Supplemental digital content is available in the text.
Key Words: Abdominal radical trachelectomy, Cervical cancer, Pregnancy
Abstract
Objectives
Cervical cancer is one of the most frequently diagnosed cancers in pregnancy. Our aim was to evaluate the safety and efficacy of abdominal radical trachelectomy (ART) for pregnant women with early-stage cervical cancer who strongly desire to preserve their pregnancies.
Methods/Materials
A retrospective observational study was performed for stage IB1 cervical cancer patients who underwent ART or radical hysterectomy (RH) at our hospital between February 2013 and June 2017. We compared differences in perioperative findings and oncologic outcomes among ART during pregnancy (ART-DP), ART, and RH groups.
Results
A total of 38 patients were included in this analysis. Six, 10, and 22 patients were assigned to the ART-DP, ART, and RH groups, respectively. There were no significant differences in the distribution of pathological TNM classifications, histology, tumor size, stromal invasion, and lymph-vascular space invasion among the 3 groups. The patients in the ART-DP group were younger than those in the RH group (P = 0.014). The ART-DP group was associated with more blood loss and prolonged surgery compared with the RH group (P = 0.017 and P = 0.014). The number of total lymph nodes in the ART-DP group was lower than that in the RH group (P = 0.036). However, there were no significant differences in age, surgical time, blood loss, or lymph node count between the ART-DP and ART groups. There were no significant differences in progression-free and overall survival times among the 3 groups, and no recurrence was observed in the ART-DP group.
Conclusions
Abdominal radical trachelectomy may be a tolerable treatment option for pregnant women with early-stage cervical cancer who strongly desire a baby.
Uterine cervical cancer is the third most common gynecological cancer and the fourth most frequent cause of cancer-related death among women worldwide.1 Almost all cervical cancers are caused by persistent infections with carcinogenic human papillomavirus (HPV),2 and effective prophylactic vaccines against representative oncogenic HPV types are available. However, HPV vaccination rates are lower compared with others, such as tetanus, diphtheria, and pertussis, in the United States.3 After the recommendation for the HPV vaccine was withdrawn by the Japanese government, the vaccination rate decreased to 1%.4–6 The cervical cancer screening rate for women is also lower in Japan compared with that in the United States.7 In particular, the screening rate for women aged 20 to 39 years is less than 20%. Consistent with these findings, the incidence of invasive cervical cancer among this 20- to 39-year age group has been increasing dramatically in recent years.8 As a result, invasive cervical cancer during pregnancy is not uncommon.
In Japan, the first visit to the obstetrics and gynecology outpatient department for pregnancy is 5 to 8 weeks of gestation, and a diagnosis of cervical cancer in pregnant women is usually determined at 7 to 10 weeks. Therefore, treatment decisions are usually required during the first trimester. For cervical cancer stage IA2 or higher during the first trimester of pregnancy, the standard treatment strategy is termination of the pregnancy and radical treatment.9 If patients have a strong desire to retain their pregnancies, some treatment options such as chemotherapy or radical trachelectomy (RT) during pregnancy can be considered.10 However, there is no standard treatment strategy for pregnant women with early-stage cervical cancer who strongly desire to preserve their pregnancies.11,12 An individualized treatment plan should be developed for each pregnant woman with early-stage cervical cancer.
Abdominal radical trachelectomy (ART) is one treatment option for early-stage cervical cancer during pregnancy.13,14 However, some guidelines do not recommend RT during pregnancy because of the limited evidence of its safety and effectiveness.11,12 On the other hand, the National Comprehensive Cancer Network guideline views RT during pregnancy more favorably, describing it as follows: RT with the preservation of pregnancy has been successfully performed in a few pregnant patients with early-stage cervical cancer. At this point, ART is still controversial as a treatment option, and more research is needed to generate evidence for the effectiveness of ART during pregnancy (ART-DP). Therefore, the aims of our study were to summarize 6 cases of patients with stage IB1 cervical cancer who underwent ART-DP in our hospital and to evaluate the safety and effectiveness of ART-DP by comparing clinicopathological characteristics among ART-DP, ART, and abdominal radical hysterectomy (RH) groups.
METHODS
A retrospective observational study for stage IB1 cervical cancer patients was performed. Clinicopathological data were collected from the records of 55 patients who underwent ART or abdominal RH for stage IB1 cervical cancer between February 2013 and January 2017. All patients received magnetic resonance (MR) imaging before radical surgery. Our criteria for ART and ART-DP are shown in Supplementary Tables 1, http://links.lww.com/IGC/A632 and 2, http://links.lww.com/IGC/A633.
Of 55 stage IB1 patients, 2 patients who underwent conversion to RH, 2 patients who underwent RH after termination of pregnancy, and 2 patients who received neoadjuvant chemotherapy before RH were excluded from this study. In addition, 11 patients who underwent RH for cervical cancer with a tumor larger than 2 cm based on preoperative MR imaging were also excluded to adjust for preoperative tumor size between ART and RH cases.
A total of 38 Japanese patients with stage IB1 cervical cancer were included in this study. We divided the 38 cases into 3 groups: ART-DP, ART, and RH. By comparing clinicopathological characteristics and prognosis among these 3 groups, we evaluated the safety and effectiveness of ART for pregnant women with early-stage cervical cancer.
Standard statistical tests including Fisher exact tests, Kruskal-Wallis tests (Dunn post hoc tests), and log-rank tests were used to analyze the clinicopathological data as appropriate. Analyses of clinicopathological data were conducted using R 3.3.3.15 A P value of less than 0.05 was considered statistically significant.
RESULTS
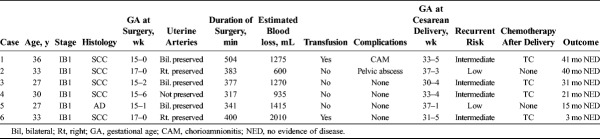
In 4 years, 6 pregnant women underwent RT for stage IB1 cervical cancer at our hospital. A summary of these 6 cases is shown in Table 1. Radical trachelectomy was performed at an average of 15 weeks and 6 days of gestation. Anesthetic management was achieved with the use of propofol16 in all cases. At least one uterine artery was preserved in 5 (83%) of 6 cases. The first 2 cases exhibited infectious complications after surgery. After modifying the closure method for the cervical canal during RT, no infectious complications were observed postoperatively. The first patient underwent emergent cesarean delivery because of premature rupture of membranes, and the other 5 patients underwent elective cesarean delivery. All patients delivered babies with no major anomalies, and their babies continue to grow and develop normally. Based on the recurrence risk, 4 patients received paclitaxel and carboplatin combination chemotherapy after delivery.
TABLE 1.
A summary of 6 cases in the ART-DP group
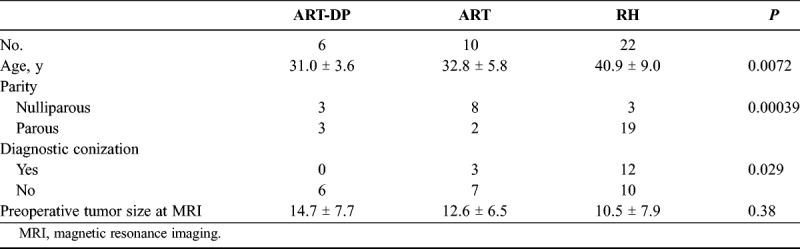
Next, to assess the safety and effectiveness of RT during pregnancy, a comparative analysis of clinicopathological characteristics among the ART-DP, ART, and RH groups was performed (Table 2). The age of onset in the ART-DP and ART groups was younger than that in the RH group (post hoc P = 0.0048 and P = 0.039), and nulliparous cases were more frequent in the ART-DP and ART groups compared with the RH group (P = 0.00039). Because preoperative tumor size was limited by the eligibility criteria, no significant difference in tumor size based on MR imaging was observed among the 3 groups.
TABLE 2.
Comparison of clinical characteristics among the 3 groups
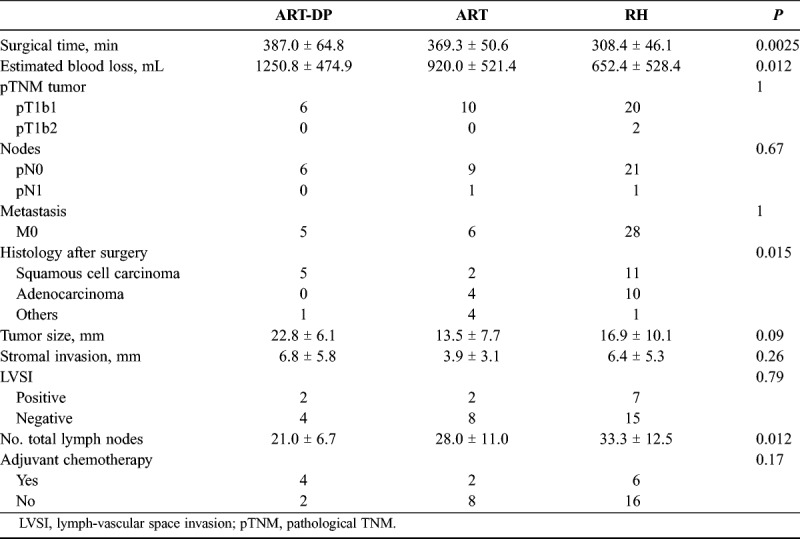
In terms of operative findings, surgical time and estimated blood loss were assessed among the 3 groups (Table 3). The ART-DP group was associated with prolonged surgery and more blood loss compared with the RH group (post hoc P = 0.0046 and P = 0.0058). However, no significant differences in surgical time and estimated blood loss between the ART-DP and ART groups were observed (post hoc P = 0.57 and P = 0.25). Preoperative autologous blood donation could not be prepared during the first trimester of pregnancy, and 2 patients (33.3%) in the ART-DP group required a blood transfusion. On the other hand, there were no significant differences in tumor size, stromal invasion, the frequency of lymph-vascular space invasion, and lymph node metastasis among the 3 groups. The number of dissected lymph nodes was lower in the ART-DP group compared with that in the RH group, but not compared with that in the ART group (post hoc P = 0.012 and P = 0.15).
TABLE 3.
Intraoperative and postoperative outcomes for patients with and without pregnancy who underwent ART or ARH
Adjuvant chemotherapy was performed based on recurrence risk. The frequency of adjuvant chemotherapy after delivery or radical surgery was not significantly different among the 3 groups. In terms of oncological results, no significant differences in progression-free and overall survival were observed among the 3 groups (Fig. 1). In particular, no recurrence was observed in the ART-DP and ART groups.
FIGURE 1.
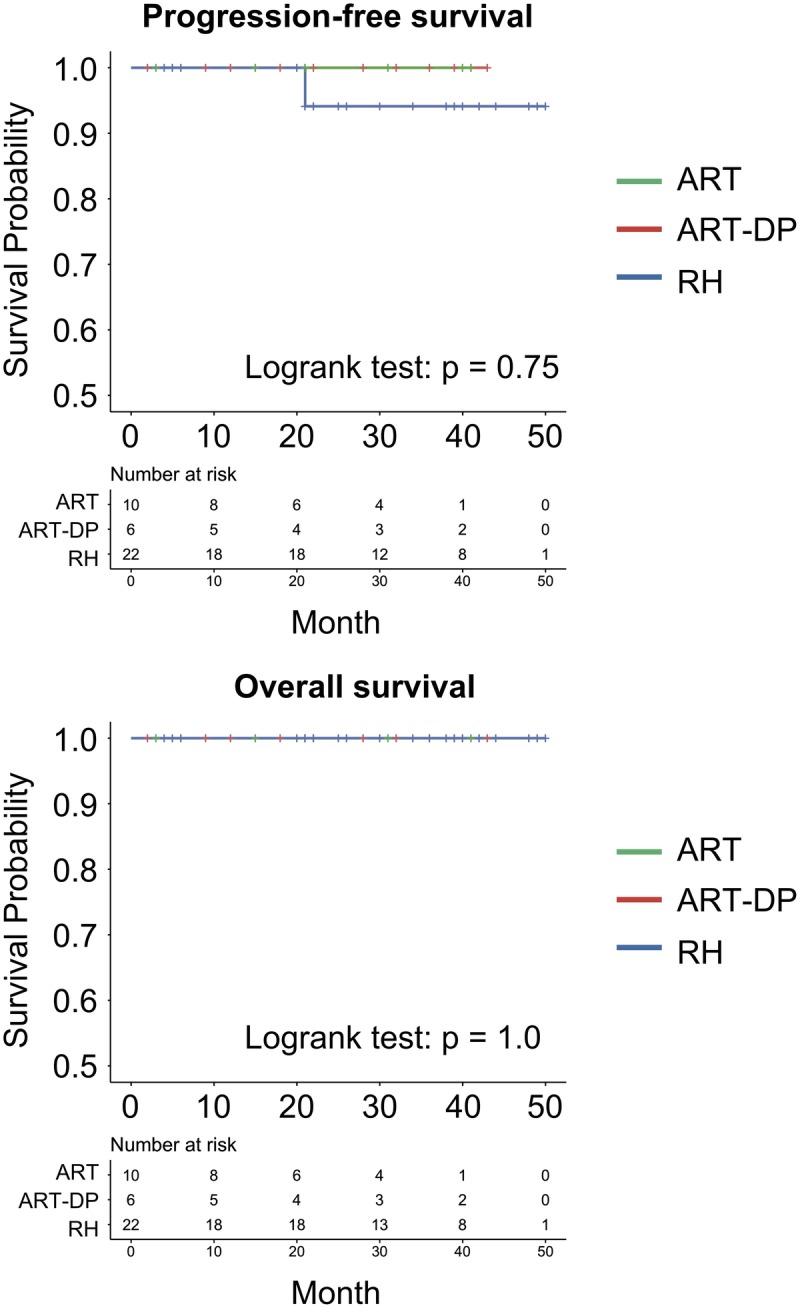
Oncologic outcomes among the ART-DP, ART, and RH groups. No significant differences in progression-free and overall survival among the 3 groups were observed (P = 0.75 and P = 1.0, respectively).
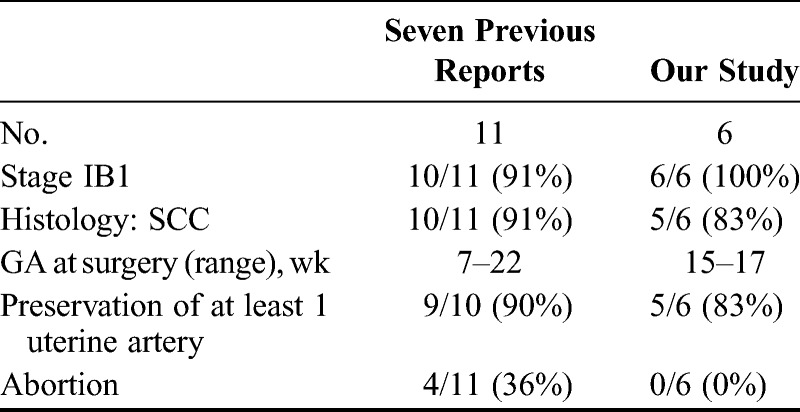
Finally, we compared clinicopathological characteristics between 11 patients with cervical cancer who underwent RT during pregnancy in 7 previous reports13,14,17–21 and our patients (Table 4). There were no significant differences in stage, histology, and the preservation rate of at least one uterine artery between the 7 previous reports and our study. Although we did not observe any spontaneous abortion cases, 4 of the 11 patients reported in the previous studies resulted in miscarriages. Of the 4 patients, 3 (75%) underwent RT before 14 weeks of gestation.
TABLE 4.
Comparison of clinical characteristics between previous reports and our study
DISCUSSION
This study revealed no obvious differences in oncological outcomes among the ART-DP, ART, and RH groups, and no differences in operative time and estimated blood loss between the ART-DP and ART groups. These findings indicate the safety and efficacy of RT for pregnant women with early-stage cervical cancer.
The management of pregnant women with early-stage cervical cancer who strongly desire to preserve their pregnancies depends on some factors: the stage of the disease, tumor size, nodal status, histologic type, and gestational age.9–12,14 Our results suggest that ART is a treatment option for stage IB1 cervical cancer with a tumor smaller than 2 cm before 18 weeks of gestation. However, based on the result that 4 of 11 ART cases (36%) reported in previous studies led to miscarriages, all guidelines do not necessarily recommend ART-DP. Three of 4 miscarriage cases (75%) underwent ART before 14 weeks of gestation, and the other miscarriage case received ART at 22 weeks of gestation with ligation of both uterine arteries, leading to intrauterine fetal death due to insufficient blood supply. Therefore, ART should be performed between 15 and 17 weeks of gestation per our criteria for ART-DP (Supplementary Table 2, http://links.lww.com/IGC/A633).
This study has some limitations that must be considered. First, the sample size may be too small to conduct statistical analyses. Second, the follow-up period may not have been long enough to assess oncological outcomes and children's growth and development. Therefore, we recognize that more cases and longer follow-ups are required to evaluate the efficacy and safety of RT during pregnancy. However, our sample size of 6 patients reflects the most cases studied in a single institute compared with previous reports (11 ART cases) to date,14 and we believe that our results are medically significant regarding ART-DP as a treatment option for pregnant women with early-stage cervical cancer.
As another limitation, we may need to consider the surgeon's expertise and skills in this study. A recent meta-analysis demonstrated that low-volume surgeon groups were significantly associated with high mortality and an increased rate of total operative complications compared with high-volume surgeon groups.22 Although specific surgeons performed RT for pregnant women, several surgeons performed RT or hysterectomy for nonpregnant women. To overcome these limitations, a multicenter prospective study on the safety and efficacy of RT for pregnant women with early-stage cervical cancer in which the surgical approach, the surgeon's expertise and skills, and the details of postoperative care are controlled by criteria is needed.
In conclusion, RT may be a tolerable treatment option for pregnant women with stage IB1 cervical cancer. Radical trachelectomy should be performed for appropriately selected patients with early-stage cervical cancer at 15 to 17 weeks of gestation at a specialized hospital.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.ijgc.net).
The authors declare no conflicts of interest.
REFERENCES
- 1.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. [DOI] [PubMed] [Google Scholar]
- 2.Steenbergen RD, Snijders PJ, Heideman DA, et al. Clinical implications of (epi)genetic changes in HPV-induced cervical precancerous lesions. Nat Rev Cancer. 2014;14:395–405. [DOI] [PubMed] [Google Scholar]
- 3.Reagan-Steiner S, Yankey D, Jeyarajah J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:850–858. [DOI] [PubMed] [Google Scholar]
- 4.Hanley SJ, Yoshioka E, Ito Y, et al. HPV vaccination crisis in Japan. Lancet. 2015;385:2571. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka Y, Ueda Y, Egawa-Takata T, et al. Outcomes for girls without HPV vaccination in Japan. Lancet Oncol. 2016;17:868–869. [DOI] [PubMed] [Google Scholar]
- 6.Yagi A, Ueda Y, Egawa-Takata T, et al. Realistic fear of cervical cancer risk in Japan depending on birth year. Hum Vaccin Immunother. 2017;13:1700–1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ueda Y, Sobue T, Morimoto A, et al. Evaluation of a free-coupon program for cervical cancer screening among the young: a nationally funded program conducted by a local government in Japan. J Epidemiol. 2015;25:50–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hori M, Matsuda T, Shibata A, et al. Cancer incidence and incidence rates in Japan in 2009: a study of 32 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 2015;45:884–891. [DOI] [PubMed] [Google Scholar]
- 9.Peccatori FA, Azim HA, Jr, Orecchia R, et al. Cancer, pregnancy and fertility: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(suppl 6):vi160–vi170. [DOI] [PubMed] [Google Scholar]
- 10.Fruscio R, Villa A, Chiari S, et al. Delivery delay with neoadjuvant chemotherapy for cervical cancer patients during pregnancy: a series of nine cases and literature review. Gynecol Oncol. 2012;126:192–197. [DOI] [PubMed] [Google Scholar]
- 11.Morice P, Narducci F, Mathevet P, et al. French recommendations on the management of invasive cervical cancer during pregnancy. Int J Gynecol Cancer. 2009;19:1638–1641. [DOI] [PubMed] [Google Scholar]
- 12.Amant F, Halaska MJ, Fumagalli M, et al. Gynecologic cancers in pregnancy: guidelines of a second international consensus meeting. Int J Gynecol Cancer. 2014;24:394–403. [DOI] [PubMed] [Google Scholar]
- 13.Enomoto T, Yoshino K, Fujita M, et al. A successful case of abdominal radical trachelectomy for cervical cancer during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2011;158:365–366. [DOI] [PubMed] [Google Scholar]
- 14.Capilna ME, Szabo B, Becsi J, et al. Radical trachelectomy performed during pregnancy: a review of the literature. Int J Gynecol Cancer. 2016;26:758–762. [DOI] [PubMed] [Google Scholar]
- 15.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 16.Terukina J, Takamatsu M, Enomoto T, et al. Anesthetic management of abdominal radical trachelectomy for uterine cervical cancer during pregnancy. J Anesth. 2017;31:467–471. [DOI] [PubMed] [Google Scholar]
- 17.Ungar L, Smith JR, Palfalvi L, et al. Abdominal radical trachelectomy during pregnancy to preserve pregnancy and fertility. Obstet Gynecol. 2006;108:811–814. [DOI] [PubMed] [Google Scholar]
- 18.Aoki Y, Inamine M, Ohishi S, et al. Radical abdominal trachelectomy for IB1 cervical cancer at 17 weeks of gestation: a case report and literature review. Case Rep Obstet Gynecol. 2014;2014:926502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karateke A, Kabaca C. Radical abdominal trachelectomy is a safe and fertility preserving option for women with early stage cervical cancer. Eur J Gynaecol Oncol. 2012;33:200–203. [PubMed] [Google Scholar]
- 20.Abu-Rustum NR, Tal MN, DeLair D, et al. Radical abdominal trachelectomy for stage IB1 cervical cancer at 15-week gestation. Gynecol Oncol. 2010;116:151–152. [DOI] [PubMed] [Google Scholar]
- 21.Mandic A, Novakovic P, Nincic D, et al. Radical abdominal trachelectomy in the 19th gestation week in patients with early invasive cervical carcinoma: case study and overview of literature. Am J Obstet Gynecol. 2009;201:e6–e8. [DOI] [PubMed] [Google Scholar]
- 22.Mowat A, Maher C, Ballard E. Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2016;215:21–33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.