Abstract
REVIVE SE (REVIVE) is a closed-ended, self-expanding stent retriever used in the RIVER JAPAN study. We present our early experience with REVIVE for revascularization of acute ischemic stroke (AIS) in patients who have failed or are ineligible for intravenous recombinant tissue plasminogen activator treatment. This prospective, single-arm, non-randomized, multicenter registry study followed up patients undergoing mechanical thrombectomy with REVIVE for 90 days. The primary endpoint was a post-procedure Thrombolysis in Cerebral Infarction (TICI) score ≥2a. Secondary endpoints were clot migration/embolization; recanalization without symptomatic intracranial hemorrhage (ICH) at 24 h; symptomatic ICH; good neurological outcome (modified Rankin Scale score ≤2 National Institute of Health Stroke Scale (NIHSS) score decrease ≥10) at day 90; device- or procedure-related serious adverse events (SAEs) and mortality at day 90. To confirm non-inferiority of REVIVE, results were compared with historical data of the Merci Retriever. About 49 patients were enrolled (median age 73 years; males 46.9%; middle cerebral artery (MCA) occlusion 83.7%; median NIHSS score 17). A post-procedure TICI score ≥2a was observed in 73.5% (36/49, 95% confidence interval [CI] 58.9–85.1) of patients. No post-procedural clot migration/embolization events occurred. Successful recanalization without symptomatic ICH was observed in 62.5% (30/48, 95% CI 47.4–76.0). The good neurological outcome was achieved in 66.7% (32/48) patients. Symptomatic ICH and device- or procedure-related SAEs were reported in 6.3% and 12.2% of patients, respectively. Two deaths were reported. REVIVE demonstrated equivalent efficacy and safety as the Merci Retriever. Results suggest that REVIVE is effective and safe in recanalizing occluded intracranial arteries in AIS.
Keywords: acute ischemic stroke, Japan, REVIVE, stent retriever, approving study
Introduction
Direct mechanical thrombectomy (MT) is an alternative option to intravenous recombinant tissue-type plasminogen activator (IV rtPA) for treatment of acute ischemic stroke (AIS).1) The first MT devices, Merci Retriever and Penumbra System were introduced in Japan in 2010 and 2011, respectively. Thereafter, open–ended, self-expanding stent retrievers such as Solitaire and Trevo Pro were approved for MT in Japan. The MT with stent retrievers in conjunction with rtPA vs. rtPA alone is associated with significant improvement of functional independence 90 days after AIS.2–6)
The REVIVE SE (REVIVE) device (Raynham, MA, USA, Codman Neuro/DePuy Synthes, Johnson and Johnson) is the first-generation, closed-ended, self-expanding stent retriever that was approved for use in Europe in August 2010. The second-generation REVIVE device was introduced in Japan and has an improved radial force compared with the original device. Initial study results demonstrated high recanalization rates in basilar, internal carotid artery (ICA), and MCA occlusions.7,8) Because the stent is compactly folded at the tip, severely tortuous cerebral arteries can be tracked, and the closed end may limit distal embolization during the MT procedure including clot retrieval.
Evidence supporting the use of any MT devices for stroke in Japanese patients is limited,9) as all these devices were introduced at around the same time in Japan. Here, we report results of the Reperfuse Ischemic Vessels with Endovascular Recanalization device in JAPAN (RIVER JAPAN) trial (NCT01895634), which was initiated to support approval of REVIVE from the Pharmaceuticals and Medical Device Agency (PMDA) in Japan at a time when no evidence of the clinical effectiveness of stent retrievers was available, and only the Merci Retriever and the Penumbra System were approved. The main objective of this prospective regulatory study with regulatory approval was to evaluate the effectiveness and safety of REVIVE for revascularization in AIS within 8 h of symptom onset in patients ineligible for treatment with IV rtPA or in whom IV rtPA was ineffective.
Methods
Study design
RIVER JAPAN was a prospective, single-arm, non-randomized, observational, multicenter registry study conducted at nine sites in Japan between June 12, 2013 (date of first signed consent form) and September 18, 2014 (last patient last visit). Eligible patients underwent MT using REVIVE (Lot: T10000) and were followed up for 90 days post-procedure. According to the principle, up to three passes of MT with REVIVE were attempted; further treatment with any approved modality, including other MT devices and pharmacological fibrinolysis was based on physician discretion during the procedure. The study was approved by the Institutional Review Board, was conducted in accordance with the Declaration of Helsinki, and is consistent with the International Conference on Harmonization Guideline for Good Clinical Practice. All patients or their representatives provided written informed consent before enrollment.
Population
Patients aged 20–85 years who had AIS within 8 h of onset (based on current approval of MT devices in Japan) at the start of procedure, or had failed or were not suitable for IV rtPA therapy, were eligible. Additional inclusion criteria were clinical signs and symptoms consistent with occlusion of segments M1 or M2 of the MCA, basilar, or vertebral artery, or intracranial segment of the ICA confirmed by angiography; Thrombolysis in Cerebral Infarction (TICI) score of 0 or 1; National Institute of Health Stroke Scale (NIHSS) score of 8–30; and modified Rankin Scale (mRS) score of 0–2 before onset. Patients with ICA dissection, angiitis, tortuosity or stenosis (>50%) of artery impeding catheter delivery to the target site, acute intracranial hemorrhage (ICH) or >2 major occluded arteries were excluded.
Efficacy endpoints
The primary endpoint was the ability of REVIVE to restore partial or total revascularization (TICI 2a or better) immediately post-procedure. Secondary endpoints included the proportion of patients with clot migration/embolization immediately post-procedure; successful recanalization within three passes without symptomatic ICH at 24 h (assessed by an independent core laboratory reader, Toranomon Hospital, 2-2-2, Toranomon, Minato-ku, Tokyo 105-8470); achievement of good neurological outcome (mRS score ≤2 or NIHSS score decrease of ≥10), and neurological outcome (mRS score, NIHSS score, Barthel Index [BI] score) at follow-up day 90; assessment of symptomatic/asymptomatic ICH at 24 h post-procedure; incidence of device-related or procedure-related serious adverse events (SAEs) at day 90; and mortality rates at day 90. Exploratory subgroup analysis included evaluation of successful recanalization (TICI score ≥2a) immediately post-procedure and at final angiogram (which included additional treatment with other devices) in patients with and without use of rtPA in patients with MCA (M1/M2) occlusion.
Procedure
Neurointerventionalists underwent a mandatory study-specific training program for the first clinical use of REVIVE to meet the criteria for using MT devices established by the Japan Stroke Society, Japan Neurosurgical Society, and Japanese Society for Neuroendovascular Therapy.10) After angiographic assessment, MT with REVIVE was initiated according to instructions for use with anticoagulation per institutional protocol. The first patient treated by each physician with the study device was considered a roll-in case; thereafter, all patients were considered non-roll-in. Use of concomitant medications was permitted. After achieving maximal TICI flow, the device was removed. In case of device failure, provisions were made to attempt the procedure with a second device, without use of accessory devices.
Efficacy assessments
Pre-procedure assessments included imaging (CT, angiography, or MRI), neurological evaluation (mRS, NIHSS, BI), and laboratory tests (PTT/activated PTT [aPTT], INR, platelet count, blood glucose). Thereafter, procedural parameters were assessed and intra- and immediate post-procedural imaging was performed. The TICI scores were assessed during and post-procedure. Follow-up evaluations included imaging and NIHSS score at 24 h and neurological assessments at discharge and at 30 and 90 days post-procedure. Day-30 and day-90 mRS and BI assessments were completed at the follow-up visit or via telephone. Evaluations were repeated at any time during the 90-day follow-up period based on investigator discretion.
Safety
Adverse events (AEs) were assessed for seriousness and relationship to the device, procedure, or both by the investigator and partly by an independent safety committee. Recanalization, clot migration/embolization, and ICH were assessed using CT, MRI, or angiographic images by an investigator and a core laboratory independent from the study sites.
Statistical analysis
Effectiveness analyses were performed using the per-protocol (PP) population, which comprised patients from the safety analysis set who fulfilled the study criteria without major protocol deviations. The safety analysis population included patients in whom the REVIVE procedure was attempted. Safety analyses were performed using the safety analysis set (SAS). Descriptive data analysis was performed using SAS version 9.2 (SAS Institute). For ordinal and continuous variables, descriptive results included number of patients, mean ± standard deviation (SD), median (minimum, maximum), etc. If necessary, the two-sided 95% CI of the mean value was calculated. Categorical variables are presented by percent, along with numerator and denominator. If necessary, the two-sided 95% CI of the rate was calculated.
To confirm non-inferiority of REVIVE vs. the Merci Retriever, results were compared with historical data from the Mechanical Embolus Removal in Cerebral Ischemia (MERCI)11) and Multi-MERCI12) trials. Therefore, the study’s threshold success rate was considered to be 50%, with an assumed 80% success rate of REVIVE vs. the historical Merci Retriever rate of approximately 50%. With an exact binomial test of superiority and a one-sided alpha of 0.025, power is 96.5% for 39 patients. Considering a drop-out rate of 20%, ≥50 patients needed to be enrolled. The null and alternative hypotheses are defined with n = REVIVE success rate: null hypothesis H0: π = 0.5; alternative hypothesis H1: π > 0.5. The power is the sum of all probability that the lower limit of 95% CI exceeds the threshold success rate of 50%. The SAS 9.2 POWER procedure ONESAMPLEFREQ method was used for the power calculation.
Results
Demographics and baseline characteristics
A total of 56 patients were screened, and 49 were enrolled (intention-to-treat [ITT] population). No patients were excluded from the PP or safety populations. Median age was 73 years (range 25–85 years), and 46.9% (23/49) were male. More patients (83.7% [41/49]) had MCA (M1/M2) occlusion, with median baseline NIHSS score of 17 (range 8–29) (Table 1). About 47 patients completed the 30-day follow-up (two deaths were reported) and 46 completed the 90-day follow-up (one additional patient withdrew informed consent).
Table 1.
Summary of demographics and baseline characteristics
| Patient characteristics | N = 49 |
|---|---|
| Sex, % (n) | |
| Male/female | 46.9 (23)/53.1 (26) |
| Age, years | |
| Mean ± SD | 70.6 ± 10.7 |
| Median (range) | 73.0 (25–85) |
| <70, % (n) | 40.8 (20) |
| ≥70, % (n) | 59.2 (29) |
| Primary disease, % (n) | |
| Acute ischemic stroke | 100.0 (49) |
| Medical history, % (n) | |
| No/yes | 89.8 (44)/10.2 (5) |
| Surgical history, % (n) | |
| No/yes | 81.6 (40)/18.4 (9) |
| Concomitant medication, % (n) | |
| No/yes | 2.0 (1)/98.0 (48) |
| Occluded hemisphere (N = 48), % (n) | |
| Left/right | 41.7 (20)/58.3 (28) |
| Target occlusion,a % (n) | |
| MCA (M1/M2) | 83.7 (41) |
| BA | 2.0 (1) |
| VA | 0.0 (0) |
| ICA | 14.3 (7) |
| Other | 0.0 (0) |
| Diameter of artery distal, mm | |
| Mean ± SD | 1.90 ± 0.40 |
| Median (range) | 1.80 (1.3–2.9) |
| Proximal to occlusion, mm | |
| Mean ± SD | 2.40 ± 0.60 |
| Median (range) | 2.40 (1.1–3.9) |
| Length of occlusion, mmb | |
| Mean ± SD | 13.80 ± 8.19 |
| Median (range) | 11.80 (1.5–40.8) |
| TICI score, pre-procedure, % (n) | |
| 0 | 89.8 (44) |
| 1 | 10.2 (5) |
| ≥2a | 0.0 (0) |
| Prior IV tPA, % (n) | |
| No/yes | 20.4 (10)/79.6 (39) |
| rtPA dose, mgc | |
| Mean ± SD | 34.42 ± 8.19 |
| Median (range) | 32.40 (19.2–57.0) |
| rtPA duration, minc | |
| Mean ± SD | 60.7 ± 4.0 |
| Median (range) | 60.0 (50–73) |
| mRS score, before onset, % (n) | |
| 0 | 87.8 (43) |
| 1 | 6.1 (3) |
| 2 | 6.1 (3) |
| ≥3 | 0.0 (0) |
| Baseline NIHSS score | |
| Mean ± SD | 17.9 ± 6.0 |
| Median (range) | 17 (8–29) |
| ≤17, % (n) | 53.1 (26) |
| >17, % (n) | 46.9 (23) |
| Baseline BI score | |
| Mean ± SD | 99.9 ± 0.7 |
| Median (range) | 100.0 (95–100) |
| ASPECTS | |
| Mean ± SD | 8.9 ± 1.5 |
| Median (range) | 9 (5–10) |
| DWI-ASPECTS | |
| Mean ± SD | 7.2 ± 2.3 |
| Median (range) | 7 (2–11) |
| PTT, secd | |
| Mean ± SD | 12.00 ± 0.57 |
| Median (range) | 12.00 (11.6–12.4) |
| aPTT, sece | |
| Mean ± SD | 28.81 ± 6.34 |
| Median (range) | 27.75 (22.3–55.1) |
| INR | |
| Mean ± SD | 1.122 ± 0.281 |
| Median (range) | 1.040 (0.86–2.31) |
| Platelets, × 104/μL | |
| Mean ± SD | 21.28 ± 6.57 |
| Median (range) | 20.30 (9.4–37.5) |
| Blood glucose, mg/dL | |
| Mean ± SD | 153.20 ± 64.32 |
| Median (range) | 126.00 (89.0–303.0) |
| Roll-in/non-roll-in, % (n) | |
| Roll-in | 38.8 (19) |
| Non-roll-in | 61.2 (30) |
In case multiple affected arteries are reported per subject, proximal artery will be prioritized and counted as a single lesion,
n = 47,
n = 39,
n = 2,
n = 48, aPTT: activated partial thromboplastin time, ASPECTS: Alberta Stroke Program Early CT Score, BA: basilar artery, BI: Barthel Index, DWI-ASPECTS: diffusion-weighted imaging ASPECTS, ICA: internal carotid artery, IV: intravenous, INR: international normalized ratio, MCA: middle cerebral artery, mRS: modified Rankin Scale, NIHSS: National Institute of Health Stroke Scale, PTT: partial thromboplastin time, rtPA: recombinant tissue plasminogen activator, SD: standard deviation, TICI: Thrombolysis In Cerebral Infarction Scale, VA: vertebral artery.
Procedural parameters
Median time from symptom onset to REVIVE insertion was 230 min (approximately 3.8 h, range 133–458 min) and median time of REVIVE use was 34 min (range 7–128 min) (Table 2). Mean (± SD) number of passes with REVIVE was 2.2 ± 1.2, and only one patient received two REVIVE devices. Additional procedures with other devices were required in 38.8% (19/49) of patients.
Table 2.
Procedural parameters
| Procedural parameters | |
|---|---|
| Time from symptom onset to introduction of study device, min | |
| Mean ± SD | 258.3 ± 83.2 |
| Median (range) | 230.0 (133–458) |
| Time from symptom onset to final angiogram, min | |
| Mean ± SD | 322.4 ± 95.9 |
| Median (range) | 307.0 (176–554) |
| Time study device was used, min | |
| Mean ± SD | 37.7 ± 27.2 |
| Median (range) | 34.0 (7–128) |
| Units of study device used (N = 49), % (n) | |
| 1 | 98.0 (48) |
| 2 | 2.0 (1) |
| 3 | 0.0 (0) |
| 4 | 0.0 (0) |
| Number of passes (N = 49) | |
| Mean ± SD | 2.2 ± 1.2 |
| Median (range) | 2.0 (1–5) |
| 1 | 38.8 (19) |
| 2 | 16.3 (8) |
| 3 | 34.7 (17) |
| 4 | 2.0 (1) |
| 5 | 8.2 (4) |
| ≥6 | 0.0 (0) |
| Additional procedure (N = 49), % (n) | |
| No/yes | 61.2 (30)/38.8 (19) |
| Merci Retriever (N = 19) | 10.5 (2) |
| Penumbra (N = 19 ) | 57.9 (11) |
| Other (N = 19) | 31.6 (6) |
SD: standard deviation.
Primary endpoint
Recanalization (TICI score ≥2a) was observed immediately post-procedure with REVIVE in 73.5% (36/49, 95% CI 58.9–85.1) of patients.
Secondary effectiveness endpoints
No post-procedural clot migration/embolization was reported with REVIVE immediately after the procedure. However, clot migration/embolization was observed in 4.1% (2/49) of patients at the final angiogram, who had both had additional treatment with the Penumbra system.
Successful recanalization without symptomatic ICH at 24 h was observed in 62.5% of patients (30/48, 95% CI 47.4–76.0) within three passes.
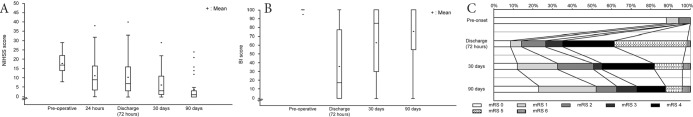
A gradual increase in the percentage of patients with good neurological outcome (mRS ≤ 2 or decrease in NIHSS of ≥10) was observed over time, almost doubling between 24 h and 90-days post-procedure: 37.5% (18/48) at 24 h, 51.0% (25/49) at discharge/72 h, 63.3% (31/49) at 30-day follow-up, and 66.7% (32/48) at 90-day follow-up. Similarly, a gradual decrease in post-procedural mean total NIHSS score was observed over time, decreasing to about one-fifth of the initial score by 90-days post-procedure: pre-procedure, 17.9 ± 6.0; at 24 h, 11.2 ± 8.8; at discharge/72 h, 10.4 ± 9.8; at 30-day follow-up, 6.2 ± 7.1; at 90-day follow-up, 3.8 ± 6.5 (Fig. 1A). Mean total BI scores were 99.9 ± 0.7 pre-procedure (pre-ictus); 35.8 ± 39.3 at discharge/72 h; 63.2 ± 39.4 at 30-day follow-up; and 75.4 ± 37.2 at 90-day follow-up (Fig. 1B). mRS 0–2 scores over time were 100.0% (49/49) pre-procedure (pre-ictus); 26.5% (13/49) at discharge/72 h, 51.0% (25/49) at 30-day follow-up, and 62.5% (30/48) at 90-day follow-up (Fig. 1C).
Fig. 1.
Neurological outcome over the study period: (A) NIHSS score, (B) BI score, and (C) mRS score over the study period. BI: Barthel Index, mRS: modified Rankin Scale, NIHSS: National Institute of Health Stroke Scale.
According to the core laboratory’s assessment, recanalization (TICI score ≥2a) was observed in 63.3% (31/49, 95% CI 48.3–76.6) of patients immediately post-procedure and 83.7% (41/49, 95% CI 70.3–92.7) of patients at final angiogram.
Exploratory subgroup analysis
Recanalization (TICI score ≥2a) was observed immediately post-procedure with REVIVE in 74.4% of patients (29/39, 95% CI 57.9–87.0) with rtPA, vs. 70.0% (7/10, 95% CI 34.8–93.3) without rtPA. At final angiogram, which included those with additional treatment, recanalization was observed in 91.8% of patients (45/49, 95% CI 80.4–97.7): with rtPA, 92.3% (36/39, 95% CI 79.1–98.4); without rtPA, 90.0% (9/10, 95% CI 55.5–99.7). Recanalization of MCA (M1/M2) was observed immediately post-procedure in 78.0% (32/41, 95% CI 62.4–89.4) and 95.1% (39/41, 95% CI 83.5–99.4) of patients at final angiogram. Recanalization was observed immediately post-procedure in 68.4% (13/19, 95% CI 43.4–87.4) in the roll-in group vs. 76.7% (23/30, 95% CI 57.7–90.1) in the non-roll-in group, and at final angiogram in 89.5% (17/19, 95% CI 66.9–98.7) in the roll-in group vs. 93.3% (28/30, 95% CI 77.9–99.2) in the non-roll-in group.
Safety
ICH was observed at 24 h post-procedure in 31.3% of patients (15/48, 95% CI 18.7– 46.3): with rtPA, 23.7% (9/38, 95% CI 11.4–40.2); without rtPA, 60.0% (6/10, 95% CI 26.2–87.8). Of the 15 patients, three (with rtPA) had symptomatic and 12 had asymptomatic (six with and six without rtPA) ICH.
Overall incidence of AEs, including procedure or device non-related event; for example, fever, headache, and other common symptom, was 95.9% (47/49, 95% CI 86.0–99.5). The most frequent device-related AEs were ICH (18.4% [9/49]), followed by intraoperative cerebral artery occlusion (12.2% [6/49]), and subarachnoid hemorrhage (12.2% [6/49]). The most frequent procedure-related AE was ICH (18.4% [9/49]) followed by intraoperative cerebral artery occlusion (14.3% [7/49]) and subarachnoid hemorrhage (12.2% [6/49]).
At 90-day follow-up, the incidence of SAEs was 32.7% (16/49, 95% CI 19.9–47.5). The most frequent system/organ class of SAEs was nervous system disorders (20.4% [10/49]), and the most frequent term of SAE was cerebral infarction (8.2% [4/49]). Among the SAEs, seven were considered device- or procedure-related and occurred in six patients; four were considered device-related, and six were considered procedure-related.
In total, 2 (4.1%) deaths were reported during the study: one within 24 h due to worsening of ischemic stroke (not considered device- or procedure-related), and one within 4 days due to non-occlusive mesenteric ischemia (considered procedure-related). Device malfunction was reported in 26.5% of patients (13/49, 95% CI 14.9–41.1), of which 10.2% (5/49, 95% CI 3.4–22.2) were considered device-related.
Discussion
In contrast to Europe and the United States,3,4,6) MT using stent retrievers is new in Japan, and evidence supporting use in the Japanese population is limited.9) The RIVER JAPAN study was a regulatory study for PMDA approval of REVIVE, and designed to show non-inferiority to MERCI11) and Multi-MERCI12) trials. Thus, primary efficacy endpoint of RIVER JAPANA is recanalization (TICI score ≥2a). At the beginning of the RIVER JAPAN study, Solitaire FR and Trevo Pro were not approved in Japan; however, during the study, both were approved without regulatory studies, based on the evidence of the SWIFT13) and TREVO II14) studies, respectively. Furthermore, during PMDA review for REVIVE approval, five randomized controlled trials (RCTs) were published and reliable evidence for MT using a stent retriever was established.2–6) The results of RIVER JAPAN showed equivalent efficacy and safety to the endovascular treatment group of these RCTs (Table 3), suggesting that REVIVE could deliver a similar clinical outcome to other approved MT devices in Japan. For this comparison, we use same criteria of recanalization (TICI score ≥2b).
Table 3.
Comparison with endovascular arm of five randomized studies
| Parameter | Randomized study | |||||
|---|---|---|---|---|---|---|
| MR CLEAN2) | REVASCAT3) | ESCAPE4) | EXTEND-IA5) | SWIFT-PRIME6) | RIVER JAPAN | |
| N | 233 | 103 | 165 | 35 | 98 | 49 |
| Age, years (mean) | 65.8* | 65.7 | 7* | 68.6 | 65.0 | 70.6 |
| NIHSS (median) | 17 | 17 | 16 | 17 | 17 | 17 |
| ASPECTS (median) | 9 | 7 | 9 | – | 9 | 9 |
| IV rtPA | 85% | 68% | 73% | 100% | 100% | 79.6% |
| Stent used | 97% | 100% | 86.1% | 81.8% | 100% | 100% |
| ICA | 25.7% | 25.5% | 27.6% | 31% | 18% | 14.3% |
| TICI 2b/3 | 59% | 65.7% | 72.4% | 86% | 88% | 67.3% |
| mRS 0–2 at day 90 | 32.6% | 43.7% | 53.0% | 71% | 60.2% | 62.5% |
| sICH | 7.7% | 4.9% | 3.6% | 0% | 0% | 6.3% |
| Mortality | 21% | 18.4% | 10.4% | 9% | 9% | 4.1% |
Median, ASPECTS: Alberta Stroke Program Early CT Score, ICA: internal carotid artery, IV: intravenous, mRS: modified Rankin Scale, NIHSS: National Institute of Health Stroke Scale, rtPA: recombinant tissue plasminogen activator, sICH: symptomatic intracranial hemorrhage, TICI: Thrombolysis In Cerebral Infarction Scale.
RIVER JAPAN study presents the early experience using REVIVE for treatment of AIS. This prospective, non-randomized, observational, multicenter registry study did not include a comparison arm(s). Yet, because of the importance of understanding the effectiveness and safety of REVIVE vs. other devices, comparison to historical results from trials evaluating other devices is reasonable. However, the RIVER JAPAN study was originally designed to compare a stent retriever with the MERCI device and conducted as regulatory study, comparisons should be considered with caution, given differences in study designs, investigator experience, sample sizes, sites, and accessibility of occlusion, and ethnicity.
Treatment with REVIVE restored blood flow (TICI score ≥2a) in 73.5% of patients, and the lower limit of the 95% CI (58.9%) was above the 50% threshold for success. Restoration of blood flow was marginally higher (74.4%) with than without (70.0%) use of rtPA. Overall, recanalization was achieved in 91.8% of patients, including those who had additional treatment, at the final angiogram. Core laboratory assessment rates were lower than those observed by site investigators. Recanalization rates immediately post-procedure improved with experience, increasing from 68.4% (during roll-in) to 76.7% (after roll-in). Reperfusion rates reported for the newer stent retrievers in non-Japanese patients (TICI 2 or 3: Trevo Pro 86% to 93%14–16) and Solitaire 88.8%17)) have improved in comparison to the Merci Retriever (Thrombolysis in Myocardial Infarction [TIMI] 2 or 3: MERCI 48.2%11) and Multi-MERCI 55%12)) and the Penumbra System (TIMI 2 or 3: 81.6%).18) Overall, stent retrievers have demonstrated improved recanalization rates and clinical outcome compared to the Merci Retriever. A significant difference in successful recanalization (TICI score of 2b or 3) was noted between stent retrievers (Trevo and Solitaire: 82%) and Merci Retrievers (62%) in patients with large cerebral artery occlusion (P = 0.016).19)
Neurological outcome (mRS 0–2) after treatment with REVIVE may be considered significantly better than after treatment with the Merci Retriever because the lower limit of the 95% CI (47.4) for REVIVE was higher than the upper limit of the 95% CI (44) for the Merci Retriever. The proportion of patients with mRS 0–2 was 62.5% (30/48, 95% CI 47.4–76.0) at the 90-day follow-up in RIVER JAPAN; 27.7% (36/130) in MERCI; 36% (59/164, 95% CI 29–44) in Multi-MERCI; 58–71% with Solitaire5,6,13); 40–55% with Trevo Pro14–16); and 25–40% with Penumbra.20,21)
No clot migration/embolization was reported post-procedure with REVIVE. Distal embolization in a previously uninvolved artery was reported in three cases in the MERCI11) and one case in the Multi-MERCI12) studies, as well as with newer open–ended stent retrievers (Solitaire, 5–18.2%).5,22,23)
The incidence of symptomatic ICH (6.3%) in RIVER JAPAN was similar to that reported in the MERCI (7.8%)11) and Multi-MERCI (9.8%)12) studies: Solitaire (0–20%),3,6,7,23–26) and Trevo Pro (5–12%).15,16,27) Similarly, asymptomatic ICH was observed in 25% of patients (12/48, 95% CI 13.6–39.6); MERCI 27.7%,11) Multi-MERCI 30.5%,12) Solitaire 16.5–40%,3,23,25) and Trevo Pro 41%.14) The number of deaths (2 [4.1%]) reported at 90-day follow-up in RIVER JAPAN was considerably lower than that reported in MERCI (43.5%)11) and Multi-MERCI (34%)12) studies: Solitaire 6.9–30%,3,6,7,13,17,23–26) Trevo Pro 20–33%,14–16,27,28) Penumbra, 24–32%.20,21,29) These results were equivalent from other studies of mechanical thrombectomy.
The incidence of device-related or procedure-related SAEs at 90-day follow-up was 12.2% (6/49, 95% CI 4.6–24.8). Among the SAEs, seven were considered device- or procedure-related in six patients; four were considered device-related; and six were considered procedure-related: MERCI (procedure, 7.1%; device, 4.3%)11) and Multi-MERCI (procedure, 5.5%; device, 2.4%)12) studies; Solitaire (procedure, 5.4–14%; device, 2.5–9%)13,24); and Trevo Pro (procedure, 8–15%; device, 5%).14,15,28)
Limitations of the study include its small sample size, non-randomized study design, and absence of direct comparison with other devices or treatment regimens. Neurointerventionalists were trained and needed to fulfill the criteria for performance and training standards for endovascular ischemic stroke treatment in Japan.10,30) Despite these limitations, results of RIVER JAPAN demonstrate the closed-ended, stent-based design of REVIVE enables quick restoration of blood flow past the occluding thrombus during the procedure, as well as safe clot retrieval. The basket should be able to open a channel and circumferentially displace the thrombus for immediate restoration of blood flow and improve access to fibrinolytic agents, while the closed end should provide better protection from distal embolization before clot retrieval. The range of effectiveness and safety outcomes observed in literature suggests that further studies should evaluate MT devices based on the difficulty of the MT procedure. The choice of MT device and its final evaluation will then depend on the pre-procedural angiogram.
Conclusions
The REVIVE device is effective and safe in recanalizing occluded intracranial arteries in AIS. Indirect comparison using historical data suggests REVIVE has equivalent, if not better, efficacy, and safety compared with the Merci Retriever. Furthermore, a favorable 90-day clinical outcome supports REVIVE as a valuable MT device option for AIS.
Acknowledgments
The RIVER JAPAN study was sponsored and funded by Johnson & Johnson K.K. Medical Company. Editorial support, in the form of medical writing, assembling tables and creating high-resolution images based on authors’ detailed directions, collating author comments, copyediting, fact checking, and referencing, was provided by Cactus Communications, and funded by Johnson and Johnson/Codman Co. Ltd.
Footnotes
Study centers
- Kobe City Medical Center General Hospital: Nobuyuki Sakai, Hirotoshi Imamura, Kenichi Todo, Tomoyuki Kono, Taku Hoshi, Sho Murase, Hidemitsu Adachi, Shinsuke Sato, Yohei Mineharu, Mikiya Beppu, Kampei Shimizu, Teishiki Shibata, Katsunori Asai
- Ota Memorial Hospital: Shinzo Ota
- Kohnan Hospital: Yasushi Matsumoto, Ryushi Kondo, Kenichi Sato, Ichiro Suzuki, Kuniyasu Niizuma
- Yamagata City Hospital Saiseikan: Rei Kondo, Morio Nagahata
- National Cerebral and Cardiovascular Center: Tetsu Satow, Hiroshi Yamagami, Mikito Hayakawa, Kazunori Toyoda
- Saiseikai Toyama Hospital: Michiya Kubo
- National Hospital Organization Kyushu Medical Center: Tomoyuki Tsumoto, Yuichiro Tsurusaki, So Tokunaga
- Gifu University: Yukiko Enomoto
- Nakamura Memorial Hospital: Taketo Kataoka, Yasushi Ito, Yuji Matsumaru, Shinichi Yoshimura, Kenji Sugiu.
Conflicts of Interest Disclosure
All authors who are members of The Japan Neurosurgical Society (JNS) or Japan Stroke Society (JSS) have registered self-reported COI disclosure statements through the website for JNS and JSS members.
Nobuyuki Sakai; UNRELATED: Consultancy: Achieva, Biomedical Solutions, Cardiatis, Codman/Johnson and Johnson, Medtronic, Microvention/Terumo, Penumbra, Pulsar Vascular, Stryker; Grants; Microvention/Terumo (research grant)1;. All co-authors have no conflict of interest for this manuscript.
Money paid to the institution.
References
- 1).Frendl A, Csiba L: Pharmacological and non-pharmacological recanalization strategies in acute ischemic stroke. Front Neurol 2: 32, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Berkhemer OA, Fransen PS, Beumer D, et al. : A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372: 11–20, 2015 [DOI] [PubMed] [Google Scholar]
- 3).Jovin TG, Chamorro A, Cobo E, et al. : Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372: 2296–2306, 2015 [DOI] [PubMed] [Google Scholar]
- 4).Goyal M, Demchuk AM, Menon BK, et al. : Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372: 1019–1030, 2015 [DOI] [PubMed] [Google Scholar]
- 5).Campbell BC, Mitchell PJ, Kleinig TJ, et al. : Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372: 1009–1018, 2015 [DOI] [PubMed] [Google Scholar]
- 6).Saver JL, Goyal M, Bonafe A, et al. : Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372: 2285–2295, 2015 [DOI] [PubMed] [Google Scholar]
- 7).Möhlenbruch M, Stampfl S, Behrens L, et al. : Mechanical thrombectomy with stent retrievers in acute basilar artery occlusion. AJNR Am J Neuroradiol 35: 959–964, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Rohde S, Haehnel S, Herweh C, et al. : Mechanical thrombectomy in acute embolic stroke: preliminary results with the revive device. Stroke 42: 2954–2956, 2011 [DOI] [PubMed] [Google Scholar]
- 9).Shindo A, Kawanishi M, Kawakita K, et al. : Treatment of acute cerebral artery occlusion using the Penumbra system: our early experience. Neurol Med Chir (Tokyo) 54: 441–449, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Japan Stroke Society. Japan Cranial Nerve Endovascular Treatment Society Second edition. First edition (August 2009); revised April 2015 http://www.jsts.gr.jp/img/noukessen.pdf.
- 11).Smith WS, Sung G, Starkman S, et al. MERCI Trial Investigators : Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke 36: 1432–1438, 2005 [DOI] [PubMed] [Google Scholar]
- 12).Smith WS, Sung G, Saver J, et al. : Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke 39: 1205–1212, 2008 [DOI] [PubMed] [Google Scholar]
- 13).Saver JL, Jahan R, Levy EI, et al. : Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet 380: 1241–1249, 2012 [DOI] [PubMed] [Google Scholar]
- 14).Nogueira RG, Lutsep HL, Gupta R, et al. : Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet 380: 1231–1240, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Jansen O, Macho JM, Killer-Oberpfalzer M, Liebeskind D, Wahlgren N, TREVO Study Group : Neurothrombectomy for the treatment of acute ischemic stroke: results from the TREVO study. Cerebrovasc Dis 36: 218–225, 2013 [DOI] [PubMed] [Google Scholar]
- 16).Binning MJ, Adel JG, Maxwell CR, et al. : Early postmarket experience after US Food and Drug Administration approval with the Trevo device for thrombectomy for acute ischemic stroke. Neurosurgery 75: 584–589; discussion 589, 2014 [DOI] [PubMed] [Google Scholar]
- 17).Stampfl S, Hartmann M, Ringleb PA, Haehnel S, Bendszus M, Rohde S: Stent placement for flow restoration in acute ischemic stroke: a single-center experience with the Solitaire stent system. AJNR Am J Neuroradiol 32: 1245–1248, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Penumbra Pivotal Stroke Trial Investigators : The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke 40: 2761–2768, 2009 [DOI] [PubMed] [Google Scholar]
- 19).Broussalis E, Trinka E, Hitzl W, Wallner A, Chroust V, Killer-Oberpfalzer M: Comparison of stent-retriever devices versus the Merci retriever for endovascular treatment of acute stroke. AJNR Am J Neuroradiol 34: 366–372, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Frei D, Gerber J, Turk A, et al. : The SPEED study: initial clinical evaluation of the Penumbra novel 054 Reperfusion Catheter. J Neurointerv Surg 5(Suppl 1): i74–i76, 2013 [DOI] [PubMed] [Google Scholar]
- 21).Sallustio F, Koch G, Di Legge S, et al. : Intra-arterial thrombectomy versus standard intravenous thrombolysis in patients with anterior circulation stroke caused by intracranial arterial occlusions: a single-center experience. J Stroke Cerebrovasc Dis 22: e323–e331, 2013 [DOI] [PubMed] [Google Scholar]
- 22).Nguyen TN, Malisch T, Castonguay AC: Balloon guide catheter improves revascularization and clinical outcomes with the Solitaire device: analysis of the North American Solitaire Acute Stroke Registry. Stroke 45: 141–145, 2014 [DOI] [PubMed] [Google Scholar]
- 23).Castaño C, Dorado L, Guerrero C, et al. : Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke 41: 1836–1840, 2010 [DOI] [PubMed] [Google Scholar]
- 24).Pereira VM, Gralla J, Davalos A, et al. : Prospective, multicenter, single-arm study of mechanical thrombectomy using Solitaire Flow Restoration in acute ischemic stroke. Stroke 44: 2802–2807, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Kim JE, Kim AR, Paek YM, Cho YJ, Lee BH, Hong KS: Safety and efficacy of mechanical thrombectomy with the Solitaire device in large artery occlusion. Neurol India 60: 400–405, 2012 [DOI] [PubMed] [Google Scholar]
- 26).Mokin M, Dumont TM, Veznedaroglu E, et al. : Solitaire Flow Restoration thrombectomy for acute ischemic stroke: retrospective multicenter analysis of early postmarket experience after FDA approval. Neurosurgery 73: 19–25; discussion 25–26, 2013 [DOI] [PubMed] [Google Scholar]
- 27).San Román L, Obach V, Blasco J, et al. : Single-center experience of cerebral artery thrombectomy using the TREVO device in 60 patients with acute ischemic stroke. Stroke 43: 1657–1659, 2012 [DOI] [PubMed] [Google Scholar]
- 28).Kabbasch C, Mpotsaris A, Chang DH, et al. : Mechanical thrombectomy with the Trevo ProVue device in ischemic stroke patients: does improved visibility translate into a clinical benefit? J Neurointerv Surg 8: 778–782, 2016 [DOI] [PubMed] [Google Scholar]
- 29).Behme D, Kowoll A, Mpotsaris A, et al. : Multicenter clinical experience in over 125 patients with the Penumbra Separator 3D for mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg 8: 8–12, 2016 [DOI] [PubMed] [Google Scholar]
- 30).Meyers PM, Schumacher HC, Alexander MJ, et al. : Performance and training standards for endovascular ischemic stroke treatment. AJNR Am J Neuroradiol 31: E8–E11, 2010 [PMC free article] [PubMed] [Google Scholar]