Abstract
Certain nutrients are able to exert health promoting effects. The consumption of Brassicaceae vegetables has increased given their reported beneficial effects on human health, due to their high content of nutraceutical compounds. The health benefits appear to be associated with the presence of glucosinolates and flavonoids. Certain nutraceutics have been revealed to have anti-inflammatory action. In the present study, the anti-inflammatory properties of Eruca sativa seed extract (ESE) were evaluated in NSC-34 motor neurons exposed to the cell culture medium of lipopolysaccharide (LPS)-stimulated RAW 264.7 macrophages. Treatment with LPS-stimulated RAW 264.7 medium induced apoptosis and the expression of Toll-like receptor 4 (TLR4) and cyclooxygenase 2 (COX2) in NSC-34 motor neurons. Additionally, the stimulation of NSC-34 motor neurons with the medium of LPS-treated macrophages triggered the expression of NLR family pyrin domain containing 3 (NLRP3) inflammasome proteins and the production of pro-inflammatory cytokines. Pre-treatment with ESE counteracted the apoptosis and production of pro-inflammatory cytokines in NSC-34 motor neurons treated with the medium of LPS-treated RAW 264.7. It also eliminated COX2 and TLR4/NLRP3 inflammasome expression. In addition, pre-treatment with ESE was able to restore interleukin 10 expression in NSC-34 cells. These results demonstrate the anti-inflammatory and neuroprotective effects of ESE.
Keywords: brassicaceae, Eruca sativa seed, motor neuron, neuroinflammation, neuroprotection
Introduction
Some nutrients present in food possessed some medicinal properties and may be used for the prevention and/or treatment of different diseases. Generally, these nutrients are called nutraceutic, a term derived from ‘nutrition’ and ‘pharmaceutics’ (1). Nutraceutics received a lot of attention because of their potential therapeutic effects, but also thanks to their safety. Indeed, given that they are natural compounds, nutraceutics can be safer and without adverse reactions. Among nutraceutical compounds, glucosinolates (GLSs) and flavonoids are among the most investigated categories.
In the last decades the consumption of members of the Brassicaceae family increased, because they are able to exert beneficial effects on human health, due to their content in nutraceutics (2). In particular, Brassicaceae are known to contain GLSs, that mediate some of the health benefits, but the health promoting effects seem to be associated also with the presence of phenolic compounds, including flavonoids (3,4). In particular, Brassica seeds seemed very rich in GLSs (5). Brassicaceae family includes vegetables normally consumed in our diet such as broccoli, Brussels sprouts, cabbage and collards. Another member of this family is Eruca sativa, generally known as rocket salad, that is an edible plant widespread in the Mediterranean area, known for its medicinal properties. Indeed, Eruca sativa extracts were reported to exert antioxidant, antiplatelet, antithrombotic, anticancer and antimicrobial properties (6–9). Eruca sativa, including its seeds, contained different compounds known for their nutraceutic potential, including GLSs and flavonoids (9,10). Interestingly, these classes of nutraceutics have shown neuroprotective effects, thank to their antioxidant and anti-inflammatory activities (11–13), suggesting their use for the prevention of neurodegenerative diseases.
The anti-inflammatory action of these compounds is particularly interesting considering that inflammation plays a main role in different pathologies. Indeed, inflammation acts as a defensive response when a tissue is damaged by toxins or infective agents in order to repair the tissue and eliminate the causative factors, but, when it is prolonged, it may be detrimental. In particular, nervous system is more sensitive to inflammation compared to other tissues, given its limited regeneration capacity. Indeed, neuroinflammation has been associated with different disorders, including neurodegenerative diseases (14,15). During neuroinflammation, different mechanisms cause neuronal degeneration and death, including the release of different cytokines by activated microglia and the infiltration of the central nervous system by immune cells from the periphery (14). Given this, the research is focused on the discovery of new anti-inflammatory compounds that can be helpful for the treatment and/or prevention of neurodegenerative disorders.
The aim of this study was the evaluation of the anti-inflammatory potential of Eruca sativa seed extract (ESE). Specifically, we evaluated the anti-inflammatory and neuroprotective effects exerted by ESE pre-treatment in NSC-34 motor neurons exposed to the culture medium of lipopolysaccharide (LPS)-stimulated RAW 264.7 macrophages.
Materials and methods
ESE preparation and characterization
Eruca sativa seeds were supplied by SAIS spa (Cesena, Italy; license: no. 12, 6/7/1973; authorization from Regione Emilia Romagna 43) and guaranteed by the producer for the quality and the genetic homogeneity of the product. Seeds were soaked for 15 min in 1% sodium hypochlorite and washed with tap water. Subsequently, the seeds were air dried at a temperature of 30°C for approximately 8–12 min, were ground and again air dried with forced ventilation. ESE was characterized by HPLC analysis.
For cell culture experiments, ESE was dissolved in dimethyl sulfoxide (DMSO) and diluted in the cell culture medium.
RAW 264.7 macrophage cell culture and treatment
RAW 264.7, a murine macrophage cell line obtained from ‘Centro Substrati Cellulari, Istituto Zooprofilattico Sperimentale della Lombardia e dell'Emilia’ (Brescia, Italy) were cultured in monolayer at 37°C in a moisturized atmosphere of 5% CO2 and 95% air using DMEM-high glucose medium (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) supplemented with 10% fetal bovine serum (FBS; Sigma-Aldrich; Merck KGaA). In order to induce an inflammatory state, cells were grown until 70–80% confluence was reached, and after they were incubated with 1 µg/ml LPS from Escherichia coli 0111:B4 (Sigma-Aldrich; Merck KGaA) for 24 h. Untreated cells were used as control. At the end of the treatment, cells were either fixed or harvested for other analyses, while the culture medium was collected to carry out experiments with NSC-34 cells. All the experiments were made in triplicates and repeated three independent times.
NSC-34 motor neurons cell culture and treatment with the culture medium of LPS-stimulated RAW 264.7
NSC-34 motor neurons, a murine cell line acquired from Cedarlane/CELLutions Biosystems Inc. (Burlington, ON, Canada), were cultured in DMEM-high glucose medium (Sigma-Aldrich; Merck KGaA) with the addiction of 10% FBS (Sigma-Aldrich; Merck KGaA), at 37°C in a moisturized atmosphere of 5% CO2 and 95% air. We evaluated the cytotoxicity of ESE, exposing NSC-34 cells for 24 h to different concentrations of ESE. In particular, we tested the following concentrations of ESE: 0.1, 0.2, 0.3 and 0.4 µg/ml. To examine anti-inflammatory effects of ESE against LPS-induced inflammation, NSC-34 cells were pre-treated for 24 h with ESE. At the end of pre-treatment, medium was replaced with cell-free conditioned medium from LPS-stimulated RAW 264.7 macrophage, and incubated for 24 h. As controls, NSC-34 were incubated with the medium of unstimulated RAW 264.7. Cells treated with vehicle (<0.1% DMSO) or with the ESE alone were also included as controls. Then, motor neuronal cells were fixed for eosin/hematoxylin staining or immunocytochemistry analysis. All the experiments were done in triplicate and repeated for three independent times.
Eosin and hematoxylin staining
RAW 264.7 and NSC-34 morphological changes were evaluated by eosin and hematoxylin staining applying a standard protocol. Cells, grown on coverslips (10 mm; Thermo Fisher Scientific, Darmstadt, Germany), were fixed with 4% paraformaldehyde (Santa Cruz Biotechnology, Inc., Dallas, TX, USA) for 15 min at room temperature. Cells were washed with 1X phosphate-buffered saline (PBS) and stained with hematoxylin Harris (Bio-Optica, Milan, Italy) for 1 min, rinsed with tap water, stained with eosin (Bio-Optica) for 5 min, and rinsed with distilled water. After, coverslips were dehydrated with ethanol series (Carlo Erba Reagents, Valde-Reuil, France; 50, 70, 80, 96, and 100%) and xylene (J.T. Baker, Deventer, The Netherlands). Subsequently, coverslips were mounted on microscope slides with mounting medium (Eukitt, Carlo Erba Reagents, Valde-Reuil, France) and allowed to dry. Microscopy was performed using a light microscope (Leica DM 2000 combined with Leica ICC50 HD camera) with the objective ×20 (for RAW 264.7 macrophages) or ×40 (for NSC-34 motoneurons). All images are representative of three independent experiments.
Immunocytochemistry
RAW 264.7 macrophages and NSC-34 motor neurons were grown on coverslips (10 mm; Thermo Fisher Scientific, Oberhausen, Germany) and, at the end of the treatments, they were fixed with 4% paraformaldehyde at room temperature for 15 min and after washed with PBS (pH 7.5). Then, cells were incubated with 3% hydrogen peroxide (H2O2) at room temperature for 15 min to suppress the endogenous peroxidase activity. After three washes with PBS, cells were blocked with horse serum +0.1% Triton X-100 for 20 min and incubated overnight at 4°C with primary antibodies. In particular, RAW 264.7 cells were incubated with the following antibodies against examined proteins: mouse monoclonal antibody against interleukin (IL)-1β (cat. no. 12242; 1:100; Cell Signaling Technology, Inc., Danvers, MA, USA), rabbit polyclonal antibody against Fas Ligand (FasL; cat. no. ab15285; 1:100; Abcam, Cambridge, UK), goat polyclonal antibody against P-selectin (cat. no. sc-6943; 1:50; Santa Cruz Biotechnology, Inc.) and rat monoclonal antibody against IL-10 (cat. no. sc-73309; 1:100; Santa Cruz Biotechnology, Inc.).
NSC-34 were incubated with the following primary antibodies against examined proteins: rabbit polyclonal antibody against tumor necrosis factor-α (TNF-α; cat. no. 3707; 1:250; Cell Signaling Technology, Inc.), rat monoclonal antibody against IL-10 (cat. no. sc-73309; 1:100; Santa Cruz Biotechnology, Inc.), rabbit polyclonal antibody against FasL (cat. no. ab15285; 1:100; Abcam), mouse monoclonal antibody against cyclooxygenase 2 (COX2; cat. no. sc-166475; 1:100; Santa Cruz Biotechnology, Inc.), rabbit monoclonal antibody against caspase 1 (cat. no. ab108362; 1:100; Abcam), rat monoclonal antibody against NLR family pyrin domain containing 3 (NLRP3; cat. no. MAB7578; 1:100; R&D Systems, Minneapolis, MN, USA), rabbit polyclonal antibody against IL-18 (cat. no. ab191152; 1:100; Abcam), mouse monoclonal antibody against IL-1β (cat. no. 12242; 1:100; Cell Signaling Technology, Inc.) and mouse monoclonal antibody against Toll-like receptor 4 (TLR4; cat. no. ab22048; 1:100; Abcam).
After, cells were washed with PBS and incubated with biotinylated secondary antibody (1:200; Vector Laboratories, Inc., Burlingame, CA, USA) and streptavidin AB Complex-HRP (ABC-kit from Dako, Glostrup, Denmark). The immunostaining was developed with the DAB peroxidase substrate kit (Vector Laboratories, DBA Italia S.r.l., Milan, Italy; brown color; positive staining) and counterstaining with nuclear fast red (Vector Laboratories, DBA Italia S.r.l.; pink background; negative staining).
The immunocytochemical assays were repeated three times and each experimental group was plated in duplicate, for a total of 6 coverslips for each antibody. With the aim of calculating the percentage of positive cells stained, the images were captured using a light microscopy (LEICA DM 2000 combined with LEICA ICC50 HD camera) with an objective ×40 and the densitometric analysis was carried out using the software LEICA Application Suite ver. 4.2.0. Quantitative analysis was performed on 6 coverslips by covering approximately 90% of the total area.
Protein extraction and western blot analysis
At the end of the treatment, RAW 264.7 cells were harvested and lysed using buffer A [320 mM sucrose, 10 mM, 1 mM EGTA, 2 mM EDTA, 5 mM NaN3, 50 mM NaF, β-mercaptoethanol, and protease/phosphatase inhibitor cocktail (Roche Molecular Diagnostics, Branchburg, NJ, USA)] in ice for 15 min, and centrifuged at 1,000 × g for 10 min at 4°C. The supernatant was collected as cytosolic extract. The obtained pellet was lysed using buffer B [150 mM NaCl, 10 mM Tris-HCl (pH 7.4), 1 mM EGTA, 1 mM EDTA, Triton X-100, and protease/phosphatase inhibitor cocktail (Roche Molecular Diagnostics)] in ice for 15 min and centrifuged at 15,000 × g for 30 min at 4°C. The supernatant was harvested as nuclear extract. Protein concentrations were analyzed using the Bradford assay (Bio-Rad Laboratories, Inc., Hercules, CA, USA). Twenty µg of proteins were heated for 5 min at 95°C and resolved by SDS-polyacrylamide gel electrophoresis (SDS-PAGE) and after transferred onto a PVDF membrane (Immobilon-P, Millipore, DBA Italia S.r.l., Milan, Italy).
After, membranes were blocked with 5% skim milk in PBS for 1 h at room temperature and incubated overnight at 4°C with the following primary antibodies: Rabbit polyclonal antibody against TNF-α (cat. no. 3707; 1:500; Cell Signaling Technology, Inc.) and rat monoclonal antibody against IL-10 (cat. no. sc-73309; 1:500; Santa Cruz Biotechnology, Inc.). After the membranes were washed with PBS 1X and incubated with horse radish peroxidase (HRP)-conjugated goat anti-rabbit or chicken anti-rat IgG secondary antibody (cat. nos. sc-2004 and sc-2956, respectively; 1:2,000; Santa Cruz Biotechnology, Inc.) for 1 h at room temperature. In order to evaluate if blots were loaded with equal amounts of proteins, membranes were incubated with antibody for glyceraldehyde 3-phosphate dehydrogenase (GAPDH) HRP Conjugated (cat. no. 3683; 1:1,000; Cell Signaling Technology, Inc.). The relative expression of protein bands was analyzed using an enhanced chemiluminescence system (Luminata Western HRP Substrates; Millipore, DBA Italia S.r.l.) and protein bands were acquired with ChemiDoc™ MP System (Bio-Rad Laboratories, Inc.) and quantified using the computer program ImageJ software. All blots are representative of three independent experiments.
Statistical data analysis
Statistical analysis was performed using GraphPad Prism version 6.0 computer software program (GraphPad Software, Inc., La Jolla, CA, USA). The data were statistically analyzed by Student's t-test for the comparison between 2 groups or by one-way ANOVA test and Bonferroni post hoc test for multiple comparisons. P<0.05 was considered to indicate a statistically significant difference. Results are reported as mean ± SEM of N experiments.
Results
Characterization of Eruca sativa seed
ESE was chemically characterized by HPLC. Analysis showed that glucoerucin was the GLS present in higher quantity in ESE, and in particular the extract contained 46.36 mg glucoerucin/g of ESE. Moreover, the ESE contained 0.16 mg/g dry weight of ascorbic acid and 1.99 mg/g dry weight of total flavonoids.
Evaluation of the presence of inflammation in LPS-treated RAW 264.7 macrophages
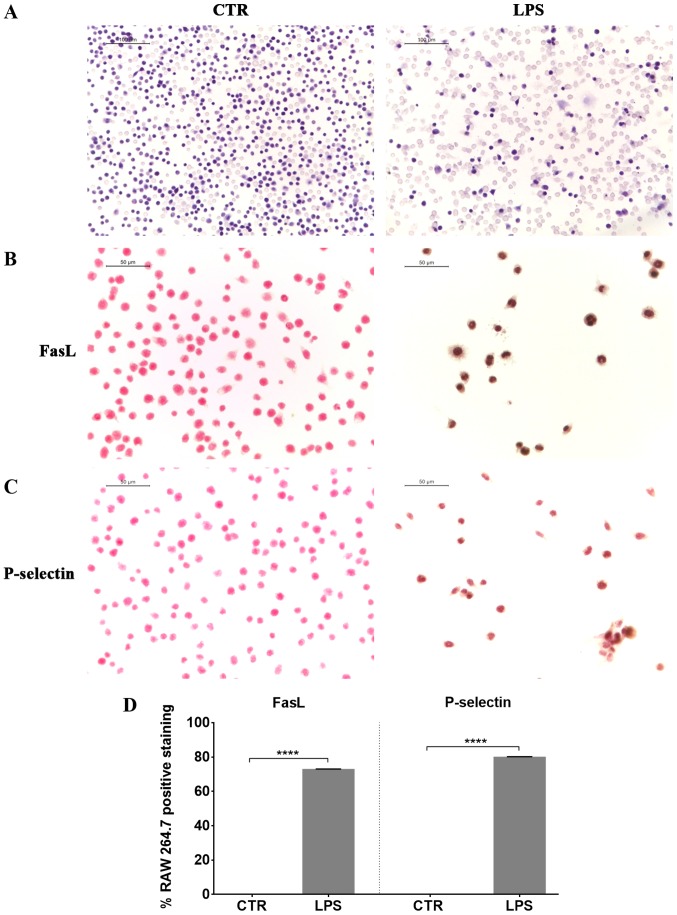
At first we induced inflammation in RAW 264.7 cells, exposing them to LPS. Eosin and hematoxylin staining of LPS stimulated RAW 264.7 showed morphological changes, such as an increase in cell size and the extension of lamellipodia and filopodia (Fig. 1). We observed a positive staining for FasL in LPS treated cells compared to controls (Fig. 1), indicating the induction of apoptosis in LPS-treated macrophages. Furthermore, RAW 264.7 macrophages exposed to LPS presented a positive staining for P-selectin (Fig. 1).
Figure 1.
Lipopolysaccharide (LPS) stimulation induced morphological changes, cell death and P-selectin expression in RAW 264.7 macrophages. (A) Eosin and hematoxylin staining showed an increase in cell size and the production of lamellipodia and filopodia in LPS-stimulated RAW 264.7 compared to control cells (Scale bar=100 µm). Moreover, LPS stimulation induced apoptosis, as indicated by the expression of (B) FasL, and expression of (C) P-selectin as showed by immunocytochemistry with (D) quantitative analysis of positive staining (Scale bar=50 µm). ****P<0.0001, significant differences in LPS-stimulated RAW 264.7 (n=6) vs. control (CTR) (n=6).
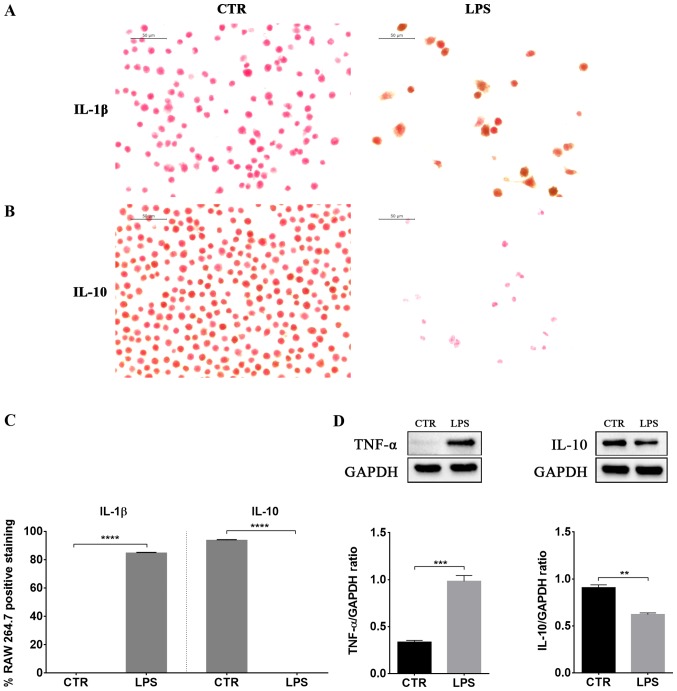
LPS-induced inflammation was associated with increased protein levels of the pro-inflammatory cytokines TNF-α and IL-1β (Fig. 2). Instead, IL-10 levels, a well known anti-inflammatory cytokine, decreased in LPS stimulated macrophages compared to control cells (Fig. 2).
Figure 2.
Lipopolysaccharide (LPS) stimulated RAW 264.7 macrophages expressed pro-inflammatory cytokines but not the anti-inflammatory cytokine interleukin (IL)-10. Immunocytochemical localization for (A) IL-1β and (B) IL-10 with (C) quantitative analysis of positive staining and (D) western blot analysis of cytokines tumor necrosis factor-α (TNF-α) and IL-10, showed that LPS treatment increased TNF-α and IL-1β levels, while IL-10 levels decreased. Scale bar=50 µm. **P<0.01, ***P<0.001, ****P<0.0001, significant differences in LPS-stimulated RAW 264.7 (n=6 for immunocytochemistry; n=3 for western blotting) vs. control (CTR; n=6 for immunocytochemistry; n=3 for western blotting). GAPDH, glyceraldehyde 3-phosphate dehydrogenase.
Evaluation of ESE anti-inflammatory and neuroprotective effects in NSC-34 motor neurons exposed to the medium of LPS-treated RAW 264.7
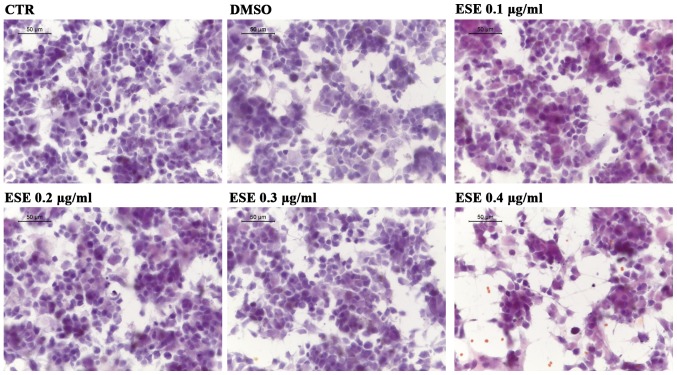
After confirming the presence of inflammation in macrophages, we evaluated whether ESE was able to counteract the inflammation induced in NSC-34 by the medium of LPS-treated RAW 264.7. At first we assessed whether the ESE caused cytotoxicity or morphological changes in NSC-34, using the concentrations of the extract 0.1, 0.2, 0.3 and 0.4 µg/ml. Our results showed no cytotoxicity for the concentrations 0.1, 0.2 and 0.3 µg/ml of ESE, while the highest concentration showed a moderate cytotoxicity, associated with the presence of cell debris (Fig. 3). Given that the extract was dissolved in DMSO, we included in our analysis also NSC-34 motor neurons incubated with a concentration of DMSO comparable to that used for the highest concentration of ESE, but no cytotoxicity was observed (Fig. 3).
Figure 3.
Evaluation of morphological changes in NSC-34 motor neurons exposed to different concentrations of Eruca sativa seed extract (ESE). Hematoxylin and eosin staining showed no cytotoxicity with the concentrations 0.1, 0.2 and 0.3 µg/ml of ESE. Only the highest concentration (0.4 µg/ml) showed a moderate cytotoxicity. Given that the extract was dissolved in dimethyl sulfoxide (DMSO), we evaluated also a concentration of DMSO comparable to that used for the highest concentration of ESE, but no cytotoxicity was observed. Scale bar=50 µm.
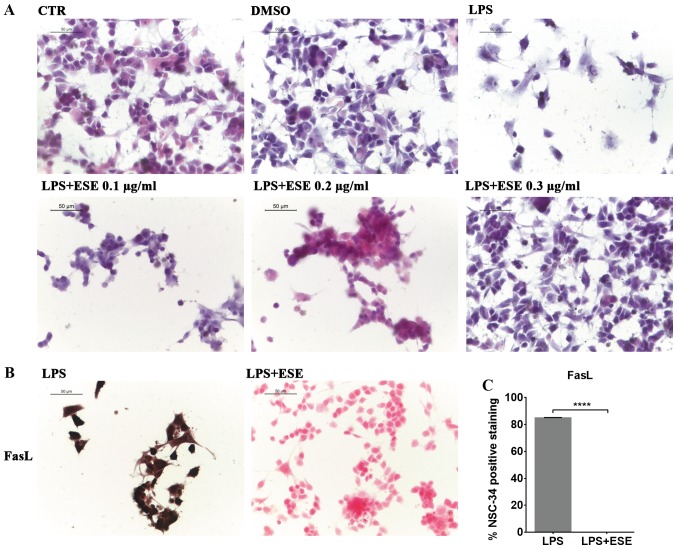
We evaluated the morphological changes induced in NSC-34 by the medium of LPS-stimulated RAW 264.7. By eosin/hematoxylin staining, we observed that NSC-34 motor neurons exposed to the medium of LPS-treated RAW 264.7 showed cell death and degeneration. However, only the pre-treatment with ESE 0.3 µg/ml was able to prevent LPS-induced morphological changes, preserving the neural morphology that was similar to that of control cells (Fig. 4A). Instead, lower concentrations of the extract were not able to counteract LPS induced effects (Fig. 4A), while we did not evaluate the concentration 0.4 µg/ml of ESE, given its moderate cytotoxicity. For this reason we decided to continue the experiments with the concentration 0.3 µg/ml of ESE.
Figure 4.
Evaluation of morphological changes and apoptosis in NSC-34 motoneurons exposed to the cell culture medium of lipopolysaccharide (LPS)-stimulated RAW 264.7 macrophages and pre-treated with Eruca sativa seed extract (ESE). (A) Eosin/Hematoxylin staining in NSC-34 cells exposed to LPS conditioned medium showed cell death and degeneration. Pre-treatment with ESE at the concentration 0.3 µg/ml was able to counteract LPS-induced morphological changes, while lower concentrations were not able to exert protection. (B) Immunocytochemistry and (C) quantitative analysis of positive staining showed FasL expression in NSC-34 motor neurons treated with the medium of LPS-stimulated RAW 264.7, indicating the induction of apoptosis. However, pre-treatment with ESE was able to abolish FasL expression. Scale bar=50 µm. ****P<0.0001 significant differences in NSC-34 treated with the medium of LPS-stimulated RAW 264.7 (n=6) vs. NSC-34 treated with the medium of LPS-stimulated RAW 264.7 + ESE (n=6). DMSO, dimethyl sulfoxide.
The treatment of NSC-34 motor neurons with the medium of LPS-stimulated RAW 264.7, induced apoptosis associated with FasL positive staining (Fig. 4B). However, our results showed that the pre-treatment with ESE was able to counteract apoptosis, as demonstrated by FasL negative staining (Fig. 4B and C). NSC-34 control cells, and those incubated with DMSO or with ESE alone did not express FasL (data not shown).
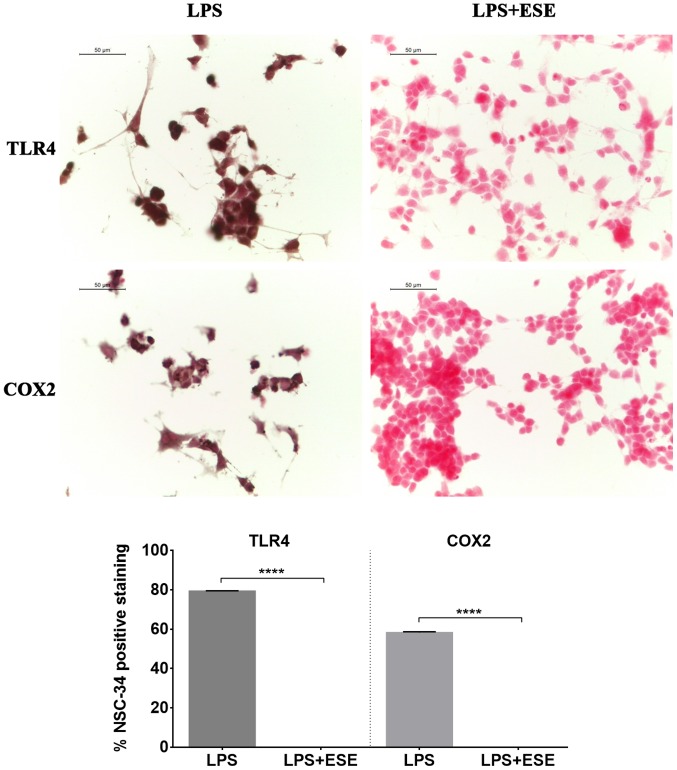
We observed TLR4 positive staining in NSC-34 motor neurons exposed to the culture medium of LPS-stimulated macrophages (Fig. 5). Moreover, we evaluated also COX2 expression, and we found that NSC-34 motor neurons stimulated with the medium of LPS-treated RAW 264.7 macrophages showed a positive staining for COX2 (Fig. 5). These results suggested that inflammation depends on both TLR4 and COX2 pathway activation. Interestingly, NSC-34 pre-treated with ESE did not express TLR4 and COX2 proteins. NSC-34 motor neurons used as controls or incubated with DMSO, or with the extract alone did not show expression of neither TLR4 nor COX2 (data not shown), indicating the absence of inflammation.
Figure 5.
Eruca sativa seed extract (ESE) abolished Toll-like receptor 4 (TLR4) and cyclooxygenase 2 (COX2) expression. Immunocytochemistry and quantitative analysis of positive staining indicated that NSC-34 treated with the medium of lipopolysaccharide (LPS)-stimulated RAW 264.7 showed a positive staining for TLR4 and COX2, but the pre-treatment with ESE was able to abolish the expression of TLR4 and COX2. Scale bar=50 µm. ****P<0.0001 significant differences in NSC-34 treated with the medium of LPS-stimulated RAW 264.7 (n=6) vs. NSC-34 treated with the medium of LPS-stimulated RAW 264.7 + ESE (n=6).
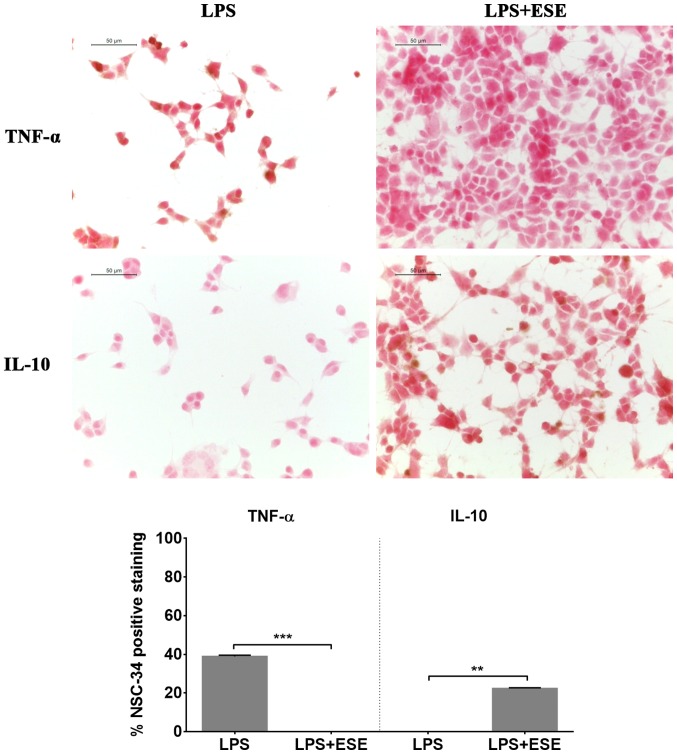
Moreover, we evaluated cytokine levels and observed that NSC-34 cells exposed to the culture medium of LPS-stimulated RAW 264.7 did not show the expression of IL-10, but they showed a positive staining for the pro-inflammatory cytokine TNF-α (Fig. 6). Pre-treatment with ESE recovered the expression of IL-10, while the expression of the pro-inflammatory cytokine was abolished. Cells incubated with DMSO or with the seed extract alone expressed IL-10, but not TNF-α (data not shown).
Figure 6.
Eruca sativa seed extract (ESE) abolished tumor necrosis factor-α (TNF-α) expression and recovered interleukin (IL)-10 expression. Immunocytochemistry and quantitative analysis of positive staining showed that the treatment with the medium of lipopolysaccharide (LPS)-stimulated RAW 264.7 increased in NSC-34 the expression of TNF-α, but the pre-treatment with ESE was able to counteract the increase of the pro-inflammatory cytokine. Moreover, the pre-treatment with the seed extract was able to induce the expression of the anti-inflammatory cytokine IL-10. Scale bar=50 µm. **P<0.01, ***P<0.001 significant differences in NSC-34 treated with the medium of LPS-stimulated RAW 264.7 (n=6) vs. NSC-34 treated with the medium of LPS-stimulated RAW 264.7 + ESE (n=6).
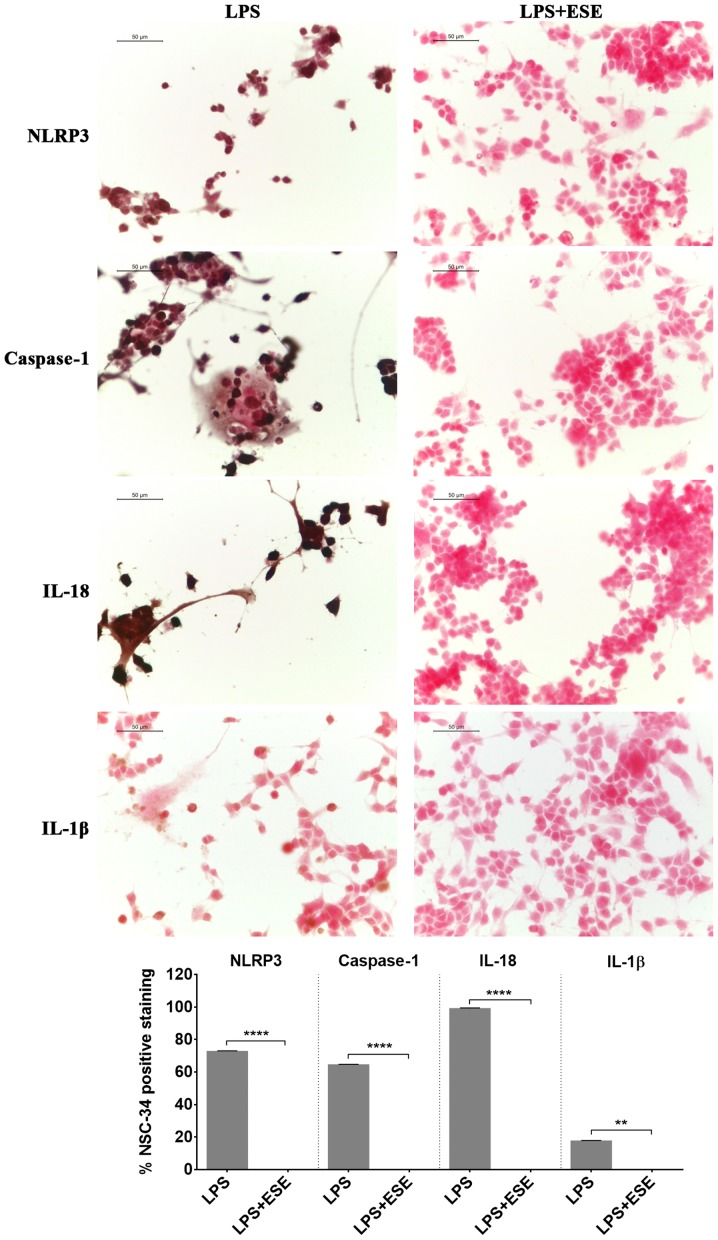
Inflammation may be also mediated by a protein complex known as inflammasome, a cytoplasmic protein complex that mediates pro-inflammatory responses. It is formed by a pattern recognition receptor, acting like sensor of damage, such as of pathogen associated molecular patterns, that when activated, induced the production of active caspase 1 (16,17). The NLRP3 inflammasome, formed by NLRP3 that belongs to the NOD-like receptor (NLR) family, is the most studied. When the inflammasome is activated, the cleavage of pro-caspase 1 is induced to form the active caspase 1, that in turn converts the inactive IL-18 and IL-1β into the active forms, triggering inflammation (16,17). We found NLRP3 and caspase 1 positive staining in NSC-34 stimulated with the LPS-conditioned medium of RAW 264.7 macrophages indicating the activation of inflammasome. According to the activation of caspase 1, we observed the expression of the proinflammatory cytokines IL-18 and IL-1β (Fig. 7). However, the pre-treatment of NSC-34 with ESE was able to abolish the expression of NLRP3 and caspase 1 and, consequently, the production of IL-18 and IL-1β (Fig. 7). NSC-34 control cells, or incubated with DMSO or with the extract alone, did not express inflammasome proteins (data not shown).
Figure 7.
Eruca sativa seed extract (ESE) inhibited NLR family pyrin domain containing 3 (NLRP3) inflammasome. Immunocytochemistry and the quantitative analysis of positive staining showed that the treatment with the conditioned medium of lipopolysaccharide (LPS) treated RAW 264.7 macrophages induced the activation of NLRP3 inflammasome in NSC-34 motor neurons. The pre-treatment with ESE was able to abolish the expression of inflammasome proteins. Scale bar=50 µm. **P<0.01, ****P<0.0001 significant differences in NSC-34 treated with the medium of LPS-stimulated RAW 264.7 (n=6) vs. NSC-34 treated with the medium of LPS-stimulated RAW 264.7 + ESE (n=6).
Discussion
Nutrition plays a main role in human health, and may influence the development and progression of chronic diseases, including neurodegenerative disorders (18). For this reason the use of nutritional supplements and plant extracts in disease prevention is of great importance, especially for neurodegenerative conditions, where the therapeutic options are limited. In particular, Brassicaceae vegetables consumption has demonstrated different health benefits, thank to the presence of different phytochemicals (2,19,20).
The aim of our work was to evaluate the anti-inflammatory effects of ESE. We focalized our attention on neuroinflammation, that plays a pivotal role in different neurodegenerative disorders (14,15). For this reason, we evaluated the anti-inflammatory properties of the extract in NSC-34 motor neurons exposed to the cell culture medium of LPS-stimulated RAW 264.7 macrophages. The ESE contained the GLS glucoerucin, ascorbic acid and flavonoids. As reported in the literature, the GLSs present in bigger amount in Eruca sativa seeds is glucoerucin (21,22).
Our results confirmed the induction of inflammation in LPS-stimulated RAW 264.7. Indeed, LPS-treated RAW 264.7 showed morphological changes, including the extension of lamellipodia and filopodia and an increased cell size, as reported in literature (23). Moreover, it is known that LPS was able to induce apoptosis in macrophages, through the autocrine secretion of TNF-α and the production of nitric oxide (NO) (24). Accordingly, in our model we observed the induction of apoptosis as demonstrated by FasL positive staining in LPS treated cells compared to controls. FasL is a member of the TNF family of cytokines that binds the Fas receptor, one of the TNF-receptor family of proteins. The Fas-FasL system plays a main role in the induction of the extrinsic apoptotic pathway (25). Moreover, our results showed the expression of P-selectin in RAW 264.7 macrophages exposed to LPS. P-selectin is an adhesion molecule expressed mainly in platelets and endothelial cells, but it was reported that it may be also expressed in macrophages (26). Selectins mediate the leukocyte extravasation and rolling on vascular surface in order to permit to reach the inflammation site, and in particular some cytokines and LPS are able to increase P-selectin transcription (27). LPS induced inflammation is mediated by the release of pro-inflammatory cytokine (28). Indeed, also in our model we observed that LPS treatment increased the protein levels of the pro-inflammatory cytokines TNF-α and IL-1β in RAW 264.7, while the level of the anti-inflammatory cytokine IL-10 decreased.
After having assessed the presence of inflammation in RAW 264.7 macrophages exposed to LPS, we evaluated whether ESE was able to counteract the inflammation induced in NSC-34 by the medium of LPS-treated RAW 264.7. We observed that the pre-treatment with 0.3 µg/ml ESE was able to prevent LPS-induced morphological changes and apoptosis, as demonstrated by FasL negative staining. Notably, the system Fas-FasL showed an increased expression in the brain during inflammation, neurologic and neurodegenerative diseases, associated with elevated apoptosis (29).
NSC-34 pre-treated with ESE did not express TLR4 and COX2 proteins, indicating that the anti-inflammatory and neuroprotective action of ESE may be mediated by the inhibition of TLR4 and COX2 pro-inflammatory pathways. TLR4 was shown to be involved in neuroinflammation in the brain, and has a role in neurodegenerative diseases, such as Alzheimer's disease, Parkinson's disease, amyotrophic lateral sclerosis and multiple sclerosis (30). Moreover, it was reported that COX2 expression may be triggered by pro-inflammatory cytokines such as IL-1β and TNF-α (31,32). Interestingly, the inhibition of TLR4 signaling has shown neuroprotective effects (33,34). Also COX2 inhibition has shown protective effects. Indeed, it was observed that the use of celecoxib, a COX2 inhibitor, showed neuroprotective effects in NSC-34 exposed to the supernatant of LPS-stimulated macrophages, inhibiting the release of pro-inflammatory mediators from activated macrophages (35). Furthermore, COX2 inhibition showed also protective action on neurons exposed to excitotoxic stimuli (36). ESE was shown to decrease COX2 gene expression level in a model of rat mammary gland carcinogenesis induced by 7,12 dimethylbenz(α)anthracene (DMBA), and to exert antioxidant, anti-inflammatory and anticancer activities (37). Moreover, other Brassicaceae extracts were able to inhibit COX2 expression (38).
Notably, the pre-treatment with ESE recovered the expression of IL-10, while the expression of the pro-inflammatory cytokine was abolished, indicating the capacity of ESE of counteracting inflammation, inhibiting the release of TNF-α. Furthermore, it was able to induce an anti-inflammatory and prosurvival response associated with IL-10 production. Interestingly, IL-10 is a potent anti-inflammatory cytokine that regulate host immune response (39). In the brain, other than its anti-inflammatory effect inhibiting the production of pro-inflammatory cytokines, IL-10 is able to mediate neurogenesis and exerts a prosurvival effect in neurons (40,41). Zhou et al (42) reported that IL-10 was able to exert prosurvival and neuroprotective actions on spinal cord neurons, protecting them against excitotoxicity in vitro.
Moreover, we observed the activation of the NLRP3 inflammasome in NSC-34 cells treated with the medium of LPS-treated RAW 264.7, associated with the presence of IL-18 and IL-1β. The NLRP3 inflammasome is the most studied. After inflammasome activation, pro-caspase 1 is cleaved to produce the active caspase 1, leading to the production of IL-18 and IL-1β, inducing pro-inflammatory responses, that have a role also in some nervous system disorders (16,17). It is known that the signaling mediated by TLR4, whose expression increased in LPS stimulated NSC-34, is necessary for the priming of the inflammasome, inducing the transcription of NLRP3 and pro-IL-1β, whose amounts during the resting state are not sufficient for inflammasome activation (16). However, ESE pre-treatment abolished the expression of NLRP3 inflammasome proteins and the production of IL-18 and IL-1β. Moreover, data reported that COX2, that in our model was expressed in LPS stimulated NSC-34, may act as a regulator of the NLRP3 inflammasome. Indeed, it was shown that COX2 was able to promote NLRP3 inflammasome activation in macrophages, regulating in this way the release of IL-1β, while the genetic knockdown or COX2 inhibition reduced the priming and the activation of NLRP3 inflammasome (43).
Interestingly, some natural compounds were reported to be able to regulate NLRP3 inflammasome, including GLSs and flavonoids (44,45). However, to our knowledge this is the first study demonstrating the ability of ESE to inhibit NLRP3 inflammasome activation. Given the involvement of inflammasome also in central nervous system disorders, it is possible to speculate that the abolition of inflammasome activation could be a good strategy to counteract neuroinflammation in nervous system pathologies.
All together, our data indicated that ESE was able to reduce inflammation, mediating in this way neuroprotective effects, protecting NSC-34 motor neurons from cell death. Notably, our results showing the anti-inflammatory properties of ESE are in line with other evidence showing the anti-inflammatory properties of other Brassicaceae extracts (38,46,47).
In conclusion, our results showed that ESE was able to induce anti-inflammatory and neuroprotective effects in NSC-34 motor neurons exposed to the culture medium of LPS-stimulated RAW 264.7 macrophages. In particular, it exerted these actions inhibiting COX2, TLR4, NLRP3 inflammasome pathways, and consequently limiting pro-inflammatory cytokines production and apoptosis. These results confirm the health promoting effects of Brassicaceae extracts and encourage their use as dietary supplement in the prevention/treatment of those pathological conditions where inflammation plays a pivotal role.
Acknowledgements
The study was supported by current research funds 2017 of IRCCS ‘Centro Neurolesi Bonino-Pulejo’, Messina, Italy.
Glossary
Abbreviations
- COX2
cyclooxygenase 2
- DMSO
Dimethyl sulfoxide
- ESE
Eruca sativa seed extract
- FasL
Fas Ligand
- FBS
fetal bovine serum
- GAPDH
Glyceraldehyde 3-phosphate dehydrogenase
- GLS
glucosinolate
- H2O2
hydrogen peroxide
- HRP
horse radish peroxidase
- IL
interleukin
- LPS
lipopolysaccharide
- NLR
NOD-like receptor
- NLRP3
NLR Family Pyrin Domain Containing 3
- NO
nitric oxide
- PBS
phosphate buffered saline
- TLR
Toll-like receptor
- TNF-α
tumor necrosis factor-α
References
- 1.Kalra EK. Nutraceutical-definition and introduction. AAPS Pharm Sci. 2003;5:E25. doi: 10.1208/ps050325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Björkman M, Klingen I, Birch AN, Bones AM, Bruce TJ, Johansen TJ, Meadow R, Mølmann J, Seljåsen R, Smart LE, Stewart D. Phytochemicals of Brassicaceae in plant protection and human health-influences of climate, environment and agronomic practice. Phytochemistry. 2011;72:538–556. doi: 10.1016/j.phytochem.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Cartea ME, Francisco M, Soengas P, Velasco P. Phenolic compounds in Brassica vegetables. Molecules. 2011;16:251–280. doi: 10.3390/molecules16010251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prakash D, Gupta C. Glucosinolates: The phytochemicals of nutraceutical importance. J Complement Integr Med. 2012;9:13. doi: 10.1515/1553-3840.1611. [DOI] [PubMed] [Google Scholar]
- 5.Bhandari SR, Jo JS, Lee JG. Comparison of glucosinolate profiles in different tissues of nine brassica crops. Molecules. 2015;20:15827–15841. doi: 10.3390/molecules200915827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khoobchandani M, Ganesh N, Gabbanini S, Valgimigli L, Srivastava MM. Phytochemical potential of Eruca sativa for inhibition of melanoma tumor growth. Fitoterapia. 2011;82:647–653. doi: 10.1016/j.fitote.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Khoobchandani M, Ojeswi BK, Ganesh N, Srivastava MM, Gabbanini S, Matera R, Iori R, Valgimigl L. Antimicrobial properties and analytical profile of traditional Eruca sativa seed oil: Comparison with various aerial and root plant extracts. Food Chem. 2010;120:217–224. doi: 10.1016/j.foodchem.2009.10.011. [DOI] [Google Scholar]
- 8.Fuentes E, Alarcon M, Fuentes M, Carrasco G, Palomo I. A novel role of Eruca sativa Mill. (rocket) extract: Antiplatelet (NF-κB inhibition) and antithrombotic activities. Nutrients. 2014;6:5839–5852. doi: 10.3390/nu6125839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarwar Alam M, Kaur G, Jabbar Z, Javed K, Athar M. Eruca sativa seeds possess antioxidant activity and exert a protective effect on mercuric chloride induced renal toxicity. Food Chem Toxicol. 2007;45:910–920. doi: 10.1016/j.fct.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 10.Bell L, Oruna-Concha MJ, Wagstaff C. Identification and quantification of glucosinolate and flavonol compounds in rocket salad (Eruca sativa, Eruca vesicaria and Diplotaxis tenuifolia) by LC-MS: Highlighting the potential for improving nutritional value of rocket crops. Food Chem. 2015;172:852–861. doi: 10.1016/j.foodchem.2014.09.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dinkova-Kostova AT, Kostov RV. Glucosinolates and isothiocyanates in health and disease. Trends Mol Med. 2012;18:337–347. doi: 10.1016/j.molmed.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Spencer JP, Vafeiadou K, Williams RJ, Vauzour D. Neuroinflammation: Modulation by flavonoids and mechanisms of action. Mol Aspects Med. 2012;33:83–97. doi: 10.1016/j.mam.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 13.Orhan IE, Daglia M, Nabavi SF, Loizzo MR, Sobarzo-Sánchez E, Nabavi SM. Flavonoids and dementia: An update. Curr Med Chem. 2015;22:1004–1015. doi: 10.2174/0929867322666141212122352. [DOI] [PubMed] [Google Scholar]
- 14.Kempuraj D, Thangavel R, Natteru PA, Selvakumar GP, Saeed D, Zahoor H, Zaheer S, Iyer SS, Zaheer A. Neuroinflammation induces neurodegeneration. J Neurol Neurosurg Spine. 2016;1 pii: 1003. [PMC free article] [PubMed] [Google Scholar]
- 15.Chen WW, Zhang X, Huang WJ. Role of neuroinflammation in neurodegenerative diseases (Review) Mol Med Rep. 2016;13:3391–3396. doi: 10.3892/mmr.2016.4948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.He Y, Hara H, Núñez G. Mechanism and regulation of NLRP3 inflammasome activation. Trends Biochem Sci. 2016;41:1012–1021. doi: 10.1016/j.tibs.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou K, Shi L, Wang Y, Chen S, Zhang J. Recent advances of the NLRP3 inflammasome in central nervous system disorders. J Immunol Res. 2016;2016:9238290. doi: 10.1155/2016/9238290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Virmani A, Pinto L, Binienda Z, Ali S. Food, nutrigenomics, and neurodegeneration-neuroprotection by what you eat! Mol Neurobiol. 2013;48:353–362. doi: 10.1007/s12035-013-8498-3. [DOI] [PubMed] [Google Scholar]
- 19.Wagner AE, Terschluesen AM, Rimbach G. Health promoting effects of brassica-derived phytochemicals: From chemopreventive and anti-inflammatory activities to epigenetic regulation. Oxid Med Cell Longev. 2013;2013:964539. doi: 10.1155/2013/964539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kapusta-Duch J, Kopeć A, Piatkowska E, Borczak B, Leszczyńska T. The beneficial effects of Brassica vegetables on human health. Rocz Panstw Zakl Hig. 2012;63:389–395. [PubMed] [Google Scholar]
- 21.Iori R, Bernardi R, Gueyrard D, Rollin P, Palmieri S. Formation of glucoraphanin by chemoselective oxidation of natural glucoerucin: A chemoenzymatic route to sulforaphane. Bioorg Med Chem Lett. 1999;9:1047–1048. doi: 10.1016/S0960-894X(99)00136-5. [DOI] [PubMed] [Google Scholar]
- 22.Barillari J, Canistro D, Paolini M, Ferroni F, Pedulli GF, Iori R, Valgimigli L. Direct antioxidant activity of purified glucoerucin, the dietary secondary metabolite contained in rocket (Eruca sativa Mill.) seeds and sprouts. J Agric Food Chem. 2005;53:2475–2482. doi: 10.1021/jf047945a. [DOI] [PubMed] [Google Scholar]
- 23.Pi J, Li T, Liu J, Su X, Wang R, Yang F, Bai H, Jin H, Cai J. Detection of lipopolysaccharide induced inflammatory responses in RAW264.7 macrophages using atomic force microscope. Micron. 2014;65:1–9. doi: 10.1016/j.micron.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 24.Xaus J, Comalada M, Valledor AF, Lloberas J, López-Soriano F, Argilés JM, Bogdan C, Celada A. LPS induces apoptosis in macrophages mostly through the autocrine production of TNF-alpha. Blood. 2000;95:3823–3831. [PubMed] [Google Scholar]
- 25.Ashe PC, Berry MD. Apoptotic signaling cascades. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27:199–214. doi: 10.1016/S0278-5846(03)00016-2. [DOI] [PubMed] [Google Scholar]
- 26.Tchernychev B, Furie B, Furie BC. Peritoneal macrophages express both P-selectin and PSGL-1. J Cell Biol. 2003;163:1145–1155. doi: 10.1083/jcb.200310079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McEver RP. Selectins: Initiators of leucocyte adhesion and signalling at the vascular wall. Cardiovasc Res. 2015;107:331–339. doi: 10.1093/cvr/cvv154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rossol M, Heine H, Meusch U, Quandt D, Klein C, Sweet MJ, Hauschildt S. LPS-induced cytokine production in human monocytes and macrophages. Crit Rev Immunol. 2011;31:379–446. doi: 10.1615/CritRevImmunol.v31.i5.20. [DOI] [PubMed] [Google Scholar]
- 29.Choi C, Benveniste EN. Fas ligand/Fas system in the brain: Regulator of immune and apoptotic responses. Brain Res Brain Res Rev. 2004;44:65–81. doi: 10.1016/j.brainresrev.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 30.Trotta T, Porro C, Calvello R, Panaro MA. Biological role of Toll-like receptor-4 in the brain. J Neuroimmunol. 2014;268:1–12. doi: 10.1016/j.jneuroim.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 31.Hoozemans JJ, Veerhuis R, Janssen I, Rozemuller AJ, Eikelenboom P. Interleukin-1beta induced cyclooxygenase 2 expression and prostaglandin E2 secretion by human neuroblastoma cells: Implications for Alzheimer's disease. Exp Gerontol. 2001;36:559–570. doi: 10.1016/S0531-5565(00)00226-6. [DOI] [PubMed] [Google Scholar]
- 32.Mark KS, Trickler WJ, Miller DW. Tumor necrosis factor-alpha induces cyclooxygenase-2 expression and prostaglandin release in brain microvessel endothelial cells. J Pharmacol Exp Ther. 2001;297:1051–1058. [PubMed] [Google Scholar]
- 33.Ulbrich F, Kaufmann K, Roesslein M, Wellner F, Auwärter V, Kempf J, Loop T, Buerkle H, Goebel U. Argon mediates anti-apoptotic signaling and neuroprotection via inhibition of Toll-like receptor 2 and 4. PLoS One. 2015;10:e0143887. doi: 10.1371/journal.pone.0143887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Paola M, Sestito SE, Mariani A, Memo C, Fanelli R, Freschi M, Bendotti C, Calabrese V, Peri F. Synthetic and natural small molecule TLR4 antagonists inhibit motoneuron death in cultures from ALS mouse model. Pharmacol Res. 2016;103:180–187. doi: 10.1016/j.phrs.2015.11.020. [DOI] [PubMed] [Google Scholar]
- 35.Huang Y, Liu J, Wang LZ, Zhang WY, Zhu XZ. Neuroprotective effects of cyclooxygenase-2 inhibitor celecoxib against toxicity of LPS-stimulated macrophages toward motor neurons. Acta Pharmacol Sin. 2005;26:952–958. doi: 10.1111/j.1745-7254.2005.00136.x. [DOI] [PubMed] [Google Scholar]
- 36.Strauss KI, Marini AM. Cyclooxygenase-2 inhibition protects cultured cerebellar granule neurons from glutamate-mediated cell death. J Neurotrauma. 2002;19:627–638. doi: 10.1089/089771502753754091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abdel-Rahman S, Shaban N, Haggag A, Awad D, Bassiouny A, Talaat I. Inhibition of NF-κB, Bcl-2 and COX-2 Gene expression by an extract of Eruca sativa seeds during rat mammary gland carcinogenesis. Asian Pac J Cancer Prev. 2015;16:8411–8418. doi: 10.7314/APJCP.2015.16.18.8411. [DOI] [PubMed] [Google Scholar]
- 38.Herz C, Tran HT, Márton MR, Maul R, Baldermann S, Schreiner M, Lamy E. Evaluation of an aqueous extract from horseradish root (Armoracia rusticana Radix) against lipopolysaccharide-induced cellular inflammation reaction. Evid Based Complement Alternat Med. 2017;2017:1950692. doi: 10.1155/2017/1950692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sabat R, Grütz G, Warszawska K, Kirsch S, Witte E, Wolk K, Geginat J. Biology of interleukin-10. Cytokine Growth Factor Rev. 2010;21:331–344. doi: 10.1016/j.cytogfr.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 40.Lobo-Silva D, Carriche GM, Castro AG, Roque S, Saraiva M. Balancing the immune response in the brain: IL-10 and its regulation. J Neuroinflammation. 2016;13:297. doi: 10.1186/s12974-016-0763-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pereira L, Font-Nieves M, Van den Haute C, Baekelandt V, Planas AM, Pozas E. IL-10 regulates adult neurogenesis by modulating ERK and STAT3 activity. Front Cell Neurosci. 2015;9:57. doi: 10.3389/fncel.2015.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhou Z, Peng X, Insolera R, Fink DJ, Mata M. Interleukin-10 provides direct trophic support to neurons. J Neurochem. 2009;110:1617–1627. doi: 10.1111/j.1471-4159.2009.06263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hua KF, Chou JC, Ka SM, Tasi YL, Chen A, Wu SH, Chiu HW, Wong WT, Wang YF, Tsai CL, et al. Cyclooxygenase-2 regulates NLRP3 inflammasome-derived IL-1β production. J Cell Physiol. 2015;230:863–874. doi: 10.1002/jcp.24815. [DOI] [PubMed] [Google Scholar]
- 44.Lee HW, Lee CG, Rhee DK, Um SH, Pyo S. Sinigrin inhibits production of inflammatory mediators by suppressing NF-κB/MAPK pathways or NLRP3 inflammasome activation in macrophages. Int Immunopharmacol. 2017;45:163–173. doi: 10.1016/j.intimp.2017.01.032. [DOI] [PubMed] [Google Scholar]
- 45.Tőzsér J, Benkő S. Natural compounds as regulators of NLRP3 inflammasome-mediated IL-1β production. Mediators Inflamm. 2016;2016:5460302. doi: 10.1155/2016/5460302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sadeghi H, Mostafazadeh M, Sadeghi H, Naderian M, Barmak MJ, Talebianpoor MS, Mehraban F. In vivo anti-inflammatory properties of aerial parts of Nasturtium officinale. Pharm Biol. 2014;52:169–174. doi: 10.3109/13880209.2013.821138. [DOI] [PubMed] [Google Scholar]
- 47.Kook SH, Choi KC, Lee YH, Cho HK, Lee JC. Raphanus sativus L. seeds prevent LPS-stimulated inflammatory response through negative regulation of the p38 MAPK-NF-κB pathway. Int Immunopharmacol. 2014;23:726–734. doi: 10.1016/j.intimp.2014.11.001. [DOI] [PubMed] [Google Scholar]