Abstract
Background
Kidney impairment constitutes severe risk for cardiovascular disease, stroke and all-cause mortality, and early identification and prevention of kidney impairment is critical to effective management of prognostic risk in community residents. Previous studies have validated that carotid-femoral pulse wave velocity (cfPWV) is a significant factor associated with chronic kidney disease. However, whether cfPWV is associated with moderately reduced glomerular filtration rate (GFR) remains unclear. This analysis was designed to examine the association of moderately reduced GFR with cfPWV and central pulse pressure (cPP) in Chinese middle-aged and elderly community residents.
Methods
There were 875 community residents enrolled in this analysis, and then cfPWV and cPP were assessed in all participants following the standard procedure.
Results
Entire cohort had a median (range) age of 66 (45–88) years, and 65.4% were women. Both cfPWV and cPP differed significantly between participants with and without moderately reduced GFR (P < 0.05 for all). Logistic regression analyses indicated that cfPWV and cPP had the significant association with moderately reduced GFR (P < 0.05 for all).
Conclusion
This analysis demonstrated the significant association of cfPWV and cPP with moderately reduced GFR in Chinese middle-aged and elderly community residents.
Keywords: Carotid-femoral pulse wave velocity, Central pulse pressure, Moderately reduced glomerular filtration rate
Background
Kidney impairment constitutes severe risk for cardiovascular disease, stroke and all-cause mortality, and early identification and prevention of kidney impairment are critical to effective management of prognostic risk in community residents. Recently, more and more attention has been given to the association of arterial stiffness and central hemodynamics with kidney impairment, especially early kidney impairment [1]. Previous studies have validated that carotid-femoral pulse wave velocity (cfPWV) can serve as not only a noninvasive measure of central artery stiffness, but also a significant factor associated with chronic kidney disease (CKD) [2–4]. However, whether cfPWV is associated with moderately reduced glomerular filtration rate (GFR) remains unclear, especially in Chinese middle-aged and elderly community residents. Further studies are needed to assess the association between cfPWV and moderately reduced GFR.
Several reports have indicated the evidence of CKD present in patients with abnormal central hemodynamics indicated by elevated central pulse pressure (cPP) [5–7]. Moreover, recent study has suggested that cPP rather than peripheral pulse pressure (pPP) is reflective of CKD [8]. However, whether both cPP and pPP are closely associated with moderately reduced GFR is unclear, especially in Chinese middle-aged and elderly community residents. Thus, this analysis was designed to: 1) assess the association between cfPWV and moderately reduced GFR; and 2) observe the cPP and pPP in their association with moderately reduced GFR in Chinese middle-aged and elderly community residents.
Methods
Study population
There were 937 participants aged 45 years and older in this analysis. According to the stratified cluster sampling design of health check-up program from May 2007 to July 2009, all participants were permanent residents of four communities in three districts (Fengtai, Shijingshan and Daxing) of Beijing, China. Of those participants, 62 participants had GFR below 60 ml/min/1.73 m2. Therefore, this analysis had 875 participants. This analysis was approved by Ethics Committee of Chinese People’s Liberation Army General Hospital (Beijing, China). Written consent was obtained from each participant.
Arterial stiffness and hemodynamics
Following the standard procedures, peripheral blood pressure was measured on brachial artery with mercury sphygmomanometer (Yuwell medical equipment & supply Co., Ltd., Jiangsu, China). Blood pressure was measured in duplicate and averaged. Pulse pressure (PP) was calculated as systolic blood pressure minus diastolic blood pressure. Participants with systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg or hypotensive drugs were regarded to have hypertension. Arterial stiffness was evaluated by a device designed for automatic cfPWV analysis (Createch Industrie, Garges les Gonesse, France). Radial artery pressure waveform was evaluated by a device designed for automatic pulse wave analysis (SphygmoCor, Sydney, Australia), and the corresponding cPP was calculated with its transfer function. Their technical characteristics have been described previously [9].
Laboratory examination
Blood sample was drawn in the morning after the overnight fasting and examined by central laboratory on the same date. Concentrations of fasting plasma glucose (FPG), triglyceride, high-density lipoprotein-cholesterol (HDL-c), low-density lipoprotein-cholesterol (LDL-c) and serum creatinine were examined with enzymatic assays (Roche Products Ltd., Basel, Switzerland). Diabetes mellitus referred to those with FBG ≥ 7.0 mmol/L or hypoglycemic treatment. Chinese modified Modification of Diet in Renal Disease equation was used as an evaluation of GFR: 175 × serum creatinine (mg/dL)-1.234 × age (year)-0.179 × 0.79 (if female) [10]. Range of moderately reduced GFR was from 60 mL/min/1.73m2 to 89 mL/min/1.73m2. Laboratory examination was completed by qualified technicians without knowledge of clinical information.
Statistical analysis
Statistical analysis was implemented with Statistical Package for the Social Science version 17 (SPSS, Inc., Chicago, IL, USA). Categorical data were reported as number and percentage. Continuous data were reported as mean and standard deviation for variables with a normal distribution, and median and interquartile range for non-normally distributed variables. Difference between groups was assessed by Student’s t-test for continuous data with a normal distribution, Mann–Whitney U test for non-normally distributed data and x2 test for categorical data. Pearson’s correlation for continuous variables with normal distribution and Spearman’s correlation for categorical variables were used to evaluate their simple correlation of GFR with cfPWV and PP. Logistic regression analysis (Enter) was used to evaluate multivariate association of cfPWV and PP with moderately reduced GFR after adjustment of age, HDL-c and LDL-c. Age, HDL-c and LDL-c, rather than gender, hypertension, diabetes mellitus, FPG and triglyceride, were significant in univariate analysis with moderately reduced GFR, and included as the adjustment of multivariate analysis with moderately reduced GFR. Two-sided P value < 0.05 was accepted as significant.
Results
Entire cohort had a median (range) age of 66 (45–88) years, and 65.4% (572 participants) were women. Prevalence of hypertension and diabetes mellitus were 52.7% (461 participants) and 24.3% (213 participants), respectively. Characteristics of the study cohort with and without moderately reduced GFR were depicted in Table 1. Age, HDL-c and LDL-c were significantly different between participants with and without moderately reduced GFR (P < 0.05 for all). cfPWV differed significantly between participants with and without moderately reduced GFR (P < 0.05). Both cPP and pPP had the significant difference between participants with and without moderately reduced GFR (P < 0.05 for all).
Table 1.
Characteristics of the study cohort with and without moderately reduced GFR
| Characteristics | Normal GFR (n = 370) | moderately reduced GFR (n = 505) | P value |
|---|---|---|---|
| Age (year)a | 65(60–70) | 67(62-72) | < 0.001 |
| Males (%) | 121(32.7) | 182(36.0) | 0.305 |
| Hypertension (%) | 184(49.7) | 277(54.9) | 0.134 |
| Diabetes mellitus (%) | 102(27.6) | 111(22.0) | 0.057 |
| pPP (mmHg)a | 50(40–60) | 55(46-65) | < 0.001 |
| FPG (mmol/L)a | 5.1(4.4-5.8) | 5.0(4.4–5.8) | 0.969 |
| Triglyceride (mmol/L)a | 1.5(1.2-2.2) | 1.5(1.2–2.1) | 0.616 |
| HDL-c (mmol/L)a | 1.4(1.1-1.6) | 1.3(1.1–1.6) | 0.030 |
| LDL-c (mmol/L)a | 3.0(2.5-3.4) | 3.1(2.6–3.5) | 0.014 |
| GFR (ml/min/1.73 m2)a | 101.6(94.5–113.9) | 80.1(74.2–85.2) | < 0.001 |
| cfPWV (m/s)a | 11(10–13) | 12(10-15) | < 0.001 |
| cPP (mmHg)a | 42(35–51) | 46(38-56) | < 0.001 |
amedian (interquartile range)
GFR glomerular filtration rate, pPP peripheral pulse pressure, FPG fasting plasma glucose, HDL-c high-density lipoprotein-cholesterol, LDL-c low-density lipoprotein-cholesterol, cfPWV carotid-femoral pulse wave velocity, cPP central pulse pressure
Either two of cfPWV, cPP and pPP were significantly correlated with each other (P < 0.001 for all; cfPWV and cPP: r = 0.368; cfPWV and pPP: r = 0.374; cPP and pPP: r = 0.797) (See Fig. 1). GFR was significantly correlated with age, HDL-c, LDL-c, cfPWV, cPP and pPP (P < 0.05 for all). Simple correlation and multivariate association of cfPWV and PP with moderately reduced GFR were shown in Table 2. In Logistic regression analyses, age, HDL-c and LDL-c were significantly associated with moderately reduced GFR (P < 0.05 for all). cfPWV had the significant association with moderately reduced GFR (P < 0.05). There was the significant association of cPP and pPP with moderately reduced GFR (P < 0.05 for all).
Fig. 1.
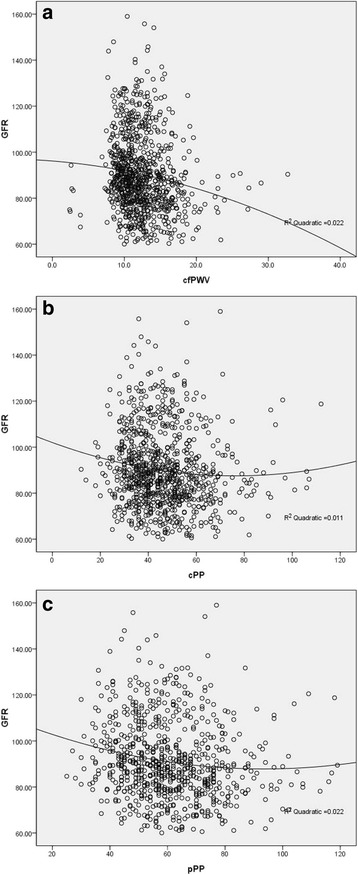
a scatter plot between GFR and cfPWV; b scatter plot between GFR and cPP; c scatter plot between GFR and pPP. GFR: glomerular filtration rate; cfPWV: carotid-femoral pulse wave velocity; cPP: central pulse pressure; pPP: peripheral pulse pressure
Table 2.
Association of cfPWV and PP with moderately reduced GFR in Logistic regression analyses
| Variables | r value | P value | HR value (95%CI) | P value | |
|---|---|---|---|---|---|
| cfPWV model | Age (year) | −0.195 | < 0.001 | 1.026(1.004–1.048) | 0.018 |
| HDL-c (mmol/L) | 0.101 | 0.003 | 0.682(0.479–0.970) | 0.033 | |
| LDL-c (mmol/L) | −0.080 | 0.017 | 1.237(1.023–1.494) | 0.028 | |
| cfPWV (m/s) | −0.179 | < 0.001 | 1.066(1.013–1.121) | 0.014 | |
| cPP model | Age (year) | −0.195 | < 0.001 | 1.027(1.006–1.049) | 0.011 |
| HDL-c (mmol/L) | 0.101 | 0.003 | 0.685(0.482–0.974) | 0.035 | |
| LDL-c (mmol/L) | −0.080 | 0.017 | 1.238(1.024–1.495) | 0.027 | |
| cPP (mmHg) | −0.132 | < 0.001 | 1.015(1.004–1.026) | 0.009 | |
| pPP model | Age (year) | −0.195 | < 0.001 | 1.030(1.009–1.051) | 0.004 |
| HDL-c (mmol/L) | 0.101 | 0.003 | 0.687(0.483–0.977) | 0.037 | |
| LDL-c (mmol/L) | −0.080 | 0.017 | 1.242(1.027–1.501) | 0.025 | |
| pPP (mmHg) | −0.172 | < 0.001 | 1.012(1.003–1.022) | 0.012 |
cfPWV carotid-femoral pulse wave velocity, PP pulse pressure, GFR glomerular filtration rate, HRhazard ratio, CI confidence interval, cPP central pulse pressure, pPP peripheral pulse pressure, HDL-c high-density lipoprotein-cholesterol, LDL-c low-density lipoprotein-cholesterol
Discussion
This analysis had two main findings in Chinese middle-aged and elderly community residents: firstly, cfPWV was significantly associated with moderately reduced GFR; secondly, both cPP and pPP had the significant association with moderately reduced GFR.
cfPWV is a noninvasive representative of central arterial stiffness [2, 4]. In previous studies, cfPWV has been shown to be closely linked to CKD [1, 3]. There were the scarce and controversial studies appraising the relationship of cfPWV with moderately reduced GFR, and it is necessary to determine the association of cfPWV with moderately reduced GFR, especially in Chinese middle-aged and elderly community residents [11]. This analysis confirmed that the significant association existed between cfPWV and moderately reduced GFR.
Central and peripheral hemodynamics are commonly assessed by cPP and pPP, respectively. Previous researches have realized that increased cPP rather than pPP correlated with reduced kidney blood flow and GFR in patients with CKD, and even in those after kidney transplantation [5–8]. However, it is uncertain for the association of cPP and pPP with moderately reduced GFR, especially in Chinese middle-aged and elderly community residents. This analysis found that both cPP and pPP were significantly associated with moderately reduced GFR in Chinese middle-aged and elderly community residents. Association of moderately reduced GFR with cfPWV, cPP and pPP was all significant in this analysis, and future studies are needed to evaluate the relative value of theses methods in evaluating arterial function.
Conclusion
This analysis demonstrated the significant association between cfPWV and moderately reduced GFR. Meanwhile, both cPP and pPP were significantly associated with moderately reduced GFR in Chinese middle-aged and elderly community residents.
Acknowledgments
We appreciated all the participants for their contribution to this study.
Funding
This work was supported by grants from National Key Basic Research Project (2012CB517503 and 2013CB530804), Health Special Scientific Research Project of Chinese People’s Liberation Army (12BJZ34 and 14BJZ12), Sanya Medical and Health Science and Technology Innovation Project (2016YW21), and Clinical Scientific Research Supporting Fund of Chinese People’s Liberation Army General Hospital (2017FC-CXYY-3009). The funding bodies played no role in study design, data acquisition, analysis and interpretation or manuscript preparation and submission.
Availability of data and materials
In attempt to preserve the privacy of patients, clinical data of patients will not be shared. The datasets used during this analysis are available from the corresponding author on reasonable request.
Abbreviations
- cfPWV
carotid-femoral pulse wave velocity
- CKD
chronic kidney disease
- cPP
central pulse pressure
- FPG
fasting plasma glucose
- GFR
glomerular filtration rate
- HDL-c
high-density lipoprotein-cholesterol
- LDL-c
low-density lipoprotein-cholesterol
- pPP
peripheral pulse pressure
- SPSS
Statistical Package for the Social Science
Authors’ contributions
FS, GY, LLM, YP: contributed to the design of study, performed the data collection and statistical analyses, and drafted the paper. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This analysis was approved by Ethics Committee of Chinese People’s Liberation Army General Hospital (Beijing, China). Written consent was obtained from each participant. Declaration of Helsinki was followed while conducting this analysis.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shihui Fu, Email: xiaoxiao0915@126.com.
Yi Guo, Email: guoyi612@126.com.
Leiming Luo, Phone: 86-10-88 626 362, Email: lleim@sina.com.
Ping Ye, Phone: 86-10-88 626 362, Email: sci301@126.com.
References
- 1.Pannier B, Guerin AP, Marchais SJ, et al. Stiffness of capacitive and conduit arteries: prognostic significance for end-stage renal disease patients. Hypertension. 2005;45:592–596. doi: 10.1161/01.HYP.0000159190.71253.c3. [DOI] [PubMed] [Google Scholar]
- 2.Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–2605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 3.Ohya Y, Iseki K, Iseki C, et al. Increased pulse wave velocity is associated with low creatinine clearance and proteinuria in a screened cohort. Am J Kidney Dis. 2006;47:790–797. doi: 10.1053/j.ajkd.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 4.Tillin T, Chambers J, Malik I, et al. Measurement of pulse wave velocity: site matters. J Hypertens. 2007;25:383–389. doi: 10.1097/HJH.0b013e3280115bea. [DOI] [PubMed] [Google Scholar]
- 5.M T, Jankowski P, Peltier M, et al. Intraaortic pulse pressure amplification in subjects at high coronary risk. Hypertension. 2010;55:327–332. doi: 10.1161/HYPERTENSIONAHA.109.142851. [DOI] [PubMed] [Google Scholar]
- 6.Wang KL, Cheng HM, Chuang SY, et al. Central or peripheral systolic or pulse pressure: which best relates to target organs and future mortality? J Hypertens. 2009;27:461–467. doi: 10.1097/HJH.0b013e3283220ea4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fesler P, Safar ME, du Cailar G, et al. Pulse pressure is an independent determinant of renal function decline during treatment of essential hypertension. J Hypertens. 2007;25:1915–1920. doi: 10.1097/HJH.0b013e3281fbd15e. [DOI] [PubMed] [Google Scholar]
- 8.Neisius U, Bilo G, Taurino C, et al. Association of central and peripheral pulse pressure with intermediate cardiovascular phenotypes. J Hypertens. 2012;30:67–74. doi: 10.1097/HJH.0b013e32834e12d8. [DOI] [PubMed] [Google Scholar]
- 9.Asmar R, Benetos A, Topouchian J, et al. Assessment of arterial distensibility by automatic pulse wave velocity measurement.Validation and clinical application studies. Hypertension. 1995;26:485–490. doi: 10.1161/01.HYP.26.3.485. [DOI] [PubMed] [Google Scholar]
- 10.Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–2944. doi: 10.1681/ASN.2006040368. [DOI] [PubMed] [Google Scholar]
- 11.Upadhyay A, Hwang SJ, Mitchell GF, et al. Arterial stiffness in mild-to-moderate CKD. J Am Soc Nephrol. 2009;20:2044–2053. doi: 10.1681/ASN.2009010074. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
In attempt to preserve the privacy of patients, clinical data of patients will not be shared. The datasets used during this analysis are available from the corresponding author on reasonable request.


