Abstract
Objective:
To compare the efficacy and functional outcome of Glasgow Coma Scale (GCS) score with that of Acute Physiology and Chronic Health Evaluation Score II (APACHE II) in patients with multiple trauma admitted to the ICU.
Methods:
This cross-sectional study included 125 patients with traumatic brain injury associated with systemic trauma admitted to the ICU of Shahid Kamyab Hospital, Mashhad, between September 2015 and December 2016. On the day of admission, data were collected from each patient to calculate GCS and APACHE II scores. Sensitivity, specificity, and correct outcome prediction was compared between GCS and APACHE II.
Results:
Positive predictive value (PPV) at the cut-off points was higher in APACHE II (80.6%) compared with GCS (69.2%). However, negative predictive value (NPV) of GCS was slightly higher in comparison with APACHE II. Moreover, the area under the receiver operating characteristic (ROC) curve for sensitivity and specificity of GCS and APACHE II showed no significant difference (0.81±0.04 vs. 0.83±0.04; p=0.278 respectively).
Conclusion:
Our study suggested that there was no considerable difference between GCS and APACHE II scores for predicting mortality in head injury patients. Both scales showed acceptable PPV, while APACHE II showed better results. However, the utilization of GCS in the initial assessment is recommended over APACHE II as the former provides higher time- and cost-efficiency.
Key Words: Head trauma, GCS, APACHE II, Mortality
Materials and Methods
Study settings and approval
This cross-sectional study investigated 125 patients with acute head trauma admitted to the ICU of the Shahid Kamyab Hospital, Mashhad, Iran, from September 2015 to December 2016. Patients under 16 years of age, sedated patients, those connected to ventilators, those with trauma in the maxillofacial zone, and patients who were injured while being under the influence of illicit drugs or alcohol were excluded from the study. All the investigations conformed to the principles outlined in the Declaration of Helsinki. Informed written consent was obtained from each patient and the study was approved by the Ethics Committee of Mashhad University of Medical Science (code: 922366).
Data collection
At the time of ICU admission, a trained physician simultaneously calculated the GCS and APACHE II scores for each patient, before any sedation. The GCS is composed of three different tests: eye opening, verbal responses, and motor responses. The scores range from 3 (minimum) to 15 (maximum) and lower scores represent poor response to the practitioner's examination. The APACHE II scoring system, first introduced by Knaus et al. in 1985, uses 12 different physiological factors to evaluate critically ill patients within their first 24 hours of admission to the ICU. In this study, we calculated the APACHE II scores using the Knaus et al. method. In the APACHE II system, scores range from 0 to 71 and unlike the GCS system, higher values of APACHE II shows poorer outcome and higher risk of death [9].
Moreover, we assessed the Injury Severity Score (ISS) for each patient at the time of admission. It is a method for numerical description of the overall severity of injuries and is calculated by adding the squares of the highest scores from Abbreviated Injury Scale (AIS) in order of severity scale ranging from 1 to 6 (currently untreatable), making an overall score ranging from 0 to 75 [12].
Admission Period and Mortality
The first day of admission to the ICU was defined as the first 24 hour after the patients entered the hospital emergency room. Early mortality was defined as death of a patient before the 7th day of admission, while late mortality was defined as death of a patient after the 7th day of admission.
Data Analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS), version 16 for Windows (SPSS Science, Apache Software Foundation, Chicago, IL, USA). Descriptive statistics (mean, median, standard deviation (SD), and interquartile range) was determined for all variables. Normality of the data was assessed using the Kolmogorov-Smirnov test. Baseline demographic and clinical characteristics were compared between groups using independent samples t-test, Mann-Whitney test, chi-square test, or Fisher’s exact test where appropriate. In all tests, a P value below 0.05 was considered statistically significant. Receiver Operating Characteristic (ROC) curve was drawn for each scale. The area under the ROC curve was measured to determine the scales’ reliability and discrimination power and compared between the two scales.
Based on gathered information, diagnostic indices such as sensitivity, specificity, negative predictive value (NPV) and positive predictive value (PPV) was calculated to determine and compare the ability of the GCS and APACHE II scales to predict hospital mortality.
Youden index was calculated to specify the best cutoff point for the two diagnostic scales. This index ranges from 0 to 1 and its 0 value means that the diagnostic test gives the same proportion of positive results for groups with and without a specific disease, while 1 indicates that there are no false positive nor false negative predictions [13].
Results
This study included 125 patients, of whom 101 (80.8%) were males. The subjects were aged 16 to 90 years. Among the patients, 44 (35.2 %) died during their stay at the hospital, while 81 (64.8%) were discharged alive and in good condition. The median (quartiles) of staying period for the patients was 11 (6-24) days and the majority of patients (54.5 %) stayed less than 14 days. Among the 44 dead patients, 9.3 % died within the first day of admission and the rate of early mortality was 46.5 %.As shown in Table 1, car accident was the most frequent cause of injury (35.2%) and had the highest survival rate (76.7%). The mortality rate was highest (63.6 %) in injuries with other causes that included gunshots, fights, home disturbances, work related injuries and lightning strike. Overall, mean score of APACHE II scale was 14.9±6.2. The APACHE II scores were significantly different between dead and alive patients (19.4±5.5 vs. 12.4±5.5; p<0.001 respectively). There were no significant differences in APACHE II score between male and female subjects neither in the dead nor in the alive group.
Table 1.
Demographic and etiologic data of our study.
| Demographic and etiologic features | N (%) | |
|---|---|---|
| Sex | Male | 101 (80.8) |
| Female | 24 (19.2) | |
| Age (y) b | 34 (25-60) | |
| Mortality status | Dead | 44 (35.2) |
| Alive | 81 (64.8) | |
| Cause of injury | Car accident | 46 (36.8) |
| Motorcycle accident | 38 (30.4) | |
| Fall | 12 (9.6) | |
| Other causesa | 29 (23.2) | |
| ISS score b | 27 (17-35) | |
| GCS score b | 9 (6-15) | |
| APACHE II score c | 14.9±6.2 | |
Other causes included gunshots, fights, home disturbances, work related injuries and lightning strike;
Data are expressed as median (Q1-Q3) due to their non-normal distribution;
Data are expressed as mean ± SD due to their normal distribution.
The overall median score of GCS was 9.0 (6.0-15.0). There was a significant difference in the GCS score between dead (6 (3.0-9.0)) and alive (12 (7.0-15.0)) patients (p<0.001). Male subjects in the dead group had considerable lower GCS scores compared to female subjects (3 (5.5-7.0) vs. 10 (8-11.75); p=0.001; respectively). The median score for ISS was 27 (17-35) and it was ranged between 3 and 75. ISS was not different within genders (p>0.05), but dead subjects had significantly higher scores in ISS system, compared with alive ones (34.0 (27.0-43.0)) vs. 21.0(11.0-29.0), respectively; p<0.001).
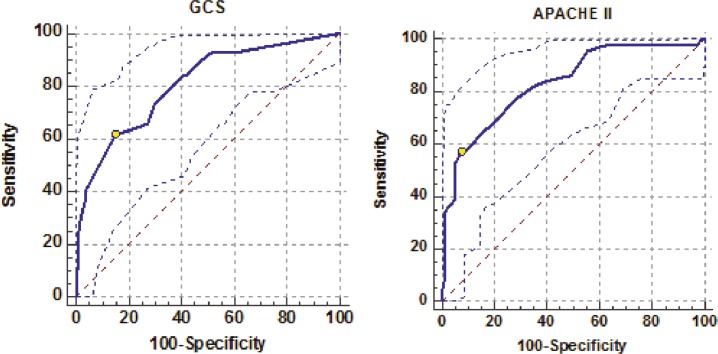
No association was found between hospital mortality and the type of injury (p>0.05). Mean scores for none of the APACHE II, ISS and GCS were significantly associated with type of injury (p>0.05). The best cut-off points for APACHE II and GCS were 19 and 6, respectively. Detailed information of GCS and APACHE II scales on sensitivity, specificity, PPV, NPV, Youden index, and area under the ROC curve at the best cut-off point for hospital mortality are shown in Table 2. In addition, there was no significant difference regarding the area under the ROC curve between the GCS (0.81±0.04) and APACHE II (0.83±0.04) scales (p>0.05). The ROC curves drawn at different cut-off values for GCS and APACHE II scales are depicted in Figure 1.
Table 2.
Comparison of GSC and APACHE II scores for hospital mortality prediction.
| Scale | CP a | Sensitivity | Specificity | YI b | AUC c | PPV d | NPV e | 95%CI f |
|---|---|---|---|---|---|---|---|---|
| GCS | 6 | 61.4% | 85.1% | 0.46 | 0.81±0.04 | 69.2 | 80.2 | 0.73-0.87 |
| APACHE II | 19 | 56.9.72% | 92.6.0% | 0.50 | 0.83±0.03 | 80.6 | 79.8 | 0.75-0.89 |
CP: Cut-off Point;
YI: Youden Index;
AUC: area under the ROC curve;
PPV: Positive Predictive Value;
NPV: Negative Predictive Value;
CI: confidence interval
Fig. 1.
ROC curves drawn at different cut-off values for GCS and APACHE II scales. The area under the curve for APACHE II is larger, but there is no statistically significant difference when compared with that of GCS.
Discussion
Severely injured patients with multiple traumas are at risk of life-threatening complications and demand rapid decision making in an emergency setting. Paying attention to their comorbidities and concomitant medical conditions has an important role in proper management of these patients [14]. Traumatic brain injuries are among the most severe and fatal injuries [15] . The routine initial assessment currently done in the emergency units in Iran is mostly GCS and the use of APACHE II scale is still limited and under controversy [3].
GCS is based on basic responses to stimuli and is essential in measuring neurological function and severity of head injury in traumatic patients [16] . It is simple, practical, time-efficient, and cost-effective and it helps to unification and ease of communication between the medical staff regarding the condition of patients. GCS score is easy to measure not only by the physicians but also by trained paramedics [17].
One of the disadvantages of GCS is that it is difficult to measure in some specific conditions, e.g. in sedated patients, those connected to ventilator, those with maxillofacial trauma, and those injured under the influence of illicit drugs or alcohol, all of whom were excluded from this study to minimize the researcher bias [18].
APACHE II scale has been shown to have promising outcomes in evaluating patients in emergency units [19, 20] . APACHE II not only includes GCS but also uses 11 other physiologic factors that include both clinical and laboratory data.
ISS is an anatomical scoring system that is associated with mortality, morbidity, hospital stay, and overall severity of injuries. There are several downsides to the use of ISS in the initial evaluation of critically injured patients in emergency department. First, since ISS is directly related to AIS, any error in AIS increases the chance of error in ISS. Moreover, different patterns of injury on different sites and organs can result in same ISS scores. Most importantly, since complete description of injuries require thorough investigation and examination of the patient, anatomical scoring systems like ISS are not efficacious tools for initial evaluation and screening in an emergency setting, especially in ICU patients [12].
In the current study, we found the most frequent cause of ICU admission to be road traffic accidents. Similar results have been previously reported by Majdan et al., who showed traumatic brain injuries are significantly associated with road traffic accidents [15] .
Our results showed that APACHE II had higher specificity but lower sensitivity compared with GCS. This finding suggests that APACHE II scale has more power in recognizing critically ill patients with higher chances of survival, who are in greater need for ICU care.
The ROC curve results showed no significant difference between the GCS and APACHE II scales, suggesting that APACHE II is not necessarily a better mortality predictor in patients with head trauma. Measuring the APACHE II score demands more time and budget, the items that are of utmost importance in emergency care.
On the one hand, in the developing countries, the rate of accidents and subsequent head injuries are higher, compared to the developed countries. On the other hand, the healthcare budgets are usually lower in the developing countries, compared to the developed ones. This discrepancy highlights the need for an initial assessment method that is less costly and more time-efficient, since it is important to reduce the costs of management and treatment in emergency units and hospitals.
The findings of this study demonstrated that there was no significant difference between GCS and APACHE II scales for predicting hospital mortality in patients with head injury. Although both of the scales showed desirable PPV, APACHE II yielded better results. However, t it is important to reduce the expenses of management and treatment in hospitals. Considering all aspects, it seems that in comparison with APACHE II, GCS is a more accessible method particularly for quick initial evaluation of critically injured patients with head trauma.
One of our limitations was that the follow-up was limited to the period of hospital stay. Due to the lack of trained staff, limited budget, and low socioeconomic status in most of the patients, the patients were not followed for long-term outcomes after their discharge. In addition, this study was carried out in a single center. Although our hospital is the main referral center for traumatic patients in the Northeast of Iran, further multicenter studies would be of help in order to achieve results that are more reliable.
In conclusion, our study suggested that there was no considerable difference between GCS and APACHE II scores for predicting mortality in head injury patients. Both scales showed acceptable PPV, while APACHE II showed better results. However, the utilization of GCS in the initial assessment is recommended over APACHE II as the former provides higher time- and cost-efficiency.
Acknowledgements
The authors would like to thank all the subjects participating in the study. This study was financially supported by Mashhad University of Medical Science (MUMS), Iran.
Conflict of Interest:
The Authors have none to declare.
References
- 1.Bae JY, Groen RS, Kushner AL. Surgery as a public health intervention: common misconceptions versus the truth. Bull World Health Organ. 2011;89(6) doi: 10.2471/BLT.11.088229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peden M. Global collaboration on road traffic injury prevention. Int J Inj Contr Saf Promot. 2005;12(2):85–91. doi: 10.1080/15660970500086130. [DOI] [PubMed] [Google Scholar]
- 3.Modaghegh MH, Saremi E, Mohamadian M, Jafarzadeh R. Characteristics of trauma in North East Iran and the prevention strategies. Arch Iran Med. 2013;16(10):576–9. [PubMed] [Google Scholar]
- 4.Khuri SF, Daley J, Henderson W, Hur K, Demakis J, Aust JB, et al. The Department of Veterans Affairs' NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care National VA Surgical Quality Improvement Program. Annals of surgery. 1998;228(4) doi: 10.1097/00000658-199810000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grmec Š, Gašparovic V. Comparison of APACHE II, MEES and Glasgow Coma Scale in patients with nontraumatic coma for prediction of mortality. Critical Care. 2000;5(1) doi: 10.1186/cc973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chesnut RM. Glasgow Coma Score versus severity systems in head trauma. Critical care medicine. 1998;26(1):10–1. doi: 10.1097/00003246-199801000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Balestreri M, Czosnyka M, Chatfield DA, Steiner LA, Schmidt EA, Smielewski P, et al. Predictive value of Glasgow Coma Scale after brain trauma: change in trend over the past ten years. J Neurol Neurosurg Psychiatry. 2004;75(1):161–2. [PMC free article] [PubMed] [Google Scholar]
- 8.McNett M. A review of the predictive ability of Glasgow Coma Scale scores in head-injured patients. J Neurosci Nurs. 2007;39(2):68–75. doi: 10.1097/01376517-200704000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Critical care medicine. 1985;13(10):818–29. [PubMed] [Google Scholar]
- 10.Weingarten S, Bolus R, Riedinger MS, Maldonado L, Stein S, Ellrodt AG. The principle of parsimony: Glasgow Coma Scale score predicts mortality as well as the APACHE II score for stroke patients. Stroke. 1990;21(9):1280–2. doi: 10.1161/01.str.21.9.1280. [DOI] [PubMed] [Google Scholar]
- 11.Rocca B, Martin C, Viviand X, Bidet P, Saint-Gilles HL, Chevalier A. Comparison of four severity scores in patients with head trauma. The Journal of trauma. 1989;29(3):299–305. doi: 10.1097/00005373-198903000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Baker SP, o'Neill B, Haddon Jr W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96. [PubMed] [Google Scholar]
- 13.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1): 32–35. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 14.Moeinipour A, Zarifian A, Sheikh Andalibi MS, Shamloo AS, Ahmadabadi A, Amouzeshi A, et al. The Best Anticoagulation Therapy in Multiple-Trauma Patients with Mechanical Heart Valves: Evaluation of Latest Guidelines and Studies. Heart Surg Forum. 2015;18(6):E271–4. doi: 10.1532/hsf.1348. [DOI] [PubMed] [Google Scholar]
- 15.Majdan M, Mauritz W, Wilbacher I, Janciak I, Brazinova A, Rusnak M, et al. Traumatic brain injuries caused by traffic accidents in five European countries: outcome and public health consequences. Eur J Public Health. 2013;23(4):682–7. doi: 10.1093/eurpub/cks074. [DOI] [PubMed] [Google Scholar]
- 16.Davis DP, Vadeboncoeur TF, Ochs M, Poste JC, Vilke GM, Hoyt DB. The association between field Glasgow Coma Scale score and outcome in patients undergoing paramedic rapid sequence intubation. J Emerg Med. 2005;29(4):391–7. doi: 10.1016/j.jemermed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 17.Menegazzi JJ, Davis EA, Sucov AN, Paris PM. Reliability of the Glasgow Coma Scale when used by emergency physicians and paramedics. J Trauma. 1993;34(1):46–8. doi: 10.1097/00005373-199301000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Meredith W, Rutledge R, Fakhry SM, Emery S, Kromhout-Schiro S. The conundrum of the Glasgow Coma Scale in intubated patients: a linear regression prediction of the Glasgow verbal score from the Glasgow eye and motor scores. J Trauma. 1998;44(5):839–45. doi: 10.1097/00005373-199805000-00016. [DOI] [PubMed] [Google Scholar]
- 19.Vassar MJ, Lewis FR, Chambers JA, Mullins RJ, O'brien PE, Weigelt JA, et al. Prediction of outcome in intensive care unit trauma patients: a multicenter study of Acute Physiology and Chronic Health Evaluation (APACHE), Trauma and Injury Severity Score (TRISS), and a 24-hour intensive care unit (ICU) point system. J Trauma. 1999;47(2):324–9. doi: 10.1097/00005373-199908000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Donnino MW, Salciccioli JD, Dejam A, Giberson T, Giberson B, Cristia C, et al. APACHE II scoring to predict outcome in post-cardiac arrest. Resuscitation. 2013;84(5):651–6. doi: 10.1016/j.resuscitation.2012.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]