Abstract
Family conflict in adolescents with type 1 diabetes (T1D) has been linked to worse disease management (i.e. glycemic control, adherence to treatment regimen) and reduced quality of life. We sought to examine parental risk factors associated with increased levels of diabetes-specific family conflict and to investigate the discrepancies between parent and adolescent reports of conflict. Adolescents with T1D and their parents (N=120 dyads) completed measures of diabetes-specific family conflict. Adolescents also reported on health-related quality of life, and parents reported on demographic information. Clinical data were obtained from adolescents’ medical records. Adolescents reported significantly greater levels of conflict than their parents around direct diabetes management tasks (e.g. checking blood sugars) and indirect management tasks (e.g. carrying supplies for high or low blood sugars). Several demographic factors were associated with family conflict, including parental education, marital status, and household income. Discrepancies between parent and adolescent reports of family conflict were significantly associated with diabetes-related outcomes. Specifically, higher quality of life was related to discrepancies between parent and adolescent reports of conflict around indirect management tasks. In addition, poorer glycemic control was related to discrepancies between parent and adolescent reports of high family conflict around direct diabetes management tasks. These results support obtaining both the adolescent and parent report of conflict for unique information regarding family’s functioning.
Keywords: family conflict, type 1 diabetes, informant discrepancies, health-related quality of life, glycemic control
Type 1 diabetes (T1D) is one of the most prevalent childhood chronic health conditions, in which the pancreas fails to produce insulin, resulting in the dysregulation of blood glucose levels in the body. To maintain tight control over blood glucose levels, adolescents are directed to adhere to a complicated treatment regimen which includes monitoring blood glucose levels at least 4–5 times daily, and balancing insulin administration with diet, exercise, and daily activities. Failure to adhere to this regimen may lead to both acute illness and long-term health complications (e.g., eye, kidney, and heart disease; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group, 2000). Despite this knowledge, most youth with T1D struggle with adherence, and thus fall short of meeting the American Diabetes Association (ADA) recommendations for optimal glycemic control. Although managing T1D can be difficult at any age, adolescence presents unique challenges when trying to adhere to a complex treatment regimen. During this developmental stage, adolescents begin to take responsibility for many tasks previously completed by parents, and adolescents’ shift towards independence and the associated increase in responsibility for diabetes management is often associated with less optimal glycemic control, with only 17% of adolescents meet the ADA’s recommendation for glycemic control (Miller et al., 2015). Therefore, it is critical that we identify risk factors for poor adherence and glycemic control.
With the developmental transition toward increased independence, family dynamics can shift and become strained during adolescence, leading to stress, poor family functioning and increased conflict (Allison & Shultz, 2004). Parents of adolescents with T1D report increased levels of family conflict related to the demands of managing the disease and shifting responsibilities (Moore, Hackworth, Hamilton, Northam, & Cameron, 2013). This diabetes-related family conflict has been strongly and consistently linked to poorer glycemic control (Hilliard, Wu, Rausch, Dolan, & Hood, 2013; Williams, Laffel, & Hood, 2009) and poorer diabetes management (Drotar et al., 2013; Hilliard, Holmes, et al., 2013; Maliszewski, Patton, Midyett, & Clements, 2017). In addition to problems with physical health, higher levels of family conflict have been consistently shown to predict lower adolescent quality of life, even after controlling for demographic variables, duration of disease, and glycemic control (Weissberg-Benchell et al., 2009).
While diabetes-related family conflict has been consistently linked with poorer outcomes in youth with T1D, little research has identified whether conflict over particular aspects of the diabetes regimen separately account for these relationships. Direct management tasks are part of basic adherence to the treatment regimen, such as remembering to check blood sugars and administering the appropriate amount of insulin. Indirect management tasks refer to indirectly managing diabetes, such as remembering clinic appointments and carrying supplies to treat low and high blood sugars. One of the few studies to distinguish between these types of conflict determined that youth- and parent-reported conflict over direct management tasks was more strongly associated with poorer quality of life and poorer glycemic control than conflict over indirect tasks (Hood, Butler, Anderson, & Laffel, 2007). Another study found that conflict around direct management tasks (but not indirect tasks) mediated the relationship between negative caregiver affect around blood glucose monitoring and glycemic control (Gray, Dolan, & Hood, 2013). However, although both of these studies included multiple reporters (caregiver and child) of conflict, these reports were analyzed separately.
Given that diabetes-specific conflict has been established as a significant risk factor for poor quality of life and glycemic control in youth with T1D, further attention is needed to understand discrepancies between informants, to guide the efforts of providers and researchers who work with these families. Parents and adolescents frequently disagree in their reports of various behaviors, such as behavior problems and aspects of the family environment, and as noted by De Los Reyes and Kazdin (2005), these discrepancies in reports offer an opportunity for better understanding of the phenomenon, as well as points of intervention. Greater discrepancies in parent and child reports on family conflict predict increased symptoms of psychopathology in children over time (De Los Reyes, 2011), and discrepancies in perceptions of diabetes-specific family conflict have been linked with poorer diabetes outcomes. For example, Rybak and colleagues (2017) recently conducted latent profile analyses and found that incongruent reports of family conflict, particularly when parents reported higher levels of conflict than their adolescents, were linked with worse glycemic control and poorer health-related quality of life. However, while previous studies have examined the relationship between discrepancies between parent and child reports of diabetes-related family functioning, T1D researchers have not used the most recently recommended methods to examine discrepancies in parent and adolescent reports, polynomial regression analyses (e.g., Laird & De Los Reyes, 2013). For example, calculating difference scores between parent and adolescent reports (subtracting one informant’s score from the other’s) tests a directional difference, which assumes that the reports are orthogonal to each other, when in reality, they are often positively correlated (Laird & De Los Reyes, 2013). In contrast, regression analyses including interaction terms allow us to examine different patterns of discrepancies that cannot be tested with difference scores. For example, we can test whether glycemic control or quality of life is better when both parent and adolescent reports of conflict are low, or whether it is better when the parent reports low conflict, even if the adolescent reports high conflict (and vice versa). These analyses provide information above and beyond the individual informants’ reports of conflict and have important implications for assessment and interventions to address family conflict and improve outcomes in this high-risk population.
Current Study
The current study aimed to examine discrepancies between parent and adolescent reports of diabetes-related family conflict, related to both indirect and direct diabetes management, and to determine how these discrepancies related to quality of life and glycemic control in adolescents with T1D. Based on previous research (e.g., Laird & De Los Reyes, 2013; Nelemans et al., 2016), we hypothesized that greater congruence between parent and adolescent reports of low levels of conflict would be associated with better quality of life. In contrast, we hypothesized that higher adolescent reports of family conflict, relative to parent reports, would be associated with poorer glycemic control (e.g., Rybak et al., 2017). In addition, we explored whether family conflict related to indirect or direct management tasks was more strongly associated with quality of life or glycemic control.
Methods
Participants
Participants in the study included 120 adolescent-parent dyads, who agreed to be part of a larger positive psychology intervention (NCT02746627). Adolescents with T1D were approached at their regular diabetes clinic appointments at a large Southeastern academic medical center. Eligibility criteria for adolescents were (1) between the age of 13–17, (2) a diagnosis of T1D for at least 6 months to avoid disruptions related to initial diagnosis1, (3) no other major health problems, (4) no current participation in other intervention studies, and (5) an A1c value between 8.0–12.0% at the time of enrollment. Among the 183 adolescents that were approached, 63 (34%) declined to participate, most often citing lack of time and interest as the reason. There were no significant differences between participants and non-participants related to age, mean A1c, sex, or race/ethnicity.
Procedures
The study was approved by the university’s Institutional Review Board/Human Research Protection Program, with parents and adolescents providing consent or assent. Upon enrollment, researchers provided adolescents and one of their parents with tablets in clinic and they completed electronic questionnaires through a secure web application immediately before or after their clinic appointment (REDCap; Harris, et al., 2009). A1c values were obtained from a point-of-care assessment on their day of enrollment. Both parents and adolescents were compensated for their time.
Measures
Demographic variables
The parent who participated in the study provided demographic information such as age, income, race/ethnicity, marital status, and paternal and maternal education levels. Parents also reported adolescent sex, duration of diabetes, and treatment type (i.e. pump or injections).
Family conflict
Parents and adolescents each completed the Revised Diabetes Family Conflict Scale (Hood, Butler, Anderson, & Laffel, 2007), which assesses the extent parents and adolescents argue with one another about diabetes management tasks. This scale consists of 19 tasks rated from 1 (almost never argue) to 3 (almost always argue). Direct management tasks are part of basic adherence to the treatment regimen, such as remembering to check blood sugars and administering the appropriate amount of insulin. Indirect management tasks refer to indirectly managing diabetes through tasks that relate to direct care tasks, such as remembering clinic appointments and carrying supplies to treat low and high blood sugars. Items are summed for a total conflict score, and the direct and indirect items are summed for the subscale scores (scores range from 19–57 for total conflict, 10–30 for indirect conflict, and 9–27 for direct conflict). Higher scores indicate higher levels of family conflict. In our sample, the internal reliability for adolescent reports of direct and indirect conflict were high (Cronbach’s α = .93 and .95, respectively) and the internal reliability of the parent reports for direct and indirect conflict were adequate to high (Cronbach’s α = .89 and .90, respectively).
Health-related quality of life
Adolescents reported on their health-related quality of life using the Pediatric Quality of Life Inventory (PedsQL) 3.0 Diabetes Module (Varni, et al., 2003). This scale contains 28 items, which assesses problems associated with diabetes symptoms, treatment barriers, worry, and communication over the past month. The total scaled score ranges from 0–100, with higher scores indicating better quality of life. Internal consistency was .87 in our sample.
Glycemic control
A1c values were obtained from a point-of-care assessment on adolescents’ day of enrollment at their routine clinic visit. The A1c test provides the average level of blood glucose over the previous 3 months. Higher values indicate worse glycemic control, and the ADA recommends a target A1c of < 7.5% for adolescents with T1D (ADA, 2016). The A1c test was performed using a Bayer Diagnostics DCA2000® Analyzer.
Data analysis plan
Statistical analyses were performed using IBM SPSS Statistics 23. Overall, of the data collected, 4% was missing, and missing family conflict data for individual items were imputed using mean imputation. In our preliminary analyses, we conducted nonparametric tests to identify demographic risk factors related to diabetes-related family conflict, to account for equal distribution in the sample. To test our main aim, we examined discrepancies in parent and adolescent reports of family conflict with several steps. First, we conducted paired means t-tests to assess whether adolescents and parents reported different mean levels of direct and indirect conflict. Next, we calculated bivariate correlations to determine associations between parent and adolescent reports of conflict. Finally, in line with recommendations for testing whether informant discrepancies predict outcomes (Edwards et al., 2004; Laird & De Los Reyes, 2013), we conducted a series of polynomial regression analyses. Adolescents’ quality of life and glycemic control were each regressed on adolescent and parent reports of direct and indirect diabetes-related family conflict (both centered) and the two-way interaction between adolescent and parent reports. In addition, the models included quadratic terms of adolescent and parent-reported conflict. Finally, the models included a set of coefficients one order higher in magnitude, including cubed terms and quadratic interactions (Edwards, 1994). These terms were retained if they significantly improved the fit of the model. Post-hoc probing of significant interaction terms was conducted with simple slopes analyses at high (+1 SD) and low (−1 SD) levels of the moderators (Cohen, Cohen, West & Aiken, 2003) to show whether outcomes (quality of life and glycemic control) were better when informants disagreed regardless of informant levels, informants agreed regardless of informant levels, or whether the effect of disagreement or agreement differed as a function of informant levels.
Results
Preliminary Results
The adolescent sample was 52.5% female and the mean age was 14.84 years (SD = 1.46). Most adolescents identified as White, non-Hispanic (87.5%). About half used an insulin pump (50.8%) and the average duration of diabetes was 6.33 years (SD = 3.70). The mean A1c in our sample was 9.16% (SD = 0.90). The parental sample was 85% female and 15% male. The sample consisted of 97% biological parents and 3% other caregivers (e.g. grandparent, stepparent). The mean age of parents was 42.94 (SD = 5.91). Paternal educational attainment in our sample was 35.8% with high school education or less, 25.8% with some college, and 38.3% were college graduates. Maternal educational attainment in our sample was 16.7% with high school education or less, 37.5% with some college, and 45.8% were college graduates. The annual household income distribution in our sample was fairly balanced, with 26.7% reporting earning ≤$39,999, 37.5% earning $40,000–79,999, and 35.8% earning ≥$80,000. The majority of parents were married/partnered (90.8%) and identified as White, non-Hispanic (90.8%).
Preliminary Analyses
As seen in Table 1, several parental demographic factors were significantly associated with family conflict. Specifically, lower levels of paternal education were related to significantly higher levels of direct conflict reported by parents, and to significantly greater levels of indirect conflict reported by adolescents. Furthermore, maternal education was related to parent reports of both indirect and direct conflict. Household income and marital status were was significantly related only to parent-reported indirect conflict, such that parents in the lowest income category (<$40,000/year) reported higher levels of indirect conflict, married/partnered parents reported less indirect family conflict than single parents. There were no significant differences in family conflict for race/ethnicity.
Table 1.
Demographic Differences in Adolescent- and Parent-Reported Direct and Indirect Family Conflict
| Mean Rank | Mean Rank | Mean Rank | X2 | df | |
|---|---|---|---|---|---|
| Paternal Education | High school or less | Some college | College graduates | ||
| Parent-reported direct | 73.03 | 52.03 | 50.54 | 11.070** | 2 |
| Parent-reported indirect | 69.71 | 54.95 | 53.47 | 5.882 | 2 |
| Adolescent-reported direct | 64.33 | 54.36 | 55.53 | 2.082 | 2 |
| Adolescent-reported indirect | 70.65 | 51.79 | 56.88 | 6.174* | 2 |
| Maternal Education | High school or less | Some college | College graduates | ||
| Parent-reported direct | 70.88 | 63.00 | 50.65 | 6.485* | 2 |
| Parent-reported indirect | 70.53 | 64.48 | 51.36 | 6.338* | 2 |
| Adolescent-reported direct | 69.11 | 57.17 | 55.78 | 2.313 | 2 |
| Adolescent-reported indirect | 72.90 | 59.40 | 56.89 | 3.215 | 2 |
| Annual Household Income | <$40,000 | $40–80,000 | >$80,000 | ||
| Parent-reported direct | 69.66 | 56.81 | 52.71 | 4.608 | 2 |
| Parent-reported indirect | 73.11 | 51.80 | 57.07 | 7.795* | 2 |
| Adolescent-reported direct | 60.48 | 61.57 | 53.87 | 1.274 | 2 |
| Adolescent-reported indirect | 64.52 | 63.48 | 54.40 | 2.104 | 2 |
|
| |||||
| Mean Rank | Mean Rank | U | z | ||
|
| |||||
| Marital Status | Married | Single | |||
| Parent-reported direct | 55.06 | 68.35 | 994.50 | −1.87 | |
| Parent-reported indirect | 54.77 | 72.22 | 969.00 | −2.52* | |
| Adolescent-reported direct | 56.63 | 63.87 | 1129.00 | −1.02 | |
| Adolescent-reported indirect | 57.78 | 67.98 | 1168.50 | −1.43 | |
| Race | White | Non-White | |||
| Parent-reported direct | 58.01 | 63.65 | 478.50 | −.508 | |
| Parent-reported indirect | 59.32 | 61.23 | 569.50 | −.180 | |
| Adolescent-reported direct | 56.67 | 75.95 | 385.50 | −1.81 | |
| Adolescent-reported indirect | 59.39 | 71.45 | 479.00 | −1.10 | |
Note. Kruskal-Wallis tests were performed for paternal education, maternal education, and annual household income. Mann-Whitney tests were performed for marital status and race.
p<.05.
p<.01.
p<.001.
Discrepancies in Parent and Adolescent Reports of Diabetes-Related Family Conflict
To examine discrepancies in parent and adolescent report of family conflict, we conducted paired-sample t-tests, as described above. Adolescents reported significantly higher mean levels of conflict than parents for both direct diabetes-related tasks (t(111) = −3.22, p = .002, d = 0.31) and indirect diabetes-related tasks (t(117) = −6.23, p < .001, d = 0.58). The bivariate associations between parent and adolescent reports were moderate, but significant, for direct conflict (r = .27, p = .003) and indirect conflict (r = .25, p = .006), similar to other studies of parent and adolescent reports of child behavior problems and family functioning.
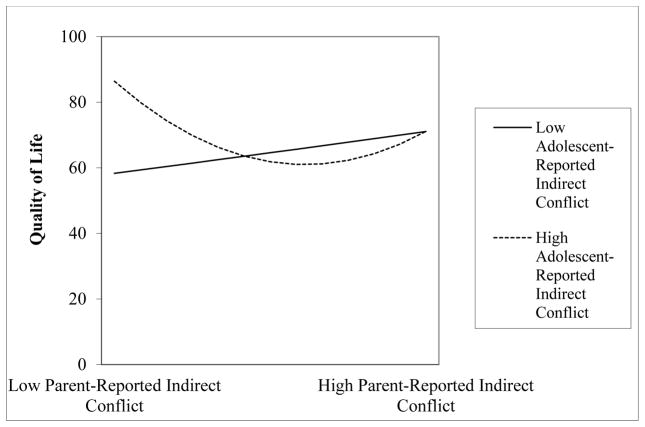
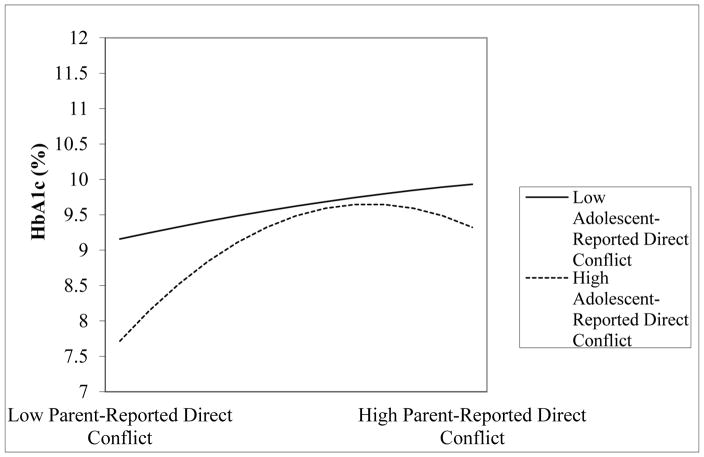
Table 2 presents the results of the polynomial regression models predicting diabetes-related quality of life and glycemic control from parent and adolescent reports of diabetes-related conflict. The interaction term for adolescent-reported indirect conflict and the quadratic effect of parent-reported indirect conflict predicting quality of life was significant (adolescent report x parent report squared) (β = 3.74, p = .003). As seen in Figure 1, the highest level of quality of life was associated with a discrepancy between low levels of parent-reported conflict and high levels of adolescent-reported conflict around indirect management tasks. In addition, the interaction term for adolescent-reported direct conflict with the quadratic effect of parent-reported direct conflict predicting glycemic control was significant (adolescent report x parent report squared) (β = -.20, p = .030). As seen in Figure 2, parent-reported conflict was more strongly associated with HbA1c at low levels of adolescent-reported conflict than at high levels of adolescent-reported conflict. These findings indicate that the discrepancy of high parent-reported direct conflict and low adolescent-reported conflict were associated with the poorer glycemic control.
Table 2.
Parent and Adolescent Reports of Diabetes-Related Conflict as Predictors of Diabetes-Related Outcomes
| Quality of Life | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Predictor | Direct Conflict | Indirect Conflict | ||||
| β | SE | p | β | SE | p | |
| Adolescent Report | −1.48 | 1.29 | .255 | −1.38 | 3.24 | .671 |
| Parent Report | −2.34 | 1.43 | .106 | −0.42 | 3.00 | .888 |
| Adolescent Squared | 2.82 | 1.52 | .065 | 6.86 | 2.68 | .012 |
| Adolescent X Parent | −0.94 | 1.23 | .446 | −4.66 | 2.45 | .060 |
| Parent Squared | −0.03 | 1.16 | .979 | 3.78 | 3.13 | .230 |
| Adolescent cubed | −4.22 | 2.49 | .093 | |||
| Parent X Adolescent Squared | −2.60 | 1.91 | .176 | |||
| Adolescent X Parent Squared | 3.74 | 1.23 | .003 | |||
| Parent Cubed | −0.87 | 1.17 | .461 | |||
| Model R2 | .11 | .027 | .21 | .002 | ||
|
| ||||||
| Glycemic Control | ||||||
|
| ||||||
| Predictor | Direct Conflict | Indirect Conflict | ||||
| β | SE | p | β | SE | p | |
| Adolescent Report | −0.07 | 0.23 | .764 | 0.19 | 0.10 | .063 |
| Parent Report | 0.40 | 0.22 | .068 | 0.18 | 0.16 | .289 |
| Adolescent Squared | −0.32 | 0.12 | .0067 | −0.34 | 0.14 | .016 |
| Adolescent X Parent | 0.14 | 0.11 | .198 | −0.01 | 0.08 | .929 |
| Parent Squared | −0.23 | 0.12 | .057 | −0.10 | 0.09 | .228 |
| Adolescent cubed | 0.23 | 0.13 | .070 | |||
| Parent X Adolescent Squared | −0.22 | 0.12 | .072 | |||
| Adolescent X Parent Squared | −0.20 | 0.09 | .030 | |||
| Parent Cubed | 0.07 | 0.09 | .406 | |||
| Model R2 | .18 | .001 | .04 | .075 | ||
Note. Higher order terms were only retained if they significantly improved model fit.
Figure 1.
Adolescent’s quality of life in relation to parent-reported indirect conflict at high (+1 SD) and low (−1 SD) levels of adolescent-reported indirect conflict.
Figure 2.
Adolescent’s HbA1c in relation to parent-reported direct conflict at high (+1 SD) and low (−1 SD) levels of adolescent-reported direct conflict.
Discussion
Our study draws attention to the links between diabetes-specific family conflict and outcomes in adolescents with T1D. The results from the current study indicated significant discrepancies between parent and adolescent reports of conflict on both direct and indirect tasks, and these discrepancies were related to quality of life (indirect conflict) and glycemic control (direct conflict). Using polynomial regression analyses to examine discrepancies between adolescent and parent-reports of diabetes-specific family conflict offers important information. Unlike difference scores, the use of interaction terms allows us to test whether discrepancies or congruence between adolescent and parent reports of family conflict are more strongly associated with diabetes-related outcomes.
First, we found statistically significant differences in parent and adolescent reports of conflict, with adolescents reporting significantly higher levels of all types of conflict, similar to findings by Rybak and colleagues (2017). The current study replicates and builds on these findings, revealing new information regarding differential effects of the types of diabetes-related conflict related to quality of life and glycemic control. Furthermore, informant discrepancies in diabetes-related family conflict accounted for significant differences in adolescents’ quality of life and glycemic control. Specifically, quality of life was highest when there was a discrepancy between parents’ and adolescents’ reports of indirect conflict, such that parents reported lower levels of conflict and adolescents reported higher levels of conflict. These findings were somewhat surprising, but may be due to adolescents perceiving discussions around indirect management (e.g., remembering to bring supplies) as less serious than conflict around direct management tasks. In contrast, discrepancies between parents’ and adolescents’ reports of conflict around direct management were associated with the poorest glycemic control, with the highest HbA1c related to low levels of adolescent-reported conflict and high levels of parent-reported conflict. These findings may reflect parents’ frustration around adolescents’ poor adherence to direct management tasks (e.g., checking blood glucose, administering insulin), which are likely to be related to poorer glycemic control.
Several limitations in the current study must be addressed. First, study participants agreed to be part of an intervention study and were targeted due to their poor glycemic control; therefore, these findings may not generalize to adolescents with better glycemic control. Additionally, this study uses a cross-sectional study design, which prohibits our ability to determine causality of the relationships. Furthermore, it may be useful to also incorporate other measures of family functioning (i.e. communication/problem-solving, parental monitoring) to recognize the basis of the conflicts and determine ways to improve diabetes management among adolescents. Lastly, our sample had a relatively small percentage of minority and single parent families, reflecting the clinic population.
Despite these limitations, the results of this study can inform recommendations for clinical practice and guide future research. Our findings highlight the relationship between discrepancies in perceptions of family conflict and diabetes outcomes, suggesting that it could be beneficial to adopt screening protocols to collect parent and adolescent reports of family functioning in regards to diabetes management. These data could inform recommendations regarding the transition to more independent care and target interventions toward those at an elevated risk of high family conflict and poor disease management. Future studies should also aim to investigate the effect of parental gender on perceptions of family conflict, as some studies have identified gender differences (Renk, Liljequist, Simpson, & Phares, 2005). In addition, although longitudinal studies are needed to understand the direction of effects, this study uniquely examines how discrepancies in parent and adolescent reports of diabetes-specific family conflict around direct and indirect management tasks relate to diabetes-realted outcomes in distinct ways. Researchers and clinicians may reach different conclusions, depending on who reports on family conflict. Further, these findings indicate that examining the discrepancies between parent and adolescent reports adds to our understanding above and beyond individual reports of family conflict. Thus, a greater understanding of how best to assess conflict may be an important step toward improving diabetes outcomes in this high-risk population.
Acknowledgments
This work was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (DP3DK097678). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of NIH. This study is registered with ClinicalTrials.gov (NCT02746627). A portion of the ideas and results of the study were presented at the 37th Annual Meeting and Scientific Sessions of the Society of Behavioral Medicine, Washington, D.C.
Footnotes
Only one participant had been diagnosed less than 12 months.
References
- Allison BN, Schultz JB. Parent-adolescent conflict in early adolescence. Adolescence. 2004;39:101. [PubMed] [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes - 2016. Diabetes Care. 2016;39:S1–S106. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied Multiple Correlation/regression Analysis for the Behavioral Sciences. UK: Taylor & Francis; 2003. [Google Scholar]
- De Los Reyes A. Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2011;40:1–9. doi: 10.1080/15374416.2011.533405. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. New England Journal of Medicine. 2000;2000:381–389. doi: 10.1056/NEJM200002103420603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drotar D, Ittenbach R, Rohan JM, Gupta R, Pendley JS, Delamater A. Diabetes management and glycemic control in youth with type 1 diabetes: Test of a predictive model. Journal of Behavioral Medicine. 2013;36:234–245. doi: 10.1007/s10865-012-9426-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards JR. The study of congruence in organizational behavior research: Critique and a proposed alternative. Organizational Behavior & Human Decision Processes. 1994;58:51–100. [Google Scholar]
- Gray WN, Dolan LM, Hood KK. Impact of blood glucose monitoring affect on family conflict and glycemic control in adolescents with type 1 diabetes. Diabetes Research & Clinical Practice. 2013;99:130–135. doi: 10.1016/j.diabres.2011.12.020. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard ME, Holmes CS, Chen R, Maher K, Robinson E, Streisand R. Disentangling the roles of parental monitoring and family conflict in adolescents’ management of type 1 diabetes. Health Psychology. 2013;32:388–396. doi: 10.1037/a0027811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard ME, Wu YP, Rausch J, Dolan LM, Hood KK. Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. Journal of Adolescent Health. 2013;52:28–34. doi: 10.1016/j.jadohealth.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood K, Butler D, Anderson B, Laffel L. Updated and revised diabetes family conflict scale. Diabetes Care. 2007;30:1764–1769. doi: 10.2337/dc06-2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird RD, De Los Reyes A. Testing informant discrepancies as predictors of early adolescent psychopathology: Why difference scores cannot tell you what you want to know and how polynomial regression may. Journal of Abnormal Child Psychology. 2013;41:1–14. doi: 10.1007/s10802-012-9659-y. [DOI] [PubMed] [Google Scholar]
- Maliszewski G, Patton SR, Midyett LK, Clements MA. The interactive effect of diabetes family conflict and depression on insulin bolusing behaviors for youth. Journal of Diabetes Science and Technology. 2017;11:493–498. doi: 10.1177/1932296816664363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KM, Foster NC, Beck RW, Bergenstal RM, DuBose SN, DiMeglio LA, … Tamborlane WV. Current state of type 1 diabetes treatment in the US: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015;38:971–978. doi: 10.2337/dc15-0078. [DOI] [PubMed] [Google Scholar]
- Moore SM, Hackworth NJ, Hamilton VE, Northam EP, Cameron FJ. Adolescents with Type 1 Diabetes: parental perceptions of child health and family functioning and their relationship to adolescent metabolic control. Health & Quality of Life Outcomes. 2013;11:50. doi: 10.1186/1477-7525-11-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelemans SA, Branje SJT, Hale WW, Goossens L, Koot HM, Oldehinkel AJ, Meeus WHJ. Discrepancies between perceptions of the parent–adolescent relationship and early adolescent depressive symptoms: An illustration of polynomial regression analysis. Journal of Youth & Adolescence. 2016;45:2049–2063. doi: 10.1007/s10964-016-0503-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renk K, Liljequist L, Simpson JE, Phares V. Gender and age differences in the topics of parent-adolescent conflict. The Family Journal. 2005;13:139–149. [Google Scholar]
- Rybak TM, Ali JS, Berlin KS, Klages KL, Banks GG, Kamody RC, … Diaz-Thomas AM. Patterns of family functioning and diabetes-specific conflict in relation to glycemic control and health-related quality of life among youth with type 1 diabetes. Journal of Pediatric Psychology. 2017;42:40–51. doi: 10.1093/jpepsy/jsw071. [DOI] [PubMed] [Google Scholar]
- Varni JW, Burwinkle TM, Jacobs JR, Gottschalk M, Kaufman F, Jones KL. The PedsQL™ in type 1 and type 2 diabetes reliability and validity of the pediatric quality of life inventory™ generic core scales and type 1 diabetes module. Diabetes Care. 2003;26:631–637. doi: 10.2337/diacare.26.3.631. [DOI] [PubMed] [Google Scholar]
- Weissberg-Benchell J, Nansel T, Holmbeck G, Chen R, Anderson B, Wysocki T, Laffel L. Generic and diabetes-specific parent-child behaviors and quality of life among youth with type 1 diabetes. Journal of Pediatric Psychology. 2009;34:977–988. doi: 10.1093/jpepsy/jsp003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LB, Laffel LM, Hood KK. Diabetes-specific family conflict and psychological distress in paediatric Type 1 diabetes. Diabetic Medicine. 2009;26:908–914. doi: 10.1111/j.1464-5491.2009.02794.x. [DOI] [PMC free article] [PubMed] [Google Scholar]