Abstract
We aim to evaluate the association of systolic and diastolic blood pressure (SBP and DBP) with estimated urinary sodium (Na) and potassium(K) excretions, and their gram-to-gram Na/K ratio across various salt-diet regions during 2005–2009 in China. A prospective cohort study was conducted to recruit 46,285 participants in China. A single fasting morning urine specimen was collected to estimate 24-hour urinary Na and K excretion using Kawasaki formula. Means of estimated Na and K were 5.7 ± 1.7 and 2.1 ± 0.5 grams/day, respectively, and mean estimated Na/K ratio was 2.8 ± 0.8. Adjusted analyses showed 1.70 mmHg SBP and 0.49 mmHg DBP increase per 1-g increment of estimated Na, while 1.10 mmHg SBP and 0.91 mmHg DBP decrease for one-gram increase of K. A significant increase in SBP (4.33 mmHg) and DBP (1.54 mmHg) per 1 unit increase in Na/K ratio was observed. More changes of SBP (4.39 mmHg) and DBP (1.67 mmHg) per one-unit increase of Na/K ratio were observed in low-salt regions, though significant changes were also found in moderate- and heavy-salt regions (P for heterogeneity < 0.01). Conclusively, decreasing sodium combined with increasing potassium is likely to have a more beneficial effect than decreasing sodium alone, even if those were living in low-salt regions.
Introduction
Hypertension is a major risk factor for cardiovascular diseases, chronic renal impairments, and mortality1–4. A diet lower in sodium and higher in potassium consumption is recommended for reducing the risk of hypertension and potentially cardiovascular diseases5–12. A positive association between sodium intake and blood pressure was shown in different populations and regions of the world13–15, including our ProspectiveUrban and Rural Epidemiology (PURE) study, a large, international, prospective cohort study16. In addition, a number of studies found that certain subpopulations such as older individuals, people with obesity, and hypertensive individuals show greater BP increases in response to higher sodium intake15–18. Conversely, higher potassium intake has been shown to mitigate BP response to higher sodium intake19.
In the PURE study, in which China representedalmost half of cohort (42%), mean sodium excretion was markedly higher than countries from other parts of the world (5.6 vs. 4.5 grams per day)16. It was also found that the slope of the association between sodium excretion and BP became increasingly steeper at higher levels of sodium excretion (ie, <3 g/day, 3 to 5 g/day, and >5 g/day)16. Currently, no country on earth consumes the recommended amount of sodium (ie, <2.3 g/day, or lower). This recmmendation may be particularly ineffective in China, where average intake exceeds 5 g/day in most areas of the country. Therefore, adding potassium in table salt is recommened to Chinese7,20. China is known to having various local cultures and customs. Different areas within China have different levels of salt intake, from high sodium intake in Jiangxi Province and to more moderate amounts of sodium in Xinjiang Province, Shanxi Province. PURE-China recruited participants from communities in 12 out of 31 provinces, municipalities, autonomous regionsrepresenting a diverse range of salt intake from very high to moderate levels of intake across the country21,22. Salt restriction in China has decreased mean daily salt intake from 12.0 in 2002 to 9.6 grams in 2012 (10.9 to 9.0 grams in urban areas and 12.4 to 10.2 gram in rural areas), but these national survey in China calculated daily salt intake via dietary questionnaires23,24. Our primary aim was to evaluate the association patterns of 24-hour estimated sodium and potassium excretion using spot urine sample, and their gram-to-gram ratio (sodium vs. potassium) with blood pressure in overall PURE-China study and in different salt classified regions from National Dietary Survey in 200223.
Methods
Study design and participants
As an important part of global multi-center international, community-based cohort study called as prospective urban and rural epidemiological (PURE) study from 17 countries across five continents25, baseline recruitments were conducted during 2005–2009 with almost 1:1 urban-to-rual recruitmen proportion in 12 provinces,municipalities, autonomous regions of China, involving 46,285 Chinese aged 35–70 years residing in 115 urban and rural communities. Detailed description for PURE-China were reported elsewhere22,26. Briefly, provinces and communities were selected per economic and socio-cultural diversity across regions to achieve long-term follow-ups for at least 10 years with high-quality data collection at modest budget. Three-level cluster sampling was performed to enroll potential participants, including province, community, and household. The protocol and informed consent were reviewed and approved by the institutional review board at Fuwai Hospital of Chinese Academy of Medical Sciences and Beijing Hypertension League Institute. All methods were performed in accordance with the relevant guidelines and regulations.
Data collection
All households in the selected communities were enrolled, if they had at least one member aged between 35 and 70 years and intended to stay at the current address for more than four years. Written informed consent forms were provided before questionnaire interview, physical examination and sample collection. Socio-demographic, self-reported disease history (such as hypertension, diabetes, stroke, and angina, heart attack, and coronary artery diseases), tobacco use, alcohol consumption, and physical activities were collected via a structured questionnaire, and physical examination was conducted to collect weight, height, hip circumference, waist circumference, systolic blood pressure and diastolic blood pressure by trained physicians for each participant. Two blood pressure (BP) readings were taken on the right arm using an Omron automatic digital BP monitor (Omron HEM-757, OMRON Healthcare, Scarborough, ON, Canada), which was provided to all the centers. An appropriate size cuff was selected and centered over the brachial artery. Subjects had to rest for at least 5 minutes prior to measurement without smoking, exercising, eating, or climbing stairs within 30 minutes. Both systolic and diastolic BPs were recorded. The means of the two measures were used for our analyses.
A single fasting midstream urine specimen was collected for each participant in the morning of recruitment day, which was frozen at −20 to −70 °C and then delivered to the study center lab in Beijing for the analyses of sodium (Na+), potassium (K+), and creatinine (Cr)16. The former two were examined by emission flame photometry and the latter one by the Jaffe methods. The Kawasaki formula27 was used to estimate 24-hour urinary sodium and potassium excretion as surrogates for sodium and potassium intake.
Statistical analyses
The Statistical Analysis System (SAS 9.4 for Windows; SAS Institute Inc., Cary, NC, USA) software was used for all statistical analyses in this study. Only baseline data were used for analyses. Continuous variables were shown as the mean ± standard deviation (SD), and categorical variables as numbers (n) and percentages (%).
The changes in systolic and diastolic blood pressure per 1 g (43.5 mmol) of sodium excretion or 1 g (25.6 mmol) of potassium excretion were calculated in multivariable linear regressions adjusted for gender, age, education level, salt-diet regions, body mass index (BMI), and alcohol intake. The linear regressions were used to estimate the association of the gram-to-gram ratio for urinary sodium-to-potassium with blood pressure adjusting for the above-mentioned covariates. Systolic/diastolic blood pressure (SBP/DBP) ≥ 140/90 mmHg or self-reported hypertension history or having blood pressure medication was defined as prevalent hypertension. Multivariate logistic regressions were conducted to analyze the associations of hypertension risk with urinary sodium, potassium, and ratio of sodium to potassium.
The effect of sodium or potassium or their ratio on blood pressure or hypertension risk was further assessed at different levels of sodium (<5, 5–6, >6 g/day) or potassium (<1.8, 1.8–2.2, >2.2 g/day), or sodium-to-potassium ratio (<2.3, 2.3–3.0, >3.0). Three regions were divided by daily salt intake according to National Dietary Survey in 2002, which was conducted using multi-stage random cluster sampling method and 272,023 population were screened across 31 administrative regions23. For example, more than 8 grams of daily salt intake was defined as heavy-salt region (Beijing, Jiangsu Province, Jiangxi Province, and Liaoning Province), 7 to 8 g as moderate-salt region (Qinghai Province, Shaanxi Province, and Shandong Province), less than 7 grams as low-salt region (Inner Mongolia, Sichuan Province, and Yunnan Province, Shanxi Province, and Xinjiang Province). Subgroup analyses based on various salt-diet regions were conducted to evaluate above-mentioned associations. Mixed linear models were used to evaluate heterogeneity across subgroup analyses, such as various salt regions, sodium groups, potassium groups, and their ratio groups.
Results
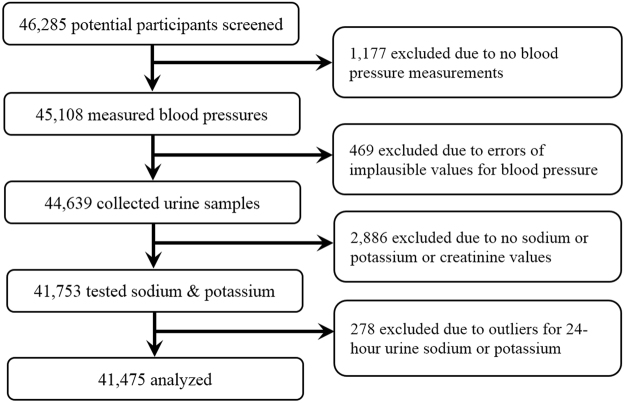
Between 2005 and 2009, PURE-China screened and recruited a total of 46,285 participants, and 1,177 were excluded due to missing values of blood pressure measurements. In order to analyze the associations between blood pressure and uriary sodium/potassium levels, 469 were deleted due to outliers for blood pressure (i.e. SBP < 70 or >260 mmHg and DBP < 40 or >140 mmHg), 2,886 due to no sodium and/or potassium and/or creatinine values; and 278 due to outlers for 24-hour urine sodium or potassium (i.e. sodium > 12 g/day and potassium > 4 g/day). Finally, 41,475 were used for analyses (Fig. 1).
Figure 1.
Flow chart of participant selection.
Among 41,475 participants, more females were enrolled (59.2%) and mean age were 51.4 ± 9.4 years old (ranged from 35 to 70). 16,882 lived in heavy-salt regions (Beijing, Jiangsu Province, Jiangxi Province, and Liaoning Province), 12,851 in moderate-salt regions (Qinghai Province, Shaanxi Province, and Shandong Province), and 11,742 in low-salt regions (Inner Mongolia, Sichuan Province, and Yunnan Province, Shanxi Province, and Xinjiang Province). Participants in heavy-salt regions were 2 years older than those in other two regions (52.3 vs. 50.9 formoderate-salt and 50.5 for low-salt regions). More participants had college degree or higher in low-salt regions (14.5%) than heavy- and moderate-salt regions (6.2% and 6.8%). The mean of 24-hour urinary sodium exertion was the highest in moderate-salt regions (6.1 ± 1.8 g/day, equal to 15.3 gram salt intake), next heavy-salt regions (5.5 ± 1.6 g/day, equal to 13.8 grams salt intake), then low-salt regions (5.3 ± 1.6 g/day, equal to 13.3 gram salt intake), while the mean of 24-hour urinary potassium excertion was the same across various salt-diet regions (2.1 ± 0.5 g/day). Gram-to-gram ratio for urinary sodium vs. potassium excretion also was the highest in moderate-salt regions (3.0 ± 0.8), compared with heavy-salt regions (2.7 ± 0.7) and low-salt regions (2.6 ± 0.7). Both SBP and DBP were the highest in moderate-salt regions (SBP, 137.0 ± 22.5 mmHg; DBP, 84.1 ± 12.7 mmHg), and hypertension prevalence was 47.4%, which were much higher than heavy-salt regions (42.8%), low-salt regions (39.3%). More details can be found in Table 1.
Table 1.
Characteristics of the eligible participants in the Sodium and Potassium Study from PURE-China Cohort.
| Characteristics | % (n) | |||
|---|---|---|---|---|
| Total (n = 41,475) | Heavy-salt regions1 (n = 16,882) | Moderate-salt regions1 (n = 12,851) | Low-salt regions1 (n = 11,742) | |
| Female sex | 59.2 (24,546) | 60.1 (10,153) | 56.8 (7,295) | 60.5 (7,098) |
| Age at recruitment (years, mean ± STD) | 51.4 ± 9.4 | 52.3 ± 8.9 | 50.9 ± 9.6 | 50.5 ± 9.8 |
| Education level | ||||
| Less than high school graduate | 33.7 (13,973) | 28.9 (4,870) | 39.7 (5,104) | 34.1 (3,999) |
| High school graduate | 57.3 (23,765) | 64.7 (10,916) | 53.2 (6,840) | 51.2 (6,009) |
| Some college or more | 8.7 (3,608) | 6.2 (1,040) | 6.8 (868) | 14.5 (1,700) |
| Missing values | 0.3 (129) | 0.3 (56) | 0.3 (39) | 0.3 (34) |
| Body mass index (BMI, kg/m2, mean ± STD) | 24.6 ± 4.0 | 24.8 ± 4.0 | 24.6 ± 3.8 | 24.5 ± 4.0 |
| <25 | 54.8 (22,723) | 53.6 (9,054) | 56.0 (7,190) | 55.2 (6,479) |
| 25-29.9 | 35.4 (14,677) | 36.2 (6,108) | 35.32 (4,542) | 34.3 (4,027) |
| ≥ 30 | 7.1 (2,955) | 7.8 (1,310) | 6.4 (821) | 7.0 (824) |
| Missing values | 2.7 (1,120) | 2.4 (410) | 2.3 (298) | 3.5 (412) |
| Waist-to-hip ratio (WHR, mean ± STD) | 0.86 ± 0.07 | 0.86 ± 0.07 | 0.86 ± 0.06 | 0.86 ± 0.08 |
| > 0.9 for men or > 0.85 for women | 42.5 (17,605) | 41.8 (7,049) | 44.2 (5,685) | 41.5 (4,871) |
| Sodium excretion2 (g/day, mean ± STD) | 5.7 ± 1.7 | 5.5 ± 1.6 | 6.1 ± 1.8 | 5.3 ± 1.6 |
| <3 | 3.5 (1,447) | 3.8 (648) | 1.9 (243) | 4.7 (556) |
| 3-5 | 34.3 (14,211) | 36.0 (6,082) | 25.7 (3,299) | 41.1 (4,830) |
| > 5 | 62.3 (25,817) | 60.1 (10,152) | 72.4 (9,309) | 54.1 (6,356) |
| Potassium excretion2 (g/day, mean ± STD) | 2.1 ± 0.5 | 2.1 ± 0.5 | 2.1 ± 0.5 | 2.1 ± 0.5 |
| <1.9 | 36.5 (15,148) | 37.7 (6,356) | 34.8 (4,473) | 36.8 (4,319) |
| 1.9-2.5 | 44.9 (18,625) | 45.5 (7,675) | 45.0 (5,778) | 44.1 (5,172) |
| > 2.5 | 18.6 (7,702) | 16.9 (2,851) | 20.2 (2,600) | 19.2 (2,251) |
| Ratio for sodium vs. potassium2 (mean ± STD) | 2.8 ± 0.8 | 2.7 ± 0.7 | 3.0 ± 0.8 | 2.6 ± 0.7 |
| <2.0 | 15.1 (6,244) | 15.8 (2,660) | 10.2 (1,314) | 19.3 (2,270) |
| 2.0-3.0 | 51.7 (21,453) | 52.6 (8,880) | 46.8 (6,011) | 55.9 (6,562) |
| > 3.0 | 33.2 (13,778) | 31.6 (5,342) | 43.0 (5,526) | 24.8 (2,910) |
| Creatinine excretion3 (g/day, mean ± STD) | 1.2 ± 0.3 | 1.2 ± 0.3 | 1.3 ± 0.3 | 1.2 ± 0.3 |
| Systolic blood pressure (mmHg, mean ± STD) | 133.5 ± 22.0 | 132.3 ± 21.6 | 137.0 ± 22.5 | 131.2 ± 21.7 |
| <120 | 28.6 (11,856) | 30.2 (5,097) | 22.3 (2,864) | 33.2 (3,895) |
| 120-139 | 38.0 (15,764) | 38.2 (6,449) | 38.8 (4,981) | 36.9 (4,334) |
| ≥ 140 | 33.4 (13,855) | 31.6 (5,336) | 39.0 (5,006) | 29.9 (3,513) |
| Diastolic blood pressure (mmHg, mean ± STD) | 82.8 ± 12.3 | 82.3 ± 11.9 | 84.1 ± 12.7 | 82.2 ± 12.2 |
| <60 | 1.3 (552) | 1.3 (222) | 1.4 (177) | 1.3 (153) |
| 60-89 | 72.7 (30,148) | 74.4 (12,556) | 68.7 (8,828) | 74.6 (8,764) |
| ≥ 90 | 26.0 (10,775) | 24.3 (4,104) | 35.7 (3,846) | 24.1 (2,825) |
| Self-reported hypertension or had blood pressure medication or blood pressure ≥ 140/90 mmHg | ||||
| No | 56.8 (23,555) | 57.2 (9,664) | 52.6 (6,759) | 60.7 (7,132) |
| Yes | 43.2 (17,920) | 42.8 (7,218) | 47.4 (6,092) | 39.3 (4,610) |
| Self-reported diabetes or fasting glucose >7.0 mmol/L | ||||
| No | 90.8 (37,661) | 89.6 (15,124) | 92.3 (11,862) | 90.9 (10,675) |
| Yes | 9.2 (3,814) | 10.4 (1,758) | 7.7 (989) | 9.1 (1,067) |
| Self-reported stroke | ||||
| No | 97.9 (40,596) | 97.7 (16,488) | 98.1 (12,604) | 98.0 (11,504) |
| Yes | 1.9 (785) | 2.1 (362) | 1.6 (200) | 1.9 (223) |
| Missing values | 0.2 (94) | 0.2 (32) | 0.4 (47) | 0.1 (15) |
| Self-reported angina, heart attack or coronary artery diseases | ||||
| No | 93.7 (38,855) | 94.6 (15,968) | 92.7 (11,915) | 93.4 (10,972) |
| Yes | 6.3 (2620) | 5.4 (914) | 7.3 (936) | 6.6 (770) |
| Tobacco use | ||||
| Never | 72.3 (30,003) | 69.3 (11,702) | 77.4 (9,944) | 71.2 (8,357) |
| Former | 4.7 (1,964) | 4.4 (748) | 3.6 (468) | 6.4 (748) |
| Current | 21.8 (9,060) | 24.6 (4,153) | 18.4 (2,359) | 21.7 (2,548) |
| Missing values | 1.1 (448) | 1.7 (279) | 0.6 (80) | 0.8 (89) |
| Alcohol consumption | ||||
| Never | 75.4 (31,290) | 73.3 (12,376) | 81.4 (10,454) | 72.0 (8,460) |
| Former | 3.2 (1,329) | 2.6 (433) | 2.2 (285) | 5.2 (611) |
| Current | 20.8 (8,620) | 23.1 (3,902) | 16.2 (2,081) | 22.5 (2,637) |
| Missing values | 0.6 (236) | 1.0 (171) | 0.2 (31) | 0.3 (34) |
| Levels of physical activities | ||||
| Low | 12.2 (5,049) | 12.1 (2,036) | 13.7 (1,763) | 10.7 (1,250) |
| Medium | 41.7 (17,311) | 43.8 (7,398) | 43.9 (5,646) | 36.3 (4,267) |
| High | 41.6 (17,250) | 40.8 (6,886) | 37.2 (4,779) | 47.6 (5,585) |
| Missing values | 4.5 (1,865) | 3.3 (562) | 5.2 (663) | 5.5 (640) |
| Total cholesterol (mmol/L, mean ± STD) | 4.7 ± 1.0 | 4.7 ± 1.0 | 4.6 ± 1.0 | 4.8 ± 1.1 |
| ≥6.47 | 4.0 (1,642) | 3.4 (576) | 3.4 (442) | 5.3 (624) |
| Triglycerides (mmol/L, mean ± STD) | 1.6 ± 1.2 | 1.5 ± 1.2 | 1.6 ± 1.2 | 1.6 ± 1.1 |
| ≥4.50 | 2.4 (1,013) | 2.5 (423) | 2.6 (328) | 2.2 (262) |
| LDL cholesterol (mmol/L, mean ± STD) | 2.6 ± 0.8 | 2.6 ± 0.8 | 2.6 ± 0.8 | 2.6 ± 0.9 |
| >4.14 | 2.9 (1,199) | 2.5 (427) | 2.8 (362) | 3.5 (410) |
| HDL cholesterol (mmol/L, mean ± STD) | 1.4 ± 0.4 | 1.4 ± 0.4 | 1.3 ± 0.3 | 1.4 ± 0.4 |
| <0.91 | 8.8 (3,640) | 9.2 (1,552) | 10.3 (1,323) | 6.5 (765) |
| Fasting glucose (mmol/L, mean ± STD) | 5.6 ± 1.6 | 5.8 ± 1.5 | 5.1 ± 1.7 | 5.7 ± 1.4 |
| >7.00 | 7.6 (3,157) | 8.7 (1,467) | 6.1 (787) | 7.7 (903) |
Note: STD, standard deviance; LDL, low-density lipoprotein; HDL, high-density lipoprotein;
1Per National Diet Salt Intake in 200228, PURE-China centers were classified three salt-diet regions: heavy-salt regions (>8 grams of daily salt intake) included Beijing, Jiangsu Province, Jiangxi Province, and Liaoning Province; moderate-salt regions (7 to 8 grams) included Qinghai Province, Shaanxi Province, and Shandong Province; low-salt regions (<7 grams) included Inner Mongolia, Sichuan Province, and Yunnan Province, Shanxi Province, and Xinjiang Province.
2Estimated excretion was calculated by a fasting morning urine specimen on the basis of the Kawasaki formula18;
3Creatinine excretions were determined according to a formula including age, sex, weight, and height, which also was used in Kawasaki formula to estimate sodium and potassium excretion.
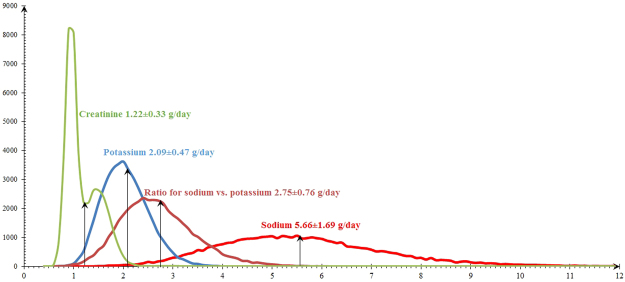
Distribution for 24-hour sodium, potassium, their ratio, and creatinine excretion were illustrated in Fig. 2, with the means for 24-hour sodium, potassium, creatinine excretion of 5.7, 2.1, and 1.2 g/day, respectively. In total, 62.3% had an estimated sodium excretion of more than 5 g per day, 34.3% between 3 and 5 g per day, and only 3.5% lessthan 3 g per day. 36.5% of 24-hour potassium excretion were estimated less than 1.9 g/day, 44.9% ranged from 1.9 to 2.5 g per day, and 18.6% more than 2.5 g/day. The mean ratio of sodium vs. potassium was 2.8, accounting for 84.9% of this ratio ≥ 2.
Figure 2.
Distribution for 24-hour sodium, potassium, creatinine excretion, and ratio for sodium vs. potassium.
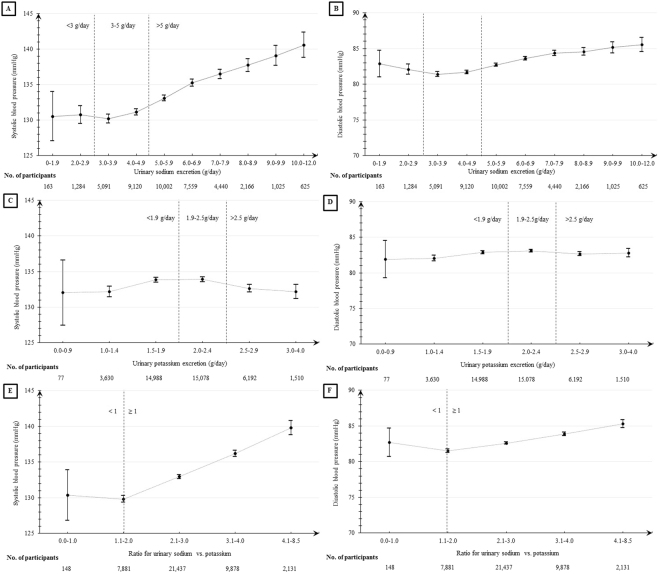
Table 2 described the associations of blood pressure with 24-hour urinary sodium and potassium excretion per one unit increase adjustedfor gender, age, education level, salt-diet regions, body mass index, and alcohol intake or unadjusted for any counfounder. The positive association of urine sodium excreation was found for both SBP and DBP, but larger slope was seen for SBP than DBP. A significantly steeper slope for association at the level of sodium excretion at 5–6 g/day (2.10 mmHg, 95% CI, 0.75–3.44; P < 0.01) was observed than that at level of between >6 g/day (1.64 mmHg, 95% CI, 1.37–1.92; P < 0.01) or less than 5 g/day (0.89 mmHg, 95% CI, 0.45–1.33; P = 0.08) (Fig. 3A). Similar trend with much smaller slope was observed for DBP (Fig. 3B). Inverse U-shape association of urinary potassium excretion with SBP and DBP were illustrated in Fig. 3C and 3D, respectively. Significant inverse associations were estimated at level of more than 2.2 g/day of potassium excretion (SBP, −2.30 mmHg decrease, 95% CI, −3.32 to −1.29; P < 0.01; DBP, 1.44 mmHg decrease, 95% CI, −2.04 to −0.84; P < 0.01). The ratio was calculated using 24-hour uriary sodium excretion divided by 24-hour urinary potassium excretion. Obvious positive associations of this ratio with both 4.33 mmHg of SBP (95% CI, 4.07 to 4.59) and 1.54 mmHg of DBP (95% CI, 1.39 to 1.69) were obtained in linear regressions (P < 0.01) (Table 2, Fig. 3E for SBP, Fig. 3F for DBP), especially for the ratio of 2.3–3.0.
Table 2.
Associations of blood pressure with 24-hour urinary sodium and potassium excretion per one-unit increase.
| Sodium/potassium excretion | No. | Crude model | Adjusted mode1 | ||
|---|---|---|---|---|---|
| Changes in BP (95% CI) | P value | Changes in BP (95% CI) | P value | ||
| Systolic blood pressure | |||||
| Per 1-g increase of sodium excretion | 41,475 | 1.55 (1.42,1.67) | <0.01 | 1.70 (1.58, 1.82) | <0.01 |
| Sodium <5 g/day | 15,658 | 0.56 (0.08, 1.05) | 0.02 | 0.89 (0.45, 1.33) | <0.01 |
| Sodium 5–6 g/day | 10,002 | 2.62 (1.16, 4.08) | <0.01 | 2.10 (0.75, 3.44) | <0.01 |
| Sodium >6 g/day | 15,815 | 1.29 (1.00, 1.59) | <0.01 | 1.64 (1.37, 1.92) | <0.01 |
| Per 1-g increase of potassium excretion | 41,475 | −0.29 (−0.75, 0.17) | 0.21 | −1.10 (−1.53, −0.67) | <0.01 |
| Potassium <1.8 g/day | 11,742 | 5.08 (2.75, 7.41) | <0.01 | 1.28 (−0.84, 3.40) | 0.24 |
| Potassium 1.8–2.2 g/day | 13,925 | 0.13 (−3.11, 3.36) | 0.94 | 0.02 (−2.94, 2.99) | 0.99 |
| Potassium >2.2 g/day | 15,808 | −2.16 (−3.24, −1.08) | <0.01 | −2.30 (−3.32, −1.29) | <0.01 |
| Per one unit increase of ratio2 | 41,475 | 3.74 (3.46, 4.02) | <0.01 | 4.33 (4.07, 4.59) | <0.01 |
| Ratio <2.3 | 12,144 | 2.94 (1.62, 4.27) | <0.01 | 4.14 (2.93, 5.36) | <0.01 |
| Ratio 2.3-3.0 | 15,553 | 6.01 (4.31, 7.72) | <0.01 | 5.68 (4.12, 7.24) | <0.01 |
| Ratio >3.0 | 13,778 | 3.32 (2.60, 4.03) | <0.01 | 3.64 (2.98, 4.28) | <0.01 |
| Diastolic blood pressure | |||||
| Per 1-g increase of sodium excretion | 41,475 | 0.66 (0.59, 0.73) | <0.01 | 0.49 (0.42, 0.56) | <0.01 |
| Sodium <5 g/day | 15,658 | −0.01 (−0.28, 0.26) | 0.92 | −0.09 (−0.35, 0.16) | 0.48 |
| Sodium 5-6 g/day | 10,002 | 1.13 (0.30, 1.96) | 0.01 | 0.64 (−0.16, 1.44) | 0.11 |
| Sodium >6g/day | 15,815 | 0.53 (0.37, 0.69) | <0.01 | 0.52 (0.36, 0.68) | <0.01 |
| Per 1-g increase of potassium excretion | 41,475 | 0.24 (−0.01, 0.50) | 0.06 | −0.91 (−1.16, −0.66) | <0.01 |
| Potassium <1.8 g/day | 11,742 | 2.24 (0.96, 3.52) | <0.01 | −0.31 (−1.53, 0.92) | 0.63 |
| Potassium 1.8-2.2 g/day | 13,925 | 0.18 (−1.61, 1.97) | 0.85 | −0.80 (−2.50, 0.90) | 0.35 |
| Potassium >2.2 g/day | 15,808 | −0.47 (−1.09, 0.14) | 0.13 | −1.44 (−2.04, −0.84) | <0.01 |
| Per one unit increase of ratio2 | 41,475 | 1.43 (1.27, 1.58) | <0.01 | 1.54 (1.39, 1.69) | <0.01 |
| Ratio <2.3 | 12,144 | 0.65 (−0.10, 1.40) | 0.09 | 0.84 (0.12, 1.55) | 0.03 |
| Ratio 2.3-3.0 | 15,553 | 2.78 (1.82, 3.74) | <0.01 | 2.48 (1.56, 3.39) | <0.01 |
| Ratio >3.0 | 13,778 | 1.37 (0.97, 1.76) | <0.01 | 1.56 (1.19, 1.94) | <0.01 |
Note: BP, blood pressure (mmHg); CI, confidence interval;
1Adjusted for gender, age, education level, geographic region, body mass index (BMI), and alcohol intake;
2Ratio meant 24-hour urinary sodium excretion divided by 24-hour urinary potassium.
Figure 3.
Means and 95% confidence intervals of systolic and diastolic blood pressure by urinary sodium excretion (A,B), potassium excretion (C,D), and ratio of sodium vs. potassium (E,F).
We also divided the total population into three sodium excretion subgroups (<5, 5–6, >6 g/day) and examined the patterns of association between potassium excretion and blood pressure in each sodium level. Further subgroup analyses using salt-diet regions also were presented in Table 3. Stronger negative associations between potassium excretion and systolic blood pressure was shown at 5 to 6 gram/day sodium excretion than those at >6 gram/day, whatever for heavy- or moderate- or low-salt regions, but the largest associations were observed at <5 gram/day sodium excretion in moderate-salt regions (−4.66 mmHg; 95% CI, −6.45 to −2.87) and low-salt regions (−5.29 mmHg; 95% CI, −6.65 to −3.94). The strongest negative association was also observed for diastolic blood pressure (−2.39 mmHg; 95% CI, −2.96 to −1.82) among overall population, those living in heavy-salt regions and low-salt regions.
Table 3.
Adjusted associations of blood pressure with 24-hour urinary potassium excretion at various levels of urinary sodium excretion.
| Subgroups of urinary sodium excretion | No. | 24-hour urinary potassium excretion | |||
|---|---|---|---|---|---|
| Crude model | Adjusted mode1 | ||||
| Changes in BP (95% CI) | P value | Changes in BP (95% CI) | P value | ||
| Systolic blood pressure | |||||
| All regions | |||||
| Sodium <5 g/day | 15,658 | −1.86 (−2.75, −0.97) | <0.01 | −1.43 (−5.13, −3.50) | <0.01 |
| Sodium 5–6 g/day | 10,002 | −3.97 (−5.00, −2.94) | <0.01 | −4.76 (−5.71, −3.80) | <0.01 |
| Sodium >6 g/day | 15,815 | −3.75 (−4.50, −3.00) | <0.01 | −3.40 (−4.10, −2.70) | <0.01 |
| Heavy-salt regions 2 | |||||
| Sodium <5 g/day | 6,730 | −0.43 (−1.78, 0.92) | 0.53 | −3.38 (−4.63, −2.13) | <0.01 |
| Sodium 5–6 g/day | 4,254 | −3.62 (−5.21, −2.02) | <0.01 | −5.27 (−6.75, −3.79) | <0.01 |
| Sodium >6 g/day | 5,898 | −2.30 (−3.56, −1.05) | <0.01 | −3.02 (−4.21, −1.84) | <0.01 |
| Moderate-salt regions 2 | |||||
| Sodium <5 g/day | 3,542 | −1.07 (−3.02, 0.88) | 0.28 | −4.66 (−6.45, −2.87) | <0.01 |
| Sodium 5–6 g/day | 2,948 | −2.65 (−4.59, −0.72) | <0.01 | −3.22 (−5.01, −1.44) | <0.01 |
| Sodium >6 g/day | 6,361 | −3.40 (−4.60, −2.21) | <0.01 | −2.77 (−3.88, −1.67) | <0.01 |
| Low-salt regions 2 | |||||
| Sodium <5 g/day | 5,386 | −3.94 (−5.42, −2.46) | <0.01 | −5.29 (−6.65, −3.94) | <0.01 |
| Sodium 5–6 g/day | 2,800 | −4.81 (−6.71, −2.90) | <0.01 | −5.14 (−6.89, −3.38) | <0.01 |
| Sodium >6 g/day | 3,556 | −4.95 (−6.47, −3.44) | <0.01 | −3.92 (−5.32, −2.52) | <0.01 |
| Diastolic blood pressure | |||||
| All regions | |||||
| Sodium <5 g/day | 15,658 | −0.28 (−0.77, 0.21) | 0.27 | −1.77 (−2.25, −1.30) | <0.01 |
| Sodium 5-6 g/day | 10,002 | −1.47 (−2.06, −0.88) | <0.01 | −2.39 (−2.96, −1.82) | <0.01 |
| Sodium >6 g/day | 15,815 | −1.18 (−1.60, −0.76) | <0.01 | −1.73 (−2.14, −1.32) | <0.01 |
| Heavy-salt regions 2 | |||||
| Sodium <5 g/day | 6,730 | 0.19 (−0.55, 0.93) | 0.62 | −1.46 (−2.18, −0.74) | <0.01 |
| Sodium 5–6 g/day | 4,254 | −1.34 (−2.23, −0.44) | <0.01 | −2.62 (−3.50, −1.75) | <0.01 |
| Sodium >6 g/day | 5,898 | −0.78 (−1.48, −0.09) | 0.03 | −1.92 (−2.61, −1.24) | <0.01 |
| Moderate-salt regions 2 | |||||
| Sodium <5 g/day | 3,542 | 0.00 (−1.10, 1.10) | 1.00 | −2.06 (−3.11, −1.01) | <0.01 |
| Sodium 5–6 g/day | 2,948 | −0.95 (−2.07, 0.16) | 0.09 | −1.77 (−2.84, −0.70) | <0.01 |
| Sodium >6 g/day | 6,361 | −0.77 (−1.44, −0.10) | 0.03 | −1.08 (−1.73, −0.43) | <0.01 |
| Low-salt regions 2 | |||||
| Sodium <5 g/day | 5,386 | −1.00 (−1.82, −0.18) | 0.02 | −2.09 (−2.88. −1.30) | <0.01 |
| Sodium 5–6 g/day | 2,800 | −1.96 (−3.06, −0.86) | <0.01 | −2.64 (−3.70, −1.58) | <0.01 |
| vSodium >6 g/day | 3,556 | −2.11 (−2.97, −1.26) | <0.01 | −2.22 (−3.05, −1.39) | <0.01 |
Note: BP, blood pressure (mmHg); CI, confidence interval;
1Adjusted for age, sex, education level, body mass index (BMI), and alcohol intake.
2Per National Diet Salt Intake in 200228, PURE-China centers were classified three salt-diet regions: heavy-salt regions (>8 grams of daily salt intake) included Beijing, Jiangsu Province, Jiangxi Province, and Liaoning Province; moderate-salt regions (7 to 8 grams) included Qinghai Province, Shaanxi Province, and Shandong Province; low-salt regions (<7 grams) included Inner Mongolia, Sichuan Province, and Yunnan Province, Shanxi Province, and Xinjiang Province.
Hypertension risk was also evaluated using logisitic regression adjusted for gender, age, education level, salt-diet regions, BMI, and alcohol intake, presented in Table 4. 7% increase, 19% decrease, and 27% increase risks of hypertension were found per one unit increase of sodium, potassium, and their ratio, respectively (P < 0.01). 11% increase and 13% decrease of hypertension risk was related to sodium excretion per one gram increase at the level of more than 6 g per day and <5 g/day, respectively. Moreover, 34% and 19% decrease of hypertension was shown for urinary potassium excretions at 1.8–2.2 g/day (P = 0.01) and >2.2 g/day (P < 0.01). 36% and 35% increase of hypertension risks was found per one unit increase of ratio for sodium vs. potassium when this ratio between 2.3 and 3.0 (OR, 1.36; 95% CI, 1.14 to 1.62), and more than 3 (OR, 1.35; 95% CI, 1.26 to 1.45), but 4% decrease of hypertension risk if this ratio was lessthan 2.3 (OR, 0.96; 95% CI, 0.83 to 1.10; P = 0.53).
Table 4.
Adjusted associations of hypertension prevalence with 24-hour urinary sodium and potassium excretion per one-unit increase.
| Sodium/potassium excretion | No. | Crude model | Adjusted model2 | ||
|---|---|---|---|---|---|
| Odds ratio (95% confidence interval) | P value | Odds ratio (95% confidence interval) | P value | ||
| Per 1-g increase of sodium excretion | 41,475 | 1.04 (1.03, 1.06) | <0.01 | 1.07 (1.05, 1.08) | <0.01 |
| Sodium <5 g/day | 15,658 | 0.87 (0.83, 0.91) | <0.01 | 0.87 (0.83, 0.92) | <0.01 |
| Sodium 5–6 g/day | 10,002 | 1.13 (0.98, 1.30) | 0.08 | 1.09 (0.94, 1.27) | 0.26 |
| Sodium >6 g/day | 15,815 | 1.07 (1.04, 1.10) | <0.01 | 1.11 (1.08, 1.15) | <0.01 |
| Per 1-g increase of potassium excretion | 41,475 | 0.91 (0.87, 0.95) | <0.01 | 0.81 (0.78, 0.85) | <0.01 |
| Potassium <1.8 g/day | 11,742 | 1.41 (1.15, 1.73) | <0.01 | 0.99 (0.78, 1.24) | 0.89 |
| Potassium 1.8–2.2 g/day | 13,925 | 0.75 (0.56, 1.00) | 0.05 | 0.66 (0.48, 0.91) | 0.01 |
| Potassium >2.2 g/day | 15,808 | 0.84 (0.76, 0.93) | <0.01 | 0.81 (0.72, 0.91) | <0.01 |
| Per one unit increase of ratio3 | 41,475 | 1.15 (1.12, 1.18) | <0.01 | 1.27 (1.24, 1.31) | <0.01 |
| Ratio <2.3 | 12,144 | 0.86 (0.76, 0.98) | 0.02 | 0.96 (0.83, 1.10) | 0.53 |
| Ratio 2.3-3.0 | 15,553 | 1.29 (1.10, 1.52) | <0.01 | 1.36 (1.14, 1.62) | <0.01 |
| Ratio >3.0 | 13,778 | 1.24 (1.16, 1.32) | <0.01 | 1.35 (1.26, 1.45) | <0.01 |
1Self-reported hypertension or had blood pressure medication or blood pressure ≥ 140/90 mmHg; CI, confidence interval;
2Adjusted for gender, age, education level, geographic region, body mass index (BMI), and alcohol intake;
3Ratio means 24-hour urinary sodium excretion divided by 24-hour urinary potassium.
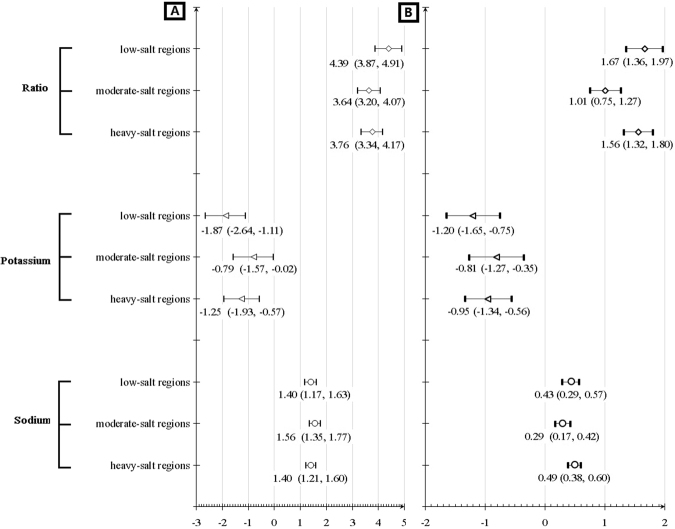
Changes of SBP and DBP per one unit increase of 24-hour urinary sodium, potassium, and their ratio were also estimated after adjusted for age, gender, education level, geographic region, BMI, and alcohol intake and categorized by various salt-diet regions based on National Dietary Survey in 200228, and detailed results were illustrated in Fig. 4. Around one mmHg of SBP and about a half mmHg of DBP increase was obtained when increasing one gram of sodium excretions, whatever heavy-, moderate, or low-salt regions (P < 0.05).Additionally, the effects of potassium excretion increase on reducing blood pressure also seemed effective in all regions, especially for low-salt region (SBP: −1.87 mmHg, 95% CI, −2.64 to −1.11; DBP: −1.20 mmHg, 95% CI, −1.65 to −0.75). Blood pressure with statistical significance increased substantially along with ratio increase of sodium vs. potassium (3 to 5 mmHg for SBP and 1 to 2 mmHg for DBP per one-unit increase), specially for low-salt region (SBP: 4.39 mmHg, 95% CI, 3.87 to 4.91; DBP: 1.67 mmHg, 95% CI, 1.36 to 1.97).
Figure 4.
Changes of systolic (A) and diastolic (B) blood pressure per one unit increase of 24-hour urinary sodium excretions, 24-hour urinary potassium excretions, and their ratio for sodium vs. potassium by various salt-diet regions.
Discussions
This paper is the first to divide PURE-China centers into three salt intake levels (high, moderate, low) per National Dietary Survey in 200223. However, we did not observe expected higher-sodium excretion in heavy-salt regions, while moderate-salt regions were found to have the highest sodium excretion and blood pressure levels including Qinghai Province, Shaanxi Province, and Shandong Province. The reasons of this variation might be different daily salt estimation approaches. The 2002 National Dietary Survey used questionnaire collection of daily salt intake, while our study used morning fasting urine estimates, which is regarded as more accurate due to better capturing of discretionary sodium use which comprises a substantial amount of total sodium intake in China. Similar to previous studies8,14,15, a positive association of urinary sodium and inverse association of urinary potassium with both SBP and DBP was found in all salt-intake regions, especially for low-salt regions. High potassium excretions seemed more effective to control blood pressure at 5 to 6 gram/day of sodium excretions than higher sodium excretion subgroup. Additionally, urinary sodium/potassium ratio was more closely associated with BP than estimation from urinary sodium alone or potassium alone, especially low-salt regions. Hence, sodium restriction and potassium addition might be more effective to control blood pressure.
Highsodium intake is prominent in Chinese dietary15,16,24,29–32, though sodium restriction strategies have been promoted in population-based interventions in the past decases7,33–35, and mean daily salt intake decreased from 12.0 in 2002 to 9.6 grams in 2012 (10.9 to 9.0 grams in urban areas and 12.4 to 10.2 gram in rural areas)23,24. As a famous epidemiological study involving in 12 provinces, automous regions, or municipalities with 1:1 of urban-to-rural cluster sampling ratio, higher sodium excretions(5.7 g/day, equal to about 14.3 grams salt intake) estimated using single fasting urine specimen were also reported for China than other PURE countries16, which also was much higher than a maximum sodium intake recommended by current guidelines36,37. Low potassium excretions seemed to be a global problem with the mean level at around 2 g/day, simlar with PURE-China results, all of which were much lower than the adequate intake levels recommended37,38, but within the range recommended by China23. It is worth mentioning that males had higher sodium excretions (6.1 vs. 5.4 g/day) and blood pressure (SBP: 135.1 vs. 132.3 mmHg; DBP: 84.1 vs. 82.0 mmHg) than females, which were consistent with previousstudies conducted in China reporting higher sodium intake and BP among males than females7,15,20.
Further subgroup analyses were performed to evaluate the relationships of potassium excretions with blood pressure at various groups of sodium excretions, which would be helpful to infer potential effects of potassium intervention on controlling blood pressure at different levels of salt intake. Since the Chinese population has high sodium intake, we have smaller numbers at the lower levels of sodium intake and so have limited power to draw reliable conclusions for <3 gram/day of sodium intake group. However, our findings suggest that high potassium intake would be more effective in helping to lower blood pressure at higher levels of sodium intake. Hence, potassium addition in diet should be enhanced further, especially for those with high-salt diet.
In our study of the baseline data, a strong positive association between sodium intake and Na+/K+ ratio versus hypertension risk was found at higher levels of sodium intake (ie, >6 g/day). Further, an association between higher potassium intake and lower hypertension risk was found only at high potassium intake levels. Hence, more attention for salt restriction should be paid to those with high levels of urinary sodium and sodium/potassium ratio.
Our PURE-China study had the same limitations with global PURE16,25. For example, firstly, formula-derived estimates of 24-hour urinary excretion was used for analyses, not actual urinary excretion. Only spot urine sample was collected for each participant on one day may not stand for actual urinary sodium and potassium intake levels. Secondly, though our PURE-China adopted cluster sampling with 1:1 urban-to-rural sampling ratio and involved in 12 administrative regions, our population were not representative to mean levels at the local regions, which might be the reason why our sodium levels per National Dietary Survey in 200223 were inconsistent with common sense. Specially, achieving good follow-up retention is the primary goal for PURE study. Finally, our hypertension definition based on self-reports by participants and blood pressure measurements twice one the same day, which were not routine clinical diagnosis, but our definition was easy to use in most epidemiological studies12,13,15,20,24. Poor hypertension awareness in Chinese population may underestimate hypertension prevalence for PURE-China22, while only two repeated BP measurements about five-minute apart might overestimate hypertension prevalence25.
Conclusions
Though we did not observe expected trend based on salt classifications per National Dietary Survey in 2002, our PURE-China results confirm that less sodium intake may result in blood pressure decrease and potassium increase strategies were more needed to be generalized across various salt-intake regions, even if those are living in low-salt regions.
Acknowledgements
Besides co-authors listed in this study, we would like to thank those who supported our study and what they did with our sincere gratitude, especially for site coordinators, physicians, nurses, questionnaire interviewers, and laboratory personnel in all participating centers and communities, including: 1China Coordination Center Beijing Office: Lisheng Liu, Hongye Zhang, Jian Li, Kean Wang, Xiaoru Cheng, Xixin Hou, Xuan Jia; 2Jishuitan Hospital, Beijing: Di Chen, Dong Li, Hui Jin, Jiwen Tian; 3Shunyi District Center for Disease Control & Prevention, Beijing: Yindong Li, Kai You, Changqing Li, Songjian Zhang, Wenlong Cheng, Hongye Zhang; 4Shijingshan District Hospital of Traditional Chinese Medicine, Beijing: Honghong Li, Qiang Zhou, Xu Xu, Yanhong Sun, Jinling Di, Jianquan Wu, Mei Wang; 5Bayannaoer Center for Disease Control & Prevention, Inner Mongolia: Minzhi Cao, Shiying Zhang, Aiying Han; 6Wujin District Center for Disease Control & Prevention, Changzhou City, Jiangsu Province: Jianxin Zhou, Yihong Zhou, Deren Qiang, Jianfang Wu, Zhaowei Li, Jing Qin, Suyi Shi, Zhihua Fan, Alin Qian, Lingyun Pan, Minrui Xu, Yibing Cui; 7Jiangsu Provincial Hospital: Jun Li, Yongzhen Mo; 8Jiangsu Province Center for Disease Control & Prevention: Quanyong Xiang, Ye Cao; 9Jiangxinzhou Community Health Service Center, Nanjing City, Jiangsu Province: Zhenzhen Qian, Zhengrong Liu; 10Nanhu District Health Service Center, Nanjing City, Jiangsu Province: Xiangrong He, Changlin Dong, Ming Wan; 11Xiaohang Hospital, Nanjing City, Jiangsu Province: Jinhua Tang; 12Nanchang Center for Disease Control & Prevention, Nanchang City, Jiangxi Province: Rensheng Lei, Lihua Hu, Shuwei Xiong; 13Qingshanhu Community Health Service Center, Nanchang City, Jiangxi Province: Ning Li, Xincheng Tang, Dan Zou, Qilu Gan, Shuli Ye; 14Shenyang 242 Hospital, Shenyang City, Liaoning Province: Yu Liu; 15Daxing District Health Center, Shenyang City, Liaoning Province: Minfan Fu, Qiuyuan Wang; 16RedCross Hospital, Shenyang City, Liaoning Province: Baoxia Guo, Huilian Feng, Xiaojie Xing; 17Xining Center for Disease Control & Prevention, Xining City, Qinghai Province: Yuqing Yang, Wenqiang Xu, Haibin Ma, Yali Wang; 18Huizu Hospital, Xining City, Qinghai Province: Youzhu Yang, Xiaolan Ma, Yan Hai, Zhe Xie, Yuanting Ma; 19Huaxi Hospital, Chengdu City, Sichuan Province: Xiaoyang Liao, Qian Zhao,Chuan Zou; 20Jianshe Road Community Health Service Center, Chengdu City, Sichuan Province: Guofan Xu, Jiankang Liu; 21Dayicaichang Town Health Center, Sichuan Province: Xiaolin Zhang, Wenqing Deng; 22Shandong Province Cardiovascular Disease Research Institute, Shandong Province: Fanghong Lu, Hua Zhang, Shangwen Sun, Yingxin Zhao, Zhendong Liu, Falian Sun; 23Jingle County Hospital, Shanxi Province: Yinsheng Wu, Guoqin Liu; 24Xinghualing District Balingqiao Community Health Service Station, Taiyuan City, Shanxi Province: Yan Hou, Junying Wang, Hua Wei; 25Electronic Science and Technology University Hospital, Xi’an City, Shaanxi Province: Xiaoxia Li, Yahong Zhi, Tianlu Liu; 26Yanliang District Guanshan Town Hospital, Xi’an City, Shaanxi Province: Peng Zhang; 27Hetian Center for Disease Control & Prevention, Hetian City, Xinjiang Province: Ayoufu Aideer Aili, Mitiwula, Reshalaiti, Hui Wang; 28Damenglong Town Health Center, Xishuangbanna Prefecture, Yunnan Province: Qiyun Wang, Jinkui Yang, Kehua Li; 29Mengla County Center for Disease Control & Prevention, Xishuangbanna Prefecture, Yunnan Province: Huaxing Liu, Chunmei Liu; 30Yunnan Province Center for Disease Control & Prevention, Yunnan Province: Yize Xiao.
Author Contributions
Lu Yin wrote the main manuscript text; Lu Yin, Guijuan Deng, Yi Sun performed statistical analyses and double-checking; Lu Yin, Andrew Mente, Xiaoyun Liu, Xinhua Zhang, Xingyu Wang, Yang Wang, Wei Li conducted study design and manuscript revisions; Jian Bo, Hui Chen, Xu Liu, Nan Gao, Xiulin Bai, and Sumathy Rangarajan collected data and data cleaning.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bath P, et al. International Society of Hypertension (ISH): statement on the management of blood pressure in acute stroke. J Hypertens. 2003;21:665–672. doi: 10.1097/00004872-200304000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Chalmers J, et al. International Society of Hypertension (ISH): statement on blood pressure lowering and stroke prevention. J Hypertens. 2003;21:651–663. doi: 10.1097/00004872-200304000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Ettehad D, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 4.Xie X, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–443. doi: 10.1016/S0140-6736(15)00805-3. [DOI] [PubMed] [Google Scholar]
- 5.Aaron KJ, Sanders PW. Role of dietary salt and potassium intake in cardiovascular health and disease: a review of the evidence. Mayo Clin Proc. 2013;88:987–995. doi: 10.1016/j.mayocp.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cook NR, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP) BMJ. 2007;334:885–888. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Du S, et al. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. 2014;99:334–343. doi: 10.3945/ajcn.113.059121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mu J, et al. Family-based randomized trial to detect effects on blood pressure of a salt substitute containing potassium and calcium in hypertensive adolescents. Am J Hypertens. 2009;22:943–947. doi: 10.1038/ajh.2009.136. [DOI] [PubMed] [Google Scholar]
- 9.Noubiap JJ, Bigna JJ, Nansseu JR. Low sodium and high potassium intake for cardiovascular prevention: evidence revisited with emphasis on challenges in sub-Saharan Africa. J Clin Hypertens (Greenwich) 2015;17:81–83. doi: 10.1111/jch.12439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Donnell M, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–623. doi: 10.1056/NEJMoa1311889. [DOI] [PubMed] [Google Scholar]
- 11.Rebholz CM, et al. Urine angiotensinogen and salt-sensitivity and potassium-sensitivity of blood pressure. J Hypertens. 2015;33:1394–1400. doi: 10.1097/HJH.0000000000000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339:b4567. doi: 10.1136/bmj.b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mente A, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet. 2016;388:465–475. doi: 10.1016/S0140-6736(16)30467-6. [DOI] [PubMed] [Google Scholar]
- 14.Tabara Y, et al. Descriptive epidemiology of spot urine sodium-to-potassium ratio clarified close relationship with blood pressure level: the Nagahama study. J Hypertens. 2015;33:2407–2413. doi: 10.1097/HJH.0000000000000734. [DOI] [PubMed] [Google Scholar]
- 15.Yan L, et al. Relationships Between Blood Pressure and 24-Hour Urinary Excretion of Sodium and Potassium by Body Mass Index Status in Chinese Adults. J Clin Hypertens (Greenwich) 2015;17:916–925. doi: 10.1111/jch.12658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mente A, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371:601–611. doi: 10.1056/NEJMoa1311989. [DOI] [PubMed] [Google Scholar]
- 17.Appel LJ, et al. Effects of reduced sodium intake on hypertension control in older individuals: results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE) Arch Intern Med. 2001;161:685–693. doi: 10.1001/archinte.161.5.685. [DOI] [PubMed] [Google Scholar]
- 18.Kwagyan J, et al. Obesity and Cardiovascular Diseases in a High-Risk Population: Evidence-Based Approach to CHD Risk Reduction. Ethn Dis. 2015;25:208–213. [PMC free article] [PubMed] [Google Scholar]
- 19.Sacks FM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 20.Chen, X. et al. Urinary sodium or potassium excretion and blood pressure in adults of Shandong province, China: preliminary results of the SMASH project. J Am Soc Hypertens9, 754–762, doi:S1933-1711(15)00602-6 (2015). [DOI] [PubMed]
- 21.Gu H, et al. Hypertension prevalence, awareness, treatment and control among Han and four ethnic minorities (Uygur, Hui, Mongolian and Dai) in China. J Hum Hypertens. 2015;29:555–560. doi: 10.1038/jhh.2014.123. [DOI] [PubMed] [Google Scholar]
- 22.Li W, et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47 000 people from China. J Hypertens. 2016;34:39–46. doi: 10.1097/HJH.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 23.Wang, L. The First Report–2002 Comprehensive Report of Chinese Nutrition and Health Status. (People’s Medical Publishing House, 2005).
- 24.Yu, D. et al. Salt intake among Chinese adults in 2010–2012. Zhonghua Yu Fang Yi Xue Za Zhi50, 217–220. [Chinese], 10.3760/cma.j.issn.0253-9624.2016.03.005 (2016). [DOI] [PubMed]
- 25.Teo K, Chow CK, Vaz M, Rangarajan S, Yusuf S. The Prospective Urban Rural Epidemiology (PURE) study: examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J. 2009;158:1–7 e1. doi: 10.1016/j.ahj.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 26.Peng Y, Li W, Wang Y, Bo J, Chen H. The cut-off point and boundary values of waist-to-height ratio as an indicator for cardiovascular risk factors in Chinese adults from the PURE study. PLoS One. 2015;10:e0144539. doi: 10.1371/journal.pone.0144539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kawasaki T, Itoh K, Uezono K, Sasaki H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharmacol Physiol. 1993;20:7–14. doi: 10.1111/j.1440-1681.1993.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 28.Yang, X. G. National Survey Report 2 for Nutritional and health status of Chinese residents − 2002 dietary and nutrient intake status. (2006).
- 29.Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ297, 319–328 (1988). [DOI] [PMC free article] [PubMed]
- 30.Ge Z, et al. Association between 24 h urinary sodium and potassium excretion and the metabolic syndrome in Chinese adults: the Shandong and Ministry of Health Action on Salt and Hypertension (SMASH) study. Br J Nutr. 2015;113:996–1002. doi: 10.1017/S0007114514003833. [DOI] [PubMed] [Google Scholar]
- 31.O’Donnell MJ, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306:2229–2238. doi: 10.1001/jama.2011.1729. [DOI] [PubMed] [Google Scholar]
- 32.Yan L, et al. Population-based association between urinary excretion of sodium, potassium and its ratio with albuminuria in Chinese. Asia Pac J Clin Nutr. 2016;25:785–797. doi: 10.6133/apjcn.092015.33. [DOI] [PubMed] [Google Scholar]
- 33.Li N, et al. The Effects of a Community-Based Sodium Reduction Program in Rural China - A Cluster-Randomized Trial. PLoS One. 2016;11:e0166620. doi: 10.1371/journal.pone.0166620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McLaren L, et al. Population-level interventions in government jurisdictions for dietary sodium reduction. Cochrane Database Syst Rev. 2016;9:CD010166. doi: 10.1002/14651858.CD010166.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang X, et al. Does education level affect the efficacy of a community based salt reduction program? - A post-hoc analysis of the China Rural Health Initiative Sodium Reduction Study (CRHI-SRS) BMC Public Health. 2016;16:759. doi: 10.1186/s12889-016-3454-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eckel RH, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S76–99. doi: 10.1161/01.cir.0000437740.48606.d1. [DOI] [PubMed] [Google Scholar]
- 37.Institute of Medicine. Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. (The National Academies Press, 2005).
- 38.Diet, nutrition and the prevention of chronic diseases. World Health Organ Tech Rep Ser 916, i-viii, 1–149, backcover (2003). [PubMed]