Abstract
Most nursing programs lack curriculum on substance use. This project evaluated 3 didactic instructional methods for teaching baccalaureate nursing students about screening, brief intervention, and referral to treatment for substance use. In-person, asynchronous narrated slides and interactive online instructional methods were all effective in developing students’ competency; however, active learning methods (in-person and interactive online course) were more effective in changing students’ attitudes about their role in screening and intervening for drug use.
Keywords: brief intervention; nursing education; Screening, Brief Intervention, and Referral to Treatment (SBIRT); substance abuse; substance use disorders
Prelicensure nursing programs often inadequately prepare graduates to deal with the substance use issues they will encounter in their patients.1 In 2015, 66.7 million Americans reported binge alcohol use, 17.3 million reported heavy alcohol use in the past month, and 15.7 million had an alcohol use disorder.2 Moreover, diagnosable substance use disorders are as prevalent as other chronic, relapsing disorders such as diabetes and asthma.3 Yet, a review of 27 baccalaureate nursing programs in the northeast United States found minimal didactic and clinical instruction relating to substance use, with most programs reporting 1 to 5 hours of instruction.4 In particular, clinical skills to address substance use were taught infrequently, and only 37% of responding schools provided curriculum on counseling patients with substance use issues. Without adequate preparation, nurses are ill-equipped to address the prevalent substance use issues they will encounter in patients.
Screening, brief intervention, and referral to treatment (SBIRT) for substance use is an evidence-based practice that equips health professionals with a standardized mechanism for screening and intervening with patients using substances at risky or harmful levels.5 The screening process begins with a 2-item universal screen, followed by a targeted screen for patients who screen positive on the universal screen. Based on the results of the targeted screen, patients are categorized into low risk, risky, harmful, or severe risk zones, which, like other health assessments, allows providers to know what intervention is appropriate. Patients in the risky or harmful zones then receive a 5- to 15-minute motivational interviewing–based brief intervention designed to enhance their motivation to change their substance use. Patients who screen in the severe zone may have a substance use disorder and receive a referral to treatment to connect with specialty addiction care. Screening, brief intervention, and referral to treatment is being used across settings including primary care, emergency departments, women’s health clinics, schools, and mental health clinics and can be implemented by a variety of health professionals, including nurses.
Nurses are well positioned to address substance use with the SBIRT model,6 especially as behavioral health is integrated more routinely into health care. A number of projects have embedded SBIRT training into baccalaureate and graduate nursing education with positive outcomes, including high training satisfaction, increased knowledge, and improved attitudes, confidence, self-efficacy, and self-perceived competence toward addressing substance use.7-12 An SBIRT training initiative targeting family nurse practitioner students showed that students who reported higher levels of perceived competence posttraining were more likely to screen for substance use during their clinical practice, underscoring the importance of infusing this curriculum.8
After previous grants to train medical residents, in 2013, the Substance Abuse and Mental Health Services Administration (SAMHSA) began funding health professions training programs, including undergraduate and graduate nursing programs, to design and implement SBIRT training programs into health professions education. The University of Missouri-Kansas City (UMKC) SBIRT Training program was funded by SAMHSA to infuse SBIRT training into the BSN, advanced practice nursing, and masters of social work programs at the UMKC School of Nursing and Health Studies. The aims of the current study were to (1) determine whether BSN students can be prepared to competently deliver SBIRT and (2) compare methods in delivering SBIRT didactic instruction.
Online Teaching Strategies in Nursing Education
Nursing, like many other academic fields, has transitioned to offer online learning opportunities for students. Some common online teaching strategies in nursing education include Wikis, podcasts, video captures, video recordings of lectures, asynchronous narrated slides, and discussion boards.13 In addition, instructors use Web 2.0 teaching tools—such as asynchronous online modules, virtual role-playing, simulation, and online forums—that incorporate case studies and interactive exercises to promote learning.14-17 Case-based learning takes students through interactive patient case studies, allowing them to simultaneously learn and apply knowledge in realistic scenarios. In an effort to benchmark best practices in delivering nursing curriculum online, active learning was identified as a quality indicator of educational practices.18 Active learning means that the student is an active participant in the learning process, and applies course content to critical thinking exercises. Active learning contributes to students’ course outcomes, satisfaction, engagement, and deeper learning.18-20
Nursing Students’ Satisfaction, Knowledge, and Skills With Online Learning Strategies
Online or distance learning is a widely accepted instructional strategy, and students, including nursing students, have generally demonstrated high levels of satisfaction, gains in knowledge, and demonstration of skills. A systematic review of 9 randomized controlled studies found that distance learning in nursing education produced equal or superior gains in knowledge as compared with traditional classroom learning, as well as some improvement in nursing skill performance and generally high learner satisfaction.21 In a study of 35 RN-to-BSN students enrolled in a course using an online delivery format, video-recorded lectures, narrated slides, and discussion boards had the 3 highest mean ratings by students.13 However, students had a mean age of 35 years and may have been most familiar with traditional lecture delivery methods, leading to their preference for video-recorded lectures and narrated slides, which are most similar to a classroom lecture.
Another study of 83 graduate first-year preregistration nursing students used a blended approach—asynchronous online module plus a 90-minute practical clinical skills class—to deliver a clinical skills module.22 Students reported satisfaction with online learning for developing clinical skills and a preference for a blended approach that also included classroom learning. They found video clips containing demonstrations of clinical skills to be the most useful online learning approach and online readings to be the least useful. Another study of undergraduate nursing students found that case-based learning contributed to more consistent practice and improved patient assessment skills as compared with students who participated in a traditional lecture and discussion.23
UMKC-SBIRT Project Instructional Methods
The goal of the training project was to help students achieve competency in practicing SBIRT, including universal and targeted screening for substance use, delivering a brief negotiated interview, and referring patients to treatment when appropriate. Across 3 years, SBIRT education was integrated into the Management of Mental Health course for each consecutive junior year group of BSN students. Screening, brief intervention, and referral to treatment education included didactic instruction, role-play with classmates, standardized patient (SP) practice, and clinical experience to help students achieve competency. Didactic instruction covered what is SBIRT, screening for substance use, communication style (emphasizing motivational interviewing), brief negotiated interview model of a brief intervention, and referral to treatment. After didactic instruction, all students role-played with peers, practiced with 2 SPs, and implemented SBIRT in their clinical rotations (or role-played with peers if clinical sites did not allow).
Methods for delivering SBIRT didactic instruction varied across the 3 groups. In group 1, instruction was delivered in-person in the classroom using interactive learning strategies (multiple question-and-answer sections, paired exercises). In addition to the SBIRT content, this group also received instruction on the continuum of substance use and addiction as a chronic, relapsing brain disease. Role-play between students was conducted in class. Students then practiced with 2 SPs on separate dates 2 weeks apart and received written feedback after analyses of their audio-recorded sessions.
Group 2 included asynchronous, narrated slides. Students accessed the didactic instruction on SBIRT, as well as on the continuum of substance use and addiction as a chronic, relapsing brain disease, asynchronously via narrated slide presentations posted through the university’s online learning system. The slide presentations were the same as those used with the in-person group, but the instructor audio-recorded narration for each slide. Role-play practice was completed in class. Students then practiced with 2 SPs on the same date, with a faculty supervisor giving live feedback after the first encounter and written feedback after analyses of the second, audio-recorded encounter.
In the third group, the instruction was delivered via a 4-hour, asynchronous, interactive online course. The course covered the same SBIRT curriculum as the other 2 groups. The online course, available at www.sbirt.care, took learners on a primary care clinic staff orientation on SBIRT led by the nurse manager and accompanied by a nurse practitioner and a social worker. The course included interactive features such as case studies, quiz questions, and a situational branching scenario that allowed students to practice the brief intervention in incremental substeps and receive immediate feedback from a prerecorded patient and SBIRT coach. The course incorporated audio narration exploring common questions about SBIRT and a 4-part video series. After the online course, students role-played with peers in class. Students then practiced with 2 SPs on the same date, with a faculty supervisor giving live feedback after the first encounter and written feedback after analyses of the second, audio-recorded encounter.
Methods
Participants
Across 3 years (2014-2016), 256 BSN students were trained (in-person, 95; narrated slides, 99; online course, 62 [lower enrollment during 2016]). This included students in the regular and accelerated BSN tracks. Of the 256 total students, 238 completed both precourse and postcourse surveys (92.6% completion rate) and were included in the analysis. The in-person group had 92 students, the narrated slides group had 91 students, and the online course group had 55 students. Most students were white (78.6%), African American (13.9%), or Hispanic (12.2%) and female (81.5%).
Instruments
Students completed surveys before and immediately after SBIRT training. Surveys covered knowledge, attitudes, and training satisfaction. Posttraining skills were also assessed.
Knowledge about SBIRT was assessed with the SBIRT Knowledge Measure developed for this project by SBIRT teaching faculty. The 14 items of this scale are in a true/false and multiple-choice format and assess knowledge of screening (eg, how scores on the screening tools used in the project match to risk zones) and brief intervention (eg, steps of the brief negotiated interview, examples of motivational interviewing skills). A sum of the number of correct items (0-14) is used.
Attitudes about working with patients who use alcohol and drugs were assessed with the 30-item Alcohol and Alcohol Problems Perception Questionnaire (AAPPQ) and the 22-item Drug and Drug Problems Perception Questionnaire (DDPPQ).24,25 Items are scored on a 7-point Likert scale, with possible responses ranging from 1 (strongly disagree) to 7 (strongly agree), and subscales are constructed as the mean of the items in the scale. Higher scores indicate more positive attitudes. This study reports on 5 subscales with acceptable reliability: role adequacy (having adequate knowledge about working with patients who use substances), role legitimacy (feeling that it is appropriate to intervene with patients about their substance use), role support (support from colleagues to work with patients on substance issues), task specific self-esteem, and work satisfaction (all related specifically to patients who use substances). Coefficient αs for this sample ranged from .732 to .936 for the AAPPQ and from .734 to .944 for the DDPPQ.
Attitudes about counseling confidence were assessed with a 4-item Counseling Confidence subscale, adapted from Chun et al.26 Items ask about confidence for performing the aspects of SBIRT and are scored on a 4-point scale from 1 (not at all) to 4 (very). The mean of the items is used, and coefficient α for this sample was .836.
Training satisfaction was assessed with the Center for Substance Abuse Treatment Immediate Follow-up Training Satisfaction tool. Four items ask about satisfaction with the quality of the training, instruction, and materials, and 1 item asks about effectiveness in working in the topic area. Items are scored on a 5-point scale from 1 (very dissatisfied) to 5 (very satisfied). The mean of the items is used.
Skills to conduct a brief intervention with the SPs were assessed with the Brief Intervention Observation Sheet (BIOS) competency scale The BIOS includes a composite score of 10 items in a yes/no format that assessed completion of the steps of a brief intervention. A second score used 1 item to assess the overall motivational interviewing style used by the student during the brief intervention, rated on a 7-point scale from 1 (not at all) to 7 (very effectively). Only the scores from the second SP interaction, all of which were audio-recorded, were used in the analyses.
Procedures and Data Analysis
Surveys were administered at baseline and immediately after the training. Skills were assessed during interaction with an SP using a competency scale. Surveys were anonymous; students generated a personal code to match precourse and postcourse surveys and skills. These evaluation methodologies were approved by the university’s institutional review board. Data were entered into the statistical analysis program SPSS (version 23) (IBM Corp, Armonk, New York), and descriptive statistics were generated. Pretraining group equivalence (instructional design group) was tested via 1-way analyses of variance (ANOVAs) on knowledge and attitude scales. Effect of the training was assessed via repeated-measures ANOVAs with post hoc, Bonferroni-corrected, between-group t tests to assess posttraining knowledge and attitude differences among the instructional methods or by 1-way ANOVAs with post hoc, Bonferroni-corrected, between-group t tests for training satisfaction and skills.
Results
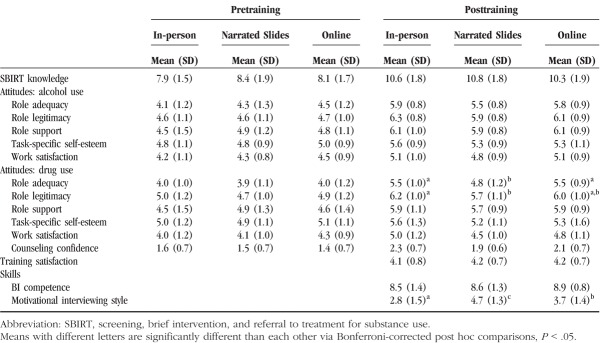
Results of the pretraining analyses of instructional design groups showed that all 3 groups were equivalent; there were no significant differences between the groups on knowledge or attitudes. The time effect for all repeated-measures ANOVAs was significant, Fs > 11.03, Ps < .001. All groups increased their knowledge, and their attitudes became more positive after training (Table). The Table shows the means and standard deviations results of post-hoc comparisons of post-training knowledge and attitudes per group. In addition, the Table shows the group means and standard deviations, as well as post-hoc comparisons for training satisfaction and skills post-training.The 3 groups had similar levels of knowledge of SBIRT and training satisfaction posttraining.
Table.
Comparison of 3 Instructional Methods for SBIRT
Regarding attitudes, there was a significant difference in drug-related role adequacy and role legitimacy posttraining between the groups. Post hoc comparisons showed significantly higher perceptions of role adequacy posttraining in the in-person and online groups than the narrated slides group. For drug role legitimacy, there were significantly higher perceptions of drug role legitimacy posttraining in the in-person than the narrated slides group, with the narrated slides and online groups being similar (Table).
Regarding SBIRT skills, there was a significant difference in motivational style during SP practice. The narrated slides group showed significantly higher motivational interviewing style than the online course group, which was significantly higher than the in-person group (Table).
Discussion
This study demonstrated that BSN students can be prepared to competently deliver SBIRT. Students educated using all 3 instructional methods increased their knowledge, scoring an average of 76% correct on the knowledge tool. Students’ attitudes toward working with patients who use alcohol or drugs became more positive, as did their confidence to provide counseling (brief intervention) for substance use. In addition, students across groups completed an average of 8.6 of 10 brief intervention skills, with a moderate degree (3.8/7) of motivational interviewing style.
The second goal of the study was to compare methods in delivering SBIRT didactic instruction. Results suggest that both in-person and online instructional methods can be effective in delivering substance use education to baccalaureate nursing students. No differences in knowledge acquisition, training satisfaction, or competency in delivering a brief intervention were found across the 3 instructional methods. However, there were a few differences on the other measures. Although attitudes were generally the same across didactic instructional methods, posttraining, the narrated slides group showed lower drug-related role adequacy than the in-person and online course groups and lower drug-related role legitimacy than the in-person group. The groups prepared using more active learning methods indicated that they had a better working knowledge of substance use and related problems and more right to ask patients about their substance use when necessary. Interestingly, the narrated slides group performed better than the other 2 groups in motivational style during the SP practice.
Nursing education, similar to many other fields, is increasingly delivered online, whether in a hybrid or fully online approach. Active learning is considered a quality indicator of online nursing education18 and can be used effectively through various e-learning strategies. In relation to active learning, the current study found that, generally, all 3 instructional methods produced similar results, except for 2 instances when the least interactive method (narrated slides) produced lower levels of attitude change compared with more interactive online or in-person approaches. The significance of attitude change, especially when involving substance use, should be considered when selecting an instructional method, as health care workers’ attitudes toward patients with substance use issues could affect the quality of care provided.27
It is important to balance an instructional method’s ease of delivery and time required for faculty to deliver substance use education with its outcomes on students’ knowledge, attitudes, and skills. Results of this evaluation suggest that an interactive online course produces similarly positive outcomes as in-person or recorded lecture (voice-over, PowerPoint). After the time-intensive process of developing an interactive online course, use of the finished product requires less faculty time to deliver and replicate across student cohorts. It is also a sustainable strategy for infusing substance use education in the case of faculty turnover or lack of faculty training on the content. Because curriculum on substance use is substantially lacking in most baccalaureate nursing programs,4 identifying and implementing sustainable instructional methods are essential.
Strengths and Limitations
One strength of this study was its demonstration that undergraduate nursing students can be prepared to competently deliver SBIRT in approximately 6 hours of coursework, including didactic instruction and practice with classmates and SPs. Another strength is that it demonstrated that an interactive online course was as effective as in-person education in changing students’ knowledge, attitudes, and skills.
One limitation of this study is that the sample included 3 consecutive years of BSN students (convenience sample), rather than random assignment of students to the 3 instructional methods. In addition, there were fewer students in the online interactive course group than the other 2 groups because of a change in program enrollment. In addition, it is possible that variability in how SPs portrayed their case scenarios contributed to differences in motivational style scores across the 3 groups (although most SP actors were retained across the 3 years, 2 from the in-person group did not continue).
Recommendations
Undergraduate nursing programs should equip students with the skills to address the substance use issues that they are likely to encounter in their clinical practice. Screening, brief intervention, and referral to treatment provides an evidence-based framework for doing so. After SBIRT training, Agley et al8 found that students who reported higher levels of perceived competence in delivering SBIRT were more likely to screen for substance use, the first step in addressing this prevalent public health concern. Screening, brief intervention, and referral to treatment curriculum that combines didactic instruction—whether in-person or in an interactive online format—with hands-on practice with classmates and SPs provides students with the necessary preparation to competently screen and intervene for substance use.
Footnotes
This work is supported by grant TI025355 from the Department of Health and Human Services, Substance Abuse and Mental Health Services Administration.
The authors declare no conflicts of interest.
Published ahead of print: August 15, 2017
References
- 1.Murphy-Parker D. Screening, brief intervention, and referral to treatment: a need for educational reform in nursing. Nurs Clin North Am. 2013;48(3):485-489. [DOI] [PubMed] [Google Scholar]
- 2.Center for Behavioral Health Statistics and Quality. Key Substance Use and Mental Health Indicators in the United States: Results From the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16-4984, NSDUH Series H-51). Rockville, MD: Substance Abuse and Mental Health Services Administration (SAMHSA); 2016. [Google Scholar]
- 3.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689-1695. [DOI] [PubMed] [Google Scholar]
- 4.Mollica MA, Hyman Z, Mann CM. Alcohol related content in undergraduate nursing curricula in the northeastern United States. J Psychosoc Nurs Ment Health Serv. 2011;49(6):22-31. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Planning and Implementing Screening and Brief Intervention for Risky Alcohol Use: A Step-by-Step Guide for Primary Care Practices. Atlanta, GA: CDC, National Center on Birth Defects and Developmental Disabilities; 2014. [Google Scholar]
- 6.Finnell DS, Nowzari S, Reimann B, Fischer L, Pace E, Goplerud E. Screening, brief intervention, and referral to treatment (SBIRT) as an integral part of nursing practice. Subst Abus. 2014;35(2):114-118. [DOI] [PubMed] [Google Scholar]
- 7.Kane I, Mitchell AM, Puskar KR, et al. Identifying at risk individuals for drug and alcohol dependence: teaching the competency to students in classroom and clinical settings. Nurse Educ. 2014;39(3):126-134. [DOI] [PubMed] [Google Scholar]
- 8.Agley J, McNelis AM, Carlson JM, et al. If you teach it, they will screen: advanced practice nursing students’ use of screening and brief intervention in the clinical setting. J Nurs Educ. 2016;55(4):231-235. [DOI] [PubMed] [Google Scholar]
- 9.Rassool GH, Rawaf S. Predictors of educational outcomes of undergraduate nursing students in alcohol and drug education. Nurse Educ Today. 2008;28(6):691-701. [DOI] [PubMed] [Google Scholar]
- 10.Tanner TB, Wilhelm SE, Rossie KM, Metcalf MP. Web-based SBIRT skills training for health professional students and primary care providers. Subst Abus. 2012;33(3):316-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vadlamudi RS, Adams S, Hogan B, Wu T, Wahid Z. Nurses’ attitudes, beliefs and confidence levels regarding care for those who abuse alcohol: impact of educational intervention. Nurse Educ Pract. 2008;8(4):290-298. [DOI] [PubMed] [Google Scholar]
- 12.O’May F, Gill J, McWhirter E, Kantartzis S, Rees C, Murray K. A teachable moment for the teachable moment? A prospective study to evaluate delivery of a workshop designed to increase knowledge and skills in relation to alcohol brief interventions (ABIs) amongst final year nursing and occupational therapy undergraduates. Nurse Educ Pract. 2016;20:45-53. [DOI] [PubMed] [Google Scholar]
- 13.Abell C, Williams D. Attitudes of RN-to-BSN students regarding teaching strategies utilized in online courses. Comput Inform Nurs. 2014;32(9):437-439. [DOI] [PubMed] [Google Scholar]
- 14.Sessoms D. Interactive instruction: creating interactive learning environments through tomorrow’s teachers. Int J Technol Teach Learn. 2008;4(2):86-96. [Google Scholar]
- 15.Baptiste D, Shaefer SJM. Online module to assure success as prelicensure nursing students’ transition to professional practice. Quarter Rev Dist Educ. 2015;16(4):1-5. [Google Scholar]
- 16.Oermann MH. Technology and teaching innovations in nursing education. Nurse Educ. 2015;40(2):55-56. [DOI] [PubMed] [Google Scholar]
- 17.Wilmont SS. Moving beyond PowerPoint: faculty innovators are taking off. AJN Report. 2016;116(1):19-20. [DOI] [PubMed] [Google Scholar]
- 18.Billings DM, Connors HR, Skiba DJ. Benchmarking best practices in web-based nursing courses. ANS Adv Nurs Sci. 2001;23(3):41-52. [DOI] [PubMed] [Google Scholar]
- 19.Stevenson EL, Gordon HA. Students as active learners and teaching partners in the clinical setting. Nurse Educ. 2014;39(2):52-53. [DOI] [PubMed] [Google Scholar]
- 20.Hampton D, Pearce PF. Student engagement in online nursing courses. Nurse Educ. 2016;41(6):294-298. [DOI] [PubMed] [Google Scholar]
- 21.Du S, Liu Z, Liu S, et al. Web-based distance learning for nurse education: a systematic review. Int Nurs Rev. 2013;60(2):167-177. [DOI] [PubMed] [Google Scholar]
- 22.Bloomfield JG, Jones A. Using e-learning to support clinical skills acquisition: exploring the experiences and perceptions of graduate first-year pre-registration nursing students—a mixed method study. Nurse Educ Today. 2013;33(12):1605-1611. [DOI] [PubMed] [Google Scholar]
- 23.Raurell-Torredà M, Olivet-Pujol J, Romero-Collado À, Malagon-Aguilera MC, Patiño-Masó J, Baltasar-Bagué A. Case-based learning and simulation: useful tools to enhance nurses’ education? Nonrandomized controlled trial. J Nurs Scholarsh. 2015;47(1):34-42. [DOI] [PubMed] [Google Scholar]
- 24.Watson H, Maclaren W, Shaw F, Nolan A. Measuring Staff Attitudes to People With Drug Problems: The Development of a Tool. Glasgow, Scotland: Scottish Executive Drug Misuse Research Programme; 2003. [Google Scholar]
- 25.Terhorst L, Gotham HJ, Puskar KR, et al. Factor structure of the Alcohol and Alcohol Problems Perception Questionnaire (AAPPQ) in a sample of baccalaureate nursing students. Res Nurs Health. 2013;36(4):412-422. [DOI] [PubMed] [Google Scholar]
- 26.Chun TH, Spirito A, Rakowski W, D’Onofrio G, Woolard RH. Beliefs and practices of pediatric emergency physicians and nurses regarding counseling alcohol-using adolescents. Pediatr Emerg Care. 2011;27(9):812-825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brener L, Von Hippel W, Kippax S, Preacher KJ. The role of physician and nurse attitudes in the health care of injecting drug users. Subst Use Misuse. 2010;45(7-8):1007-1018. [DOI] [PubMed] [Google Scholar]