Abstract.
Despite the high burden of rotavirus diarrhea, uptake of rotavirus vaccines in Asia remains low. This primarily stems from a perception of rotavirus as a non-life-threatening pathogen amidst a background of competing health priorities and limited resources. In the largest pediatric hospital of Bangladesh, where there is a fierce competition for beds, we found that between November 2015 and October 2016, 12% of 23,064 admissions were due to gastrointestinal infections, 54% of which were caused by rotavirus. One in four cases requiring hospitalization, or 5,879 cases, was refused because of unavailability of beds. Most refused cases were of pneumonia (22%), severe perinatal asphyxia (17%), preterm birth complications (7%), and meningitis (2%), all of which bear high risks of death or disability, if not treated timely. When determining vaccine policies and conducting vaccine impact studies, it would be shortsighted to not consider the impact on morbidity and mortality of cases that are refused admission because of the hospitalization of children with a preventable disease as rotavirus diarrhea. In our hospital, routine use of a rotavirus vaccine with 41% efficacy will release 629 beds per year to accommodate previously refused cases. Based on evidence, we make the case that introduction of this vaccine in Bangladesh and the surrounding region will prevent morbidity and mortality, both directly and indirectly, and help us ensure survival and well-being of all children.
INTRODUCTION
Rotavirus is estimated to cause 111 million episodes of diarrhea that lead to 200,000 deaths every year, most of which occur in low- and middle-income countries (LMICs).1 The high disease burden led the World Health Organization (WHO) to recommend global use of rotavirus vaccine in 2009, specifically in countries with high mortality from childhood diarrhea.2 Two Gavi-funded vaccines have been introduced in 92 countries and have had major impact on rotavirus deaths and hospitalization.3 However, uptake of the vaccines in Asia remains low and the reasons likely vary by country.4 The lag in Bangladesh, despite being Gavi-eligible for the vaccine, is primarily due to the decline in mortality rates associated with rotavirus diarrhea seen in hospitals.5 In this article, we discuss how such direct estimates can mask indirect effects that a rotavirus vaccine can have on childhood mortality by reducing the competition for hospital beds and saving resources. Using data and experience from the largest pediatric hospital in Bangladesh, we argue that the introduction of a rotavirus vaccine will not only reduce morbidity because of diarrhea, but also morbidity and mortality due to other communicable and non-communicable diseases by increasing access to healthcare.
THE FIERCE COMPETITION FOR HOSPITAL BEDS IS EXACERBATED BY ROTAVIRUS
The hesitation of policy-makers to introduce this vaccine in countries such as Bangladesh primarily stems from a perception of rotavirus as a non-life-threatening pathogen amidst a background of competing health priorities and limited resources. Given the considerable reduction in diarrhea-related mortality in recent years, this may be understandable. We recently showed that 97% of rotavirus diarrhea cases are discharged within 48 hours.6 Based on such data, vaccines against pneumonia and meningitis have rightly been prioritized. However, looking past mortality figures, rotavirus diarrhea is one of the predominant causes of hospitalization in developing countries such as Bangladesh.6,7 Furthermore, mortality rate for a child experiencing moderate to severe diarrhea is eight times higher in the 2 months after hospitalization due to the diarrheal episode.8 Although the actual numbers remain unknown, mortality is likely to be even higher for cases that are not treated or receive delayed/suboptimal care.
In resource-poor, densely populated countries such as Bangladesh, competition for beds in public children’s hospitals is fierce. According to the 2009 World Health Statistics, there are only three beds per 10,000 population in comparison with that of 31 in the United States.9 Sick children requiring immediate hospitalization are often refused admission because of unavailability of beds. There are no specific referral systems in place, and with no tracking of patients turned back, there are no data on the impact of such refusals. It is very likely that refused cases have the most adverse outcomes due to the lack of or delayed appropriate care. Thus, any disease, regardless of mortality figures, that has a large footprint on hospital-bed usage will exacerbate treatment and outcome of other diseases in the context of limited beds.
In LMICs, meningitis, pneumonia, preterm birth, birth asphyxia, and neonatal sepsis are common causes of death and disability, especially when they are not treated immediately. In South Asia, of about 1.9 million deaths of children under 5 years of age, meningitis, sepsis, and pneumonia are responsible for over 25% of them and preterm-birth complications for another 25%.10 Considering the life-threatening risks of these diseases, several vaccines are recommended by the WHO and, consequently, have been introduced in LMICs. Introduction of Haemophilus influenza type B (Hib) vaccine in 2009 dramatically reduced the burden of diseases caused by Hib to near-elimination.11 Pneumococcal conjugate vaccines have been introduced in many developing countries to fight pneumococcal diseases such as severe pneumonia and meningitis.12 Although the vaccine is expected to reduce the burden of pneumococcal diseases, its protection against a limited number of serotypes means that the impact will not be as dramatic as Hib vaccine and there will be continued demand for hospital beds for the treatment of these diseases. Appropriate care at a health facility significantly increases survival of a child with severe pneumonia. Similarly, children with birth asphyxia who receive care are much more likely to survive without sequelae.
When determining vaccine policies and vaccine impact studies, it would be shortsighted to not consider the impact on morbidity and mortality of cases that are refused admission because of the hospitalization of children with a preventable disease such as rotavirus diarrhea.
EFFECT OF ROTAVIRUS ON THE OVERALL HEALTH SYSTEM SHOULD BE MEASURED WHEN ASSESSING VACCINE IMPACT: EVIDENCE FROM BANGLADESH
To our knowledge, there are no published data regarding the impact of bed occupancy by preventable cases on refusal of hospitalization of critical non-preventable illnesses. In our experience from working in Dhaka Shishu (Children) Hospital (DSH), the largest pediatric hospital of Bangladesh with 640 beds (37% non-paying) that provides care to patients between 0 months and 18 years, many critical cases requiring immediate care are refused hospitalization. To gain a better understanding of the dynamics of bed usage, we looked at admission and refusal records in the hospital between November 2015 and October 2016.
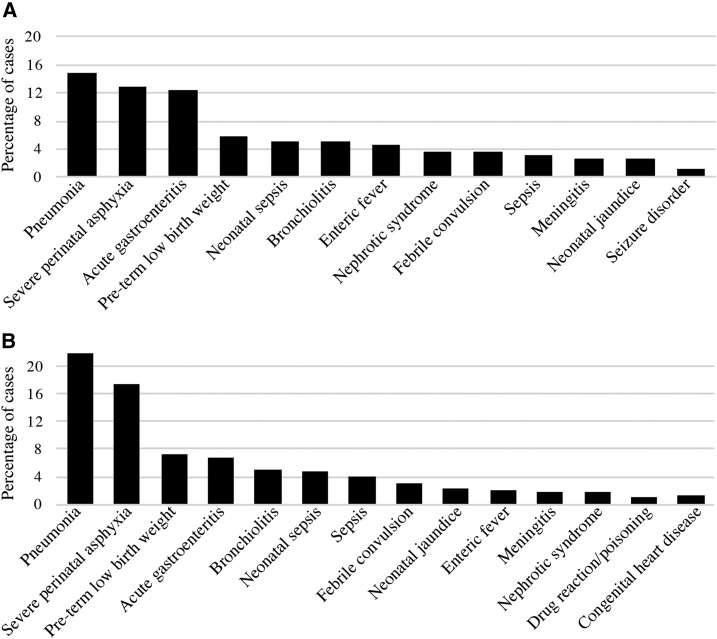
During this time, a total of 23,064 cases were admitted and 5,879 cases were refused because of unavailability of beds. Twelve percent (2,842/23,064) children were admitted because of acute gastroenteritis (AGE), 54% of which are caused by rotavirus.6 On the other hand, analysis by clinical signs of the refused cases showed that most of these were cases of pneumonia (N = 1,285; 22%), severe perinatal asphyxia (N = 1,020; 17%), preterm birth complications (N = 423; 7%), and meningitis (N = 102; 2%) (Figure 1). More than half of these refusals occurred in the evening/night, when most of the severe cases tend to arrive. As DSH does not have a delivery facility, preterm babies and neonates with asphyxia, which together sum up to 31% of refused cases, are referred from other facilities and often arrive later in the day. Similarly, cases of severe pneumonia and meningitis frequently come from geographically distant areas following referrals from facilities without the expertise to deal with them. Such late-arrivals often find the hospital at full-capacity, with a substantial fraction of beds occupied by AGE cases. Although we did not follow the refused cases, it is likely that many of these children succumb to the disease or survive with disability because of inappropriate or delayed treatment.
Figure 1.
Distribution of cases that were hospitalized (A) and refused hospitalization (B) in Dhaka Shishu (Children) Hospital, between November 2015 and October 2016. (A) A total of 23,064 cases were hospitalized. (B) A total of 5,879 cases were refused hospitalization because of unavailability of beds. Diseases that accounted for > 1% of all admissions/refusals are shown.
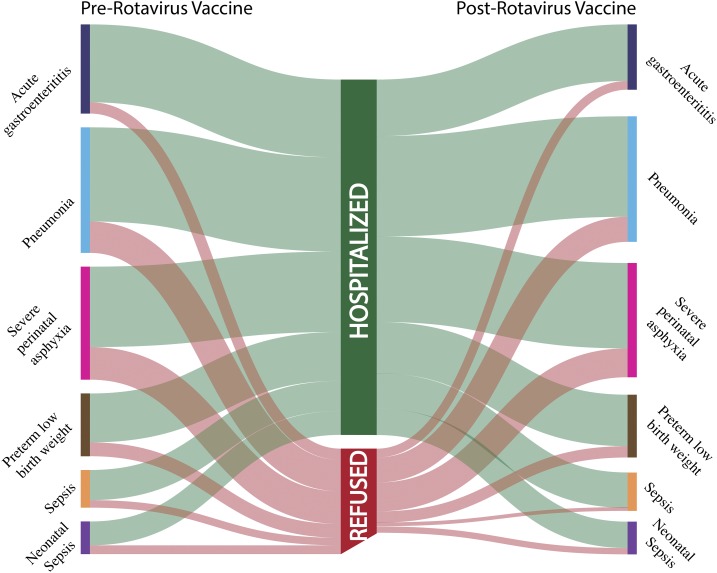
Another recent study in Bangladesh showed that the use of rotavirus vaccine reduced severe acute diarrhea by 41%, when vaccine coverage of 100% is attained, which is concordant with results obtained from phase III clinical trials of the vaccine conducted in the country.4,13 As 12% or 2,842 of total 23,064 admissions are due to AGE in DSH per year, and rotavirus is responsible for 54% of AGE cases and occupies 1,535 beds, a rotavirus vaccine with 41% efficacy will release 629 beds per year. In other words, 629 additional babies can be admitted per year, which is 11% of the 5,879 refused cases, if rotavirus vaccine is routinely used in Bangladesh (herd immunity was not taken into consideration). Therefore, in addition to reducing diarrheal episodes in children, rotavirus vaccine can potentially indirectly help save lives and prevent disabilities and have an impact on the overall health system in Bangladesh and the region. Figure 2 illustrates hypothetical direct and indirect impact of rotavirus vaccine on other communicable and non-communicable diseases.
Figure 2.
An illustration of hypothetical direct and indirect impact of rotavirus vaccine on other communicable and non-communicable illnesses. Bars at either end represent the distribution of the current top six diagnosis of hospitalized and refused cases seeking care at Dhaka Shishu Hospital (DSH). Each colored bar represents a disease. The widths of the ribbons from each bar represent the proportions. The green ribbons represent the proportion of cases that were hospitalized, and the red ribbons represent those that were refused. As acute gastroenteritis care seeking decreases after vaccination, decreased competition for beds results in fewer cases of other diseases being refused (represented by narrower red ribbons on the right compared with the left). This figure is not based on a specific calculation, but is an illustration of how rotavirus vaccine can lead to direct and indirect impacts based on admission and refusal data from DSH and results of rotavirus vaccine trial and efficacy studies performed in Bangladesh.
Impact of a vaccine is often documented by a decrease in burden of the disease at the specific health facilities after introduction. In a scenario where hospital beds are almost always full and patients are often refused hospitalization, a decrease in incidence of a disease may not be reflected in hospital admissions due to the “buffering” effect of previously refused cases and may lead to underestimation of vaccine benefits. Therefore, understanding refusals and bed occupancy is crucial to estimate vaccine impact on reducing stress on the health system, in addition to direct reduction of mortality and morbidity due to a particular disease.
It is undoubtedly true that a general expansion of the health system, including greater availability of beds with proportional increases in personnel and resources, is paramount. Realistically, however, this is an expensive goal decades away from fulfillment. Although on that path of improvement, prevention by a vaccine is a low hanging fruit that will help in reducing deaths and disabilities caused due to several communicable and non-communicable diseases.
ROTAVIRUS VACCINE IS A VACCINE THAT WE SHOULD ALL COME TOGETHER FOR
When a preventable-disease takes up many beds in a hospital, where neonates and children seeking urgent care are frequently refused admission because of unavailability of beds, prevention of that disease should become a priority. Rotavirus is not a problem of only gastroenterologists or diarrheal teams, but of all pediatricians and public health professionals. Based on data from Bangladesh, here we make the case that introduction of this vaccine in Bangladesh and the region will prevent morbidity and mortality, both directly and indirectly. It will help us to continue our global efforts toward ensuring survival and well-being of all children.
Acknowledgments
We are grateful to Ms. Maksuda Islam and Md. Jamaluddin for their assistance with preparation of the dataset and to Mr. Sudipta Saha for his guidance with preparation of the figures and editing the article.
Disclosures: Samir K. Saha has received research grants from GlaxoSmithKline, Sanofi Pasteur, and Pfizer. Mathuram Santosham has received research grants from GlaxoSmithKline and Pfizer, has served on their scientific advisory committees, and has also accepted honoraria for speaking engagements from them.
REFERENCES
- 1.Tate JE, Burton AH, Boschi-Pinto C, Steele AD, Duque J, Parashar UD, WHO-coordinated Global Rotavirus Surveillance Network, 2012. 2008 estimate of worldwide rotavirus-associated mortality in children younger than 5 years before the introduction of universal rotavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis 12: 136–141. [DOI] [PubMed] [Google Scholar]
- 2.WHO Meeting of the Immunization Strategic Advisory Group of Experts , 2009. Conclusions and recommendations. Wkly Epidemiol Rec 84: 517–532. [PubMed] [Google Scholar]
- 3.International Vaccine Access Center , 2017. Vaccine Information and Epidemiologu Window, (View-Hub) Available at: http://www.view-hub.org. Accessed June 12, 2017.
- 4.Kirkwood CD, Steele AD, 2017. Rotavirus vaccine will have an impact in Asia. PLoS Med 14: e1002298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halder AK, Gurley ES, Naheed A, Saha SK, Brooks WA, Arifeen SE, Sazzad HMS, Kenah E, Luby SP, 2009. Causes of early childhood deaths in urban Dhaka, Bangladesh. PLoS ONE 4: e8145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanmoy AM, et al. 2016. Rotavirus surveillance at a WHO-coordinated invasive bacterial disease surveillance site in Bangladesh: a feasibility study to integrate two surveillance systems. PLoS One 11: e0153582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Satter SM, Gastanaduy PA, Islam K, Rahman M, Rahman M, Luby SP, Heffelfinger JD, Parashar UD, Gurley ES, 2017. Hospital-based surveillance for rotavirus gastroenteritis among young children in Bangladesh: defining the potential impact of a rotavirus vaccine program. Pediatr Infect Dis J 36: 168–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kotloff KL, et al. 2013. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet 382: 209–222. [DOI] [PubMed] [Google Scholar]
- 9.WHO, 2009 World Health Statistics, 2009 Geneva, Switzerland: World Health Organization. Available at: http://www.who.int/whosis/whostat/2009/en/. Accessed June 12, 2017.
- 10.Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, Lawn JE, Cousens S, Mathers C, Black RE, 2016. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the sustainable development goals. Lancet 388: 3027–3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sultana NK, Saha SK, Emran Al HM, Modak JK, Sharker MAY, Arifeen El S, Cohen AL, Baqui AH, Luby SP, 2013. Impact of introduction of the Haemophilus influenzae type b conjugate vaccine into childhood immunization on meningitis in Bangladeshi infants. J Pediatr 163 (Suppl): S73–S78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saha SK, et al. Pneumococcal Study Group , 2016. Epidemiology of invasive pneumococcal disease in Bangladeshi children before introduction of pneumococcal conjugate vaccine. Pediatr Infect Dis J 35: 655–661. [DOI] [PubMed] [Google Scholar]
- 13.Zaman K, et al. 2017. Effectiveness of a live oral human rotavirus vaccine after programmatic introduction in Bangladesh: a cluster-randomized trial. PLoS Med 14: e1002282. [DOI] [PMC free article] [PubMed] [Google Scholar]