposits remained.
The pathogenesis is still controversial and it is up to debate whether the term “idiopathic” is appropriate for the condition.
Conflicts of interest
None of the authors have any conflict of interests to declare.
Funding
No funding
Ethical approval
No ethical approval needed.
Consent
The patient in the manuscript has signed a written consent.
Author contributions
Ali Tareen: Drafted the first version of the manuscript and critical revision of the manuscript for important intellectual content.
Rami Mossad Ibrahim: Critical revision of the manuscript for important intellectual content
Guarantor
Ali Tareen
Acknowledgement
The authors thank Dr. Lene Sjø from Department of Pathology Rigshospitalet for assisting in preparing pathology photos.
References
- 1.Lei X., Liu B., Wu J. Idiopathic scrotal calcinosis: report of two cases and review of literature. Int. J. Dermatol. 2012;51(2):199–203. doi: 10.1111/j.1365-4632.2011.04922.x. [DOI] [PubMed] [Google Scholar]
- 2.Shah V., Shet T. Scrotal calcinosis results from calcification of cysts derived from heir follicles: a series of 20 cases evaluating the spectrum of changes resulting in scrotal calcinosis. Am. J. Dermatopathol. 2007;29:172–175. doi: 10.1097/01.dad.0000246465.25986.68. [DOI] [PubMed] [Google Scholar]
- 3.Dubey S., Sharma R., Maheshwari V. Scrotal calcinosis: idiopathic or dystrophic? Dermatol. Online J. 2010;16(February 15 (2)):5. [PubMed] [Google Scholar]
- 4.Walsh, Fairley Calcifying disorders of the skin. J. Am. Acad. Dermatol. 1995;33:693–706. doi: 10.1016/0190-9622(95)91803-5. [DOI] [PubMed] [Google Scholar]
- 5.Reiter, El-Shabrawi, Leinweber Calcinosis cutis: part I. Diagnostic pathway. J. Am. Acad. Dermatol. 2011;65:1–12. doi: 10.1016/j.jaad.2010.08.038. [DOI] [PubMed] [Google Scholar]
- 6.Lewinski H.M. Lymphangiome der Haut mit Verkalklem Inhalt. Arch Pathol Anat. 1883;91:371–374. [Google Scholar]
- 7.Pompeo A., Molina W., Pohlman G. Idiopathic scrotal calcinosis: a rare entity and a review of the literature. Can Urol Assoc J. 2013;7(5-6):E439–41. doi: 10.5489/cuaj.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silver R.M. Clinical aspects of systemic sclerosis (scleroderma) Ann. Rheum. Dis. 1991;50(Suppl 4):854–861. doi: 10.1136/ard.50.suppl_4.854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yencha M.W. Head and neck pilomatricoma in the pediatric age group: a retrospective study and literature review. Int. J. Pediatr. Otorhinolaryngol. 2001;57(2):123–128. doi: 10.1016/s0165-5876(00)00449-3. [DOI] [PubMed] [Google Scholar]
- 10.Ichiki Y., Akiyama T., Shimozawa N., Kondo N., Kitajima Y. An extremely severe case of cutaneous calcinosis with juvenile dermatomyositis, and successful treatment with diltiazem. Br. J. Dermatol. 2001;144(4):894–897. doi: 10.1046/j.1365-2133.2001.04153.x. [DOI] [PubMed] [Google Scholar]
- 11.Sallum A.M., Pivato F.C., Doria-Filho U., Aikawa N.E., Liphaus B.L., Marie S.K., Silva C.A. Risk factors associated with calcinosis of juvenile dermatomyositis. J. Pediatr. 2008;84(1):68–74. doi: 10.2223/JPED.1746. [DOI] [PubMed] [Google Scholar]
- 12.Swinehart J.M., Golitz L.E. Scrotal calcinosis: dystrophic calcification of epidermoid cysts. Arch. Dermatol. 1982;118:985–988. doi: 10.1001/archderm.118.12.985. [DOI] [PubMed] [Google Scholar]
- 13.Shapiro L., Platt N., Torres-Rodriguez V.M. Idiopathic calcinosis of the scrotum. Arch. Dermatol. 1979;102:199–204. [PubMed] [Google Scholar]
- 14.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016 doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 16.Wright S., Navsaria H., Leigh I.M. Idiopathic scrotal calcinosis is idiopathic. J. Am. Acad. Dermatol. 1991;24:727–730. doi: 10.1016/0190-9622(91)70110-n. [DOI] [PubMed] [Google Scholar]
- 17.Saladi R.N., Persaud A.N., Phelps R.G., Cohen S.R. Scrotal calcinosis: is the cause still unknown. J. Am. Acad. Dermatol. 2004;51:S97–101. doi: 10.1016/j.jaad.2004.01.039. [DOI] [PubMed] [Google Scholar]
- 18.Song D., Lee K.H., Kang W.H. Idiopathic calcinosis of the scrotum: histopathologic observations of fifty-one nodules. J. Am. Acad. Dermatol. 1988;19:1095–1101. doi: 10.1016/s0190-9622(88)70278-9. [DOI] [PubMed] [Google Scholar]