Abstract.
Community-led total sanitation (CLTS) is a common method for promoting sanitation in low-income settings. This cluster-randomized trial evaluated an intervention to improve inclusion of people with disability in CLTS through training facilitators. A qualitative study examined intervention acceptability. The trial included 171 people with disabilities (78 control and 93 intervention) living in 15 intervention and 15 control communities. In the intervention arm, respondents were more likely to participate in a community meeting about sanitation (+18.7%, 95% confidence interval [CI]: 3.2, 34.2) and to have been visited to discuss sanitation (+19.7, 95% CI: 0.6, 37.8). More intervention households improved latrine access for the disabled member (+9%, CI: −3.1, 21.0). Inclusive CLTS could improve sanitation access for people with disability but requires support to households beyond that provided in this trial.
INTRODUCTION
An estimated one billion people worldwide live with a disability, of whom around 80% are in low-income countries.1 People with disabilities are often poor2 and face a range of barriers to full participation in society.1 Access to safe sanitation is believed to be problematic for people with disabilities3 as they face additional barriers to those faced by most of the estimated 2.4 billion people who lack adequate sanitation.4 However, quantitative data are lacking.
Improving access to sanitation for poor households remains a challenge. Ensuring that people with disabilities are not left behind in this process requires changes to sanitation hardware as well as program implementation and content (software). Community-led total sanitation (CLTS) is a community mobilization approach designed to facilitate rapid uptake of basic, low-cost household sanitation. Inclusive CLTS aims to ensure that no sectors of the population are systematically excluded from this process. Inclusion of people with disabilities entails raising community awareness about the problems they face in accessing sanitation, disseminating information about low-cost adaptations to overcome physical barriers to sanitation access, and action by implementers to try to ensure that people with disabilities are able to participate in decision-making. There is a growing body of literature documenting efforts to address the sanitation needs of people with disabilities.5–7 However, trials have not been undertaken to assess the effectiveness of these interventions among people with disabilities.
To achieve significant impact, sanitation solutions for people with disabilities need to be deliverable at scale for little additional cost. This study aimed to evaluate whether a 3-day introductory training on inclusion would be effective in bringing about changes in sanitation access for people with disabilities by changing the way CLTS was delivered. Such an intervention would have potential for rapid scale through existing CLTS training and delivery structures with additional costs only relating to the initial training.
METHODS
Study site.
The study was conducted in rural and peri-urban areas of Rumphi district in northern Malawi.
Study design.
A mix of quantitative and qualitative methods was used in a consecutive manner to assess the impact of the intervention. First, the intervention was evaluated quantitatively using a cluster-randomized trial. This was followed by a qualitative component comprising in-depth interviews with people with disabilities and their caregivers in both study arms. The rationale for using a mixed-method approach in this study was to assess not just whether the intervention would work but also, through the qualitative work, describe the experiences of people with disabilities in relation to the intervention and identify factors which enabled or prevented improvements to sanitation access.
Four traditional authorities (TAs, an administrative unit) were purposively selected from the 10 TAs within Rumphi district. Three of these TAs had not previously received CLTS and the fourth CLTS had been implemented in very few communities. A fifth TA which had previously received no CLTS was excluded on logistical grounds as too remote to allow fieldwork with the time and resources available. Thirty group village headmen (GVHs) were selected randomly from across these TAs (GVHs are administrative units comprising clusters of villages and are the unit of intervention for CLTS in the district). Four villages were randomly selected from within each GVH for data collection. Following baseline data collection, 15 GVHs were randomly allocated to the intervention arm and 15 to the control arm. The intervention arm received a CLTS intervention delivered by facilitators who had attended a rapid training for inclusive implementation of CLTS (described in detail in the later paragraphs). The control arm received standard CLTS delivered by facilitators who had not attended this training.
The intended primary outcome measure was the difference, postintervention, between intervention and control arms, in the proportion of people with disabilities who accessed a poorer level of sanitation than other members of their household. Sanitation level was defined using Joint Monitoring Program for Water Supply and Sanitation (JMP) definitions of no access, unimproved sanitation, and improved sanitation.8 However, the baseline survey showed few people with disabilities used a different place for defecation than other household members. Therefore, the primary outcome was changed to the proportion of households that made changes to their latrine in the preceding 12 months, with the aim of facilitating access for the person with disabilities. Secondary outcomes included the reported desire to make changes to the latrine and inclusion/participation in elements of the intervention by people with disabilities.
Sampling process.
Quantitative methods.
We aimed to detect a 20% difference in the proportion of households that had made changes to the latrine or built a new one in the last 12 months. In the absence of field-data, we assumed, conservatively, that in the control arm, 30% of households with a person with disabilities would make changes to an existing latrine or build a new one. The intervention was assumed to increase this figure to 50%. A sample of 103 households with a person with disabilities per study arm would be sufficient to detect a 20% difference in the primary outcome variable between intervention and control arms at the 0.05 confidence level with 80% power. We assumed a GVH-level intracluster correlation coefficient of 0.05, necessitating a sample size of 175 households with a person with disabilities per arm, with the expectation of including 14 people with disabilities per GVH. The required number of GVHs was thus 13 per arm. We included 15 GVHs per arm to allow for loss to follow-up.
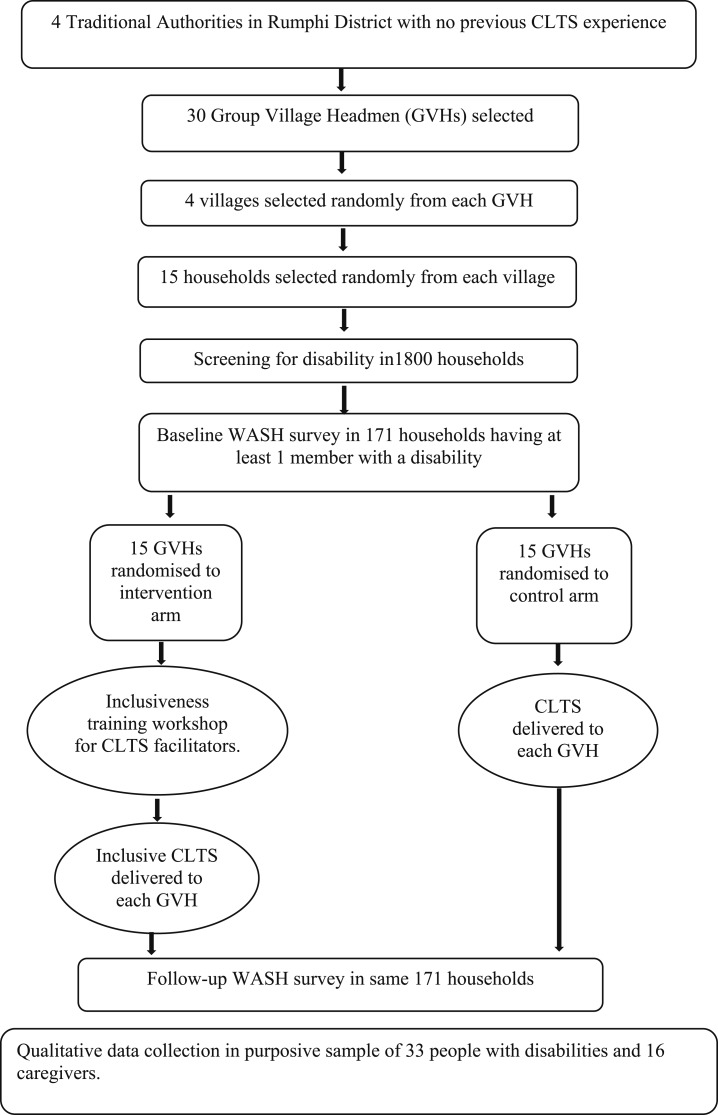
We assumed a prevalence of disability conservatively at 5% based on previous studies and the 2008 Population and Housing Census of Malawi.9 We assumed a mean household size of five persons. To achieve a sample of 175 persons with disabilities per arm, it was, therefore, necessary to screen a minimum of 1,759 households. We screened 15 households per village across four villages per GVH across 15 GVH per arm, making 1,800 households screened at baseline. A flow chart of the study design and sampling strategy is presented in Figure 1.
Figure 1.
Flow diagram of the trial process.
Qualitative methods.
Respondents were primarily drawn from the quantitative sampling frame and were purposively selected across all TAs to include people with a range of age, gender, and impairment types. The following factors were considered when selecting participants: the level of difficulty an individual experienced when accessing WASH facilities at baseline and whether they had made changes to their WASH facilities at follow-up. Additional individuals were included from households found to have made a change to their sanitation. These households were identified through village leaders, health surveillance assistants or community-based rehabilitation workers.
Data collection methods.
Quantitative methods.
Fifteen households were selected from each village through a random walk procedure. At baseline, a screening questionnaire comprising the Washington Group Extended Set of Questions on Functioning10 was administered to a household respondent (the primary female caregiver, where possible, or head of household) to identify those having at least one member with disabilities. Having a disability was defined as reporting or being reported to have a lot of difficulty with or being unable to perform any of the core domains of activity (seeing, hearing, mobility, cognition, self-care, communicating, and upper body movement). Individuals less than 2 years of age were excluded.
In households where a person with disabilities was identified, a verbally administered questionnaire was used to collect basic social, demographic, and economic data and to assess sanitation access both for the household and for the individual member(s) with a disability. The household respondent reported on the usual place of defecation for household members. Respondents with a disability reported on their own practices, including whether they used the same place for defecation as other household members and, if not, what their usual place of defecation was. If a person with disabilities was unable to understand and/or respond to verbal questions, either because of their disability or because they were too young, the primary caregiver responded on their behalf. A spot-check observation was used to record presence and quality (improved/unimproved) of a household latrine.
Follow-up data on sanitation access were collected from the same households, by similar means, approximately 6 months after the delivery of the intervention. The follow-up questionnaire also assessed attendance at the CLTS triggering event and occurrence of follow-up visits (see Intervention section and Table 2 for descriptions of the CLTS process) to the household and included questions and confirmatory spot-check observation to assess whether any changes had been made to improve sanitation access and/or whether changes were desired.
Table 2.
Modified community-led total sanitation (CLTS) implementation plan developed by facilitators following inclusiveness training
| Standard CLTS plan | Modified, inclusive CLTS plan | |
|---|---|---|
| Pre-triggering | Meet with the village leader to arrange community meeting. | Specifically request that people with disabilities and elderly people should attend. |
| Determine location for the meeting. | The location should be in a place that is easy to access and is as close to where people with disabilities live as possible. | |
| Community members are expected to find their own way to the meeting. | People with disabilities to be assisted to come to the meeting if needed. | |
| Triggering | People are free to sit or stand wherever they like during the community event. | Invite people with disabilities to sit at the front. |
| Participatory mapping of community. | Map to include symbols for households with family members with disabilities. | |
| Community map which households have toilets. | Map to also indicate toilets, water points and handwashing facilities that are accessible for people with disabilities. | |
| “Squatting demonstration” activity to illustrate the problems some people with disabilities may have using a standard latrine | ||
| Provide basic information on construction of latrines and handwash stations. | Provide additional information on making facilities more accessible for people with disabilities (e.g., support rails, strings for guidance, seats). | |
| Establish WASH committee to oversee implementation of community WASH plan. | Include people with disabilities on the WASH committee. | |
| Follow-up | Community make plan to improve sanitation and end open defecation. | Encourage construction of more accessible toilets. |
| Facilitators make follow-up visits to monitor progress and provide support to WASH committee. | Visits to include targeting people with disabilities in their homes and conducting accessibility audits with them. | |
| Facilitators track toilet construction. | Facilitators track accessibility by asking “can everyone in the family use the toilet/hand washing facility?” |
Data were collected by 14 enumerators (13 at follow-up) who received training at baseline and follow-up. The same enumerators collected data in both the intervention and control arms. Three enumerators left after the baseline and were replaced by two new enumerators at follow-up.
Qualitative methods.
Qualitative data were collected at follow-up and in the intervention arm only from 28 respondents. The qualitative interview guides are available online: ehg.lshtm.ac.uk/wash-disability. All respondents also completed a demonstration whereby they enacted their routine means of accessing and using sanitation and handwashing facilities. Qualitative data were collected by a team of four researchers, all of whom had conducted WASH and disability-related qualitative research in the past. The research team included one representative of the Federation of Disability Organizations in Malawi, who was also a person with disabilities. Qualitative data were collected at the same time as the quantitative data.
Consent.
Participation was on the basis of informed, written consent. Guardians/caregivers provided consent for individuals under 18 or with severe intellectual impairments.
Intervention.
Delivery of CLTS activities in both arms of the trial was overseen and implemented by a nongovernmental organization, the Church of Central Africa Presbyterian, Synod of Livingstonia Development Department (CCAP-SOLDEV). Implementation was carried out in partnership with village-level health surveillance assistants (employees of the government of Malawi).
Standard CLTS (control arm).
The CLTS process has been described in detail elsewhere.11 GVHs in the control arm received CLTS delivered by trained facilitators. In each community, there was a pair of facilitators, one from CCAP-SOLDEV and one a village health worker. CLTS delivery followed the guidelines set out in the Government’s Open Defecation Free (ODF) Malawi Strategy.12 This comprised the following steps:
-
1.
A pre-triggering meeting with the village head to obtain permission and support for a community meeting.
-
2.
A community meeting (“triggering event”) to raise awareness of the problem of open defecation through participatory methods such as community mapping of latrines and open defecation sites, and to mobilize the community to address their sanitation problems by facilitating the development of an action plan and identifying champions to take it forward.
-
3.
A series of at least five follow-up visits made by the facilitators to the community to provide support and monitor progress toward the elimination of open defecation. Support visits could include visits to individual households as well as meetings with groups of key and/or active individuals.
Triggering events took place during April 2015. Follow-up visits started approximately 2 weeks after the community-level triggering and continued over a period of up to approximately 6 months or until ODF was defined as no human feces evident in the environment, all households either have a latrine or share a latrine, all latrines provide privacy, all latrines have drop-hole covers, and all latrines have a handwashing place. The metric does not specifically consider people with disabilities who may not open defecate but may be unable to access the same sanitation facility as other household members. The last follow-up visits took place during October 2015.
Inclusive CLTS (intervention arm).
CLTS in the intervention arm was delivered by a different group of facilitator pairs. During April 2015, before implementation in the intervention arm, these facilitators attended a 3-day training workshop on inclusive WASH led by one of the authors (H.J.) and informed by a CLTS inclusivity guide.13 The aim of the workshop was to raise awareness about disability and its impact on an individual’s WASH access and participation in communal activities, as well as about potential mitigation in terms of hardware (e.g., ramps or guide rails to ease access) and software. Software included training on the inclusion of people with a disability in the CLTS process as well as tools to encourage community-level discussion and raise awareness in relation to the needs of people with a disability. The content of the workshop is summarized in Table 1. More details of the training are provided in Jones et al.14 At the end of the workshop, participants produced a plan of actions intended to make CLTS more inclusive of people with disabilities. A comparison of the components of standard and inclusive CLTS is given in Table 2.
Table 1.
Summary of inclusiveness training
| Day | Activity |
|---|---|
| Day 1: context setting | Classroom-based, facilitated discussions and activities, including a “squatting activity”14,17 highlighting that different users have different needs and that consultation with users is crucial when designing facilities. |
| Purpose: share experience of problems accessing water, sanitation and hygiene and identify possible solutions to improve access. | |
| Day 2: household visits | An adapted form of the Accessibility and Safety Audit18 was introduced and practiced by participants during visits to households with people with disabilities. |
| Purpose: allow facilitators to learn about sanitation and hygiene challenges first-hand from people with disabilities and train facilitators on participatory approaches to generate solutions. | |
| Day 3: action planning | Small groups discussed local case studies and a role-play provided practice in making community mapping as inclusive as possible. Finally, participants produced a community-led total sanitation (CLTS)+ action plan, drawing on their learning. This outlined what health surveillance assistants would do differently to make the CLTS process more inclusive. |
| Purpose: to understand how standard CLTS is delivered and encourage the facilitators to generate ideas about how it could be made more inclusive. |
Triggering for the intervention arm was conducted during June 2015. Follow-up visits started approximately 2 weeks later and continued for a period of up to approximately 6 months or until ODF status was reached. The last follow-up visits took place during December 2015.
Data management and analysis.
Statistical analysis.
Binary outcome variables were analyzed by two different model approaches. If no baseline value for a particular outcome variable was available (e.g., attendance at a community-triggering event), we used additive binomial regression models to calculate prevalence differences between the intervention and control arm (distribution family: binomial, link function: identity). For outcomes with available baseline values, we calculated the difference between the value at follow-up and at baseline (change score) for each arm. The change scores were then compared across arms using linear regression (family: Gaussian, link: identity). For both types of model, we used generalized estimating equations with robust standard errors to account for clustering at the level of GVH. One outcome variable (time needed to reach latrine) was measured in categories of < 5, 5–10, 11–15, 16–30, and > 30 minutes. We used interval regression to compare this outcome across trial arms at follow-up. For this model, clustering at the GVH level was accounted for by using robust standard errors. All analyses were done in Stata 12.0 (Stata Corp., College Station, TX).
Qualitative analysis.
Interviews were audio recorded, translated, and transcribed and then thematically analyzed by the one of the authors (S.W.). Data were anonymized and categorized by respondent gender, age, geographical location, impairment type, and study arm. Coding was done through a deductive, “top-down” analysis15 based on the study objectives. This included coding of responses by exposure to the intervention (including awareness, attendance, and participation) and perceptions of change (physical and social). Analysis followed a six-step process,16 allowing emergent themes to be identified across the entire dataset and refined. Quotes were selected to illustrate themes.
Integration of quantitative and qualitative components.
Although the quantitative and qualitative research teams worked closely during data collection, the methods were integrated only at the point of analysis. A preliminary analysis of the two datasets was done separately and then findings were compared and contrasted through meetings between the authors. In particular, the qualitative data was used to elucidate any unusual patterns or results that emerged from the quantitative data.
Ethics.
This study received ethical approval from the London School of Hygiene & Tropical Medicine and the Republic of Malawi National Committee of Research in the Social Sciences and Humanities.
RESULTS
Quantitative.
The prevalence of disability was found to be 2.6% (95% confidence interval [CI]: 2.4–2.8). These results are discussed elsewhere (Mactaggart et al., unpublished data). The trial included 171 people with disabilities (78 control versus 93 intervention, living in 70 versus 89 households) surveyed at baseline and follow-up. Overall, differences across arms in baseline characteristics were small, and the arms were well balanced (Table 3). However, there were marked imbalances in baseline values for two outcome variables in particular: household access to an improved latrine (more common in the control arm), and water availability near the latrine (more common in the intervention arm). These are shown in Table 5. On average, there were more people with disabilities per GVH in the intervention arm than the control arm.
Table 3.
Baseline characteristics of control and intervention arm clusters
| Control (N = 70) | Intervention (N = 89) | |
|---|---|---|
| Cluster characteristics | ||
| households with person with disabilities per cluster (mean, SD) | 5.2 (2.4) | 6.6 (3.0) |
| Household characteristics | ||
| Ethnic group | ||
| Tumbuka, % | 94.9 | 91.4 |
| Other, % | 5.1 | 8.6 |
| Religion | ||
| Catholic, % | 26.9 | 30.1 |
| CCAP, % | 35.9 | 26.9 |
| Other Christian, % | 30.7 | 33.3 |
| Other, % | 6.4 | 9.7 |
| Main source of income | ||
| Agriculture, % | 71.8 | 65.9 |
| Small trade, % | 9.0 | 9.9 |
| Casual labor, % | 6.4 | 6.6 |
| Other, % | 12.8 | 17.6 |
| Monthly income | ||
| < 5,000, % | 37.7 | 36.6 |
| 5,000–< 10,000, % | 26.0 | 29.0 |
| ≥ 10,000, % | 36.4 | 34.4 |
| Household WASH characteristics | ||
| Main drinking water source | ||
| Piped into compound, % | 6.4 | 3.2 |
| Piped water from neighbor, % | 1.3 | 3.2 |
| Public tap/standpipe, % | 6.4 | 14.0 |
| Tubewell/borehole, % | 75.6 | 72.0 |
| Protected well, % | 1.3 | 1.1 |
| Unprotected well/spring, % | 2.6 | 3.2 |
| Surface water, % | 6.4 | 3.2 |
| Sanitation access | ||
| Pit latrine with slab, % | 29.5 | 18.5 |
| Pit latrine without slab, % | 60.3 | 67.4 |
| Use the neighbor's facility, % | 6.4 | 9.8 |
| Other, % | 3.9 | 1.1 |
| No facility, open defecation, % | 0.0 | 3.3 |
| Handwashing place | ||
| Present, % | 9.0 | 11.8 |
| With water available, % | 3.9 | 7.5 |
| With soap available, % | 0.0 | 4.3 |
Table 5.
Effect of the intervention on study outcomes
| Control % (N = 78) | Intervention % (N = 93) | Crude difference (%) | 95% CI* | Adjusted difference (%)† | 95% CI* | |
|---|---|---|---|---|---|---|
| HH built new latrine or changed existing latrine in the last 12 months | 46.2 | 44.6 | 0.2 | −19.5 to 19.1 | – | – |
| Household access to improved latrine | ||||||
| Baseline | 29.5 | 19.6 | −10.1 | – | – | – |
| Follow-up | 20.5 | 14.0 | −6.5 | −18.6 to 5.6 | 4.6 | −12.3 to 21.6 |
| Sanitation at baseline | ||||||
| Private pit latrine with slab | 29.5 | 19.6 | – | – | – | – |
| Private pit latrine without slab | 60.3 | 67.4 | – | – | – | – |
| Uses neighbors latrine | 10.3 | 10.9 | – | – | – | – |
| Open defecation | 0.0 | 2.2 | – | – | – | – |
| Sanitation at follow-up | ||||||
| Private pit latrine with slab | 20.5 | 14.1 | – | – | – | – |
| Private pit latrine without slab | 66.7 | 77.2 | – | – | – | – |
| Uses neighbors latrine | 12.8 | 7.6 | – | – | – | – |
| Open defecation | 0.0 | 1.1 | – | – | – | – |
| Time to travel to latrine (minutes) | ||||||
| Baseline | 5.7 (5.5) | 5.1 (4.2) | −0.6 | – | – | – |
| Follow-up | 4.3 (2.8) | 4.0 (2.7) | −0.3 | −1.2 to 0.6 | −0.2 | −1.1 to 0.7 |
| Able to use latrine as often as required | ||||||
| Baseline | 92.3 | 93.5 | 1.2 | – | – | – |
| Follow-up | 92.2 | 93.4 | 1.3 | −7.6 to 10.2 | −1.1 | −9.7 to 7.4 |
| Able to use latrine without assistance | ||||||
| Baseline | 92.3 | 91.2 | 0.9 | – | – | – |
| Follow-up | 89.7 | 91.4 | 1.2 | −6.1 to 8.5 | 4.8 | −1.0 to 10.5 |
| Water available near latrine for handwashing | ||||||
| Baseline | 3.9 | 12.1 | 8.2 | – | – | – |
| Follow-up | 42.3 | 58.7 | 16.1 | −4.3 to 36.1 | 11.1 | −11.9 to 34.3 |
| Able to use latrine without coming into contact with feces | ||||||
| Baseline | 82.1 | 89.0 | 6.9 | – | – | – |
| Follow-up | 87.2 | 88.2 | −0.2 | −9.0 to 8.6 | −4.0 | −17.1 to 9.2 |
| Household made changes to latrine to improve access for person with disability | 23.1 | 29.0 | 5.7 | −9.5 to 20.9 | – | – |
| Latrine access is reported to be easier following changes | 16.7 | 25.8 | 9.0 | −3.1 to 21.0 | – | – |
| Wants changes to latrine | ||||||
| Baseline | 68.0 | 71.0 | 3.0 | – | – | – |
| Follow-up | 61.5 | 55.9 | −5.5 | −22.8 to 11.8 | −7.5 | −32.1 to 17.2 |
CI = confidence interval.
95% CI adjusted for cluster at group village headmen level.
Adjusted for baseline differences using change scores.
The characteristics of the enrolled people with disabilities are shown in Table 4. There were slightly more children under 10 years and females with disabilities in the intervention arm. Walking difficulties were more common in the intervention arm, whereas difficulties in understanding, being understood, and in learning were more common in the control arm. Other disability-related characteristics were well balanced across arms.
Table 4.
Characteristics of people with disabilities
| Control arm N = 78 | Intervention arm N = 93 | |
|---|---|---|
| Age (years) | ||
| < 10, % | 6.4 | 15.1 |
| 10–< 20, % | 18.0 | 11.8 |
| 20–< 70, % | 42.3 | 41.9 |
| ≥ 70, % | 33.3 | 31.2 |
| Female, % | 44.9 | 52.7 |
| Functioning | ||
| Needs glasses or contact lenses | 4.1 | 8.3 |
| Difficulty seeing | ||
| A lot, % | 26.8 | 27.8 |
| Cannot do at all, % | 4.2 | 5.6 |
| Difficulty hearing | ||
| A lot, % | 20.6 | 15.8 |
| Cannot do at all, % | 2.7 | 4.2 |
| Needs assistance for moving around, % | 12.8 | 14.0 |
| Uses cane or stick, % | 18.0 | 18.3 |
| Uses crutches, % | 1.3 | 1.1 |
| Uses artificial limb, % | 1.3 | 1.1 |
| Uses wheelchair, % | 2.6 | 3.2 |
| Participants ≥ 18 years | N = 59 | N = 69 |
| Uses sign language | 1.8 | 6.9 |
| Difficulty communicating | ||
| A lot, % | 9.1 | 11.0 |
| Cannot do at all, % | 0.0 | 1.4 |
| Difficulty remembering or concentrating | ||
| A lot, % | 7.3 | 15.1 |
| Cannot do at all, % | 0.0 | 0.0 |
| Difficulty with self-care | ||
| A lot, % | 9.1 | 8.2 |
| Cannot do at all, % | 1.8 | 2.7 |
| Difficulty raising a 2 L bottle of water | ||
| A lot, % | 7.3 | 6.9 |
| Cannot do at all, % | 1.8 | 0.0 |
| Difficulty using fingers and hands | ||
| A lot, % | 5.4 | 2.7 |
| Cannot do at all, % | 1.8 | 0.0 |
| Participants < 18 years | N = 19 | N = 24 |
| Difficulty walking compared with children of similar age | ||
| A lot, % | 10.5 | 16.7 |
| Cannot do at all, % | 5.3 | 16.7 |
| Difficulty with self-care | ||
| A lot, % | 10.5 | 13.6 |
| Cannot do at all, % | 10.5 | 4.6 |
| Difficulty understanding what others say | ||
| A lot, % | 42.1 | 26.1 |
| Cannot do at all, % | 10.5 | 17.4 |
| Difficulty being understood by others | ||
| A lot, % | 42.1 | 21.7 |
| Cannot do at all, % | 0.0 | 8.7 |
| Difficulty learning new things | ||
| A lot, % | 36.8 | 21.7 |
| Cannot do at all, % | 5.26 | 4.4 |
| Difficulty remembering | ||
| A lot, % | 26.3 | 8.7 |
| Cannot do at all, % | 10.5 | 8.7 |
Table 5 shows the effect of the intervention on the study outcomes. Baseline values are shown where available. More households in the intervention arm made changes to the latrine to make access easier for the people with disabilities (primary outcome), but the confidence intervals were wide and included null.
Household access to improved sanitation decreased in both arms during follow-up, but more in the control arm. We believe this was due to changes over time in the way in which enumerators applied the somewhat subjective JMP sanitation definitions. In the intervention arm compared with the control, there was a decrease in people with disabilities wanting further changes to the latrine (crude effect −5.5%, after accounting for baseline imbalance −7.5%). Again this difference was marked by a wide confidence interval that included null. There was little effect of the intervention on the other outcomes (i.e., time it takes to travel to the latrine, ability to use the latrine as often as required, ability to use the latrine without assistance, and ability to use the latrine without coming into contact with feces).
The results suggest that the CLTS activities reached more households which included members with disabilities in the intervention arm than the control arm. Compared with the control arm, more households in the intervention arm were aware that a sanitation meeting took place, attended the meeting, were visited by program staff to discuss sanitation, and were invited to learn more about how to make latrine access easier or participate in program activities. This difference between the intervention and control arm was evident whether the respondent was a person with disabilities or another household member. These results are shown in Table 6.
Table 6.
Intervention reach
| Control % (N = 70 for HH respondent, N = 78 for disabled) | Intervention % (N = 89 for HH respondent, N = 93 for disabled) | Difference (%) | 95% CI | |
|---|---|---|---|---|
| Aware that sanitation meeting took place | ||||
| Household respondent | 76.9 | 89.3 | 12.2 | 0.0 to 24.4 |
| Household member with disability | 73.1 | 83.9 | 10.2 | −4.6 to 25.0 |
| Meeting attendance | ||||
| Household respondent | 46.2 | 61.3 | 15.3 | 0.1 to 31.3 |
| Household member with disability | 37.2 | 55.9 | 18.7 | 3.2 to 34.2 |
| Was visited to discuss sanitation | ||||
| Household respondent | 51.3 | 72.0 | 19.9 | 3.9 to 36.0 |
| Household member with disability | 48.7 | 69.9 | 19.2 | 0.6 to 37.8 |
| Was visited to discuss how to make latrine access easier | ||||
| Household respondent | 18.0 | 43.0 | 26.1 | 13.7 to 38.6 |
| Household member with disability | 15.4 | 36.6 | 21.6 | 9.5 to 33.7 |
| Was invited to participate in program activities | ||||
| Household respondent | 30.8 | 49.5 | 18.4 | 2.6 to 34.2 |
| Household member with disability | 25.6 | 41.9 | 15.9 | −0.2 to 32.1 |
CI = confidence interval.
Qualitative.
In-depth interviews and demonstrations were conducted with 28 people in the intervention arm. Ten interviews involved only the respondent with a disability as these individuals accessed sanitation independently. Thirteen interviews involved both the person with disabilities and their caregiver as these caregivers were involved in supporting sanitation access to some degree. The remaining five interviews only involved the caregivers because of severe communication limitations of the person with disabilities. During interviews, the intervention process was explored, from the point of being invited to a triggering event through to implementing sanitation change.
Respondents with disabilities reported that being invited to attend the triggering meeting was unusual as they were usually excluded from community events:
“That was the only time I have attended a community meeting… people don’t even bother to tell me about the meetings to save me from the trouble of getting to the venue.” (Man, visual and physical impairment, 57)
“When there are … other meetings … my friends get invited and I don’t.” (Man, physical impairment, 26)
“It was unusual and interesting because I don’t get invited to meetings because of mobility challenges.” (Man, physical impairment, 43)
However, being invited to the triggering event did not always lead to attendance. The main reasons for non-attendance were that the meeting venue was too far away or too difficult to reach:
“I couldn’t … go on my own because I can’t see but if someone were there to direct me I would have.” (Woman, visual and hearing impairments, 73)
“If there was transportation available I would take them [her two children with disabilities] but otherwise I am weak and I can’t support them to travel long distances.” (Caregiver of a woman with a cognitive impairment, 45 and a man with physical and cognitive impairments, 28)
Respondents reported that community meetings were always called in the same location and that no change had been made for the triggering events.
Among those who had attended, few respondents had asked questions at the meeting or shared their experiences. One mother explained:
“I had something to say about my daughter’s conditions but I didn’t speak up. There were too many people and questions.” (Caregiver of a girl with physical and cognitive impairment, 13)
Those who did ask questions were mainly concerned about whether they would receive assistance (financial or through labor).
It transpired that community meetings are only normally attended by one member of a household, who then shares the information with the others. Thus, when people with disabilities were specially invited, they often attended in place of another family member. This was found to reduce the perceived likelihood of change being made at a household level:
“I would like it if [my family] could make changes for me. But I haven’t sat down with my son to discuss about it … He didn’t go to the meeting. Maybe if he had gone things would have happened more quickly.” (Woman, physical impairment, 59)
During triggering events, mapping households of people with disabilities as well as accessible water and sanitation points was not always done, but was considered acceptable and not discriminatory when it did happen:
“They said we should put stones on the households with people with disabilities including my son and other people. It was good because they explained that sanitation issues are important to children and people with disabilities.” (Caregiver of a boy, 8, with epilepsy)
In practice, the “squatting activity” rarely involved people with disabilities. It was the facilitators who demonstrated what squatting was like for people who are visually or physically impaired. However, this too appeared to be well accepted by people with disabilities attending the meeting:
“It didn’t offend me at all to see someone pretending to be disabled. Rather, I felt like the person was being supportive because it was like he was in our shoes.” (Man, physical impairment, 43)
Another respondent reported that even though he did not say anything during the meeting, the squatting demonstration led to him having discussions with some of his friends later about the challenges he faces.
The intervention was intended to provide information about different low-cost modifications for how to make toilets more accessible. However, in practice the only ideas shared by facilitators were raised seats and guide ropes/poles. It was also the intention that facilitators would actively include people with disabilities on the WASH committees that were being established. Only one person with disabilities was appointed to a committee, but several respondents said that they would have liked to have a position on the WASH committee, had they been asked.
When doing follow-up visits, there was evidence that facilitators had specifically sought out households where there was a person with disability. However, the formal process of conducting an “accessibility audit” was, in practice, replaced with a less structured discussion. Consequently, people with disabilities perceived the follow-up visits to be about educating them rather than a consultative process to generate appropriate adaptions for their needs:
“We didn’t have a discussion it was just a short chat, less than 15 minutes, to enlighten us on what we needed to do. He didn’t ask anything, he just suggested that we should make changes to the toilet including a raised seat.” (Woman, physical impairment, 22)
“They didn’t discuss about the challenges that my grandmother meets they just started telling us what we should do to build a toilet for her.” (Caregiver of a woman with physical impairment, 84)
Many participants with disabilities were not actively involved in the discussion during the follow-up visits, as intended. Instead, facilitators mainly talked to other family members:
“[The facilitator] mostly finds me asleep when he visits so he talks to my wife… He once found me sitting outside but he still talked to my wife” (Man, visual and physical impairment, 57)
“They spoke to me instead of my father and they asked me about the challenges he faces…It was harder for him to communicate with them so that’s why they let him relax and talked to me instead.” (caregiver of a man with visual and physical impairment, 75)
One of the reported barriers to change was the perceived cost. Respondents estimated that the changes they wanted to make would cost them between 5,000 Malawian Kwacha (MWK) (£5.60) and 50,000 MWK (£56.06). This expense was seen as either impossible or a longer term project:
“It will be difficult to find the money I think it will take us up to a year to get that much.” (Caregiver of a woman with physical impairment, 84)
“I don’t know how much the construction would cost… but I think I wouldn’t be able to afford it because the cost of caring for my daughter is already higher than others.” (Caregiver of a girl with cognitive and physical impairment, 13).
“I wish I had the toilet of my dreams but I know won’t be able to do that because of financial problems” (Man, physical impairment, 43)
By contrast, most of the people who had made changes to their facilities said that these changes cost nothing as they were made from local materials and constructed by family members or neighbors in less than a day. Those who did spend money on adaptations spent between 1,500 MWK (£1.68) and 8,000 MWK (£8.96) and said that it was a worthwhile investment given the benefit it had had for the household member with a disability:
“It was not much. We saw how difficult it was for him to access the toilet with his sight problems and the seat makes it more accessible” (Caregiver of a man with visual and physical impairment, 75)
“Considering we are assisting our daughter it was a worthwhile investment.” (Caregiver of a woman with physical impairment, 22)
The other main factor that prevented some participants from making changes was the physical inability to independently build a toilet or adaptive technology. This often resulted in inaction because of having to rely on family or community members:
“Who is going to build it for me? … They said they are going to build it for me but they haven’t done it yet. They say they are busy with farming first.” (Woman with physical impairment, 80)
“I also thought about making changes but the person who was supposed to make the change attended a funeral away from this village.” (Man with, physical impairment, 26)
“I am currently just reflecting on the changes we need to do to the latrine because my husband passed away and I’m unable to manage doing it alone.” (Caregiver of a woman with cognitive impairment, 18)
Many respondents mentioned longer term plans for change:
“I decided to start working on the toilet straight after the meeting, within the same week…But it will take time.” (Caregiver of a woman with physical impairment, 84)
Because the facilitators reduced the thoroughness of the consultations during the follow-up visits and predominantly promoted a limited range of adaptive technologies (raised seats and guiding poles), people with more complex needs found that the intervention was less relevant to them and as such were less likely to have made change.
“I had thought about making changes but what they told us was not suitable to my daughter’s condition because she defecates on herself. I was expecting more information on how to take care of my daughter because here at home we don’t have many options. But when they came the advice they taught us was the same as at the meeting - about … moulding the floor so that there is a seat … None of this was useful because with [my daughter’s] condition, she can’t sit and support herself.” (Caregiver of a girl with physical and cognitive impairments, 13)
“The discussions were relevant but they just weren’t relevant to my son, his situation’s different.” (Caregiver of a boy with physical and cognitive impairments, 8)
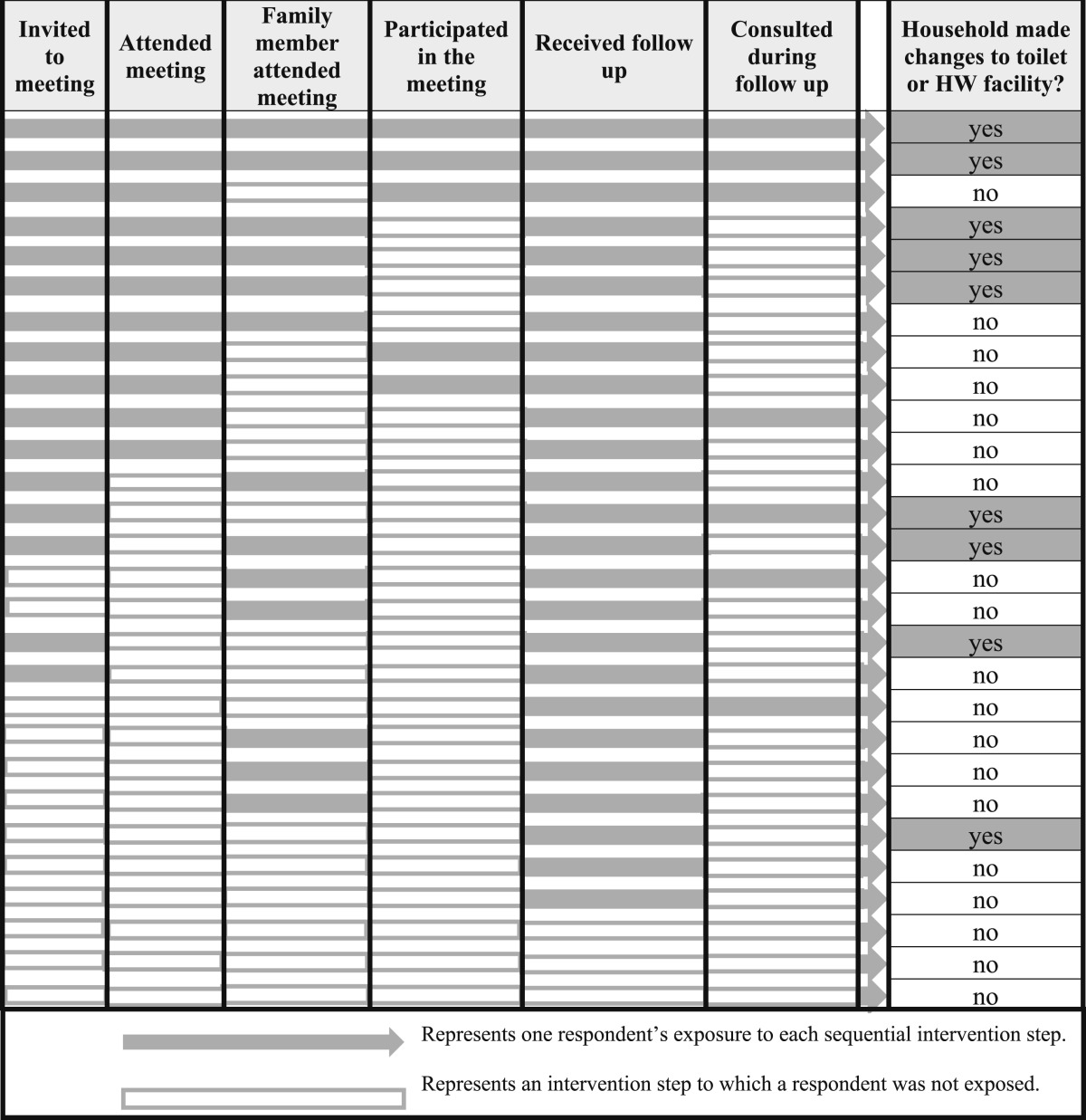
Intervention exposure.
Table 7 summarizes qualitative data obtained through interviews with the 28 respondents in the intervention arm. It describes their exposure to each of the sequential steps of the intervention and the association with observed changes to household sanitation. The results from this small, non-random sample must be interpreted with caution and cannot be used to infer causality. However, the results suggest that the more components of the intervention the participant was exposed to, the more likely it was that changes would be made. Concordant with the quantitative data, it suggests that receiving an invitation to the meeting was associated with attendance. It also suggests that the follow-up visits were the most effective component for reaching people with disabilities in the community and that in some cases, exposure to this alone was sufficient to enable change. However, it indicates that the intervention struggled to achieve full participation from people with disabilities, both in the triggering events and the follow-up. It appears that people with disabilities who attended the triggering event with another family member were more likely to see changes made to their household sanitation.
Table 7.
Respondent exposure to each sequential step of the intervention (based on qualitative interviews with 28 participants in the community-led total sanitation + intervention arm)
DISCUSSION
Our study provides further support to those who argue the need for improved WASH among people with disabilities3,4 as evidenced by the proportion of our respondents who were unable to use a latrine without risk of fecal contact and the proportion who wish to see changes made to their latrine (Table 5). Our results suggest that the training provided to CLTS facilitators resulted in them planning a more inclusive intervention. Our data indicate a trend toward greater reach of the intervention among people with disabilities and their households as a result of the more inclusive approach. Actual change to sanitation facilities was rare and our study was underpowered to detect these differences.
Our qualitative data support the finding that inclusive CLTS approaches promote a higher degree of participation of people with disabilities in WASH activities. However, the findings also suggest that plans for more inclusive implementation developed by the facilitators following training were only partially implemented. It may be that if additional support were provided following initial training, it could help CLTS facilitators put their learning into action and build their confidence and skills in communicating and consulting appropriately with people with disabilities.
Even with additional support, there may be elements of the CLTS process that, for good reasons, may not be easily amenable to change. For example, the location of community meetings may be determined by various factors including availability of space, shade, and seating; etiquette; and custom. These factors, along with the likely dispersal of households with members with disabilities, may mean that moving the meeting site to improve accessibility entails greater planning and forethought than was assumed during training. It was also apparent that people with disabilities rarely attended any community meetings. As such, it may be ambitious and even inappropriate to expect them to participate fully in what may be their first, or one of their first ever, public meetings. Inclusion of people with disabilities in the community-based, volunteer WASH committees (responsible for encouraging and monitoring sanitation uptake at community level) may require more awareness raising and knowledge about the contribution that people with disabilities can make. This is particularly the case as a common principal activity of these committees is to undertake regular house-to-house inspections which may be difficult for people with mobility or sensory impairments.
Actually achieving change to make household sanitation more accessible for people with disabilities presented a number of problems. Facilitators and people with disabilities were often not familiar with the variety of low-cost modifications that have been proposed, and consultation with people with disabilities tended to be brief and somewhat superficial. In these circumstances, there was little by way of collaborative creation of individual solutions. Rather facilitators tended to fall back on promoting two options, raised seats for people with physical impairments, and guide poles/rope for people with visual impairments. Where they were confronted with an individual with a more complex need or a different type of impairment, they often did not take time to discuss the situation and were unable to identify appropriate solutions.
Jones and Wilbur6 present a compilation of information on low-cost technologies. Hard and soft copies of this compendium were provided to the implementing agency as a resource to be made available to CLTS facilitators. However, after completion of the training, this did not happen. In any case, as a model for scale-up provision of this volume in its current format to every CLTS facilitator would not be sustainable and there is a need to explore alternatives. The growing availability of digital media may provide an opportunity for this.
It is also likely that making changes to household sanitation for people with disabilities require additional time and support and may require some additional costs. The follow-up period of this study may have been too short to capture the full extent of change. The findings suggest that it would be helpful to encourage people with disabilities to attend the triggering meeting along with another member of their household and also highlight the potential importance of household visits by the facilitators as a means to encourage change.
Our study was limited by the much smaller sample size achieved compared with what we had planned because of the unexpectedly low prevalence of disability. Furthermore, the CLTS activities in intervention and control arm triggered 2 months apart, which in a randomized trial is not an ideal scenario. Responses of study participants may have been subject to responder bias. Enumerators were not informed of the intervention status of communities, but may have deduced this from responses to their direct questions on intervention exposure. There were also important strengths, including the cluster-randomized design, complementary qualitative data collection, and the use of standardized tools to measure disability and WASH access.
CONCLUSIONS
Inclusive CLTS has potential to improve sanitation access for people with a disability and increase their involvement in the process. However, in many households achieving change may require additional information and support (beyond that provided in the current trial) to overcome barriers such as financial costs (actual or perceived), technical abilities, and access to labor as well as to strengthen the ability of people with a disability to advocate for the changes they desire. Facilitators may also need additional, initial support in the field if they are to put into practice effectively the ideas generated and learned through rapid inclusiveness training. The training itself, comprising 3 days, is probably too resource intensive to be applied at scale and there is a need to identify critical elements of this that could be included within the standard training provided to CLTS facilitators (in Malawi this is provided more than 4–5 days for groups of up to 25 facilitators and includes 2–3 days classroom-based and 2 days of field training.). The potential of inclusive CLTS is also constrained by the existing, low-cost hardware modifications as these are not able to mitigate the effects of all impairment types. This mixed methods study demonstrates the value of qualitative data in contributing to our understanding of how and why particular outcomes were achieved. Nevertheless, the lack of conclusive quantitative results remains a weakness. This came about, in part, because of unexpected issues with the sample size and also because of the nature of the indicators used. Future quantitative studies might benefit from the use of indicators that are able to capture more nuanced data on the quality of sanitation and the experience of use than those used in the present study.
Acknowledgments:
The CLTS intervention was delivered by CCAP-SOLDEV. Qualitative data were collected by Lizzie Shaba, Sembe Banda, and Overstone Kondowe and we would also like to thank the team of enumerators involved in the quantitative data collection. Much of the preparatory work was carried out by our colleague and friend James Milner who lost his life in the course of this study. He is greatly missed. This research has been funded by Australian Aid (Australian Government Department of Foreign Affairs and Trade) through the Australian Development Research Awards Scheme under an award entitled “Disability and its impact on safe hygiene and sanitation.” The views expressed in this publication are those of the authors and not necessarily those of the Commonwealth of Australia. The Commonwealth of Australia accepts no responsibility for any loss, damage, or injury resulting from reliance on any of the information or views contained in this publication.
REFERENCES
- 1.World Health Organization , 2011. World Bank. World Report on Disability. Geneva, Switzerland: WHO. [Google Scholar]
- 2.Banks L, Polack S, 2013. The Economic Costs of Exclusion and Gains of Inclusion of People with Disabilities: Evidence from Low and Middle Income Countries. London, United Kingdom: CBM. [Google Scholar]
- 3.Groce N, Bailey N, Lang R, Trani JF, Kett M, 2011. Water and sanitation issues for persons with disabilities in low- and middle-income countries: a literature review and discussion of implications for global health and international development. J Water Health 9: 617–627. [DOI] [PubMed] [Google Scholar]
- 4.White S, Kuper H, Itimu-Phiri A, Holm R, Biran A, 2016. A qualitative study of barriers to accessing water, sanitation and hygiene for disabled people in Malawi. PLoS One 11: e0155043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Danquah L, 2014. Undoing Inequity: Inclusive Water, Sanitation and Hygiene Programmes that Deliver for All in Uganda. Full Mid-Term Review Report. London, United Kingdom: WaterAid. [Google Scholar]
- 6.Jones H, Wilbur J, 2014. Compendium of Accessible WASH Technologies. London, United Kingdom: WEDC, SHARE, WaterAid. [Google Scholar]
- 7.Norman WR, 2010. Water, Sanitation and Disability in Rural West Africa: Enhancing Access and Use of WASH Facilities. Mechanicsburg, PA: Messiah College. [Google Scholar]
- 8.JMP , 2014. Progress on Drinking Water and Sanitation–2014 Update: WHO and UNICEF. Geneva, Switzerland: WHO.
- 9.Munthali A, 2011. Situation Analysis of PWDs in Malawi. Zomba, Malawi: Center for Social Research, University of Malawi.
- 10.Washington Group on Disability Statistics , 2011. Washington Group—Extended Question Set on Functioning. Luxembourg, Europe: CDC. [Google Scholar]
- 11.Kar K, Chambers R, 2008. Handbook on Community-Led Total Sanitation. London, United Kingdom: Plan International and Institute of Development Studies. [Google Scholar]
- 12.The Government of Malawi, 2011. Open Defecation Free Malawi Strategy 2011–2015. Lilongwe, Malawi: Ministry of Agriculture, Irrigation and Water Development.
- 13.Wilbur J, Jones H, 2014. Frontiers of CLTS Issue 3: Disability-making CLTS Fully Inclusive—Community-Led Total Sanitation. Brighton, United Kingdom: Institute of Development Studies.
- 14.Jones H, Singini W, Holm R, White S, 2016. CLTS Plus: Making CLTS Ever More Inclusive. 39th WEDC International Conference, July 11–15, 2016, Kumasi, Ghana. [Google Scholar]
- 15.Hayes N, 1997. Theory-led thematic analysis: social identification in small companies. Hayes N, ed. Doing Qualitative Analysis in Psychology. Hove, United Kingdom: Psychology Press. [Google Scholar]
- 16.Braun V, Clarke V, 2006. Using thematic analysis in psychology. Qual Res Psychol 3: 77–101. [Google Scholar]
- 17.Jones H, 2012. Designing a Pit Latrine Slab. Loughborough, United Kingdom: WEDC and WaterAid. [Google Scholar]
- 18.WEDC , 2012. Accessibility Audit of Water & Sanitation Facilities. Loughborough, United Kingdom: Loughborough University. [Google Scholar]