Introduction
Rapid, reliable and efficient communication in healthcare systems with finite resources promises to improve patient care. Telephone engagement has effectively monopolised the referral process in the acute setting. Hence, traditional inter-hospital referral networks are potentially time consuming, not expeditious and frustrating. There is often no comprehensive documented communication record or audit trail. Social media, however, suggest that instantaneous, secure and dependable exchanges of information can occur via alternative conduits, potentially transforming the acute clinical referral system. The National On-Call Referral System (NORSe) was established in 2010 as an alternative referral paradigm.
We explore the literature evidence surrounding the clinical impact of the NORSe referral system and analogous models. Early evidence suggests that NORSe may minimise delays in obtaining specialist advice and management, particularly in the acute setting. It enables the specialist to receive and address a large number of fact intense referrals that would otherwise be unpalatable and unmanageable. We summarise recent developments with the NORSe and give an overview of its clinical applications and links with clinical governance.
NORSe and similar models promise to change the way we communicate as doctors, making the process more efficient, with a robust audit trail facilitating service appraisal and training.
Keywords: NORSe, Online referral, Electronic referral
Introduction
There is centralisation within the NHS in the provision of services. Certain specialties and areas of expertise are retained within a number of units. There are, for example, 234 NHS trusts in England;1 however, within the UK only 50 centres provide plastic surgery services.2 There are 30 centres with neurosurgical facilities.3 Patients may therefore present to emergency units without the prerequisite expertise locally for their presenting complaints. Alternatively, they develop conditions while hospitalised for which the admitting hospital does not provide services. The NHS infrastructure requires communication between base hospitals and specialist units. The traditional modes of referral necessitate telephone communication via hospital switchboards, which can be protracted and an imprecise process. Often there is no clear documentation or audit trail of the exchange between the referrer and receiving unit. The introduction of the NORSe seeks to transform and facilitate the communication between acute centres in the UK providing secondary, tertiary and quaternary care.
We interrogated PubMed, Medline and Google Scholar databases for published data on online and electron emergency medical and surgical referral pathways. Our approach included published papers, audits presented at regional meetings and data provided by NORSe providers on on the facilities of NORSe.
The origins of NORSe
The NORSe began in the West Midlands at the University Hospitals of Birmingham NHS Foundation Trust (UHBT) in 2010.4 At that time, the acronym stood for the Neurosurgical On-call Referral System. It was used as a means of facilitating and expediting the referral process to the neurosurgical unit from hospitals within the locality. The clinical lead of the UHBT neurosurgical team recently confirmed that 50% of the workload originates from referrals from other hospitals in the region and, before NORSe, a problem was identified.5
The traditional referral process was inefficient. The referrer would expend significant periods of time waiting for the operator at both the base and specialist hospital. Further time would be expended waiting for the neurosurgeon. The latter could be occupied addressing another referral. In addition, there could be little or no consensus on the content of communication between clinicians. NORSe potentially provided the solution to these dilemmas. Referrals were made online via a secure server through individualised healthcare professional accounts. Communications were received by the specialist, who could then relay the plan to the parent team via the same interface. The system gained plaudits, won awards and was credited for reducing costs in neurosurgery at the foundation trust.6 Following local success and popularity, the UHBT in collaboration with the information technology service provider Intouch with Health sought to disseminate the system throughout the UK.
The Current NORSe
In the current manifestation of the NORSe, individual healthcare professionals create an account on the NORSe referral portal. In the West Midlands, this is accessed through a weblink.7 The registration process requires clinicians to submit NHS mail account details and a mobile telephone number both of which are then linked to this account and acts as a basis of communication and alerting the clinician as to when new information has been added to the NORSe account. The portal will only accept NHS mail email addresses for registration purposes. The Department of Health in the UK has specifically approved NHS mail as secure email service for the transmission of patient information.8
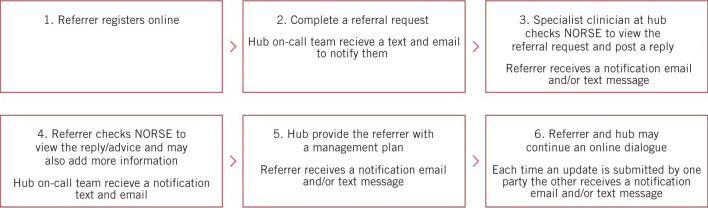
Referrals are made through personal accounts. The process occurs according to the schema shown in Figures 1 and 2.9,10 Both written information and pictures can be transferred. At the specialist centre the team receives notification as soon as a referral is made through mobile devices such as telephones. The specialist unit can respond in a variety of ways. They can request further images, ask for further investigations, recommend treatments, request transfers. Similarly, the referrer is notified when new information is added to their NORSe account via text message and email. Although referrals are made through personalised accounts other clinicians can be added to the referral pathway by the original referrer. They are then able to access the details of the NORSe referral and enter data themselves. This is significant because it allows continuity of care even in the context of shift work.
Figure 1.
The NORSe referral process
Figure 2.
The Norse referral process for specialist clinicians
The system has several advantages. It:
avoids delay at switchboard, which benefits all switchboard users at both sites
avoids delay with waiting for the specialist
avoids the situation where the specialist is occupied with another referral
provides a robust documentation trail of the content of the referral made by the referrer (avoiding errors in reciprocal documentation)
provides robust documentation of the advice from the specialist by the specialities (avoiding errors in reciprocal documentation) to which both referrer and specialist can refer
allow for effective division of labour at both specialist and referral centres.
Clinical applications
NORSe has been applied to a number of specialties. The system is well suited to plastic surgery and hand trauma in cases where patients present to units without this expertise on site. It is currently also used for pelvic–acetabular trauma surgical advice. A renal referral service is also available in certain regions where patients may require dialysis or sophisticated investigation. The system does not exclude the possibility of verbal communication if it is considered that instantaneous guidance is required. The interface lends itself potentially less well to certain specialities where the acuity of presentation may warrant more expeditious communication. This could include vascular surgery in patients with acute ischaemia or abdominal aortic aneurysm disease. However, even in this speciality, patients presenting with the sequel of critical ischaemia or subacute ischaemia might be suited to this referral pathway.
There are disciplines where the systems could have potentially significant benefits and as such remains an untapped resource. Notable examples include oncology in instances of suspected metastatic spinal cord compression (MSCC). The National Institute for Health and Care Excellence (NICE) guidelines create the role of the MSCC coordinator, who is to be the first point of contact in instances of suspected MSCC, with support from the senior clinical advisor.11,12 The guidance advocates a telephone triage to assess the need and urgency of investigations, transfer and treatment. With the formation of strategic clinical networks by the Health and Social Care Act 2012 such clinicians may reside in larger centres and may not be available onsite at every trust.13 The NICE guidance expressly requires that there exists a robust and dependable referral infrastructure for MSCC. However, there remains a general lack of awareness regarding MSCC referral pathways, with referrals, at times, being made primarily to very junior clinicians in trauma and orthopaedics.14 The quantity and referral source diversity of MSCC lends itself well to NORSe.
NORSe has features that facilitate patient data handling and work patterns in the NHS. It has the capacity to generate a ‘handover report‘ with a list of active referrals. The report contains clinical details such that it can operate as a handover document and tracks the stage of patients through the management process.9 NORSe can also produce a ‘waiting list view’ capturing patients who are awaiting transfer to the specialist unit or repatriation to the parent centre.9 It can also be used for educational and appraisal purposes, as it allows users to record and collate the entirety of their referrals through the NORSe portal and the final disposition clinical advice requests.
The law and information governance
NORSe abides by the Caldicott principles of patient information, in particular the requirement that the access to patient information should be on a strict need to know basis.15 The Health and Social Care Act 2012 legislated for the creation of the Health and Social Care Information Centre. The latter became NHS Digital.16 This body provides guidance and promotes the effective and secure use of information technology to facilitate the provision of healthcare. NHS Digital awards Milestone Achievement certification to products that satisfy their validations and verification tests.17 Information technology products are evaluated on a number of parameters relating to utility, functionality and safety. These successful interfaces then enter a Compliance Catalogue.18 NORSe is ostensibly not on this list. However, the network satisfies a number of NHS Digital requirements, notably using the same secure socket layer (SSL) encryption facility.19
Other models
Individual trusts, regions and hospital clusters are developing their own online referral systems. As yet there is no single model that is universally used. The advantage of this is that each model is specifically adapted to the specific needs of each particular area and healthcare nexus. However, significant saving may potentially be achieved with a single system that is trialled and refined in a single strategical clinical network and then applied incrementally across the UK. NHS digital would be in a unique position to orchestrate a similar venture. The difficulty lies in the fact that there exist a number of inveterate systems in the UK. In Oxford, the Oxford Acute Referral System is currently operative. In North Yorkshire, Referapatient by Bloomsbury Health is the favoured model.20
Studies based on prototypes of the current referral models show significant benefits in the form of clinician efficiency and time saving. Neurosurgeons at the National Hospital for Neurology and Neurosurgery, London, compared two 14-day periods before and after implementation of an online referral system.21 One immediate advantage reported was that the on-call bleep was freed for urgent and immediate communications. Following introduction of an electronic referral process the percentage of missed bleeps fell from 16% to 9%. The number of calls received from referrers requesting further clarification fell by half from 10 to 5 calls per day. Documentation of new referrals increased from 43% to 85% with responses to referrals rising from 74% to 98%. Average response times fell from 148 to 24 minutes.22 An internal audit at St Bartholomew Hospital, London, found similar results. However, tellingly, they found that a more expeditious referral pathway resulted in fewer unnecessary admissions, which fell from 94% to 24% for neurosurgical patients.22 Hence, the introduction of the system facilitated the referral process and promoted safe practice. Indeed, prior to the advent of an electronic referral system some had questioned if free neurosurgical services were sustainable within the current NHS infrastructure given the time and personal sequestered in attending to emergency referrals.23
The NHS has at times been criticised for not embracing technology. However, NORSe provides an innovative means of connecting clinicians facilitating and expediting patient care. Its arrival is timely given the 2014 NHS England forecast document Five-Year Forward View predicts a greater need for specialist centres, particularly in instances where outcomes are linked to patient volume.24 Telephone engagement need no longer be the exclusive means of telecommunication. New modes may provide efficient and effective alternatives provided patient data and safety are protected. NORSe and analogous programmes represent an opportunity to exploit similar technology to that used in high-fidelity, high-volume, rapid social media models for the benefit of healthcare. It has parallels with WhatsApp and may be a forerunner of a healthcare manifestation of this popular communication paradigm.
References
- 1.NHS Choices Authorities and trusts. http://www.nhs.uk/servicedirectories/pages/nhstrustlisting.aspx (cited January 2018).
- 2.British Association of Plastic Reconstructive and Aesthetic Surgeons Plastic surgery in the UK. http://www.bapras.org.uk/public/about-plastic-surgery/plastic-surgery-in-the-uk (cited January 2018).
- 3.Society of British Neurological Surgeons Neurosurgical units. http://www.sbns.org.uk/index.php/neurosurgical-units (cited January 2018).
- 4.Digital Health UHB commercialises online referral tool. https://www.digitalhealth.net/2015/05/uhb-commercialises-online-referral-tool (cited January 2018).
- 5.NORSe Network On-Call Referral Service. Cirencester: Intouch with Health; 2016. http://www.intouchwithhealth.co.uk/wp-content/uploads/2016/11/NORSe-Flyer-v4.pdf (cited January 2018). [Google Scholar]
- 6.Building Better Health Neurological On-call Referral System wins award. 30 March 2012. http://www.buildingbetterhealthcare.co.uk/news/article_page/Neurological_Oncall_Referral_System_wins_award/77160 (cited January 2018).
- 7.West Midlands NORSe referral portal. https://nww.norse.uhb.nhs.uk/login.aspx.
- 8.NHS Digital NHSmail. https://digital.nhs.uk/nhsmail (cited January 2018).
- 9.NORSe National On-call Referral Service: how NORSE works. http://www.urgentnorse.org/how-norse-works.aspx (cited January 2018).
- 10.NORSe National On-call Referral Service: specialists. http://www.urgentnorse.org/specialists.aspx (cited January 2018).
- 11.National Institute for Health and Care Excellence Metastatic Spinal Cord Compression in Adults: Risk Assessment, Diagnosis and Management. Clinical Guideline CG75. London: NICE; 2008. [PubMed] [Google Scholar]
- 12.Al-Qurainy R, Collis E. Metastatic spinal cord compression: diagnosis and management. 2016; : i2,539. [DOI] [PubMed] [Google Scholar]
- 13.National Cancer Registration and Analysis Service. UK Cancer e-Atlas – Guide. http://www.ncin.org.uk/cancer_information_tools/eatlas/guide (cited January 2018).
- 14.Brooks FM, Ghatahora A, Brooks MC et al. Management of metastatic spinal cord compression: awareness of NICE guidance. 2014; (Suppl 1): S255–S259. [DOI] [PubMed] [Google Scholar]
- 15.Taylor P. Caldicott 2 and patient data. 2013; : f226. [DOI] [PubMed] [Google Scholar]
- 16.NHS Digital About us. https://digital.nhs.uk/about-nhs-digital (cited January 2018).
- 17.NHS Digital Solution assurance. https://digital.nhs.uk/solution-assurance (cited January 2018).
- 18.NHS Digital Compliance catalogue. https://digital.nhs.uk/solution-assurance/compliance-catalogue (cited January 2018).
- 19.NHS Digital Services supported by the SSD team. https://digital.nhs.uk/services-SSD http://www.ouh.nhs.uk/services/oars/default.aspx (cited January 2018).
- 20.Matloob SA, Hyam JA, Thorne L, Bradford R. Improving neurosurgical communication and reducing risk and registrar burden using a novel online database referral platform. 2016; : 191–194. [DOI] [PubMed] [Google Scholar]
- 21.Oxford University Hospitals Oxford Acute Referral System (OARS). http://www.ouh.nhs.uk/services/oars/default.aspx (cited January 2018).
- 22.Elyas A, Kostisiak M, Prasad V, Paraskevopolous D. Improving communication and reducing risk in a Neurosurgery Unit using an online acute referral system. Barts Health NHS Trust Neurosurgery Referral Audit. https://www.bloomsburyhealth.org/renal (cited January 2018).
- 23.Holsgrove DT, Johnston NJ, Leggate JR. On-call neurosurgery: can this continue as a free service? 2011; (4): 475–477. [DOI] [PubMed] [Google Scholar]
- 24.NHS . London: NHS; 2014. [Google Scholar]