Abstract
Objective
Because no study has tested for interactions between risk factors in the prediction of future onset of each eating disorder, this exploratory study addressed this lacuna to generate hypotheses to be tested in future confirmatory studies.
Method
Data from three prevention trials that targeted young women at high risk for eating disorders due to body dissatisfaction (N=1271; M age 18.5, SD 4.2) and collected diagnostic interview data over 3-year follow-up were combined to permit sufficient power to predict onset of anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder (BED), and purging disorder (PD) using classification tree analyses, an analytic technique uniquely suited to detecting interactions.
Results
Low BMI was the most potent predictor of AN onset, and body dissatisfaction amplified this relation. Overeating was the most potent predictor of BN onset, and positive expectancies for thinness and body dissatisfaction amplified this relation. Body dissatisfaction was the most potent predictor of BED onset, and overeating, low dieting, and thin-ideal internalization amplified this relation. Dieting was the most potent predictor of PD onset, and negative affect and positive expectancies for thinness amplified this relation.
Conclusions
Results provided evidence of amplifying interactions between risk factors suggestive of cumulative risk processes that were distinct for each disorder; future confirmatory studies should test the interactive hypotheses generated by these analyses. If hypotheses are confirmed, results may allow interventionists to target ultra high-risk subpopulations with more intensive prevention programs that are uniquely tailored for each eating disorder, potentially improving the yield of prevention efforts.
Keywords: risk factors, prospective, interactions, anorexia nervosa, bulimia nervosa, binge eating disorder, purging disorder
Eating disorders affect 13% of females and are characterized by chronicity, relapse, distress, impaired social functioning, and increased risk for future obesity, depression, suicide, substance abuse, and mortality (Allen, Byrne, Oddy, & Crosby, 2013; Arcelus, Mitchell, Wales, & Nielsen, 2011; Stice, Marti, & Rohde, 2013; Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011). It is critical to identify risk factors that predict future onset of eating disorders because this information informs basic science regarding the etiology of eating disorders, informs that content of prevention programs, and identifies high-risk populations to target with selective prevention programs (Kraemer, Stice, Kazdin, & Kupfer, 2001). Only five studies have examined risk factors assessed at baseline that predict future onset of each DSM-IV or DSM-5 eating disorder among individuals confirmed to be initially free of these disorders, which provides rigorous evidence of temporal precedence.
Two studies examined risk factors for anorexia nervosa (AN). Low BMI and low dieting predicted onset of threshold or subthreshold AN over a 5-year follow-up in a community sample of adolescent girls (Stice & Bohon, 2013). Low BMI and impaired social functioning predicted onset of threshold or subthreshold AN over 3-year follow-up in the high-risk sample of young women with body dissatisfaction examined in the present report (Stice, Rohde, Shaw, & Gau, 2017).
Five studies examined risk factors for bulimia nervosa (BN). Dieters versus non-dieters showed elevated onset of threshold or subthreshold BN onset over a 1-year follow-up in adolescent girls (Patton, Johnson-Sabine, Wood, Mann, & Wakeling, 1990). Weight concerns, drive for thinness, body dissatisfaction, ineffectiveness, negative affectivity, dieting, and alcohol use, and low interoceptive awareness predicted onset of threshold or subthreshold BN over 4-year follow-up in adolescent girls (Killen et al., 1996). Dieting and psychiatric problems predicted BN onset over 3-year follow-up in adolescent girls (Patton, Selzer, Coffey, Carlin, & Wolfe, 1999). Elevated BMI, social pressure for thinness, thin-ideal internalization, dieting, fasting, negative affect, social support deficits, and early puberty predicted onset of threshold or subthreshold BN over 5-year follow-up in adolescent girls (Stice, Davis, Miller, & Marti, 2008a; Stice & Bohon, 2013). Social pressure to be thin and body dissatisfaction predicted onset of threshold or subthreshold BN over a longer 7-year follow-up from the same sample (Stice, Marti, & Durant, 2011a). Thin-ideal internalization, positive expectances from thinness, denial of the costs of pursuit of the thin ideal, body dissatisfaction, dieting, overeating, fasting, negative affect, impaired social functioning, and mental health care predicted threshold or subthreshold BN onset over 3-year follow-up in the high-risk sample of body-dissatisfied young women examined herein (Stice et al., 2017).
Two studies examined risk factors for binge eating disorder (BED). Social pressure for thinness predicted onset of threshold or subthreshold BED over 7-year follow-up in adolescent girls (Stice et al., 2011a). Thin-ideal internalization, positive expectances regarding thinness, body dissatisfaction, dieting, overeating, negative affect, impaired social functioning, and mental health care predicted BED onset over 3-year follow-up in the high-risk sample of young women examined herein (Stice et al., 2017).
Two studies examined risk factors for purging disorder (PD). Thin-ideal internalization, body dissatisfaction, and dieting predicted PD onset over 7-year follow-up in adolescent girls (Stice et al., 2011a). Thin-ideal internalization, positive expectances about thinness, denial of costs of pursuing the thin ideal, body dissatisfaction, dieting, fasting, overeating, excessive exercise, negative affect, impaired social functioning, and mental health care predicted PD onset over 3-year follow-up in the high-risk sample of young women examined herein (Stice et al., 2017).
Data from these five studies have advanced knowledge regarding risk processes for each of the eating disorders, but none tested for interactions among risk factors in the prediction of future onset of each eating disorder, which should inform etiologic theories, the optimal content of prevention programs for the various eating disorders, and identification of high-risk subpopulations for selective prevention programs. Thus, the overarching goal of this report was to use machine learning-based classification tree analysis (CTA) to investigate potential interactions between risk factors in the prediction of each type of eating disorder. Classification tree analysis (CTA), a recursive partitioning analytic approach, is optimal for detecting nonlinear interactions between risk factors (Breiman, Friedman, Stone, & Olshen, 1984), making it uniquely suited to address the goal of this report. CTA first identifies the single most potent risk factor that predicts the dichotomous outcome and selects the optimal cut-point on that risk factor that creates subgroups with maximally different probabilities for the outcome. This process is then repeated in each of the identified subgroups, or branches, in a recursive fashion until there are no remaining predictors or the minimal node size is reached. Interactions in CTA take a somewhat different form than the cross-product terms used in logistic regression (Loh, 2011). If the predictors identified for two branches differ, it signifies that the predictive effects of those two risk factors depend on the level of the first risk factor in the previous split of the sample, and hence reflects an interaction. It is also possible that the next optimal cut-points to emerge from a branch involve multiple levels of the same risk factor, which may signify a non-linear (e.g., quadratic) relation.
The low incidence of certain eating disorders, particularly AN, makes it difficult to detect risk factors for each eating disorder. Indeed, one of the largest prospective studies did not identify a single participant who showed onset of AN during the follow-up (McKnight Investigators, 2003). One solution is to use a high-risk design wherein participants at elevated risk for the disorder of interest are followed. Prospective high-risk designs have been used to elucidate risk factors for various psychiatric disorders, such as depression (LeMoult, Ordaz, Kircanski, Singh, & Gotlib, 2015) and substance abuse (Chassin, Pitts, DeLucia, & Todd, 1999). The present study combined data from three large eating disorder prevention trials that targeted young women at high-risk for future eating disorders by virtue of body dissatisfaction, which increased the incidence of threshold and subthreshold AN, BN, BED, and PD over 3-year follow-up, improving our ability to correctly classify individuals as developing each of these eating disorders. A previous report using data from this high-risk sample focused on the main effects of risk factors that predicted onset of AN, BN, BED, and PD (Stice et al., 2017), but did not test for interactions between risk factors. The goal of the present report was to conduct exploratory analyses regarding the interactions between risk factors assessed in this sample in predicting future onset of AN, BN, BED, and PD, to characterize the interacting relations between the risk factors examined in this unique data set.
We investigated various factors theorized to increase risk for eating disorders in several etiologic theories (e.g., Berg, Thompson, Obremski-Brandon, & Coovert, 2002; Hohlstein, Smith, & Atlas, 1998; Stice, 1994), including thin-ideal internalization, positive expectances for thinness, denial of costs of pursuing the thin ideal, body dissatisfaction, weight control behaviors, dieting, and negative affect. For instance, the dual pathway model posits that pressure to be thin and internalization of the thin beauty ideal contributes to body dissatisfaction, which in turn increases risk for both unhealthy dietary restriction and increased negative affect, which both theoretically increase risk for onset of binge eating and compensatory weight control behaviors (Stice, 1994). Similarly, expectancy theory posits that expecting that dieting and thinness result in greater social acceptance putatively increases risk for both restricting anorexia nervosa and bulimia nervosa, and expecting that eating reduces negative affect increases risk for binge eating (Hohlstein et al., 1998). We also investigated the predictive effects of prodromal eating disorder symptoms, based on evidence that fasting predicted future BN onset (Stice et al., 2008a). Specifically, we tested whether a low body weight, overeating, fasting, and excessive exercise predicted onset of AN, BN, BED, and PD. Finally, we examined the predictive effects of impaired social functioning and mental health care because, as reviewed above, they have predicted future onset of eating disorders, even though etiologic theories have not included these risk factors.
Methods
Participants and Procedures
We combined data from one efficacy trial (Trial 1; Stice, Marti, Spoor, Presnell, & Shaw, 2008b) and two effectiveness trials (Trial 2; Stice, Rohde, Shaw, & Gau, 2011b; Trial 3; Stice, Rohde, Butryn, Shaw, & Marti, 2015) that used parallel recruitment and assessment procedures, resulting in a sample of 1,272 participants (M age = 18.5, SD = 4.2). The sample was composed of 10% Asian/Pacific Islander, 5% African American, 11% Hispanic, 2% Native American, 67% Caucasian, and 4% who specified other or mixed heritage. Parental education was 11% high school graduate or less, 18% some college, 37% college graduate, and 33% advanced graduate/professional degree.
Design of Randomized Prevention Trials
Mailings and fliers were used to recruit female students for trials evaluating body acceptance interventions at high schools (Trial 1 and 2) and colleges (Trial 1 and 3). Informed consent was obtained from participants (and parents for minors). We required that participants report body image concerns during a phone screen for enrollment. Trial 1 participants were randomized to the Body Project dissonance-based eating disorder prevention program, the Healthy Weight eating disorder prevention program, an expressive writing comparison condition, or assessment-only control condition. Trial 2 and 3 participants were randomized to the Body Project or educational brochure control condition. We included dummy coded variables that reflected the conditions in the trials (e.g., coded 1 for participants assigned to the Body Project prevention program and 0 for participants assigned to other conditions) to control for intervention condition. Participants completed surveys and interviews at baseline and at 1-, 6-, 12-, 24-, and 36-month follow-up. Additional details can be found in Stice et al. (2008b, 2011b, 2015).
Measures
Eating pathology
The 30-item semi-structured Eating Disorder Diagnostic Interview (EDDI; Stice et al., 2013) assessed eating disorder symptoms over the past 3 months at baseline and since previous interview at follow-ups. Participants reported symptoms on a month-by-month basis over the follow-up (response options varied across items). DSM-5 criteria for eating disorders, operationalized in Table 1 and in Stice et al. (2017), were used. We focused on subthrehold AN rather than atypical AN, because we did not collect data on weight history, which is necessary to diagnose atypical AN. Overeating included counts of eating rapidly, eating until uncomfortably full, eating large amounts when not hungry, eating alone due to embarrassment, feeling depressed or guilty after overeating, and feeling upset about being out of control while overeating. Fasting reflected the number of times/week in past 3 months 2 meals in a row were skipped to compensate for overeating. Excessive exercise reflected the number of times/week in the past 3-months that participants engaged in vigorous exercise for more than 1 hour or moderate exercise for more than 2 hours to compensate for overeating. Inter-rater agreement for 298 randomly selected participants (ICC = .88) and 1-week test-retest reliability for 282 randomly selected participants (ICC = .95) in the combined sample were high.
Table 1.
Diagnostic Criteria for DSM-5 Eating Disorders
| Eating disorder | |
| Anorexia nervosa | Body mass index (BMI) less than 85% of the median expected for age and gender |
| Definite fear of weight gain more than 75% of the days for at least 3 months | |
| Weight and shape were one of the main aspects of self-evaluation | |
| Bulimia nervosa | At least four uncontrollable binge-eating episodes per month for at least 3 months |
| At least four compensatory behavior episodes per month for at least 3 months | |
| Weight and shape was definitely one of the main aspects of self-evaluation | |
| Binge eating disorder | At least four uncontrollable binge-eating episodes/days per month for at least 3 months |
| Less than one compensatory behavior on average per month during this period | |
| Marked distress about binge eating | |
| Binge eating characterized by three or more of the following: rapid eating; eating until uncomfortably full; eating large amounts when not physically hungry; eating alone because of embarrassment; feeling disgusted, depressed, or guilty after overeating | |
| Feeding or eating disorder-not elsewhere classified | |
| Subthreshold anorexia nervosa | BMI between 90% and 85% of that expected for age and gender |
| Definite fear of weight gain more than 25% of the days for at least 3 months | |
| Weight and shape were one of the main aspects of self-evaluation | |
| Purging disorder | At least four episodes of self-induced vomiting or diuretic/laxative use for weight control purposes per month for at least 3 months |
| Less than one uncontrollable binge-eating episode on average per month during this period | |
| Weight and shape were one of the main aspects of self-evaluation | |
Note. Anorexia nervosa took diagnostic precedence over bulimia nervosa and binge eating disorder.
Thin-ideal internalization
The 8-item Ideal-Body Stereotype Scale–Revised assessed thin-ideal internalization (Stice et al., 2008b). Response options ranged from 1 = strongly disagree to 5 = strongly agree. This scale has shown internal consistency (α = .91), test–retest reliability (r = .80), predictive validity for BN, BED, and PD onset, and sensitivity to detecting intervention effects (Stice et al., 2008b, 2017; α = .68 in the present sample).
Thinness expectancy
The 9-item Thinness Expectancy scale (Hohlstein et al., 1998) was used to assess expected social and psychological benefits from achieving thinness. Response options ranged from 1 = strongly disagree to 5 = strongly agree. This scale has shown internal consistency (α = .86) and predictive validity for onset of body dissatisfaction, BN, BED, and PD (Stice et al., 2017; Stice & Whitenton, 2002; α = .90 in the present sample).
Denial of thin ideal pursuit costs
We created 5 items assessing denial of costs associated with pursuing the thin ideal (e.g., The risks associated with severe dieting are overrated). Response options ranged from 1 = strongly disagree to 5 = strongly agree. This scale has shown internal consistency (α = .82), test-retest reliability (r = .87), and predictive validity for onset of BN and PD (Stice, Rohde, Gau, & Shaw, 2012, Stice et al., 2017; α = .77 in the present sample).
Body dissatisfaction
Nine items from the Satisfaction and Dissatisfaction with Body Parts Scale (Berscheid, Walster, & Bohrnstedt, 1973) assessed dissatisfaction with various body parts. Response options ranged from 1 = extremely satisfied to 5 = extremely dissatisfied. This scale has shown internal consistency (α = .94), test–retest reliability (r = .90), predictive validity for onset of BN, BED, and PD, and sensitivity to detecting intervention effects (Stice et al., 2008b, 2017; α = .91 in the present sample).
Weight control behaviors
We used the 5-item Weight Control scale to assess self-reported dietary and exercise behaviors used to control weight (e.g., I have eaten more fruits and vegetables). Response options ranged from 1 = strongly disagree to 5 = strongly agree. It has shown internal consistency (α = .82), test-retest reliability (r = .63), and sensitivity to detecting intervention effects (Stice, Presnell, Gau, & Shaw, 2007; α = .81 in the present sample).
Dieting
The 10-item Dutch Restrained Eating Scale (van Strien, Frijters, van Staveren, Defares, & Deurenberg, 1986) assesses the frequency of various dieting behaviors. Response options ranged from 1 = never to 5 = always. This scale has shown internal consistency (α = .95), test–retest reliability (r = .82), convergent validity with reported caloric intake (but not objectively measured intake), predictive validity for onset of BN, BED, and PD, and sensitivity to detecting intervention effects (Stice et al., 2008b, 2017; van Strien et al., 1986; α = .92 in the present sample).
Negative affect
Different measures of negative affect were used for each trial (at the request of grant reviewers). We therefore used z-score transformations to standardize scores so they could be combined into a single negative affect variable. In Trial 1 negative affect was assessed with the sadness, guilt, and fear/anxiety subscales from the Positive Affect and Negative Affect Scale-Revised (PANAS-X; Watson & Clark, 1992). Response options ranged from 1 = not at all to 5 = extremely. This 20-item measure has shown internal consistency (α = .95), test-retest reliability (r = .78), predictive validity for BN symptom onset, and sensitivity to detecting intervention effects (Stice et al., 2008b). In Trial 2 negative affect was assessed with the 20-item Center for Epidemiologic Studies-Depression Scale (CESD; Radloff, 1977). Response options ranged from 0 = never to 5 = most of the time. It has shown internal consistency (α = .74 – .91), reliability (test-retest r = .57 – .59), and convergent validity with clinician ratings of depressive symptoms (M r = .88; Andrews, Lewinsohn, Hops, & Roberts, 1993). In Trial 3 negative affect was assessed with the 21-item Beck Depression Inventory (Beck et al., 1988). Response options varied across items. It has shown internal consistency (α = .73–.95), test-retest reliability (r = .60–.90), convergent validity with clinician ratings of depressive symptoms, and sensitivity to detecting intervention effects (M r = .75; Beck et al., 1988; Stice et al., 2015). The average convergent validity coefficient across multiple independent samples was r = .58, providing evidence that these three measures tap a similar construct, particularly given that the average 1-week test-retest coefficient for these measures was an r = .66, providing an upper-limit to the potential magnitude of convergent validity coefficients (Andrews et al., 1993; Beck, Steer, & Garbin, 1988; Denollet & Vries, 2006; Watson, Clark, & Tellegen, 1988; Wilcox et al., 1998).
Impaired social functioning
Impairment in the family, peer group, romantic, and school domains was measured with 17 items from the Social Adjustment Scale-Self Report for Youth (Weissman, Orvaschel, & Padian, 1980). Response options ranged from 1 = never to 5 = always. The original scale has shown convergent validity with clinician and collateral ratings (M r = .72) and sensitivity to detecting treatment effects (Weismann & Bothwell, 1976). The 17-item version has shown internal consistency (α = .77), test–retest reliability (r = .83), predictive validity for future onset of AN, BN, BED, and PD, and sensitivity to detecting intervention effects (Stice et al., 2008b, 2017; α = .75 in the present sample).
Mental health utilization
Participants reported the frequency of visits to mental health care providers. Receipt of care in the last 6-months was coded “1” and no health care coded “0”. This item showed 1-year test-retest reliability (r = .89), predictive validity for BN, BED, and PD, and sensitivity to detecting intervention effects (Stice et al., 2008b; Stice et al., 2013, 2017).
Body mass
The BMI (kg/m2; Pietrobelli et al., 1998) was calculated based on height, measured to the nearest millimeter using portable stadiometers, and weight, assessed to the nearest 0.1 kg using digital scales with participants wearing light indoor clothing without shoes. Height and weight were measured twice and averaged. Age- and sex-adjusted BMI centiles (Faith, Saelens, Wilfley, & Allison, 2001) were used to determine whether participants were underweight for AN. BMI has shown convergent validity (r = .80 – .90) with direct measures of body fat (Pietrobelli et al., 1998) and predictive validity for future onset of AN (Stice et al., 2017).
Statistical Methods
Preliminary analyses compared the three samples on demographic factors and tested the assumption that the measures showed similar internal reliability across the three samples.
CTA was used to test whether the risk factors predicted future onset of subthreshold or threshold eating disorders. We tested whether we could classify participants who developed AN (2.1% incidence), BN (5.9% incidence), BED (6.0% incidence), or PD (5.2% incidence) over the 3-year follow-up from those who did not develop each of those eating disorders. For each tree, those participants who met criteria for the targeted subthreshold or threshold eating disorder at baseline were excluded. For example, if a participant had subthreshold AN at baseline then they were excluded from the AN tree but not from the BN, BED, and PD trees.
Several decisions are made during CTA. The first involved the splitting criteria. We used the Gini index as our splitting criteria, which measures the total variance across the classes and reflects the impurity of a node. When a node has a small Gini index (a pure node) it indicates the node contains predominately one class. Predictors that when split create purer nodes are selected over predictors that result in more heterogeneous splits per the Gini index. Although it is valuable to detect the interactions between risk factors that emerged in this unique data set, it is also important to avoid overfitting CTA models. Several steps were taken to reduce overfitting, including setting the minimum size that a node cannot be further split (20), setting the minimum size for a terminal node (10), setting the threshold complexity parameter (0.01), and using cross-validation. We explored multiple approaches to pruning our trees via cross-validation including randomly splitting the data into training and testing data sets and applying the one standard error rule and using the complete data set with k-folds (k = 10) cross validation (James et al. 2013). However, both approaches pruned all the branches from all trees. This was not unexpected because CTA involving rare or small classes (as in our study) suffer from class imbalance and difficulty separating the predictor space (Sun, Wong, & Kamel 2009). Because of this, we report the F-measure, the harmonic mean between the true positive rate and positive predictive rate, and the G-mean, the square root of the true positive rate and true negative rate (Sun et al., 2009), for our unpruned trees rather than prune. Both the F-measure and the G-mean range between 0 and 1 with higher values indicative of more accurate models.
As a sensitivity check to our CTA, we considered two alternative classification methods: random forest and boosting classification (James et al. 2013). A random forest classification takes a large number (B) bootstrap samples to construct B classification trees. For each sample, each time the tree is to be split, the algorithm selects a random subsample m of the predictors and only one of these selected m predictors is used to construct the split. This process is repeated until a tree has been constructed. By using a subsample of the available predictor space, the trees should be de-correlated across the samples and result in more reliable estimates. Boosting classification is like the random forest except that multiple trees are grown sequentially using all available predictors with a modified data set rather than bootstrapped samples of the original data. Friedman, Hastie, and Tibshirani (2001) and James et al. (2013) provide more details regarding random forests and boosting. For random forest classification, we set B to 500 and m to the square root of the number of risk variables. For boosting, we grew 5000 trees and set the tuning parameter to 0.001.
All analyses were performed in R (R Core Team 2017). CTA was performed using the rpart library (Therneau, Atkinson, & Ripley, 2017); random forests with the randomForest library (Liaw & Wiener, 2002), and boosting with the gbm library (Ridgeway et al., 2017). It is important to note that CTA, random forests, and boosting are non-parametric statistical techniques, and as such, do not have distributional or linearity assumptions.
Results
Preliminary Analyses
The means and SD for all predictors, as well as the correlations between the risk factors were reported previously (Stice et al., 2017). The average correlation among the risk factors was .14 (range = .01 – .54), suggesting that the risk factors were relatively independent. The previous report also confirmed that this sample had elevated body dissatisfaction relative to a representative community sample (Stice et al., 2017). Table 2 reports the age, ethnic/racial composition, and parental education (a proxy for socioeconomic status) for the three samples, which varied in these demographic factors. Given that ethnicity/race and parental education have not been found to predict future onset of eating disorders and showed only small correlations with the risk factors in the combined sample (M r = .02; largest r = .20, which was between age and thin-ideal internalization), it is unlikely that variation in these demographic factors biased the predictive effects.
Table 2.
Demographics and effect sizes by Body Project Study.
| Study | State | N | Age (SD) | Non-Hispanic white (%) | Hispanic (%) | Parent college degree (%) | ||
|---|---|---|---|---|---|---|---|---|
| BP-I | OR | 0 | 17.05 (1.42) | 59.66% | 18.28% | 77.63% | ||
| TX | 481 | |||||||
| PA | 0 | |||||||
|
|
||||||||
| BP-II | OR | 306 | 16.24 (1.30) | 83.44% | 2.65% | 59.33% | ||
| TX | 0 | |||||||
| PA | 0 | |||||||
|
|
||||||||
| BP-III | OR | 195 | 21.48 (5.42) | 64.73% | 9.54% | 72.37% | ||
| TX | 157 | |||||||
| PA | 133 | |||||||
|
| ||||||||
| Variable | BP-I v. BP-II | BP-I v. BP-III | BP-II v. BP-III | |||||
|
| ||||||||
| p | Effect size | p | Effect size | p | Effect size | |||
|
| ||||||||
| Age | < .001 | 0.59 | < .001 | 3.18 | < .001 | 0.97 | ||
| Non-Hispanic White | < .001 | 0.54 | .239 | 0.10 | <.001 | 0.43 | ||
| Hispanic | <.001 | 0.56 | <.001 | 0.26 | .002 | 0.31 | ||
| Parent college degree | <.001 | 0.40 | .148 | 0.12 | <.001 | 0.28 | ||
Note. For age, the effect size measure was Cohen’s d and the statistical test was a t-test and for the other variables, the effect size measure was Cohen’s w and the statistical test was a Wald test. For both effect size measures, an effect size of 0.20 is small, 0.50 is medium, and 0.80 is large.
We also examined the assumption that the measures showed similar internal consistency across the three samples. Cronbach’s alphas were similar across the samples: thin-ideal internalization (α range: .63 – .73), thinness expectances (α range: .90 – .91), denial of thin ideal pursuit costs (α range: .74 – .78), body dissatisfaction (α range: .87 – .91), weight control behaviors (α range: .81 – .82), dieting (α range: .92 – .92), negative affect (α range: .89 – .95), impaired social functioning (α range: .75 – .76). These data suggest that the measures showed similar internal reliability across the three samples.
We attempted to conduct more formal tests of factorial invariance across the samples, but preliminary analyses suggested that some scales did not show unidimensionality, resulting in poor model fits for the configural models. For example, for the body dissatisfaction scale, the fit measures were: CFI = .916, TLI = .888, and RMSEA = .191 and for the dieting scale, the fit measures were: CFI = .972, TLI = .964, and RMSEA = .114. Standardized loadings across the samples ranged from .615 – .900 for body dissatisfaction and from .654 – .900 for dieting, indicating the items all loaded highly on a factor but that there was unexplained covariation among the items that resulted in poor model fit. Additionally, the large sample size almost assured we would reject the null hypothesis of invariance with the chi-squared test. Little, Preacher, Selig, & Card (2007) suggest using the RMSEA for assessing improvement in fit instead of using this test. For both body dissatisfaction and dieting, while the RMSEAs continued to suggest poor fit for the weak invariance model, the RMSEAs did decrease from .191 to .164 for body dissatisfaction and from .114 to .089 for dieting implying that fit did improve, substantially, when constraints were imposed even though this improvement was not statistically significant.
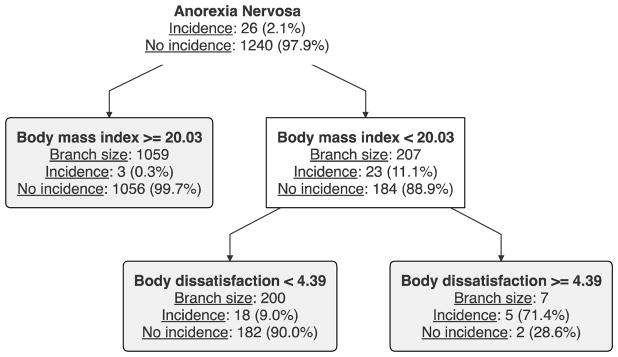
Anorexia Nervosa
Figure 1 shows the classification tree for AN. Two predictors were identified as important for classifying participants into those who subsequently developed AN versus those who did not: BMI and body dissatisfaction. BMI emerged as the most potent predictor: for participants in the upper 83% of BMI the incidence of AN onset was 0.3% versus 11.1% for participants in the lower 17% of BMI. Among participants in the lower 17% of BMI, the incidence of AN was 9.0% for participants in the lower 89% of body dissatisfaction, versus 71.4% for participants in the upper 11% of body dissatisfaction. Thus, results provide evidence of a 2-way amplifying interaction between BMI and body dissatisfaction, wherein young women with a confluence of low BMI and elevated body dissatisfaction were at very high risk of developing AN.
Figure 1.
Classification tree for anorexia nervosa.
Note. The gray, rounded nodes are terminal.
The overall classification rate for the tree was .982 compared to .979 for the null tree (where all participants are predicted not to develop AN) and the F-measure was .303 and the G-mean was .438. Both random forest and boosting identified BMI as the most important predictor followed by dieting. The random forest identified BMI as being 3 times more important than body dissatisfaction (which had roughly equivalent importance to dieting), whereas boosting identified BMI as being 7 times more important than body dissatisfaction and 4 times more important than dieting. Thus, these results confirm that BMI is the most important predictor and provided some support for the importance of body dissatisfaction.
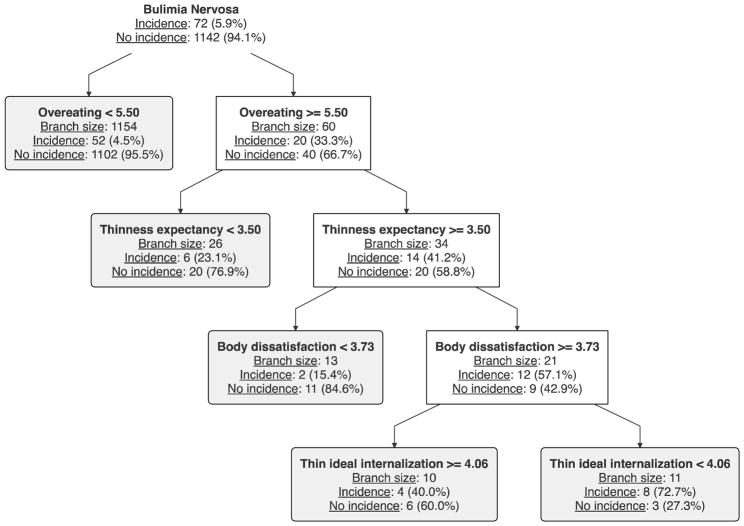
Bulimia Nervosa
Figure 2 shows the classification tree for BN. Overeating, positive expectancies for thinness, body dissatisfaction, and thin-ideal internalization were identified as important classifiers of whether a participant would subsequently develop BN. The first split occurred at the 95th percentile of overeating. For those in the lower 95% of overeating, the incidence of BN was 4.5%, versus 33.3% for those in the upper 5% of overeating. Among those with higher overeating scores, the incidence of BN was 23.1% for those in the lower 65% of positive thinness expectancies, versus 41.2% for those in the upper 35% of positive thinness expectancies. Of those with higher overeating and thinness expectancy, the incidence of BN onset was 15.4% for participants in the lower 67% of body dissatisfaction scores, versus 57.1% for those participants in the upper 33% of body dissatisfaction. Among those participants with higher overeating, positive thinness expectancies, and body dissatisfaction, the incidence of BN onset was 40% for participants in the upper 22% of thin-ideal internalization, versus 72.7% for participants in the lower 78% of thin-ideal internalization. Thus, results provide evidence of a 4-way amplifying interaction between overeating, thinness expectancy, body dissatisfaction, and thin idea internalization, wherein young women with a confluence of high overeating, thinness expectancy, and body dissatisfaction, and low thin ideal internalization are at the highest risk of developing BN.
Figure 2.
Classification tree for bulimia nervosa.
Note. The gray, rounded nodes are terminal.
The overall classification rate for this tree was .945 compared to .937 for the null tree. The F-measure was .193 and the G-mean was .333, respectively. The random forest identified overeating and BMI as the two most important predictors. Boosting identified the thin-ideal internalization and negative affect as having the greatest predictive power, but suggested that overeating and body dissatisfaction had similar predictive power. However, many predictors had nearly equivalent importance to these predictors (e.g., positive thinness expectancy and denial of costs of pursuing the thin ideal). Therefore, all three methods suggested that overeating was important and two methods identified body dissatisfaction and thin-ideal internalization as important.
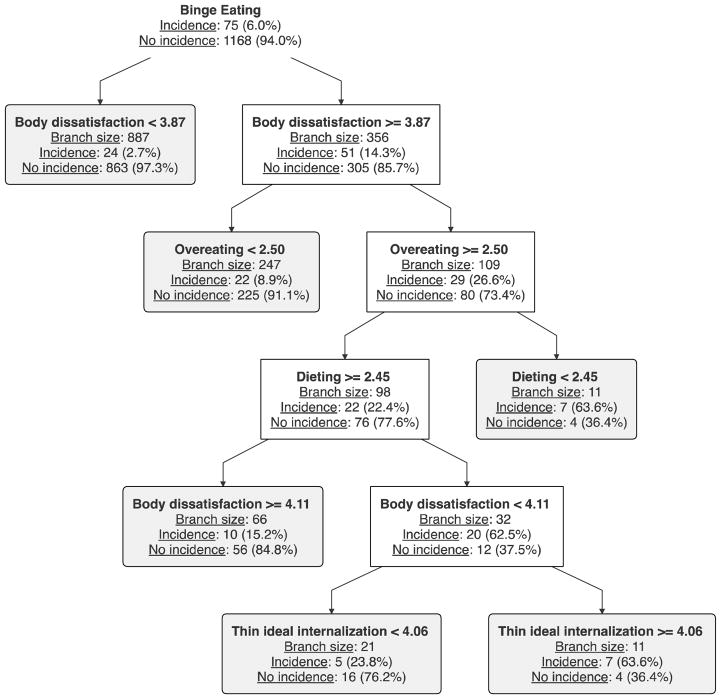
Binge Eating Disorder
The classification tree for BED is shown in Figure 3. Four risk factors were identified as important for predicting BED: body dissatisfaction, overeating, dieting, and thin-ideal internalization. The first branching occurred for body dissatisfaction. Among those in the lower 71% of body dissatisfaction, the incidence of BED was 2.7%, versus 14.3% for those in the upper 29% of body dissatisfaction. Among participants with higher body dissatisfaction, the incidence of BED was 8.9% for those in the lower 82% of overeating, versus 26.6% in the upper 18% of overeating. Among participants with higher body dissatisfaction and higher overeating, the incidence of BED was 63.6% for those in the lower 41% on dieting versus 22.4% for those in the upper 59% of dieting. Among the participants with higher body dissatisfaction, higher overeating, and higher dieting, the incidence of BED was 15.2% for those in the upper 17% of body dissatisfaction, versus 62.5% for those between the 71st and 83rd percentile of body dissatisfaction. Among this latter group, the incidence of BED was 63.6% for those in the upper 23% of thin-ideal internalization, versus 23.8% for those in the lower 77% of thin-ideal internalization. Results provide evidence of two pathways leading to BED. Young women with high body dissatisfaction, high overeating, and low dieting, and young women with high body dissatisfaction, high overeating, high dieting, and high thin ideal internalization are both at high risk of developing BED.
Figure 3.
Classification tree for binge eating disorder.
Note. The gray, rounded nodes are terminal.
The overall classification rate for this tree was .944 compared to .936 for the null tree. The F-measure was .288 and the G-mean was .431. As with BN, the random forest identified overeating, functional impairment, and body dissatisfaction as having the greatest importance, while boosting identified body dissatisfaction, negative affect, and dieting as most importance. Thus, all three methods selected body dissatisfaction as important and two methods identified overeating and dieting as important.
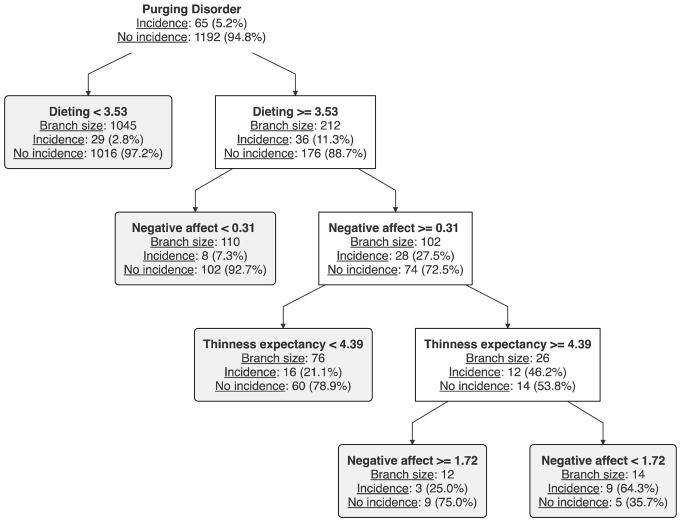
Purging Disorder
The classification tree for PD is presented in Figure 4. Dieting, negative affect, and positive thinness expectancies were identified as important for classifying whether participants would develop PD. Elevated dieting emerged as the most potent risk factor; among those in the upper 17% of dieting the incidence of PD was 11.3%, versus 2.8% for those in the lower 83% of dieting. Among those with higher dieting, the incidence of PD was 27.5% for those in the upper 31% of negative affect, versus 7.3% for those in the lower 69% of negative affect. Among those with higher dieting and higher negative affect, the incidence of PD onset was 46.2% for those in the upper 8% of positive thinness expectances, versus 21.1% for those with in the lower 92% of positive thinness expectances. Among those with higher dieting, higher positive thinness expectances, and negative affect scores greater than the 69th percentile, the incidence of PD was 64.3% for those for those between the 69th and 93rd percentiles of negative affect, versus 25.0% for those in the highest 7% of negative affect, suggesting that extremely high negative affect serves as a protective factor against developing PD. Results provide evidence of a complex nonlinear 3-way interaction between dieting, negative affect, and positive thinness expectances, wherein elevated negative affect and positive expectances regarding thinness amplify the risk conveyed by elevated dieting in the prediction of PD onset, but very high negative affect attenuated risk for PD onset.
Figure 4.
Classification tree for purging disorder.
Note. The gray, rounded nodes are terminal.
The overall classification rate for this tree was .951 compared to .945 for the null tree. The F-measure was .227 and the G-mean was .371. The random forest again failed to identify any one predictor as most important. In contrast, boosting identified negative affect as the most important variable (almost twice as important as dieting, the next most important variable). This corroborates the findings in the PD tree that shows additional branching associated with negative affect but a single branching for dieting.
Discussion
The goal of this report was to use CTA to test for potential interactions between risk factors in the prediction of future onset of AN, BN, BED, and PD using data from a unique large sample of individuals at elevated risk for future onset of eating disorders by virtue of body dissatisfaction that permitted sufficient sensitivity to address this novel research question. With regard to the prediction of future AN onset, results suggested that a low BMI was the most potent predictor, and that elevated body dissatisfaction amplified the predictive effects of a low BMI, wherein participants with a low BMI and elevated body dissatisfaction were at very high risk of developing AN, showing an incidence of 71%. This tree therefore suggested a 2-way interaction wherein body dissatisfaction amplifies the risk conveyed by low BMI in predicting future AN onset. The F-measure was .303 and the G-mean was .438, providing evidence of moderate prediction accuracy. Random forest and boosting confirmed that BMI was the most important predictor followed by body dissatisfaction and to a lessor extent dieting. Results converge with prior evidence that a low BMI increased risk for future onset of AN in an independent data set (Stice & Bohon, 2013), which is reassuring given the exploratory nature of CTA. Results from these two studies may imply that etiologic models for AN should incorporate low BMI as a core risk factor, though it is unclear whether the low BMI occurs because some biological factor (high satiety signaling or low hunger signaling of gut hormones) or extreme fat phobia, which could reflect parental attitudes towards obesity. Findings also suggest that body dissatisfaction increases risk for future AN onset, though it only did so for individuals with a low BMI. The presence of high body dissatisfaction among low-weight young women may reflect extreme fat phobia that drives the caloric restriction that results in AN. The evidence of an amplifying interaction between low BMI and high body dissatisfaction in the prediction of future AN onset is novel. Although it will be important to confirm this interactive hypothesis in future high-risk studies, results imply that etiologic theories should include a low BMI as a core risk factor, as well as the amplifying effect of body dissatisfaction, neither of which has received much attention in etiologic formulations. Assuming these effects replicate, results suggest that it might be useful to implement selective prevention programs with adolescent girls who have a confluence of low BMI and high body dissatisfaction, and further than it might be useful to promote increased caloric intake and body acceptance in the prevention programs.
In terms of the prediction of future BN onset, results provided evidence of a complex 4-way interaction between overeating, positive expectations regarding thinness, body dissatisfaction, and thin-ideal internalization, which included a non-linear effect of positive thinness expectances. Results suggest that overeating was the most potent predictor of BN onset, and that elevated positive expectances regarding thinness and body dissatisfaction amplified the risk convened by overeating in the prediction of BN onset, resulting in an incidence of BN onset of 57%. Paradoxically, among those with a confluence of these risk factors, relatively lower pursuit of the thin ideal was associated with increased risk for BN onset. Pursuit of the thin ideal may serve as a protective factor among these individuals, reducing risk for binge eating, a core symptom of BN. The F-measure was .193 and the G-mean was .333, suggesting that the predictive accuracy for this tree was somewhat lower than for the AN tree. The random forest and boosting identified several predictors with similar importance suggesting that multiple risk factors may play a role in predicting BN onset. Results dovetail with prior evidence that body dissatisfaction increases risk for BN (Killen et al., 1996), which is reassuring given the exploratory nature of CTA. However, the evidence that positive expectances for thinness and body dissatisfaction amplifies the risk conveyed by overeating is novel. Assuming effect replicate in a future high-risk studies, results may imply that it would be important to incorporate overeating as a key risk factor for BN into etiologic models, and to consider including the amplifying interactions with positive expectances regarding thinness and body dissatisfaction, which are suggestive of a cumulative risk factor model. If these results replicate, it would suggest that that it might be fruitful to target adolescent girls with a confluence of elevated overeating, positive expectances regarding thinness, and body dissatisfaction, and further that it might be useful to implement prevention programs that have reduced overeating and body dissatisfaction (Neumark-Sztainer et al., 1995; Stice et al., 2008b, in press) and to also attempt to reduce positive expectances regarding thinness.
With regarding to BED, results suggested a complex 4-way interaction between body dissatisfaction, overeating, dieting, and thin-ideal internalization, which included a non-linear effect for body dissatisfaction. Body dissatisfaction emerged as the most potent risk factor in predicting BED onset. Results indicated that elevated overeating amplified the predictive effects of body dissatisfaction, which is a novel finding. Unexpectedly according to existing etiologic theories, results suggested that low dieting amplified the risk conveyed by the combination of elevated body dissatisfaction and overeating, resulting in a node in which 64% of participants showed BED onset. Findings imply that elevated dieting may serve as a protective factor against developing BED for individuals who overeat and have body dissatisfaction. Perhaps people who are not attempting to reduce overeating are more likely to show onset of binge eating, the hallmark of BED. Paradoxically, results also suggest that relatively lower body dissatisfaction among those with elevated body dissatisfaction was associated with higher BED onset, which is challenging to reconcile with the fact that body dissatisfaction was the single more potent predictor of BED onset. Results might communicate that there is a non-linear relation between body dissatisfaction and BED onset. Perhaps extremely high body dissatisfaction is a protective factor because it reduces the likelihood of binge eating. Findings suggest that CTA may be a particularly useful technique for identifying protective factors, which have been difficult to identify with standard predictive approaches that focus on main effects in the entire sample. The final split suggested that lower thin-ideal internalization mitigates the risk conveyed by the combination of overeating, body dissatisfaction, and dieting, reducing the incidence of BED onset to 24%, versus the 64% observed for individuals with higher thin-ideal internalization. The F-measure was .288 and the G-mean was .431, suggesting moderate accuracy of the tree. As with BN, random forest did not identify any one predictor as more important than other predictors, while boosting identified body dissatisfaction, negative affect, and mental health care as slightly more important. However, neither technique identified a single predictor as the most important, suggesting multiple predictors of relative equal importance for predicting BED. If findings replicate in an independent sample, they might imply that etiologic models for BED should incorporate amplifying interactions between body dissatisfaction and overeating, and potentially the protective effects of higher dieting among overeaters and the non-linear effects of body dissatisfaction. Again assuming these findings replicate, results suggest that there might be merit in targeting individuals with a confluence of body dissatisfaction, overeating, and low dieting, as well as those with higher dieting that is accompanied by lower body dissatisfaction. Echoing the implications from the BN tree, these findings may imply that prevention programs that reduce body dissatisfaction and overeating (Celio et al., 2000; Stice et al., 2008b, in press) may be particularly effective in reducing risk for BED, as well as prevention programs that have reduced pursuit of the thin ideal (Stice et al., 2008b).
In terms of predicting PD onset, results provided evidence for a 3-way interaction between dieting, negative affect, and positive thinness expectances, which included a non-linear effect of negative affect. Dieting emerged as the most potent predictor of PD onset, replicating previous findings from an independent sample (Stice et al., 2011a), which is reassuring given the exploratory nature of CTA. Results suggested that elevated negative affect amplified the relation between elevated dieting and risk for PD onset, which is a novel finding, with over 27% of individuals with a confluence of these two risk factors showing PD onset. There was also evidence that positive expectances regarding thinness further amplified risk for PD onset, which is another novel finding, with over 46% of those with a confluence of these three risk factors showing PD onset. Further, data suggested that among participants with these three risk factors, individuals with relatively higher negative affect showed a lower incidence of PD onset. These results suggest that very high negative affect may serve as a protective factor, potentially because anhedonia reduces appetite and caloric intake. Thus, this tree suggested that negative affect amplified the risk of high dieting, that high positive thinness expectancies amplified the risk of high negative affect, but that high negative affect paradoxically mitigated the risk of high positive thinness expectances. The F-measure was .227 and the G-mean was .371, suggesting moderate predictive accuracy of this tree. Although the random forest did not identify any one predictor as most important, boosting suggested that negative affect as the most important variable, consistent with the evidence that it emerged twice in this tree. If these finding replicate in an independent sample, they might suggest it would be useful to include the amplifying interaction between dieting, negative affect, and positive thinness expectances, which implies a cumulative risk factor model might have merit. Assuming these findings replicate, the results may imply that it might be optimal for selective prevention programs for PD to target young women with a confluence of dieting, negative affect, and positive thinness expectances, and further that interventions that reduce dieting, negative affect, and positive expectances regarding thinness (Neumark-Sztainer et al., 1995; Rohde et al., 2015; Stice et al., 2008b) might prove useful in preventing future PD onset.
It is important to consider the limitations of this study when interpreting the findings. First, because this study examined young women at high-risk for eating disorders by virtue of body dissatisfaction, results may not generalize to other populations. Although high-risk designs are useful for increasing sensitivity to detecting predictive effects for rare disorders, examining individuals with a particular risk factor may bias the results toward risk factors that correlate with that risk status, and away from those not correlated with that risk status. Fortunately, this high-risk sample also showed elevated thin-ideal internalization, dieting, and overeating (Stice et al., 2017). It is important to note that there was no evidence of a greater restriction in range, as indexed by the SD, for body dissatisfaction (0.79) relative to the other risk factors examined in this study, such as thin ideal internalization (0.53) and dieting (0.90) (Stice et al., 2016). Second, although the measures showed similar internal reliability across the three samples, confirmatory factor analyses revealed that some of measures did not show unidimensionality, which led us to not conduct formal tests of factorial invariance across the samples. The fact that these measures have shown internal reliability and temporal reliability (reviewed in the measures section), as well as predictive validity and sensitivity to detecting intervention effects, in multiple samples, implies that confidence can be placed in the findings, despite the fact that some measures might not be unidimensional. Third, although we examined several factors that have been included in etiologic models for eating disorders and examined the predictive effects of prodromal symptoms, we did not assess biological risk factors that might play a role in the etiology of eating disorders. Future prospective high-risk studies should assess biological risk factors. Fourth, although prospective data are useful for establishing the temporal precedence between the risk factors and subsequent onset of the pathological condition, prospective data does not permit causal inferences. Ideally randomized prevention trials will confirm that reducing the identified risk factors produces a significant reduction in future onset of the particular eating disorder relative to participants randomly assigned to some sort of credible alternative intervention comparison condition, which is necessary to rule out the possibility that differential demand characteristics and expectances drive reductions in eating disorder onset.
In conclusion, results from this unique large sample of individuals at high-risk for eating disorders provided evidence of several amplifying interactions between risk factors that appeared to be distinct for AN, BN, BED, and PD. The evidence of amplifying interactions between risk factors is a unique contribution to the literature and suggests that it might be prudent for etiologic theories to incorporate a cumulative risk factor process. Further, the evidence of protective factors, such as high dieting and very high negative affect is another novel contribution, though those applied to somewhat rare high-risk subgroups, highlighting the importance of considering interactions among risk factors in etiologic theories. The amplifying interactions and protective factors identified herein also provide unique evidence that there may be qualitatively distinct risk pathways to these eating disorders. More generally, the fact that the risk factors for each of the examined eating disorders were distinct is a third novel contribution, which implies that etiologic processes for these disorders might be qualitatively distinct. As noted, it will be important for future confirmatory studies to test the interactive hypotheses generated by these exploratory analyses. If the hypotheses are confirmed, results may allow interventionists to target ultra high-risk subpopulations with more intensive prevention programs that are uniquely tailored for each eating disorder, which might improve the yield of prevention efforts. This is critical because even the most promising eating disorder prevention programs at best produced a 60% reduction in future eating disorder onset over multiple-year follow-up periods, signaling that an important public health priority is to develop even more effective prevention programs.
Highlights.
First test for interactions between risk factors for eating disorder onset.
Low BMI interacted with body dissatisfaction to predict anorexia nervosa onset.
Overeating and thin-ideal internalization interacted to predict bulimia nervosa.
Body dissatisfaction and overeating interacted to predict binge eating disorder.
Dieting and negative affect interacted to predict purging disorder.
Acknowledgments
This research was supported by NIH grants MH/DK061957, MH070699, and MH086582.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen K, Byrne S, Oddy H, Crosby R. Eating Disorders in Adolescents: Prevalence, Stability, and Psychosocial Correlates in a Population-Based Sample of Male and Female Adolescents. Journal of Abnormal Psychology. 2013;122:720–32. doi: 10.1037/a0034004. [DOI] [PubMed] [Google Scholar]
- Andrews JA, Lewinsohn PM, Hops H. Psychometric properties of scales for the measurement of psychosocial variables associated with depression in adolescence. Psychological Reports. 1993;73:1019–1046. doi: 10.2466/pr0.1993.73.3.1019. [DOI] [PubMed] [Google Scholar]
- Arcelus J, Mitchell A, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. JAMA Psychiatry. 2011;68:724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RM, Garbin M. Psychometric properties of the Beck Depression Inventory: 25 years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Berg P, Thompson JK, Obremski-Brandon K, Coovert M. The tripartite influence model of body image and eating disturbance: A covariance structure modeling investigation testing the meditational role of appearance comparison. Journal of Psychosomatic Research. 2002;53:1007–1020. doi: 10.1016/s0022-3999(02)00499-3. [DOI] [PubMed] [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychology Today. 1973;7:119–131. [Google Scholar]
- Celio AA, Winzelberg AJ, Wilfley DE, Eppstein-Herald D, Springer EA, Dev P, et al. Reducing risk factors for eating disorders: Comparison of an internet- and classroom-delivered psychoeducational program. Journal of Consulting and Clinical Psychology. 2000;68:650–657. [PubMed] [Google Scholar]
- Chassin L, Pitts S, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. Journal of Abnormal Psychology. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- Denollet J, Vries J. Positive and negative affect within the realm of depression, stress and fatigue: The 2-factor distress model of the Global Mood Scale (GMS) Journal of Affective Disorders. 2006;91:171–180. doi: 10.1016/j.jad.2005.12.044. [DOI] [PubMed] [Google Scholar]
- Hohlstein L, Smith G, Atlas J. An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychological Assessment. 1998;10:49–58. [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L, et al. Weight concerns influence the development of eating disorders: a 4-year prospective study. Journal of Consulting and Clinical Psychology. 1996;64:936–940. doi: 10.1037//0022-006x.64.5.936. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Kupfer D. How do risk factors work? Mediators, moderators, independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- LeMoult J, Ordaz S, Kircanski K, Singh M, Gotlib I. Predicting first onset of major depression in young girls: Interaction of diurnal cortisol and negative life events. Journal of Abnormal Psychology. 2015;124:8450–859. doi: 10.1037/abn0000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little TD, Preacher KJ, Selig JP, Card NA. New developments in latent variable panel analyses of longitudinal data. International Journal of Behavioral Development. 2007;31(4):357–365. https://doi.org/10.1177/0165025407077757. [Google Scholar]
- Loh WY. Classification and regression trees. Data Mining and Knowledge Discovery. 2011;1:14–23. [Google Scholar]
- McKnight I. Risk factors for the onset of eating disorders in adolescent girls: Results of the McKnight longitudinal risk factor study. American Journal of Psychiatry. 2003;160:248–254. doi: 10.1176/ajp.160.2.248. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Butler R, Palti H. Eating disturbances among adolescent girls: Evaluation of a school-based primary prevention program. Journal of Nutritional Education. 1995;27:24–31. [Google Scholar]
- Patton GC, Johnson-Sabine E, Wood K, Mann AH, Wakeling A. Abnormal eating attitudes in London school girls- a prospective epidemiological study: outcome at twelve month follow-up. Psychological Medicine. 1990;20:383–394. doi: 10.1017/s0033291700017700. [DOI] [PubMed] [Google Scholar]
- Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R. Onset of adolescent eating disorders: population based cohort study over 3 years. BMJ. 1999;318:765–768. doi: 10.1136/bmj.318.7186.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrobelli A, Faith MS, Allison DB, Gallagher D, Chiumello G, Heymsfield SB. Body mass index as a measure of adiposity among children and adolescents: A validation study. The Journal of Pediatrics. 1998;132:204–210. doi: 10.1016/s0022-3476(98)70433-0. [DOI] [PubMed] [Google Scholar]
- Radloff LS. A CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rohde P, Stice E, Marti N. Development and predictive effects of eating disorder risk factors during adolescence: Implications for prevention efforts. International Journal of Eating Disorders. 2015;48:187–198. doi: 10.1002/eat.22270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Gau J. Effectiveness trial of an indicated cognitive-behavioral group adolescent depression prevention program versus bibliotherapy and brochure control at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2015;83:736–747. doi: 10.1037/ccp0000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santonastaso P, Friederici S, Favaro A. Full and partial syndromes in eating disorders: A 1-year prospective study of risk factors among female students. Psychopathology. 1999;32:50–56. doi: 10.1159/000029067. [DOI] [PubMed] [Google Scholar]
- Stice E. A review of the evidence for a sociocultural model of bulimia nervosa and an exploration of the mechanisms of action. Clinical Psychology Review. 1994;14:633–661. [Google Scholar]
- Stice E, Bohon C. Eating Disorders. In: Beauchaine TP, Hinshaw SP, editors. Child and Adolescent Psychopathology. Hoboken, New Jersey: Wiley and Sons; 2013. pp. 715–738. [Google Scholar]
- Stice E, Davis K, Miller N, Marti CN. Fasting increases risk for onset of binge eating and bulimic pathology: A 5-year prospective study. Journal of Abnormal Psychology. 2008a;117:941–946. doi: 10.1037/a0013644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Gau J, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: Predictive specificity in high-risk adolescent females. Journal of Abnormal Psychology. 2017;126:38–51. doi: 10.1037/abn0000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Durant S. Risk factors for onset of eating disorders: Evidence of multiple risk pathways from an 8-year prospective study. Behaviour Research and Therapy. 2011a;49:622–627. doi: 10.1016/j.brat.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal of Abnormal Psychology. 2013;122:445–457. doi: 10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008b;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Presnell K, Gau J, Shaw H. Testing mediators of intervention effects in randomized controlled trials: An evaluation of two eating disorder prevention programs. Journal of Consulting and Clinical Psychology. 2007;75:20–32. doi: 10.1037/0022-006X.75.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Shaw H. Effect of a dissonance-based prevention program on risk for eating disorder onset in the context of eating disorder risk factors. Prevention Science. 2012;13:129–139. doi: 10.1007/s11121-011-0251-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Gau J. An effectiveness trial of a selected dissonance- based eating disorder prevention program for female high school students: Long-term effects. Journal of Consulting and Clinical Psychology. 2011b;79:500–508. doi: 10.1037/a0024351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Gau J. An experimental therapeutics test of whether adding dissonance-induction activities improves the effectiveness of a selected obesity and eating disorder prevention program. International Journal of Obesity. doi: 10.1038/ijo.2017.251. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Marti N. Efficacy trial of a selective prevention program targeting both eating disorders and obesity among female college students: 1- and 2-year follow-up effects. Journal of Consulting and Clinical Psychology. 2013b;81:183–189. doi: 10.1037/a0031235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Whitenton K. Risk factors for body dissatisfaction in adolescent girls: A longitudinal investigation. Developmental Psychology. 2002;38:669–678. doi: 10.1037//0012-1649.38.5.669. [DOI] [PubMed] [Google Scholar]
- Swanson S, Crow S, Le Grange D, Swendsen J, Merikangas K. Prevalence and correlates of eating disorders in adolescents: Results from the national comorbidity survey replication adolescent supplement. JAMA Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Strien T, Frijters JE, Van Staveren WA, Defares PB, Deurenberg P. The predictive validity of the Dutch Restrained Eating Scale. International Journal of Eating Disorders. 1986;5:747–755. [Google Scholar]
- Watson D, Clark LA. Affects separable and inseparable: On the hierarchical arrangement of the negative affects. Journal of Personality and Social Psychology. 1992;62:489–505. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Orvaschel H, Padian N. Children's symptom and social functioning self-report scales comparison of mothers' and children's reports. Journal of Nervous and Mental Disease. 1980;168:736–740. doi: 10.1097/00005053-198012000-00005. [DOI] [PubMed] [Google Scholar]
- Wilcox H, Field T, Prodromidis M, Scafidi F. Correlations between the BDI and CES-D in a sample of adolescent mothers. Adolescence. 1998;33:565–574. [PubMed] [Google Scholar]