Abstract
Background
P-phenylenediamine (PPD) has been identified as the most frequent contact sensitizer of hair dye and the clinical characteristics of hair dye contact allergy (HDCA) are diverse.
Objective
The purpose of this study was to identify the clinical characteristics of HDCA and to assess the relationships between HDCA, exposure time to PPD and PPD positivity.
Methods
We analyzed 105 patients with patch test-confirmed hair dye allergy who presented between July 2009 and March 2015. Clinical symptoms, signs, associated skin diseases, involved ACD area, and patterns of hair dye use were obtained by reviewing medical records and by interview.
Results
HDCA was more common in women and in individuals aged more than 50 years. Pruritus was the most common symptom; erythematous macules and patches were the most frequently observed clinical signs. The most common site of HDCA was the face and non-specific eczema and urticaria were frequently observed with HDCA. Exposure time to hair dye, represented as frequency and duration, showed a positive correlation with the area affected by hair dye allergy (p<0.001). Hair dye allergy was identified in most patients (80%) before diagnosis by patch test. However, only 28.6% of all patients stopped using hair dye, even after the diagnosis was confirmed.
Conclusion
The extent of hair dye allergy involvement was related to exposure time to hair dye. For effective treatment of HDCA, it is important to properly educate patients with HDCA about the clinical manifestations of HDCA and to keep away from allergens.
Keywords: Allergic contact dermatitis, Hair dyes, Phenylenediamines
INTRODUCTION
Hair care products are a major source of lifestyle-related chemical exposure in the general population, especially since hair dye use is becoming an integral part of modern culture1,2. Hair dyes are usually used to conceal gray hair or to change hair color and hair dyeing is frequently performed in Korea3,4. Kim et al.5 reported that 63.8% of the Korean population has dyed their hair. Allergic contact dermatitis (ACD) from hair dye is a worldwide problem of individuals who dye their hair1,6. P-phenylenediamine (PPD) is the most frequent contact sensitizer present in hair care products and is a primary patch test screening agent for hair dye contact allergy (HDCA)2,3,6,7. The clinical findings of hair dye allergy vary and include typical ACD, lichen simplex chronicus, non-specific eczema and dermographism on the hair dye-exposed area or/and extended area6. In severe cases, acute systemic adverse effects such as angioedema, upper airway obstruction, rhabdomyolysis, and acute renal failure have also been reported2. We investigated 105 patients with hair dye allergy with a positive PPD patch test result to identify the clinical characteristics of hair dye allergy and to clarify the relationships between hair dye allergy, duration of hair dye use, and frequency of hair dye use.
MATERIALS AND METHODS
Study subjects and study design
The study was conducted on 105 patients with HDCA suspected by hair dye contact history and clinical symptoms. All cases of HDCA were confirmed by patch test using the Korean standard series (KOR-1000, Chemotechnique®; Sweden) and the thin-layer rapid use epicutaneous (TRUE) Test (Smart-Practice, Phoenix, AZ, USA). Patients were treated between July 2009 and March 2015 at The Catholic University of Korea, Catholic Medical Center. The clinical symptoms, signs, associated skin diseases, involved area, and exposure time to hair dye were obtained by reviewing medical records and by interview. This study was approved by The Ethics Committee of Seoul St. Mary's Hospital, The Catholic University of Korea (IRB no. XC17REDI0053).
Patch test and reaction grading
The Korean standard series and the TRUE Test system were used to diagnose HDCA. Patch tests were read on days 2 and 4 according to the recommendations of the International Contact Dermatitis Research Group (ICDRG). According to the ICDRG criteria, reaction grade was documented as – (negative reaction), ? (doubtful reaction), 1+ (weakly positive), 2+ (strongly positive), and 3+ (extremely positive). Patients showing 1+, 2+, or 3+ reactions to PPD were considered to have HDCA.
Review of medical records and interview
Information about the clinical manifestations of hair dye allergy was retrospectively collected by reviewing the medical records of the 105 patients with patch test-confirmed hair dye allergy. The collected information included each subject's age, sex, clinical symptoms and signs, extent of contact dermatitis involvement (direct area and indirect area), combined skin problems, patch test PPD positivity, duration of hair dye use (years), frequency of hair dye use (number of applications/year), whether the subject continued hair dye use after the diagnosis, and the extent of skin lesion improvement.
The extent of contact dermatitis was determined by the involved area. Some of the patients had contact dermatitis on direct contact areas such as the face, scalp and neck, whereas others had contact dermatitis on both direct and indirect areas, including the trunk and upper/lower extremities. 1+ reaction groups and 2+, 3+ reaction groups was classified as weakly positive and strongly/extremely positive group respectively.
Statistical analysis
Statistical analyses were performed using SAS ver. 9.4 (SAS Institute, Cary, NC, USA). The p-values <0.05 were considered significant. Correlations between exposure time to hair dye and extent of HDCA, other combined skin problems, and PPD positivity were calculated using the Mann-Whitney test.
RESULTS
Demographic characteristics
Of the 105 subjects enrolled in the study, 31 (29.5%) were male and 74 (70.5%) were female. The mean age was 52.9 years and two-thirds of the patients were over 50 years of age (Table 1).
Table 1. Sex and age distribution (n=105).
| n (%) | |
|---|---|
| Sex | |
| Male | 31 (29.5) |
| Female | 74 (70.5) |
| Age (y) | |
| ≤9 | 0 (0.0) |
| 10~19 | 2 (1.9) |
| 20~29 | 4 (3.8) |
| 30~39 | 8 (7.6) |
| 40~49 | 21 (20.0) |
| 50~59 | 35 (33.3) |
| ≥60 | 35 (33.3) |
Clinical characteristics
1) Clinical signs and symptoms of hair dyeing
The patients had various clinical symptoms including pruritus, pricking, dryness, and burning or tingling sensations. The most common symptom was pruritus, which was seen in 75 patients (71.4%). Nine patients (8.6%) had a pricking sensation, 2 (1.9%) had dryness and 1 (1.0%) had a burning or tingling sensation. Clinical signs such as erythematous macules and patches, erythematous papules and plaques, scales, oozing and others (crust, yperpigmentation, vesicles and blisters, lichenification, swelling and fissures) were also seen. The most common clinical sign was erythematous macules and patches (56.2%), followed by scales (8.6%), erythematous papules and plaques (7.6%) and oozing (6.7%) (Table 2).
Table 2. Clinical symptoms and signs of hair dye contact allergy (n=105).
| n (%) | |
|---|---|
| Symptom | |
| Pruritus | 75 (71.4) |
| Pricking | 9 (8.6) |
| Dryness | 2 (1.9) |
| Burning/tingling sensation | 1 (1.0) |
| Sign | |
| Erythematous macules, patches | 59 (56.2) |
| Scales | 9 (8.6) |
| Erythematous papules, plaque | 8 (7.6) |
| Oozing | 7 (6.7) |
| Crust | 4 (3.8) |
| Hyperpigmentation | 4 (3.8) |
| Vesicles, blisters | 3 (2.9) |
| Lichenification | 3 (2.9) |
| Swelling | 3 (2.9) |
| Fissures | 3 (2.9) |
| Combined skin problems | |
| Non-specific eczema | 27 (25.7) |
| Urticaria | 15 (14.3) |
| Prurigo simplex, prurigo nodularis | 9 (8.6) |
| Seborrheic dermatitis | 8 (7.6) |
| Lichen simplex chronicus | 3 (2.9) |
| Total | 52 (49.5) |
2) Combined skin problems
Fifty-two patients (49.5%) had combined skin problems out of the 105 patients. Twenty-seven patients (25.7%) showed eczematous lesions other than hair dye contact dermatitis, such as nummular eczema, pompholyx, and hand eczema. Fifteen patients (14.3%) had urticarial problems, including acute or chronic urticaria, symptomatic dermographism and solar urticaria. Nine patients (8.6%) had prurigo simplex or prurigo nodularis, 8 (7.6%) had seborrheic dermatitis, and 3 (2.9%) had combined lichen simplex chronicus (Table 2).
3) Distribution of skin lesions
The face (57.1%) was the most commonly involved area, followed by the scalp (36.2%), neck (34.3%), trunk (29.5%), hand (21.0%) and upper extremities (20.0%) (Table 3). Among the 105 patients diagnosed with HDCA, 68 (64.8%) had contact dermatitis only on a direct contact area such as the face, scalp or neck. Thirty-seven patients (35.2%) had contact dermatitis on both a direct area and an indirect contact area.
Table 3. Distribution of skin lesions (n=105).
| n (%) | |
|---|---|
| Site | |
| Face | 60 (57.1) |
| Scalp | 38 (36.2) |
| Neck | 36 (34.3) |
| Trunk | 31 (29.5) |
| Hand | 22 (21.0) |
| Upper extremity | 21 (20.0) |
| Lower extremity | 7 (6.7) |
| Genital area | 2 (1.9) |
| Extent | |
| Direct | 68 (64.8) |
| Indirect | 37 (35.2) |
4) Patch test result
Of the 105 patients who showed positive result on PPD, 61 patients showed multiple antigen positivity. Most common antigen detected was nickel which 37 patients showed positive result. Second most common antigen was cobalt chloride (22), followed by potassium dichromate (18), mercury (II) amino chloride (11), thiuram mix (9), formaldehyde (9), fragrance mix (8), balsam of peru (7), paraben mix (7) and others (imidazolidinyl urea, neomycin sulfate, colophonium, thimerosal, mercapto mix, quanterium-15, lanolin alcohol, captan, 2-mercaptobenzothiazole, tixocortol-21-pivalate).
5) Patch test positivity on PPD
Forty-four patients (41.9%) showed a weakly positive result, 44 patients (41.9%) showed a strongly positive result and 17 patients (16.2%) showed an extremely positive result on the patch test with PPD (Table 4).
Table 4. Patch test positivity for P-phenylenediamine (n=105).
| n (%) | |
|---|---|
| 1+ (weakly positive) | 44 (41.9) |
| 2+ (strongly positive) | 44 (41.9) |
| 3+ (extremely positive) | 17 (16.2) |
6) Frequency and duration of hair dye use
We next analyzed the frequency (number of applications/year) and duration (years) of hair dye use. Regarding frequency, 30 patients (28.6%) used hair dye less than 5 times a year (less than once every two months), 51 patients (48.6%) used hair dye 6 to 11 times a year (more than once every two months and less than once a month), 11 patients (10.5%) used hair dye 12 to 23 times a year (more than once a month and less than twice a month) and 10 patients (9.5%) used hair dye more than 24 times a year (more than twice a month) (Table 5).
Table 5. Frequency and duration of hair dye use (n=105).
| n (%) | |
|---|---|
| Frequency (time/yr) | |
| <5 | 30 (28.6) |
| 6~11 | 51 (48.6) |
| 12~23 | 11 (10.5) |
| ≥24 | 10 (9.5) |
| Duration (yr) | |
| <5 | 11 (10.5) |
| 5~10 | 43 (41.0) |
| >10 | 48 (45.7) |
Regarding the duration of hair dye use, 11 patients (10.5%) had been using hair dye for less than 5 years, 43 patients (41.0%) had been using hair dye for 5 to 10 years, and 48 patients (45.7%) had been using hair dye for more than 10 years (Table 5).
7) Exposure time to hair dye and extent of HDCA, PPD positivity, and combined dermatologic problems
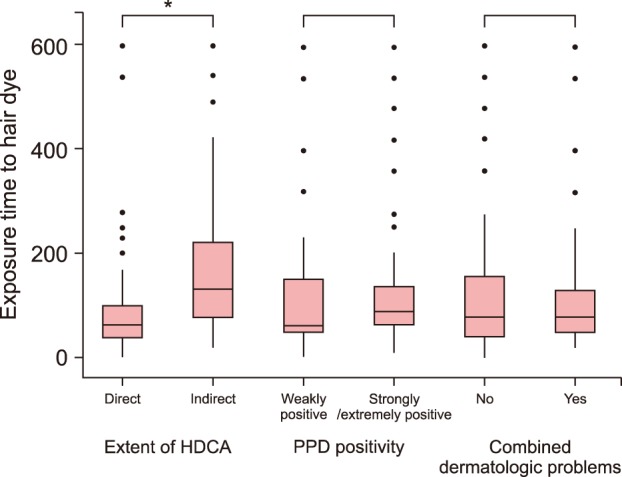
We next evaluated the relationships between hair dye exposure time and the extent of HDCA, PPD positivity and presence of combined dermatologic problems. We defined the exposure time to hair dye as hair dye duration (years) X frequency (number of applications/year). We excluded 3 patients who had incorrect information about exposure time to hair dye. Exposure time to hair dye was statistically significantly correlated with the extent of HDCA involvement (direct and indirect). We found that individuals who used hair dye more frequently showed contact dermatitis lesions both in the direct contact area and the indirect area (p=0.001) (Fig. 1). However, exposure time to hair dye was not significantly correlated with PPD positivity (p=0.27) (Fig. 1). Similarly, exposure time to hair dye was not significantly correlated with the presence of combined dermatologic problems (p=0.30) (Fig. 1).
Fig. 1. Duration of hair dye use, frequency of hair dye use, P-phenylenediamine (PPD) positivity and combined dermatologic problems. Exposure time to hair dye (duration [years]×frequency [number of applications/year]) and extent of hair dye contact allergy involvement (direct; mean=60.0 and indirect; mean=130.0) showed a statistically significant correlation (p=0.001). Regarding exposure time to hair dye and PPD positivity (weakly positive, mean=116.83; strongly/extremely positive, mean=127.64), no statistically significant relationship was found (p=0.27). Exposure time to hair dye and the presence of combined dermatologic problems (no, mean=128.7; yes, mean=117.4) did not show a statistically significant correlation (p=0.30). HDCA: hair dye contact allergy.
8) Recognition of hair dye allergy, continuation of hair dye use, and clinical improvement
Eighty-four patients (80.0%) were recognized or suspected to have hair dye allergy before the patch test diagnosis. We next analyzed whether people tended to discontinue hair dye use when they were diagnosed with HDCA. Out of the 105 patients diagnosed with HDCA, only 30 patients (28.6%) stopped using hair dye. Nineteen patients (63.3%) showed clinical improvement after discontinuation of dye use, compared to only 11 patients out of 75 (14.7%) who showed clinical improvement after continued hair dye use.
DISCUSSION
PPD is an aromatic amine that is used for hair dyes and henna tattoos8. PPD is also a common allergen and is commonly suspected to be the cause of HDCA9. In European, North American and Asian general populations, 1 to 6% of all patients with dermatitis have been reported to be sensitized to PPD; these percentages rise to 38% to 97% in patients with hair dye dermatitis8,10. Another study reported a median prevalence of PPD sensitization in Asia of 4.3%9. High positive reactivity rates to PPD have been reported in Korea11,12,13,14,15. These high rates seem to be related to the increased demand for hair coloring and the trend for individuals to begin using hair dye for cosmetic purposes at a relatively young age. Henna tattoos might also be an important source of PPD exposure and sensitization1,16,17.
Our study found a higher prevalence in women (70.5%) than men, similar to the findings of previous studies9,16,18,19,20,21,22. This finding reflects the higher exposure of women23. In a European cross-sectional study of individuals from the general population, 50.9% of all individuals were found to have used hair colorants at least once in their lifetime; 78% were female and 20% were male24. In a study conducted in Korea, women (57.8%) showed higher prevalence than man (42.2%) similar to our study9.
The prevalence was higher in older patients, particularly individuals over 50 years of age (66.7%). In Korea, the onset of hair graying usually starts in the third or fourth decade of life25. In a study conducted in Korea, patients over 50 years of age showed higher prevalence (86.7%) similar to our study9.
We also analyzed the clinical symptoms and signs of patients with HDCA. The most commonly observed symptom was pruritus (71.3%). Pricking sensations (8.6%), dryness (1.9%) and burning or tingling sensations (1.0%) were also detected. Among the clinical signs evaluated, erythematous macules and patches were observed on 59 patients (56.2%) and second most common sign was erythematous papules and plaques (7.6%). Our findings are similar to those of previous studies. Kim et al.5 reported that pruritus was the most common side effect related to hair dye use; eye tingling sensations, erythema, scales, vesicles, oozing, edema, and swelling were also reported. The clinical features of HDCA vary from mild contact dermatitis in a localized area or disseminated generalized dermatitis to severe complications including contact urticaria, angioedema, erythema multiforme-like lesions, hair loss, rhinitis, bronchospasms, asthma, and renal toxicity, the latter of which can be life threatening26,27. Dermatologic problems like atopic dermatitis are also potential risk factors for contact sensitivity because the impaired skin barrier leads to increased allergen penetration28.
We found that the face (57.1%) was the most frequently affected site, followed by the scalp (36.2%) and neck (34.3%). Similar result was reported in the study conducted in Korea. Lee et al.9 reported the face as the most frequently affected site, followed by the scalp. We grouped the face, scalp, and neck as direct contact areas and other areas such as the trunk, hand, upper extremities, lower extremities, and feet as indirect contact areas. In our study, 68 people (64.8%) had HDCA only on the direct contact area, while 37 people (35.2%) showed skin lesions on both the direct and indirect areas. Similar to our study, other studies have reported that the forehead was the most common location showing an allergic reaction to PPD, followed by the eyes, ears, and then scalp; these direct contact areas also showed more severe presentation9,17,21,29. Allergy contact dermatitis from PPD derivatives also seems to be related to lichen planus or lichenoid eruptions6,30,31,32. In another study, Chey et al.6 reported that patients with hair dye ACD and combined chronic skin lesions such as lichen simplex chronicus showed chronic skin lesion improvement after discontinuing hair dye use.
A total of 52 patients (49.5%) had multiple skin problems. Eczematous lesions (25.7%) including nummular eczema, pompholyx and hand eczema were the most common.
The second most common problem was urticaria (14.3%), including acute or chronic urticaria, symptomatic dermographism and solar urticaria. Prurigo simplex or prurigo nodularis (8.6%), seborrheic dermatitis (7.6%) and lichen simplex chronicus (2.9%) were also detected.
Many studies have reported that individuals with ACD may develop more severe allergic reactions when exposed to causative allergens and that increases in exposure duration and frequency might lead to more severe clinical presentation9. We observed that skin lesions were more widespread in patients who had longer exposure time to hair dye. However, exposure time to hair dye was not significantly correlated with PPD patch test reactivity. Similarly, exposure time to hair dye was not significantly correlated with the number of combined skin lesions. The absence of observable significant correlations might be due to the small number of patients in this study; further large-scale multicenter studies are needed to test this hypothesis.
Most patients (80%) were recognized or suspected of having hair dye allergy before the patch test diagnosis. However, only 28.6% of the patients stopped hair dye use, even after diagnosis was confirmed. For effective treatment of HDCA, it is important to properly educate patients with HDCA about the clinical manifestations of HDCA and to keep away from allergens.
This study is important because we focused on the clinical characteristics of HDCA and the relationships between exposure time to hair dye, severity of HDCA, and combined skin disease.
Our study does have some limitations. First, it could have selection bias and/or recall bias, since it was conducted at a university hospital in a retrospective manner. Second, we only studied PPD as an allergen causing HDCA. However, widely used commercial hair dyes include many other allergens and individuals with allergic reactions to PPD have been reported to show frequent cross-reactions with other dyes, local anesthetics, and black rubber antioxidants16,33. Since the number of patients in this study was relatively small and the study was not conducted across the entire Korean population, further large-scale multicenter studies are needed.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
References
- 1.Almeida PJ, Borrego L, Limiñana JM. Age-related sensitization to p-phenylenediamine. Contact Dermatitis. 2011;64:172–174. doi: 10.1111/j.1600-0536.2010.01834.x. [DOI] [PubMed] [Google Scholar]
- 2.Patra AP, Shaha KK, Rayamane AP, Dash SK, Mohanty MK, Mohanty S. Paraphenylenediamine containing hair dye: an emerging household poisoning. Am J Forensic Med Pathol. 2015;36:167–171. doi: 10.1097/PAF.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 3.Kim H, Kim K. Prevalence of potent skin sensitizers in oxidative hair dye products in Korea. Cutan Ocul Toxicol. 2016;35:204–207. doi: 10.3109/15569527.2015.1076434. [DOI] [PubMed] [Google Scholar]
- 4.Handa S, Mahajan R, De D. Contact dermatitis to hair dye: an update. Indian J Dermatol Venereol Leprol. 2012;78:583–590. doi: 10.4103/0378-6323.100556. [DOI] [PubMed] [Google Scholar]
- 5.Kim JE, Jung HD, Kang H. A survey of the awareness, knowledge and behavior of hair dye use in a Korean population with gray hair. Ann Dermatol. 2012;24:274–279. doi: 10.5021/ad.2012.24.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chey WY, Kim KL, Yoo TY, Lee AY. Allergic contact dermatitis from hair dye and development of lichen simplex chronicus. Contact Dermatitis. 2004;51:5–8. doi: 10.1111/j.0105-1873.2004.00252.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee HS, Lin YW. Permeation of hair dye ingredients, p-phenylenediamine and aminophenol isomers, through protective gloves. Ann Occup Hyg. 2009;53:289–296. doi: 10.1093/annhyg/mep009. [DOI] [PubMed] [Google Scholar]
- 8.Pot LM, Scheitza SM, Coenraads PJ, Blömeke B. Penetration and haptenation of p-phenylenediamine. Contact Dermatitis. 2013;68:193–207. doi: 10.1111/cod.12032. [DOI] [PubMed] [Google Scholar]
- 9.Lee JY, Kim CW, Kim SS. Analysis of the results from the patch test to para-phenylenediamine in the TRUE test in patients with a hair dye contact allergy. Ann Dermatol. 2015;27:171–177. doi: 10.5021/ad.2015.27.2.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krasteva M, Bons B, Ryan C, Gerberick GF. Consumer allergy to oxidative hair coloring products: epidemiologic data in the literature. Dermatitis. 2009;20:123–141. [PubMed] [Google Scholar]
- 11.Thyssen JP, White JM European Society of Contact Dermatitis. Epidemiological data on consumer allergy to p-phenylenediamine. Contact Dermatitis. 2008;59:327–343. doi: 10.1111/j.1600-0536.2008.01427.x. [DOI] [PubMed] [Google Scholar]
- 12.Patel S, Basketter DA, Jefferies D, White IR, Rycroft RJ, McFadden JP, et al. Patch test frequency to p-phenylenediamine: follow up over the last 6 years. Contact Dermatitis. 2007;56:35–37. doi: 10.1111/j.1600-0536.2007.00779.x. [DOI] [PubMed] [Google Scholar]
- 13.Handa S, De D, Mahajan R. Epidemiological trends in contact dermatitis to hair dye: Comparing para-phenylenediamine positivity after a decade long interval. Indian J Dermatol Venereol Leprol. 2011;77:511–512. doi: 10.4103/0378-6323.82386. [DOI] [PubMed] [Google Scholar]
- 14.Lee GY, Kim JK, Kim KJ. A study of the results of patch test in patients with contact dermatitis. Korean J Dermatol. 2007;45:908–914. [Google Scholar]
- 15.Hong YJ, Choi HY, Kim KJ, Lee GY, Kim DW, Kim SJ, et al. TRUE test in patients with contact dermatitis: a multicenter study. Korean J Dermatol. 2011;49:661–669. [Google Scholar]
- 16.Thomas BR, White IR, McFadden JP, Banerjee P. Positive relationship-intensity of response to p-phenylenediamine on patch testing and cross-reactions with related allergens. Contact Dermatitis. 2014;71:98–101. doi: 10.1111/cod.12255. [DOI] [PubMed] [Google Scholar]
- 17.LaBerge L, Pratt M, Fong B, Gavigan G. A 10-year review of p-phenylenediamine allergy and related para-amino compounds at the Ottawa Patch Test Clinic. Dermatitis. 2011;22:332–334. doi: 10.2310/6620.2011.11044. [DOI] [PubMed] [Google Scholar]
- 18.Coenraads PJ, Nater JP, van der. Prevalence of eczema and other dermatoses of the hands and arms in the Netherlands. Association with age and occupation. Clin Exp Dermatol. 1983;8:495–503. doi: 10.1111/j.1365-2230.1983.tb01816.x. [DOI] [PubMed] [Google Scholar]
- 19.Ho SG, Basketter DA, Jefferies D, Rycroft RJ, White IR, McFadden JP. Analysis of para-phenylenediamine allergic patients in relation to strength of patch test reaction. Br J Dermatol. 2005;153:364–367. doi: 10.1111/j.1365-2133.2005.06742.x. [DOI] [PubMed] [Google Scholar]
- 20.Schäfer T, Böhler E, Ruhdorfer S, Weigl L, Wessner D, Filipiak B, et al. Epidemiology of contact allergy in adults. Allergy. 2001;56:1192–1196. doi: 10.1034/j.1398-9995.2001.00086.x. [DOI] [PubMed] [Google Scholar]
- 21.Søsted H, Hesse U, Menné T, Andersen KE, Johansen JD. Contact dermatitis to hair dyes in a Danish adult population: an interview-based study. Br J Dermatol. 2005;153:132–135. doi: 10.1111/j.1365-2133.2005.06588.x. [DOI] [PubMed] [Google Scholar]
- 22.Diepgen TL, Ofenloch RF, Bruze M, Bertuccio P, Cazzaniga S, Coenraads PJ, et al. Prevalence of contact allergy in the general population in different European regions. Br J Dermatol. 2016;174:319–329. doi: 10.1111/bjd.14167. [DOI] [PubMed] [Google Scholar]
- 23.Schuttelaar ML, Vogel TA, Rui F, Kręcisz B, Chomiczewska-Skora D, Kieć-Świerczyńska M, et al. ESSCA results with the baseline series, 2002-2012: p-phenylenediamine. Contact Dermatitis. 2016;75:165–172. doi: 10.1111/cod.12583. [DOI] [PubMed] [Google Scholar]
- 24.Diepgen TL, Naldi L, Bruze M, Cazzaniga S, Schuttelaar ML, Elsner P, et al. Prevalence of contact allergy to P-phenylenediamine in the European general population. J Invest Dermatol. 2016;136:409–415. doi: 10.1016/j.jid.2015.10.064. [DOI] [PubMed] [Google Scholar]
- 25.Jo SJ, Paik SH, Choi JW, Lee JH, Cho S, Kim KH, et al. Hair graying pattern depends on gender, onset age and smoking habits. Acta Derm Venereol. 2012;92:160–161. doi: 10.2340/00015555-1181. [DOI] [PubMed] [Google Scholar]
- 26.Helaskoski E, Suojalehto H, Virtanen H, Airaksinen L, Kuuliala O, Aalto-Korte K, et al. Occupational asthma, rhinitis, and contact urticaria caused by oxidative hair dyes in hairdressers. Ann Allergy Asthma Immunol. 2014;112:46–52. doi: 10.1016/j.anai.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Barrientos N, Abajo P, de Vega MM, Dominguez J. Erythema multiforme-like eruption following allergic contact dermatitis in response to para-phenylenediamine in a temporary henna tattoo. Int J Dermatol. 2014;53:e348–e350. doi: 10.1111/ijd.12285. [DOI] [PubMed] [Google Scholar]
- 28.Gupta M, Mahajan VK, Mehta KS, Chauhan PS. Hair dye dermatitis and p-phenylenediamine contact sensitivity: a preliminary report. Indian Dermatol Online J. 2015;6:241–246. doi: 10.4103/2229-5178.160253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Søsted H, Agner T, Andersen KE, Menné T. 55 cases of allergic reactions to hair dye: a descriptive, consumer complaint-based study. Contact Dermatitis. 2002;47:299–303. doi: 10.1034/j.1600-0536.2002.470508.x. [DOI] [PubMed] [Google Scholar]
- 30.Buckley WR. Lichenoid eruptions following contact dermatitis. AMA Arch Derm. 1958;78:454–457. doi: 10.1001/archderm.1958.01560100028005. [DOI] [PubMed] [Google Scholar]
- 31.Mandel EH. Lichen planus-like eruptions caused by a color-film developer. Arch Dermatol. 1960;81:516–519. doi: 10.1001/archderm.1960.03730040020004. [DOI] [PubMed] [Google Scholar]
- 32.Roed-Petersen J, Menné T. Allergic contact dermatitis and lichen planus from black-and-white photographic developing. Cutis. 1976;18:699–700. [PubMed] [Google Scholar]
- 33.Goon AT, Gilmour NJ, Basketter DA, White IR, Rycroft RJ, McFadden JP. High frequency of simultaneous sensitivity to Disperse Orange 3 in patients with positive patch tests to para-phenylenediamine. Contact Dermatitis. 2003;48:248–250. doi: 10.1034/j.1600-0536.2003.00049.x. [DOI] [PubMed] [Google Scholar]


