Abstract
Background
Heart failure is a major and growing medical and economic problem worldwide as 1–2% of the healthcare budget are spent for heart failure. The prevalence of heart failure has increased over the past decades and it is expected that there will be further raise due to the higher proportion of elderly in the western societies. In this context cost-of-illness studies can significantly contribute to a better understanding of the drivers and problems which lead to the increasing costs in heart failure.
The aim of this study was to perform a systematic review of published cost-of-illness studies related to heart failure to highlight the increasing cost impact of heart failure.
Methods
A systematic review was conducted from 2004 to 2016 to identify cost-of-illness studies related to heart failure, searching PubMed (Medline), Cochrane, Science Direct (Embase), Scopus and CRD York Database.
Results
Of the total of 16 studies identified, 11 studies reported prevalence-based estimates, 2 studies focused on incidence-based data and 3 articles presented both types of cost data. A large variation concerning cost components and estimates can be noted. Only three studies estimated indirect costs. Most of the included studies have shown that the costs for hospital admission are the most expensive cost element. Estimates for annual prevalence-based costs for heart failure patients range from $868 for South Korea to $25,532 for Germany. The lifetime costs for heart failure patients have been estimated to $126.819 per patient.
Conclusions
Our review highlights the considerable and growing economic burden of heart failure on the health care systems. The cost-of-illness studies included in this review show large variations in methodology used and the cost results vary consequently. High quality data from cost-of-illness studies with a robust methodology applied can inform policy makers about the major cost drivers of heart failure and can be used as the basis of further economic evaluations.
Electronic supplementary material
The online version of this article (10.1186/s12872-018-0815-3) contains supplementary material, which is available to authorized users.
Keywords: Heart failure, Cost-of-illness, Economic burden, Heart disease
Background
The burden of heart failure
Heart failure (HF) is a major and growing medical and economic problem, with high prevalence and incidence rates worldwide [1, 2]. HF is defined as a pathophysiological state in which an abnormality of cardiac function is responsible for the failure of the heart to pump blood at a rate commensurate with the requirements of the metabolizing tissues [3]. It has been estimated that 0.4–2.2% of the population in industrialized countries suffer from HF [4], with between 500,000–600,000 incident cases diagnosed each year [5]. HF affects especially the elderly, with 80% of HF-related hospitalizations and 90% of HF-related deaths occurring among patients aged 65 years or older [6]. The prevalence of HF has increased over the past decades [7]. It is expected that there will be a further rise due to a higher proportion of elderly people and better survival rates of patients with conditions such as hypertension, diabetes, etc., which trigger the development of HF [7, 8]. In addition, two thirds of the patients are readmitted to hospital within one year [9]. The mortality rate for patients with HF is high, as showed in the MAGGIC meta-analysis includes individual data on 39,372 patients with 40,2% died during a median follow-up of 2,5 years [10]. A recently published study demonstrated that the 30-day readmission rates for HF are higher than for pneumonia or acute myocardial infarction [11].
Due to the high and increasing prevalence rates, HF constitutes an enormous economic burden for the healthcare systems in industrialized countries. For example, Europa and USA spent 1–2% of their annual healthcare budget on HF [6]. The global economic burden of HF is estimated at $108 billons per annum, with $65 billons attributed to direct and $43 billons to indirect costs [12]. The US is the biggest contributor to the global HF costs and is responsible for 28.4% of total global HF spend [12]. Europa accounts for 6.83% of total global HF costs [12].
Due to the considerable cost impact of HF on healthcare systems, it is necessary to have a better understanding of the cost aspects and the specific cost drivers. In this context, Cost-of-Illness (COI) studies are an important tool to analyze the economic burden of HF and to provide information on the cost drivers to clinicians and health policy makers. On the basis of transparent and detailed cost components this is aimed at improving the planning and development of healthcare services and optimization of the allocation of healthcare expenditures and medical resources [13]. COI studies are often restricted to a certain country, deal with small patient groups or present only a part of all illness costs. Therefore, it is important to summarize the results of different COI-studies in a systematic way.
Background on cost-of-illness studies
COI studies estimate the resources consumed and lost as a result of a particular disease. Results from the COI studies can improve understanding of the economic burden that a specific disease may have on society as whole, healthcare providers, and the individual patient. COI studies can also provide a fundamental basis for further economic evaluations, such as cost-effectiveness-, cost-utility- and cost-benefit analysis [14].
Perspective
COI studies can be conducted from various perspectives. Based on the chosen perspective, the cost estimation can vary. The most popular perspectives are the societal perspective and the viewpoints of the patient, the insurance company or the healthcare providers.
Epidemiological approach
COI studies follow two different epidemiological approaches, either the prevalence- or the incidence-based approach. Prevalence-based studies measure costs, which occur with prevalent cases over a specified time period, usually 1 year [15].
The incidence-based approach focusses on lifetime costs attributed to a disease. The costs are measured from the onset of a disease [15].
Method of resource quantification
COI studies use two different methods to estimate costs. The bottom-up approach (“person-based”) assigns costs to individuals with the health condition of interest, for example by using data from real cases [15]. The top-down method (“population-based”) allocates parts of aggregated costs to specific diseases.
Objectives
The aim of this study was to perform a systematic review of recently published COI studies related to HF to highlight the increasing cost impact associated with this disease and identify the major cost drivers.
Methods
We conducted a systematic literature search for journal articles between 2004 and 2016 in the following databases: PubMed (Medline), Cochrane, Science Direct (Embase), Scopus and CRD (Centre for Reviews and Dissemination) York Database incl. National Health Service Economics Evaluation Database (NHS EED). To identify relevant COI-studies for HF, appropriate disease-related MeSH terms were used (Additional file 1). The references or citations of the retrieved articles were reviewed for additional articles (citation snowballing). The search methodology was in line with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [16] except for the use of the PICOS (population, intervention, comparators, outcomes, study design) review system.
Inclusion and exclusion criteria
Search results were transferred to EndNote, version X7, and reviewed independently by two researchers. The inclusion and exclusion criteria were adopted from the CHEC list [17] and the BMJ guidelines for authors and peer reviewers of economic submissions [18]. Although the two checklists were developed for the assessment of economic evaluations, we derived criteria that are also relevant for the evaluation of cost-of-illness studies. These criteria are listed in the appendix (Additional file 2). Furthermore they were in accordance with the check list for COI evaluation in the guide to critical evaluation of COI studies developed by Larg et al. [15].
HF can be categorized in two entities, systolic HF and diastolic HF. Systolic heart failure is defined as the entity in which the ejection fraction is reduced. In diastolic HF the ejection fraction is preserved. Owan et al. has shown that 53% of patients suffer from systolic and 47% from diastolic heart failure [19]. As our aim was to analyze all entities of HF independently of the pathophysiologic mechanism, we excluded papers dealing only with systolic/diastolic HF.
General characteristics of the studies
To provide a comprehensive understanding, the included studies were analyzed in terms of country, epidemiological approach (prevalent vs. incident), study period, perspective (societal, healthcare provider, etc.), main data sources and the identification of HF patients. When the study perspective or the epidemiological approach were not clearly specified in the studies, two investigators achieved consensus by discussion.
Standardization of costs
The reported costs in the included studies were transferred from the local currency in the year of the costs to the inflated values in local currency for the year 2016 [20]. This cost data was exchanged to US-dollars by using the gross domestic product purchasing power parity (PPP) [21]. This methodology can be used for COI studies in order to reach better comparability between the different currencies [22].
Results
The search procedure is shown in the PRISMA Flow Diagram (Fig. 1: Data acquisition flowchart). The systematic literature search identified 17,329 potential relevant articles. After removing 9166 duplicates, there were 8163 studies, which were screened by title and abstract. 8068 papers were excluded because they did not deal with COI studies of HF. Of the remaining 95 articles, another 79 studies did not fulfill the inclusion criteria shown in the Appendix. In all, 16 articles were identified in this review and analyzed by their study characteristics and cost data.
Fig. 1.
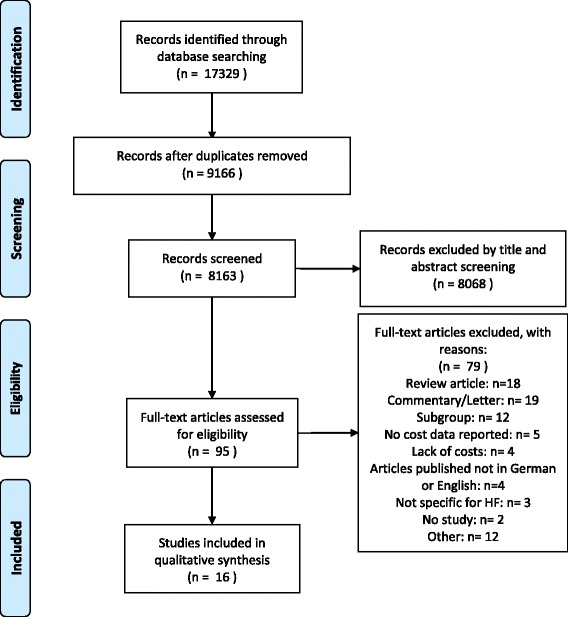
Data acquisition flowchart
Study characteristics
Study characteristics are summarized in Tables 1 and 2. Reviewed COI studies showed results for ten countries. Eight studies were conducted in Europa, and six in North America. The study population size ranged from a minimum of 115 to a maximum of 475,019. The mean age of the study population varied from 58 to 81.6 years. Three studies [23–25] reported the mean age of different subgroups (HF-group vs. no-HF control group). Eleven articles had a prevalent and two an incident epidemiological approach. Three studies provided both types of results [25–27]. Twelve studies adopted the perspective of a third-party payer and six articles were categorized as a prospective study.
Table 1.
COI-studies in HF: Summary of main study characteristics
| Reference | Country | Study size | Epidemiological approach | Method of Resource Quantification | Study period | Perspective | Study design | Mean age |
|---|---|---|---|---|---|---|---|---|
| Voigt 2014 [35] | USA | – | Prevalenta | Mixeda | 2007–2012 | Sa | R | – |
| Corrao 2014 [33] | Italy | 26,949 | Incident | Top-downa | 2011 | P | R | 79 |
| Czech 2013 [36] | Poland | – | Prevalenta | Mixeda | 2009–2011 | P | R | – |
| Delgado 2013 [37] | Spain | 374 | Prevalenta | Bottom-upa | 2010 | S | Pr | 62 |
| Dunlay 2011 [34] | USA | 1054 | Incidenta | Top-downa | 1987–2006 | Pa | R | 76,8 |
| Bogner 2010 [24] | USA | 7996 | Prevalenta | Bottom-upa | 2000–2001 | P | R | 77,8–81,4 |
| Zugck 2010 [30] | Germany | 86,493 | Prevalenta | Top-downa | 2002 | Pa | R | – |
| Neumann 2009 [29] | Germany | – | Prevalenta | Top-downa | 2000–2007 | Pa | R | – |
| Liao 2007 [23] | USA | 4860 | Prevalent | Top-down | 1992–2003 | Pa | Pr | 75,6- 78,2 |
| Liao 2006 [25] | USA | 881 | Mixed | Top-down | 1992–1998 | Pa | Pr | 77,6- 81,6 |
| Agvall 2005 [28] | Sweden | 115 | Prevalenta | Bottom-upa | 1999–2000 | Pa | R | 77 |
| Ory 2005 [26] | USA | 17,835 | Mixed | Bottom-upa | 1999–2001 | Pa | Pr | 76,4 |
| Stafylas 2016 [38] | Greece | 307 | Prevalent | Top-downa | 2009–2011 | P | Pr | 66 |
| Lee 2016 [31] | South Korea | 475,019 | Prevalent | Top-down | 2014 | P / S | R | – |
| Murphy 2016 [27] | Ireland | 1292 | Mixeda | Mixeda | 2013 | Pa | R | 74,5 |
| Ogah 2014 [32] | Nigeria | 239 | Prevalent | Mixeda | 2009–2010 | S | Pr | 58 |
anot clearly stated in the study, consensus by discussion
S – societal; P – third-party payer; R – retrospective; Pr - prospective
Table 2.
Main data sources and definition of HF in the included studies
| Study | Main data sources | Definition of HF |
|---|---|---|
| Voigt, 2014 [35] | Agency for Healthcare Research and Quality (AHRQ) National Association for Home Care & Hospice (NAHC) National Ambulatory Medical Care Survey (NAMCS) National Hospital Ambulatory Medical Care Survey (NHAMCS) Centers for Medicare & Medicaid Services (CMS) |
ICD-9 (428.x, 402.01, 402.11, 402.91, 398.91, 404.01, 404.11, 404.91, 416.9, 425.4, 518.4, 786) |
| Corrao, 2014 [33] | Italian National Health System (NHS) database from Lombardy | ICD-9 (428, 402.01, 402.11, 402.91) |
| Czech, 2013 [36] | Medical data from randomly selected outpatient units and inpatient facilities linked with patient interview data (POLKARD study) | – |
| Delgado, 2013 | Medical records from specialized cardiology clinics, questionnaires and interviews (patients and caregivers) | Symptomatic patients (NYHA II-IV) with a diagnosis of HF at least 6 months previously |
| Dunlay, 2011 [34] | Medical records and billing data from Olmsted County Healthcare Expenditure and Utilization Database (OCHEUD), a population-based database in Olmsted County, Minnesota, USA | ICD-9 (428) |
| Bogner, 2010 [24] | Administrative database of a large urban academic health care system Medicare claims database |
ICD-9 (428.0, 428.1, 428.9, 402.01, 402.11, 402.91) |
| Zugck, 2010 [30] | Database of the public health insurance, cohort selected by randomly prescribed date of birth Federal Office of Statistics, Germany |
ICD-10 (I50) |
| Neumann, 2009 [29] | Federal Office of Statistics, Germany | ICD-10 (I50) |
| Liao, 2007 [23] Liao, 2006 [25] |
Cardiovascular Health Study (prospective, community-based, observational study) Medicare linked files |
Hospitalization for HF or self-report of a physician diagnosis of HF |
| Agvall, 2005 [28] | Hospital records from two healthcare centers Swedish National Medical Agency price list |
ICD-10 (I50) |
| Ory, 2005 [26] | Longitudinal database of Prescription Solutions, a pharmacy benefit and medical management organization |
ICD-9 (398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.91) |
| Stafylas, 2016 | EURObservational Research Programme: The Heart Failure Pilot Survey (ESC-HF Pilot) EOPYY- Greek National Organization for Health Care Provision |
Hospitalization for HF or HF diagnosis according to clinical judgement of the responsible cardiologist |
| Lee, 2016 [31] | Claims data from the National Health Insurance (NHI) Claims data from Medical Aid (MA) |
ICD-10 (I11.0, I13.0, I13.2, I50.x) |
| Murphy, 2016 | National Casemix Program, patient interviews, hospital records | ICD-10 |
| Ogah, 2014 [32] | Abeokuta HF registry (hospital registry), patient interviews | ICD-10 |
To identify HF patients, the studies used different methods. Six articles referred to the ICD-10 (International Classification of Diseases), [27–32], five to the ICD-9 [24, 26, 33–35] and five [23, 25, 36–38] didn’t specify the ICD classification.
Because HF is usually accompanied by many underlying diseases, it is often difficult to identify the correct cases of HF based on the diagnosis codes of ICD. Lee et al. [31] showed that by defining HF only as the primary diagnosis the HF cases decrease by 46% in contrast to define HF cases as primary and secondary diagnosis (using the same ICD-codes). By further analyzes he showed, that 75% of patients with HF, which was defined as a secondary diagnosis had a primary diagnosis which was related to HF, such as hypertension or angina pectoris. Thus, defining HF only as the primary diagnosis might lead to an under-specification of HF [31].
A second study of Voigt et al. [35] calculated costs for HF as the primary diagnosis (HF in isolation, HFI) and HF as one of multiple diagnosis/part of a disease milieu (HF syndrome, HFS). As a consequence, costs range between 70.8 (HFI)- 127.0 (HFS) billion dollars. This might show the great underestimation of economic burden, if defining HF only as the primary diagnosis [35].
Epidemiological data
HF shows high prevalence rates with 12.4 per 1000 persons suffering from this chronic condition [31]. The prevalence rates increase with age [29, 31, 36], with patients aged 65 or older showed 9.2-fold higher prevalence and 1.6 higher costs than 19–64 aged population [31]. Neumann et al. [29] analyzed that patients 65 or older shows 10-times higher prevalence rates than 45–65 aged patients.
Incidence rates are also high with 2.4–3.8 per 1000 persons [33]. HF results in a severe mortality rate with 1-year mortality after HF hospitalization of 24% [33]. Stafylas et al. [38] showed that the mortality rates are higher for patients, who were hospitalized for HF (24,3%) than for HF patients treated outpatient (7,7%).
The included studies reported high, similar readmission rates for HF between 42% and 44,9% [26, 28, 38].
Of the included articles, two separated the cost data by gender [28, 29] and both reported higher costs for women.
Cost components
To enable better comparability, prevalence-based studies were grouped separately from the incidence-based ones.
Cost components of the prevalence-based approach
The cost components of the included studies were subject to large variations (Table 3). Most of the articles considered the economic burden of HF only in terms of direct costs, such as costs attributed to hospitalization, medication, home care, etc. Two studies [31, 37] additionally accounted for the costs of informal care. Informal caregiving was defined as care provided by individuals who were not professional social or health care workers [37]. The indirect costs in terms of loss of productivity were considered only by three studies [31, 32, 35]. Lee et al. [31] calculated caregiver’s costs as the product of the average annual inpatient days per patient due to HF and the average market price for the daily charge of a helper. He also calculated indirect costs in terms of productivity loss due to morbidity and mortality for ages under 65 by using mathematical equations derived from the human capital approach.
Table 3.
Summary of the cost components (studies with an incident and mixed approach are underlined)
| Cost components | (37) | (29) | (36) | (35) | (28) | (23) | (24) | (30) | (38) | (31) | (32) | (27) | (34) | (33) | (26) | (25) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Direct costs | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Inpatient care | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Medication | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Laboratory | ✓ | ✓ | ✓ | |||||||||||||
| Physicians | ✓ | ✓ | ||||||||||||||
| Intensive care units | ✓ | ✓ | ||||||||||||||
| Nursing home | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Outpatient care | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Hospital Outpatient care | ✓ | ✓ | ✓ | |||||||||||||
| Physicians | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Specialist | ✓ | |||||||||||||||
| Home care | ✓ | ✓ | ||||||||||||||
| Medication | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Laboratory /Procedures | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||
| Paramedical staff | ✓ | ✓ | ✓ | |||||||||||||
| Medical transport | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Indirect costs | ✓ | ✓ | ✓ | |||||||||||||
| Informal care costs | ✓ | ✓ |
In the prospective, observational study Delgado et al. [37] estimated the costs of informal care by recording the hours of caregiving provided. The maximum number of caregiving hours per person was limited to 112 (16 h per day for 7 days of caregiving weekly). The number of hours was multiplied with the mean costs of an hour of home care.
Ogah et al. [32] calculated the costs for productivity loss by recording the days of lost work and multiplying them with the minimum wage.
Among the aspects of direct costs, hospital admission and medication were examined in most of the papers. Agvall et al. [28] and Czech et al. [36] estimated the costs for treatment in intensive care units apart from the hospitalization costs. There were also differences in the outpatient care cost components. Whereas most of the included studies reported costs for outpatient medication and physician visits, five articles reported cost data for laboratory and procedures [28, 29, 32–34, 38] such as speech and physical therapy. The economic burden of home care was estimated by Voigt and Delgado et al. [35, 37]. Home care referred to care which was provided by professional caregivers at home.
Cost components of the incidence-based group
In comparison to the prevalence-based group, the articles with an incidence-based or mixed approach have less cost components (Table 3). All studies included costs for inpatient care, and all except one [25] considered the costs for medication. None of the studies estimated the costs for home care, nursing homes, informal caregiving or indirect costs.
Cost estimates
The main economic estimates are presented in Table 4. The total annual costs per patient ranged from $868 for South Korea [31] to $25,532 for Germany [30]. Two articles [29, 35] accounted the costs not per patient, but analyzed the whole economic burden of HF per year in an aggregated way. The hospitalization costs are the greatest cost component of overall healthcare costs. Among total healthcare costs, expenditures for medication are the second largest issue [33, 37]. Due to hospitalization costs, room and board were the greatest contributor (43% of inpatient costs), following by procedures, imaging and laboratory testing [34]. Dialysis was responsible for the highest part of procedural costs, but it was needed only by a small number of patients [34].
Table 4.
Summary of cost estimates (studies with an incident and mixed approach are underlined)
| Reference | Year of cost data | Country | Reported annual costs in local currency (costs per patient) | Local currency in 2016 | $US (2016 PPP) | % of inpatient costs of all direct costs | Expenditure on health, per capita, US$ (2016 PPP) |
|---|---|---|---|---|---|---|---|
| Voigt, 2014 [35] | 2012 | USA | $60.2 - $115.4ba(direct costs) $70.8 - $127.0ba(total costs) |
$62.9 - $120.7ba $74.0 - $133.0ba |
62.9–120.7ba 74.0–133.0ba |
66 | 9892 |
| Czech, 2013 [36] | 2010 | Poland | 7739 PLN | 8312 PLN | 4755 | 92e | 1798 |
| Delgado, 2013 | 2010 | Spain | 4860€ (healthcare costs) | 5166€ | 7792 | 58e | 3248 |
| Bogner, 2010 [24] | 2009 | USA | 22,230$b | 24,873$b | 24,873b | 84 | 9892 |
| Zugck, 2010 [30] | 2002 | Germany | 11,794–16,303 €c | 14,297–19,762 €c | 18,472–25,532c | 72 | 5551 |
| Neumann, 2009 [29] | 2006 | Germany | 2.879b €a | 3.293b €a | 4.255ba | 60 | 5551 |
| Liao, 2007 [23] | 2006 | USA | $10,832 | 12,907$ | 12,907 | 65e | 9892 |
| Agvall, 2005 [28] | 2000 | Sweden | 37,060 SEK | 44,971 SEK | 5044 | 47 | 5488 |
| Stafylas, 2016 | 2014 | Greece | 4411 € | 4295 € | 7053 | 73e | 2223 |
| Ogah, 2014 [32] | 2010 | Nigeria | 2128$ | 2343$ | 2343 | 44 | NA |
| Lee, 2016 [31] | 2016 | South Korea | 868$ (perspective of third-party-payer) 1414$ (perspective of society) |
868$ 1414$ |
868 1414 |
53 | NA |
| Dunlay, 2011 [34] | 2007 | USA | 109.541$ (lifetime costs from HF diagnosis until death) | 126.819$ | 126.819 | 77 | 9892 |
| Corrao, 2014 [33] | 2011 | Italy | 11,100 € | 11,597 € | 15,952 | 92e | 3391 |
| Liao, 2006 [25] | 2000 | USA | 32,580–33,023$ (prevalent group)d 45,604–49,128$ (incident group)d |
45,406–46,023$d 63,557–68,468$d |
45,406–46,023d 63,557–68,468d |
65–67 70–72 |
9892 |
| Ory, 2005 [26] | 2000 | USA | 14,465$ (prevalent group) 17,744$ (incident group) |
20,159$ 24,729$ |
20,159 24,729 |
NA | 9892 |
| Murphy, 2016 | 2013 | Ireland | 12,206 € (patients with preserved EF) 13,011 € (patients with reduced EF) |
12,194 € 12,999 € |
15,334 16,330 |
92e 96e |
5528 |
aAggregated costs for all HF patients
bCosts aggregated for two years
cCosts depend on number of visits to doctors
dCumulated costs for 5 years
enot clearly stated in the study
SEK Swedish kronas, PLN Polish Zloty, b Billions, EF ejection fraction
The study of Delgado et al. [37] considered the burden of costs of informal caregiving per patient. He estimated that 59.1 to 69,8% were due to informal care costs. Additionally, he showed that the healthcare and informal care costs for HF were rapidly increasing with the number of hospital admissions, contributing to overall increases in total costs for HF. Of the included studies Dunlay et al. [34] presented the lifetime costs for HF for the longest study period.
Ory et al. [26] reported that newly diagnosed patients had significantly higher healthcare charges than the prevalent group. Furthermore, he described that – in comparison to the control group without HF- the patients with HF created four times higher total healthcare costs.
The study of Ogah et al. [32] was the only one conducted in a low/middle income country (Nigeria). 46% of the total costs were contributable to inpatient and 54% to outpatient costs [32]. Inpatient costs were lower than in high-income countries because in these countries the utilization of expensive medical equipment and surgery are higher. Ogah et al. [32] showed that 90% of direct outpatient costs are due to medication and transportation costs for monthly follow-up visits, which were mostly made through out-of-pocket payments.
Predictors of increasing costs
Some studies estimated cost predictors, which are shown in Table 5. A higher NYHA stage [23, 25, 37, 38], kidney dysfunction [25, 38] and the comorbidity of HF and diabetes mellitus [24, 34] were considered as the most common reasons of increasing costs for HF patients. Two studies [23, 33] reported that that comorbid conditions of HF were much more associated with greater costs than prevalent HF alone. Comorbidities in HF cause ¾ of all readmissions in HF patients [33]. Dunlay et al. [34] conducted a study with an incident epidemiological approach and analyzed that diabetes mellitus caused an increase in lifetime costs of HF patients of 25%. Bogner et al. [24] also emphasized that diabetes mellitus has substantial influence on the costs of managing HF patients, extends the hospital stay and worsens the prognosis. A study analyzed that a preserved ejection fraction (> = 50%) in HF patients leads to an increasing cost impact of 24% [34]. In contrast, Liao et al. [25] showed that there was no statistically significant difference between HF patients with normal and reduced EF due to the 5-year cumulative costs.
Table 5.
Predictors of increasing costs
| Reference | Predictors of increasing costs (x times higher costs) |
|---|---|
| Stafylas, 2016 | • NYHA stage • Kidney dysfunction |
| Lee, 2016 [31] | • Age > = 65 (1.6) • Number of hospitalizations (9.7 for one hospitalization) |
| Bogner, 2010 [24] | • Diabetes mellitus (0.4) |
| Dunlay, 2011 [34] | • Diabetes mellitus (0.25) • Ejection fraction > = 50 (0.24) |
| Liao, 2006 [25] | • NYHA stage (NYHA 4–0.77, NYHA 3–0.12) • Kidney dysfunction (creatinine > = 1.4 mg/dl – 0.48) • Coronary artery disease (0.32) • COPD (0.38) • Hypertension (0.27) |
| Liao, 2007 [23] | • NYHA stage (NYHA 3/4–0.41) • Coronary artery disease (0.66) • Kidney dysfunction (0.13) • COPD (0.44) |
| Delgado, 2013 | • NYHA stage (NYHA 3/4: 0.6–0.8 times higher costs than NYHA 2) |
The severity of HF is classified by NYHA (New York Heart Association) stages [1]. Of the included studies, only two [36, 37] separated the cost data by NYHA stage (Table 6). Czech et al. [36] gave very detailed information on cost data by NYHA class I-IV, estimating the total annual costs as well as the average costs of hospitalization for HF by NYHA stage. Delgado et al. [37] reported economic data for NYHA stages II-IV and estimated the total costs for HF by combining the NYHA groups III and IV. He emphasized the rising costs and the significantly increased use of health services and social services, as formal and informal care, by NYHA stage. Both studies showed that the economic burden of HF is dependent on the NYHA stage and the costs rise with advanced stages, disregarding NYHA stage I. Thus, it is important to act early and to prevent the progression of HF to more advanced and highly symptomatic forms. Czech et al. [36] reported for NYHA I high annual as well as hospitalization costs and assumed that this could be attributable to the higher proportion of special cardiology interventions in this group. Additionally, he described that NYHA IV was responsible for more than 70% of total annual costs for HF.
Table 6.
Costs by NYHA stage
| Reference | Year of cost data | Country | NYHA I | NYHA II | NYHA III | NYHA IV | Total costs per patient and year |
|---|---|---|---|---|---|---|---|
| local currency in year of costs/ local currency in 2016/ $US in 2016, PPP |
|||||||
| Delgado, 2013 (direct costs) |
2010 | Spain | – | 3789€/ 4028€/ 6075$ |
6832€/ 7262€/ 10,953$ |
4860€/ 5166€/ 7792$ |
|
| Delgado, 2013 (total costs) |
2010 | Spain | – | 10,283–14,459€/ 10,931–15,370€/ 16,487–23,183$ |
18,265–23,721€/ 19,416–25,215€/ 29,285–38,032$ |
12,995–18,220€/ 13,814–19,368€/ 20,836–29,213$ |
|
| Czech, 2013 [36] | 2010 | Poland | a | 5,315PLN/ 5,708PLN/ 3265$ |
8,116PLN/ 8,717PLN/ 4987$ |
21,273PLN/ 22,847PLN/ 13,070$ |
7739PLN/ 8312PLN/ 4755$ |
a Costs are reported, but not listed here
PLN Polish Zloty
Distribution of costs
Two articles [25, 34] compared the cost data of patients in the first year of HF diagnosis to the previous year in order to investigate the impact of HF on the costs (Table 7). Dunlay et al. [34] reported an 318% increase in costs in the year of HF diagnosis. He also examined that the costs for HF were high at the time of initial diagnosis, decreased then, reached a stable, relative low level and increased again at the end of life. Liao et al. [25] estimated in his study that the development of HF had a greater than 200% increase in total costs compared to the year before diagnosis. This strong rise was especially generated by the inpatient cost component. After that he detected a decrease of costs, but they were still higher than in the year before HF diagnosis out to year 5, if only survivors were examined.
Table 7.
Comparison of costs
| Reference | Year of costs | Country | Year prior to HF diagnosis | Year beginning with HF diagnosis | Difference in costs (local currency in year of costs) | Difference in costs (local currency in 2016) | Difference in costs ($US in 2016, PPP) | Raise of the costs in % |
|---|---|---|---|---|---|---|---|---|
| Dunlay, 2011 [34] | 2007 | USA | 8219$ | 34,372$ | 26,153$ | 30,278$ | 30,278 | 318 |
| Liao, 2006 [23] | 2000 | USA | 6650–6752$ | 24,882–25,503$ | 18,232–18,751$ | 25,409–26,133$ | 25,409–26,133 | 274–278 |
Discussion
Our systematic review highlights the economic impact of HF as a rising burden for high-income countries. Furthermore, it also uncovers the large heterogeneity of COI studies focused on HF.
Comparison of the cost data
The main findings of our review are reported in Table 4 and are focused on the highest annual per-patient costs reported for the USA [24] and Germany [30]. Our review shows that the costs for hospital admission contribute significantly to the overall direct costs for HF (ranging from 44 to 96%). Previously published studies accounted that about two-thirds of the direct HF healthcare costs are due to hospitalization [6, 39]. The high inpatient costs are a result of high readmission rates, with 23% of HF patients readmitted to hospital stay within 6 months [6]. A further aspect of our analyses is the considerable increase in costs with advanced NYHA stage, with NYHA stage IV being the most expensive. Biermann et al. [5] estimated similar results for patients with systolic HF. An earlier review [40] estimated that patients with NYHA IV produce between 8 and 30 times higher healthcare costs than patients with NYHA II. We have shown that costs rise rapidly after a confirmed HF diagnosis (Table 7). Although HF is a chronic condition causing high lifetime costs, particularly the first year after a HF diagnosis and the end-of-life care are the most expensive ones. Two studies from the USA [41] and Canada [42] analyzed the last 180 days of life of HF patients and concluded that in the last six months of life, there is a large increase in costs and resource use. Unroe et al. [41] as well as Kaul et al. [42] analyzed that the costs during the last 180 days rose from $28,766 to $36,215 between the years 2000–2007 for the USA [41] and from $25,069 to $27,983 (Canadian dollars) between the years 2000–2006 for Canada [42].
Other studies also report a rise in costs relating to HF over time, but especially in the last two decades. Stewart et al. [39] reported a rise of direct medical costs from £716 million in 1995 to £905 million in 2000 for the UK. Liao et al. [6] presented an increase of HF-related costs for different countries (Spain, Canada, Sweden and Scotland) by 40–71%.
The need for standards for future COI-studies in HF
Our review highlighted not only the large economic burden of HF, but also the heterogeneity of the studies and lack of cost data. For better comparison of research data, future COI studies should use a standardized approach regarding methodology, in particular regarding criteria concerning the selection of HF patients and data, the inclusion of different cost drivers and the presentation of results.
Thus, further COI studies in HF should clearly state the ICD codes, which were used for identification of HF patients. Additionally, an attribution of cost data to the specific ICD code number could achieve a better comparison between COI studies. As presented in recently published papers, using different ICD codes may lead to an over- or underestimation of HF diagnosis [43, 44].
COI studies should present cost data for the whole HF group and disaggregate them consistently for sub-entities, as systolic or diastolic HF. Importantly, COI studies should emphasize clearly stating the use of the exact diagnoses (including relevant ICD codes). It should be clearly stated, if HF is defined as the primary or secondary diagnosis, as this difference influences the cost estimates. The inclusion of comorbidities would give detailed information on the cost drivers and show opportunities for decreasing costs.
In addition, the study perspective and a distinction between COI approaches should be indicated [18]. This review emphasizes that indirect costs are a significant contributor to total costs and more effort is needed to estimate these costs accurately and consistently. In addition, informal care costs are an important contributor to the COI of HF [37].
As there are many differences between healthcare systems in different countries, high-quality cost data is needed from COI studies to facilitate comparisons between countries and cost trends. Crucially, more robust data from future COI studies is needed to provide a sound basis for cost-effectiveness studies to identify the most cost-effective therapies.
Another aspect in our systematic review highlights that most of the studies are conducted in Europe and USA. But as HF is a global problem, we need more COI-studies from low-and middle-income countries as demanded in a recently published study [45].
Study limitations
The cost data we included in our systematic review derived from a heterogeneous set of studies with different methodologies used, to collect the data. This lack of a standard method for collecting the cost data may impact some of our findings. The included studies were conducted in different countries with various healthcare systems. This may lead to an over- or underestimation of some cost data, as the included studies not clearly describe, which costs are included in their analyses. For example, some studies present the costs in a detailed way, whereas other studies aggregate particular costs to one cost position.
Conclusion
Our review highlights the considerable and growing economic burden of HF on the health care systems of industrialized countries. The trend for rising costs has especially been more significant during the last 20 years and future demographic developments predict more dramatic rises in the future. Due to the high economic burden of HF -especially in terms of inpatient costs- we need more compelling and innovative strategies to counteract the effects of HF. Reducing admission rates in acute HF is the most promising approach to decrease the economic burden of HF. In this context telemonitoring devices like a wireless pulmonary artery pressure monitoring system are promising new innovations [46–48]. As reported in a recently published study [49] this device has the potential to reduce the hospitalization rates for symptomatic HF by 37% and to lead to a significant cost reduction. The COI studies included in this review showed large variations in methodology used and the cost results vary as a consequence. Future COI studies would greatly benefit from a detailed presentation of cost components. Our review shows that there is a lack on cost data and further research is needed to highlight the economic burden of indirect costs of HF. High quality data from COI studies with a robust methodology applied can inform policy makers about the major cost drivers of HF and can be used as the basis of further economic evaluations.
Additional files
List of search terms, databases and results of each search. (DOCX 13 kb)
Criteria used for inclusion/exclusion of reviewed articles. (DOCX 14 kb)
Acknowledgements
The present work was performed in fulfillment of the requirements for obtaining the degree “Dr. med.” for author Wladimir Lesyuk at the Medical Faculty of Friedrich-Alexander-University Erlangen-Nürnberg.
Funding
This project was funded by the German Federal Ministry of Education Research (BMBF) as part of the National Cluster of Excellence “Medical Technologies – Medical Vallex EMN” (Project grant No. 13EX1013B).
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- COI
Cost-of-Illness
- HF
Heart failure
- NYHA
New York Heart Association
Authors’ contributions
WL collected, analysed and interpreted the data. He was also a major contributor in writing the manuscript. CK checked the data results. PK supervised and corrected the work. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12872-018-0815-3) contains supplementary material, which is available to authorized users.
Contributor Information
Wladimir Lesyuk, Email: wladimir.lesyuk@uk-erlangen.de.
Christine Kriza, Email: christinekriza@hotmail.com.
Peter Kolominsky-Rabas, Email: Peter.Kolominsky@uk-erlangen.de.
References
- 1.Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the heart failure association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM) Eur Heart J. 2008;29(19):2388–2442. doi: 10.1093/eurheartj/ehn309. [DOI] [PubMed] [Google Scholar]
- 2.Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289(2):194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 3.Remme WJ, Swedberg K. Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J. 2001;22(17):1527–1560. doi: 10.1053/euhj.2001.2783. [DOI] [PubMed] [Google Scholar]
- 4.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biermann J, Neumann T, Angermann CE, Düngen HD, Erbel R, Herzog W, et al. Resource use and costs in systolic heart failure according to disease severity: a pooled analysis from the German competence network heart failure. Journal of Public Health (Germany) 2012;20(1):23–30. doi: 10.1007/s10389-011-0452-0. [DOI] [Google Scholar]
- 6.Liao L, Allen LA, Whellan DJ. Economic burden of heart failure in the elderly. PharmacoEconomics. 2008;26(6):447–462. doi: 10.2165/00019053-200826060-00001. [DOI] [PubMed] [Google Scholar]
- 7.Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure? Europace : European pacing, arrhythmias, and cardiac electrophysiology : Journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2011;13 Suppl 2:ii13–ii17. [DOI] [PubMed]
- 8.Bundkirchen A, Schwinger RHG. Epidemiology and economic burden of chronic heart failure. European Heart Journal, Supplement. 2004;6(D):D57–D60. doi: 10.1016/j.ehjsup.2004.05.015. [DOI] [Google Scholar]
- 9.Reed SD, Whellan DJ, Li Y, Friedman JY, Ellis SJ, Pina IL, et al. Economic evaluation of the HF-ACTION (heart failure: a controlled trial investigating outcomes of exercise training) randomized controlled trial: an exercise training study of patients with chronic heart failure. Circulation Cardiovascular quality and outcomes. 2010;3(4):374–381. doi: 10.1161/CIRCOUTCOMES.109.907287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pocock SJ, Ariti CA, McMurray JJ, Maggioni A, Kober L, Squire IB, et al. Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies. Eur Heart J. 2013;34(19):1404–1413. doi: 10.1093/eurheartj/ehs337. [DOI] [PubMed] [Google Scholar]
- 11.Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, Krumholz HM. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: a retrospective observational cohort study. PLoS Med. 2014;11(9):e1001737. doi: 10.1371/journal.pmed.1001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cook C, Cole G, Asaria P, Jabbour R, Francis DP. The annual global economic burden of heart failure. Int J Cardiol. 2014;171(3):368–376. doi: 10.1016/j.ijcard.2013.12.028. [DOI] [PubMed] [Google Scholar]
- 13.Wimo A. The art of cost of illness. Journal of Alzheimer's disease : JAD. 2010;19(2):617–619. doi: 10.3233/JAD-2010-1268. [DOI] [PubMed] [Google Scholar]
- 14.Wang XJ, Lopez SE, Chan A. Economic burden of chemotherapy-induced febrile neutropenia in patients with lymphoma: a systematic review. Crit Rev Oncol Hematol. 2015;94(2):201–212. doi: 10.1016/j.critrevonc.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 15.Larg A, Moss JR. Cost-of-illness studies: a guide to critical evaluation. PharmacoEconomics. 2011;29(8):653–671. doi: 10.2165/11588380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology (Cambridge, Mass) 2011;22(1):128. doi: 10.1097/EDE.0b013e3181fe7825. [DOI] [PubMed] [Google Scholar]
- 17.Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care. 2005;21(2):240–245. [PubMed] [Google Scholar]
- 18.Drummond MF, Jefferson TO Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ economic evaluation working party. BMJ (Clin Res ed) 1996;313(7052):275–283. doi: 10.1136/bmj.313.7052.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 20.OECD . Consumer Price Index. 2016. [Google Scholar]
- 21.OECD . PPP. 2016. [Google Scholar]
- 22.Payne KA, Huybrechts KF, Caro JJ, Craig Green TJ, Klittich WS. Long term cost-of-illness in stroke: an international review. PharmacoEconomics. 2002;20(12):813–825. doi: 10.2165/00019053-200220120-00002. [DOI] [PubMed] [Google Scholar]
- 23.Liao L, Anstrom KJ, Gottdiener JS, Pappas PA, Whellan DJ, Kitzman DW, et al. Long-term costs and resource use in elderly participants with congestive heart failure in the cardiovascular health study. Am Heart J. 2007;153(2):245–252. doi: 10.1016/j.ahj.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 24.Bogner HR, Miller SD, de Vries HF, Chhatre S, Jayadevappa R. Assessment of cost and health resource utilization for elderly patients with heart failure and diabetes mellitus. J Card Fail. 2010;16(6):454–460. doi: 10.1016/j.cardfail.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liao L, Jollis JG, Anstrom KJ, Whellan DJ, Kitzman DW, Aurigemma GP, et al. Costs for heart failure with normal vs reduced ejection fraction. Arch Intern Med. 2006;166(1):112–118. doi: 10.1001/archinte.166.1.112. [DOI] [PubMed] [Google Scholar]
- 26.Ory C, Vanderplas A, Dezii C, Chang E. Congestive heart failure: attributable costs within the managed care setting. Journal of Pharmaceutical Finance, Economics and Policy. 2005;14(2):87–97. doi: 10.1300/J371v14n02_07. [DOI] [Google Scholar]
- 27.Murphy TM, Waterhouse DF, James S, Casey C, Fitzgerald E, O'Connell E, et al. A comparison of HFrEF vs HFpEF's clinical workload and cost in the first year following hospitalization and enrollment in a disease management program. Int J Cardiol. 2017;232:330–335. doi: 10.1016/j.ijcard.2016.12.057. [DOI] [PubMed] [Google Scholar]
- 28.Agvall B, Borgquist L, Foldevi M, Dahlstrom U. Cost of heart failure in Swedish primary healthcare. Scand J Prim Health Care. 2005;23(4):227–232. doi: 10.1080/02813430500197647. [DOI] [PubMed] [Google Scholar]
- 29.Neumann T, Biermann J, Neumann A, Wasem J, Ertl G, Dietz R, et al. Heart failure: the commonest reason for hospitalization in Germany - medical and economic perspectives. Dtsch Arztebl Int. 2009;106(16):269–275. doi: 10.3238/arztebl.2009.0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zugck C, Muller A, Helms TM, Wildau HJ, Becks T, Hacker J, et al. Health economic impact of heart failure: an analysis of the nationwide German database. Deutsche medizinische Wochenschrift (1946) 2010;135(13):633–638. doi: 10.1055/s-0030-1251912. [DOI] [PubMed] [Google Scholar]
- 31.Lee H, Oh SH, Cho H, Cho HJ, Kang HY. Prevalence and socio-economic burden of heart failure in an aging society of South Korea. BMC Cardiovasc Disord. 2016;16(1):215. doi: 10.1186/s12872-016-0404-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ogah OS, Stewart S, Onwujekwe OE, Falase AO, Adebayo SO, Olunuga T, et al. Economic burden of heart failure: investigating outpatient and inpatient costs in Abeokuta, Southwest Nigeria. PLoS One. 2014;9(11):e113032. doi: 10.1371/journal.pone.0113032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Corrao G, Ghirardi A, Ibrahim B, Merlino L, Maggioni AP. Burden of new hospitalization for heart failure: a population-based investigation from Italy. Eur J Heart Fail. 2014; [DOI] [PubMed]
- 34.Dunlay SM, Shah ND, Shi Q, Morlan B, VanHouten H, Long KH, et al. Lifetime costs of medical care after heart failure diagnosis. Circ Cardiovasc Qual Outcomes. 2011;4(1):68–75. doi: 10.1161/CIRCOUTCOMES.110.957225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Voigt J, Sasha John M, Taylor A, Krucoff M, Reynolds MR, Michael Gibson C. A reevaluation of the costs of heart failure and its implications for allocation of health resources in the United States. Clin Cardiol. 2014;37(5):312-21. [DOI] [PMC free article] [PubMed]
- 36.Czech M, Opolski G, Zdrojewski T, Dubiel JS, Wizner B, Bolisega D, et al. The costs of heart failure in Poland from the public payer's perspective. Polish programme assessing diagnostic procedures, treatment and costs in patients with heart failure in randomly selected outpatient clinics and hospitals at different levels of care: POLKARD. Kardiol Pol. 2013;71(3):224–232. doi: 10.5603/KP.2013.0032. [DOI] [PubMed] [Google Scholar]
- 37.Delgado JF, Oliva J, Llano M, Pascual-Figal D, Grillo JJ, Comin-Colet J, et al. Health care and nonhealth care costs in the treatment of patients with symptomatic chronic heart failure in Spain. Rev Esp Cardiol. 2014;67(8):643-50. [DOI] [PubMed]
- 38.Stafylas P, Farmakis D, Kourlaba G, Giamouzis G, Tsarouhas K, Maniadakis N, et al. The heart failure pandemic: the clinical and economic burden in Greece. Int J Cardiol. 2017;227:923–929. doi: 10.1016/j.ijcard.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 39.Stewart S, Jenkins A, Buchan S, McGuire A, Capewell S, McMurray JJ. The current cost of heart failure to the National Health Service in the UK. Eur J Heart Fail. 2002;4(3):361–371. doi: 10.1016/S1388-9842(01)00198-2. [DOI] [PubMed] [Google Scholar]
- 40.Berry C, Murdoch DR, McMurray JJ. Economics of chronic heart failure. Eur J Heart Fail. 2001;3(3):283–291. doi: 10.1016/S1388-9842(01)00123-4. [DOI] [PubMed] [Google Scholar]
- 41.Unroe KT, Greiner MA, Hernandez AF, Whellan DJ, Kaul P, Schulman KA, et al. Resource use in the last 6 months of life among medicare beneficiaries with heart failure, 2000-2007. Arch Intern Med. 2011;171(3):196–203. doi: 10.1001/archinternmed.2010.371. [DOI] [PubMed] [Google Scholar]
- 42.Kaul P, McAlister FA, Ezekowitz JA, Bakal JA, Curtis LH, Quan H, et al. Resource use in the last 6 months of life among patients with heart failure in Canada. Arch Intern Med. 2011;171(3):211–217. doi: 10.1001/archinternmed.2010.365. [DOI] [PubMed] [Google Scholar]
- 43.Khand AU, Shaw M, Gemmel I, Cleland JG. Do discharge codes underestimate hospitalisation due to heart failure? Validation study of hospital discharge coding for heart failure. Eur J Heart Fail. 2005;7(5):792–797. doi: 10.1016/j.ejheart.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 44.Goff DC, Jr, Pandey DK, Chan FA, Ortiz C, Nichaman MZ. Congestive heart failure in the United States: is there more than meets the I(CD code)? The Corpus Christi heart project. Arch Intern Med. 2000;160(2):197–202. doi: 10.1001/archinte.160.2.197. [DOI] [PubMed] [Google Scholar]
- 45.Callender T, Woodward M, Roth G, Farzadfar F, Lemarie JC, Gicquel S, et al. Heart failure care in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med. 2014;11(8):e1001699. doi: 10.1371/journal.pmed.1001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abraham WT, Adamson PB, Bourge RC, Aaron MF, Costanzo MR, Stevenson LW, et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet (London, England) 2011;377(9766):658–666. doi: 10.1016/S0140-6736(11)60101-3. [DOI] [PubMed] [Google Scholar]
- 47.Abraham WT, Stevenson LW, Bourge RC, Lindenfeld JA, Bauman JG, Adamson PB. Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: complete follow-up results from the CHAMPION randomised trial. Lancet (London, England) 2016;387(10017):453–461. doi: 10.1016/S0140-6736(15)00723-0. [DOI] [PubMed] [Google Scholar]
- 48.Dagres N, Hindricks G. Pulmonary pressure, telemedicine, and heart failure therapy. Lancet (London, England) 2016;387(10017):408–410. doi: 10.1016/S0140-6736(15)00808-9. [DOI] [PubMed] [Google Scholar]
- 49.Kolominsky-Rabas PL, Kriza C, Djanatliev A, Meier F, Uffenorde S, Radeleff J, et al. Health economic impact of a pulmonary artery pressure sensor for heart failure Telemonitoring: a dynamic simulation. Telemed J E Health. 2016;22(10):798-808. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List of search terms, databases and results of each search. (DOCX 13 kb)
Criteria used for inclusion/exclusion of reviewed articles. (DOCX 14 kb)
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information files.


