Abstract
Vasospasm immediately after lower extremity arterial bypass may represent an uncommon cause of early graft failure. We report a successful case of catheter-directed, intra-arterial continuous vasodilator infusion to salvage a bypass graft threatened by severe, refractory vasospasm after incomplete response to nicardipine, verapamil, and nitroglycerin boluses. A continuous nitroglycerin infusion was administered for 24 hours, by which time the vasospasm resolved. At 12 months postoperatively, the graft remained patent with normal results of vascular laboratory studies. This report demonstrates that in cases of refractory vasospasm after peripheral bypass, continuous vasodilator infusion can be an effective treatment to prevent early graft failure.
Pathologic vasospasm can be caused by both physiologic and mechanical mechanisms, such as nonocclusive mesenteric ischemia,1 medications,2 local bone and soft tissue trauma, and direct vessel injury.2, 3, 4 Vasospasm has been described in almost every vascular bed, most frequently after coronary artery bypass grafting,5, 6, 7, 8 microvascular anastomoses,9, 10 and renal-mesenteric bypass grafts.11 Indeed, vasospasm is a common occurrence after arterial manipulation during surgery, particularly in the population of younger patients.9, 11 Acute vasospasm generally resolves during a few hours postoperatively with supportive measures, such as fluid resuscitation and electrolyte repletion; it rarely persists long enough to cause permanent deleterious effects. However, if persistent, refractory vasospasm is observed in the setting of a new arterial bypass, this may represent a special case in which bypass patency may be at risk. We describe a case of a lower extremity bypass that was acutely threatened by severe refractory vasospasm and was successfully salvaged with catheter-directed, intra-arterial infusion of vasodilators during a 24-hour period. The patient provided consent for this case report, and it was exempt from Institutional Review Board approval at our institution.
Case report
A 44-year-old man presented to our institution several hours after suffering a low-velocity gunshot wound to the distal calf. The distal tibia and fibula were fractured, displaced, and unstable. On neurovascular evaluation, the foot was insensate with diminished motor function, and no palpable pulses or Doppler signals were obtainable distal to the injury. The decision was made to proceed to the operating room for combined vascular evaluation and orthopedic stabilization.
Two proximal tibial and one transcalcaneal fixator pins were placed, and an A-frame external fixation was fashioned to minimize interference with potential tibial arterial access. After reduction and external fixation, lower extremity arteriography was performed through contralateral common femoral artery access. This demonstrated normal arterial inflow but cessation of flow in all three tibial arteries at the site of the bullet track, consistent with injury of all three tibial arteries (Fig 1). Given the patient's sensory and motor deficits as well as the concern that these deficits may be attributed to ischemia, we thought urgent revascularization of the foot was necessary.
Fig 1.
Initial (left) lower extremity arteriogram (before bypass). Initial arteriography demonstrated normal arterial flow through the superficial femoral, popliteal, proximal anterior tibial, posterior tibial (PT), and peroneal arteries with cessation of flow through all three tibial arteries at the level of the bullet track at the ankle.
As this was a traumatic injury and the inflow vessels were otherwise normal, we elected to perform a tibial-pedal bypass with a short graft, as is our standard practice for traumatic injuries. Contralateral proximal great saphenous vein was harvested. The posterior tibial (PT) artery was exposed in the midcalf through a standard medial approach. The distal PT artery was exposed posterior and inferior to the medial malleolus. A curved Kelly-Wick tunneler was used to fashion a subcutaneous tunnel around the soft tissue defect from the bullet track. Arterial clamping was performed 1 to 2 cm proximal and distal to the arteriotomies with Yasargil clips. The great saphenous vein was reversed, and bypass was performed between the arterial access points.
Immediately after completion of the bypass, the distal pulse was weak, so we performed completion angiography, which revealed sluggish flow in the graft and a string-of-beads appearance just before the proximal anastomosis, potentially consistent with clamp-related spasm (Fig 2). The graft anastomoses were free of stenosis. A 3-mm angioplasty balloon was used in an attempt to treat the focal area of string-of-beads spasm, but this yielded only a transient result. Intra-arterial vasodilators also yielded a temporary improvement. At case completion, the graft pulse was present only with a systolic blood pressure of 120 mm Hg or higher. At this point, we thought further interrogation was unlikely to yield much benefit and that the vasospasm would likely resolve within a few hours postoperatively; therefore, we transferred the patient to the intensive care unit (ICU) for neurovascular monitoring and fluid resuscitation.
Fig 2.
Completion arteriography after posterior tibial (PT)-pedal bypass. After PT-pedal bypass with reversed saphenous vein graft, completion arteriography demonstrated a patent bypass graft with no anastomotic stenosis, graft kinking, or stenosis. However, there was sluggish flow in the graft and a string-of-beads appearance just before the proximal anastomosis, potentially consistent with clamp-related spasm.
Postoperatively, the patient's vascular examination findings declined to the point that 6 hours later, there was no pulse in the graft and no distal Doppler signals despite fluid resuscitation that maintained adequate urine output and systolic blood pressure. Given the concern for early graft failure, he was taken back to the operating room for arteriography. This revealed severe vasospasm of the inflow and outflow PT and a patent bypass graft with worsening sluggish flow (Fig 3). The graft appeared to be at imminent risk of failure. We thought that further endovascular mechanical strategies, such as balloon angioplasty, would be of limited value or counterproductive and that medical treatment of vasospasm would likely be of more benefit.
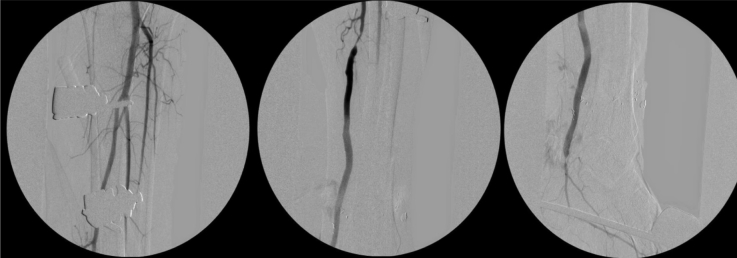
Fig 3.
Arteriogram 6 hours after bypass. Six hours postoperatively, there was no graft pulse and no distal arterial signals, prompting concern for graft failure. However, arteriography demonstrated a patent bypass with no anastomotic stenosis with sluggish flow due to worsening diffuse vasospasm involving all three tibial arteries. PT, Posterior tibial.
Thus, nitroglycerin boluses were administered directly into the PT, but with only a temporary benefit. At this point, we elected to use a protocol of three different vasodilators. This protocol consisted of catheter-directed intra-arterial bolus administration of nicardipine 12.5 mg, verapamil 10 mg, and nitroglycerin in 200-μg bolus aliquots for a total of 2000 μg. Repeated arteriography immediately after vasodilator injection demonstrated moderate improvement in the caliber of PT inflow and outflow and brisker flow through the PT and the bypass graft (Fig 4). There were palpable graft pulses and distal Doppler signals; however, the caliber of the PT was still somewhat narrowed compared with the patient's original prebypass arteriogram. Therefore, we elected to leave a catheter in the tibioperoneal trunk for prolonged catheter-directed intra-arterial infusion of vasodilators. The patient was returned to the ICU with a 6F Destination sheath (Terumo Interventional Systems, Somerset, NJ) and 0.018-inch Quick-Cross catheter (Spectranetics, Colorado Springs, Colo) in place. Nitroglycerin was infused through the catheter at 50 μg/min and heparin was infused at 500 units/h through the side port of the sheath to prevent thrombosis, with a plan to reassess the need for continued vasodilator infusion in 24 hours.
Fig 4.
Arteriography 6 hours after bypass following bolus vasodilator administration. Repeated arteriography after bolus vasodilator infusion with nicardipine, verapamil, and nitroglycerin demonstrated substantial improvement in the vasospasm with brisk flow through the bypass. PT, Posterior tibial.
The following day, there was a strongly palpable pulse in the graft with Doppler signals in the distal foot. In addition, the patient had restoration of normal sensory function in the foot and motor function was limited by pain, thus confirming the suspicion that his neurapraxia was in part due to prolonged ischemia. Further need for continued vasodilator infusion was assessed at 24 hours by holding the nitroglycerin infusion for 2 hours with close evaluation of the graft pulse. The graft pulse did not change during this time; thus, we elected not to obtain a third arteriogram and to remove the catheter and sheath at the bedside in the ICU. The remainder of the patient's postoperative course was unremarkable, and he was discharged to a skilled nursing facility because of his social situation. The patient returned for follow-up 1 month, 6 months, and 12 months postoperatively, at which time duplex ultrasound demonstrated a widely patent bypass graft without stenosis, with normal velocities and waveforms; the toe-brachial index was 0.92.
Discussion
This report demonstrates successful prolonged, catheter-directed, intra-arterial vasodilator infusion used to salvage a bypass graft threatened by vasospasm. Numerous drugs and mixtures of drugs have been used to treat vasospasm; however, there is no conclusive evidence demonstrating the advantage of any particular medication or cocktail of medications over others.7, 9 Vasodilator use during arterial interventions has been well described in a number of scenarios. In the coronary bypass and microsurgical literature, topical vasodilators have been used to maintain graft patency.6, 7, 8, 9, 10 In the cardiac literature, directed radial arterial vasodilator injection has been used to facilitate sheath insertion or to assist with radial artery harvesting.12, 13
Vasospasm has also commonly been described in the renal and mesenteric arteries, especially after arterial bypass11 or in the setting of nonocclusive mesenteric ischemia.1 In both settings, it has classically been described as having a “string-of-sausages” appearance on arteriography with alternating stenoses and dilations. The mainstay of treatment is to correct the underlying cause with fluid administration, optimization of cardiac output, and elimination of vasopressors. In refractory cases, vasodilator infusion with papaverine, nitroglycerin, and prostaglandins has been described, but experience has been largely anecdotal, and the dose, duration, and selection of drugs have not been standardized.14, 15
To treat the vasospasm in our case, we used the protocol of the aggressive treatment arm of the Intra-arterial Vasospasm Trial (IVT),16 a trial investigating pharmacologic modalities for alleviating cerebral vasospasm after subarachnoid hemorrhage. While medications and dosages used were co-opted from the neurointerventional literature on cerebral vasospasm,16 the applicability of these vasodilators to other vascular beds, including those of the lower extremity, appears to be valid. If the IVT study demonstrates superiority of a multidrug cocktail for cerebral vasospasm, it is reasonable to use such a strategy for critical vasospasm in other vascular beds in which such events are too rare to anticipate substantial high-level evidence to guide therapy.
Others have reported treatment of acute peripheral vasospasm with directed intra-arterial injection of bolus vasodilators.17 Continuous vasodilator infusion has been previously described in case reports for treatment of refractory cerebral vasospasm due to subarachnoid hemorrhage.18, 19 However, our report of a continuous catheter-directed, intra-arterial vasodilator infusion for many hours to treat refractory vasospasm after a peripheral surgical bypass is novel. Our patient demonstrated a partial response to on-table high-dose intra-arterial bolus vasodilator administration; however, the response was incomplete and transitory and potentially inconsistent with maintenance of bypass patency. Although balloon angioplasty has been demonstrated to be safe and effective for the treatment of vasospasm in the cerebral circulation and the lower extremity, it was not effective for our patient.2, 20 In addition, heparin infusion through the sheath was performed in our patient as an adjunct to vasodilator infusion to prevent thrombosis of the catheter and sheath.
Vasospasm after arterial bypass is commonly transitory and resolves over several hours with conservative measures, such as adequate fluid resuscitation, and correction of acidosis and electrolyte imbalance. Before vasospasm is treated as the cause of poor graft flow, it is critical to first rule out and to correct any fixed mechanical obstruction, such as graft kinking or compression, flow-limiting dissection, clamp injury, or anastomotic stenosis. The traditional teaching of orthopedic reduction and fixation before arterial bypass is performed is useful as long as it does not delay vascular repair because fracture reduction may improve blood flow and obviate the need for arterial reconstruction, and getting the extremities to appropriate length is critical to constructing the appropriate conduit length. Also, temporary anticoagulation with a heparin infusion can be considered to prevent graft thrombosis when vasospasm is severe.21
Although the presence of refractory vasospasm severe enough to threaten a bypass is rare, the contribution of vasospasm to acute postoperative graft failure may be under-recognized. When such cases are identified and bolus vasodilators alone appear to be an insufficient treatment, the option of catheter-directed vasodilator infusion should be considered.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Trompeter M., Brazda T., Remy C.T., Vestring T., Reimer P. Non-occlusive mesenteric ischemia: etiology, diagnosis, and interventional therapy. Eur Radiol. 2002;12:1179–1187. doi: 10.1007/s00330-001-1220-2. [DOI] [PubMed] [Google Scholar]
- 2.Raval M.V., Gaba R.C., Brown K., Sato K.T., Eskandari M.K. Percutaneous transluminal angioplasty in the treatment of extensive LSD-induced lower extremity vasospasm refractory to pharmacologic therapy. J Vasc Interv Radiol. 2008;19:1227–1230. doi: 10.1016/j.jvir.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Bory M., Mattei M., Egre A., Benichou M., Mostefakara S., Djiane P. [Acute ischemic syndrome and apparently spontaneous spasms of the lower leg arteries] Coeur Med Interne. 1979;18:607–611. [PubMed] [Google Scholar]
- 4.Kaneyama J., Kawarada O., Sakamoto S., Harada K., Ishihara M., Yasuda S. Vasospastic limb ischemia presenting acute and chronic limb ischemia. Ann Vasc Dis. 2014;7:169–172. doi: 10.3400/avd.cr.13-00113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buxton A.E., Goldberg S., Harken A., Hirshfield J., Kastor J.A. Coronary-artery spasm immediately after myocardial revascularization: recognition and management. N Engl J Med. 1981;304:1249–1253. doi: 10.1056/NEJM198105213042101. [DOI] [PubMed] [Google Scholar]
- 6.He G.W., Taggart D.P. Antispastic management in arterial grafts in coronary artery bypass grafting surgery. Ann Thorac Surg. 2016;102:659–668. doi: 10.1016/j.athoracsur.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 7.Mussa S., Guzik T.J., Black E., Dipp M.A., Channon K.M., Taggart D.P. Comparative efficacies and durations of action of phenoxybenzamine, verapamil/nitroglycerin solution, and papaverine as topical antispasmodics for radial artery coronary bypass grafting. J Thorac Cardiovasc Surg. 2003;126:1798–1805. doi: 10.1016/s0022-5223(03)00943-7. [DOI] [PubMed] [Google Scholar]
- 8.He G.W., Taggart D.P. Spasm in arterial grafts in coronary artery bypass grafting surgery. Ann Thorac Surg. 2016;101:1222–1229. doi: 10.1016/j.athoracsur.2015.09.071. [DOI] [PubMed] [Google Scholar]
- 9.Vargas C.R., Iorio M.L., Lee B.T. A systematic review of topical vasodilators for the treatment of intraoperative vasospasm in reconstructive microsurgery. Plast Reconstr Surg. 2015;136:411–422. doi: 10.1097/PRS.0000000000001431. [DOI] [PubMed] [Google Scholar]
- 10.Ricci J.A., Koolen P.G., Shah J., Tobias A.M., Lee B.T., Lin S.J. Comparing the outcomes of different agents to treat vasospasm at microsurgical anastomosis during the papaverine shortage. Plast Reconstr Surg. 2016;138:401e–408e. doi: 10.1097/PRS.0000000000002430. [DOI] [PubMed] [Google Scholar]
- 11.Gewertz B.L., Zarins C.K. Postoperative vasospasm after antegrade mesenteric revascularization: a report of three cases. J Vasc Surg. 1991;14:382–385. doi: 10.1067/mva.1991.29896. [DOI] [PubMed] [Google Scholar]
- 12.Parbhoo R.K., Wetz K., Tschampel M., Pompili V., Schenko E., Mavko L. Innovative approach to preparing radial artery cocktails in response to manufacturer shortages of nitroglycerin and verapamil. Hosp Pharm. 2014;49:628–633. doi: 10.1310/hpj4907-628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dharma S., Shah S., Radadiya R., Vyas C., Pancholy S., Patel T. Nitroglycerin plus diltiazem versus nitroglycerin alone for spasm prophylaxis with transradial approach. J Invasive Cardiol. 2012;24:122–125. [PubMed] [Google Scholar]
- 14.Mitsuyoshi A., Tachibana T., Kondo Y., Momono T., Aoyama H. What we can learn from cases of synchronous acute mesenteric obstruction and nonocclusive mesenteric ischemia: how to reduce the acute mesenteric ischemia-related mortality rate. Ann Vasc Surg. 2016;32:133.e11–133.e17. doi: 10.1016/j.avsg.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 15.Mahlke C., Kühn J.P., Mensel B., Schreiber A., Juretzko A., Steinbach A. Iloprost, prostaglandin E1, and papaverine relax human mesenteric arteries with similar potency. Shock. 2017;48:333–339. doi: 10.1097/SHK.0000000000000866. [DOI] [PubMed] [Google Scholar]
- 16.The Intra-arterial Vasospasm Trial (IVT) https://clinicaltrials.gov/ct2/show/NCT01996436 Available at: Accessed December 8, 2016.
- 17.Mustapha J.A., Saab F., McGoff T., Heaney C., Diaz-Sandoval L., Sevensma M. Tibio-pedal arterial minimally invasive retrograde revascularization in patients with advanced peripheral vascular disease: the TAMI technique, original case series. Catheter Cardiovasc Interv. 2014;83:987–994. doi: 10.1002/ccd.25227. [DOI] [PubMed] [Google Scholar]
- 18.Helbok R., Zangerle A., Chemelli A., Beer R., Benke T., Ehling R. Continuous intra-arterial nimodipine infusion in refractory symptomatic vasospasm after subarachnoid hemorrhage. Springerplus. 2016;5:1807. doi: 10.1186/s40064-016-3495-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mayer T.E., Dichgans M., Straube A., Birnbaum T., Müller-Schunk S., Hamann G.F. Continuous intra-arterial nimodipine for the treatment of cerebral vasospasm. Cardiovasc Intervent Radiol. 2008;31:1200–1204. doi: 10.1007/s00270-008-9346-0. [DOI] [PubMed] [Google Scholar]
- 20.Patel A.S., Griessenauer C.J., Gupta R., Adeeb N., Foreman P.M., Shallwani H. Safety and efficacy of non-compliant balloon angioplasty for the treatment of subarachnoid hemorrhage-induced vasospasm: a multicenter study. World Neurosurg. 2017;98:189–197. doi: 10.1016/j.wneu.2016.10.064. [DOI] [PubMed] [Google Scholar]
- 21.Bruder M., Won S.Y., Kashefiolasl S., Wagner M., Brawanski N., Dinc N. Effect of heparin on secondary brain injury in patients with subarachnoid hemorrhage: an additional 'H' therapy in vasospasm treatment. J Neurointerv Surg. 2017;9:659–663. doi: 10.1136/neurintsurg-2016-012925. [DOI] [PubMed] [Google Scholar]