Abstract
Background
Since Middle East respiratory syndrome (MERS) infection was first reported in 2012, many studies have analysed its transmissibility and severity. However, the methodology and results of these studies have varied, and there has been no systematic review of MERS. This study reviews the characteristics and associated risk factors of MERS.
Method
We searched international (PubMed, ScienceDirect, Cochrane) and Korean databases (DBpia, KISS) for English- or Korean-language articles using the terms “MERS” and “Middle East respiratory syndrome”. Only human studies with > 20 participants were analysed to exclude studies with low representation. Epidemiologic studies with information on transmissibility and severity of MERS as well as studies containing MERS risk factors were included.
Result
A total of 59 studies were included. Most studies from Saudi Arabia reported higher mortality (22–69.2%) than those from South Korea (20.4%). While the R0 value in Saudi Arabia was < 1 in all but one study, in South Korea, the R0 value was 2.5–8.09 in the early stage and decreased to < 1 in the later stage. The incubation period was 4.5–5.2 days in Saudi Arabia and 6–7.8 days in South Korea. Duration from onset was 4–10 days to confirmation, 2.9–5.3 days to hospitalization, 11–17 days to death, and 14–20 days to discharge. Older age and concomitant disease were the most common factors related to MERS infection, severity, and mortality.
Conclusion
The transmissibility and severity of MERS differed by outbreak region and patient characteristics. Further studies assessing the risk of MERS should consider these factors.
Keywords: MERS, Middle East respiratory syndrome, Infectivity, Severity, Mortality
Background
Middle East respiratory syndrome (MERS) was first reported in 2012 in Saudi Arabia [1]. Although most patients are linked to the Arabian Peninsula geographically, MERS has been detected in many other parts of the world [2]. A large MERS cluster was also observed in 2015 in South Korea [3].
MERS causes sporadic infection and intrafamilial and healthcare-associated infection. Its symptoms can vary from asymptomatic infection to death. Despite the infection’s association with high mortality, specified antiviral therapy is lacking, especially for patients with concomitant diseases [2].
Many previous studies have assessed the risks of MERS, such as factors dictating severity or an infection risk, yet the indices they present vary. For example, the case fatality rate was found to be 25.9% in the Middle East area, but 20.4% in South Korea [4]. The incubation period was reported to be 6.83–7 days in South Korea [4, 5], but 5.5 in a study using data from multiple areas [6] and 5.2 in Saudi Arabia [7]. Accurate assessment of the risk of MERS is essential for predicting and preventing infection.
A systematic review of the risk of MERS, as covered in previous studies, is potentially helpful for predicting this spread, and its future impact. This study aimed at reviewing the risk of MERS, focusing on indices related to infectivity and severity.
Methods
We searched international (PubMed, ScienceDirect, Cochrane) and Korean databases (DBpia, KISS) using the term “MERS” or “Middle East respiratory syndrome”, encompassing articles published after 2000. The search process was conducted in October 2017. We also manually searched the reference lists of the included studies.
Human studies were included, while animal studies and reviews were excluded. Only articles in English or Korean were included. Even if a study collected data on humans, such as collecting specimens from religious pilgrims, it was excluded if there were no MERS patients in the study sample. Additionally, case studies including fewer than 20 MERS patients were excluded as they were considered as having insufficient MERS patient numbers and representative information.
The included studies were classified as epidemiologic studies and those covering risk factors of MERS. In the epidemiologic category, indices related to the risk of MERS were divided into two categories; related to infectivity and related to severity. The index related to infectivity included the reproduction number (R), attack rate, incubation period, serial interval, and days from onset to confirmation. The index related to severity included the case fatality rate (CFR), days from onset to hospitalization, days from onset to discharge, days from onset to death, and days from hospitalization to death.
In the risk factor category, factors related to infection, transmission, severity, and mortality of MERS were analysed. Even if the included studies investigated factors that were related to mortality, when they did not analyse risk factors of severity or mortality using appropriate statistical methods (e.g., regression analysis, Cox proportional hazards model) or only compared prevalence factors, we excluded them from the risk factor category. In all categories, we extracted the study period, number of participants, and geographical region where the data were collected using a data extraction form confirmed after pilot assessment.
Results
A total of 3009 studies were searched, and 2717 were reviewed, excluding 292 duplicate studies. After the title and abstract review, a further 1804 and 663 were excluded, respectively. Another four studies were included via a manual search, which left a total of 58 studies for analysis (Fig. 1).
Fig. 1.
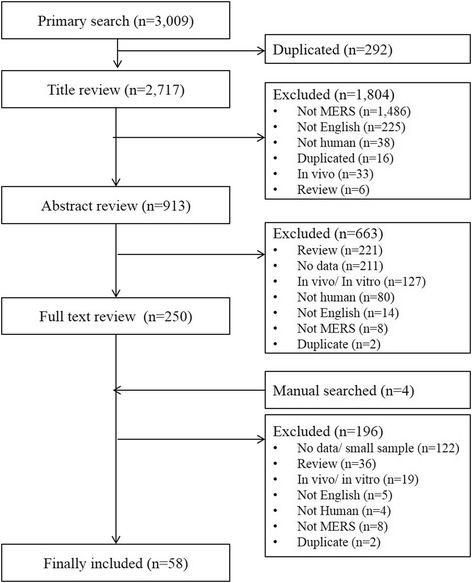
Flow of the systematic review in this study
Epidemiologic studies
The 38 of total 58 included studies were classified as epidemiologic studies (Table 1).
Table 1.
Epidemiologic studies of MERS, 2012–2017
| Author (year) | Country | Study period | No. of patients (M/F) Age of patients |
Fatality rate | Contact/ comorbidity | Index related to infectivity | Index related to severity |
| Ahmed (2017) [31] | Saudi Arabia | 2015–2017 | 537 (370/167) 55 ± 17.9 |
218/537 (40.6%) | • Comorbidity: 73.9% • Contacts - Hospital-acquired: 38.7% - Household: 9.9% - Camel: 25.3% - Unknown: 26.1% |
• Onset to confirmation: 4 days (IQR: 2–7 days) | |
| Alenazi (2017) [12] | Saudi Arabia | 2015 | 130 (66/64) 63.5 (community-acquired), 64.7 (healthcare-acquired), 40.1 (HCW) |
51/130 (39.2%) | • Contacts - Community-acquired: 20% - Healthcare-acquired: 46.9% - HCWs: 33.1% |
• R - Hospital-acquired: 0.98 for 2nd, 0.64 for 3rd, 0.23 for 4th generation |
|
| El- Bushra (2017) [21] | Saudi Arabia | 2015 | 87 n.r. |
n.r. | • Contacts - 20 primary, 39 first, 18 s, 7 third, 3 fourth generation |
• Secondary attack rate/10,000: 42 (95% CI: 33–54) | |
| Kim (2017) | South Korea | 2015 | 186 (111/75) 55 |
38/186 (19.9%) |
• Contacts - Hospital (99.4%) - Household (0.6%) - Community (0%) • Comorbidity - 29/38 fatalities had underlying disease |
||
| Park (2017) [23] | South Korea | 2015 | 25 (13/12) 71a (IQR: 38–86) |
25/11 (44.0%) | • Attack rate: 3.7% • Incubation period: 6.1 days |
||
| Sha (2017) [29] | Middle East area/ South Korea |
2012–2016 | 683 (423/260) 50–60 (fatal), 38–46 (non-fatal) |
182 (26.6%) (Middle East: 25.9%, South Korea: 13.8%) |
• Comorbidity - 67.9% in fatal, 22.2% in nonfatal cases |
• Incubation period - 4.5–5 days in Middle East area - 6 days in South Korea |
• Onset to confirmation - 8 days in fatal, 4 days in nonfatal in Middle East area - 4 days in fatal, 5 days nonfatal in South Korea • Onset to death - 11.5 days in Middle East area - 11 days in South Korea • Onset to discharge - 14 days in Middle East area - 17 days in South Korea |
| Sherbini (2017) [32] | Saudi Arabia | 2014 | 29 (20/9) 45 ± 12 |
10 (34%) | • Comorbidities - Diabetes (31%) - Chronic kidney disease (27%) |
• Symptoms to hospitalization: 2.9–5 days | |
| Assiri (2016) [36] | Saudi Arabia | 2014–2015 | 38 (28/10) 51 (range 17–84) |
21/38 (55.3%) | • Contacts - 13 HCWs - 15 were associated with 1 dialysis unit |
• Onset to death/discharge: 17 days (range 1.0–84.0) | |
| Cho (2016) [5] | South Korea | 2015 | 82 (53/29) 57 (patients and visitors), 38 (HCW) |
n.r. | • Contacts - Patients: 40.2% - Visitors: 50% - HCWs: 9.8% • Comorbidity - 24 (29%) had underlying disease |
• Incubation period: 7 days (range: 2–17, IQR: 5–10) • Overall attack rate - Patients in the emergency room: 4% (30/ 675) - Visitors: 6% (38/683) |
|
| Halim (2016) [33] | Saudi Arabia | 2016 | 32 (20/12) 43.99 ± 13.03 |
14/32 (43.8%) | • From symptom to hospitalization - 5.3 ± 3.3 days • Total length of stay - 15 ± 3.6 days |
||
| Liu (2016) | Taiwan | 2012–2015 | 1368 (883/476)a 49 (range: 2–90) |
35.6% (487/1368) • CFR 7.03% for HCW - 36.96% for non-HCW |
• Contacts - Patients: 46.2% - Family members or visitors: 34.9% - HCW: 18.9% |
• Onset to death - 13 (4–17) days for HCP - 12 (1–52) days for non-HCW • Onset to confirmation - 6 (1–14) days for HCP - 10 (1–21) days for non-HCW |
|
| Mohd (2016) [40] | Saudi Arabia | 2014–2015 | 80 (48/32) 40a |
• 10% (8/80) | • Comorbidity - Not different from non-MERS groups |
||
| Park (2016) [24] | South Korea | 2015 | 23 (13/10) 66a (range: 31–87) in hospital A; 74.5a (range: 60–82) in hospital B |
11/23 (47.8%) | • Generation - 23 in 2nd; 3 in 3rd |
• Incubation period - 7.8 days (95% CI: 6.0–10.0) • Serial interval - 14.6 days (95% CI, 12.9–16.5) • Secondary attack rate - 15.8% in hospital A - 14.3% in hospital B |
• Time to deathc - 12.5 days (IQR: 5.5–19) in hospital A - 11 days (IQR: 9–16) in hospital B |
| Virlogeux (2016) [25] | South Korea | 2015 | 170 (98/72) 54.6 ± 16.2 |
36/170 (21%) | Incubation period: 6.9 days (95% CI: 6.3–7.5) | ||
| Chowell (2015) [8] | Saudi Arabia, South Korea | 2013–2015 | 973 MERS and 7634 SARS cases n.r. |
n.r. | • Contacts - 43.5–100% were linked to healthcare setting in MERS |
R0 (95% CI) - MERS: 0.91 (0.36–1.44) - SARS: 0.95 (0.67–1.23) Infection rate of disease among HCWs: - MERS: 13.4–13.5% - SARS: 18.8–57.1% |
|
| Cowling (2015) [26] | South Korea | 2015 | 166 (101/65) 55.4 (range: 16–87) |
24/166 (14.5%) | • Contacts - 119 cases had contact with a confirmed case - 30/166 (18%) were healthcare personnel |
• Incubation period: 6.7 days • Serial interval: 12.6 days. |
|
| KCDC (2015) [4] | South Korea | 2015 | 186 (111/75) 55a (IQR: 42–66) |
36/186 (19.4%) | • Contacts - 44.1% patients exposed in hospitals - 32.8% caregivers - 13.4% HCWs • Comorbidities - 45.2% |
• Incubation period - 6.83 days (95% CI: 6.31,7.36) |
|
| Ki (2015) [3] | South Korea | 2015 | 186 (111/75) 50s in men and 60s in women |
36/186 (19.4%) | • Generation - 28 in 1st (15.1%); 125 in 2nd (67.2%); 32 in 3rd (17.2%); 2 were not certain • Contacts - Same hospital: 82 (44%) - Family/healthcare aides/visitors: 71 (38%) - HCWs: 31 (17%) • Comorbidities - 77 (41%) had underlying diseases |
• Incubation period: 6.5 days (2–16 days). | • From symptom onset to confirmation: 5 days (0–17 days) • From symptom onset to discharge from the hospital: 20 days (8–41 days). • From symptom onset to death: 13 days (1–41 days) |
| Ministry of Health, South Korea (2016) [27] | South Korea | 2015 | 186 (111/75) 50s (21.6%), 60s (19.9%) |
38/186 (20.4%) | • Generation - 28 in 2nd, 120 in 3rd, 26 in 4th, 11 in unclear/ unknown • Contacts - 82 patients in hospital - 63 family members/ visitors - 39 HCWs - 2 others |
• Incubation period - 6.83 days (95% CI: 6.31–7.36) |
|
| Noorwali (2015) [37] | Saudi Arabia | 2014 | 261 (171/90) n.r. |
110/261 (42%) | • Contacts - 84 HCWs - 177 non-HCWs |
||
| Park (2015) [28] | South Korea | 2015 | 37 (21/16) 51.7 (range: 24–79) |
6/37 (16.2%) | • Generation - 1 in 1st, 25 in 2nd, 11 in 3rd • Contacts - 20 patients - 12 relatives of patients - 3 HCWs - 1 unrelated visitors • Comorbidities - 5/6 in fatal, 3/31 in nonfatal |
Incubation period - 6 days (95% CI: 4–7 days) |
• Symptom onset to confirmation - 6.5 days (95% CI: 4–9) for all cases - 9 days for second cases - 4 days for third cases |
| Drosten (2014) [22] | Saudi Arabia | 2013 | 26 (17/9) 55a (range: 2–83) |
18/26 (69.2%) | • Contacts - 280 household contacts |
• Secondary transmission: 4% | |
| Assiri (2013) [7] | Saudi Arabia | 2012–2013 | 47 (36/11) n.r. |
28/47 (60%) | • Comorbidities - 45 had underlying comorbid medical disorders (96%) |
• Incubation period: 5.2 days | |
| Breban (2013) [9] | Multiple areas | 2012–2013 | 64 (44/17) b 56a (IQR 41–68.5) |
38/64 (59.4%) | n.r. | • R0: 0.69 (95% CI 0.50–0.92) | |
| Oboho (2012) [38] | Saudi Arabia | 2014 | 255 (174/81) 45a (IQR:30–59) |
93 (36.5%) | • Contacts - 40 of 191 symptomatic were HCWs (20.9%) |
n.r. | |
| Penttinen (2013) [41] | Multiple areas | 2012–2013 | 133 (51/77) b n.r. |
45% | • Contacts - 14 primary cases, 129 cases on transmission |
• Proportion to ICU: 60 cases (45%) |
|
| Estimating the index of infectivity and severity using secondary data | |||||||
| Author (year) | Country | Study period | Indexes related to infectivity | Index related to severity | |||
| Chang (2017) [18] | South Korea | 2015 | • R0 - 8.097 |
||||
| Choi (2017) [15] | South Korea, Saudi Arabia | 2015 | • R0 - 3.9 in South Korea - 1.9–3.9 in Saudi Arabia (1.9 in Riyadh, 3.9 in Jeddah) |
||||
| Eifan (2017) [13] | Saudi Arabia | 2013–2015 | • R - 0.85–0.97 |
||||
| Zhang (2017) [17] | South Korea | 2015 | • R - 2.5–7.2 |
||||
| Kim (2016) [16] | South Korea | 2015 | • R0 - 5.4 (95% CI: 4.61–6.19) in period 1 - 0.14 (95% CI: 0.04–0.26) in period 2 • Infectivity of hospitalized patients - 22 (95% CI: 18.73–25.27) in period 1 - 1 (95% CI: 0.16–1.84) in period 2 |
||||
| Lessler (2016) [39] | Saudi Arabia | 2012–2014 | • CFR: 22% (95% CI: 18, 25) | ||||
| Kucharski (2015) [10] | Multiple areas | 2012–2013 | • R0: 0.47 (95% CI: 0.29–0.80) | ||||
| Mizumoto (2015) [35] | South Korea | 2015 | • CFR: 20.0% (95% CI): 14.6, 26.2). | ||||
| Xia (2015) [19] | South Korea | 2015 | • R0 - 4.422 in early stage - 0.385 with control |
from hospitalization to death: 15.16 (0–42) (mean, range) | |||
| Cauche-mez (2014) [6] | Multiple areas | 2012–2013 | • Incubation period - 5.5 (95% CI: 3.6–10·2) • R0: 0.8–1.3 |
• CFR - 74% (95% CI: 49–91) for first cases - 21% (95% CI: 7–42) for second cases |
|||
| Chowell (2014) [11] | Saudi Arabia | 2013 | • R overall - 0.45 (95% CI: 0.29, 0.61) under the surveillance-bias scenario - 0.88 (95% CI: 0.58, 1.20) under the differential-transmissibility scenario |
||||
| Poletto (2014) [14] | Middle East area | 2012–2013 | • R: 0.50 (95% CI: 0.30–0.77) | ||||
CI confidence interval, ICU intensive care unit, IQR interquartile range, HCW healthcare worker, SARS severe acute respiratory syndrome
aMedian age, the others are mean age
bInformation of several participants was missing
cDefinition is not clear in this study
R value
R value, representing the reproduction number, indicates the average number of secondary cases generated by infectious individuals. Thirteen studies reported R value of MERS. Four studies that used data from multiple areas had R < 1.0 [6, 8–10]. Studies using Saudi Arabia or Middle East area data reported R < 1, at 0.45–0.98 [11–14], though one reported 1.9–3.9 [15]. Studies using South Korea data showed higher values, at 2.5–8.09 [16–19], in the early stage, and < 1 in the later period [20] or with control intervention [19].
Attack rate
A total of eight studies reported the attack rate. Four reported the overall or secondary attack rate, and the other four reported the attack rate of specific participant groups. Two studies conducted in Saudi Arabia showed 0.42% [21] and 4% [22] secondary attack rates. Studies in South Korea showed secondary attack rates of 3.7% in one study [23] and 14.3–15.8% in another [24].
Two studies reported the attack rate among healthcare workers (HCWs). One study in South Korea reported a MERS incidence of 1.5% among HCWs [20], and another study using multiple area data reported a 13.4–13.5% infection rate among HCWs [8]. The attack rate among hospital patients was 4% in one study [5] and 22% in the early and 1% in the later period in another [16].
Incubation period
The incubation period is the period between infection and appearance of signs of a disease. A total of 12 studies reported the incubation period of MERS. Nine used data from South Korea and showed a 6–7.8 day incubation period [3–5, 23–28]. One study using data from Saudi Arabia reported a 5.2 day incubation period [7], and another using data from multiple areas reported a 5.5 day incubation period [6]. Sha et al. compared the incubation periods between the Middle East area and South Korea and reported 4.5–5 and 6 days, respectively [29].
Serial interval
The serial interval of an infectious disease represents the duration between symptom onset of a primary case and of its secondary cases. Two studies used South Korea data, reporting serial intervals of MERS of 12.6 and 14.6 days, respectively [24, 26].
Days from onset to confirmation
Among five studies reporting days from onset to confirmation, three studies used data from South Korea. One study analysing all South Korea cases reported 5 days from onset to confirmation [3]. Park et al. reported 6.5 days for all cases, 9 for second generation and 4 for third generation [28]. One study from Taiwan reported 6 days for HCWs and 10 for non-HCWs [30]. A study from Saudi Arabia reported 4 days from onset to confirmation [31]. Sha et al. compared the data from Middle East and South Korea areas and reported 4–8 and 4–5 days, respectively [29].
Days from onset to hospitalization
Two studies from Saudi Arabia reported days from onset to hospitalization. One reported 2.9–5 days [32], and the other reported 5.3 days [33].
Mortality
Twenty-six studies reported on MERS-related mortality. Ten reported the mortality rate in South Korea as 14.5–47.8% [3, 4, 23–26, 28, 29, 34, 35]; one of which, including all MERS patients in South Korea, reported a mortality rate of 20.4% [27]. Ten studies analysing data from Saudi Arabia reported higher mortality rates, of 22–69.2% [7, 12, 22, 31–33, 36–39], although others reported mortality rates 10% [40] and 19.9% [21]. A Taiwanese study reported a mortality rate of 35.6% [30]. Studies using data from multiple areas reported mortality rates ranging from 26.6% [29] to 59.4% [9, 41].
Days from onset to discharge
Three studies reported days from MERS onset to discharge. Sha et al. reported 14 days in the Middle East area and 17 in South Korea [29]. One study from Saudi Arabia reported 17 days [36], and another in South Korea reported 20 [3].
Days from onset to death
Two Korean studies reported similar periods of 11–13 days from onset to death: 11–12.5 in Park et al. [24] and 13 in Ki et al. [3]. Although one study from Saudi Arabia reported longer than 17 days from onset to death [36], Sha et al., comparing data between the Middle East and South Korea, reported similar periods of 11.5 and 11 days, respectively [29]. One Taiwanese study also reported a similar period of 12–13 days [30].
Days from hospitalization to death
Two studies reported a similar length of hospitalization: 15 [33] and 15.2 days [19].
Risk factors related to mortality
Of the 20 studies included in the risk factor category, four were duplicates of studies in the epidemiologic category as they had information regarding the epidemiologic index and risk factors (Table 2).
Table 2.
Factors related to infection, transmission, severity, and mortality of MERS
| Author (year) | Study period | No. of participants (Total/death) |
Country | Predictors | Significant factors |
|---|---|---|---|---|---|
| Risk factors of infection | |||||
| Alraddadi (2016) [42] | 2014 | 146 (30 cases, 116 controls) | Saudi Arabia | Travel history, animal-related exposure, food exposure, underlying health conditions and behaviors | Direct dromedary exposure in 2 weeks, concomitant with diabetes or heart disease, currently smoking tobacco |
| Hastings (2016) [43] | 2014 | 78 | Saudi Arabia | Nationality, sex, age group, hospital setting, outbreak week | Older age, outbreak week, nationality |
| Risk factors of transmission (spreader) | |||||
| Kang (2017) [44] | 2015 | 186 | South Korea | Age, sex, comorbidity, symptoms, laboratory test, clinical outcome, phase in transmission, incubation period, symptom onset to isolation, non-isolated in-hospital days, symptom onset to diagnosis | Fever, chest X-ray abnormality in > 3 lung zones, more non-isolated in-hospital days |
| Kim (2017) [34] | 2015 | 186 | South Korea | Underlying respiratory disease, cycle threshold value, symptom onset to diagnosis, no. of contacts, hospitalization or emergency room before isolation | Lower cycle threshold value, hospitalization or emergency room visit before isolation |
| Majumder (2017) [45] | 2015 | 186 | South Korea | Sex, age, comorbidity, case class (HCW, visitor, patient), case outcome (recovered/deceased) | Deceased case outcome |
| Risk factors of severity | |||||
| Zhao (2017) [46] | 2014–2015 | 21 | Saudi Arabia | CD4 T cell, CD8 T cell, PRNT50 | Higher PRNT50, higher CD4 T cell response |
| Ko (2016) [48] | 2015 | 45 | South Korea | Demographics (age, sex, BMI, underlying disease), symptoms (fever, myalgia, cough, sputum, diarrhea), laboratory test (white blood cell, hemoglobin, thrombocytopenia, lymphopenia, albumin, bilirubin, aspartate transaminase, alanine transaminase, blood urea nitrogen, creatinine, C-reactive protein, lactate dehydrogenase, threshold cycle value of PCR) | • Pneumonia development: older age, fever, thrombocytopenia, lymphopenia, C-reactive protein ≥2 mg/dL, lower threshold cycle value of PCR < 28 • Respiratory failure: male, hypertension, low albumin concentration, thrombocytopenia, lymphopenia, C-reactive protein |
| Feikin (2015) [47] | 2014 | 102 | Saudi Arabia | Age, sex, underlying illness, week of specimen collection, MERS-CoV virus load | • Severity: older age, underlying illness, high MERS-CoV virus load • Mortality: older age, underlying illness, high MERS-CoV virus load |
| Saad (2014) [49] | 2012–2014 | 70 | Saudi Arabia | Age, gender, occupation, acquisition of infection, comorbidity, radiological findings, concomitant infections, laboratory abnormalities | • ICU care: concomitant infection, decreased albumin • Mortality: older age |
| Risk factors of mortality | |||||
| Adegboye (2017) [50] | 2012–2015 | 959/317 (33%) | Saudi Arabia | Sex, age, comorbidity, animal contact, camel contact, HCW, secondary contact, clinical experience | Older age, comorbidity, non-HCW, fatal clinical experience |
| Ahmed (2017) [51] | 2014–2016 | 660/197 (29.8%) | Saudi Arabia | Age, sex, nationality, symptomatic, HCW, severity, source of infection, regions | • 3-day mortality: older age, non-HCW, hospital-acquired infection • 30-day mortality: older age, non-HCW, pre-existing illness, severity, hospital-acquired infection |
| Sha (2017) [29] | 2012–2016 | 216/56 (25.9%) in Middle East area, 174/24 (13.8%) in South Korea | Middle East Area/South Korea | Age, sex, exposure to camel or other animals, comorbidity, disease progress (days) | Older age (Middle East, South Korea), high comorbidity (Middle East, South Korea), longer days from onset to confirmation of infection (Middle East), longer hospitalized days (Middle East) |
| Sherbini (2017) [32] | 2014 | 29/10 (34.5%) | Saudi Arabia | Sex, symptoms, history of chronic disease, duration of disease before hospitalization, vital signs, temperature, blood pressure | Older age, gastrointestinal symptoms, longer duration of symptoms prior to hospitalization, diabetes mellitus, chronic kidney disease, smokers, lower blood pressure |
| Nam (2017) [56] | 2015 | 25/11 (44%) | South Korea | - Epidemiologic (age, sex, hospital, inpatient, staying in the same room as the index case, smoking, preexisting pneumonia, chronic lung disease, incubation period) - Clinical symptom - Laboratory examinations |
Male, pre-existing pneumonia, smoking history, incubation period of less than 5 days, leukocytosis, abnormal renal function at diagnosis, respiratory symptoms. |
| Yang (2017) [52] | 2012–2016 | 1743/559 (32.1%) | Multiple area | Age, sex, comorbidity, epidemic period, contact pattern, country | Older age, comorbidity, epidemic later period |
| Almekhlafi (2016) [57] | 2012–2014 | 31/23 (74.2%) | Saudi Arabia | Age, comorbidity, initial manifestations, procedures (non-invasive ventilation, invasive ventilation, continuous renal replacement therapy), need for vasopressor | Need for vasopressors |
| Alsahafi (2016) [53] | 2012–2015 | 924/ 425 (46%) | Saudi Arabia | Age, sex, comorbidities, location of acquisition (household, inpatient, HCW) | Older age, cardiac disease, cancer, household patients, HCW |
| Virlogeux (2016) [25] | 2015 | 170/36 (21%) | South Korea | Age, sex, incubation period | Older age, shorter incubation period |
| Cha (2015) | 2015 | 30/5 (16.7%) | South Korea | Age, sex, chronic kidney disease, diabetes, hypertension, comorbidity, estimated glomerular filtration rate, mechanical ventilator | None |
| Majumder (2015) [54] | 2015 | 159/35 (22%) | South Korea | Five potential covariates were analyzed: sex, age, concurrent health condition status, health care worker status, time from onset to diagnosis | Older age, pre-existing concurrent health conditions |
| KCDC (2015) [4] | 2015 | 186/36 (19.4%) | South Korea | Sex, age, case classification, respiratory disease, diabetes, cardiac disease, chronic kidney disease, malignancy | Older age, underlying respiratory disease |
| Das (2015) [58] | 2014 | 55/19 (35%) | Saudi Arabia | Age, chest radiographic score, absolute lymphocyte count, no. of comorbidities, congestive heart failure, hypertension, diabetes | Chest radiographic score |
| Al Ghamdi (2016) [59] | 2014 | 51/19 (37%) | Saudi Arabia | Beta interferon, alpha interferon, hydrocortisone, Ribavirin, APACHE score | APACHE score |
| Choi (2016) [55] | 2016 | 186/33 (17.7%) | South Korea | Age, sex, HCW, coexisting medical condition, symptoms at admission, vital signs at admission, laboratory abnormalities at admission, treatment | Age ≥ 55 years, occurrence of dyspnea during the disease course, presence of concomitant medical conditions including diabetes or chronic lung disease, systolic blood pressure < 90 mmHg at admission, leukocytosis at admission, use of mechanical ventilation |
APACHE acute physiologic and chronic health evaluation, ICD intensive care unit, HCW healthcare worker, PCR polymerase chain reaction, PRNT plaque reduction neutralization test
Factors related to MERS infection
Two studies reported on the risk factors of MERS infection. Alraddadi et al. [42] analysed the effect of non-human contact, including travel history, animal-related exposure, food exposure, health condition, and behaviour and reported direct dromedary exposure, diabetes or heart disease, and smoking as risk factors of MERS infection. Another study reported older age, outbreak week, and nationality as risk factors [43].
Factors related to MERS transmission
Three studies analysed factors associated with spreaders. Non-isolated in-hospital days, hospitalization or emergency room visits before isolation, deceased patients, and clinical symptoms, including fever, chest X-ray abnormality in more than three lung zones, and the cycle threshold value, were related to spreaders [34, 44, 45].
Factors related to MERS severity
Four studies reported risk factors of MERS severity. The included studies showed that the PRNT50 and CD4 T cell response [46] as well as a high MERS virus load [47] were associated with the severity of MERS. Additionally, male sex; older age; concomitant disease, including hypertension; and symptoms, including fever, thrombocytopenia, lymphopenia, and low albumin concentration, were related to MERS severity or secondary disease [47–49].
Factors related to MERS mortality
Fifteen studies reported risk factors of mortality in MERS patients. Older age [4, 25, 32, 49–55] and comorbidity [29, 50–52, 54], including diabetes [32, 55], chronic kidney disease [32], respiratory disease [4, 55], pneumonia [56], cardiac disease, and cancer [53], were the most prevalent in the included studies. Male sex was reported as a risk factor in one study [56]. Smoking [32, 56] and location of acquisition [51, 53] were also reported. While one study noted that HCW, as a profession, was associated with mortality [53], non-HCWs were reported to be related to mortality in two other studies [50, 51].
Additionally, a shorter incubation period [25, 56], longer duration of symptoms [32], more days from onset to confirmation [29], later epidemic period [52], and longer hospitalized days [29] were reported as mortality risk factors.
Symptoms at diagnosis, including abnormal renal function [56], respiratory symptoms [56], gastrointestinal symptoms [32], lower blood pressure [32, 55], and leucocytosis [55, 56], were also found to be associated with mortality in MERS patients.
Severity of illness, [50, 51] such as need for vasopressors [57], chest radiographic score [58], health condition [59], use of mechanical ventilation [55], and occurrence of dyspnoea [55] were also found to increase the mortality risk.
Epidemiological index of MERS between the Middle East area and South Korea
The characteristics of MERS differ between South Korea and the Middle East area. The R value of MERS was reported to be below 1 in the Middle East area, except in one study [15], but was from 2.5–8.1 in South Korea [15–19]. Although studies using data from the Middle East area reported 0.42–4% secondary attack rates, studies in South Korea reported 4–6% secondary attack rates for patients or hospital visitors [5], and 3.7–15.8% for the overall attack rate [23, 24]. The MERS incubation period was reported to be 4.5–5.2 days in the Middle East area [7, 29], but this period was found to be slightly longer in South Korea [3–5, 23–28].
The severity of MERS also differed between the Middle East area and South Korea. Mortality of MERS patients was found to be 20.4% in South Korea based on a report including all cases [27], but most studies from Saudi Arabia reported higher rates, from 22 to 69.2% [7, 22, 33, 37–39]. Days from onset to confirmation were similar, 4–8 days in the Middle East area [29, 31] and 4–6.5 days in South Korea [3, 28, 29]. Days from onset to discharge were slightly longer in South Korea, 14–17 days in the Middle East area [29, 36] and 17–20 days in South Korea [3, 29] (Table 3).
Table 3.
Epidemiologic index of MERS between the Middle East area and South Korea
| Index | Saudi Arabia/Middle East area | South Korea (Study including all Korean cases) |
|---|---|---|
| Mortality | 22–69.2% (Two of ten studies reported lower mortality than 20%) |
14.5–47.8% (20.4%) |
| R-value | 0.45–0.98 (Only one study reported 1.9–3.9) |
• 2.5–8.1 • Less than 1 in later period or with control intervention |
| Attack rate | 0.42–4% | 3.7–15.8% |
| Incubation period | 4.5–5.2 days | 6–7.8 days (6.83 days) |
| Serial interval | – | 12.6–14.6 days |
| Days from onset to confirmation | 4–8 days | 4–6.5 days (5 days) |
| Days from onset to hospitalization | 2.9–5.3 days | – |
| Days from onset to discharge | 14–17 days | 17–20 days |
| Days from onset to death | 11.5–17 days | 11–13 days |
Discussion
The transmissibility and severity of MERS were different by outbreak countries, especially between the Middle East area and South Korea. The virus, host, and environmental factors may be the causes of the MERS outbreak-related differences between the two regions. From the standpoint of viral factors, there was a mutation of the MERS coronavirus (MERS-CoV) in the South Korea outbreak. Kim et al. [60] reported a point mutation in the receptor-binding domain of the viral spike protein in MERS-CoV, and another study showed that MERS-CoV in South Korea had higher genetic variability and mutation rates [61]. Individual characteristics can also affect MERS transmission. As previous studies showed, there is an association between older age and MERS infection [43], severity [48], and mortality [4, 50], and the population structure may be related to transmission and severity. Additionally, individuals aware of MERS were found to be more likely to practice preventive behaviour [62], which differed by demographic characteristics [63, 64]. The transmission environment may also contribute to the difference. While many MERS cases were contracted through exposure to camels in Saudi Arabia [42], the South Korea outbreak involved multiple generations of secondary infections caused by intra-hospital and hospital-to-hospital transmission [3, 65]. Strategies considering various factors are therefore needed to assess the impact of MERS and to better control its spread.
Although several studies have reported the overall R value [9, 10, 14, 19], others have shown that this value this can be variable based on the generation or a control intervention [11, 16, 19]. Especially in the South Korea epidemic, the R value was particularly high in the early stage or first generation, at 4.42–5.4, though it later decreased to 0.14–0.39 [16, 19]. Further studies should consider and analyse the variation of the R value depending on the period or control intervention.
While earlier studies on infectious diseases assumed a homogeneous infection ability of a population, recent studies have shown the existence of so-called super spreaders, individuals with a high potential to infect others in many infectious diseases, including Ebola and severe acute respiratory syndrome (SARS) [66]. The role of the super spreader is also important in the spread of MERS. In South Korea, 83.2% of MERS patients were associated with five super-spreading events [27]. Stein et al. [67] asserted that super spreaders were related with the host, pathogen, and environmental factors, and Wong et al. [66] reported that individual behaviours could also contribute to disease spread.
There are variations in the mortality and attack rates among studies using South Korea data. For example, Park et al. [24] reported a 47.8% MERS mortality, while reports from the Korean Ministry of Health and Welfare showed 20.4% MERS mortality. This disparity may, in part, be due to small sample sizes. Park et al. [24] included only 23 patients because the study was conducted in an early phase of a MERS outbreak. We excluded studies that included cases with < 20 subjects, which were mostly case series, to reduce those types of biases.
The present review found that older age and concomitant disease were risk factors of MERS infection and mortality. These results are consistent with a recent systematic review that reported older age, male, and an underlying medical condition as predictors of death related to MERS [68]; therefore, these factors should be prioritized in protection and treatment procedures.
One limitation of this study was the possibility of subject duplication. Especially in South Korea, the Korean government publishes MERS reports that include all patients. The epidemiologic index in other studies might be biased since they included partial Korean patients and were analysed in the middle of an outbreak. However, we included those studies because they showed the characteristics of MERS in different situations and different stages.
We did not conduct a meta-analysis because of the small number of studies for each index, which might be another limitation of this study. Although this study reviewed the risk factors of MERS and their impact, assessing the effect size of each risk factor is important. More studies investigating the effect of risk factors on MERS need to be constantly conducted.
Conclusion
Most studies on the transmissibility and severity of MERS have originated from Saudi Arabia and South Korea. Even though the R0 value in South Korea was higher than that in Saudi Arabia, mortality was higher in Saudi Arabia. The most common factors behind MERS infection and mortality were older age and concomitant disease. Future studies should consider the risk of MERS based on the outbreak region and patient characteristics. The results of the present study are valuable for informing further studies and health policy in preparation for MERS outbreaks.
Funding
This work was supported by the National Research Council of Science & Technology (NST) grant by the Korea government (MSIP) (No. CRC-16-01-KRICT) and Korea Institute of Oriental Medicine (G17273).
Abbreviations
- CD4
Cluster of differentiation 4
- CFR
Case fatality rate
- MERS
Middle East respiratory syndrome
- PRNT
Plaque reduction neutralization test
- SARS
Severe acute respiratory syndrome
Authors’ contributions
JEP (corresponding author) designed the study, and conducted the data search and the analysis with JEP (1st author). SYJ and ARK participated in the data review. JEP (corresponding) drafted the manuscript, and JEP (1st), SYJ, and ARK revised it. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ji-Eun Park, Email: janesky@kiom.re.kr.
Soyoung Jung, Email: syjung@kiom.re.kr.
Aeran Kim, Email: arkim@kiom.re.kr.
Ji-Eun Park, Phone: +82-42-868-9496, Email: jepark@kiom.re.kr.
References
- 1.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367(19):1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO MERS-CoV global summary and risk assessment. 2016. [Google Scholar]
- 3.Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015; 10.4178/epih/e2015033. [DOI] [PMC free article] [PubMed]
- 4.Korea Centers for Disease Control & Prevention Middle East respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect. 2015;6(4):269–278. doi: 10.1016/j.phrp.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH, et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016;388(10048):994–1001. doi: 10.1016/S0140-6736(16)30623-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cauchemez S, Fraser C, Van Kerkhove MD, Donnelly CA, Riley S, Rambaut A, et al. Middle East respiratory syndrome coronavirus: quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect Dis. 2014;14(1):50–56. doi: 10.1016/S1473-3099(13)70304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, Al-Rabiah FA, Al-Hajjar S, Al-Barrak A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13(9):752–761. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chowell G, Abdirizak F, Lee S, Lee J, Jung E, Nishiura H, et al. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015;13:210. doi: 10.1186/s12916-015-0450-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Breban R, Riou J, Fontanet A. Interhuman transmissibility of Middle East respiratory syndrome coronavirus: estimation of pandemic risk. Lancet. 2013;382(9893):694–699. doi: 10.1016/S0140-6736(13)61492-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kucharski AJ, Althaus CL. The role of superspreading in Middle East respiratory syndrome coronavirus (MERS-CoV) transmission. Euro Surveill. 2015;20(25):14–18. doi: 10.2807/1560-7917.ES2015.20.25.21167. [DOI] [PubMed] [Google Scholar]
- 11.Chowell G, Blumberg S, Simonsen L, Miller MA, Viboud C. Synthesizing data and models for the spread of MERS-CoV, 2013: key role of index cases and hospital transmission. Epidemics. 2014;9:40–51. doi: 10.1016/j.epidem.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alenazi TH, Al Arbash H, El-Saed A, Alshamrani MM, Baffoe-Bonnie H, Arabi YM, et al. Identified transmission dynamics of Middle East respiratory syndrome coronavirus infection during an outbreak: implications of an overcrowded emergency department. Clin Infect Dis. 2017;65(4):675–679. doi: 10.1093/cid/cix352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eifan SA, Nour I, Hanif A, Zamzam AMM, AlJohani SM. A pandemic risk assessment of Middle East respiratory syndrome coronavirus (MERS-CoV) in Saudi Arabia. Saudi J Biol Sci. 2017;24(7):1631–1638. doi: 10.1016/j.sjbs.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poletto C, Pelat C, Levy-Bruhl D, Yazdanpanah Y, Boelle PY, Colizza V. Assessment of the Middle East respiratory syndrome coronavirus (MERS-CoV) epidemic in the Middle East and risk of international spread using a novel maximum likelihood analysis approach. Euro Surveill. 2014;19(23) [DOI] [PubMed]
- 15.Choi S, Jung E, Choi BY, Hur YJ, Ki M. High reproduction number of Middle East respiratory syndrome coronavirus in nosocomial outbreaks: mathematical modelling in Saudi Arabia and South Korea. J Hosp Infect. 2017; 10.1016/j.jhin.2017.09.017. [DOI] [PMC free article] [PubMed]
- 16.Kim Y, Lee S, Chu C, Choe S, Hong S, Shin Y. The characteristics of middle eastern respiratory syndrome coronavirus transmission dynamics in South Korea. Osong Public Health Res Perspect. 2016;7(1):49–55. doi: 10.1016/j.phrp.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang XS, Pebody R, Charlett A, de Angelis D, Birrell P, Kang H, et al. Estimating and modelling the transmissibility of Middle East respiratory syndrome CoronaVirus during the 2015 outbreak in the Republic of Korea. Influenza Other Respir Viruses. 2017;11(5):434–444. doi: 10.1111/irv.12467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang HJ. Estimation of basic reproduction number of the Middle East respiratory syndrome coronavirus (MERS-CoV) during the outbreak in South Korea, 2015. Biomed Eng Online. 2017;16(1):79. doi: 10.1186/s12938-017-0370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xia ZQ, Zhang J, Xue YK, Sun GQ, Jin Z. Modeling the transmission of Middle East respirator syndrome corona virus in the Republic of Korea. PLoS One. 2015;10(12):e0144778. doi: 10.1371/journal.pone.0144778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim CJ, Choi WS, Jung Y, Kiem S, Seol HY, Woo HJ, et al. Surveillance of the Middle East respiratory syndrome (MERS) coronavirus (CoV) infection in healthcare workers after contact with confirmed MERS patients: incidence and risk factors of MERS-CoV seropositivity. Biomed Res Int. 2016;22(10):880–886. doi: 10.1016/j.cmi.2016.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El Bushra HE, Al Arbash HA, Mohammed M, Abdalla O, Abdallah MN, Al-Mayahi ZK, et al. Outcome of strict implementation of infection prevention control measures during an outbreak of Middle East respiratory syndrome. Am J Infect Control. 2017;45(5):502–507. doi: 10.1016/j.ajic.2016.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Drosten C, Meyer B, Muller MA, Corman VM, Al-Masri M, Hossain R, et al. Transmission of MERS-coronavirus in household contacts. N Engl J Med. 2014;371(9):828–835. doi: 10.1056/NEJMoa1405858. [DOI] [PubMed] [Google Scholar]
- 23.Park JW, Lee KJ, Lee KH, Lee SH, Cho JR, Mo JW, et al. Hospital outbreaks of Middle East respiratory syndrome, Daejeon, South Korea, 2015. Emerg Infect Dis. 2017;23(6):898–905. doi: 10.3201/eid2306.160120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park SH, Kim YS, Jung Y, Choi SY, Cho NH, Jeong HW, et al. Outbreaks of Middle East respiratory syndrome in two hospitals initiated by a single patient in Daejeon, South Korea. Infect Chemother. 2016;48(2):99–107. doi: 10.3947/ic.2016.48.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Virlogeux V, Park M, Wu JT, Cowling BJ. Association between severity of MERS-CoV infection and incubation period. Emerg Infect Dis. 2016;22(3):526–528. doi: 10.3201/eid2203.151437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cowling BJ, Park M, Fang VJ, Wu P, Leung GM, Wu JT. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill. 2015;20(25):7–13. doi: 10.2807/1560-7917.ES2015.20.25.21163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ministry of Health and Welfare, Republic of Korea . MERS white book. 2016. [Google Scholar]
- 28.Park HY, Lee EJ, Ryu YW, Kim Y, Kim H, Lee H, et al. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surveill. 2015;20(25):1–6. doi: 10.2807/1560-7917.ES2015.20.25.21169. [DOI] [PubMed] [Google Scholar]
- 29.Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44. doi: 10.1007/s00705-016-3062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu M, Jiang C, Donovan C, Wen Y, Sun W. Middle East respiratory syndrome and medical students: letter from China. Int J Environ Res Public Health. 2015;12(10):13289–13294. doi: 10.3390/ijerph121013289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ahmed AE. Diagnostic delays in 537 symptomatic cases of Middle East respiratory syndrome coronavirus infection in Saudi Arabia. Int J Infect Dis. 2017;62:47–51. doi: 10.1016/j.ijid.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sherbini N, Iskandrani A, Kharaba A, Khalid G, Abduljawad M, Al-Jahdali H. Middle East respiratory syndrome coronavirus in Al-Madinah City, Saudi Arabia: demographic, clinical and survival data. J Epidemiolo Glob Health. 2017;7(1):29–36. doi: 10.1016/j.jegh.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Halim AA, Alsayed B, Embarak S, Yaseen T, Dabbous S. Clinical characteristics and outcome of ICU admitted MERS corona virus infected patients. Egypt J Chest Dis Tuberc. 2016;65(1):81–87. doi: 10.1016/j.ejcdt.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim SW, Park JW, Jung HD, Yang JS, Park YS, Lee C, et al. Risk factors for transmission of Middle East respiratory syndrome coronavirus infection during the 2015 outbreak in South Korea. Clin Infect Dis. 2017;64(5):551–557. doi: 10.1093/cid/ciw768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mizumoto K, Saitoh M, Chowell G, Miyamatsu Y, Nishiura H. Estimating the risk of Middle East respiratory syndrome (MERS) death during the course of the outbreak in the Republic of Korea, 2015. Int J Infect Dis. 2015;39:7–9. doi: 10.1016/j.ijid.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Assiri A, Abedi GR, Bin Saeed AA, Abdalla MA, al-Masry M, Choudhry AJ, et al. Multifacility outbreak of Middle East respiratory syndrome in Taif, Saudi Arabia. Emerg Infect Dis. 2016;22(1):32–40. doi: 10.3201/eid2201.151370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Noorwali AA, Turkistani AM, Asiri SI, Trabulsi FA, Alwafi OM, Alzahrani SH, et al. Descriptive epidemiology and characteristics of confirmed cases of Middle East respiratory syndrome coronavirus infection in the Makkah Region of Saudi Arabia, March to June 2014. Ann Saudi Med. 2015;35(3):203–209. doi: 10.5144/0256-4947.2015.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oboho IK, Tomczyk SM, Al-Asmari AM, Banjar AA, Al-Mugti H, Aloraini MS, et al. 2014 MERS-CoV outbreak in Jeddah--a link to health care facilities. N Engl J Med. 2015;372(9):846–854. doi: 10.1056/NEJMoa1408636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lessler J, Salje H, Van Kerkhove MD, Ferguson NM, Cauchemez S, Rodriquez-Barraquer I, et al. Estimating the severity and subclinical burden of Middle East respiratory syndrome coronavirus infection in the Kingdom of Saudi Arabia. Am J Epidemiol. 2016;183(7):657–663. doi: 10.1093/aje/kwv452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mohd HA, Memish ZA, Alfaraj SH, McClish D, Altuwaijri T, Alanazi MS, et al. Predictors of MERS-CoV infection: a large case control study of patients presenting with ILI at a MERS-CoV referral hospital in Saudi Arabia. Travel Med Infect Dis. 2016;14(5):464–470. doi: 10.1016/j.tmaid.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Penttinen PM, Kaasik-Aaslav K, Friaux A, Donachie A, Sudre B, Amato-Gauci AJ, et al. Taking stock of the first 133 MERS coronavirus cases globally--is the epidemic changing? Euro Surveill. 2013;18(39) [DOI] [PubMed]
- 42.Alraddadi BM, Watson JT, Almarashi A, Abedi GR, Turkistani A, Sadran M, et al. Risk factors for primary Middle East respiratory syndrome coronavirus illness in humans, Saudi Arabia, 2014. Emerg Infect Dis. 2016;22(1):49–55. doi: 10.3201/eid2201.151340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hastings DL, Tokars JI, Abdel Aziz IZ, Alkhaldi KZ, Bensadek AT, Alraddadi BM, et al. Outbreak of Middle East respiratory syndrome at tertiary care hospital, Jeddah, Saudi Arabia, 2014. Emerg Infect Dis. 2016;22(5):794–801. doi: 10.3201/eid2205.151797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kang CK, Song KH, Choe PG, Park WB, Bang JH, Kim ES, et al. Clinical and epidemiologic characteristics of spreaders of Middle East respiratory syndrome coronavirus during the 2015 outbreak in Korea. J Korean Med Sci. 2017;32(5):744–749. doi: 10.3346/jkms.2017.32.5.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Majumder MS, Brownstein JS, Finkelstein SN, Larson RC, Bourouiba L. Nosocomial amplification of MERS-coronavirus in South Korea, 2015. Trans R Soc Trop Med Hyg. 2017;111(6):261–269. doi: 10.1093/trstmh/trx046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao J, Alshukairi AN, Baharoon SA, Ahmed WA, Bokhari AA, Nehdi AM, et al. Recovery from the Middle East respiratory syndrome is associated with antibody and T-cell responses. Sci Immunol. 2017;2(14). [DOI] [PMC free article] [PubMed]
- 47.Feikin DR, Alraddadi B, Qutub M, Shabouni O, Curns A, Oboho IK, et al. Association of higher MERS-CoV virus load with severe disease and death, Saudi Arabia, 2014. Emerg Infect Dis. 2015;21(11):2029–2035. doi: 10.3201/eid2111.150764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ko J-H, Park GE, Lee JY, Lee JY, Cho SY, Ha YE, et al. Predictive factors for pneumonia development and progression to respiratory failure in MERS-CoV infected patients. J Inf Secur. 2016;73(5):468–475. doi: 10.1016/j.jinf.2016.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saad M, Omrani AS, Baig K, Bahloul A, Elzein F, Matin MA, et al. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis. 2014;29:301–306. doi: 10.1016/j.ijid.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Adegboye OA, Gayawan E, Hanna F. Spatial modelling of contribution of individual level risk factors for mortality from Middle East respiratory syndrome coronavirus in the Arabian Peninsula. PLoS One. 2017;12(7):e0181215. doi: 10.1371/journal.pone.0181215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ahmed AE. The predictors of 3- and 30-day mortality in 660 MERS-CoV patients. BMC Infect Dis. 2017;17(1):615. doi: 10.1186/s12879-017-2712-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang YM, Hsu CY, Lai CC, Yen MF, Wikramaratna PS, Chen HH, et al. Impact of comorbidity on fatality rate of patients with Middle East respiratory syndrome. Sci Rep. 2017;7(1):11307. doi: 10.1038/s41598-017-10402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alsahafi AJ, Cheng AC. The epidemiology of Middle East respiratory syndrome coronavirus in the Kingdom of Saudi Arabia, 2012-2015. Int J Infect Dis. 2016;45:1–4. doi: 10.1016/j.ijid.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Majumder MS, Kluberg SA, Mekaru SR, Brownstein JS. Mortality risk factors for Middle East respiratory syndrome outbreak, South Korea, 2015. Emerg Infect Dis. 2015;21(11):2088–2090. doi: 10.3201/eid2111.151231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Choi WS, Kang CI, Kim Y, Choi JP, Joh JS, Shin HS, et al. Clinical presentation and outcomes of Middle East respiratory syndrome in the Republic of Korea. Infect Chemother. 2016;48(2):118–126. doi: 10.3947/ic.2016.48.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nam H-S, Park JW, Ki M, Yeon M-Y, Kim J, Kim SW. High fatality rates and associated factors in two hospital outbreaks of MERS in Daejeon, the Republic of Korea. Int J Infect Dis. 2017;58:37–42. doi: 10.1016/j.ijid.2017.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Almekhlafi GA, Albarrak MM, Mandourah Y, Hassan S, Alwan A, Abudayah A, et al. Presentation and outcome of Middle East respiratory syndrome in Saudi intensive care unit patients. Crit Care. 2016;20(1):123. doi: 10.1186/s13054-016-1303-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Das KM, Lee EY, Al Jawder SE, Enani MA, Singh R, Skakni L, et al. Acute Middle East respiratory syndrome coronavirus: temporal lung changes observed on the chest radiographs of 55 patients. AJR Am J Roentgenol. 2015;205(3):W267–W274. doi: 10.2214/AJR.15.14445. [DOI] [PubMed] [Google Scholar]
- 59.Al Ghamdi M, Alghamdi KM, Ghandoora Y, Alzahrani A, Salah F, Alsulami A, et al. Treatment outcomes for patients with Middle Eastern Respiratory Syndrome Coronavirus (MERS CoV) infection at a coronavirus referral center in the Kingdom of Saudi Arabia. BMC Infect Dis. 2016;16:174. doi: 10.1186/s12879-016-1492-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim Y, Cheon S, Min CK, Sohn KM, Kang YJ, Cha YJ, et al. Spread of mutant Middle East respiratory syndrome coronavirus with reduced affinity to human CD26 during the South Korean outbreak. MBio. 2016;7(2):e00019. doi: 10.1128/mBio.00019-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim DW, Kim YJ, Park SH, Yun MR, Yang JS, Kang HJ, et al. Variations in spike glycoprotein gene of MERS-CoV, South Korea, 2015. Emerg Infect Dis. 2016;22(1):100–104. doi: 10.3201/eid2201.151055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alqahtani AS, Wiley KE, Mushta SM, Yamazaki K, BinDhim NF, Heywood AE, et al. Association between Australian Hajj Pilgrims' awareness of MERS-CoV, and their compliance with preventive measures and exposure to camels. J Travel Med. 2016;23(5). 10.1093/jtm/taw046. [DOI] [PMC free article] [PubMed]
- 63.Choi J-S, Kim J-S. Factors influencing preventive behavior against Middle East respiratory syndrome-coronavirus among nursing students in South Korea. Nurse Educ Today. 2016;40:168–172. doi: 10.1016/j.nedt.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kim JS, Choi JS. Middle East respiratory syndrome-related knowledge, preventive behaviours and risk perception among nursing students during outbreak. J Clin Nurs. 2016;25(17–18):2542–2549. doi: 10.1111/jocn.13295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lee SS, Wong NS. Probable transmission chains of Middle East respiratory syndrome coronavirus and the multiple generations of secondary infection in South Korea. Int J Infect Dis. 2015;38:65–67. doi: 10.1016/j.ijid.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wong G, Liu W, Liu Y, Zhou B, Bi Y, Gao GF. MERS, SARS, and Ebola: the role of super-spreaders in infectious disease. Cell Host Microbe. 2015;18(4):398–401. doi: 10.1016/j.chom.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stein RA. Super-spreaders in infectious diseases. Int J Infect Dis. 2011;15(8):e510–e513. doi: 10.1016/j.ijid.2010.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Matsuyama R, Nishiura H, Kutsuna S, Hayakawa K, Ohmagari N. Clinical determinants of the severity of Middle East respiratory syndrome (MERS): a systematic review and meta-analysis. BMC Public Health. 2016;16(1):1203. doi: 10.1186/s12889-016-3881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


