Abstract
Marked by difficulty falling or staying asleep and/or poor sleep leading to daytime dysfunction, insomnia contributes to functional impairment, poor health, and increased healthcare utilization when left untreated. As many as two-thirds of Iraq and Afghanistan military veterans complain of insomnia. Older veterans of prior conflicts report insomnia occurring since initial service, suggesting a chronic nature to insomnia in this population. Despite insomnia’s high prevalence and severe consequences, there is no theoretical model to explain either the onset or chronicity of insomnia in this growing patient population. Existing theories view insomnia as an acute, unidirectional phenomenon and do little to elucidate long-term consequences of such problems. Existing theories also fail to address mechanisms by which acute insomnia becomes chronic. This paper presents an original, integrated theoretical model that draws upon constructs from several prominent behavioral medicine theories to reconceptualize insomnia as a chronic, cyclical problem that is both a consequence and predictor of stress. Additional research examining the relationships between stress, sleep, resilience, and outcomes of interest could inform clinical and research practices. Addressing sleep problems early could potentially enhance adaptive capacity, thereby reducing the risk for subsequent negative outcomes.
Keywords: insomnia, sleep, stress, coping, resilience, veterans
Sleep is a basic biological need responsible for a range of restorative functions including emotion regulation and memory consolidation, muscle and tissue repair, and stress hormone regulation (Dement & Vaughan, 1999). Despite its necessity, sleep is often ignored as a core health behavior, rarely addressed within biopsychosocial assessments or routine primary care visits, and generally not integrated into chronic disease management programs. Sleep problems are particularly common among United States military veterans, with one-half to two-thirds of the 2.5 million U.S. military troops who served in Afghanistan (Operation Enduring Freedom, OEF) and Iraq (Operation Iraqi Freedom, OIF) complain of insomnia problems on returning home (Amin, Parisi, Gold, & Gold, 2010; Seelig et al., 2011). Insomnia complaints are also prevalent among veterans of earlier wars, including Vietnam and Korea conflicts. Additionally, many of these older veterans report that sleep problems initially began during or immediately following their military service and have persisted in the decades since separating from the military (Hughes & Martin, 2015; Ryden et al., 2015).
These findings suggest insomnia problems are chronic within veteran populations; yet, a lack of longitudinal data prohibits researchers from identifying mechanisms that contribute to such chronicity and from understanding how such problems change over a veteran’s life course. Given sleep problems are tied to a number of negative physical and psychological outcomes (Fernandez-Mendoza & Vgontzas, 2013), it is critical that researchers and clinicians develop a better understanding of this growing problem. The overarching goal of this paper is to offer a theoretical model of insomnia in the veteran population. Although this model can be applied to veterans of all ages and military cohorts, a major goal of the model is to place insomnia-like sleep problems of returning OEF/OIF veterans into a larger, lifespan context as a means of advocating for additional research on the role sleep problems may play in longterm health and aging. While military-specific stressors will be addressed, we believe that elements of this integrated model can be applied to other patient populations, including those who have experienced significant stress or trauma.
Insomnia in Military Veterans
Chronic Insomnia Disorder is a common behavioral sleep disorder clinically defined as dissatisfaction with sleep quantity or quality marked by complaints of difficulty falling or staying asleep, waking up earlier than desired, or sleep that is non-restorative and the cause of significant daytime impairment. Such problems are not related to other medical or sleep disorders, exist despite adequate opportunity and environment for sleep, and are endorsed three or more nights per week for three months or longer (American Psychiatric Association, 2013). Insomnia and/or insomnia-like symptoms are present in 27–54% of military personnel and veterans (Hoge, W. et al., 2008; Mysliwiec, McGraw, Smith, Trapp, & Roth, 2013), rates that are two to three times higher than in the general U.S. adult population (Ford, Cunningham, Giles, & Croft, 2015; Roth, 2007). The rate of incident insomnia cases in military personnel saw a 19-fold increase from 2000 to 2009 (Mysliwiec et al., 2013). The prevalence of insomnia among Veterans Health Administration (VHA) users is expected to continue to rise as many troops who served after September 11, 2001 continue to retire from military service and begin accessing VHA healthcare in the coming years (Campbell, Shattuck, Germain, & Mysliwiec, 2015).
Risk Factors
Both modifiable and non-modifiable risk factors contribute to insomnia. This paper addresses the role of stress regulation and coping in sleep problems with a behavioral etiology. Insomnia-like sleep problems may be a function of an individual’s stress response whereby poor sleep is a function of inadequate coping and/or poor regulation of stress across physiological, cognitive, and/or emotional processes. In this context, stress refers to any event or stimulus that causes a disruption in balance, or homeostasis. Laboratory studies indicate that higher baseline levels of stress reactivity are associated with insomnia and predict future cases of the disorder (Drake, Friedman, Wright, & Roth, 2011; Drake, Richardson, Roerhs, Scofield, & Roth, 2004). In addition, individuals with insomnia have been shown to report experiencing more daily stressors and negatively evaluating such stressors (Morin & Ivers, 2003).
Initial military involvement, including enlistment and basic training, present a range of different stressors and often trigger sleep disturbance due to irregular schedules and ongoing physical, social, and emotional demands (Peterson, Goodie, Satterfield, & Brim, 2008). Deployment to a war region typically requires several days of laborious travel and crossing of multiple time zones that can disrupt one’s natural circadian rhythm, or sleep schedule, and trigger sleep difficulties (Troxel et al., 2015). Deployment typically involves irregular work schedules, overnight watch demands, exposure to warzone and combat-related stressors, and risk of physical and psychological injury, including traumatic brain injury. While no research has formally documented the cause, or trajectory, of insomnia in military personnel, it is likely that one or more of the aforementioned factors served as an initial trigger of insomnia symptoms.
Recent research has focused on sleep problems among active duty military personnel, including increasing rates of incident insomnia and sleep apnea diagnoses (Mysliwiec et al., 2013), heightened mental health risks associated with insomnia symptoms (Gehrman et al., 2013), and the link between sleep and impaired work performance (Seelig et al., 2016; Troxel et al., 2015). Less research has focused on sleep after military retirement. Stressors related to military separation, or retirement, and reintegration into civilian life can also trigger insomnia (Bramoweth & Germain, 2013). Additionally, many service members experience an inability to return to a “normal” sleep schedule after experiencing short sleep duration or irregular schedules while deployed (Castro, Kintzle, & Hassan, 2015; Haynes, Parthasarathy, Bootzin, & Krakow, 2013). Additional reintegration-related stressors include readjustment to family and social circles, securing civilian employment, maintaining financial stability, and living with the physical and psychiatric comorbidities caused by deployment or combat-related stressors. These stressors can cause difficulty falling or staying asleep, or sleep that is restless and disturbed, thereby creating new sleep problems or exacerbating existing problems that began prior to or during deployment.
Consequences of Insomnia
Persistent insomnia can lead to poor health outcomes and chronic conditions (Fernandez-Mendoza & Vgontzas, 2013; Taylor et al., 2007), exacerbate symptoms of traumatic brain injury (Macera, Aralis, Rauch, & MacGregor, 2013), reduce overall quality-of-life (Katz & McHorney, 2002), and increase risk for morbidity and premature mortality (Dew et al., 2003; Kripke, Garfinkel, Wingard, Klauber, & Marler, 2002). Chronic sleep problems can also negatively impact day-to-day outcomes including task performance (Pilcher & Huffcutt, 1996), stress coping (Hamilton, Delwyn, & Karlson, 2007), and management of chronic health conditions (Ahn, Jiang, Smith, & Ory, 2014).
Function, Performance and Health Management
Chronic insomnia impairs function and performance across cognitive, emotional, social, and physical domains (Killgore, Balkin, & Westensten, 2006; Killgore et al., 2008; Pilcher & Huffcutt, 1996). Adequate functioning in these areas enables veterans to adapt to and cope with daily hassles and reintegration stressors noted earlier. However, impairments in one or more domains can reduce ability to cope with acute and ongoing stressors. As a result, functional performance and independence decline, thereby decreasing the likelihood of successful reintegration into civilian life (Institute of Medicine, 2013; Pilcher & Huffcutt, 1996).
Many of these aforementioned impairments can also reduce a veteran’s capacity to cope with health-related stressors, a concept of particular interest to clinicians and health services researchers within the VHA. Medically complex patients, defined as individuals with two or more chronic conditions, who are challenged by managing such conditions (Shippee, Shah, May, Mair, & Montori, 2012), represent a growing subgroup of veterans utilizing VHA healthcare (Yoon, Schott, Phibbs, & Wagner, 2011; Yu et al., 2003). Medical complexity is often marked by a cycle of ongoing acute and chronic health-related stressors. Patients cycle through these stressors and strive to achieve and maintain a balance between workload demands (i.e. management of chronic diseases) and physical and psychological resources (Zullig et al., 2016). Successful balance and management of stressors is bolstered by high physical and psychological reserve and capacity (Zullig et al., 2016). These new models of complexity support the idea that capacity is malleable and can be impacted by resources, behaviors, and events on individual and community levels. Although sleep problems, including insomnia, are gaining more attention within the VHA, sleep patterns and behaviors are not explicitly addressed in these models.
Mental Health
Insomnia symptoms are common among veterans with mental health disorders. In one study, more than three-quarters reported difficulty falling or staying asleep and just over one-half reported being at least moderately distressed about sleep that was restless or disturbed (Ulmer et al., 2015). Although this research sample was designed to over-recruit veterans with mental health symptoms, this same study drew attention to the notably high prevalence of sleep difficulties in veterans without a mental health diagnosis, including approximately seventy percent who met clinical criteria for poor sleep quality, defined as a score of five or greater on the Pittsburgh Sleep Quality Index (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989).
The high rate of sleep problems among veterans without mental health diagnoses is alarming given that research with veteran and non-veteran populations has found that chronic sleep problems predict incident mental health diagnoses (Baglioni et al., 2011; Breslau, Roth, Rosenthal, & Andreski, 1996; D. Ford & Kamerow, 1989; Perlis et al., 2006) and suicidal ideation (Pigeon, Britton, Ilgen, Chapman, & Conner, 2013; Pigeon, Pinquart, & Connor, 2012) as well as persistence of existing mental health problems, including depression (Pigeon, Unutzer, & Perlis, 2008), and increased risk for readmission to a partial hospitalization psychiatry program (Koffel, Thuras, Chakravorty, Germain, & Khawkaja, 2015). In a large study of OEF/OIF service members, researchers found that military personnel with predeployment insomnia symptoms had greater odds of developing depression, anxiety, and PTSD at follow-up (Gehrman et al., 2013). Another longitudinal study found that insomnia measured at four months post-deployment was a significant predictor of depression and PTSD at 12-months post-deployment (Wright et al., 2011).
While it is too early to examine the long-term effects of military service on OEF/OIF service members’ health, a great deal can be learned from studying the aging trajectories of veterans from earlier conflicts, including the Vietnam War. By better understanding how early or mid-life military service contributed to long-term outcomes in these cohorts, researchers and clinicians can develop new practices that can be translated into more effective and preventive-oriented care for veterans of more recent conflicts (Marmar, 2009). For example, nearly 40 years after the conclusion of the Vietnam War, Marmar and colleagues (2015) noted that lifetime and current diagnoses of PTSD and major depression were prevalent among veterans.
PTSD has been linked to increased healthcare utilization and costs in veterans of recent and earlier war conflicts (E. Hoge, Austin, & Pollack, 2007; Schnurr, Spiro IIII, & Paris, 2000). A growing line of research suggests that some veterans involved in earlier war conflicts experience premature functional decline and accelerated aging (Lohr et al., 2015; Wolf et al., 2016) as a result of service-related experiences and injuries, including PTSD. Much of this research points to the detrimental effects of PTSD, yet little research has isolated mechanisms that link early or mid-life military experiences to PTSD and subsequent decline. While sleep problems were not measured directly in the aforementioned studies, sleep problems are a core component of PTSD diagnostic criteria (American Psychiatric Association, 2013). Given this common symptom pattern, it is possible that untreated sleep problems of Vietnam Era veterans partially contributed to mid- or late-life PTSD. However, the lack of longitudinal data and absence of sleep questionnaires in this data prevent this hypothesis from being confirmed. The model presented here illustrates one potential pathway through which early life trauma and insomnia problems may impact mid- or late-life physical and mental health.
Insomnia and Resilience as Missing Links between Military Service and Poor Outcomes
Insomnia problems contribute to negative health outcomes and can become chronic, surfacing repeatedly over one’s life course. However, mechanisms contributing to this chronicity have not been identified. The mechanisms linking sleep problems, including insomnia, to new mental health diagnoses remain unclear. However, one hypothesized explanation is that chronic poor sleep reduces one’s coping abilities. As a result, when subsequent stressors do arise, individuals with sleep problems respond with reduced coping abilities (Gehrman et al., 2013). A reduced capacity to positively cope with stress may lead to a more negative stress outcome, such as PTSD (Benight & Bandura, 2004).
Researchers studying active duty military and veteran populations have a growing interest in resilience and its role in everything from operational readiness during deployment period to mental health and readjustment in the post-deployment period (Seelig et al., 2016; Stanley, Schaldach, Kiyonga, & Jha, 2011; Troxel et al., 2015; Young-McCaughan, Peterson, & Bingham, 2011). A recent RAND report suggested that healthy sleep is critical to resilience, operationalized as service members’ performance and operational readiness, during deployment (Troxel et al., 2015). Despite this growing interest, no consensus definition of resilience has been established nor have any theories describing the relationship between sleep, resilience, and health outcomes been proposed or tested. Further, most research has focused on active duty service members with a paucity of research on the role resilience, particularly when defined as a psychological construct rather than mere outcome, might play in sleep problems among veterans.
Much of the early resilience research was rooted in developmental psychology where researchers largely focused on resilience as a positive outcome in children who had experienced early-life stress or adversity (Garmezy, 1971; Werner, 1995). However, much of this early research only examined major life events or stressors and failed to recognize how daily stressors or hassles, such as strains related to social, occupational, or financial hardships, impact resilience. Much of the stress and coping literature suggests that the cumulative impact of daily hassles is more stressful and more detrimental to an individual’s overall psychological and physical health (Charles, Piazza, Mogle, Sliwinski, & Almeida, 2013; DeLongis, Coyne, Dakof, Folkman, & Lazarus, 1982) compared to major life events. Additionally, early resilience research ignored the concept of stress proliferation, or the idea that “stress begets stress,” meaning that individuals who experience major life stressors are more susceptible to experiencing the effects of subsequent stressors (Pearlin, Schieman, Fazio, & Meersman, 2005; Pearlin & Skaff, 1996). As suggested earlier, veterans may face a series of stressors during the re-integration period. While not empirically tested to date, it is likely that daily hassles outnumber major life events and that many of these hassles contribute to stress-induced sleep problems, including insomnia. Furthermore, bouts of insomnia may also act as daily hassles in which the cumulative effects of these repeated bouts trigger additional stress and resulting sleep problems.
More contemporary approaches recognize resilience as a dynamic, multilevel, and multicomponent capacity for adapting to stress (Masten, 2001, 2007). This capacity draws on adaptive processes and abilities across behavioral, physiological and psychological systems. Modern conceptualizations of resilience also emphasize the role of health behaviors including sleep, diet, and physical activity as important contributors to enhancing one’s resilience (Southwick, Bonnano, Masten, Panter-Brick, & Yehuda, 2014). By focusing on health behaviors, contemporary research emphasizes the importance of going “upstream” of resilience and working to identify pertinent mechanisms, such as modifiable health behaviors, that can enhance or degrade resilience.
Integrated Theoretical Model
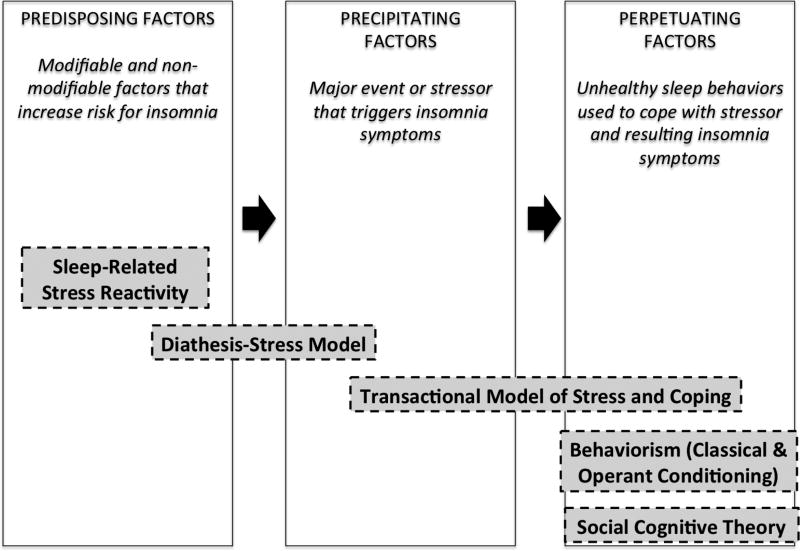
The discussions above suggest that the causes and consequences of insomnia in U.S. military veterans are complex and that sleep may play an important role in longterm mental and physical health. Below, we present an innovative integrated theoretical model that could be used to better understand the growing problem of insomnia among military veterans. This model builds on the 3P Model of Insomnia (Spielman & Glovinsky, 1991). Widely used in clinical assessment and interventions, the 3P Model provides a framework for understanding insomnia through three interrelated, sequential factors – predisposing, precipitating, and perpetuating (see Figure 1). These factors encompass genetic, constitutional, environmental, experiential, and behavioral contributors to sleep problems, respectively. The interaction between and progression across the three factors (“3Ps”) transform acute insomnia symptoms into a chronic insomnia disorder.
Figure 1. 3P Model of Insomnia: Original Framework and Integrated Theories.
Description: This model displays the three factors of the 3P Model of Insomnia – predisposing, precipitating, and perpetuating – as well as the series of behavioral health theories that are used to further describe these three factors.
Footnote: *NOTE: Original factors of 3P model enclosed in boxes outlined in solid lines. Authors’ original integration are indicated by dashed lines. The additions to this model are meant to highlight mechanisms responsible for each of the three factors and to demonstrate the overlap between and transition from one factor to the next.
Although widely regarded as the leading explanatory model of insomnia, the 3P Model could benefit from several additions which are addressed in the remainder of the paper. Our integrated model offers a more thorough understanding of insomnia by exploring the following additions. First, the model provides greater clarification of the mechanisms operating within each of the three factors. Second, unlike the 3P Model that conceptualizes insomnia and sleep problems as a consequence of a stressful event, this model recognizes sleep problems as both a stress response (consequence) and an independent stressor (predictor) that may trigger additional, negative reactions. Third, this model explores both short- and long-term consequences of insomnia, acknowledging its potential effects of insomnia on physiological, psychosocial, and cognitive domains. Finally, this model includes a dimension of time which may encourage additional studying of long-term consequences of sleep, including consideration of stress proliferation and cyclical patterns of increased stress, poor sleep, and negative outcomes that some veterans experience, including those of earlier wars.
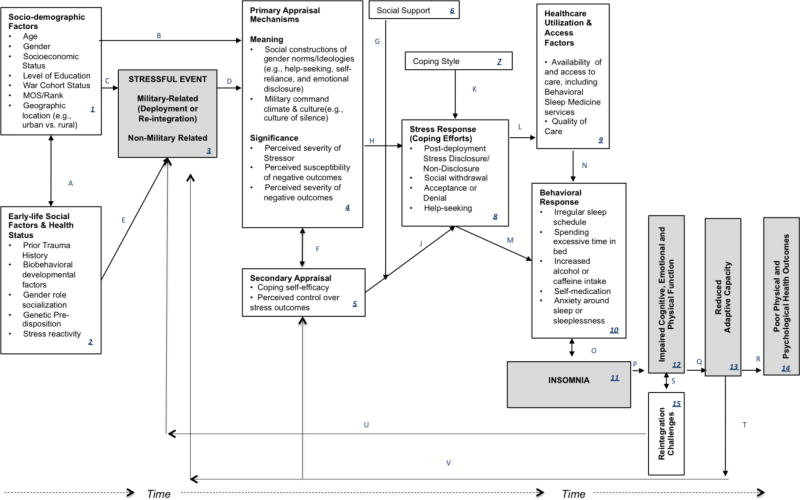
The primary aim of the integrated theoretical model presented here (Figure 2) is to encourage a broader conceptualization of insomnia problems in U.S. military veterans. The proposed model integrates and expands upon the three major components of the 3P Model: predisposing (Boxes 1 and 2), precipitating (Box 3), and perpetuating (Box 10) factors. Drawing on constructs from several key behavioral medicine theories (see Figure 1), the model depicts potential mechanisms by which a stressful event (Box 3) contributes to insomnia problems (Box 11), impaired function (Box 12), reduced resilience (Box 13), and poor health outcomes (Box 14). Unlike existing theories that assume only a unidirectional relationship between stressful events and insomnia, our model proposes that insomnia is cyclical in nature. Here, insomnia is a consequence of stress and a predictor of additional stress. Insomnia impairs function, which reduces adaptive capacity, thereby increasing one’s risk for subsequent stressful events. Thus, the cycle begins anew, potentially triggering what will become a chronic problem (Pathways U and V). As shown, this model places a particular emphasis on the consequences of chronic, untreated insomnia.
Figure 2. Integrated Theoretical Model of Insomnia Problems in US Military Veterans.
Description: This figure displays an integrated conceptual model of insomnia. This model utilizes constructs from various behavioral health theories to illustrate the cyclical nature of insomnia in United States military Veterans.
Predisposing factors
Predisposing factors of insomnia refer to modifiable and non-modifiable factors such as a genetic, biological, or psychological vulnerability to stress and/or chronic health problems. The diathesis-stress model suggests individuals possess a diathesis, or predisposing characteristic(s), that increase vulnerability to a negative stress response or outcome (Monroe & Simons, 1991). Such characteristics include genetic risk factors, sociodemographic factors, early trauma, personality traits, and biobehavioral developmental factors including neurological and cognitive functioning. Of note, adverse childhood experiences, including exposure to domestic violence, parental separation or divorce, and emotional or physical abuse, are more common among military servicemembers compared to non-servicemembers (Blosnich, Dichter, Cerulli, Batten, & Bossarte, 2014). Not only are early life events associated with poor physical and mental health outcomes in adulthood (Cabrera, Hoge, Bliese, Castro, & Messer, 2007), they may increase susceptibility to additional stressors, as described in above explanations of stress proliferation. When confronted with subsequent military or non-military stressors (Box 3), both early life events and personal characteristics may increase an individual’s risk for negative outcomes.
In addition, the theory of sleep-related stress reactivity posits that individuals with high levels of baseline stress reactivity (i.e., higher basal cortisol levels and more negative/anxious psychological dispositions) have greater susceptibility to developing insomnia (Box 2) (Drake, Pillai, & Roth, 2014). High sleep-related stress reactivity is positively associated with stress susceptibility and heightened responses across physiological and psychological domains. Stress reactivity is marked by a hyperactive adrenal system (i.e., elevated levels of stress and adrenal hormones) and poor emotional and cognitive regulation, which are manifested in an inability to sleep in a high stress situation (Drake et al., 2004; Harvey, Tang, & Browning, 2005; Perlis, Giles, Mendelson, Bootzin, & Wyatt, 1997). This diathesis, or predisposition to a negative outcome (Box 2), then interacts with a personal or environmental stressor such as military deployment, retirement, or reintegration-related challenges (Box 3) to trigger a stress response, as suggested by the Diathesis-Stress Model (Monroe & Simons, 1991).
Precipitating factors
Precipitating factors represent major life or environmental stressors that trigger insomnia-like sleep problems. As addressed above, it is the interaction between predisposing factors, or diathesis, and an environmental stressor or event (precipitating factor) that triggers a stress response (Monroe & Simons, 1991). Multiple predisposing and precipitating factors can occur sequentially or simultaneously. For some veterans, deployment-related stressors (i.e. combat exposure, service-related injury) may trigger insomnia symptoms, whereas for others, stressors related to military retirement and civilian reintegration (i.e. family obligations, occupational or financial stress, injury and/or rehabilitation challenges) may initiate these symptoms. Additionally, some veterans may experience one major stressor, or precipitating factor, while others may experience a series, of smaller, daily stressors. It is this accumulation of stressors that serves as the precipitating event for insomnia.
In addition to the interaction noted above, Lazarus and Folkman’s Transactional Model of Stress and Coping (Glanz & Schwartz, 2008) builds on the diathesis-stress model to suggest that a stress response depends on a “transaction,” or interaction, between the individual and environment. This model emphasizes that an individual’s appraisal of a stressor (i.e., precipitating event) vis-à-vis susceptibility and severity (primary appraisal) (Box 4), and perceived ability to cope with a stressor (self-efficacy) (secondary appraisal) (Box 5), directly influence the coping efforts and behaviors he or she chooses to enact (Box 8). These processes are moderated by dispositional coping style (Box 7) and degree of social support (Box 6) and mediated by coping efforts, including the use of problem- or emotion-focused strategies (Box 7). For example, some veterans who perceive military culture as discouraging stress disclosure and/or that military status artificially protects against negative outcomes (Box 4) may be less likely to disclose having experienced a stressful event and therefore less likely to seek help (Box 8). Other veterans may perceive re-integration to be stressful and a trigger for other negative outcomes (i.e. additional family or occupational stress). However, if these individuals do not have strong self-efficacy, social support or coping skills, they may be less likely to seek help for stress-induced insomnia problems (Boxes 8 and 9), and, as a result, experience significant insomnia problems and related consequences. Additional factors may also impact an individual’s decision to seek care, including the availability of and access to trained sleep specialists, prior experiences with sleep or other behavioral treatments, and personal treatment preferences.
Perpetuating factors
Acute insomnia problems become chronic through a combination of the perpetuation of unhealthy sleep behaviors and the conditioned arousal resulting from an inability to achieve and/or maintain sleep and the consequential shift in sleep patterns (Pathway O). Perpetuating factors represent unhealthy sleep behaviors used to cope with poor sleep, including following an irregular sleep schedule, spending excessive time in bed even when not sleeping, or increasing alcohol or caffeine intake to either induce sleep or wakefulness, respectively (Box 10) (Morin, 1993; Morin et al., 2006). In line with the constructs of the Transactional Model of Stress and Coping (Glanz & Schwartz, 2008), positive coping efforts reduce insomnia symptoms while negative coping efforts, including those listed above, exacerbate symptoms of poor sleep. Many of these behaviors, including spending time in bed while not sleeping or attaching negative cognitions to an inability to sleep, generate feelings of frustration, fatigue, and anxiety, each of which becomes paired, or conditioned, with the bed and bedroom. Over time, these negative thoughts and behaviors reinforce an inability to initiate and maintain quality, uninterrupted sleep. Such negative associations and reinforcement demonstrate core characteristics of classical and operant conditioning, respectively (Perlis et al., 1997).
Bandura’s Social Cognitive Theory (McAlister, Perry, & Parcel, 2008) highlights several constructs central to health behavior and health promotion. When applied to sleep, these constructs aid in further explaining the mechanisms of Spielman’s perpetuating factors (Spielman & Glovinsky, 1991), particularly how cognitions co-occurring with unhealthy sleep behaviors become associated with sleep. First, reciprocal determinism suggests that unhealthy sleep behaviors and a poor sleep environment are bidirectional, constantly influencing and reinforcing one another. Second, prolonged unhealthy behaviors diminish an individual’s capacity for self-regulation and self-efficacy for maintaining healthy, restorative sleep behaviors. Finally, chronic problems and frustration associated with not being able to sleep condition an individual’s sleep-related outcome expectations to be negative rather than positive. Negative expectations can discourage an individual from reducing unhealthy, maladaptive behaviors in favor of healthier coping strategies.
Proliferation of Sleep Problems
While the 3P Model of Insomnia provides a larger framework for understanding risk, development, and continuation of insomnia, it was not originally designed to address consequences of unresolved or residual sleep problems. The 3P Model suggests insomnia is experienced in a unidirectional, linear fashion and assumes that insomnia is resolved by treating perpetuating factors. Future studies of insomnia, including new iterations of the 3P model, could benefit from a more longitudinal approach. Such an approach should be applied to both epidemiological studies examining trajectories of insomnia and to treatment studies.
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the recommended first-line treatment for insomnia (National Institutes of Health, 2005; Qaseem et al., 2016). CBT-I targets perpetuating factors of insomnia (as shown in Box 10), including unhealthy behaviors and cognitions, and is effective in the short term (12–18 months) (Morin et al., 2006). CBTI-I and other behavioral treatments have been shown to effectively reduce insomnia symptoms and severity in veterans (Germain, Shear, Hall, & Buysse, 2007; Karlin, Trockel, Spira, Taylor, & Manber, 2015; Trockel, Karlin, Taylor, & Manber, 2014). However, some veterans continue to have either subthreshold or clinically significant symptoms following treatment (Trockel et al., 2014). The lack of long-term follow-up (i.e. beyond 6 or 12 months after treatment completion) makes it difficult to gauge the longterm trajectories of these individuals and the number who experience future bouts of insomnia. It is unclear whether these residual problems resulted from lack of sufficient follow-up (i.e. participants need additional time to adjust to a new sleep schedule and experience full treatment effects) or whether existing interventions could benefit from one or more revisions (i.e. booster sessions, general coping strategies, or tips for managing high stress reactivity). Additionally, veterans may experience an additional stressor that triggers insomnia after completing a course of CBT-I treatment. Additional research is needed to examine the extent to which prior CBT-I treatment remains effective after experiencing subsequent stressors.
One possible explanation for the chronicity of sleep problems is impaired and/or reduced coping capacity. As addressed in the first portion of this paper, poor sleep contributes to impaired cognitive and functional performance (Box 12). In line with these findings and laboratory studies demonstrating impaired performance following sleep deprivation, it is hypothesized that reduced function resulting from chronic sleep problems also negatively impact an individual’s reserve or adaptive capacity to respond to subsequent stressors (Box 12). This prediction is in line with health-related definitions of resilience, defined as a dynamic process of physiological and psychological adaptation to acute and chronic stress (Irwin, 2014; Lavretsky, 2014). Over time, chronic sleep problems, particularly sleep deprivation, lead to an ever-increasing allostatic load on physiological and psychological systems (McEwen, 2006; McEwen & Karatsoreso, 2015), thus contributing to excessive “wear and tear” on the body (Seeman, Singer, Rowe, Horwitz, & McEwen, 1997). Increasing allostatic load reduces the likelihood that an individual is able to successfully respond to or cope with subsequent stressors (Juster, McEwen, & Lupien, 2010; McEwen & Karatsoreso, 2015). This reduced stress capacity then contributes to poor physical and psychological health outcomes (Box 14).
There may be benefits to future research examining how impaired coping capacity may interact with high levels of stress reactivity, and what impact this combination of factors may have on future bouts, or relapses, of insomnia. If such an interaction is present, it may be that innovative hybrid interventions, such as those informed by principles of CBT-I and Mindfulness Based Stress Reduction (MBSR) may be effective in targeting both unhealthy sleep behaviors and underlying stress reactivity. MBSR has been shown to reduce physiological and psychological stress reactivity (Sharma & Rush, 2014) and an initial test of one such hybrid program, Mindfulness Based Therapy for Insomnia, which combines principles of CBT-I and MBSR, demonstrated promising results in reducing severity of insomnia symptoms (Ong et al., 2014). Although CBT-I curriculum teaches sleep-related coping strategies, it does not include more general stress and coping strategies. Integrating some of these strategies into behavioral sleep treatments may improve long-term coping and help reduce the likelihood of chronic insomnia.
Future directions
The proposed theoretical model highlights the etiological and clinical complexity of insomnia in U.S. military veterans, placing a particular emphasis on untreated insomnia problems. Severe sleep problems, such as insomnia, might occur at one point in time, typically triggered by a major life or environmental stressor, but their antecedents are found early in life and their consequences can extend for years or decades beyond the triggering stressful event(s). The model presented herein is meant to encourage researchers and clinicians to apply lifespan models to the problems of stress, insomnia, and health outcomes in veterans. While longitudinal data collection is time and resource intensive, such information would allow researchers to better understand the temporal nature and interrelationships between stressful events, sleep problems, and negative physical and psychological outcomes. Although not shown in this model, insomnia may co-occur with other sleep disorders, including sleep disordered breathing, restless leg syndrome, and chronic nightmares. Future iterations of the model should take a holistic approach to sleep and acknowledge these other common sleep disorders.
Sleep problems, particularly insomnia, are often assumed to be an acute consequence of deployment or reintegration. However, this model highlights the potential cyclical nature of insomnia, noting that chronic problems can deleteriously impact veterans’ long-term health and function. This model also highlights the importance of studying major life events and daily stressors as both predictors and consequences of insomnia problems. Finally, as alluded to above, sleep and resilience are likely important yet under-studied mechanisms in veterans’ long-term health. Additional research focusing on the multidimensional nature of resilience, including how physiological and psychological adaptive capacities contribute to an individual’s stress response, is warranted. Future research examining these relationships and mechanisms could prove fruitful in both clinical and research settings, particularly as an increasing number of OEF/OIF veterans retire from military service and begin to utilize both VA and community healthcare services. As our theoretical model suggests, addressing sleep problems early could potentially enhance a veteran’s adaptive capacity, thereby reducing the risk for negative physical and psychological outcomes across the lifespan. Finally, the constructs and mechanism outlined in this particular model may have application to non-veterans, including individuals who have experienced a significant life stressor or traumatic event. Future iterations of the model should highlight the mechanisms of insomnia and comorbid mental and physical health conditions.
Highlights.
Chronic insomnia problems are highly prevalent among US military Veterans
Existing theoretical models view insomnia as a unidirectional phenomenon
An integrated model is proposed that explains insomnia as a chronic, cyclical problem
Insomnia should be viewed as a both a consequence and predictor of stress
Acknowledgments
The authors wish to think Wizdom Powell, PhD, MPH who provided comments on an initial version of the conceptual model and manuscript.
Role of Funding Sources
This work was supported by facilities and resources at the Center of Innovation for Health Services Research in Primary Care at the Durham VAMC (CIN 13-410); Office of Academic Affiliations, VA Health Services Research & Development (TPH 21-000), and University of North Carolina Program on Integrative Medicine (Hughes: NIH/NCCIH T32AT003378). None of the funding sources had a role in developing this material, writing the manuscript, or the decision to submit the paper for publication.
Abbreviations
- VHA
Veterans Health Administration
- OEF
Operation Enduring Freedom
- OIF
Operation Iraqi Freedom
- PTSD
Post-traumatic Stress Disorder
- CBT-I
Cognitive Behavioral Therapy for Insomnia
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Disclosure Information
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Contributors
Dr. Hughes developed the first draft of the conceptual model and wrote the first draft of the manuscript. Drs. Ulmer, Gierisch, Hastings, and Howard served as theoretical consultants during the development of the conceptual model and assisted with review and editing of the final manuscript. All authors have contributed to and have approved the final manuscript.
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- Ahn S, Jiang L, Smith ML, Ory MG. Improvement in sleep problems among the chronic disease self-management program participants. Family & Community Health. 2014;27(4):327–355. doi: 10.1097/FCH.0000000000000045. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Desk Reference to the Diagnostic Criteria from DSM-5. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- Amin M, Parisi JA, Gold MS, Gold AR. War-related illness symptoms among Operation Iraqi Freedom/Operation Enduring Freedom returness. Military medicine. 2010;175(3):155–157. doi: 10.7205/milmed-d-90-00153. [DOI] [PubMed] [Google Scholar]
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholdzer U, Riemann D. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Benight CC, Bandura A. Social cognitive theory of posttraumatic recovery: the role of perceived self-efficacy. Behaviour research and therapy. 2004;42:1129–1148. doi: 10.1016/j.brat.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Blosnich JR, Dichter ME, Cerulli C, Batten SV, Bossarte RM. Disparities in Adverse Childhood Experiences Among Individuals with a History of Military Service. JAMA Psychiatry. 2014;71(9):1041–1048. doi: 10.1001/jamapsychiatry.2014.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramoweth AD, Germain AA. Deployment-related insomnia in military personnel and Veterans. Current Psychiatry Reports. 2013;15:401–409. doi: 10.1007/s11920-013-0401-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Roth T, Rosenthal L, Andreski PM. Sleep disturbance and psychiatric disorders: A longitudinal study of young adults. Biological Psychiatry. 1996;39(6):411–418. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;23:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Cabrera OA, Hoge CW, Bliese PD, Castro CA, Messer SC. Childhood adversity and combat as predictors of depression and post-traumatic stress in deployed troops. American Journal of Preventive Medicine. 2007;33(2):77–82. doi: 10.1016/j.amepre.2007.03.019. [DOI] [PubMed] [Google Scholar]
- Campbell J, Shattuck N, Germain A, Mysliwiec V. Introduction; Paper presented at the 29th Annual Meeting of the Association of Professional Sleep Societies; Seattle, WA. 2015. [Google Scholar]
- Castro CA, Kintzle S, Hassan AM. The combat veteran paradox: Paradoxes and dilemmas with reintegrating combat veterans and the agencies that support them. Traumatology. 2015;221(4):299–310. [Google Scholar]
- Charles ST, Piazza JR, Mogle J, Sliwinski MJ, Almeida DM. The wear and tear of daily stressors on mental health. Psychological Science. 2013;34(4):733–741. doi: 10.1177/0956797612462222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLongis A, Coyne JC, Dakof G, Folkman S, Lazarus RS. Relationship of daily hassles, uplifts, and major life events to health status. Health Psychology. 1982;1(2):119–136. [Google Scholar]
- Dement WC, Vaughan C. The promise of sleep: A pioneer in sleep medicine explores the vital connection between health, happiness, and a good night’s sleep. New York, NY: Dell Publishing Co; 1999. [Google Scholar]
- Dew MA, Hoch CC, Buysse DJ, Monk TH, Begley A, Houck PR, Reynolds CF. Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosomatic medicine. 2003;65:63–73. doi: 10.1097/01.psy.0000039756.23250.7c. [DOI] [PubMed] [Google Scholar]
- Drake CL, Friedman NP, Wright KP, Roth T. Sleep reactivity and inosmnia: Genetic and environmental influences. Sleep. 2011;34(9):1179–1188. doi: 10.5665/SLEEP.1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake CL, Pillai V, Roth T. Stress and sleep reactivity: A prospective investigation of the stress-diathesis model of insomnia. Sleep. 2014;37(8):1295–1304. doi: 10.5665/sleep.3916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake CL, Richardson G, Roerhs T, Scofield N, Roth T. Vulnerability to stress-related sleep disturbance and hyperarsoual. Sleep. 2004;27(2):285–291. doi: 10.1093/sleep/27.2.285. [DOI] [PubMed] [Google Scholar]
- Fernandez-Mendoza J, Vgontzas AN. Insomnia and its impact on physical and mental health. Current Psychiatry Reports. 2013;15:418–426. doi: 10.1007/s11920-013-0418-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford D, Kamerow D. Epidemiologic study of sleep disturbances and psychiatric disorders: An opportunity for prevention? Journal of the American Medical Association. 1989;262(11):1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- Ford E, Cunningham T, Giles W, Croft J. Trends in insomnia and excessive daytime sleepiness among US adults from 2002 to 2012. Sleep Medicine. 2015;16(3):372–378. doi: 10.1016/j.sleep.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garmezy M. Vulnerability research and the issue of primary prevention. American Journal of Orthopsychiatry. 1971;41(1):101–116. doi: 10.1111/j.1939-0025.1971.tb01111.x. [DOI] [PubMed] [Google Scholar]
- Gehrman P, Seelig AD, Jacobson IG, Boyko EJ, Hooper TI, Gackstetter GD Millennium Cohort Study Team. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep. 2013;36(7):1009–1018. doi: 10.5665/sleep.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germain A, Shear MK, Hall M, Buysse DJ. Effects of a brief behavioral treatment for PTSD-related sleep disturbances: a pilot study. Behaviour research and therapy. 2007;45:627–632. doi: 10.1016/j.brat.2006.04.009. [DOI] [PubMed] [Google Scholar]
- Glanz K, Schwartz MD. Stress, coping, and health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education. San Francisco, CA: Jossey-Bass; 2008. pp. 211–236. [Google Scholar]
- Hamilton NA, Delwyn C, Karlson C. Sleep and the affective response to stress and pain. Health Psychology. 2007;26(3):288–295. doi: 10.1037/0278-6133.26.3.288. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Tang NKY, Browning L. Cognitive approaches to insomnia. Clinical Psychology Review. 2005;25:593–611. doi: 10.1016/j.cpr.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Haynes PL, Parthasarathy S, Bootzin RR, Krakow B. Motivational enhancement therapy for insomnia in OEF/OIF Veterans: A treatment development study. Sleep. 2013;36(Supplement):A232. [Google Scholar]
- Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in US soldiers returning from Iraq. New England Journal of Medicine. 2008;358:453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- Hoge E, Austin E, Pollack M. Resilience: Research evidence and conceptual considerations for Posttraumtic Stress Disorder. Depression and Anxiety. 2007;24:139–152. doi: 10.1002/da.20175. [DOI] [PubMed] [Google Scholar]
- Hughes J, Martin JL. Sleep characteristics in Veterans Affairs Adult Day Health Care participants. Behavioral Sleep Medicine. 2015;13(3):197–207. doi: 10.1080/15402002.2013.855212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Returning home from Iraq and Afghanistan: Assessment of readjustment needs of Veterans, service members, and families. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- Irwin MR. Sleep and inflammation in resilient aging. Interface Focus. 2014;4 doi: 10.1098/rsfs.2014.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster R, McEwen BS, Lupien SJ. Allostatic load biomarkerts of chronic stress and impact on health and cognition. Neuroscience and Biobehavioral Reviews. 2010;35:2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Karlin BE, Trockel M, Spira AP, Taylor CB, Manber R. National evaluation of the effectiveness of cognitive behavioral therapy for insomnia among older versus younger veterans. International Journal of Geriatric Psychiatrty. 2015;30:308–315. doi: 10.1002/gps.4143. [DOI] [PubMed] [Google Scholar]
- Katz DA, McHorney CA. The relationship between insomnia and health-related quality of life in patients with chronic illness. Journal of Family Practice. 2002;51(3):229–235. [PubMed] [Google Scholar]
- Killgore WDS, Balkin TJ, Westensten NJ. Impaired decision making following 49 hours of sleep deprivation. Journal of Sleep Research. 2006;15(1):7–13. doi: 10.1111/j.1365-2869.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- Killgore WDS, Kahn-Greene, Lipizzi EL, Newman RA, Kamimori GH, Balkin TJ. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep medicine. 2008;9(5):517–526. doi: 10.1016/j.sleep.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Koffel E, Thuras P, Chakravorty S, Germain A, Khawkaja I. Poor sleep quality as a predictor of readmission to a psychiatry partial hospitalization program. Sleep. 2015;38(Supplement):A326. doi: 10.4088/PCC.15l01826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality Associated With Sleep Duration and Insomnia. Archives of General Psychiatry. 2002;59:131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- Lavretsky H. Resilience and Aging: Research and Practice. Baltimore, MD: Johns Hopkins University Press; 2014. [Google Scholar]
- Lohr JB, Palmer BW, Eidt CA, Aaliaboyina S, Mausbach BT, Wolkowitz OM, Jeste DV. Is Post-Traumatic Stress Disorder associated with premature senescence? A review of the literature. American Journal of Geriatric Psychiatry. 2015;23(7):709–725. doi: 10.1016/j.jagp.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macera CA, Aralis HJ, Rauch MJ, MacGregor AJ. Do sleep problems mediate the relationship between traumatic brain injury and development of mental health symptoms after deployment? Sleep. 2013;36:83–90. doi: 10.5665/sleep.2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmar CR. Mental health impact of Afghanistan and Iraq deployment: Meeting the challenge of a new generation of Veterans. Depression and Anxiety. 2009;26(6):493–497. doi: 10.1002/da.20581. [DOI] [PubMed] [Google Scholar]
- Marmar CR, Schlenger WE, Henn-Haase C, Qian M, Purchia E, Li M, Kulka RA. Course of posttraumatic stress disorder 40 years after the Vietnam war: Findings from the National Vietnam Veterans Longitudinal Study. JAMA Psychiatry. 2015;72(9):875–881. doi: 10.1001/jamapsychiatry.2015.0803. [DOI] [PubMed] [Google Scholar]
- Masten AS. Ordinary magic: Resilience processes in development. American Psychologist. 2001;56(3):227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- Masten AS. Resilience in development systems: Progress and promise as the fourth wave rises. Development and Psychopathology. 2007;19:921–930. doi: 10.1017/S0954579407000442. [DOI] [PubMed] [Google Scholar]
- McAlister AL, Perry CL, Parcel GS. How individuals, environments, and health behaviors interact: Social cognitive theory. In: Glanz K, B Rimer K, Viswanath K, editors. Health Behavior and Health Education. San Francisco, CA: Jossey-Bass; 2008. pp. 167–188. [Google Scholar]
- McEwen BS. Sleep deprivation as a neurobiologic and physiologic stressor: Allostasis and allostatic load. Metabolism Clinical and Experimental. 2006;55(Suppl 2) doi: 10.1016/j.metabol.2006.07.008. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Karatsoreso IN. Sleep deprivation and circadian disruption: Stress, allostasis, and allostatic load. Sleep Medicine Clinics. 2015;10:1–10. doi: 10.1016/j.jsmc.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, Simons AD. Diathesis-stress theories in the context of life research: Implications for the depressive disorders. Psychological bulletin. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Morin C. Insomnia: Pyschological Assessment and Management. New York: The Guilford Press; 1993. [Google Scholar]
- Morin C, Bootzin R, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia: Update of the recent evidence. Sleep. 2006;29(11):1398–1414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- Morin C, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosomatic medicine. 2003;65(259–267) doi: 10.1097/01.psy.0000030391.09558.a3. [DOI] [PubMed] [Google Scholar]
- Mysliwiec V, McGraw PR, Smith P, Trapp B, Roth BJ. Sleep disorders and associated medical comorbidities in active duty military personnel. Sleep. 2013;36(2):167–174. doi: 10.5665/sleep.2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. NIH State-of-the-Science Conference Statement on the Manifestations and Management of Chronic Insomnia in Adults. 2005 Retrieved from Bethesda, MD: [Google Scholar]
- Ong JC, Manber R, Segal Z, Zia Y, Shapiro S, Wyatt JK. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. 2014;37(9):1153–1563. doi: 10.5665/sleep.4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, Health, and the Life Course: Some Conceptual Perspectives. Journal of health and social behavior. 2005;46:205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Skaff MM. Stress and the Life Course: A Paradigmatic Alliance. The Gerontologist. 1996;36(2):239–247. doi: 10.1093/geront/36.2.239. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Giles DE, Mendelson WB, Bootzin RR, Wyatt JK. Psychophysiological insomnia: The behavioural model and a neurocognitive perspective. Journal of Sleep Research. 1997;6:179–188. doi: 10.1046/j.1365-2869.1997.00045.x. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Smith LJ, Lyness JM, Matteson SR, Pigeon WR, Jungquist C. Insomnia as a risk factor for onset of depression in the elderly. Behavioral Sleep Medicine. 2006;4:104–113. doi: 10.1207/s15402010bsm0402_3. [DOI] [PubMed] [Google Scholar]
- Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Military medicine. 2008;173(230):235. doi: 10.7205/milmed.173.3.230. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Britton P, Ilgen MA, Chapman B, Conner KR. Sleep disturbance preceding suicide among Veterans. In: Bossarte RM, editor. Veteran suicide: A public health imperative. Washington, D.C: American Public Health Association; 2013. pp. 278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pigeon WR, Pinquart M, Connor K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. Journal of Clinical Psychiatry. 2012;73(9):e1160–e1167. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Unutzer J, Perlis ML. Is insomnia a perpetuating factor for late-life depression in the IMPACT cohort? Sleep. 2008;31(4):481–488. doi: 10.1093/sleep/31.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilcher JJ, Huffcutt AJ. Effects of sleep deprivation on performance: A meta-analysis. Journal of Sleep Research & Sleep Medicine. 1996;19(4):318–326. doi: 10.1093/sleep/19.4.318. [DOI] [PubMed] [Google Scholar]
- Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD Clinical Guidelines Committee of the American College of Physicians. Management of chronic insomnia disorder in adults: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine. 2016;165:125–133. doi: 10.7326/M15-2175. [DOI] [PubMed] [Google Scholar]
- Roth T. Insomnia: Definition, prevalence, etiology, and consequences. Journal of Clinical Sleep medicine. 2007;3(5):S7–S10. [PMC free article] [PubMed] [Google Scholar]
- Ryden AM, Matsuwaka S, Mitchell MN, Fung CH, Dzierzewski JM, Song Y, Alessi CA. Prevalence of insomnia disorder decreases with age among older Veterans. Sleep. 2015;38(Supplement):A396. [Google Scholar]
- Schnurr PP, Spiro A, IIII, Paris AH. Physician-Diagnosed Medical Disorders in Relation to PTSD Symptoms in Older Male Military Veterans. Health Psychology. 2000;10(1):91–97. doi: 10.1037//0278-6133.19.1.91. [DOI] [PubMed] [Google Scholar]
- Seelig AD, Jacobson IG, Donoho CJ, Trone DW, Crum-Cianflone NF, Balkin TJ. Sleep and health resilience metrics in a large military cohort. Sleep. 2016;39(5):1111–1120. doi: 10.5665/sleep.5766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seelig AD, Jacobson IG, Smith B, Hooper TI, Boyko EJ, Gackstetter GD, Smith TC. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2011;33(12):1615–1622. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation--allostatic load and its consequences: MacArthur studies of successful aging. Archives of Internal Medicine. 1997;157:2259–2268. [PubMed] [Google Scholar]
- Sharma M, Rush SE. Mindfulness-based stress reduction as stress management intervention for healthy individuals: A systematic review. Journal of Evidence-Based Complementary & Alternative Medicine. 2014;19(4):271–286. doi: 10.1177/2156587214543143. [DOI] [PubMed] [Google Scholar]
- Shippee ND, Shah ND, May CR, Mair FS, Montori VM. Cumulative complexity: A functional, patient-centered model of patient complexity can improve research and practice. Journal of Clinical Epidemiology. 2012;65(1041–1051) doi: 10.1016/j.jclinepi.2012.05.005. [DOI] [PubMed] [Google Scholar]
- Southwick SM, Bonnano GA, Masten AS, Panter-Brick C, Yehuda R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. European Journal of Psychotraumatology. 2014;5:1–15. doi: 10.3402/ejpt.v5.25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielman A, Glovinsky PB. The varied nature of insomnia. In: Hauri PJ, editor. Case studies in insomnia. New York, NY: Plenum Press; 1991. (Reprinted from: NOT IN FILE) [Google Scholar]
- Stanley EA, Schaldach JM, Kiyonga A, Jha AP. Mindfulness-based mind fitness training: A case study of a high-stress predeployment military cohort. Cognitive and Behavioral Practice. 2011;18(566–576) [Google Scholar]
- Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of Chronic Insomnia with Medical Problems. Sleep. 2007;30(2):213–218. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- Trockel M, Karlin BE, Taylor C, Manber R. Cognitive Behavioral Therapy for Insomnia with Veterans: Evaluation of effectiveness and correlates of treatment outcomes. Behaviour research and therapy. 2014;53:41–46. doi: 10.1016/j.brat.2013.11.006. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Shih RA, Pedersen ER, Geyer L, Fisher MP, Griffin BA, Steinberg PS. Sleep in the Military: Promoting Healthy Sleep Among U.S. Servicemembers. 2015 Retrieved from Santa Monica, CA: [PMC free article] [PubMed] [Google Scholar]
- Ulmer CS, Van Voorhees E, Germain AE, Voils CI, Beckham JC VA Mid -Atlantic Mental Illness Research Education and Clinical Center Registry Workgroup. A comparison of sleep difficulties among Iraq/Afghanistan Theater Veterans with and without mental health diagnoses. Journal of Clinical Sleep medicine. 2015;11(9):995–1005. doi: 10.5664/jcsm.5012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner EE. Resilience in development. Current Directions in Psychological Science. 1995;43(3):81–85. [Google Scholar]
- Wolf EJ, Logue MW, Hayes JP, Sadeh N, Schichman SA, Stone A, Miller MW. Accelerated DNA methylation age: Associations with PTSD and neural integrity. Psychoneuroendocrinology. 2016;63:155–162. doi: 10.1016/j.psyneuen.2015.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. Journal of clinical psychology. 2011;67(12):1240–1258. doi: 10.1002/jclp.20845. [DOI] [PubMed] [Google Scholar]
- Yoon J, Schott JY, Phibbs CS, Wagner TH. Recent trends in Veterans Affairs chronic condition spending. Population Health Management. 2011;14(6):293–298. doi: 10.1089/pop.2010.0079. [DOI] [PubMed] [Google Scholar]
- Young-McCaughan S, Peterson AL, Bingham MO. The role of sleep in the health and resiliency of military personnel. 2011 Retrieved from Brussels: [Google Scholar]
- Yu W, Ravelo A, Wagner TH, Phibbs CS, Bhandari A, Chen S, Barnett PG. Prevalence and costs of chronic conditions in the VA health care system. Medical Care Research and Review. 2003;60(3 Suppl):146S–167S. doi: 10.1177/1077558703257000. [DOI] [PubMed] [Google Scholar]
- Zullig LL, Whitson HE, Hastings SN, Beadles C, Kravchenko J, Akushevich I, Maciejewski ML. A systematic review of conceptual frameworks of medical complexity and new model development. Journal of General Internal Medicine. 2016;31(3):329–337. doi: 10.1007/s11606-015-3512-2. [DOI] [PMC free article] [PubMed] [Google Scholar]