ABSTRACT:
Objective:
Children with Tourette syndrome (TS) are at risk for a variety of co-occurring conditions and learning and school problems. The purpose of this study was to determine the impact of TS and co-occurring conditions on school measures.
Methods:
Parent-reported data from the 2007–2008 and 2011–2012 National Survey of Children's Health were combined (n = 129,353 children aged 6–17 yrs). Parent report of health care provider diagnosis of TS; co-occurring mental, emotional, and behavioral conditions; learning and language conditions; and school measures were assessed. School measures included type of school, individual education plan (IEP), number of school days missed, school problems, doing well in school, doing homework, and repeating a grade. Children with TS were compared with those who never had TS on school measures accounting for co-occurring conditions.
Results:
After adjusting for demographics, compared with children without TS, children currently with TS were more likely to have an IEP, have a parent contacted about school problems, and not complete homework. After further adjusting for co-occurring conditions, only IEP status remained statistically significant. Compared with children with mild TS, children with moderate or severe TS were more likely to have an IEP, repeat a grade, encounter school problems, and not care about doing well in school.
Conclusion:
Tourette syndrome severity and co-occurring conditions are associated with school challenges and educational service needs. Awareness among health care providers, teachers and parents of the potential challenges related to both TS and co-occurring conditions would help to best support the child's education.
Index terms: Tourette syndrome, education, co-occurring conditions, public health
Tourette syndrome (TS) is a neurodevelopmental disorder characterized by motor and vocal tics that occur for at least 1 year,1 affecting between 3 and 9 per 1000 children.2–4 Tics can include simple twitches or grunts or more complex tics, such as a series of movements, shouting phrases, or repeating words. Well-known complex verbal tics such as coprolalia (involuntarily shouting out swear words) and echolalia (repeating others' words) can occur but are uncommon and not required for a diagnosis of TS. The type and severity of tics can change over time. TS often co-occurs with other mental, emotional, or behavioral disorders (MEB), including attention-deficit/hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), learning disorders (LD),5,6 and other behavioral problems,2,6 which may be more impairing than TS alone.7,8 Tics can disrupt functioning in daily activities and can result in social isolation, interpersonal conflict, peer victimization, and inability to go to school.9,10 However, information on how mental, emotional, behavioral, or learning disorders and school factors are related to each other is limited.
What Is Known About Tourette Syndrome and Education?
Previous studies have reported various school-related problems experienced by children with TS, including an increased risk for repeating a grade.11 Children with TS are more likely to show decreased academic performance and to need special education services.10,12,13
Tourette syndrome may impact school performance in different ways. The tics can physically interfere directly with studying and indirectly because they may increase stress; conversely, the stress of the classroom can increase tics.12,14 Tics, particularly when severe, can cause fatigue and chronic pain and thus interfere with learning. Children with TS may also be taken out of school because of difficulties associated with TS.10 TS may also affect schooling because of the impact on social relationships—peer problems or being teased or bullied.9,10,15 Schools may use inappropriate discipline such as punishment or suspension for tics.14,16 TS is also associated with increased absenteeism.14 Even accommodations that are intended to be helpful are often not evaluated for effectiveness12 and could have unintended consequences; for example, leaving the room when experiencing tics can make a child feel isolated, miss instructional time, or reinforce tics if leaving is seen as a welcome break.
The presence of a co-occurring condition may further impact educational outcomes. The increased risk for LD and associated problems with reading and writing,17,18 mathematical ability,19–21 and verbal functioning19,20,22,23 affect school functioning. In addition, the high prevalence of MEB in children with TS4 is likely to impact school functioning. The most common, ADHD2,5,6 may have a higher impact than TS alone,6,20 particularly in combination with other MEB.10 TS in combination with OCD is also more likely to impact school functioning than TS alone.24 Anxiety disorders may interfere with taking tests.17 Overall, children with multiple conditions are most likely to experience problems in school.10,14,25,26 Severity of TS symptoms is also associated with the severity of other issues including school competence,27 difficulties with homework and handwriting, and support from school staff.28
Need for Current Study
Although evidence suggests that children with TS may have challenges at school, most of the studies use convenience samples, focus on children with TS only, or have relatively small samples. Of the previous studies, very few examined both MEB and learning or other developmental disorders together in relation to school outcomes and included controls.10,17 The current study uses nationally representative survey data with a large sample of children without TS and examines the relationship between TS and school factors while also addressing the role of MEB and learning or other developmental disorders. The study combines data from 2 time points to allow a sufficient sample size for comparison of children with TS to those without TS.
METHODS
Sample
The National Survey of Children's Health uses parent report through telephone surveys to gather data on US children aged 0 to 17 years. The overall response rate in 2007–2008 was 46%. Cell phones were added to landlines in 2011–2012. In 2011–2012, the overall response rate was 23%; the interview completion rate, i.e., the proportion of households known to include children whose parents completed the interview, was 54.1% and 41.2% for landline and cell-phone samples, respectively. Data were gathered on 91,642 children in 2007–2008 and on 95,677 children in 2011–2012. Because the onset of tics is typically between 6 and 8 years of age,29 we included only children aged 6 to 17 years (n = 64,076 in 2007–2008 and n = 65,680 for 2011–2012), excluding cases missing data on sex (n = 178), whether a health care provider ever told them that their child had Tourette syndrome (TS) (n = 86 additional), and whether they currently had TS (n = 13 additional). We also excluded children whose parent reported that the child ever had TS but did not currently have TS (n = 126 additional), thus defining the control group without TS as “never having had TS.” As the survey asked only about TS diagnosis and not about other tics, some of these children may have had some current tic symptoms but also could have previously been falsely diagnosed. Therefore, exclusion is the more conservative approach. Thus, the final sample size for this study was 129,353 for 2007–2008 and 2011–2012 combined.
Variables
To assess TS and co-occurring conditions, parents were asked whether a doctor or other health care provider told the parent that the child ever had TS; attention-deficit/hyperactivity disorder (ADHD); behavioral or conduct problems, such as oppositional defiant disorder or conduct disorder; depression; anxiety problems; autism spectrum disorder; developmental delay; or speech problems, followed by questions about whether the child currently had the condition and how severe it was (mild, moderate, or severe). Tic severity was dichotomized into mild versus moderate or severe because of insufficient cell sizes for more fine-grained analyses. Parents were also asked whether a doctor, health care provider, teacher, or school official told them that their child had a learning disability. In 2011–2012, intellectual disability was added and language problems were added to speech problems.
To assess school measures, parents were asked questions about the past 12 months, including the type of school (public, private, or home), number of school days missed for illness or injury, how often the parent was contacted about school problems (excluding health problems), and whether the child had a written intervention plan or individual education plan (IEP) at school. Note that the question did not ask about other accommodations such as 504 plans. Parents were also asked 2 questions about their child's response to school, 1 about whether the child cared about doing well in school and another about whether their child did all required homework during the past month (in a 5-point rating scale ranging from “never” to “always”). Parents also reported whether the child had repeated a grade.
For the main analyses, the number of times contacted by the school and the number of days missed were dichotomized into 2 or fewer versus more than 2 because they were not evenly distributed, with the median and 75% percentile both being 2; thus, continuous analyses were not adequate. IEP and repeating a grade were yes/no variables. For caring about doing well and for doing homework, the variables were dichotomized into “never,” “rarely,” or “sometimes” versus “usually” or “always.” These were also not evenly distributed, with 85% of respondents selecting “usually” or “always.” For the purpose of this study, anxiety problems, depression, ADHD, and behavioral or conduct problems were grouped into mental, emotional, or behavioral disorders (MEB); other disabilities requiring special education such as learning disability, speech/language problems, intellectual disability, developmental delay, and autism spectrum disorder were grouped as learning/language conditions (LLC). Despite significant co-occurrence of all these conditions, these 2 groups were selected as being more likely to need either behavioral (MEB) or academic (LLC) accommodations.
Statistical Analysis
Weighted descriptive and regression analyses accounted for the complex sampling design, using SUDAAN. Specifying the sampling design is required for all SUDAAN procedures. With the introduction of the cell-phone sample in 2011–2012 came an additional indicator to specify whether each participant was drawn from the landline or cell-phone sample. Pooling the 2007 and 2011–2012 data required the addition of a landline specifier to all 2007 data.
Children currently with TS were compared with children who never had TS on demographics, the presence of other conditions, and school measures. All statistical comparisons were made using prevalence ratios. The first comparisons on school measures were adjusted for age, sex, and race/ethnicity and the additional comparisons were adjusted also for the presence of a co-occurring condition. Owing to unstable estimates because of small cell size, black and multiracial/other participants had to be combined into 1 group. To better understand the relative impact of TS and co-occurring conditions on a subset of school measures, analyses were conducted comparing children with combined TS, MEB, and LLC to children with TS and MEB but no LLC and children without TS, MEB, or LLC. Children with TS ever but not currently were excluded. Some cell sizes were small, resulting in somewhat unstable estimates. Cases in which the relative standard error (RSE) (standard error/prevalence ×100%) is greater than 30% are noted. Such estimates should be interpreted with caution and within the context of other results.
RESULTS
Demographics
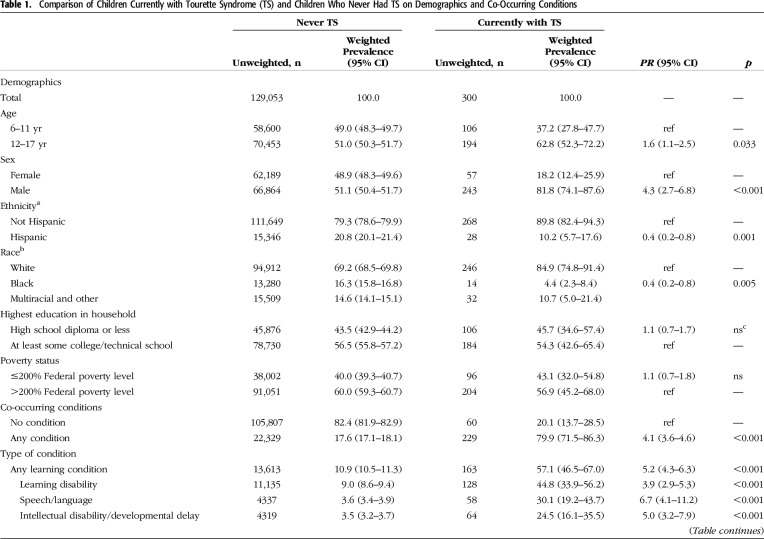
Overall, 0.29% (95% confidence interval [CI], 0.24%–0.35%) ever had Tourette syndrome (TS) and 0.19% (95% CI, 0.15%–0.24%) currently had TS, per parent report; of those currently with TS, 32.1% (95% CI, 23.0%–42.7%) were reported to have moderate to severe symptoms. Children currently with TS were more likely than those who never had TS to be male, 12 years of age or older, and of white/non-Hispanic ethnicity. Parent education or family poverty status did not differ by TS status (Table 1).
Table 1.
Comparison of Children Currently with Tourette Syndrome (TS) and Children Who Never Had TS on Demographics and Co-Occurring Conditions
Co-occurring Conditions
Children who currently had TS were more than 4 times as likely to have any of the specified co-occurring conditions compared with children who never had TS (Table 1). Of the children currently with TS, 80% had at least 1 co-occurring condition, compared with 18% of children who never had TS. Children currently with TS were more likely than those who never had TS to have mental, emotional, or behavioral disorders (MEB) (75% TS, 13% never TS) or learning/language conditions (LLC) (57% TS, 11% never TS). Attention-deficit/hyperactivity disorder and learning disability were the most common co-occurring conditions among children currently with TS (and those who never had TS) (Table 1).
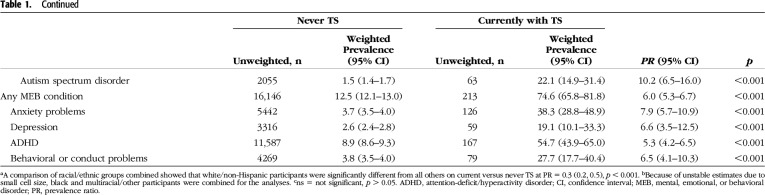
School Measures
The first question to examine was the relation between school measures and TS. After adjusting for demographics and compared with children who never had TS, children currently with TS were significantly more likely to have an individual education plan (IEP), to have a parent contacted about school problems, and to not complete homework. Repeating a grade (p = 0.06) and missing more than 2 days of school (p = 0.1) were more common among children with TS, but the difference did not reach statistical significance (Table 2). There was no association between TS currently being present and the type of school setting, or whether children cared about doing well in school. A post hoc analysis found no statistical difference between younger (ages 6–11 years) versus older (ages 12–17 years) children currently with TS on caring about doing well in school (p = 0.32).
Table 2.
Comparison of Children Currently with Tourette Syndrome (TS) and Children Who Never Had TS on School Measures
The main question was how co-occurring MEB or LLC affected the relationship of TS to school outcomes. Only the IEP status remained significant after adjusting for co-occurring conditions, i.e., children with TS were more likely to have an IEP even when other conditions were taken into account; their parents received more contacts about school problems, but the difference did not reach significance (p = 0.07; Table 2).
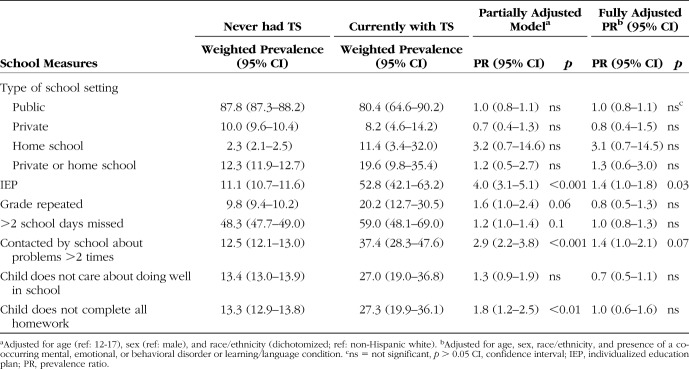
To better understand the relative impact of TS and co-occurring conditions on having an IEP, being contacted by the school, and not completing homework, analyses were conducted comparing children with combined TS, MEB, and LLC to children with TS and MEB but no LLC and children without TS, MEB, or LLC. Children who had combined TS, MEB, and LLC had the highest rates of IEP and school problems and were also significantly more likely to not complete homework. Compared with children without TS, MEB, or LLC, children who had TS, MEB, but no LLC had significantly higher rates of IEP and of being contacted by the school about problems. The difference for not completing homework reached significance, but the estimate should be interpreted with caution because the relative standard error was 32%. Children with TS but without co-occurring MEB or LLC had estimates that were very similar to children without TS or other conditions; however, the sample was too small to allow stable estimates. Similarly, the number of children with TS and LLC but without any MEB was too small to evaluate for this analysis (Table 3). To understand whether TS meant additional risk if present along with other conditions, post hoc analyses examined the differences between children with TS and MEB and children with MEB but without TS, as well as children with TS, MEB and LLC and those without TS but with MEB and LLC. The only significant effect was that TS in addition to MEB and LLC increased the likelihood of having an IEP. Otherwise, no differences emerged.
Table 3.
Comparison of Tourette Syndrome (TS) Combined with LLC or MEB on School Functioning
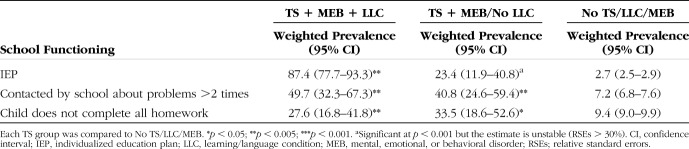
Severity
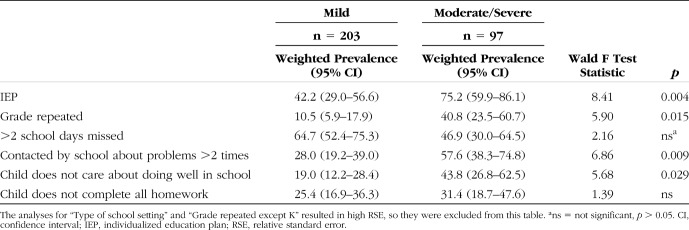
Compared with children with mild TS (unweighted n = 203), children with moderate or severe (unweighted n = 74 moderate and 23 severe) TS were more likely to have an IEP, have repeated a grade, be described as not caring about doing well in school, and to have a parent contacted about school problems (Table 4).
Table 4.
Comparison of Mild Versus Moderate/Severe Tourette Syndrome on School Functioning
Ever Diagnosed
Post hoc analyses were conducted to understand whether excluding the 126 children who previously had TS but did not currently have it would impact the findings. Although these children were older and had fewer other conditions, none of the relationships between TS and educational factors changed.
DISCUSSION
Tourette syndrome (TS) and its effect on educational success is an important concern for public health. These data confirm the well-reported associations of TS with co-occurring mental, emotional, and behavioral conditions as well as language and learning conditions. They extend on findings showing that school challenges are related to both TS and the co-occurring conditions. Although previous studies on the impact of TS on school measures focused on smaller samples, mostly examining either mental, emotional, or behavioral disorders (MEB) or learning and other special education disorders, this study used a large data set of US children currently with TS and who never had TS to report on both categories of disorders as well as the impact of TS severity. As previously found, TS was related to special education placement; however, unlike previous studies showing that co-occurring conditions were largely responsible,11,17 the current results showed that children currently with TS were more likely than those who never had TS to have an individual education plan (IEP) even taking co-occurring conditions into account.
The data also show that TS was associated with parents being contacted about school problems and children not completing all homework, but this was explained by the presence of co-occurring conditions. These findings are similar to a convenience sample of children with tic disorders,14 which also showed that academic problems and not completing homework were most common among children with TS and co-occurring conditions. As our follow-up analyses revealed, the combination of having both MEB and learning and other special education disorders along with TS resulted in a much greater impact on school measures than TS alone. Almost 90% of children with TS and both categories of disorders were receiving IEP services, which means that they have been identified by the school system as having special learning needs. Half of the parents of these children were also frequently called about school problems compared with less than 10% of parents of children without the identified conditions.
In addition, TS severity was associated with school measures; compared with children with mild TS, children with moderate or severe TS were significantly more likely to have an IEP and their parents were more likely to be contacted about school problems. A previous study among children with tic disorders also found that the severity of tics impacted academic problems.14
Although previous research has suggested that tic disorders are associated with grade retention11,17 and absenteeism,14 these measures were not significantly associated with TS in the current study. Grade retention increased for children currently with TS but was not significant before or after controlling for co-occurring conditions. In a previous study on absenteeism, parents of children with tic disorders reported that their children missed more than 3 days of school in the past year because of tics; however, no control group was included for comparison.14
Implications
These results support previous findings about the impact of TS on school measures11 but do not support that children with TS may be more likely to repeat a grade or miss school.11,14,17 Using a large nationally representative sample that includes children without TS, the present study has confirmed that children with TS are more likely to have an IEP and school problems and less likely to complete all homework. For many of these children, co-occurring conditions may be largely responsible for the school problems.
The conclusions are subject to certain limitations. All data were based on parent report. Parents reported only known diagnoses, excluding the undiagnosed cases, and the TS rate of 3 per 1000 is lower than the rate of 9 per 1000 found by the community samples.2–4 The survey asked only about TS, and the findings may not extend to other tic disorders. Severity was measured based on parent perception rather than a validated tool. Other disabilities may also have been underreported by parents. However, the school indicators that were most strongly associated with TS were about specific events (i.e., having an IEP, or being contacted by school about problems); it is likely that parents of children with TS would be equally accurate reporters as other parents. The questions about developmental disabilities between 2007 and 2011 changed slightly; however, the number of missed cases in 2007 because of the wording change is likely to be small. As the question about school intervention included only IEP, differences in other accommodations such as 504 plans or school-based intervention services could not be examined. The overall response rate was low; sampling weights were adjusted for possible nonresponse biases.30 Finally, even with 2 large data sets, the sample size was too small to allow for detailed analyses. For example, few children had TS alone or only with learning/language conditions, limiting our ability to understand the effect of TS alone on school success. However, because children with TS most often have other conditions, the findings are relevant to most children with TS. Similarly, although previous studies have shown a specific relationship of attention-deficit/hyperactivity disorder and school problems among children with TS, individual conditions were not examined given the limited sample size and substantial co-occurrence of the conditions. Cell sizes were also insufficient to consider differences in school measures among children with different racial/ethnic backgrounds. As previously reported based on data from the same National Survey of Children's Health, children who are nonwhite, or Hispanic, are less likely than children who are white or non-Hispanic to have a TS diagnosis; this may represent under-diagnosis of TS in minority populations.2,4
Despite these limitations, a comprehensive treatment plan for children with TS can address school functioning. Health care providers', teachers', and parents' awareness of potential school problems and the role of TS and co-occurring MEB or learning and other special education disorder conditions would help to best support the child's education and future health and well-being. Additional education and training may be needed for parents, teachers, and peers to recognize tic symptoms and their impact on the child so that they can support children with TS in school.14,31,32 Education can be an effective way to improve these children's school functioning.32 The Tourette Association of America (www.tourette.org) provides resources for parents, teachers, and health care providers who want to learn more about TS. Future studies are needed to understand the nature of the association between TS and learning, particularly when co-occurring with other conditions, so that appropriate interventions can be developed according to the specific strengths and needs of each child with TS.
Footnotes
Disclosure: The authors declare no conflict of interest.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
See the Video Abstract at jdbp.org
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 2.Bitsko RH, Holbrook JR, Visser SN, et al. A national profile of Tourette Syndrome, 2011-2012. J Dev Behav Pediatr. 2014;35:317–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scharf JM, Miller LL, Gauvin CA, et al. Population prevalence of Tourette syndrome: a systematic review and meta-analysis. Mov Disord. 2015;30:221–228. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Prevalence of diagnosed Tourette syndrome in persons aged 6-17 years—United States, 2007. MMWR Morb Mortal Wkly Rep. 2009;58:581–585. [PubMed] [Google Scholar]
- 5.Burd L, Freeman RD, Klug MG, et al. Tourette syndrome and learning disabilities. BMC Pediatr. 2005;5:34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gorman DA, Thompson N, Plessen KJ, et al. Psychosocial outcome and psychiatric comorbidity in older adolescents with Tourette syndrome: controlled study. Br J Psychiatry. 2010;197:36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cavanna AE, David K, Bandera V, et al. Health-related quality of life in Gilles de la Tourette syndrome: a decade of research. Behav Neurol. 2013;27:83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robinson LR, Bitsko RH, Schieve LA, et al. Tourette syndrome, parenting aggravation, and the contribution of co-occurring conditions among a nationally representative sample. Disabil Health J. 2013;6:26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Storch EA, Murphy TK, Chase RM, et al. Peer victimization in youth with tourette's syndrome and chronic tic disorder: relations with tic severity and internalizing symptoms. J Psychopathol Behav Assess. 2007;29:211–219. [Google Scholar]
- 10.Debes N, Hjalgrim H, Skov L. The presence of attention-deficit hyperactivity disorder (ADHD) and obsessive-compulsive disorder worsen psychosocial and educational problems in tourette syndrome. J Child Neurol. 2010;25:171–181. [DOI] [PubMed] [Google Scholar]
- 11.Abwender DA, Como PG, Kurlan R, et al. School problems in Tourette's syndrome. Arch Neurol. 1996;53:509–511. [DOI] [PubMed] [Google Scholar]
- 12.Packer LE. Tic-related school problems: impact on functioning, accommodations, and interventions. Behav Modif. 2005;29:876–899. [DOI] [PubMed] [Google Scholar]
- 13.Kurlan R, McDermott MP, Deeley C, et al. Prevalence of tics in schoolchildren and association with placement in special education. Neurology. 2001;57:1383–1388. [DOI] [PubMed] [Google Scholar]
- 14.Conelea CA, Woods DW, Zinner SH, et al. Exploring the impact of chronic tic disorders on youth: results from the Tourette Syndrome impact survey. Child Psychiatry Hum Dev. 2011;42:219–242. [DOI] [PubMed] [Google Scholar]
- 15.Zinner SH, Conelea CA, Glew GM, et al. Peer victimization in youth with Tourette syndrome and other chronic tic disorders. Child Psychiatry Hum Dev. 2012;43:124–136. [DOI] [PubMed] [Google Scholar]
- 16.Shady GA, Fulton WA, Champion LM. Tourette syndrome and educational problems in Canada. Neurosci Biobehav Rev. 1988;12:263–265. [DOI] [PubMed] [Google Scholar]
- 17.Comings DE, Comings BG. A controlled study of Tourette syndrome. I. Attention-deficit disorder, learning disorders, and school problems. Am J Hum Genet. 1987;41:701–741. [PMC free article] [PubMed] [Google Scholar]
- 18.De Nil LF, Sasisekaran J, Van Lieshout PHHM, et al. Speech disfluencies in individuals with Tourette syndrome. J Psychosom Res. 2005;58:97–102. [DOI] [PubMed] [Google Scholar]
- 19.Debes NM, Lange T, Jessen TL, et al. Performance on Wechsler intelligence scales in children with Tourette syndrome. Eur J Paediatr Neurol. 2010;15:146–154. [DOI] [PubMed] [Google Scholar]
- 20.Huckeba W, Chapieski L, Hiscock M, et al. Arithmetic performance in children with Tourette syndrome: relative contribution of cognitive and attentional factors. J Clin Exp Neuropsychol. 2008;30:410–420. [DOI] [PubMed] [Google Scholar]
- 21.Brookshire BL, Butler IJ, Ewing-Cobbs L, et al. Neuropsychological characteristics of children with Tourette syndrome: evidence for a nonverbal learning disability? J Clin Exp Neuropsychol. 1994;16:289–302. [DOI] [PubMed] [Google Scholar]
- 22.Eddy CM, Mitchell IJ, Beck SR, et al. Impaired comprehension of nonliteral language in Tourette syndrome. Cogn Behav Neurol. 2010;23:178–184. [DOI] [PubMed] [Google Scholar]
- 23.Schuerholz LJ, Baumgardner TL, Singer HS, et al. Neuropsychological status of children with Tourette's syndrome with and without attention deficit hyperactivity disorder. Neurology. 1996;46:958–965. [DOI] [PubMed] [Google Scholar]
- 24.Kano Y, Ohta M, Nagai Y, et al. Association between Tourette syndrome and comorbidities in Japan. Brain Dev. 2010;32:210–207. [DOI] [PubMed] [Google Scholar]
- 25.Kadesjo B, Gillberg C. Tourette's disorder: epidemiology and comorbidity in primary school children. J Am Acad Child Adolesc Psychiatry. 2000;39:548–555. [DOI] [PubMed] [Google Scholar]
- 26.Schneider J, Gadow K, Crowell J, et al. Anxiety in boys with attention-deficit/hyperactivity disorder with and without chronic multiple tic disorder. J Child Adolesc Psychopharmacol. 2009;19:737–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhu Y, Leung KM, Liu PZ, et al. Comorbid behavioural problems in Tourette's syndrome are positively correlated with the severity of tic symptoms. Aust N Z J Psychiatry. 2006;40:67–73. [DOI] [PubMed] [Google Scholar]
- 28.Wadman R, Glazebrook C, Beer C, et al. Difficulties experienced by young people with Tourette syndrome in secondary school: a mixed methods description of self, parent and staff perspectives. BMC Psychiatry. 2016;16:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leckman JF, Zhang H, Vitale A, et al. Course of tic severity in Tourette syndrome: the first two decades. Pediatrics. 1998;102:14–19. [DOI] [PubMed] [Google Scholar]
- 30.Bramlett MD, Blumberg SJ, Zablotsky B, et al. Design and operation of the National Survey of Children's Health, 2011-2012. Vital Health Stat 1 2017:1–256. [PubMed] [Google Scholar]
- 31.White SW, Sukhodolsky DG, Rains AL, et al. Elementary school teachers' knowledge of Tourette syndrome, obsessive-compulsive disorder, and attention-deficit/hyperactivity disorder: effects of teacher training. J Dev Phys Disabil. 2011;23:5–14. [Google Scholar]
- 32.Nussey C, Pistrang N, Murphy T. How does psychoeducation help? A review of the effects of providing information about Tourette syndrome and attention-deficit/hyperactivity disorder. Child Care Health Dev. 2013;39:617–627. [DOI] [PubMed] [Google Scholar]