Abstract
Background
The nulliparous term singleton vertex (NTSV) cesarean delivery rate has been recognized as a meaningful benchmark. Variation in the NTSV cesarean delivery rate among hospitals and providers suggests many hospitals may be able to safely improve their rates. The NTSV cesarean delivery rate at the authors’ institution was higher than state and national averages. This study was conducted to determine the influence of a set of quality improvement interventions on the NTSV cesarean delivery rate.
Methods
From 2008 through 2015, at a single tertiary care academic medical center, a multi-strategy approach that included provider education, provider feedback, and implementation of new policies was used to target evidence-based and inferred factors that influence the NTSV cesarean delivery rate. Data on mode of delivery, maternal outcomes, and neonatal outcomes were collected from birth certificates and administrative claims data. The Cochran-Armitage test and linear regression were used to calculate the p-trend for categorical and continuous variables, respectively.
Results
More than 20,000 NTSV deliveries were analyzed, including more than 15,000 during the intervention period. The NTSV cesarean delivery rate declined from 35% to 21% over eight years. The total cesarean delivery rate declined as well. Increase in meconium aspiration syndrome and maternal transfusion were observed.
Conclusion
Quality improvement initiatives can decrease the NTSV cesarean delivery rate. Any increased incidence of fetal or maternal complications associated with decreased NTSV cesarean delivery rate should be considered in the context of the risks and benefits of vaginal delivery compared to cesarean delivery.
Nearly one third of births in the United States occur with cesarean delivery.1 Compared to vaginal delivery, cesarean delivery is associated with increased morbidity and mortality. There is an increased risk of hemorrhage, deep vein thrombosis, infection, complications from anesthesia, complications with future pregnancies (uterine rupture and morbidly adherent placenta), and neonatal respiratory problems with cesarean delivery compared to vaginal delivery.2 Cesarean delivery also is associated with a longer hospital stay and increased cost.3 Primary cesarean deliveries account for more than half of all cesarean deliveries, and the most common indication for repeat cesarean delivery is previous cesarean delivery.4 Nulliparous term singleton vertex (NTSV) cesarean delivery quantifies the number of nulliparous women with term, singleton pregnancies with the fetus in the vertex presentation who undergo cesarean delivery. Compared to the general obstetric population, this group has fewer risk factors for cesarean delivery. The US Department of Health and Human Services (DHHS) Healthy People 2020 Objectives suggests 23.9% as a target for the NTSV cesarean delivery rate.5 Accordingly, the American College of Obstetricians and Gynecologists (ACOG), The Joint Commission, and the DHHS Healthy People 2020 goals have identified a reduction in NTSV cesarean delivery rate as a meaningful objective.4–6
The rate of NTSV cesarean delivery at our institution was higher than state and national averages.7 Several findings suggest that the NTSV cesarean delivery rate may be modifiable. First, there is significant variation in rates among hospitals and providers.8 Second, elective obstetric practices influence the NTSV cesarean delivery rate.9 Third, among primary cesarean deliveries, subjective indications for cesarean delivery occurred more frequently than objective indications.10 Finally, associations between institutional or environmental factors and the NTSV rate have been noted.11,12
We identified factors that may have contributed to a high rate of NTSV cesarean delivery at our institution. Based on a review of our own quality improvement data and our assessment of relevant environmental factors on our Labor and Delivery Unit, validated by the available published literature on the NTSV cesarean delivery rate, we targeted interpretation and management of fetal heart rate tracings, tolerance for labor, induction of labor, provider awareness of NTSV cesarean delivery rates, and environmental stress. As a meta-analysis of evidenced-based strategies on reducing cesarean delivery rates demonstrated that multifaceted strategies including audit and feedback are effective at reducing cesarean delivery,13 we utilized provider education, provider audit and feedback, and implementation of new policies to address the identified factors.
The purpose of this project was to determine the impact of a series of quality improvement interventions on the NTSV cesarean delivery rate at our institution. This report is intended to describe a multi-strategy approach to target factors that influence the NTSV cesarean delivery rate. This approach can be replicated by other institutions intending to improve NTSV cesarean delivery rate as endorsed by ACOG, the Joint Commission, and DHHS Healthy People 2020.
METHODS
Setting
The setting was a single tertiary care academic medical center performing approximately 4,700 deliveries per year during the study period. Intrapartum care was obstetrician-directed in a laborist-type model. Approximately one third of the deliveries were cared for by employed physicians, one third by private practitioners, and one third by a multi-specialty group. A maternal-fetal medicine group provided intrapartum care for complex patients.
Identification of Five Factors
Non-reassuring fetal heart rate tracing is a leading indication for primary cesarean delivery.10 In 2008, the Eunice Kennedy Shriver National Institute of Child Health and Human Development partnered with ACOG and the Society for Maternal-Fetal Medicine and published guidelines for nomenclature and a three-tiered system categorizing fetal heart rate patterns, as well as suggestions for managing each category of tracing.14 Category II, indeterminate tracings, were recognized as being unable to predict abnormal fetal acidbase status and thus not necessarily warranting management with cesarean delivery. Even Category III tracings may be initially managed with resuscitative measures. Given the frequency with which non-reassuring fetal heart rate tracing is the indication for cesarean delivery, it was reasonable to assume that standardizing language and the approach to management of fetal heart rate tracings, particularly Category II tracings, could decrease NTSV cesarean delivery.
Similar to non-reassuring fetal heart rate tracing, abnormal labor curve or failure of labor to progress also is a common indication for primary cesarean delivery.10 Abnormal labor has been reported to complicate as many as 37% of deliveries of healthy nulliparous women at term.15 Sixty-eight percent of cesarean deliveries in women at term with a fetus in a vertex presentation were performed for abnormal labor.16 For decades, the labor curve was defined by the Friedman curve.17,18 Several authors have challenged this curve and proposed a more modern labor curve that accounts for increased use of anesthesia and increased body mass index (BMI).18–21 As increased BMI has been associated with a longer first stage of labor, it is important to consider the BMI of the contemporary population.22 The modern labor curves support slower cervical change and a later transition from latent to active labor. Adopting these models should increase tolerance for labor and lead to fewer cesarean deliveries for abnormal labor.
Adopting policies that promote vaginal birth after cesarean delivery (VBAC) also may result in fewer NTSV cesarean deliveries. It is apparent that increasing VBAC rates would decrease total cesarean delivery rates. In addition, hospitals with higher rates of VBAC have been shown to have lower rates of NTSV cesarean delivery. Rosenstein et al. suggested that the ability to perform an immediate cesarean delivery may be the common link between higher VBAC rates and decreased NTSV cesarean delivery rate. They also suggest that an underlying culture that supports vaginal birth may increase VBAC rates and reduce primary cesarean delivery rates.23 It is plausible that increasing provider comfort with trial of labor after cesarean delivery (TOLAC) would increase tolerance for labor in low-risk women as well. In 2010, at a Consensus Development Conference, the National Institutes of Health (NIH) recognized TOLAC as a reasonable option for many women with a prior cesarean delivery and called on organizations to facilitate access to TOLAC.24
Increased tolerance for labor may be influenced by a provider’s skill set, including proficiency in management of shoulder dystocia. A diagnosis of gestational diabetes without evidence of macrosomia shifts the practice style toward cesarean delivery, and it has been suggested that provider discretion results in unnecessarily high cesarean delivery rates in this population.25 One possible explanation for this finding is that provider concern for shoulder dystocia leads to preemptive cesarean deliveries. It is reasonable to consider that increasing a provider’s ability to manage shoulder dystocia could therefore reduce the NTSV cesarean delivery rate.
An additional skill that may promote tolerance of labor and vaginal delivery is instrument-assisted or operative vaginal delivery. ACOG considers operative vaginal delivery an intervention that can be used to safely avoid cesarean delivery in the setting of prolonged second stage of labor and non-reassuring fetal heart rate tracings. The rate of operative vaginal delivery has declined in recent decades in the United States contributing to the increase in cesarean delivery rate.26 A recent National Institute of Child Health and Human Development workshop identified training in operative vaginal delivery as a critical component to reduce primary cesarean delivery.4 Based on these data, we assumed that the NTSV cesarean delivery rate could be decreased by increasing a provider’s ability to perform operative vaginal delivery.
Induction of labor, both medically indicated and elective, in nulliparous women at term, has been associated with a significant increase in the risk of cesarean delivery.9,27–29 Both medically indicated and elective induction of labor in nulliparous women at term have been associated with a significant increase in risk of cesarean delivery.9,28,29 Adopting guidelines that limit elective induction and induction in the setting of an unfavorable cervix would be expected to reduce the NTSV cesarean delivery rate.
As individual practice style has been identified as an important determinant of the wide variations in the rates of cesarean delivery among obstetricians, performing audits and providing feedback may increase provider awareness of NTSV cesarean delivery and improve outcomes.30–32 Indeed, Luthy et al. reported that variation in physician practice continues to be an important risk factor for cesarean delivery and described how direct feedback to providers resulted in a reduction in cesarean delivery rate.33
Changes in the environment to better position patients to have a successful vaginal birth and physicians to support a vaginal birth may result in decreased NTSV cesarean delivery rates. For example, increased support to laboring women may reduce the cesarean delivery rate.34,35 This could be accomplished by implementing guidelines that increase the likelihood that a laboring woman would have continuous support. In addition, time constraints for scheduling on the Labor and Delivery Unit, varying operating room staff availability, and physician workload have been recognized as factors that likely impact decision making surrounding cesarean delivery.4 We hypothesized that modifying aspects of the environment that increase physician stress, increase physician demand, or increase doubt in the unit’s ability to efficiently and safely achieve an emergency cesarean delivery may improve a physician’s ability to be tolerant and supportive of labor and reduce the NTSV cesarean delivery.
Interventions and Outcomes
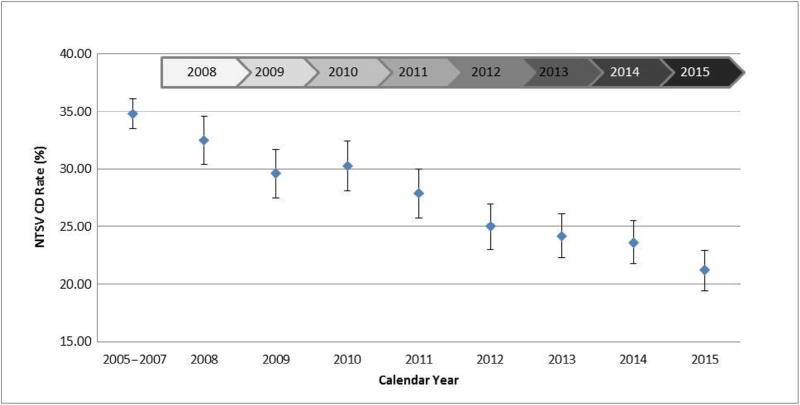
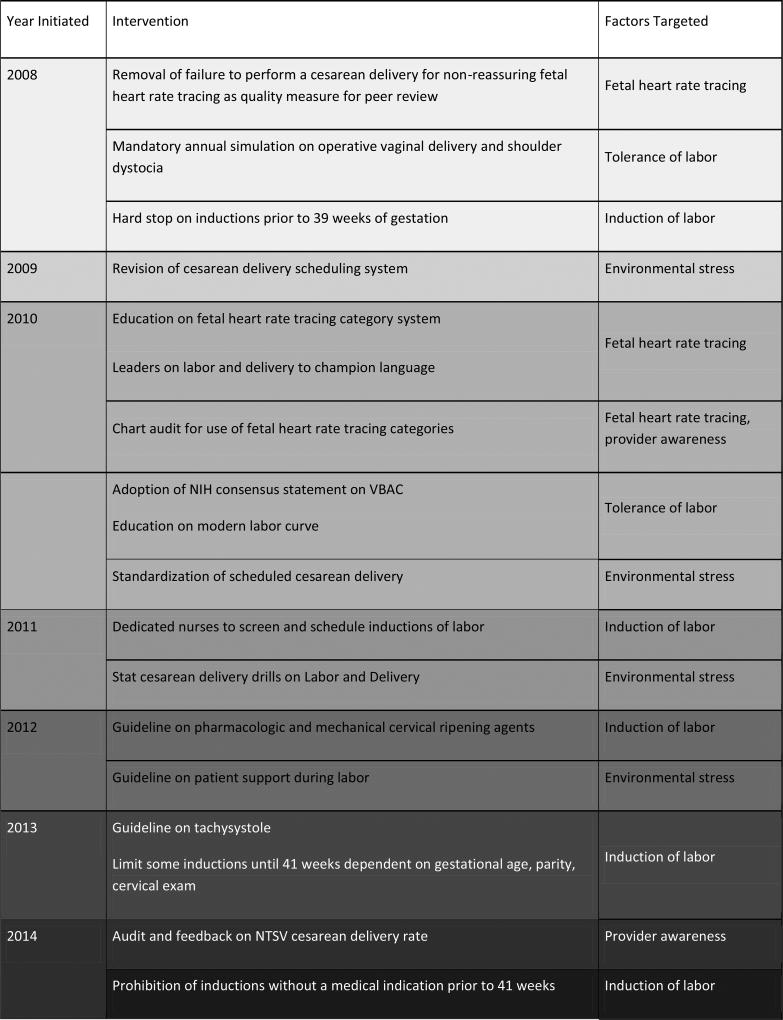
From 2008 through 2015, we implemented a series of interventions to address five factors that may influence the NTSV cesarean delivery rate (Figure 1). We addressed the first factor, standardization in interpretation and management of fetal heart rate tracings, in the following ways:36
We removed “failure to perform a cesarean delivery for non-reassuring fetal heart rate tracing” from our quality measures for our peer review committee and stopped providing provider feedback on this indicator.
We educated providers on the use of category systems to describe fetal heart rate tracings. Large posters and pocket cards with category nomenclature and details of each category were available for reference.
We changed the culture so that communication about fetal heart rate tracings required an assigned category; the term non-reassuring fetal heart rate tracing was considered inadequate at board sign-out and in chart documentation. Leaders on Labor and Delivery were present at board sign-out to champion the transition to this new language.
We conducted a chart audit to ensure that providers were consistently meeting this expectation in documentation.
Figure 1. Interventions and the Nulliparous Term Singleton Vertex (NTSV) Cesarean Delivery (CD) Rate, 2008–2015.
From 2008 through 2015, a series of interventions to address five factors that may influence the NTSV cesarean delivery rate were implemented. NIH, National Institutes of Health; VBAC, vaginal birth after cesarean delivery.
The second factor addressed was provider tolerance for labor:
We utilized mandatory participation in didactic and annual simulation training to address two areas relating to tolerance of labor: operative vaginal delivery and management of shoulder dystocia.
We adopted the NIH consensus statement on VBAC and encouraged providers to strongly consider VBAC for all eligible patients.
We provided education on the modern labor curve and redefined arrest of labor, allowing providers to avoid cesarean delivery based exclusively on failure to demonstrate cervical change at the previously expected rate. Leaders on the Labor and Delivery Unit supported provider patience with the labor curve.
Induction of labor was the third factor targeted in this initiative:
We addressed gestational age at time of induction with a hard stop on inductions prior to 39 weeks of gestation; over time, we advanced to our current state, which incorporates gestational age, parity, and cervical exam into timing of inductions and limits most inductions until 41 weeks of gestation. All requests to schedule an induction are reviewed by dedicated nurses; if they do not meet established criteria for induction, they are eligible to be approved only after review by the Director of Labor and Delivery.
We addressed cervical ripening agents with a departmental guideline outlining appropriate use of pharmacologic and mechanical (Foley bulb) agents.
We created a guideline on tachysystole to reduce the number of iatrogenic cesarean deliveries occurring with induction or augmentation of labor.
The clinical practice environment was the fourth factor we addressed. We focused on environmental factors relating to scheduled cesarean delivery, emergency cesarean delivery, and patient support:
We theorized that an inability to reliably predict when scheduled cesarean deliveries would occur and how long they would take resulted in pressure on the physicians to schedule planned cesarean deliveries for days when they were on call so that they would not interfere with clinical responsibilities off of the Labor and Delivery Unit. As a result, an individual provider would be responsible for more deliveries in a given shift. We hypothesized that the increase in workload, need to multitask, and need to coordinate multiple surgical cases may drive providers to perform intrapartum, unplanned cesarean deliveries earlier than they would otherwise. Accordingly, we changed the scheduling system so that scheduled cesarean deliveries would consistently start on time so providers could commit to scheduling them when they were not covering the Labor and Delivery Unit. We also standardized the steps for scheduled cesarean delivery in order to reduce wasted time, space, and personnel.
We implemented emergency cesarean delivery drills on the Labor and Delivery Unit. The aim of this was to increase provider confidence in the Labor and Delivery Unit’s ability to support a physician in quickly accomplishing an emergency cesarean delivery. We believed this would alleviate pressure to preemptively perform cesarean deliveries due to concern for inability to achieve emergency cesarean delivery with the level of efficiency desired by the provider.
We adopted a more liberal guideline regarding visitors on the Labor and Delivery Unit in order to increase the likelihood that a laboring woman would have continuous support.
The fifth factor, provider awareness of the NTSV cesarean delivery rate, was addressed with audit and feedback:
We implemented an audit and provided all physicians with a biannual letter with personal and departmental rates for NTSV cesarean delivery. We chose to attribute deliveries to providers based on the documented “delivering physician” of record. We recognized that at times (for example, with deliveries occurring at the change of shift), the delivering physician would not have managed a significant portion of the labor; however, we felt these accounted for the minority of a provider’s cesarean deliveries and that over time they would not make a significant difference.
The interventions were largely initiated and implemented by the Director of Labor and Delivery, a board-certified obstetrician, in collaboration with other thought leaders and support from various interdisciplinary committees that included staff from nursing and anesthesiology.
The primary outcome was the rate of NTSV cesarean delivery. We recognize that the NTSV cesarean delivery rate is a proportion and not a rate; however, we chose this terminology to remain consistent with what is commonly used in the literature. Secondary outcomes included gestational age at the time delivery; birthweight; 5-minute Apgar score; and the incidence of neonatal ICU (NICU) admission for greater than 24 hours, meconium aspiration syndrome, shoulder dystocia, episiotomy, third- and fourth-degree laceration, and maternal blood transfusion.
Methods of Evaluation
We collected data on women with NTSV deliveries. Mode of delivery was collected from an internal online birth registry that contains data entered by physicians at the time of delivery; this was supplemented with individual chart review and administrative coding databases. Comorbidities, as well as maternal and neonatal outcomes, were determined using ICD-9-CM codes (gestational hypertension 642.30– 642.34, 642.70–642.74, 642.90–642.94; preeclampsia/eclampsia 642.40–642.44, 642.50–642.54, 642.60–642.64; gestational diabetes 648.80–648.84; episiotomy 72.1, 72.21, 72.31, 73.6; third-degree laceration 664.20, 664.21, 664.24; fourth-degree laceration 664.31, 664.34; meconium aspiration syndrome 770.11, 770.12; shoulder dystocia 660.40, 660.41, 660.43) and online birth registry data. Maternal transfusion data were collected from querying our blood bank database. We compared demographic and clinical characteristics after the start of the interventions (2008–2015) to the years prior to the start of the interventions (2005–2007). Interventions were introduced sequentially beginning in 2008; however, the interventions were sustainable and therefore overlapped in time. According to the policy activities that constitute research at our institution, this work met criteria for operational improvement activities exempt from ethics review.
Data are presented as mean ± standard deviation (SD) or proportion. The Cochran-Armitage test and linear regression were used to calculate the p-trend for categorical and continuous variables, respectively. All data were analyzed using SAS 9.4 (SAS Institute Inc., Cary, North Carolina). All tests were two sided, and p values < 0.05 were considered statistically significant.
RESULTS
Study Population
A total of 51,973 deliveries occurred from 2008 through 2015. The number of annual NTSV deliveries ranged from 1,773 to 2,106, with a total of 15,144 NTSV deliveries over the intervention period. There were no meaningful differences in maternal age or insurance status during the intervention period. The proportion of white women decreased over time, but this was due to an increase in the proportion of women who were of unknown race/ethnicity. The proportion of women with gestational hypertension, preeclampsia/eclampsia, and gestational diabetes fluctuated over time, but these changes were neither consistent nor clinically meaningful (Table 1).
Table 1.
Demographics and Maternal Medical History
| 2005–2007 (N = 5,283) |
2008 (N = 1,934) |
2009 (N = 1,809) |
2010 (N = 1,783) |
2011 (N = 1,773) |
2012 (N = 1,835) |
2013 (N = 1,924) |
2014 (N = 1,980) |
2015 (N = 2,106) |
|
|---|---|---|---|---|---|---|---|---|---|
| Age at delivery (years) | 30.8 + 5.4 | 30.7 ± 5.4 | 30.8 ± 5.2 | 30.8 ± 5.3 | 30.9 ± 5.2 | 30.8 ± 5.1 | 31.2 ± 5.0 | 31.1 ± 5.0 | 31.3 ± 4.7 |
|
| |||||||||
| Race/ethnicity | |||||||||
| Asian | 798 (15.1) | 317 (16.4) | 279 (15.4) | 276 (15.5) | 250 (14.1) | 310 (16.9) | 302 (15.7) | 352 (17.8) | 299 (14.2) |
| Black | 557 (10.5) | 218 (11.3) | 197 (10.9) | 188 (10.5) | 170 (9.6) | 186 (10.1) | 147 (7.6) | 191 (9.6) | 183 (8.7) |
| Hispanic | 206 (3.9) | 77 (4.0) | 84 (4.6) | 70 (3.9) | 80 (4.5) | 63 (3.4) | 81 (4.2) | 80 (4.0) | 75 (3.6) |
| White | 3,163 (59.9) | 1,117 (57.8) | 952 (52.6) | 956 (53.6) | 972 (54.8) | 885 (48.2) | 938 (48.8) | 921 (46.5) | 842 (40.0) |
| Other/Unknown | 559 (10.6) | 205 (10.6) | 297 (16.4) | 293 (16.4) | 301 (17.0) | 391 (21.3) | 456 (23.7) | 436 (22.0) | 707 (33.6) |
|
| |||||||||
| Marital Status | |||||||||
| Single | 973 (18.4) | 418 (21.6) | 423 (23.4) | 408 (22.9) | 484 (27.3) | 566 (30.8) | 667 (34.7) | 834 (42.1) | 774 (36.8) |
| Married | 4,310 (81.6) | 1,516 (78.4) | 1,386 (76.6) | 1,375 (77.1) | 1,289 (72.7) | 1,269 (69.2) | 1,257 (65.3) | 1,146 (57.9) | 1,332 (63.2) |
|
| |||||||||
| Primary Insurance | |||||||||
| Private | 4,364 (82.6) | 1,601 (82.8) | 1,486 (82.1) | 1,459 (81.8) | 1,492 (84.2) | 1,493 (81.4) | 1,563 (81.2) | 1,595 (80.6) | 1,770 (84.0) |
| Public (Medicaid) | 919 (17.4) | 333 (17.2) | 323 (17.9) | 324 (18.2) | 281 (15.8) | 342 (18.6) | 361 (18.8) | 385 (19.4) | 336 (16.0) |
| Maternal medical history | |||||||||
| Gestational Hypertension | 461 (8.7) | 124 (6.4) | 121 (6.7) | 132 (7.4) | 128 (7.2) | 125 (6.8) | 137 (7.1) | 157 (7.9) | 187 (8.9) |
| Preeclapmsia/Eclampsia | 135 (2.6) | 47 (2.4) | 40 (2.2) | 56 (3.1) | 72 (4.1) | 69 (3.8) | 87 (4.5) | 69 (3.5) | 113 (5.4) |
| Gestational Diabetes | 182 (3.4) | 68 (3.5) | 75 (4.1) | 63 (3.5) | 89 (5.0) | 101 (5.5) | 115 (6.0) | 86 (4.3) | 93 (4.4) |
Data are presented as mean ± standard deviation or n (%).
Outcomes
The rate of NTSV cesarean delivery at our institution decreased from 34.8% prior to the intervention period to 21.2% in 2015 (Figure 1, Table 2). Total cesarean delivery rate declined as well from 40.0% to 29.1% (data not shown). There was no change in the rate of operative vaginal delivery among NTSV deliveries.
Table 2.
Outcomes
| 2005–2007 (N = 5,283) |
2008 (N = 1,934) |
2009 (N = 1,809) |
2010 (N = 1,783) |
2011 (N = 1,773) |
2012 (N = 1,835) |
2013 (N = 1,924) |
2014 (N = 1,980) |
2015 (N = 2,106) |
P-Trend Value |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Mode of Delivery | ||||||||||
| Cesarean | 1,837 (34.8) | 629 (32.5) | 535 (29.6) | 540 (30.3) | 494 (27.9) | 459 (25.0) | 466 (24.2) | 468 (23.6) | 446 (21.2) | <0.0001 |
| Vaginal | 3,446 (65.2) | 1,305 (67.5) | 1,274 (70.4) | 1,243 (69.7) | 1,279 (72.1) | 1,376 (75.0) | 1,458 (75.8) | 1,512 (76.4) | 1,660 (78.8) | |
|
| ||||||||||
| Neonatal Outcomes | ||||||||||
| Gestational age at delivery (weeks) | 39.3 ± 1.2 | 39.3 ± 1.1 | 39.3 ± 1.2 | 39.3 ± 1.1 | 39.3 ± 1.1 | 39.5 ± 1.1 | 39.6 ± 1.1 | 39.7 ± 1.1 | 39.6 ± 1.2 | <0.0001 |
| Birth weight (grams) | 3,391 ± 455 | 3,385 ± 447 | 3,377 ± 450 | 3,377 ± 466 | 3,366 ± 447 | 3,370 ± 440 | 3,373 ± 457 | 3,351 ± 460 | 3,346 ± 455 | 0.0007 |
| Apgar 1 minute <5 | 109 (2.1) | 38 (2.0) | 52 (2.9) | 64 (3.6) | 55 (3.1) | 58 (3.2) | 60 (3.1) | 73 (3.7) | 117 (5.6) | <0.0001 |
| Apgar 5 minute <5 | 10 (0.2) | 3 (0.2) | 3 (0.2) | 4 (0.2) | 6 (0.3) | 2 (0.1) | 1 (0.1) | 3 (0.2) | 8 (0.4) | 0.5697 |
| NICU Admission >24 hours | 339 (6.4) | 148 (7.7) | 150 (8.3) | 138 (7.7) | 134 (7.6) | 116 (6.3) | 123 (6.4) | 129 (6.5) | 155 (7.4) | 0.9417 |
| Meconium aspiration syndrome | 5 (0.1) | 4 (0.2) | 5 (0.3) | 3 (0.2) | 8 (0.5) | 7 (0.4) | 9 (0.5) | 10 (0.5) | 19 (0.9) | <0.0001 |
| Shoulder dystocia | 38 (0.7) | 18 (0.9) | 13 (0.7) | 19 (1.1) | 23 (1.3) | 15 (0.8) | 17 (0.9) | 14 (0.7) | 17 (0.8) | 0.7340 |
|
| ||||||||||
| Maternal Outcomes | ||||||||||
| Episiotomy | 827 (15.7) | 219 (11.3) | 166 (9.2) | 186 (10.4) | 177 (10.0) | 155 (8.4) | 108 (5.6) | 62 (3.1) | 61 (2.9) | <0.0001 |
| Third Degree Laceration | 234 (4.4) | 67 (3.5) | 90 (5.0) | 80 (4.5) | 68 (3.8) | 69 (3.8) | 50 (2.6) | 43 (2.2) | 48 (2.3) | <0.0001 |
| Fourth Degree Laceration | 21 (0.4) | 3 (0.2) | 6 (0.3) | 8 (0.4) | 6 (0.3) | 6 (0.3) | 7 (0.4) | 5 (0.3) | 8 (0.4) | 0.8696 |
| Blood transfusion | 31 (0.6) | 25 (1.3) | 21 (1.2) | 24 (1.3) | 20 (1.1) | 23 (1.3) | 22 (1.1) | 30 (1.6) | 30 (1.4) | 0.0005 |
Data are presented as mean ± standard deviation or n (%).
NICU, neonatal ICU.
The mean gestational age at the time of delivery increased from 39.3 to 39.6 weeks. There was a decline in average neonatal birth weight by approximately 45 grams. There was no difference in the incidence of 5-minute Apgar score less than 5 and no change in the incidence of NICU admission for greater than 24 hours. There was an increase in meconium aspiration syndrome over the course of our study, reaching an incidence of 0.9% in 2015. There was no change in the incidence of shoulder dystocia.
With the decline in cesarean delivery rate, there was a decline in the incidence of episiotomy and third-degree lacerations. The incidence of fourth-degree lacerations remained stable. The incidence of maternal blood transfusion increased to 1.4% by 2015, but sub-analysis—excluding the baseline years 2005–2007—demonstrated no significant trend in the incidence of transfusion (p = 0.49).
DISCUSSION
Nationwide, there has been a decline in the NTSV cesarean delivery that has exceeded the pace of decline of the overall cesarean delivery rate. In Massachusetts, the decline in NTSV cesarean delivery rate has exceeded all other states with a 19% decrease from 2009 to 2013.7 In approximately that same time span, we implemented a multi-strategy approach including provider education, provider feedback, and implementation of new policies to target the following five factors that may influence the NTSV cesarean delivery rate: interpretation and management of fetal heart rate tracings, provider tolerance for labor, induction of labor, provider awareness of NTSV cesarean delivery rate, and environmental stress. With the implementation of these quality improvement interventions aimed at decreasing NTSV cesarean delivery rate, our institution demonstrated a 39% decrease in NTSV cesarean delivery rate, meeting the DHHS Healthy People 2020 goal. In addition, the findings for secondary outcomes are reassuring. The small decline in mean birth weight of approximately 45 grams to a mean of 3,346 grams is unlikely to be clinically significant with regard to risk of NTSV cesarean delivery. The increase in the incidence of preeclampsia and diabetes would be expected to increase the rate of NTSV cesarean delivery; however, we did not observe this.
An increase in meconium aspiration syndrome was observed; however, the incidence peaked at 0.9%, which is lower than the reported incidence of 1.8% in term deliveries.37 As labor and vaginal delivery are significant risk factors for meconium aspiration syndrome, one could anticipate such an increase may accompany increasing vaginal delivery rates. The mean 5-minute Apgar score and the rate of NICU admission for more than 24 hours were stable throughout the study period. We did not detect a difference in the rate of neonatal demise (data not presented), but this study was not powered to do so. Our data are insufficient to draw a conclusion about the clinical significance of the increase in the incidence of meconium aspiration syndrome that may accompany a decrease in NTSV cesarean delivery.
The incidence of maternal transfusion increased from approximately 0.6% to 1.4%. There was no significant difference in the incidence of maternal transfusion from 2008 through 2015. An increase in maternal transfusion would not be expected, as the risk of maternal transfusion is higher with cesarean delivery compared to vaginal delivery. It is possible, however, that longer labors that result from an increase in tolerance for labor may increase the incidence of blood transfusion associated with vaginal delivery. Increasing age and BMI also are risk factors for blood transfusion and may contribute to this risk. Alternatively, the incidence of transfusion reported during the baseline years (2005–2007) may simply be an outlier. Any increase in the risk of blood transfusion that results directly from interventions that decrease the NTSV cesarean delivery rate should be considered in the context of the risks and benefits of vaginal delivery compared to primary cesarean delivery; the risk of transfusion with primary cesarean delivery is approximately 2%–4%.2
A significant unintended consequence was encountered. From 2005 to the end of 2014, the average census on Labor and Delivery increased from six to eight patients, and the average number of minutes that beds were occupied increased steadily. Between 2011 and 2015, the average number of minutes that a single patient occupied a bed on Labor and Delivery increased by 116 minutes. As the rate of NTSV cesarean delivery decreased, the amount of time that patients occupied beds on the Labor and Delivery Unit increased, leading to a perception of higher volume despite a relatively stable number of annual deliveries. We believe this is primarily a direct result of the decrease in NTSV cesarean delivery rate; there were no other changes in processes that would impact this. This higher rate of bed occupancy is likely due to the increased amount of time involved in labor and vaginal delivery compared to cesarean delivery.
There are limitations to our study. Because we used a series of interventions targeting drivers of NTSV cesarean delivery, and the effects may be cumulative, we cannot measure the impact of any single intervention. We utilized administrative data and ICD-9-CM codes. We did not have data on BMI, and increased BMI is associated with increased risk of cesarean delivery. However, in the general population, BMI has been increasing, and there is no reason to believe our sample of patients differs from the general population with regard to BMI. If BMI increased over time in our sample of women, one would expect to observe less of a reduction in NTSV cesarean delivery rate than would be observed in a sample with stable BMI. There may be confounding factors that we did not appreciate that affect NTSV cesarean delivery rate. Midwifery care was offered to approximately one third of the patients at our institution beginning in March 2014.We were unable to measure how this may have contributed to the reduction in NTSV cesarean delivery in the final 21 months of our study. A recent Cochrane Review reported no difference in cesarean delivery rates between women receiving care in a midwife-led continuity model of care and those receiving care in other models.38 Other publications suggest that midwifery care may be associated with lower rates of cesarean delivery,39 and it is plausible that the presence of midwives on the Labor and Delivery Unit could contribute to a culture that would promote vaginal birth and reduce the NTSV cesarean delivery rate.
One physician champion served as the leader of this initiative throughout the course of this study; this may be difficult to achieve at other institutions. Senior obstetricians’ interest in the provision and quality of intrapartum care may be linked to cesarean delivery rates.12 We believe the involvement of formal leaders, thought leaders, and additional stakeholders was an important element in the design of this project and would recommend that this aspect be incorporated into a comprehensive quality improvement project intended to reduce the rate of NTSV cesarean delivery.
The next step at our institution aimed to reduce NTSV cesarean delivery rate may be to limit admission to Labor and Delivery in early labor. First birth early admission rates account for a significant portion of the variation in NTSV cesarean delivery rates.9 Further study is needed to evaluate decreased rate of NTSV cesarean delivery with maternal and neonatal outcomes.
CONCLUSION
A reduction in NTSV cesarean delivery rate may have a substantial impact on health care. Hospitals can implement quality improvement initiatives reported here to decrease NTSV cesarean delivery rate. Aspects of this project such as provider education, provider feedback, and change in policy are generalizable to many institutions. Interventions to address environmental or cultural concerns can be customized to meet the needs of a particular institution. We believe the involvement of formal leaders and thought leaders was an important element in the design of this project and would recommend that this feature be incorporated into a comprehensive quality improvement project intended to reduce the rate of NTSV cesarean delivery.
Supplementary Material
Acknowledgments
Funding. The work reported in this article was conducted with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic health care centers. Related grant funding was received from the Robert Wood Johnson Foundation, the Rx Foundation, and the CRICO/Harvard Risk Management Foundation.
Footnotes
Conflicts of Interest. All authors report no conflicts of interest.
ONLINE-ONLY CONTENT
See the online version of this article for Video 1. Reducing Cesarean Deliveries.
Contributor Information
Mary A. Vadnais, Department of Obstetrics, Gynecology and Reproductive Biology, Harvard Medical School, and Maternal Fetal Medicine Physician, Department of Obstetrics and Gynecology, Beth Israel Deaconess Medical Center and Harvard Vanguard Medical Associates, Boston.
Michele R. Hacker, Obstetrics and Gynecology, Department of Obstetrics, Gynecology and Reproductive Biology, Harvard Medical School, and Vice Chair for Research, Department of Obstetrics and Gynecology, Beth Israel Deaconess Medical Center.
Neel T. Shah, Obstetrics and Gynecology, Department of Obstetrics, Gynecology and Reproductive Biology, Harvard Medical School, and Associate Faculty, Ariadne Labs for Health Systems Innovation, Boston.
JoAnn Jordan, Department of Obstetrics and Gynecology, Beth Israel Deaconess Medical Center.
Anna M. Modest, Department of Obstetrics and Gynecology, Beth Israel Deaconess Medical Center.
Molly Siegel, Department of Obstetrics and Gynecology, University of California, San Francisco.
Toni H. Golen, Obstetrics and Gynecology, Department of Obstetrics, Gynecology and Reproductive Biology, Harvard Medical School, and Vice Chair, Quality and Safety, Department of Obstetrics and Gynecology, Beth Israel Deaconess Medical Center.
References
- 1.Hamilton BE, et al. Births: preliminary data for 2013. [Accessed Nov 22, 2016];Natl Vital Stat Rep. 2014 May 29;63:1–20. http://www.cdc.gov/nchs/data/nvsr/nvsr63/nvsr63_02.pdf. [Google Scholar]
- 2.Hammad IA, et al. Complications with cesarean delivery: a review of Maternal-Fetal Medicine Units Network publications. J Matern Fetal Neonatal Med. 2014;27:463–474. doi: 10.3109/14767058.2013.818970. [DOI] [PubMed] [Google Scholar]
- 3.Childbirth Connection. The cost of having a baby in the United States. [Accessed Nov 22, 2016];Truven Health Analytics. 2013 Jan; http://transform.childbirthconnection.org/wp-content/uploads/2013/01/Cost-of-Having-a-Baby1.pdf.
- 4.Spong CY, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol. 2012;120:1181–1193. doi: 10.1097/aog.0b013e3182704880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. [Accessed Nov 22, 2016];Healthy people 2020. 2016 https://www.healthypeople.gov/2020.
- 6.The Joint Commission. Specifications manual for Joint Commission National Quality Measures (v2016A1): measure information form. [Accessed Nov 22, 2016];Perinatal Care PC-02: Cesarean Birth. 2016 https://manual.jointcommission.org/releases/TJC2016A1/MIF0167.html.
- 7.Osterman MJK, Martin JA. Trends in low-risk cesarean delivery in the United States, 1990–2013. [Accessed Nov. 22, 2016];Natl Vital Stat Rep. 2014 Nov 5;63:1–16. http://www.cdc.gov/nchs/data/nvsr/nvsr63/NVSR63_06.pdf. [PubMed] [Google Scholar]
- 8.Brennan DJ, et al. Comparative analysis of international cesarean delivery rates using 10-group classification identifies significant variation in spontaneous labor. Am J Obstet Gynecol. 2009;201:308, e1–8. doi: 10.1016/j.ajog.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 9.Main EK, et al. Is there a useful cesarean birth measure? Assessment of the nulliparous term singleton vertex cesarean birth rate as a tool for obstetric quality improvement. Am J Obstet Gynecol. 2006;194:1644–1651. doi: 10.1016/j.ajog.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 10.Barber EL, et al. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118:29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coonrad DV, et al. Nulliparous term singleton vertex cesarean delivery rates: institutional and individual level predictors. Am J Obstet Gynecol. 2008;198(694):e1–11. doi: 10.1016/j.ajog.2008.03.026. [DOI] [PubMed] [Google Scholar]
- 12.Alfirevic Z, Edwards G, Platt MJ. The impact of delivery suite guidelines on intrapartum care in "standard primigravida". Eur J Obstet Gynecol Reprod Biol. 2004;115:28–31. doi: 10.1016/j.ejogrb.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 13.Chaillet N, Dumont A. Evidence-based strategies for reducing cesarean section rates: a meta-analysis. Birth. 2007;34:53–64. doi: 10.1111/j.1523-536X.2006.00146.x. [DOI] [PubMed] [Google Scholar]
- 14.American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 106: intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009;114:192–202. doi: 10.1097/AOG.0b013e3181aef106. [DOI] [PubMed] [Google Scholar]
- 15.Kjaergaard H, et al. Incidence and outcomes of dystocia in the active phase of labor in term nulliparous women with spontaneous labor onset. Acta Obstet Gynecol Scand. 2009;88:402–407. doi: 10.1080/00016340902811001. [DOI] [PubMed] [Google Scholar]
- 16.Gifford DS, et al. Lack of progress in labor as a reason for cesarean. Obstet Gynecol. 2000;95:589–595. doi: 10.1016/s0029-7844(99)00575-x. [DOI] [PubMed] [Google Scholar]
- 17.Friedman E. The graphic analysis of labor. Am J Obstet Gynecol. 1954;68:1568–1575. doi: 10.1016/0002-9378(54)90311-7. [DOI] [PubMed] [Google Scholar]
- 18.Zhang J, et al. The natural history of the normal first stage of labor. Obstet Gynecol. 2010;115:705–710. doi: 10.1097/AOG.0b013e3181d55925. [DOI] [PubMed] [Google Scholar]
- 19.Zhang J, Troendle JF, Yancey MK. Reassessing the labor curve in nulliparous women. Am J Obstet Gynecol. 2002;187:824–828. doi: 10.1067/mob.2002.127142. [DOI] [PubMed] [Google Scholar]
- 20.Laughon SK, et al. Changes in labor patterns over 50 years. Am J Obstet Gynecol. 2012;206:419, e1–9. doi: 10.1016/j.ajog.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neal JL, et al. “Active labor” duration and dilation rates among low-risk, nulliparous women with spontaneous labor onset: a systematic review. J Midwifery Womens Health. 2010;55:308–318. doi: 10.1016/j.jmwh.2009.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kominiarek MA, et al. Contemporary labor patterns: the impact of maternal body mass index. Am J Obstet Gynecol. 2011;205:244, e1–8. doi: 10.1016/j.ajog.2011.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenstein MG, et al. Association between vaginal birth after cesarean delivery and primary cesarean delivery rates. Obstet Gynecol. 2013;122:1010–1017. doi: 10.1097/AOG.0b013e3182a91e0f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Institutes of Health Consensus Development Conference Panel. National Institutes of Health Consensus Development conference statement: vaginal birth after cesarean: new insights March 8–10, 2010. Obstet Gynecol. 2010;115:1279–1295. doi: 10.1097/AOG.0b013e3181e459e5. [DOI] [PubMed] [Google Scholar]
- 25.Naylor CD, et al. Cesarean delivery in relation to birth weight and gestational glucose tolerance: pathophysiology or practice style? JAMA. 1996;275:1165–1170. [PubMed] [Google Scholar]
- 26.Committee on Practice Bulletins–Obstetrics. ACOG Practice Bulletin No. 154: operative vaginal delivery. Obstet Gynecol. 2015;126:e56–e65. doi: 10.1097/AOG.0000000000001147. [DOI] [PubMed] [Google Scholar]
- 27.Seyb ST, et al. Risk of cesarean delivery with elective induction of labor at term in nulliparous women. Obstet Gynecol. 1999;95:600–607. doi: 10.1016/s0029-7844(99)00377-4. [DOI] [PubMed] [Google Scholar]
- 28.Yeast JD, Jones A, Poshkin M. Induction of labor and the relationship to cesarean delivery: a review of 7001 consecutive inductions. Am J Obstet Gynecol. 1999;180:628–633. doi: 10.1016/s0002-9378(99)70265-6. [DOI] [PubMed] [Google Scholar]
- 29.Ehrenthal DB, Jiang X, Strobino DM. Labor induction and the risk of cesarean delivery among nulliparous women at term. Obstet Gynecol. 2010;116:35–42. doi: 10.1097/AOG.0b013e3181e10c5c. [DOI] [PubMed] [Google Scholar]
- 30.Goyert GL, et al. The physician factor in cesarean birth rates. N Engl J Med. 1989;320:706–709. doi: 10.1056/NEJM198903163201106. [DOI] [PubMed] [Google Scholar]
- 31.Robson MS, Scudamore IW, Walsh SM. Using the medical audit cycle to reduce cesarean delivery rates. Am J Obstet Gynecol. 1996;174:199–205. doi: 10.1016/s0002-9378(96)70394-0. [DOI] [PubMed] [Google Scholar]
- 32.Scarella A, et al. Medical audit using the Ten Group Classification System and its impact on the cesarean section rate. Eur J Obstet Gynecol Reprod Biol. 2011;154:136–140. doi: 10.1016/j.ejogrb.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 33.Luthy DA, et al. Physician contribution to a cesarean delivery risk model. Am J Obstet Gynecol. 2003;88:1579–1585. doi: 10.1067/mob.2003.389. [DOI] [PubMed] [Google Scholar]
- 34.Hodnett ED, et al. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2013;(7):CD003766. doi: 10.1002/14651858.CD003766.pub5. [DOI] [PubMed] [Google Scholar]
- 35.Kennell J, et al. Continuous emotional support during labor in a US hospital. A randomized controlled trial. JAMA. 1991 May 1;265:2197–2201. [PubMed] [Google Scholar]
- 36.Vadnais MA, Golen TH. Documentation improvements following multidisciplinary educational program on electronic fetal heart rate tracings. J Matern Fetal Neonatal Med. 2011;24:741–744. doi: 10.3109/14767058.2010.529971. [DOI] [PubMed] [Google Scholar]
- 37.Singh B, et al. Meconium aspiration syndrome remains a significant problem in the NICU: outcomes and treatment patterns in term neonates admitted for intensive care during a ten-year period. J Perinatol. 2009;29:497–503. doi: 10.1038/jp.2008.241. [DOI] [PubMed] [Google Scholar]
- 38.Sandall J, et al. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev. 2016;(4):CD004667. doi: 10.1002/14651858.CD004667.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.King TL. Preventing primary cesarean sections: intrapartum care. Semin Perinatol. 2012;36:357–364. doi: 10.1053/j.semperi.2012.04.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.