Abstract
Background
Cardiovascular disease (CVD) is a leading cause of death among adults with type 2 diabetes mellitus (T2D). We recently reported that glycemic control in patients with T2D can be significantly improved through a continuous care intervention (CCI) including nutritional ketosis. The purpose of this study was to examine CVD risk factors in this cohort.
Methods
We investigated CVD risk factors in patients with T2D who participated in a 1 year open label, non-randomized, controlled study. The CCI group (n = 262) received treatment from a health coach and medical provider. A usual care (UC) group (n = 87) was independently recruited to track customary T2D progression. Circulating biomarkers of cholesterol metabolism and inflammation, blood pressure (BP), carotid intima media thickness (cIMT), multi-factorial risk scores and medication use were examined. A significance level of P < 0.0019 ensured two-tailed significance at the 5% level when Bonferroni adjusted for multiple comparisons.
Results
The CCI group consisted of 262 participants (baseline mean (SD): age 54 (8) year, BMI 40.4 (8.8) kg m−2). Intention-to-treat analysis (% change) revealed the following at 1-year: total LDL-particles (LDL-P) (− 4.9%, P = 0.02), small LDL-P (− 20.8%, P = 1.2 × 10−12), LDL-P size (+ 1.1%, P = 6.0 × 10−10), ApoB (− 1.6%, P = 0.37), ApoA1 (+ 9.8%, P < 10−16), ApoB/ApoA1 ratio (− 9.5%, P = 1.9 × 10−7), triglyceride/HDL-C ratio (− 29.1%, P < 10−16), large VLDL-P (− 38.9%, P = 4.2 × 10−15), and LDL-C (+ 9.9%, P = 4.9 × 10−5). Additional effects were reductions in blood pressure, high sensitivity C-reactive protein, and white blood cell count (all P < 1 × 10−7) while cIMT was unchanged. The 10-year atherosclerotic cardiovascular disease (ASCVD) risk score decreased − 11.9% (P = 4.9 × 10−5). Antihypertensive medication use was discontinued in 11.4% of CCI participants (P = 5.3 × 10−5). The UC group of 87 participants [baseline mean (SD): age 52 (10) year, BMI 36.7 (7.2) kg m−2] showed no significant changes. After adjusting for baseline differences when comparing CCI and UC groups, significant improvements for the CCI group included small LDL-P, ApoA1, triglyceride/HDL-C ratio, HDL-C, hsCRP, and LP-IR score in addition to other biomarkers that were previously reported. The CCI group showed a greater rise in LDL-C.
Conclusions
A continuous care treatment including nutritional ketosis in patients with T2D improved most biomarkers of CVD risk after 1 year. The increase in LDL-cholesterol appeared limited to the large LDL subfraction. LDL particle size increased, total LDL-P and ApoB were unchanged, and inflammation and blood pressure decreased.
Trial registration Clinicaltrials.gov: NCT02519309. Registered 10 August 2015
Electronic supplementary material
The online version of this article (10.1186/s12933-018-0698-8) contains supplementary material, which is available to authorized users.
Keywords: Ketosis, Carbohydrate restriction, Type diabetes, Cardiovascular disease, Risk factor, Atherogenic dyslipidemia, Inflammation, Blood pressure, Antihypertensive medication, Continuous remote care
Background
Despite advances in the prevention and treatment of cardiovascular disease (CVD), it remains the leading cause of death in adults across the world [1]. Specifically, among those with type 2 diabetes (T2D) in the US, CVD accounts for 44% of mortality [2]. T2D rates have doubled over the past 20 years [3] and CVD risk increases two to fourfold with a diagnosis of T2D [4], warranting the identification of novel interventions to combat T2D. Intensive lifestyle interventions with dietary carbohydrate restriction [5–8], including the recently described continuous remote care model, which helps patients with T2D sustain nutritional ketosis [9, 10], have demonstrated improved glycemic control concurrent with medication reduction. However, the long-term sustainability and impact of these interventions on CVD risk and lipid profiles remains a subject of debate [11, 12].
Atherogenic dyslipidemia, a known risk factor for CVD [13], is highly prevalent in patients with T2D [14] and tightly linked to high-carbohydrate diets [15]. The condition is characterized by increased triglycerides, decreased high-density lipoprotein cholesterol concentration (HDL-C) and increased small low-density lipoprotein particle number (small LDL-P). Evidence suggests that increased very low-density lipoprotein particle number (VLDL-P), and in particular large VLDL-P, may be one of the key underlying abnormalities in atherogenic dyslipidemia [14, 16–18]. Elevated concentrations of small LDL are often associated with increased total LDL particle number (LDL-P) and ApoB [19, 20]. Particularly in patients with insulin resistance and T2D, elevated LDL-P and ApoB may exist even with normal to low LDL-C values [19, 21, 22]. Reliance on LDL-C for risk assessment in T2D patients may miss the impact of atherogenic dyslipidemia and elevated LDL-P. Researchers have proposed that LDL-P or ApoB may be superior to LDL-C as a predictor of CVD [22–25].
Previous studies of carbohydrate restriction of up to 1-year found a consistent decrease in triglycerides and increase in HDL-C, while LDL-C slightly increased or decreased [15, 26–28]. Although LDL-C is a risk factor for CVD, low LDL-C may belie elevations in small LDL, LDL-P or ApoB. Conversely, increased LDL-C with a low carbohydrate diet may primarily reflect the large LDL subfraction and may not increase CVD risk if total LDL-P or ApoB concentrations are unchanged or decline.
Inflammation, as assessed by elevated high-sensitivity C-reactive protein (hsCRP) or white blood cell count (WBC) [29–32], is an independent CVD risk factor and is involved in all stages of atherogenesis [33]. Inflammation is often observed in T2D concurrent with atherogenic dyslipidemia [34] and represents an additional CVD risk even in individuals with low to normal LDL-C [35, 36]. Hypertension is an additive risk factor in this patient population. Tighter blood pressure control has been associated with reduction in the risk of deaths related to diabetes. This included decreased CVD, stroke and microvascular complications [37].
For this open label, non-randomized, controlled, before-and-after study, we investigated the effects of a continuous care intervention (CCI) on CVD risk factors. The CCI included individualized digital support with telemedicine, health coaching, education in nutritional ketosis, biometric feedback, and an online peer-support community. Given the multi-faceted pathophysiology of CVD, we assessed the 1-year responses in several biomarkers related to cholesterol and lipoprotein metabolism, blood pressure, and inflammation, as well as carotid intima media thickness (cIMT) and medication use. Some results were previously reported in relation to glycemic control [10] and are presented here as they pertain to the effectiveness of the intervention and CVD risk (i.e. body weight and hemoglobin A1c).
Methods
Intervention
As previously described [9, 10], we utilized a prospective, longitudinal study design with a cohort of patients with T2D from the greater Lafayette, Indiana, USA, region who self-selected to participate in the CCI (Clinicaltrials.gov Identifier NCT02519309). Participants in the CCI were provided access to a web-based software application (app) for biomarker reporting and monitoring including body weight, blood glucose and blood betahydroxybutyrate (BHB; a marker of ketosis). The remote care team consisted of a health coach and physician or nurse practitioner who provided nutritional advice and medication management, respectively. Participants were guided by individualized nutrition recommendations to achieve and sustain nutritional ketosis. Notably, if participants reported headaches, constipation or lightheadedness, the remote care team recommended individualized adjustments to sodium and fluid intake [10]. CCI participants self-selected to receive education via either an onsite group setting (CCI-onsite) or via the app (CCI-web). There were no instructions given to the CCI group on counting or restricting calories. The CCI participants were instructed to restrict carbohydrate, eat protein in moderation, and consume fat to satiety from the start of the study. Due to the well-known systematic errors associated with dietary records in an obese population [38], we chose not to collect diet records. Social support was provided via an online peer community. Inclusion and exclusion criteria were previously described [10]. This study was approved by the Franciscan Health Lafayette Institutional Review Board, and participants provided written informed consent.
The frequency of glucose and BHB monitoring, along with glycemic control medication management, were previously described in detail [9, 10]. Briefly, glucose and BHB levels were initially obtained daily using a blood glucose and ketone meter (Precision Xtra, Abbott; Alameda, CA, USA) to personalize nutrition recommendations and also provide a marker of adherence. The frequency of measurement was modified by the care team for each participant based on individual care needs and preferences. For participants with a history of hypertension, a home automatic sphygmomanometer was supplied. Participants reported their home readings in the app daily to weekly depending on recent control and instruction from the supervising physician. Antihypertensive prescriptions were adjusted based on home readings and reported symptoms. Health coaches responded to patient app reported readings of systolic blood pressure less than 110 mmHg with specific questions about symptoms of hypotension. Following resolution of hypertension, diuretics were the first antihypertensive medications to be discontinued, followed by beta blockers, unless the participant had a history of coronary artery disease. Angiotensin-converting-enzyme inhibitors (ACEs) and angiotensin II receptor blockers (ARBs) were generally continued due to known renal protection with diabetes [39, 40]. Statin medications were adjusted when appropriate to maintain a goal of LDL-P under 1000 nmol L−1 or participant preference after full risk—benefit discussion.
To track T2D progression in the same geography and health system as the CCI, an independent cohort of patients with T2D who received usual care (UC) were recruited. These patients were referred to registered dietitians providing dietary advice according to American Diabetes Association guidelines [41].
Outcome measures
Anthropometrics and vital signs for the CCI group were obtained at baseline, 70 days, and 1 year. A stadiometer was used to assess height and used in the calculation of body mass index. A calibrated scale in the clinic measured weight to the nearest 0.1 lb (Model 750, Detecto; Webb City, MO, USA) and values were converted to kg. Participants were provided a cellular-connected home scale for daily weight. Blood pressure was obtained manually by trained staff after participants rested in a seated position for 5 min. Adverse events were reported and reviewed by the Principal Investigator and the Institutional Review Board.
Fasting blood draws for the CCI group were collected at baseline, 70 days, and 1-year follow-up (ranging from 11 to 15 months). Blood analytes were determined via standard procedures at a Clinical Laboratory Improvement Amendment (CLIA) accredited laboratory on the day of sample collection or from stored serum. Serum aliquots were stored at − 80 °C and thawed for determination of ApoB, ApoA1, total cholesterol, triglycerides, and direct HDL-C concentrations by FDA approved methods (Cobas c501, Roche Diagnostics; Indianapolis, IN, USA). LDL was calculated using the Friedewald equation [42]. Lipid subfractions were quantified using clinical NMR LipoProfile® (LabCorp, Burlington NC, USA; [43]). The LipoProfile3 algorithm used in the present investigation was used previously to relate lipid subfractions to CVD risk [35, 44, 45]. The NMR-derived lipoprotein insulin resistance score (LP-IR) is proposed to be associated with the homeostasis model assessment of insulin resistance (HOMA-IR) and glucose disposal rate (GDR) [46]. The multifactorial 10-year atherosclerotic cardiovascular disease (ASCVD) risk score was also computed [47].
Anthropometrics, vital signs and fasting blood draws for the UC group were obtained at baseline and 1 year as described above using the same clinical facilities and laboratory and data collection methods. Home biometrics for the UC group were not tracked and 70-day outcomes were not measured.
Carotid ultrasonography for cIMT measure was performed at baseline and 1 year in CCI and UC groups to characterize atherosclerotic risk. Ultrasound technicians were trained according to protocols that were previously tested and used to assess subclinical atherosclerosis [48, 49]. The right and left common carotid arteries were imaged 1 cm distal to the carotid bulb using a L12-3 multi-frequency linear-array transducer attached to a high-resolution ultrasound system (Phillips EPIQ 5, Amsterdam, Netherlands). Longitudinal images were captured in three imaging planes: anterior, lateral, and posterior. Digital images were analyzed using edge-detection software (Carotid Analyzer for Research; Medical Imaging Application, Coralville, IA) to trace the lumen-intima and intima-medial boundaries of the artery. Analyses were performed by the same blinded investigator to obtain right and left mean arterial diameter and mean cIMT. The current study was powered to detect a ∆cIMT difference of 0.019 mm between the CCI and UC groups at alpha = 0.05 and power = 80%.
Statistics
JMP software (version 5.1, SAS Institute; Cary, SC, USA) was used for all statistical analyses except multiple imputation. Multiple imputation using multivariate normal distribution, conducted with Stata software (version 11, StataCorp; College Station, TX, USA), was used to estimate means and standard errors describing the variability between imputations. Seven hundred imputations from multivariate normal regression were run to estimate the missing values (4% missing at baseline and 22% missing at 1 year). Two-sample t tests were used to test for significance of the differences in baseline biomarker values between groups. Two-sample t tests were also used to test for differences between 1-year changes between groups. Paired t tests and analysis of covariance (ANCOVA) when adjusted for baseline covariates (sex, age, baseline BMI, insulin use (user vs. non-user), and African–American race) were used to test for significance of within-group changes. A secondary analysis was conducted with the addition of smoking status as a sixth covariate. To reduce skewness before testing for significance, triglyceride, triglyceride/HDL-C ratio and hsCRP were first log-transformed, however aside from P values, the tables present results from the untransformed data. Percent change in a given biomarker was calculated as the mean difference value divided by the mean baseline value. The standard error of percent change of a given biomarker was calculated as the standard error of the change divided by the mean baseline value. Significant changes in proportions (e.g. medication use) were tested using McNemar’s test with continuity correction in completers, and linear regression of the changes in the dichotomous states when missing outcome data were imputed.
Throughout the manuscript, standard deviations are presented within parentheses and standard errors are presented following “±” symbol. Nominal significance levels (P) are presented in the tables; however, a significance level of P < 0.0019 ensures simultaneous significance at P < 0.05 for a Bonferroni adjustment for the 26 variables examined. Unless otherwise noted, results presented are intention-to-treat analyses (all starters) with missing values estimated by imputation. Some results are designated as completer analyses (excluding participants who withdrew or lacked biomarkers at 1 year).
Results
Baseline characteristics of participants
The baseline characteristics of the 262 T2D participants who began the CCI are shown in Table 1. There were no significant differences in baseline characteristics between groups self-selecting web-based (CCI-web) and onsite education (CCI-onsite) (Additional file 1: Table S1) nor were there significant differences in biomarker changes at 1 year between the groups (Additional file 2: Table S2). Therefore, results for the two groups were combined for further analyses.
Table 1.
Baseline characteristics for participants in the continuous care intervention (CCI) and usual care (UC) groups
| All | Completers with data | |||
|---|---|---|---|---|
| N | Mean (SD) or ± SE | N | Mean (SD) or ± SE | |
| Age (years) | ||||
| CCI-all educationa | 262 | 54 (8) | 218 | 54 (8) |
| Usual carea | 87 | 52 (10) | 78 | 52 (10) |
| CCI-all vs. usual careb | 1 ± 1 | 2 ± 1* | ||
| Female (%) | ||||
| CCI-all educationa | 262 | 66.8 ± 2.9 | 218 | 65.1 ± 3.2 |
| Usual carea | 87 | 58.6 ± 5.3 | 78 | 60.3 ± 5.5 |
| CCI-all vs. usual careb | 8.2 ± 6.0 | 4.9 ± 6.4 | ||
| Smokers (%) | ||||
| CCI-all educationa | 211 | 3.8 ± 1.3 | 176 | 4.0 ± 1.5 |
| Usual carea | 87 | 14.9 ± 3.8 | 78 | 14.1 ± 3.9 |
| CCI-all vs. usual careb | − 11.2 ± 4.0† | − 10.1 ± 4.2* | ||
| Weight-clinic (kg) | ||||
| CCI-all educationa | 257 | 116.5 (25.9) | 184 | 115.4 (24.6) |
| Usual carea | 83 | 105.6 (22.2) | 69 | 106.8 (22.2) |
| CCI-all vs. usual careb | 10.9 ± 2.9‡ | 8.6 ± 3.2† | ||
| BMI (kg m−2) | ||||
| CCI-all educationa | 257 | 40.4 (8.8) | 184 | 39.9 (7.9) |
| Usual carea | 83 | 36.7 (7.3) | 69 | 37.1 (7.6) |
| CCI-all vs. usual careb | 3.7 ± 1.0‡ | 2.7 ± 1.1† | ||
| Hemoglobin A1c (%) | ||||
| CCI-all educationa | 262 | 7.60 (1.50) | 204 | 7.49 (1.40) |
| Usual carea | 87 | 7.64 (1.76) | 72 | 7.74 (1.82) |
| CCI-all vs. usual careb | −0.04 ± 0.21 | −0.25 ± 0.24 | ||
| Systolic blood pressure (mmHg) | ||||
| CCI-all educationa | 260 | 132 (14) | 187 | 133 (15) |
| Usual carea | 79 | 130 (14) | 67 | 129 (13) |
| CCI-all vs. usual careb | 2 ± 2 | 4 ± 2* | ||
| Diastolic blood pressure (mmHg) | ||||
| CCI-all educationa | 260 | 82 (8) | 187 | 82 (8) |
| Usual carea | 79 | 82 (9) | 67 | 81 (8) |
| CCI-all vs. usual careb | 0 ± 1 | 0 ± 1 | ||
| ApoB (mg dL−1) | ||||
| CCI-all educationa | 248 | 105 (29) | 186 | 103 (28) |
| Usual carea | 79 | 107 (28) | 59 | 106 (30) |
| CCI-all vs. usual careb | −2 ± 4 | −2 | ||
| ApoA1 (mg dL−1) | ||||
| CCI-all educationa | 248 | 146 (28) | 185 | 146 (29) |
| Usual carea | 79 | 149 (22) | 59 | 148 (21) |
| CCI-all vs. usual careb | −3 ± 3 | −2 ± 3 | ||
| ApoB/ApoA1 ratio | ||||
| CCI-all educationa | 248 | 0.74 (0.23) | 185 | 0.73 (0.23) |
| Usual carea | 79 | 0.73 (0.23) | 59 | 0.73 (0.25) |
| CCI-all vs. usual careb | 0.01 ± 0.03 | 0.00 ± 0.04 | ||
| Triglycerides (mg dL−1) | ||||
| CCI-all educationa | 247 | 197 (143) | 186 | 201 (153) |
| Usual carea | 79 | 283 (401) | 59 | 297 (458) |
| CCI-all vs. usual careb | −86 ± 46* | −97 ± 61 | ||
| LDL-C (mg dL−1) | ||||
| CCI-all educationa | 232 | 103 (33) | 172 | 100 (33) |
| Usual carea | 70 | 102 (36) | 48 | 100 (38) |
| CCI-all vs. usual careb | 1 ± 5 | 0 ± 6 | ||
| HDL-C (mg dL−1) | ||||
| CCI-all educationa | 247 | 42 (13) | 186 | 42 (14) |
| Usual carea | 79 | 38 (11) | 59 | 37 (11) |
| CCI-all vs. usual careb | 5 ± 2† | 5 ± 2† | ||
| Triglycerides/HDL-C ratio | ||||
| CCI-all educationa | 247 | 5.9 (7.1) | 186 | 6.1 (7.9) |
| Usual carea | 79 | 10.5 (23.2) | 59 | 11.5 (26.5) |
| CCI-all vs. usual careb | −4.6 ± 2.6 | −5.4 ± 3.5 | ||
| Large VLDL-P (nmol L−1) | ||||
| CCI-all educationa | 259 | 10 (8) | 203 | 9 (8) |
| Usual carea | 83 | 12 (12) | 68 | 12 (13) |
| CCI-all vs. usual careb | −2 ± 1 | −2 ± 2 | ||
| Total LDL-P (nmol L−1) | ||||
| CCI-all educationa | 259 | 1300 (465) | 203 | 1296 (476) |
| Usual carea | 83 | 1289 (511) | 68 | 1243 (484) |
| CCI-all vs. usual careb | 11 ± 63 | 52 ± 68 | ||
| Small LDL-P (nmol L−1) | ||||
| CCI-all educationa | 259 | 774 (377) | 203 | 778 (378) |
| Usual carea | 83 | 719 (322) | 68 | 699 (326) |
| CCI-all vs. usual careb | 55 ± 42 | 789 ± 48 | ||
| LDL-particle size (nm) | ||||
| CCI-all educationa | 259 | 20.30 (0.55) | 201 | 20.3 (0.55) |
| Usual carea | 83 | 20.33 (0.56) | 68 | 20.32 (0.55) |
| CCI-all vs. usual careb | −0.03 ± 0.07 | −0.03 ± 0.08 | ||
| Total HDL-P (μmol L−1) | ||||
| CCI-all educationa | 259 | 31.3 (6.4) | 203 | 31.7 (6.4) |
| Usual carea | 83 | 29.9 (5.8) | 68 | 30.2 (6.0) |
| CCI-all vs. usual careb | 1.4 ± 0.8 | 1.5 ± 0.9 | ||
| Large HDL-P (μmol L−1) | ||||
| CCI-all educationa | 259 | 4.3 (2.5) | 203 | 4.2 (2.5) |
| Usual carea | 83 | 3.8 (2.1) | 68 | 3.8 (2.1) |
| CCI-all vs. usual careb | 0.4 ± 0.3 | 0.4 ± 0.3 | ||
| LP-IR score | ||||
| CCI-all educationa | 259 | 72 (17) | 203 | 72 (18) |
| Usual carea | 83 | 75 (16) | 68 | 74 (17) |
| CCI-all vs. usual careb | −3 ± 2 | −2 ± 2 | ||
| C-reactive protein (mg L−1) | ||||
| CCI-all educationa | 249 | 8.5 (14.5) | 193 | 9.0 (16.1) |
| Usual carea | 85 | 8.9 (8.6) | 70 | 9.1 (9.0) |
| CCI-all vs. usual careb | −0.3 ± 1.3 | −0.1 ± 1.6 | ||
| WBC | ||||
| CCI-all educationa | 260 | 7.2 (1.9) | 204 | 7.1 (1.8) |
| Usual carea | 86 | 8.1 (2.4) | 72 | 8.3 (2.4) |
| CCI-all vs. usual careb | −0.9 ± 0.3† | −1.2 ± 0.3§ | ||
| 10-year ASCVD risk (%) | ||||
| CCI-all educationa | 198 | 11.1 (9.1) | 135 | 12.1 (9.3) |
| Usual carea | 72 | 11.8 (10.8) | 55 | 11.4 (10.8) |
| CCI-all vs. usual careb | −0.6 ± 1.4 | 0.8 ± 1.6 | ||
| CIMT-average (mm) | ||||
| CCI-all educationa | 236 | 0.681 (0.108) | 144 | 0.692 (0.113) |
| Usual carea | 84 | 0.681 (0.116) | 68 | 0.680 (0.111) |
| CCI-all vs. usual careb | −0.001 ± 0.014 | 0.013 ± 0.016 | ||
| Statin (%) | ||||
| CCI-all educationa | 262 | 50.0 ± 3.1 | 218 | 51.8 ± 3.4 |
| Usual carea | 87 | 58.6 ± 5.3 | 73 | 54.8 ± 5.8 |
| CCI-all vs. usual careb | −8.6 ± 6.1 | −3.0 ± 6.7 | ||
| Any antihypertensive medication (%) | ||||
| CCI-all educationa | 262 | 67.2 ± 2.9 | 218 | 68.4 ± 3.2 |
| Usual carea | 87 | 52.9 ± 5.4 | 73 | 50.7 ± 5.9 |
| CCI-all vs. usual careb | 14.3 ± 6.1* | 17.7 ± 6.7† | ||
| ACE or ARB (%) | ||||
| CCI-all educationa | 262 | 29.4 ± 2.8 | 218 | 28.0 ± 3.0 |
| Usual carea | 87 | 18.4 ± 4.2 | 73 | 16.4 ± 4.3 |
| CCI-all vs. usual careb | 11.0 ± 5.0* | 11.5 ± 5.3* | ||
| Diuretics (%) | ||||
| CCI-all educationa | 262 | 40.8 ± 3.0 | 218 | 41.3 ± 3.3 |
| Usual carea | 87 | 29.9 ± 4.9 | 73 | 24.7 ± 5.0 |
| CCI-all vs. usual careb | 11.0 ± 5.8 | 16.6 ± 6.1† | ||
Significant baseline difference between means or percentages are designated by the following symbols: * 0.05 > P ≥ 0.01, †0.01 > P ≥ 0.001, ‡0.001 > P ≥ 0.0001, §P < 0.0001
a Mean and standard deviations for continuous variables, percents and standard errors for categorical variables
b Difference between means or percentages ± 1 standard error of the difference
The baseline characteristics of participants with measurements at both baseline and 1 year were not significantly different from dropouts and participants with missing data after correcting for multiple comparisons (Additional file 1: Table S1). This suggests that multiple imputation may be appropriate for estimating missing values in order to estimate outcomes for all starters.
An independently recruited UC group of 87 T2D participants, which provided an observational comparison group from the same geography and health system, showed no significant differences from the CCI group in baseline characteristics except mean body weight and BMI were higher in the CCI versus the UC group (Table 1, P < 0.001).
Changes in biomarkers of CVD risk at 1 year
Two-hundred eighteen (83%) participants remained enrolled in the CCI group at 1 year. One-year changes in CVD biomarkers are detailed in Table 2 and percent changes from baseline are shown in Fig. 1. The within-CCI group changes in the following lipids and lipoproteins were all statistically significant after adjusting for multiple comparisons (P < 0.0019), reported here as mean percent difference from baseline: ApoA1 (+ 9.8%), ApoB/ApoA1 ratio (− 9.5%), triglycerides (− 24.4%), LDL-C (+ 9.9%), HDL-C (+ 18.1%), triglyceride/HDL-C ratio (− 29.1%), large VLDL-P (− 38.9%), small LDL-P (− 20.8%), LDL-particle size (+ 1.1%), total HDL-P (+ 4.9%), and large HDL-P (+ 23.5%). There were no significant changes after adjusting for multiple comparisons in total LDL-P (− 4.9%, P = 0.02) or ApoB (− 1.6%, P = 0.37).
Table 2.
1-year biomarker changes for participants in the continuous care intervention group compared to usual care group
| Completers | All starters (dropouts imputed)d |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | 1 year Mean ± SE |
Unadjusted | Adjusted for baselinec | Unadjusted | |||||
| Difference (SD) or ± SE | Significancee | Difference ± SE | Significancee | 1 year Mean ± SE |
Difference ± SE | Significancee | |||
| ∆Weight-clinic (kg) | |||||||||
| CCI-all educationa | 184 | 101.2 ± 1.6 | − 14.2 (10.3) | < 10−16 | − 13.8 ± 0.6 | < 10−16 | 102.7 ± 1.5 | − 13.8 ± 0.7 | < 10−16 |
| Usual carea | 69 | 106.8 ± 2.7 | 0.04 (5.9) | 0.95 | − 1.1 ± 1.1 | 0.29 | 107.3 ± 2.6 | − 0.2 ± 0.8 | 0.85 |
| CCI-all vs. usual careb | − 14.3 ± 1.0 | < 10−16 | − 12.7 ± 1.3 | < 10−16 | − 13.7 ± 1.1 | < 10−16 | |||
| ∆Hemoglobin A1c (%) | |||||||||
| CCI-all educationa | 204 | 6.20 ± 0.07 | − 1.29 (1.32) | < 10−16 | − 1.32 ± 0.09 | < 10−16 | 6.29 ± 0.07 | − 1.30 ± 0.09 | < 10−16 |
| Usual carea | 72 | 7.94 ± 0.22 | 0.20 (1.35) | 0.21 | 0.22 ± 0.16 | 0.17 | 7.84 ± 0.19 | 0.20 ± 0.15 | 0.18 |
| CCI-all vs. usual careb | − 1.49 ± 0.18 | 4.4 × 10−16 | − 1.54 ± 0.19 | 4.4 × 10−16 | − 1.50 ± 0.17 | < 10−16 | |||
| ∆Systolic blood pressure (mmHg) | |||||||||
| CCI-all educationa | 187 | 126 ± 1 | − 7 (16) | 1.3 × 10−8 | − 7 ± 1 | 1.6 × 10−7 | 126 ± 1 | − 6 ± 1 | 1.3 × 10−8 |
| Usual carea | 67 | 129 ± 2 | 0 (18) | 0.91 | 0 ± 2 | 0.83 | 129 ± 2 | − 1 ± 2 | 0.67 |
| CCI-all vs. usual careb | − 7 ± 2 | 0.005 | − 6 ± 3 | 0.02 | − 5 ± 2 | 0.02 | |||
| ∆Diastolic blood pressure (mmHg) | |||||||||
| CCI-all educationa | 187 | 78 ± 1 | − 4 (9) | 1.4 × 10−7 | − 4 ± 1 | 6.2 × 10−7 | 79 ± 1 | − 4 ± 1 | 7.2 × 10−8 |
| Usual carea | 67 | 81 ± 1 | 0 (10) | 0.92 | 0 ± 1 | 0.75 | 81 ± 1 | − 1 ± 1 | 0.45 |
| CCI-all vs. usual careb | − 3 ± 1 | 0.01 | − 3 ± 1 | 0.03 | − 3 ± 1 | 0.06 | |||
| ∆ApoB (mg dL−1) | |||||||||
| CCI-all educationa | 186 | 103 ± 2 | − 1 (24) | 0.69 | − 0 ± 2 | 0.82 | 104 ± 2 | − 2 ± 2 | 0.37 |
| Usual carea | 59 | 107 ± 5 | 2 (37) | 0.75 | 1 ± 4 | 0.9 | 106 ± 4 | 0 ± 4 | 0.95 |
| CCI-all vs. usual careb | − 2 ± 5 | 0.66 | − 1 ± 5 | 0.83 | − 2 ± 5 | 0.67 | |||
| ∆ApoA1 (mg dL−1) | |||||||||
| CCI-all educationa | 185 | 160 ± 3 | 14 (24) | 8.9 × 10−16 | 14 ± 2 | 4.4 × 10−16 | 160 ± 2 | 14 ± 2 | < 10−16 |
| Usual carea | 59 | 145 ± 3 | − 3 (19) | 0.18 | − 2 ± 3 | 0.55 | 147 ± 3 | − 2 ± 3 | 0.37 |
| CCI-all vs. usual careb | 18 ± 3 | 4.7 × 10−9 | 16 ± 4 | 2.2 × 10−5 | 17 ± 3 | 1.4 × 10−7 | |||
| ∆ApoB/ApoA1 | |||||||||
| CCI-all educationa | 185 | 0.67 ± 0.02 | − 0.06 (0.17) | 1.8 × 10−6 | − 0.06 ± 0.02 | 0.003 | 0.67 ± 0.02 | − 0.07 ± 0.01 | 1.9 × 10−7 |
| Usual carea | 59 | 0.76 ± 0.04 | 0.03 (0.29) | 0.42 | 0.02 ± 0.03 | 0.5 | 0.74 ± 0.03 | 0.02 ± 0.03 | 0.58 |
| CCI-all vs. usual careb | − 0.09 ± 0.04 | 0.02 | − 0.08 ± 0.03 | 0.02 | − 0.09 ± 0.03 | 0.01 | |||
| ∆Triglycerides (mg dL−1) | |||||||||
| CCI-all educationa | 186 | 151 ± 11 | − 49 (168) | 5.6 × 10−5 | − 50 ± 16 | 0.001 | 148 ± 12 | − 48 ± 13 | < 10−16 |
| Usual carea | 59 | 327 ± 65 | 30 (301) | 0.44 | 31 ± 29 | 0.27 | 305 ± 48 | 28 ± 32 | 0.43 |
| CCI-all vs. usual careb | − 80 ± 41 | 0.05 | − 81 ± 33 | 0.02 | − 76 ± 35 | 9.9 × 10−7 | |||
| ∆LDL-C (mg dL−1) | |||||||||
| CCI-all educationa | 172 | 111 ± 3 | 11 (32) | 7.7 × 10−6 | 11 ± 3 | 2.6 × 10−5 | 113 ± 3 | 10 ± 2 | 4.9 × 10−5 |
| Usual carea | 48 | 90 ± 4 | − 11 (38) | 0.05 | − 11 ± 5 | 0.03 | 90 ± 5 | − 11 ± 5 | 0.02 |
| CCI-all vs. usual careb | 22 ± 6 | 0.0003 | 22 ± 6 | 0.0002 | 21 ± 5 | 9.9 × 10−5 | |||
| ∆HDL-C (mg dL−1) | |||||||||
| CCI-all educationa | 186 | 50 ± 1 | 8 (12) | < 10−16 | 7 ± 1 | < 10−16 | 50 ± 1 | 8 ± 1 | < 10−16 |
| Usual carea | 59 | 35 ± 2 | − 2 (9) | 0.15 | − 1 ± 2 | 0.69 | 37 ± 2 | − 1 ± 1 | 0.41 |
| CCI-all vs. usual careb | 9 ± 1 | 1.7 × 10−10 | 8 ± 2 | 9.9 × 10−6 | 9 ± 2 | 1.2 × 10−8 | |||
| Triglycerides/HDL-C ratio | |||||||||
| CCI-all educationa | 186 | 4.3 ± 0.6 | − 1.8 (9.4) | < 10−16 | − 1.9 ± 0.9 | < 10−16 | 4.1 ± 0.6 | − 1.6 ± 0.7 | < 10−16 |
| Usual carea | 59 | 12.5 ± 2.7 | 0.9 (16.1) | 0.1 | 1.2 ± 1.6 | 0.16 | 11.2 ± 2.1 | 1.0 ± 1.7 | 0.24 |
| CCI-all vs. usual careb | − 2.8 ± 2.2 | 3.1 × 10−10 | − 3.1 ± 1.8 | 5.5 × 10−7 | − 2.6 ± 1.8 | 4.5 × 10−9 | |||
| ∆Large VLDL-P (nmol L−1) | |||||||||
| CCI-all educationA | 203 | 6 ± 1 | − 4 (7) | 5.6 × 10−15 | − 4 ± 1 | 1.6 × 10−14 | 6 ± 1 | − 4 ± 1 | 4.2 × 10−15 |
| Usual carea | 68 | 12 ± 2 | 0 (8) | 0.71 | 0 ± 1 | 0.60 | 12 ± 1 | 0 ± 1 | 0.77 |
| CCI-all vs. usual careb | − 3 ± 1 | 0.001 | − 3 ± 1 | 0.002 | 3 ± 1 | 0.0007 | |||
| ∆Total LDL-P (nmol L−1) | |||||||||
| CCI-all educationa | 203 | 1234 ± 30 | − 62 (375) | 0.02 | − 57 ± 29 | 0.05 | 1235 ± 29 | − 64 ± 26 | 0.02 |
| Usual carea | 68 | 1196 ± 60 | − 47 (491) | 0.43 | − 67 ± 53 | 0.21 | 1231 ± 57 | − 57 ± 56 | 0.31 |
| CCI-all vs. usual careb | − 15 ± 65 | 0.82 | 10 ± 62 | 0.87 | − 7 ± 62 | 0.91 | |||
| ∆Small LDL-P (nmol L−1) | |||||||||
| CCI-all educationa | 203 | 614 ± 22 | − 164 (332) | 2.2 × 10−12 | − 161 ± 24 | 4.1 × 10−11 | 613 ± 21 | − 161 ± 23 | 1.2 × 10−12 |
| Usual carea | 68 | 724 ± 44 | 25 (370) | 0.57 | 16 ± 45 | 0.71 | 740 ± 41 | 18 ± 42 | 0.67 |
| CCI-all vs. usual careb | − 189 ± 51 | 0.0002 | − 177 ± 52 | 0.0007 | − 179 ± 48 | 0.0002 | |||
| ∆LDL-particle size (nm) | |||||||||
| CCI-all educationa | 201 | 20.53 ± 0.04 | 0.23 (0.54) | 1.7 × 10−9 | 0.23 ± 0.04 | 8.9 × 10−9 | 20.53 ± 0.04 | 0.23 ± 0.04 | 6.0 × 10−10 |
| Usual carea | 68 | 20.25 ± 0.07 | − 0.08 (0.53) | 0.24 | − 0.08 ± 0.07 | 0.25 | 20.25 ± 0.07 | − 0.07 ± 0.06 | 0.25 |
| CCI-all vs. usual careb | 0.30 ± 0.07 | 4.4 × 10−5 | 0.31 ± 0.08 | 0.0002 | 0.30 ± 0.07 | 3.8 × 10−15 | |||
| ∆Total HDL-P (µmol L−1) | |||||||||
| CCI-all educationa | 203 | 33.2 ± 0.5 | 1.5 (4.9) | 1.2 × 10−5 | 1.5 ± 0.4 | 2.1 × 10−5 | 32.8 ± 0.4 | 1.5 ± 0.3 | 5.6 × 10−6 |
| Usual carea | 68 | 29.4 ± 0.8 | − 0.8 (4.7) | 0.15 | − 0.8 ± 0.6 | 0.23 | 29.2 ± 0.7 | − 0.7 ± 0.6 | 0.23 |
| CCI-all vs. usual careb | 2.3 ± 0.7 | 0.0004 | 2.3 ± 0.7 | 0.003 | 2.2 ± 0.7 | 0.0008 | |||
| ∆Large HDL-P (µmol L−1) | |||||||||
| CCI-all educationa | 203 | 5.3 ± 0.2 | 1.0 (2.2) | 2.5 × 10−11 | 1.0 ± 0.2 | 4.1 × 10−11 | 5.3 ± 0.2 | 1.0 ± 0.2 | 1.2 × 10−11 |
| Usual carea | 68 | 3.9 ± 0.3 | 0.1 (1.6) | 0.69 | 0.2 ± 0.3 | 0.44 | 3.9 ± 0.3 | 0.1 ± 0.2 | 0.74 |
| CCI-all vs. usual careb | 0.9 ± 0.3 | 0.0002 | 0.8 ± 0.3 | 0.01 | 0.9 ± 0.3 | 0.0004 | |||
| ∆LP-IR score | |||||||||
| CCI-all educationa | 203 | 58 ± 2 | − 14 (18) | < 10−16 | − 14 ± 1 | < 10−16 | 58 ± 1 | − 14 ± 1 | < 10−16 |
| Usual carea | 68 | 74 ± 2 | − 1 (16) | 0.73 | − 2 ± 2 | 0.41 | 75 ± 2 | − 1 ± 2 | 0.74 |
| CCI-all vs. usual careb | − 13 ± 2 | 3.8 × 10−9 | − 12 ± 3 | 6.2 × 10−6 | − 13 ± 2 | 6.2 × 10−9 | |||
| ∆C-reactive protein (mg L−1) | |||||||||
| CCI-all educationa | 193 | 5.7 ± 0.5 | − 3.3 (13.4) | < 10−8 | − 3.1 ± 1.0 | < 10−16 | 5.6 ± 0.6 | − 3.6 ± 1.1 | < 10−16 |
| Usual carea | 70 | 10.4 ± 1.8 | 1.3 (13.3) | 0.94 | 0.9 ± 1.7 | 0.88 | 10.3 ± 1.6 | 1.3 ± 1.5 | 0.93 |
| CCI-all vs. usual careb | − 4.7 ± 1.9 | 1.2 × 10−6 | − 4.0 ± 2.0 | 3.0 × 10−5 | − 4.9 ± 1.8 | 9.3 × 10−7 | |||
| ∆WBC (k mm−3) | |||||||||
| CCI-all educationa | 204 | 6.5 ± 0.1 | − 0.7 (1.4) | 2.1 × 10−11 | − 0.7 ± 0.1 | 2.1 × 10−11 | 6.6 ± 0.1 | − 0.7 ± 0.1 | 3.2 × 10−11 |
| Usual carea | 72 | 8.3 ± 0.3 | − 0.1 (1.6) | 0.76 | − 0.1 ± 0.2 | 0.74 | 8.1 ± 0.3 | − 0.1 ± 0.2 | 0.76 |
| CCI-all vs. usual careb | − 0.6 ± 0.2 | 0.003 | − 0.6 ± 0.2 | 0.004 | − 0.6 ± 0.2 | 0.003 | |||
| ∆10-year ASCVD risk (%) | |||||||||
| CCI-all educationa | 135 | 10.5 ± 0.7 | − 1.6 (5.4) | 0.0004 | − 1.5 ± 0.6 | 0.01 | 9.6 ± 0.5 | − 1.3 ± 0.3 | 4.9 × 10−5 |
| Usual carea | 55 | 12.7 ± 1.5 | 1.4 (9.3) | 0.28 | 1.1 ± 1.0 | 0.27 | 12.9 ± 1.2 | 1.2 ± 0.9 | 0.17 |
| CCI-all vs. usual careb | − 3.0 ± 1.3 | 0.03 | − 2.6 ± 1.2 | 0.03 | − 2.6 ± 1.0 | 0.008 | |||
| ∆CIMT-average (mm) | |||||||||
| CCI-all educationa | 144 | 0.695 ± 0.009 | 0.002 (0.055) | 0.63 | 0.003 ± 0.004 | 0.45 | 0.685 ± 0.010 | 0.002 ± 0.004 | 0.65 |
| Usual carea | 68 | 0.680 ± 0.013 | 0.004 (0.041) | 0.37 | 0.002 ± 0.006 | 0.74 | 0.680 ± 0.013 | 0.001 ± 0.006 | 0.87 |
| CCI-all vs. usual careb | − 0.002 ± 0.007 | 0.74 | 0.001 ± 0.008 | 0.87 | 0.001 ± 0.007 | 0.88 | |||
| ∆Statin (%) | |||||||||
| CCI-all educationa | 218 | 48.2 ± 3.4 | − 3.7 (34.4) | 0.12 | − 3.6 ± 2.4 | 0.13 | 46.7 ± 3.2 | − 3.3 ± 2.3 | 0.15 |
| Usual carea | 73 | 64.4 ± 5.6 | 9.6 (37.9) | 0.03 | 9.5 ± 4.3 | 0.03 | 67.4 ± 5.4 | 8.8 ± 4.3 | 0.04 |
| CCI-all vs. usual careb | − 13.3 ± 5.0 | 0.008 | − 13.2 ± 5.0 | 0.009 | − 12.1 ± 4.9 | 0.01 | |||
| ∆Any antihypertensive medication (%) | |||||||||
| CCI-all educationa | 218 | 56.4 ± 3.4 | − 11.9 (42.3) | 3.2 × 10−5 | − 11.9 ± 2.9 | 3.6 × 10−5 | 55.8 ± 3.3 | − 11.4 ± 2.8 | 5.3 × 10−5 |
| Usual carea | 73 | 60.3 ± 5.8 | 9.6 (41.4) | 0.05 | 9.6 ± 5.1 | 0.06 | 61.2 ± 5.6 | 8.3 ± 4.8 | 0.09 |
| CCI-all vs. usual careb | − 21.5 ± 5.6 | 0.0002 | − 21.6 ± 6.0 | 0.0004 | − 19.7 ± 5.6 | 0.0004 | |||
| ∆ACE or ARB (%) | |||||||||
| CCI-all educationa | 218 | 28.9 ± 3.1 | 0.9 (27.1) | 0.62 | 1.5 ± 1.9 | 0.42 | 30.0 ± 2.9 | 0.6 ± 1.9 | 0.76 |
| Usual carea | 73 | 21.9 ± 4.9 | 5.5 (28.3) | 0.1 | 3.7 ± 3.3 | 0.27 | 23.4 ± 4.7 | 5.0 ± 3.3 | 0.13 |
| CCI-all vs. usual careb | − 4.6 ± 3.8 | 0.23 | − 2.1 ± 3.9 | 0.59 | − 4.4 ± 3.8 | 0.24 | |||
| ∆Diuretics (%) | |||||||||
| CCI-all educationa | 218 | 31.7 ± 3.2 | − 9.6 (41.3) | 0.0006 | − 9.5 ± 2.7 | 0.0004 | 31.3 ± 3.1 | − 9.7 ± 2.7 | 0.0004 |
| Usual carea | 73 | 30.1 ± 5.4 | 5.5 (32.9) | 0.16 | 5.2 ± 4.8 | 0.28 | 33.0 ± 5.3 | 3.2 ± 4.1 | 0.44 |
| CCI-all vs. usual careb | − 15.1 ± 4.8 | 0.001 | − 14.7 ± 5.6 | 0.009 | − 12.8 ± 4.9 | 0.009 | |||
a Means (standard deviations) or ± one standard error are presented. Sample sizes, means, and significance levels refer to subjects with baseline and 1-year measurements for completers, and to 349 subjects (262 intervention and 87 usual care) for all starters. Significance levels for completers refer to one-sample t test with or without adjustment. Untransformed triglyceride and C-reactive protein values are presented, however, their statistical significances were based on their log-transformed values
b Mean differences ± one standard error are presented. Significance levels refer to two-sample t test or analysis of covariance for the differences
c Adjusted for sex, age, baseline BMI, baseline insulin use (user vs. non-user), and African–American race
d Imputed values based on 700 iterations from multivariate normal regression
e A significance level of P < 0.0019 ensures overall simultaneous significance of P < 0.05 over the 26 variables using Bonferroni correction
Fig. 1.
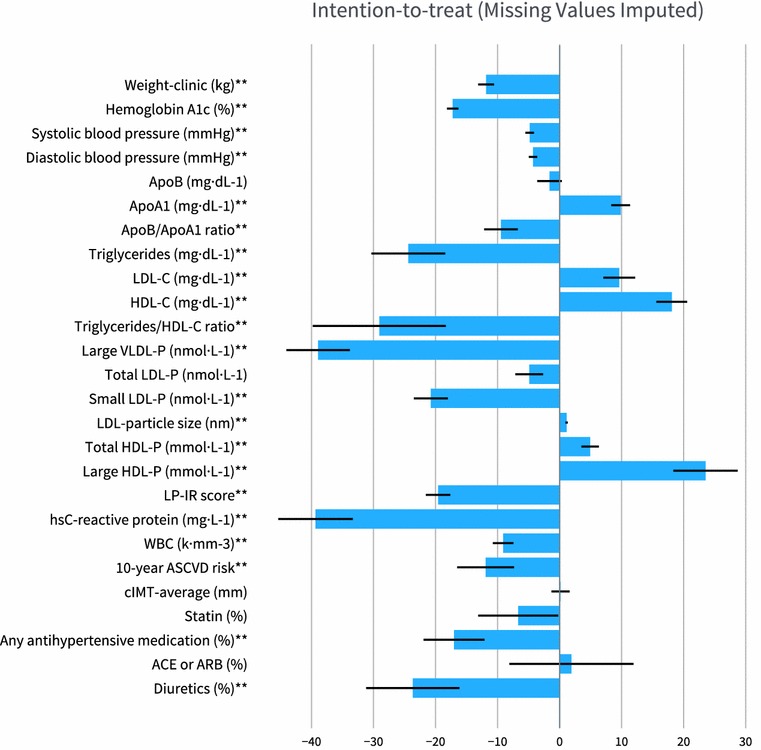
Change in biomarkers for CCI group. Bars indicate CCI group mean percent change in biomarkers based on the intention-to-treat analysis with missing values imputed. Percent change is computed as the change in mean values from baseline to 1 year divided by the mean baseline value. Percent change = 100 × [(1 year value − baseline value)/(baseline value)]. Negative values indicate a decrease from baseline to 1 year while positive values indicate an increase. The ** symbol after the biomarker label indicates a statistically significant within group change from baseline (P < 0.0019, P adjusted for multiple comparisons). Error bars represent ± SE. SE as Percent = 100 × [(1 year value SE)/(baseline value)]
The CCI group experienced significant reductions in systolic BP (− 4.8%), diastolic BP (− 4.3%), hsCRP (− 39.3%) and WBC count (− 9.1%). Regarding medication changes, (reported here as percent use at 1 year minus percent use at baseline, while Fig. 1 displays percent change of percent use) significant reductions were observed in overall use of antihypertensive medication (− 11.4%) and diuretics (− 9.7%) whereas changes in ACE or ARB (0.6%) and statin (− 3.3%) use were not significant. Significant reductions were observed in both multivariate metrics: 10-year ASCVD risk (− 11.9%) and LP-IR (− 19.6%). There was no significant change in cIMT (averaged right and left values). In addition, changes in cIMT were not significantly correlated with baseline LDL-P or LDL-C, or changes in LDL-P or LDL-C (all P ≥ 0.33).
One-year results from the UC group are provided in Table 2 and Fig. 2. Within the UC group, after adjustment for multiple comparisons there were no significant changes at 1 year. After adjusting for differences in baseline characteristics (sex, age, baseline BMI, insulin use (user vs. non-user), and African–American race) and multiple comparisons, the changes observed at 1 year for the following biomarkers were significantly different between the CCI and UC groups (mean ∆CCI − mean ∆UC, where ∆ is 1 year minus baseline): small LDL-P (− 177 nmol L−1), ApoA1 (+ 16 mg dL−1), triglyceride/HDL-C ratio (− 3.1), LDL particle size (+ 0.31 nm), HDL-C (+ 8 mg dL−1), LDL-C (+ 22 mg dL−1), hsCRP (− 4.0 mg dL−1), and LP-IR (− 12). Adding smoking status to the list of covariates mentioned above did not lead to any changes in statistical significance.
Fig. 2.
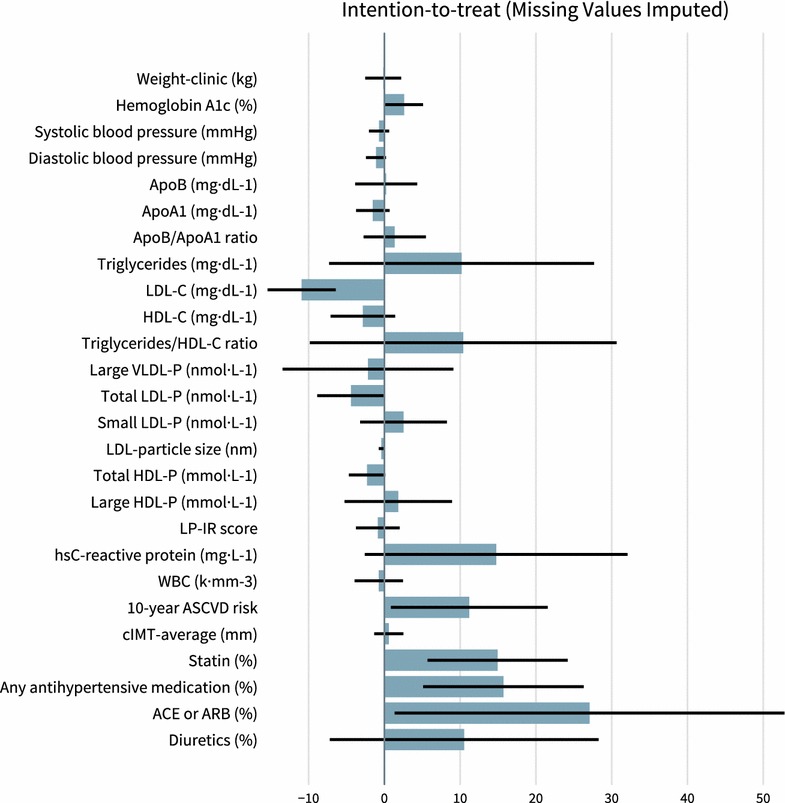
Change in biomarkers for UC group. Bars indicate UC group mean percent change in biomarkers based on the intention-to-treat analysis with missing values imputed. Percent change is computed as the change in mean values from baseline to 1 year divided by the mean baseline value. Percent change = 100 × [(1 year value − baseline value)/(baseline value)]. Negative values indicate a decrease from baseline to 1 year while positive values indicate an increase. (None of the within group changes were statistically significant, i.e. all P > 0.0019, P adjusted for multiple comparisons.) Error bars represent ± SE. SE as Percent = 100 × [(1 year value SE)/(baseline value)]
There were no significant differences in change in biomarkers between the sexes within the CCI group or between CCI and UC groups among completers (all P > 0.0019). The results related to daily weight and ketone measurements were previously reported in detail [9, 10]. In brief, almost all CCI participants (96%) reported at least one BHB value ≥ 0.5 mmol L−1 by handheld measure. Laboratory-measured BHB at 1 year (0.31 ± 0.03 mmol L−1) was almost twice as large as the baseline average in the CCI group (0.17 ± 0.01 mmol L−1). For this population, additional details on changes in other biomarkers related to glycemic control, metabolic acidosis, and liver, kidney, and thyroid health were previously reported in greater detail [9, 10]. In addition, details on safety and adverse events have previously been described [10]. A post hoc analysis of covariance on treatment versus control group differences in 1-year risk factor change suggested that weight loss was associated with as much as approximately 40–70% of the change in the following biomarkers: small LDL-P, ApoA1, triglyceride/HDL-C ratio, triglycerides, and HDL-C and over 90% of the difference in LP-IR score.
Range of outcomes
The distribution and range of intervention response for the CCI and UC groups were compared for LDL-P, small LDL-P, large VLDL-P, ApoB, ApoA1, ApoB/ApoA1 ratio, and TG/HDL-C ratio (Additional file 3: Figure S1). Ranges of change observed in the CCI group were within the ranges observed in the UC group for increases in LDL-P, small LDL-P, ApoB and ApoB/ApoA1 ratio. There were two CCI participants (2/203, 1.0%) whose change in large VLDL-P exceeded the maximum observed in the UC group (15.2 nmol L−1). There was one CCI participant (1/185, 0.5%) whose change in ApoA1 was less than the minimum observed in the UC group (− 58 mg dL−1) and one CCI participant (1/186, 0.5%) whose change in triglyceride/HDL-C ratio was higher than the maximum observed in the UC group (64.9).
Discussion
This study demonstrates that a CCI utilizing remote physician and health coach support with nutritional ketosis beneficially altered most CVD risk factors in patients with T2D at 1 year. Changes included: decreased small LDL-P, triglycerides, blood pressure and antihypertensive medication, hsCRP, and WBC count; increased HDL-C and LDL particle size; no change in LDL-P, ApoB, and cIMT and an increase in LDL-C. Combined with the previously reported improvements in glycemic control and reduction in obesity [10], which reduce CVD risk [50], these results demonstrate multiple additional benefits of the CCI with the exception of increased LDL-C.
Studies of dietary carbohydrate restriction, with a presumed increase in saturated fat intake, have shown modest changes in LDL-C levels [15, 26–28, 51]. The mean 10 mg dL−1 change observed in the CCI group in this study is numerically higher than the upper range of values reported by meta-analysis of lipid changes over 1 year related to carbohydrate restriction (− 7 to + 7 mg dL−1) [52]. Higher LDL-C is related to increased CVD risk [53, 54], but also is inversely correlated with mortality in two large prospective studies and a systemic review [55–57]. Additionally, there is no evidence that increasing or decreasing LDL-C with diet interventions has any impact on mortality. LDL-C increased in the current study but both ApoB and LDL-P, measures found to be better predictors of CVD risk, did not change significantly [20–23, 25, 58]. In addition, the reduction in small LDL-P, increase in LDL size, and decrease in large VLDL-P that occurred in the present investigation are also associated with reduced CVD risk [59–61].
A decrease in triglycerides and increase in HDL-C has also been previously reported in studies of carbohydrate restriction [15, 26–28, 50]. In patients with elevated baseline triglycerides (≥ 200 mg dL−1), a decrease in triglycerides (− 21%) and increase in HDL-C (+ 18%), which is similar to the changes observed in the intervention group in this study, has been associated with decreased CVD events [62]. Taken together, the decrease in triglycerides and increase in LDL-C may be partly due to decreased cholesterol ester transfer protein (CETP) exchange. Further studies on underlying mechanisms will help elucidate the causal relationships between the various concurrent changes in lipoproteins.
While mean response of CCI participants demonstrated an improvement in most lipid biomarkers and CVD risk factors other than LDL-C, we investigated whether a minority of participants might have unfavorable responses to the intervention. Our results suggest that a small number of participants (≤ 1%) demonstrated changes at 1 year outside the range of what was observed in a usual care population (Additional file 3: Figure S1). Thus, these results counter the concern that a significant portion of participants may have an extremely adverse reaction to the CCI (due to presumed increase in saturated fat intake) as compared to UC.
Inflammation is directly involved in all aspects of the pathogenesis of CVD [33]. High-sensitivity CRP and WBC count are widely accepted markers of inflammation and risk factors for CVD [29–32]. In addition to reducing cholesterol, reduction in inflammation may be a secondary mechanism of statins in lowering CVD risk [63–65]. The present study demonstrated a 39% reduction of hsCRP and 9% reduction in WBC count in the CCI, indicating a significant reduction in inflammation at 1 year. This response may be due in part to suppression of the NLRP3 inflammasome by BHB [66].
The reduction of blood pressure with concurrent reduction in antihypertensive medication was also significant. Blood pressure goals were recently reduced [67] and strong evidence exists that elevated blood pressure is a primary cardiovascular risk factor [68]. An analysis of a large T2D population suggested that antihypertensive medication may have limited effectiveness in reducing the prevalence of hypertension in these patients [69], whereas a study of weight loss interventions showed that a decrease in blood pressure predicted regression of carotid vessel wall volume [70]. Thus, additional lifestyle interventions that can augment blood pressure reduction such as the CCI described here may reduce CVD events. Additionally, the antihypertensives that were primarily decreased in the current study were shown to increase the risk for diabetes [71]. Their removal may represent further metabolic benefit.
Carotid intima media thickness (cIMT) is a non-invasive measure of subclinical atherosclerosis that is significantly associated with CVD morbidity and mortality [48, 49, 72, 73]. However, a recent meta-analysis in 3902 patients with T2D found that cIMT progression over an average of 3.6 years did not correlate with CVD events [72]. We found no significant change in cIMT from baseline to 1 year in either the CCI or UC groups. Progression or regression of cIMT may take multiple years to manifest and may require a larger cohort to achieve statistical significance [73]. In summary, the cIMT results from this study provide no evidence of vascular harm or benefit from 1 year of nutritional ketosis in patients with T2D.
Strengths and limitations of the study
Prior studies have demonstrated favorable improvements in atherogenic dyslipidemia with minimal or no change in LDL-C and LDL-P following managed ketogenic diets in small short-term randomized trials. This study’s strengths include its larger cohort with high retention, prospective design and 1-year duration. The study was the first to assess ApoB and ApoA1 in a T2D population adhering to a ketogenic diet. This study also has real-world application due to the outpatient setting without the use of meal replacements or food provisions.
Limitations of this study include the lack of randomization between the CCI and UC groups. In addition, the intervention provided to CCI participants was of greater intensity than UC. This was a single site study and the racial composition of study participants was predominantly Caucasian. The study was not of sufficient size and duration to determine significant differences in CVD morbidity or mortality. Since the intervention led to concurrent weight loss and improvements in cardiovascular health, it is difficult to conclude how much of the improvement can be attributed to weight loss versus other simultaneous physiological changes. In an attempt to assess the role of weight loss, a post hoc analysis of covariance on treatment versus control group differences in 1-year risk factor change suggested that weight loss was related to a large proportion of the change in: small LDL-P, ApoA1, triglyceride/HDL-C ratio, triglycerides, and HDL-C and LP-IR score. However, the results from a recent study comparing a low-fat diet group with a low-carbohydrate group, with similar weight loss at 12 months between groups, suggest that the role of weight loss may be more modest (the low-fat group showed only 15% of the HDL-C gain and 35% of the triglyceride decrease, relative to the low-carbohydrate group) [74]. Additional future studies that tightly control weight loss (and other possible mechanisms for reduction in CVD risk, e.g. diet, smoking, genetic factors, stress, etc.) would lead to better estimates of how much weight loss independently contributes to the improvements observed in the intervention group relative to other factors. Furthermore, future trials could include a longer multi-site, randomized controlled trial to allow for hard end point evaluation. Greater racial and ethnic diversity, a broader age range, and greater disease severity could also be evaluated.
Conclusions
A T2D intervention combining technology-enabled continuous remote care with individualized plans encouraging nutritional ketosis has demonstrated diabetes status improvement while improving many CVD risk factors including atherogenic dyslipidemia, inflammation and blood pressure while decreasing use of antihypertensive mediations. Ongoing research will determine the continued safety, sustainability, and effectiveness of the intervention.
Additional files
Additional file 1: Table S1. Detailed baseline characteristics for participants in the continuous care intervention (CCI) and usual care (UC) groups.
Additional file 2: Table S2. Details on 1-year biomarker changes for participants in the continuous care intervention group compared to usual care group.
Additional file 3: Figure S1. Distribution of changes in selected biomarkers for CCI and UC completers. Histograms of changes at one year for CCI (blue) and UC (gray) are overlaid. Very few (≤1%) CCI participants demonstrated changes in an undesirable direction at one year that were outside the range of changes observed in the UC group for key lipid and lipoprotein particles. (A) Apolipoprotein B (B) Apolipoprotein A1 (C) Apolipoprotein B/Apolipoprotein A1 ratio (D) LDL-P (E) Small LDL-P (F) Large VLDL-P (G) Triglyceride/HDL-C ratio.
Authors’ contributions
SJH, ALM, WWC, JPM, SDP and JSV conceptualized and designed the study. PTW performed the formal analysis. SJH and ALM contributed to the investigation. NHB and SJH wrote the original draft. NHB and PTW created the data tables and visualizations. All authors contributed to revising and editing of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors are extremely grateful to the research participants for offering their time and energy to participate in advancing scientific discovery. Thanks to Indiana University Health (IUH) staff, especially Tamara Hazbun, Monica Keyes, Danielle Wharff, Patti McKee, Joni Anderson, Zachary Roberts, Christina Selsor, and Douglas Jackson, and Virta Health staff Rachel Bolden, Sydney Rivera, and Deklin Veenhuizen for contributions to various aspects of the study including patient care, study coordination and data processing. Thanks to the health coaches who provided guidance to CCI participants: Brittanie Volk, Brent Creighton, Theresa Link, Bobbie Glon, and Marcy Abner. Thanks to Roxie McKee of IUH, Dave Gibson and Jennifer Powers of Washington University, and Teryn Sapper and staff from the Volek Laboratory at The Ohio State University for assistance in sample analysis, storage and/or transportation logistics. Thanks to Angela Fountain, Irinia Shalaurova, and Jim Otvos of LabCorp for guidance on interpreting LipoProfile results. Thank you to Ronald Krauss for guidance on lipid analysis and Ethan Weiss for critical reading of the manuscript.
Competing interests
NHB, SJH, ALM, JPM, and SDP are employees of Virta Health Corp. and have been offered stock options. SDP and JSV are founders of Virta Health Corp. PTW and KDB are paid consultants of Virta Health Corp. WWC has no competing interests.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the Franciscan Health Lafayette Institutional Review Board, and participants provided written informed consent.
Funding
The study was funded by Virta Health Corp.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ACE
angiotensin-converting-enzyme inhibitors
- ApoA1
apolipoprotein A1
- ApoB
apolipoprotein B
- ARB
angiotensin II receptor blockers
- ASCVD risk score
10-year atherosclerotic cardiovascular disease risk score
- BHB
beta-hydroxybutyrate
- BP
blood pressure
- CCI
continuous care intervention
- CCI-onsite
subset of CCI participants who selected to receive onsite education
- CCI-web
subset of CCI participants who selected to receive web-based education
- cIMT
carotid intima media thickness
- CVD
cardiovascular disease
- GDR
glucose disposal rate
- HOMA-IR
homeostatic model assessment of insulin resistance
- hsCRP
high sensitive C-reactive protein
- LP-IR
lipoprotein insulin resistance score
- T2D
type 2 diabetes
- UC
usual care
- VLDL-P
very low-density lipoprotein particle number
- WBC
white blood cell
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12933-018-0698-8) contains supplementary material, which is available to authorized users.
Contributor Information
Nasir H. Bhanpuri, Email: nbhanpuri@virtahealth.com
Sarah J. Hallberg, Email: hallbers@iuhhealth.org
Paul T. Williams, Email: 1742spyglass@comcast.net
Amy L. McKenzie, Email: amy@virtahealth.com
Kevin D. Ballard, Email: ballarkd@miamioh.edu
Wayne W. Campbell, Email: campbeww@purdue.edu
James P. McCarter, Email: jim@virtahealth.com
Stephen D. Phinney, Email: steve@virtahealth.com
Jeff S. Volek, Email: jeff@virtahealth.com
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gregg EW, Gu Q, Cheng YJ, Narayan KMV, Cowie CC. Mortality trends in men and women with diabetes, 1971 to 2000. Ann Intern Med. 2007;147:149–155. doi: 10.7326/0003-4819-147-3-200708070-00167. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) National diabetes statistics report, 2017. Atlanta: Centers for Disease Control and Prevention; 2017. pp. 1–20. [Google Scholar]
- 4.Martín-Timón I, Sevillano-Collantes C, Segura-Galindo A, Del Cañizo-Gómez FJ. Type 2 diabetes and cardiovascular disease: have all risk factors the same strength? World J Diabetes. 2014;5:444–470. doi: 10.4239/wjd.v5.i4.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saslow LR. An online intervention comparing a very low-carbohydrate ketogenic diet and lifestyle recommendations versus a plate method diet in overweight individuals with type 2 diabetes: a randomized controlled trial. J Med Internet Res. 2017;19:e36. doi: 10.2196/jmir.5806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boden G, Sargrad K, Homko C, Mozzoli M, Stein TP. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Intern Med. 2005;142:403–411. doi: 10.7326/0003-4819-142-6-200503150-00006. [DOI] [PubMed] [Google Scholar]
- 7.Yancy WS, Foy M, Chalecki AM, Vernon MC, Westman EC. A low-carbohydrate, ketogenic diet to treat type 2 diabetes. Nutr Metab. 2005;2:34. doi: 10.1186/1743-7075-2-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Westman EC, Yancy WS, Mavropoulos JC, Marquart M, McDuffie JR. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab. 2008;5:36. doi: 10.1186/1743-7075-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McKenzie A, Hallberg S, Creighton BC, Volk BM, Link T, Abner M, et al. A novel intervention including individualized nutritional recommendations reduces hemoglobin A1c level, medication use, and weight in type 2 diabetes. JMIR Diabetes. 2017;2:e5. doi: 10.2196/diabetes.6981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hallberg SJ, McKenzie AL, Williams PT, Bhanpuri NH, Peters AL, Campbell WW, et al. Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: an open-label, non-randomized, controlled study. Diabetes Ther. 2018;9:568–612. doi: 10.1007/s13300-018-0386-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wood TR, Hansen R, Sigurðsson AF, Jóhannsson GF. The cardiovascular risk reduction benefits of a low-carbohydrate diet outweigh the potential increase in LDL-cholesterol. Br J Nutr. 2016;115:1126–1128. doi: 10.1017/S0007114515005450. [DOI] [PubMed] [Google Scholar]
- 12.Mansoor N, Vinknes KJ, Veierød MB, Retterstøl K. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomised controlled trials. Br J Nutr. 2016;115:466–479. doi: 10.1017/S0007114515004699. [DOI] [PubMed] [Google Scholar]
- 13.Fruchart J-C, Sacks F, Hermans MP, Assmann G, Brown WV, Ceska R, et al. The Residual Risk Reduction Initiative: a call to action to reduce residual vascular risk in patients with dyslipidemia. Am J Cardiol. 2008;102:1K–34K. doi: 10.1016/j.amjcard.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Arca M, Pigna G, Favoccia C. Mechanisms of diabetic dyslipidemia: relevance for atherogenesis. Curr Vasc Pharmacol. 2012;10:684–686. doi: 10.2174/157016112803520864. [DOI] [PubMed] [Google Scholar]
- 15.Volek JS, Fernandez ML, Feinman RD, Phinney SD. Dietary carbohydrate restriction induces a unique metabolic state positively affecting atherogenic dyslipidemia, fatty acid partitioning, and metabolic syndrome. Prog Lipid Res. 2008;47:307–318. doi: 10.1016/j.plipres.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Taskinen M-R, Borén J. New insights into the pathophysiology of dyslipidemia in type 2 diabetes. Atherosclerosis. 2015;239:483–495. doi: 10.1016/j.atherosclerosis.2015.01.039. [DOI] [PubMed] [Google Scholar]
- 17.Ginsberg BH. Factors affecting blood glucose monitoring: sources of errors in measurement. J Diabetes Sci Technol. 2009;3:903–913. doi: 10.1177/193229680900300438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adiels M, Olofsson S-O, Taskinen M-R, Borén J. Overproduction of very low-density lipoproteins is the hallmark of the dyslipidemia in the metabolic syndrome. Arterioscler Thromb Vasc Biol. 2008;28:1225–1236. doi: 10.1161/ATVBAHA.107.160192. [DOI] [PubMed] [Google Scholar]
- 19.Cromwell WC, Otvos JD. Heterogeneity of low-density lipoprotein particle number in patients with type 2 diabetes mellitus and low-density lipoprotein cholesterol < 100 mg/dl. Am J Cardiol. 2006;98:1599–1602. doi: 10.1016/j.amjcard.2006.07.036. [DOI] [PubMed] [Google Scholar]
- 20.Sniderman AD, St-Pierre AC, Cantin B, Dagenais GR, Després J-P, Lamarche B. Concordance/discordance between plasma apolipoprotein B levels and the cholesterol indexes of atherosclerotic risk. Am J Cardiol. 2003;91:1173–1177. doi: 10.1016/S0002-9149(03)00262-5. [DOI] [PubMed] [Google Scholar]
- 21.Otvos JD, Mora S, Shalaurova I, Greenland P, Mackey RH, Goff DC. Clinical implications of discordance between low-density lipoprotein cholesterol and particle number. J Clin Lipidol. 2011;5:105–113. doi: 10.1016/j.jacl.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cromwell WC, Otvos JD, Keyes MJ, Pencina MJ, Sullivan L, Vasan RS, et al. LDL particle number and risk of future cardiovascular disease in the framingham offspring study—implications for LDL management. J Clin Lipidol. 2007;1:583–592. doi: 10.1016/j.jacl.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sniderman AD, Toth PP, Thanassoulis G, Furberg CD. An evidence-based analysis of the National Lipid Association recommendations concerning non-HDL-C and apoB. J Clin Lipidol. 2016;10:1248–1258. doi: 10.1016/j.jacl.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 24.Toth PP, Grabner M, Punekar RS, Quimbo RA, Cziraky MJ, Jacobson TA. Cardiovascular risk in patients achieving low-density lipoprotein cholesterol and particle targets. Atherosclerosis. 2014;235:585–591. doi: 10.1016/j.atherosclerosis.2014.05.914. [DOI] [PubMed] [Google Scholar]
- 25.Barter PJ, Ballantyne CM, Carmena R, Cabezas MC, Chapman MJ, Couture P, et al. Apo B versus cholesterol in estimating cardiovascular risk and in guiding therapy: report of the thirty-person/ten-country panel. J Intern Med. 2006;259:247–258. doi: 10.1111/j.1365-2796.2006.01616.x. [DOI] [PubMed] [Google Scholar]
- 26.Seshadri P, Iqbal N, Stern L, Williams M, Chicano KL, Daily DA, et al. A randomized study comparing the effects of a low-carbohydrate diet and a conventional diet on lipoprotein subfractions and C-reactive protein levels in patients with severe obesity. Am J Med. 2004;117:398–405. doi: 10.1016/j.amjmed.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 27.Volek JS, Sharman MJ, Gómez AL, DiPasquale C, Roti M, Pumerantz A, et al. Comparison of a very low-carbohydrate and low-fat diet on fasting lipids, LDL subclasses, insulin resistance, and postprandial lipemic responses in overweight women. J Am Coll Nutr. 2004;23:177–184. doi: 10.1080/07315724.2004.10719359. [DOI] [PubMed] [Google Scholar]
- 28.Volek JS, Phinney SD, Forsythe CE, Quann EE, Wood RJ, Puglisi MJ, et al. Carbohydrate restriction has a more favorable impact on the metabolic syndrome than a low fat diet. Lipids. 2008;44:297–309. doi: 10.1007/s11745-008-3274-2. [DOI] [PubMed] [Google Scholar]
- 29.Kannel WB, Anderson K, Wilson PW. White blood cell count and cardiovascular disease: insights from the Framingham Study. JAMA. 1992;267:1253–1256. doi: 10.1001/jama.1992.03480090101035. [DOI] [PubMed] [Google Scholar]
- 30.Yarnell JW, Baker IA, Sweetnam PM, Bainton D, O’Brien JR, Whitehead PJ, et al. Fibrinogen, viscosity, and white blood cell count are major risk factors for ischemic heart disease. The Caerphilly and Speedwell collaborative heart disease studies. Circulation. 1991;83:836–844. doi: 10.1161/01.CIR.83.3.836. [DOI] [PubMed] [Google Scholar]
- 31.Folsom AR, Aleksic N, Catellier D, Juneja HS, Wu KK. C-reactive protein and incident coronary heart disease in the Atherosclerosis Risk In Communities (ARIC) study. Am Heart J. 2002;144:233–238. doi: 10.1067/mhj.2002.124054. [DOI] [PubMed] [Google Scholar]
- 32.Ridker PM, Buring JE, Shih J, Matias M, Hennekens CH. Prospective study of C-reactive protein and the risk of future cardiovascular events among apparently healthy women. Circulation. 1998;98:731–733. doi: 10.1161/01.CIR.98.8.731. [DOI] [PubMed] [Google Scholar]
- 33.Libby P, Ridker PM, Hansson GK. Leducq transatlantic network on atherothrombosis. Inflammation in atherosclerosis: from pathophysiology to practice. J Am Coll Cardiol. 2009;54:2129–2138. doi: 10.1016/j.jacc.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Biondi-Zoccai GGL, Abbate A, Liuzzo G, Biasucci LM. Atherothrombosis, inflammation, and diabetes. J Am Coll Cardiol. 2003;41:1071–1077. doi: 10.1016/S0735-1097(03)00088-3. [DOI] [PubMed] [Google Scholar]
- 35.Wong ND, Zhao Y, Quek RGW, Blumenthal RS, Budoff MJ, Cushman M, et al. Residual atherosclerotic cardiovascular disease risk in statin-treated adults: the multi-ethnic study of atherosclerosis. J Clin Lipidol. 2017;11:1223–1233. doi: 10.1016/j.jacl.2017.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sampson UK, Fazio S, Linton MF. Residual cardiovascular risk despite optimal LDL cholesterol reduction with statins: the evidence, etiology, and therapeutic challenges. Curr Atheroscler Rep. 2012;14:1–10. doi: 10.1007/s11883-011-0219-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Group UPDS Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK prospective diabetes study group. BMJ. 1998;317:703–713. doi: 10.1136/bmj.317.7160.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mertz W, Tsui JC, Judd JT, Reiser S, Hallfrisch J, Morris ER, et al. What are people really eating? The relation between energy intake derived from estimated diet records and intake determined to maintain body weight. Am J Clin Nutr. 1991;54:291–295. doi: 10.1093/ajcn/54.2.291. [DOI] [PubMed] [Google Scholar]
- 39.Schmieder RE, Ruilope L-M, Barnett AH. Renal protection with angiotensin receptor blockers: where do we stand. J Nephrol. 2011;24:569–580. doi: 10.5301/JN.2011.6445. [DOI] [PubMed] [Google Scholar]
- 40.Jafar TH, Schmid CH, Landa M, Giatras I, Toto R, Remuzzi G, et al. Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann Intern Med. 2001;135:73–87. doi: 10.7326/0003-4819-135-2-200107170-00007. [DOI] [PubMed] [Google Scholar]
- 41.America Diabetes Association 4. Lifestyle management. Diabetes Care. 2017;40(Suppl 1):S33–S43. doi: 10.2337/dc17-S007. [DOI] [PubMed] [Google Scholar]
- 42.Tremblay AJ, Morrissette H, Gagné J-M, Bergeron J, Gagné C, Couture P. Validation of the Friedewald formula for the determination of low-density lipoprotein cholesterol compared with beta-quantification in a large population. Clin Biochem. 2004;37:785–790. doi: 10.1016/j.clinbiochem.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 43.Jeyarajah EJ, Cromwell WC, Otvos JD. Lipoprotein particle analysis by nuclear magnetic resonance spectroscopy. Clin Lab Med. 2006;26:847–870. doi: 10.1016/j.cll.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 44.van Schalkwijk DB, de Graaf AA, Tsivtsivadze E, Parnell LD, van der Werff-van der Vat BJC, van Ommen B, et al. Lipoprotein metabolism indicators improve cardiovascular risk prediction. PLoS ONE. 2014;9:e92840. doi: 10.1371/journal.pone.0092840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.May HT, Anderson JL, Winegar DA, Rollo J, Connelly MA, Otvos JD, et al. Utility of high density lipoprotein particle concentration in predicting future major adverse cardiovascular events among patients undergoing angiography. Clin Biochem. 2016;49:1122–1126. doi: 10.1016/j.clinbiochem.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 46.Shalaurova I, Connelly MA, Garvey WT, Otvos JD. Lipoprotein insulin resistance index: a lipoprotein particle-derived measure of insulin resistance. Metabol Syndr Relat Disord. 2014;12:422–429. doi: 10.1089/met.2014.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;2014:S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 48.Doneen AL, Bale BF. Carotid intima-media thickness testing as an asymptomatic cardiovascular disease identifier and method for making therapeutic decisions. Postgrad Med. 2013;125:108–123. doi: 10.3810/pgm.2013.03.2645. [DOI] [PubMed] [Google Scholar]
- 49.Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force endorsed by the society for vascular medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 50.UK Prospective Diabetes Study UKPDS Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. doi: 10.1016/S0140-6736(98)07019-6. [DOI] [PubMed] [Google Scholar]
- 51.Volek JS, Sharman MJ, Forsythe CE. Modification of lipoproteins by very low-carbohydrate diets. J Nutr. 2005;135:1339–1342. doi: 10.1093/jn/135.6.1339. [DOI] [PubMed] [Google Scholar]
- 52.Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy WS, Brehm BJ, et al. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med. 2006;166:285–293. doi: 10.1001/archinte.166.3.285. [DOI] [PubMed] [Google Scholar]
- 53.Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. BMJ. 2003;326:1423. doi: 10.1136/bmj.326.7404.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Giugliano RP, Pedersen TR, Park J-G, De Ferrari GM, Gaciong ZA, Ceska R, et al. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet. 2017;390:1962–1971. doi: 10.1016/S0140-6736(17)32290-0. [DOI] [PubMed] [Google Scholar]
- 55.Zuliani G, Volpato S, Dugo M, Vigna GB, Morieri ML, Maggio M, et al. Combining LDL-C and HDL-C to predict survival in late life: the InChianti study. PLoS ONE. 2017;12:e0185307. doi: 10.1371/journal.pone.0185307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Orozco-Beltran D, Gil-Guillen VF, Redon J, Martin-Moreno JM, Pallares-Carratala V, Navarro-Perez J, et al. Lipid profile, cardiovascular disease and mortality in a Mediterranean high-risk population: the ESCARVAL-RISK study. PLoS ONE. 2017;12:e0186196. doi: 10.1371/journal.pone.0186196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ravnskov U, Diamond DM, Hama R, Hamazaki T, Hammarskjöld B, Hynes N, et al. Lack of an association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly: a systematic review. BMJ Open. 2016;6:e010401. doi: 10.1136/bmjopen-2015-010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schmidt C, Bergstrom G. Apolipoprotein B and apolipopotein A-I in vascular risk prediction—a review. Curr Pharm Des. 2014;20:6289–6298. doi: 10.2174/1381612820666140620121828. [DOI] [PubMed] [Google Scholar]
- 59.Austin MA, Breslow JL, Hennekens CH, Buring JE, Willett WC, Krauss RM. Low-density lipoprotein subclass patterns and risk of myocardial infarction. JAMA. 1988;260:1917–1921. doi: 10.1001/jama.1988.03410130125037. [DOI] [PubMed] [Google Scholar]
- 60.Tani S, Yagi T, Atsumi W, Kawauchi K, Matsuo R, Hirayama A. Relation between low-density lipoprotein cholesterol/apolipoprotein B ratio and triglyceride-rich lipoproteins in patients with coronary artery disease and type 2 diabetes mellitus: a cross-sectional study. Cardiovasc Diabetol. 2017;16:123. doi: 10.1186/s12933-017-0606-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bertsch RA, Merchant MA. Study of the use of lipid panels as a marker of insulin resistance to determine cardiovascular risk. Perm J. 2015;19:4–10. doi: 10.7812/TPP/14-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bezafibrate Infarction Prevention (BIP) study Secondary prevention by raising HDL cholesterol and reducing triglycerides in patients with coronary artery disease. Circulation. 2000;102:21–27. doi: 10.1161/01.CIR.102.1.21. [DOI] [PubMed] [Google Scholar]
- 63.Ridker PM, Danielson E, Fonseca FAH, Genest J, Gotto AM, Jr, Kastelein JJP, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 64.Albert MA, Danielson E, Rifai N, Ridker PM, PRINCE Investigators Effect of statin therapy on C-reactive protein levels: the pravastatin inflammation/CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA. 2001;286:64–70. doi: 10.1001/jama.286.1.64. [DOI] [PubMed] [Google Scholar]
- 65.Asher J, Houston M. Statins and C-reactive protein levels. J Clin Hypertens (Greenwich) 2007;9:622–628. doi: 10.1111/j.1524-6175.2007.06639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Youm Y-H, Nguyen KY, Grant RW, Goldberg EL, Bodogai M, Kim D, et al. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat Med. 2015;21:263–269. doi: 10.1038/nm.3804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017 doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 68.Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 69.Kuznik A, Mardekian J. Trends in utilization of lipid- and blood pressure-lowering agents and goal attainment among the US diabetic population, 1999–2008. Cardiovasc Diabetol. 2011;10:31. doi: 10.1186/1475-2840-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shai I, Spence JD, Schwarzfuchs D, Henkin Y, Parraga G, Rudich A, et al. Dietary intervention to reverse carotid atherosclerosis. Circulation. 2010;121:1200–1208. doi: 10.1161/CIRCULATIONAHA.109.879254. [DOI] [PubMed] [Google Scholar]
- 71.Gress TW, Nieto FJ, Shahar E, Wofford MR, Brancati FL. Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. Atherosclerosis risk in communities study. N Engl J Med. 2000;342:905–912. doi: 10.1056/NEJM200003303421301. [DOI] [PubMed] [Google Scholar]
- 72.Lorenz MW, Price JF, Robertson C, Bots ML, Polak JF, Poppert H, et al. Carotid intima-media thickness progression and risk of vascular events in people with diabetes: results from the PROG-IMT collaboration. Diabetes Care. 2015;38:1921–1929. doi: 10.2337/dc14-2732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Riley WA. Cardiovascular risk assessment in individual patients from carotid intimal-medial thickness measurements. Curr Atheroscler Rep. 2004;6:225–231. doi: 10.1007/s11883-004-0036-3. [DOI] [PubMed] [Google Scholar]
- 74.Gardner CD, Trepanowski JF, Del Gobbo LC, Hauser ME, Rigdon J, Ioannidis JPA, et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion. JAMA. 2018;319:667–679. doi: 10.1001/jama.2018.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Detailed baseline characteristics for participants in the continuous care intervention (CCI) and usual care (UC) groups.
Additional file 2: Table S2. Details on 1-year biomarker changes for participants in the continuous care intervention group compared to usual care group.
Additional file 3: Figure S1. Distribution of changes in selected biomarkers for CCI and UC completers. Histograms of changes at one year for CCI (blue) and UC (gray) are overlaid. Very few (≤1%) CCI participants demonstrated changes in an undesirable direction at one year that were outside the range of changes observed in the UC group for key lipid and lipoprotein particles. (A) Apolipoprotein B (B) Apolipoprotein A1 (C) Apolipoprotein B/Apolipoprotein A1 ratio (D) LDL-P (E) Small LDL-P (F) Large VLDL-P (G) Triglyceride/HDL-C ratio.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


