Abstract
Objective:
“Stroke code” (SC) implementation in hospitals can improve the rate of thrombolysis and the timeline in care of stroke patient.
Materials and Methods:
A prospective data of patients treated for acute ischemic stroke (AIS) after implementation of “SC” (post-SC era) were analyzed (2015–2016) and compared with the retrospective data of patients treated in the “pre-SC era.” Parameters such as symptom-to-door, door-to-physician, door-to-imaging, door-to-needle (DTN), and symptom-to-needle time were calculated. The severity of stroke was calculated using the National Institutes of Health Stroke Score (NIHSS) before and after treatment.
Results:
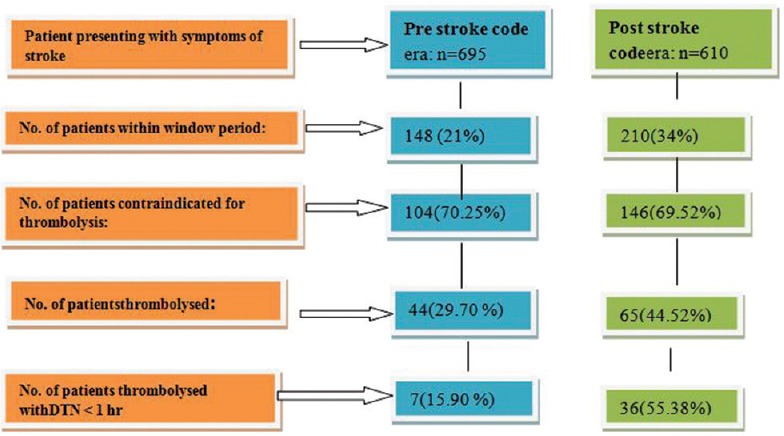
Patients presented with stroke symptoms in pre- and post-SC era (695 vs. 610) and, out of these, patients who came in window period constituted 148 (21%) and 210 (34%), respectively. Patients thrombolyzed in pre- and post-SC era were 44 (29.7%) and 65 (44.52%), respectively. Average DTN time was 104.95 min in pre-SC era and reduced to 67.28 min (P < 0.001) post-SC implementation. Percentage of patients thrombolyzed within DTN time ≤60 min in pre-SC era and SC era was 15.90% and 55.38%, respectively.
Conclusion:
Implementation of SC helped us to increase thrombolysis rate in AIS and decrease DTN time.
Keywords: Acute ischemic stroke, door to needle time, stroke code
INTRODUCTION
Stroke is a common and concerning medical problem worldwide because of the disabilities and deaths associated with it.[1] It is one of the most important causes of death both in urban and rural parts of India.[2] It is estimated that, in coming years, the burden will mostly increase in developing countries compared to developed countries.[3] India comparatively has a higher prevalence of hemorrhagic strokes compared to the west with the percentage of strokes approaching 70%–80% depending on the location.[4,5]
Time is the essence in the treatment of acute strokes both hemorrhagic and ischemic types. Prompt treatment of stroke patients is associated with better patient outcomes in the form of lesser symptomatic intracranial hemorrhage rates, better discharge destinations as well as lower inhospital mortality rates.[6,7] However, significant delays are often seen in the treatment of patients with acute stroke,[8] especially in resource-limited settings. There are multiple limitations in thrombolysis of stroke patients even in tertiary care centers.[9] Delay in treatment in the hospital can be minimized by utilizing a systematic approach.[10] Efforts are continuously made to reduce the time lag between patient arrival and initiation of treatment. “Stroke code” (SC), i.e., a rapid response system is one such approach.[8,11,12] We implemented this “SC” in the hospital. The stroke team members including the nursing staff and supporting staff were trained on “SC”. Data on the impact of SC in an Indian tertiary care setup are limited.
Objective
The objective of this study was to evaluate the impact of SC implementation on outcomes in patients with acute ischemic stroke (AIS).
MATERIALS AND METHODS
Approval from the Institutional Ethics committee was received for the study protocol. Data of patients with AIS treated after implementation of SC in 2014 (post-SC era) were analyzed and compared with the previously published pre-SC data.[9] Consecutive patients presenting with symptoms of stroke were screened at the emergency and only those patients within the window period for thrombolysis, i.e., within 4.5 h after onset of symptoms of stroke were screened. After imaging, decision for thrombolysis was made. The evaluation parameters included the National Institutes of Health Stroke Scale (NIHSS) score before and after treatment in both groups, i.e., pre- and post-SC period. Other parameters, i.e., symptom-to-door (STD), door-to-physician (DTP), door-to-imaging (DTI), and finally, door-to-needle (DTN) time were calculated and compared in patients before and after SC implementation. The improvement in thrombolyzed patients at 3 months was tracked telephonically – this improvement was assessed with the help of modified Rankin (mRS) score. The number of patients with a DTN time <60 min was compared before and after SC implementation. Furthermore, hour-wise distribution of thrombolyzed patients was analyzed [Figure 1].
Figure 1.
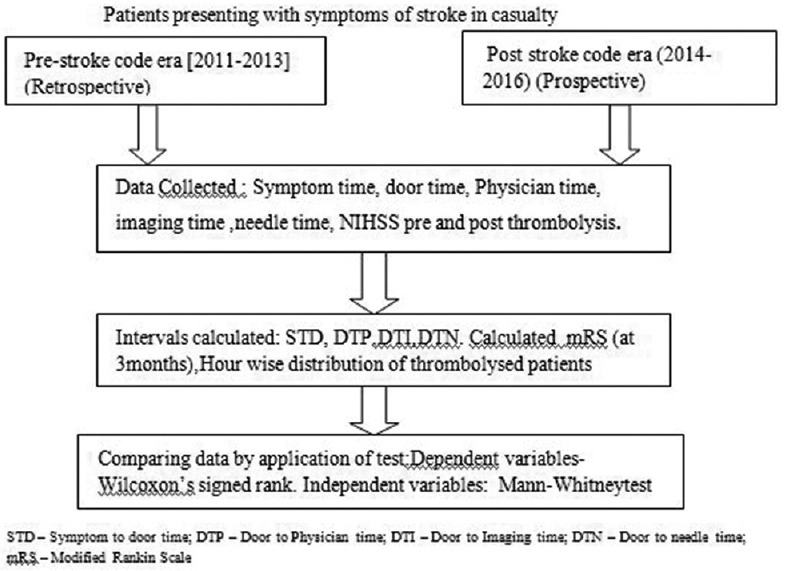
Flowchart of parameters of stroke patients used for analysis in our study
Statistical analysis
Primary analysis along with graphical representation of the data was carried out using MS Excel. Descriptive statistical analysis was carried out to explore the distributions of several characteristics of the cases studied. The results on categorical data were shown as n (% of cases) and the results on quantitative variables were shown as mean ± standard deviation. The data were checked for normality, and statistical comparisons were done using appropriate statistical tests [Figure 2]. Dependent variables were compared using Wilcoxon signed-rank test while independent variables were compared using Mann–Whitney test. Z-test of proportions was also used to compare proportions between the groups. P < 0.05 was considered to be statistically significant. The entire statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS version 20.0, IBM Corp., Armonk, NY, USA) for MS Windows.
Figure 2.
Flowchart for screening stroke patient data in pre- and poststroke code era
RESULTS
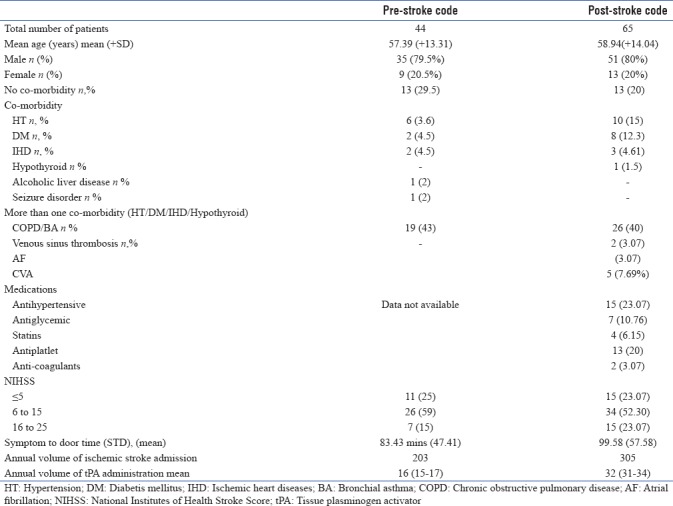
Figure 1 gives a breakup of the stroke patients presenting to the hospital during the two eras. The data of the patients thrombolyzed in the two eras (44 and 65 patients, respectively) were considered for the analysis. The mean age of patients treated pre- and post-SC was 57.39 (±13.31) and 58.94 (±12.54) years, respectively. Demographic variables and severity of stroke patients were comparable. The other baseline characteristics of patients treated pre- and post-SC are given in Table 1.
Table 1.
Baseline characteristics
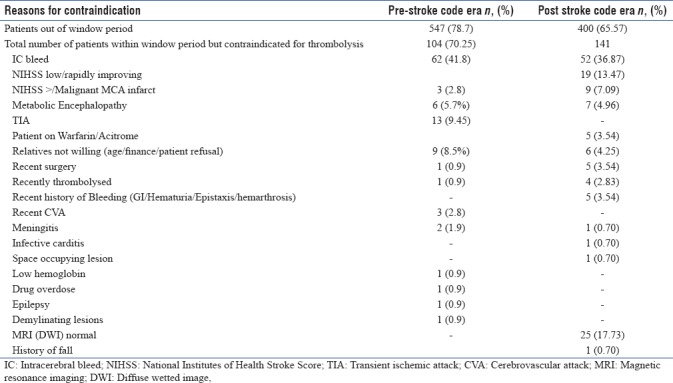
Among the patients contraindicated for thrombolysis, majority of them had intracerebral bleed 62 (41.8%) in pre-SC era and 52 (36.87%) in post-SC era. Twenty-five patients in SC era had come with symptoms of stroke, but their magnetic resonance imaging (MRI)–diffusion-weighted images (DWIs) were normal. The various reasons for contraindication for thrombolysis are depicted in Table 2.
Table 2.
Reasons for contraindications for thrombolysis
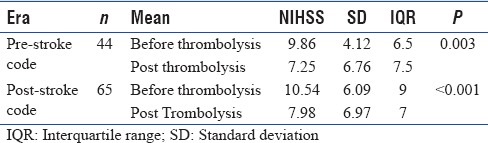
The mean NIHSS score in the pre-SC era before thrombolysis was 9. 86 (±4.12), while after thrombolysis, it reduced to 7.25 (±10.93). The change in mean NIHSS score posttreatment was not significantly different (P = 0.0003). The mean NIHSS score post-SC before treatment changed from 10.54 (±6.09) to 7.98 (±6.97) posttreatment. The change in mean NIHSS score posttreatment was statistically significant (P < 0.001). The mean NIHSS scores before and after thrombolyses in the two eras have been elucidated in Table 3. Postthrombolysis, there was significant improvement in NIHSS score in both the groups.
Table 3.
National Institutes of Health Stroke Scale change pre- and post-thrombolysis in the pre- and post-stroke code eras
The comparison of pre- and post-SC thrombolysis inhospital management timelines in terms of STD, DTP, DTI, and DTN time is given in Table 4. There was a significant reduction in DTI, DTP, and DTN time after implementation of SC (P < 0.001).
Table 4.
Comparison of pre and post-stroke code in-hospital timelines
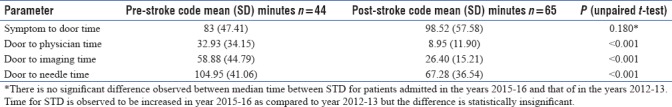
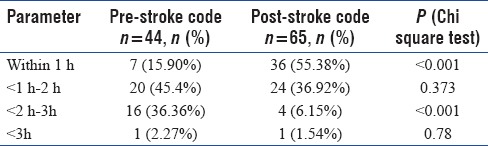
Table 5 gives a representation of the hour-wise distribution of the DTN times of the thrombolyzed patients in the two eras. The number of patients with “DTN time” ≤60 min significantly increased from 15.90% before SC implementation to 55.38% post-SC implementation which was significantly higher.
Table 5.
Hour-wise distribution of the door-to-needle time of thrombolysed patients in pre- and poststroke code era
In this study, while the STD time in post-SC era was higher than the pre-SC era by 16.58 min (±10.87), symptom-to-needle time was less by 24 min. This may be due to the improvement in DTN time in post-SC era. In the post-SC era, the patients presenting with STD time ≥60 min improvement in DTI time contributed more in reducing DTN time.
DISCUSSION
In resource-limited settings, the emergency evaluation and inability to determine eligibility for thrombolysis by the stroke team are the major inhospital delays in the management of stroke patients.[9,13] Patients presenting within 4.5 h of onset of symptoms are thrombolyzed with intravenous recombinant tissue plasminogen activator (IV tPA) treatment.[1] Therefore, timely arrival of patient and prompt treatment in this hospital is very critical. In pre-SC era, we thrombolyzed only 15.9% of acute ischemic stroke patients within 1 h of their arrival.[9] The reasons for suboptimal lysis rates for stroke in the pre-SC area could have been prehospital delay, i.e., onset to arrival time in the hospital extended beyond 4.5 h and inhospital delay in initiating treatment or both. Padma et al. had also reported similar causes for low rate of thrombolysis.[14] Given the potentially serious adverse effects of stroke, it is important to give high priority for these patients in emergency settings.[6] Having rapid response system is useful approach in reducing the time lag between patient arrival and initiation of treatment. Gomez et al. showed possibility of reducing inhospital treatment delay using rapid response system. They compared data of 12 patients treated with this approach versus 86 patients in the control group.[8] This study's population was higher compared to the Gomez et al. study, but the results were similar with significant differences being observed between the consultation intervals in the two groups.
Global guidelines for stroke recommend that DTI time should be <25 min and DTN time should be <1 h in at least 80% of the thrombolyzed patients as an important indicator of quality of stroke care.[12,15]
Similar to Olson et al., we had identified five domain which will help our rapid response team in improving DTN time.[16]
The five domains were as follows:
Stroke code protocol: Stroke protocol was drafted and made available in emergency department and also in all outpatient department units of hospital. Continuous training and education were imparted about SC throughout the hospital. This helped us to identify patients with symptoms of stroke at every level and increase the percentage of patients
Communication and teamwork: Multidisciplinary team was formed (emergency department, radiology department, medical resident/neurophysician, and intensivist). Each member identified themselves as part of a team. After initiation of SC, communication was maintained among team members during whole process till patient got thrombolyzed
Organizational/management culture: Communication with key people in administration department regarding the financial and logistic issue related to tPA and stroke treatment was undertaken. By doing so, more number of AIS patients who refused thrombolysis on financial ground or due to delay in official document preparations would be thrombolyzed. Staff and SC members were fully supported. Early thrombolysis was the goal
Performance monitoring and feedback: Initially stroke audit was conducted annually, but post-SC implementation, it is being conducted quarterly. This helped in terms of monitoring individual roles more effectively. The main reasons identified for delays in thrombolysis were availability of tPA, administrative issues, and time wasted in transportation. Hence, the tPA vial was made available in radiology, emergency, and stroke unit. Currently, the stroke patients are being thrombolyzed in imaging department rather than waiting for bed availability in stroke unit or transporting patient back in casualty
Appreciation of performance: At the same time, shortest DTN code was celebrated and members attending to the shortest code were appreciated in front of all departments.
Post-SC activation, the number and percentage of AIS patients receiving IV tPA increased from 44 (6.3%) to 65 (10.65%), from results. This is a significant decrease in the timeline of stroke thrombolysis which supports the importance of SC protocol.
Chen et al., in their study, experienced similar results after initiation of SC protocol.[17]
Thus few steps such as: Staff education (nurses, medicine resident, EMS personnel, Intensivist), dedicated SC number, prioritizing patient for imaging and keeping Stroke kit ready in emergency and radiology unit; helps to reduce the door to needle time (DTN). Elyar Sadeghi-Hokmabadi also had implemented these simple steps to reduce DTI time.[18]
The hospital's stroke protocol includes a rapid sequence MRI as a preferred imaging technique for acute stroke patients. The rapid sequence MRI protocol consists of localizer, DWI, swipe, and fluid-attenuated inversion recovery sequence. The MRI sequences for AIS patients were performed in 5 min. This MRI sequence was similar to the protocol used by Paolini et al.[19]
This study observed a previously described phenomenon called “Parkinson's law” which states that decisions will tend to take more time when physicians have more time. This phenomenon was observed in the relationship between faster STD time and slower DTN time.[20] In patients presenting with STD time <60 min, the DTI and DTN times were 10 min and 15 min more than the patients presenting late or ≥60 min [Table 3].
The rates of thrombolysis in AIS in India are very poor. This is mainly because of the prehospital delay.[14] A study conducted at All India Institute of Medical Sciences, New Delhi, a premier tertiary care institute of the country has reported inability to thrombolyze 38% otherwise eligible patients. This was due to delay in evaluation and treatment.[14] In this study, there was no significant difference in the prehospital delay after implementation of SC as indicated by two parameters, i.e., STD and symptom-to-needle time [Table 4]. In fact, the onset-to-door time was more in SC era. The shorter DTN time observed for SC era group compensated for longer STD time, i.e., there was an overall reduction in symptom-to-needle time by 24 min. There was only 12.6% reduction in symptom-to-needle time. Thus, more patients with longer prehospital delays may have received IV tPA due to SC protocol.[17] Patient safety was not compromised in these borderline patients. This was evidenced by less intracerebral bleed in these patients.
As described by Fonarow et al., the borderline association between SC timeline and good neurological outcome signifies the importance of earlier the better goal in AIS management.[21,22] Kim et al. also depicted that thrombolysis within the first 60 min after onset is associated with best outcome for patients with AIS.[22] Although there was immediate neurological improvement which was evident by decrease in NIHSS score, the 3-month mRS score would be a better measure of disability benefit. Unfortunately, this study's protocol did not include collection of mRS score and should be considered a major limitation of the study.
The significantly better short-term outcomes with thrombolysis in golden hour emphasize the importance of interventions to accelerate prehospital care.[22]
If the hospital has basic pre-requisites to give stroke care, then this simple cost effective protocolised “stroke code” approach, tailor made to Indian conditions will help to increase the rate of thrombolysis and reduction in timeline of thrombolysis of stroke.
This rapid response system can help to reduce inhospital treatment delay, but for prehospital delay, there is a need of having effective community-based stroke awareness programs. Both these activities should be done simultaneously.
A retrospective study design and a small number of patient population from single center are the main limitations of this study. Nevertheless, the results provide significant insights about importance and benefits of “SC” implementation. Based on these observations, we recommend larger studies in Indian population to confirm these findings.
CONCLUSION
Implementation of SC was significantly effective in increasing percentage of thrombolysis of AIS. Significant reduction in thrombolysis timelines such as “DTP time,” “DTI time,” and “DTN time” was observed after implementation of “SC.” Furthermore, we have observed benefits in NIHSS score in post-SC patients. Thus a tailor made guideline/step-by-step approach that suits indian conditions especially in areas with poor resources would be beneficial to the public at large. We strongly recommended that wherever feasible, hospitals should try and implement this simple, cost-effective practice to improve outcomes of acute stroke management. To overcome prehospital delay, we suggest that there is a need of having effective regular community-based stroke awareness programs along with better-coordinated emergency transport services.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to acknowledge the timely help and support provided by Dr. Rohit Kodagali in the various stages of manuscript preparation.
REFERENCES
- 1.Paramasivam S. Current trends in the management of acute ischemic stroke. Neurol India. 2015;63:665–72. doi: 10.4103/0028-3886.166547. [DOI] [PubMed] [Google Scholar]
- 2.Kalkonde YV, Deshmukh MD, Sahane V, Puthran J, Kakarmath S, Agavane V, et al. Stroke is the leading cause of death in rural Gadchiroli, India: A Prospective community-based study. Stroke. 2015;46:1764–8. doi: 10.1161/STROKEAHA.115.008918. [DOI] [PubMed] [Google Scholar]
- 3.Murthy JM. Thrombolysis for stroke in India: Miles to go. Neurol India. 2007;55:3–5. doi: 10.4103/0028-3886.30415. [DOI] [PubMed] [Google Scholar]
- 4.Pandian JD, Sudhan P. Stroke epidemiology and stroke care services in India. J Stroke. 2013;15:128–34. doi: 10.5853/jos.2013.15.3.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Truelsen T, Begg S, Mathers C. The Global Burden of Cerebrovascular Disease. [Last accessed on 2017 Aug]. Available from: http://www.WHO statistics:cerebrovascular disease stroke pdf .
- 6.Jin H, Zhu S, Wei JW, Wang J, Liu M, Wu Y, et al. Factors associated with prehospital delays in the presentation of acute stroke in Urban China. Stroke. 2012;43:362–70. doi: 10.1161/STROKEAHA.111.623512. [DOI] [PubMed] [Google Scholar]
- 7.Fonarow GC, Smith EE, Saver JL, Reeves MJ, Bhatt DL, Grau-Sepulveda MV, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: Patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123:750–8. doi: 10.1161/CIRCULATIONAHA.110.974675. [DOI] [PubMed] [Google Scholar]
- 8.Gomez CR, Malkoff MD, Sauer CM, Tulyapronchote R, Burch CM, Banet GA, et al. Code stroke. An attempt to shorten inhospital therapeutic delays. Stroke. 1994;25:1920–3. doi: 10.1161/01.str.25.10.1920. [DOI] [PubMed] [Google Scholar]
- 9.Gurav SK, Zirpe KG, Wadia RS, Pathak MK, Deshmukh AM, Sonawane RV, et al. Problems and limitations in thrombolysis of acute stroke patients at a tertiary care center. Indian J Crit Care Med. 2015;19:265–9. doi: 10.4103/0972-5229.156468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meretoja A, Kaste M. Pre- and in-hospital intersection of stroke care. Ann N Y Acad Sci. 2012;1268:145–51. doi: 10.1111/j.1749-6632.2012.06664.x. [DOI] [PubMed] [Google Scholar]
- 11.National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 12.Jauch EC, Saver JL, Adams HP, Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 13.Kamal N, Sheng S, Xian Y, Matsouaka R, Hill MD, Bhatt DL, et al. Delays in door-to-needle times and their impact on treatment time and outcomes in get with the guidelines-stroke. Stroke. 2017;48:946–54. doi: 10.1161/STROKEAHA.116.015712. [DOI] [PubMed] [Google Scholar]
- 14.Padma MV, Singh MB, Bhatia R, Srivastava A, Tripathi M, Shukla G, et al. Hyperacute thrombolysis with IV rtPA of acute ischemic stroke: Efficacy and safety profile of 54 patients at a tertiary referral center in a developing country. Neurol India. 2007;55:46–9. doi: 10.4103/0028-3886.30426. [DOI] [PubMed] [Google Scholar]
- 15.Ringelstein EB, Chamorro A, Kaste M, Langhorne P, Leys D, Lyrer P, et al. European stroke organisation recommendations to establish a stroke unit and stroke center. Stroke. 2013;44:828–40. doi: 10.1161/STROKEAHA.112.670430. [DOI] [PubMed] [Google Scholar]
- 16.Olson DM, Cox M, Constable M, Britz GW, Lin CB, Zimmer LO, et al. Development and initial testing of the stroke rapid-treatment readiness tool. J Neurosci Nurs. 2014;46:267–73. doi: 10.1097/JNN.0000000000000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen CH, Tang SC, Tsai LK, Hsieh MJ, Yeh SJ, Huang KY, et al. Stroke code improves intravenous thrombolysis administration in acute ischemic stroke. PLoS One. 2014;9:e104862. doi: 10.1371/journal.pone.0104862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sadeghi-Hokmabadi E, Taheraghdam A, Hashemilar M, Rikhtegar R, Mehrvar K, Mehrara M, et al. Simple in-hospital interventions to reduce door-to-CT time in acute stroke. Int J Vasc Med 2016. 2016 doi: 10.1155/2016/1656212. 1656212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paolini S, Burdine J, Verenes M, Webster J, Faber T, Graham CB, et al. Rapid short MRI sequence useful in eliminating stroke mimics among acute stroke patients considered for intravenous thrombolysis. J Neurol Disord. 2013;1:137. doi: 10.4172/2329-6895.1000137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sauser-Zachrison K, Shen E, Sangha N, Ajani Z, Neil WP, Gould MK, et al. Safe and effective implementation of telestroke in a US community hospital setting. Perm J. 2016;20:11–5. doi: 10.7812/TPP/15-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fonarow GC, Zhao X, Smith EE, Saver JL, Reeves MJ, Bhatt DL, et al. Door-to-needle times for tissue plasminogen activator administration and clinical outcomes in acute ischemic stroke before and after a quality improvement initiative. JAMA. 2014;311:1632–40. doi: 10.1001/jama.2014.3203. [DOI] [PubMed] [Google Scholar]
- 22.Kim JT, Fonarow GC, Smith EE, Reeves MJ, Navalkele DD, Grotta JC, et al. Treatment with tissue plasminogen activator in the golden hour and the shape of the 4.5-hour time-benefit curve in the national United States get with the guidelines-stroke population. Circulation. 2017;135:128–39. doi: 10.1161/CIRCULATIONAHA.116.023336. [DOI] [PubMed] [Google Scholar]


