Abstract.
To assess the knowledge, attitude, and preventive practices related to kala-azar in Madhepura district of Bihar, a community-based cross-sectional study was carried out in November 2014. A total of 353 households were interviewed from 24 villages of four blocks of Madhepura district. Data were collected using structured interview schedule. For knowledge, attitude, and preventive practice indexes, scores were assigned to individual questions based on the accuracy of responses. Univariate and binary logistic regressions were applied for the analysis. Eighty-four percent households had heard of kala-azar disease, but only 15.9% could recognize that sand flies were responsible for transmitting the disease. Overall, only 43.9% had fair knowledge on kala-azar disease (e.g., mode of transmission, signs and symptoms, and the outcome if left untreated) and the vector (breeding place, season, and biting time). Almost 48.6% had a favorable attitude toward treatability and management of kala-azar and 37.7% practiced proper mechanism to prevent and control kala-azar. Occupation emerged as a significant predictor for all three indexes. Other important predictors for the attitude index were literacy, household type, households ever had a kala-azar case, and knowledge index. Despite 61.8% of the households ever reported to have a member diagnosed with kala-azar, the overall knowledge of the disease and vector, attitude, and practices about prevention and control of kala-azar was found to be lagging. Therefore, our investigation suggests that further strengthening of comprehensive knowledge about kala-azar and preventive practices is needed.
INTRODUCTION
Visceral leishmaniasis, popularly known as kala-azar, is a systemic parasitic disease, caused by Leishmania donovani complex.1 Humans and domestic animals, mainly dogs, are the reservoirs of the parasite. The disease is characterized by irregular fever, substantial weight loss, enlargement of the spleen and liver, pancytopenia, anemia, leukopenia, bone marrow suppression, and immunosuppression, making a patient susceptible to super-added infections.2,3 The disease is a progressive and, sometimes, asymptomatic infection and if left untreated, is fatal,4 with a mortality rate of almost 100%.5
Kala-azar is considered as one of the major public health problems in 88 countries affecting approximately 350 million people.6 Globally, an estimated 1.3 million new cases occur every year with more than 50,000 deaths.7 Most of the affected countries are in the tropics and subtropics. The majority (90%) of the world’s kala-azar cases occur in India, Bangladesh, Nepal, Sudan, Brazil, and Ethiopia.8 India, Nepal, and Bangladesh alone harbor an estimated 67% of the global kala-azar disease burden.9 The governments of these countries aspired to eliminate kala-azar by 2015 (later extended to 2017 in India), by implementing multipronged approach to reduce the annual incidence of kala-azar to less than one case per 10,000 individuals.10
In India, kala-azar is transmitted by an infected female sand fly, Phlebotomus argentipes.11 This sand fly breeds in peridomestic environments having microclimatic conditions with high organic matter that serves as food for larvae.11 Endemic kala-azar is most prevalent in certain pockets of the eastern states of India, namely, Bihar, Jharkhand, Uttar Pradesh, and West Bengal. These states provide the aforesaid favorable climatic and environmental conditions for the progression of vector. However, 90% of the country’s burden of kala-azar is confined to the state of Bihar.12 In Bihar, 70% of kala-azar cases are spread across 10 districts, which are located in the floodplains of north Bihar. These districts are Muzaffarpur, Vaishali, Saharsa, Purnia, Araria, East Champaran, Saran, Sitamarhi, Samastipur, and Madhepura, in order of contribution.13
In 1990–1991, the Government of India launched a centrally sponsored program to control and eradicate kala-azar in endemic states. The efforts have recently been accelerated under the National Health Mission, which focuses on early case detection, complete case management, and vector control.10,14 Success and effectiveness of the prevention and control program of kala-azar mainly depends on the participation of the community. Therefore, the cooperation of the affected population is essential for the success of program activities. Hence, under the program, efforts have also been made to make the community aware of the disease, its features, diagnostic and treatment options, prevention, existing schemes, incentives, and other aspects.
As the government is keen on eliminating the disease, it becomes necessary to understand the extent of the awareness, preventive attitudes, and practices among the communities as these are important determinants for the success of the program. Little is known about the community’s knowledge and perception about the disease and its management in endemic15 areas such as Madhepura district. Madhepura has remained one of the endemic districts of Bihar and India for many decades15 and is also one of the poorest districts of eastern Bihar.16 This district, with 95.4% rural population, is located in the plains of the Kosi River and often affected by flood, famines, and drought.17 The present study aims to assess the knowledge, preventive attitudes, and practices of the community toward kala-azar in Madhepura district of Bihar.
METHODS
A cross-sectional study was carried out in Madhepura district of eastern Bihar in 2014. Annual record of kala-azar cases for every block (an administrative unit and district subdivision in a state) of the district was obtained from the office of Assistant Chief Medical Officer, Madhepura, for the years 2011, 2012, and 2013. As there was high fluctuation in the number of reported cases from year to year, four administrative blocks were randomly selected from the list of 13 blocks in the district. Furthermore, six villages were selected randomly from each block, which comprised 24 villages in total. Mapping and listing of the selected villages (3,627 households) was carried out to identify the households with suspected and confirmed kala-azar cases in previous 3 years. A total of 353 households were identified based on the abovementioned criteria and interviewed to assess the knowledge, practices, and preventive attitudes toward kala-azar. All the selected households participated in the study. Data were collected using a structured interview schedule. The respondent was the head or the knowledgeable person of the household who could provide information about the members of the household, housing conditions, economic status, and availability of basic amenities in the house. The respondent may or may not be the confirmed/suspected case of kala-azar. Data were entered and analyzed using SPSS 21 (IBM Corp., Armonk, NY). Descriptive statistics and binary logistic regression was applied to analyze the data.
Indexes of knowledge, preventive attitude, and practices (KAP) toward kala-azar and its prevention were computed. Knowledge index used 10 questions on kala-azar disease and its vector. Each correct response for an index of knowledge was given a score of 1 (Tables 2 and 3) and every wrong or “don’t know” response was scored 0. For attitude index, seven questions were used; each positive response was scored as 1 and “not sure” was given a score of 0.5 (Table 4) and negative/“don’t know” response was recoded with 0 score. Similarly, to assess the practice toward prevention of kala-azar, eight questions were incorporated and scores were assigned based on correct responses (Table 5). Levels of KAPs were then recategorized using their mean values as a cutoff score into two categories, that is, good/positive (score higher than mean) and poor/negative (score lower than mean).
Table 2.
Knowledge on kala-azar disease among the study participants in Madhepura district, Bihar, India, 2014 (percentage) (N = 296)
| Variables | Categories | Percentage | Frequency |
|---|---|---|---|
| Heard of kala-azar (N = 352) | Yes* | 84.1 | 296 |
| No | 15.9 | 56 | |
| Kala-azar as a communicable disease (N = 296) | Yes* | 22.0 | 65 |
| No | 51.0 | 151 | |
| Don’t know | 27.0 | 80 | |
| Mode of transmission† | Mosquito bites | 79.9 | 155 |
| Sand fly bites* | 18.6 | 36 | |
| Polluted water | 13.9 | 27 | |
| Other | 3.6 | 7 | |
| Don’t know | 34.5 | 102 | |
| Signs and symptoms†‡ | Fever for than 15 days | 92.8 | 192 |
| Loss of weight | 31.4 | 65 | |
| Enlargement of liver | 20.8 | 43 | |
| Enlargement of spleen | 4.3 | 9 | |
| Change of complexion | 9.2 | 19 | |
| Loss of appetite | 4.8 | 10 | |
| Pain in abdomen | 0.5 | 1 | |
| Don’t know | 30.1 | 89 | |
| Outcome if untreated | Death* | 98.0 | 290 |
| Other | 2.0 | 6 | |
| Groups most affected by kala-azar† | Poor* | 68.6 | 188 |
| Scheduled caste/tribe | 28.1 | 77 | |
| Women | 28.1 | 77 | |
| Children | 28.8 | 79 | |
| Agricultural laborers* | 13.9 | 38 | |
| Anyone | 15.0 | 41 | |
| Don’t know | 7.4 | 22 |
Other responses were scored 0.
Correct response and assigned score 1 in index.
Multiple responses.
Scores were assigned for single response and combination of responses: 0.5 for only fever, 0.5 for only weight loss, 0.5 for weight loss and loss of appetite, change in complexion was given a score of 1.0, other combinations were assigned 1.0 score, and “don’t know any symptom” was scored as 0.
Table 3.
Knowledge on various aspects of kala-azar vector among study participants in Madhepura district, Bihar, India, 2014 (percentage) (N = 296)
| Variables | Categories | Percentage | Frequency |
|---|---|---|---|
| Recognized vector | Yes* | 15.9 | 47 |
| No | 84.1 | 249 | |
| Season for kala-azar spread | Rainy season* | 22.7 | 67 |
| Winter* | 11.5 | 34 | |
| Summer | 36.5 | 108 | |
| Other | 5.0 | 15 | |
| Don’t know | 24.6 | 72 | |
| Biting time of vector | Dawn | 17.9 | 53 |
| Dusk | 4.1 | 12 | |
| Midnight* | 33.4 | 99 | |
| Daytime | 2.0 | 6 | |
| Any time | 6.1 | 18 | |
| Don’t know | 36.5 | 108 | |
| Breeding place†‡ | Polluted water | 64.4 | 112 |
| Garbage sites | 33.9 | 59 | |
| Dark places | 28.7 | 50 | |
| Cracks and crevice in the house | 12.1 | 21 | |
| Thatched roof | 11.5 | 20 | |
| Dense vegetation/shrubland | 2.3 | 8 | |
| Cattle sheds | 7.5 | 13 | |
| Humid places | 6.3 | 11 | |
| Don’t know | 41.2 | 122 | |
| Overall knowledge on kala-azar/vector | Good | 43.9 | 130 |
| Not good | 56.1 | 166 |
Other responses were scored 0.
Correct response was given score 1 in index.
Multiple responses.
0 score for no knowledge, 0.5 score for providing one to two places of breeding, and 1 score for three or more places of breeding.
Table 4.
Preventive attitudes toward kala-azar and its treatability among study participants in Madhepura district of Bihar, 2014 (percentage) (N = 296)
| Variables | Categories | Percentage | Frequency |
|---|---|---|---|
| Kala-azar to be kept as secret | Yes | 4.7 | 14 |
| No* | 92.2 | 273 | |
| Not sure† | 3.1 | 9 | |
| Seriousness of the disease as compared with malaria | More* | 57.8 | 171 |
| Equally* | 9.8 | 29 | |
| Less | 2.7 | 8 | |
| Can’t say | 29.7 | 88 | |
| Community participation to prevent kala-azar | Yes* | 24.0 | 71 |
| No | 30.7 | 91 | |
| Don’t know | 45.3 | 134 | |
| Preferred place of treatment | Public sector* | 84.1 | 249 |
| Private sector† | 15.5 | 46 | |
| Other | 0.4 | 1 | |
| Early diagnosis helps treatment of disease | Yes* | 80.7 | 239 |
| No | 8.1 | 24 | |
| Don’t know | 11.2 | 33 | |
| Complete cure of the disease | Yes* | 80.7 | 239 |
| No | 8.2 | 24 | |
| Don’t know | 11.1 | 33 | |
| Inconsistent treatment affects recovery | Yes* | 64.2 | 190 |
| Not sure† | 17.6 | 52 | |
| Don’t know | 18.2 | 54 | |
| Preventive attitude | Positive | 48.6 | 144 |
| Negative | 51.4 | 152 |
Other responses were scored 0.
Response was given a score of 1 in index.
Response was given a score of 0.5 in index.
Table 5.
Practices toward the control and prevention of kala-azar among study participants in Madhepura district of Bihar, 2014 (percentage) (N = 353)
| Variables | Categories | Percentage | Frequency |
|---|---|---|---|
| Prevention of sand flies*† | Use coil | 14.7 | 40 |
| Create smoke | 87.9 | 240 | |
| Mosquito net | 5.1 | 15 | |
| Others | 4.0 | 11 | |
| No | 7.4 | 22 | |
| Use of bed net | Don’t have bed net | 25.0 | 89 |
| Have, but don’t use | 2.5 | 9 | |
| Have, all members use‡ | 39.9 | 141 | |
| Have, some members use§ | 32.2 | 114 | |
| Sleep outdoors in | |||
| Rainy season | Yes | 3.4 | 12 |
| No‡ | 96.6 | 341 | |
| Winter season | Yes | 5.1 | 18 |
| No‡ | 94.9 | 335 | |
| Summer season‖ | Yes | 50.1 | 177 |
| No | 49.9 | 176 | |
| Inside house/premises | |||
| Bamboo plantation | Yes | 89.2 | 315 |
| No‡ | 10.8 | 38 | |
| Marshy land | Yes | 46.5 | 164 |
| No‡ | 53.6 | 189 | |
| Vegetation | Yes | 64.8 | 228 |
| No‡ | 35.2 | 124 | |
| Damp area | Yes | 51.0 | 180 |
| No‡ | 49.0 | 173 | |
| Practice | Good practice | 37.7 | 133 |
| Poor practice | 62.3 | 220 |
Other responses were scored 0.
Multiple responses.
Use of any preventive method has been given a score of 1 in index.
Response was given a score of 1 in index.
Response was given a score of 0.5 in index.
Not considered in index.
Ethical clearance for conducting the study was obtained from the Institutional Review Board of the International Institute for Population Sciences, Mumbai, India. A written informed consent was obtained from each participant of the study. Assurance of the confidentiality of the responses was provided to ensure that the information given by them in the study will not be used for any other purposes other than research.
RESULTS
Sociodemographic characteristics of participants.
Fifty-six percent of the participants were males (Table 1). The mean age of the participants was 41.7 years (standard deviation [SD] ± 17.1). The majority of the participants were Hindus (93.8%), 92.7% belonged to schedule caste/tribe or other backward caste. Half of the participants were working in the agricultural sector. Literacy rate among the study participants was 35.1%. Eighty-one percent households had a below poverty line (BPL), card and 65.4% were living in a house made up of temporary material (kaccha), 31.2% lived in houses constructed with combination of temporary and permanent materials (semi-pucca), and 3.4% had houses made up of permanent material (pucca). More than three-fifths of the households had at least one member, who had been diagnosed with kala-azar anytime in the past.
Table 1.
Sociodemographic characteristics of study participants in Madhepura district, Bihar, 2014 (N = 353)
| Characteristics | Categories | Percentage | Frequency |
|---|---|---|---|
| Sex | Male | 55.5 | 196 |
| Female | 44.5 | 157 | |
| Age | ≤ 29 | 27.2 | 98 |
| 30–40 | 28.2 | 100 | |
| 41–59 | 21.2 | 75 | |
| 60+ | 23.2 | 82 | |
| Religion | Hindu | 93.8 | 331 |
| Others | 6.2 | 22 | |
| Caste* | Scheduled caste/tribe | 29.2 | 103 |
| Other backward caste | 63.5 | 224 | |
| Others | 7.3 | 26 | |
| Literacy | Illiterate | 64.9 | 229 |
| Literate | 35.1 | 124 | |
| Occupation | Not working | 15.6 | 55 |
| Agriculture | 50.1 | 177 | |
| Nonagriculture | 34.3 | 121 | |
| Below poverty line card | Yes | 80.7 | 285 |
| No | 19.3 | 68 | |
| House type† | Kaccha | 65.4 | 231 |
| Semi-pucca | 31.2 | 110 | |
| Pucca | 3.4 | 12 | |
| Household ever had a case of kala-azar | Yes | 61.8 | 218 |
| No | 38.2 | 135 |
Kaccha refers to the house made of temporary materials, such as grass, straw, bamboo, mud, leaves, plastic, wood, and unburnt bricks; pucca house is made of permanent materials, such as wood, bricks, cement, metal, stone blocks, iron, metal sheet, tiles, or polyvinyl chloride material; and semi-pucca house is made of mix of temporary and permanent material.
The scheduled castes and scheduled tribes are officially designated groups of socially disadvantaged people in India and are recoded in the Constitution of India.
Classification is based on the material used to construct the floor, rood, and walls.
Knowledge about kala-azar and the vector.
The respondents were asked about their awareness on the vector-borne diseases and 52% reported being aware of one or more vector-borne diseases. Those who were aware about vector-borne diseases, namely, malaria (67.2%), kala-azar (66.7%), dengue fever (24.6%), and filaria (4.9%). Knowledge about kala-azar disease has been presented in Table 2.
Among all participants, 84.1% (296) had heard of kala-azar, 22% knew that the disease is infectious, and 98% said that the disease can be fatal if left untreated. Nearly 66% reported being aware of the mode of transmission of the disease; 18.6% reported that the disease could be transmitted through the bite of an infected sand fly and 79.9% mentioned mosquito bite. Nearly 70% knew one or more symptoms of kala-azar; 92.8% reported that fever for more than 15 days is the primary sign/symptom of kala-azar. Other reported symptoms were weight loss (31.4%), liver enlargement (20.8%), and change in complexion (9.2%). The respondents believed that the most of the affected people were poor (68.6%), children (28.8%), of schedule caste/schedule tribe (28.1%), women (28.1%), and agricultural laborers (13.9%).
From a total of 296 respondents who had heard of the disease, a few (15.9%) could recognize the picture of a sand fly (Table 3). One-fourth of them were not aware of the season in which kala-azar spreads; among those who were aware, 22.7% reported that the disease spreads during rainy season. About one-third of the participants knew that the sand fly bites at night whereas 36.5% were not aware of this fact. More than half were aware of one or more breeding places of kala-azar vector, such as stagnant/polluted water (64.4%), garbage sites (33.4%), dark places (28.7%), cracks and crevices (12.1%), and thatched roof (11.5%). The score for knowledge toward kala-azar disease and vector ranged from 0 to 10 with a mean of 4.5 (SD ± 1.3). According to the overall score, 43.9% had good knowledge of kala-azar disease and the vector. Those who were aware of kala-azar, knew about the disease and vector from health workers (42.9%) and friends/relatives (49%). Role of radio/television in spreading the awareness on kala-azar was limited to 4.7% of the participants and 8.8% reported to get awareness from newspaper/magazine.
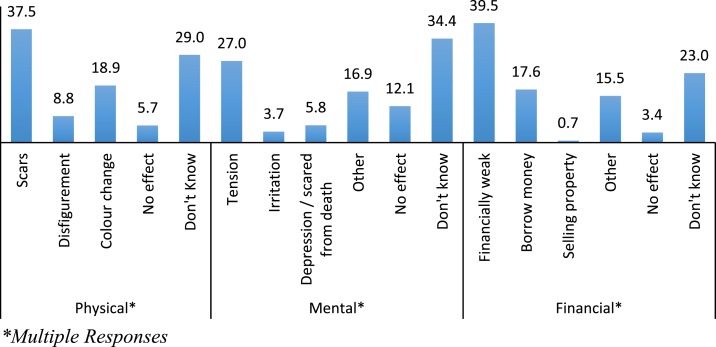
Regarding the effect of illness on the individual and the family, 65.2% asserted that kala-azar leaves marks on skin in the form of scars (37.5%), changes body color (18.9%), and leads to disfigurement (8.8%) (Figure 1). Forty-three percent also reported that the illness affects the mental health of the patient, causes stress (27%), irritation (3.7%), and depression/fear of death (5.8%). Nearly 74% opined that when a family member gets kala-azar, the household becomes financially weak (39.5%), forced to borrow money (17.6%), and sometimes even sell the property (0.7%).
Figure 1.
Knowledge on the aftereffects of kala-azar among study participants in Madhepura district of Bihar, 2014 (N = 296) (percentage). * Multiple Responses. This figure appears in color at www.ajtmh.org.
Preventive attitude toward kala-azar.
Seven questions (Table 4) were included to assess the preventive attitude people have toward kala-azar. The majority of the participants (92.2%) disagreed with the statement that the incidence of kala-azar in the family should be kept secret. Approximately 58% believed that kala-azar is a serious disease as compared with malaria whereas 9.8% opined both diseases are equally serious. Twenty-four percent participants were of the opinion that controlling kala-azar through community participation is possible.
Eighty-one percent believed that early diagnosis can cure the disease early and same proportion reported that complete cure of the disease is possible. The public health-care facilities were the most common choice of place for treatment (84.1%), followed by the private sector (15.5%). More than 60% believed that inconsistent or incomplete treatment of the disease could affect the recovery of the patient. The value of preventive attitude index ranged from 0.5 to 7 with a mean score of 5.1 (SD ± 1.2). In all, less than half of the respondents (48.6%) had a positive attitude toward the treatability of kala-azar disease.
Practice toward prevention and control of kala-azar.
The study found that the majority of the participants adopted some mechanisms to avoid the insect (vector) bite. For instance, 88% created smoke by burning dry leaves, waste, etc., 14.7% used mosquito coils, and 5.1% used a mosquito net. Three-quarters of the households possessed at least one mosquito net and all members of 39.9% households used the mosquito net while sleeping. The practice of sleeping outdoors during summer season was found among 50.7% participants. Ninety-two percent of the households had bamboo plantation in-and-around their dwellings and 49% lived near a marshy land. A “practice index” was constructed based on the eight indicators with a score ranging from 1 to 8 and an average of 4.8 (SD ± 1.3). The result of the overall “practice index” shows that 37.7% of households follow “good practice” for prevention and control of kala-azar (Table 5).
Determinants of KAP indexes.
The study also attempted to assess the effect of various background variables on the KAPs related to kala-azar (Table 6). Binary logistic regression analysis was carried out for all three indexes, namely, index of knowledge (model 1), index of preventive attitude (model 2), and index of practices (model 3) separately. The selected independent variables were age, sex, literacy, occupation, BPL cardholder status, household type and households with ever-had kala-azar case, and index of knowledge. Results suggest that participants working in agricultural (odds ratio [OR]: 3.772, confidence interval [CI]: 1.597–8.906) and nonagricultural sectors (OR: 4.023, CI: 1.670–9.681) were approximately four times more likely to have good knowledge toward kala-azar compared with nonworking participants. Similarly, literate participants (OR: 2.719, CI: 1.469–5.032), those living in better houses (semi-pucca/pucca) (OR: 2.556, CI: 1.450–4.505), working (agricultural [OR: 4.869, CI: 1.987–11.932] or nonagricultural sectors [OR: 2.699, CI: 1.085–6.709]), and those who possessed good knowledge about kala-azar (OR: 3.006, CI: 1.769–5.106), were more likely to have positive attitude toward prevention of kala-azar compared with their respective counterparts. The households with no history of kala-azar had less positive preventive attitude toward kala-azar (OR: 0.502, CI: 0.284–0.889) than households with a history of kala-azar. Besides, participants working in agricultural sector, living in kaccha houses, and aged 30–40 years were less likely to follow “good practices” to prevent kala-azar than their counterparts (Table 6).
Table 6.
Results of binary logistics regression (odds ratio [OR]) showing effects of background variables on indexes of knowledge, preventive attitude, and practices related to kala-azar in the Madhepura district, 2014
| Variables | Categories | Knowledge index | Preventive attitude index | Practices index | |||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Sex | Male* | – | – | – | – | – | – |
| Female | 0.928 | 0.541–1.592 | 1.430 | 0.796–2.571 | 0.776 | 0.448–1.343 | |
| Age group | ≤ 29* | – | – | – | – | – | – |
| 30–40 | 1.307 | 0.670–2.550 | 0.938 | 0.458–1.922 | 0.513 | 0.263–0.999 | |
| 41–59 | 1.461 | 0.717–2.977 | 1.113 | 0.518–2.393 | 0.554 | 0.273–1.124 | |
| 60+ | 1.564 | 0.743–3.296 | 1.475 | 0.658–3.306 | 0.550 | 0.262–1.153 | |
| Caste | SC/ST* | – | – | – | – | – | – |
| Non-SC/ST | 0.741 | 0.423–1.299 | 1.400 | 0.755–2.594 | 1.193 | 0.675–2.106 | |
| Literacy | Illiterate* | – | – | – | – | – | – |
| Literate | 1.697 | 0.970–2.969 | 2.719 | 1.469–5.032 | 1.089 | 0.614–1.930 | |
| Occupation | Not working* | – | – | – | – | – | – |
| Agriculture | 3.772 | 1.597–8.906 | 4.869 | 1.987–11.932 | 0.453 | 0.215–0.955 | |
| Nonagriculture | 4.023 | 1.670–9.681 | 2.699 | 1.085–6.709 | 0.662 | 0.309–1.419 | |
| Below poverty line card | Yes* | – | – | – | – | – | – |
| No | 1.170 | 0.627–2.184 | 0.982 | 0.502–1.922 | 0.845 | 0.448–1.591 | |
| House type | Kaccha* | – | – | – | – | – | – |
| Semi-pucca/pucca | 1.318 | 0.789–2.200 | 2.556 | 1.450–4.505 | 0.534 | 0.314–0.910 | |
| HH ever had a case of kala-azar | Yes* | – | – | – | – | – | – |
| No | 0.959 | 0.569–1.618 | 0.502 | 0.284–0.889 | 0.877 | 0.516–1.489 | |
| Knowledge index | Not good* | – | – | – | – | – | – |
| Good | – | – | 3.006 | 1.769–5.106 | 1.004 | 0.607–1.662 | |
| Constant | – | 0.172 | – | 0.071 | – | 2.227 | – |
CI = confidence interval; SC/ST = scheduled caste/scheduled tribe. Dependent variable: knowledge: not good (0) and good (1); preventive attitude: negative (0) and positive (1); practice: poor (0) and good (1).
Reference Category
DISCUSSION
Kala-azar remains one of the major public health problem in India, and its prevention and control is a priority.18 In recent years, the prevalence of kala-azar has reduced in other endemic states of India except Bihar. Awareness of the disease and correct knowledge to carry out appropriate practices toward the disease prevention and control emerged as important factors in the eradication of kala-azar. Hence, the article examined KAP related to kala-azar and its prevention in Madhepura district of Bihar.
In the study area, 84% of the participants had heard of kala-azar disease; this level of awareness was noted to be lesser than several studies conducted in India and the world.1,19–21 In addition, knowledge of the fact that kala-azar is a communicable disease and humans are one of the major reservoirs was recorded among 22% participants, which is again lower than other studies.19,22 The low awareness may be attributed to the low level of literacy (35%) and the high level of poverty (81% BPL cardholders) in the study population.
Only 19% study participants knew that sand fly is the cause of kala-azar transmission and very few could recognize the image of a sand fly. On the other hand, the majority of the participants (80%) said that mosquitos were responsible for the spread of kala-azar. Lack of correct knowledge toward the spread of disease is alarming as people at risk are unable to identify the vector, which further reduces the chances of protecting themselves from the bite of sand flies. Studies conducted in other high endemic areas also reflected similar results22–24 and proposed to enhance the level of awareness about kala-azar vector.24 Singh et al.,19 on the contrary, reflected that even if the community perceives mosquito as a vector of kala-azar, the preventive measures to be undertaken against the vector-borne diseases, including, kala-azar remain the same.
Awareness of signs and symptoms of a disease is a prerequisite for early treatment. However, in our study, 30% of the participants had no knowledge of signs/symptoms of kala-azar, although the disease has been endemic in the study area for many decades.13 In fact, the level of poor awareness about the sign and symptoms of kala-azar was much higher or similar to the findings of studies conducted in rural Bihar and other countries.1,21 Few other studies showed better knowledge of the symptoms in similar endemic areas.20,25 However, the knowledge that outcome of the untreated disease is death was found to be universal in our study. This might be due to repeated interactions of the community with the health personnel about kala-azar treatment and management and their own experiences.
Knowledge about the information on biting time and peak season of the spread of the disease is essential to avoid human–vector contact.19,21 In Madhepura (our study), this knowledge was found to be quite low. But in the case of studies conducted on malaria and dengue, the level of knowledge about the vector biting time, season, and breeding place was reported to be much higher in various communities.26,27 Overall comprehensive knowledge about kala-azar and the vector seemed to be very low in the community.
Our findings revealed the limited role of mass media on generating awareness about kala-azar. The study highlighted the important role played by relatives and friends and the efforts of the local health workers in spreading awareness of kala-azar. These findings were consistent with the results of a study on kala-azar conducted in the Muzaffarpur district, Bihar.21 On the other hand, the studies carried out on other vector-borne diseases, such as malaria and dengue, reflected the substantial role of mass media in awareness generation.28,29
Communities with diagnosed cases of kala-azar perceived the disease as more life-threatening than other vector-borne diseases, and the demand for treatment was high.30,31 In this study too, more than half of the participants believed that kala-azar is a much more serious disease than malaria. However, more than three-fourths reported that kala-azar is treatable and complete cure is also possible. Regarding treatment seeking behavior, most participants reported that they preferred accessing public health-care facilities for treatment. This could be due to the efforts of the local government authorities in sensitizing people about the treatability of the disease and availability of treatment options only at government facilities. Several studies have revealed that an incidence of vector-borne disease not only affects the physical and mental health of a patient but also has an impact on the family’s financial condition.25,32,33 Most of our study participants also gave similar opinions while talking about the aftereffects of kala-azar.
Kala-azar is also considered to be a poverty-related disease and affects the poorest of the poor.25,34,35 People living in remote rural areas with low nutrition, low education, and poor quality of housing are primarily affected by the disease.25,30 The findings from the present study concurs with this fact as most participants dwelled in poor living conditions (BPL cardholder and population living in kaccha houses). Most participants also opined that endemic kala-azar mainly affects the poor community and agreed that poverty and unhygienic conditions are responsible for the spread of disease. Apart from this, the presence of vegetation, water bodies, and pattern of settlements largely influence the sand fly population.18,36 Researchers have also found that the presence of shrubland/grassland37 and bamboo plantations34,38 near dwellings are likely to provide favorable breeding conditions for sand flies. Many of these factors were found in abundance in our study area in Madhepura district, making the population exposed to endemic kala-azar.
The effect of background characteristics on KAP indexes was also assessed. Occupation of the participants showed considerable positive influence on knowledge and attitude indexes. The finding that participants involved in agricultural activities had poor practices toward control/prevention of kala-azar indicates that the nature of work of the participants does not allow them to have good practice despite having good knowledge and favorable attitude. House type was positively associated with knowledge and preventive attitude index. As expected, good knowledge affected the attitude toward kala-azar.
Overall, the study found that in the study area, most participants had heard of kala-azar and were knowledgeable about certain aspects of disease treatment and management, especially the place of treatment, signs/symptoms, the seriousness of the disease, effect of untreated disease, curability of the disease, and impact on household economics and finances. Moreover, their knowledge on the communicable nature of the disease, vector, mode of transmission, time/season of bite, preventive measures, and role of the community in disease control was limited. In general, existing strategies adopted to eliminate kala-azar in endemic states of India aimed to foster behavioral change and communication activities to support efforts to eradicate the disease. However, our findings revealed that such strategic efforts may not be reaching the people in the affected areas effectively. The overall interventions to prevent and control the vector-borne disease indicate a wide gap among different eradication strategies. Lack of comprehensive knowledge about kala-azar needs to be addressed at the grass-root level and accompanied by preventive measures. Therefore, our study suggests further strengthening and rigorous implementation of knowledge-based strategies to increase the level of awareness about the disease, its vector and spread, and its transmission and prevention. This will ensure the community’s participation in the effective prevention and control of kala-azar.
Acknowledgments:
We express our earnest thanks to IIPS, Mumbai, for funding the study; the State Officials for granting permission to conduct the study and providing relevant information; and district officials for their support and cooperation in data collection. We are extremely grateful to our research staff for their assistance in collecting data for the study. The American Society of Tropical Medicine and Hygiene assisted with publication exepenses.
REFERENCES
- 1.Alemu A, Alemu A, Esmael N, Dessie Y, Hamdu K, Mathewos B, Birhan W, 2013. Knowledge, attitude and practices related to visceral leishmaniasis among residents in Addis Zemen town, south Gondar, northwest Ethiopia. BMC Public Health 13: 382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGwire BS, Satoskar AR, 2014. Leishmaniasis: clinical syndromes and treatment. QJM 107: 7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ready PD, 2014. Epidemiology of visceral leishmaniasis. Clin Epidemiol 3: 147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barrett MP, Croft SL, 2012. Management of trypanosomiasis and leishmaniasis. Br Med Bull 104: 175–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bogitsh BJ, Carter CE, Oeltmann TN, 2013. Blood and tissue protozoa I: hemoflagellates. Human Parasitology, 4th edition. Waltham, MA: Academic Press, 85–113. [Google Scholar]
- 6.Hossain M, Jamil KM, 2011. Geographical distribution of kala-azar in south Asia. Jha T, Noiri E, eds. Kala Azar in South Asia. Dordrecht, The Netherlands: Springer. [Google Scholar]
- 7.World Health Organization , 2014. Status of Vaccine Research and Development of Vaccines for leishmaniasis, Prepared for WHO PD-VAC Available at: http://www.who.int/immunization/research/meetings_workshops/Leishmaniasis_vaccineRD_Sept2014.pdf. Accessed March 16, 2016.
- 8.Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, Cano J, Jannin J, den Boer M; WHO Leishmaniasis Control Team , 2012. Leishmaniasis worldwide and global estimates of its incidence. PLoS One 7: e35671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hotez PJ, Remme JH, Buss P, Alleyne G, Morel C, Breman JG, 2004. Combating tropical infectious diseases: report of the disease control priorities in developing countries project. Clin Infect Dis 38: 871–878. [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Health and Family Welfare (MOHFW) , 2016. National Kala-Azar Elimination Program New Delhi, India: National Vector Borne Disease Control Program, Director General of Health Services. Available at: http://nvbdcp.gov.in/kal13.html. Accessed March 16, 2016.
- 11.Ministry of Health and Family Welfare (MOHFW) , 2016. Kala-Azar or Visceral leishmaniasis New Delhi, India: National Vector Borne Disease Control Program, Director General of Health Services. Available at: http://nvbdcp.gov.in/kala-azar.html. Accessed March 16, 2016.
- 12.Sunder S, More DK, Singh MK, Singh VP, Sharma S, Makharia A, Kumar PC, Murray HW, 2000. Failure of pentavalent antimony in visceral leishmaniasis in India: report from the center of the Indian epidemic. Clin Infect Dis 31: 1104–1107. [DOI] [PubMed] [Google Scholar]
- 13.Govil D, Sahoo H, Pedgaonkar S, Das KC, 2016. Magnitude of visceral leishmaniasis (kala-azar) in Bihar with insights from Madhepura district. Artha Vijnana LVIII: 339–348. [Google Scholar]
- 14.Ostyn B, et al. 2008. Vector control by insecticide-treated nets in the fight against visceral leishmaniasis in the Indian subcontinent, what is the evidence? Trop Med Int Health 13: 1073–1085. [DOI] [PubMed] [Google Scholar]
- 15.Govil D, Sahoo H, Pedgaonkar S, Das KC, 2016. Magnitude, Causes and Consequences of Kala-azar in India: A Study of Eastern Bihar. Unpublished report. Mumbai, India: International Institute for Population Sciences.
- 16.Ghosh PP, 2007. Poverty and Social Assessment: A District-Wise Study of Bihar Asian Development Research Institute, Patna, India. Monograph (02/2007). Available at: http://brlp.in/documents/11369/125465/Poverty+and+Social+Assessment+-+A++districtwise+study+of+Bihar.pdf/8a3c0c07-7021-45c8-8dbb-cb5d6190a9e3. Accessed March 16, 2016.
- 17.Directorate of Census Operations Bihar , 2014. District Census Handbook Madhepura: Village and Town Wise Primary Census Abstract (PCA), Series-11, Part Xii-B. Bihar, India: Census of India 2011.
- 18.Bhunia GS, Kesari S, Chatterjee N, Kumar V, Das P, 2012. Localization of kala-azar in the endemic region of Bihar, India based on land use/land cover assessment at different scales. Geospat Health 6: 177–193. [DOI] [PubMed] [Google Scholar]
- 19.Singh SP, Reddy DCS, Mishra RN, Sundar S, 2006. Knowledge, attitude, and practices related to kala-azar in a rural area of Bihar State, India. Am J Trop Med Hyg 75: 505–508. [PubMed] [Google Scholar]
- 20.Mondal D, Singh SP, Kumar N, Joshi A, Sundar S, Das P, Siddhivinayak H, Kroeger A, Boelaert M, 2009. Visceral leishmaniasis elimination programme in India, Bangladesh, and Nepal: reshaping the case finding/case management strategy. PLoS Negl Trop Dis 3: e355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siddiqui NA, Kumar N, Ranjan A, Pandey K, Das VNR, Verma RB, Das P, 2010. Awareness about kala-azar disease and related preventive attitudes and practices in a highly endemic rural area of India. Southeast Asian J Trop Med Public Health 41: 1–12. [PubMed] [Google Scholar]
- 22.Hassan MM, Banaga AO, Frah EA, Nour BYM, 2012. Assessment of knowledge, attitude and practice about sandfly and visceral leishmaniasis control activities in rural area of Gedarif state, Sudan. Al-Neelain Medical Journal 2: 4. [Google Scholar]
- 23.Pardo RH, Carvajal A, Ferro C, Davies CR, 2006. Effect of knowledge and economic status on sand fly control activities by householders at risk of cutaneous leishmaniasis in the subandean region of Huila department, Colombia. Biomedica 26 (Suppl 1): 167–179. [PubMed] [Google Scholar]
- 24.Sarkari B, Qasem A, Shafaf MR, 2014. Knowledge, attitude, and practices related to cutaneous leishmaniasis in an endemic focus of cutaneous leishmaniasis, southern Iran. Asian Pac J Trop Biomed 4: 566–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahluwalia IB, et al. 2003. Visceral leishmaniasis: consequences of a neglected disease in a Bangladeshi community. Am J Trop Med Hyg 69: 624–628. [PubMed] [Google Scholar]
- 26.Singh R, Musa J, Singh S, Ebere UV, 2014. Knowledge, attitude and practices on malaria among the rural communities in Aliero, northern Nigeria. J Family Med Prim Care 3: 39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dhawan G, Joseph N, Pekow PS, Rogers CA, Poudel KC, Bulzacchelli MT, 2014. Malaria-related knowledge and prevention practices in four neighbourhoods in and around Mumbai, India: a cross-sectional study. Malar J 13: 303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Isa A, Loke YK, Smith JR, Papageorgiou A, Hunter PR, 2013. Mediational effects of self-efficacy dimensions in the relationship between knowledge of dengue and dengue preventive behaviour with respect to control of dengue outbreaks: a structural equation model of a cross-sectional survey. PLoS Negl Trop Dis 7: e2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bowen HL, 2013. Impact of a mass media campaign on bed net use in Cameroon. Malar J 12: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boelaert M, Criel B, Leeuwenburg J, Van Damme W, Le Ray D, Van der Stuyft P, 2000. Visceral leishmaniasis control: a public health perspective. Trans R Soc Trop Med Hyg 94: 465–471. [DOI] [PubMed] [Google Scholar]
- 31.Mishra RN, Singh SP, Vanlerberghe V, Sundar S, Boelaert M, Lefèvre P, 2010. Lay perceptions of kala-azar, mosquitoes and bed nets in Bihar, India. Trop Med Int Health 15 (Suppl 2): 36–41. [DOI] [PubMed] [Google Scholar]
- 32.Rijal S, Koirala S, Van der Stuyft P, Boelaert M, 2006. The economic burden of visceral leishmaniasis for households in Nepal. Trans R Soc Trop Med Hyg 100: 838–841. [DOI] [PubMed] [Google Scholar]
- 33.Gopalan SS, Das A, 2009. Household economic impact of an emerging disease in terms of catastrophic out-of-pocket healthcare expenditure and loss of productivity: investigation of an outbreak of chikungunya in Orissa, India. J Vector Borne Dis 46: 57–64. [PubMed] [Google Scholar]
- 34.Hasker E, Singh SP, Malaviya P, Picado A, Gidwani K, Singh RP, Menten J, Boelaert M, Sundar S, 2012. Visceral leishmaniasis in rural Bihar, India. Emerg Infect Dis 18: 1662–1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boelaert M, Meheus F, Sanchez A, Singh SP, Vanlerberghe V, Picado A, Meessen B, Sundar S, 2009. The poorest of the poor: a poverty appraisal of households affected by visceral leishmaniasis in Bihar, India. Trop Med Int Health 14: 639–644. [DOI] [PubMed] [Google Scholar]
- 36.Sudhakara S, Srinivasb T, Palitc A, Karc SK, Battacharya SK, 2006. Mapping of risk prone areas of kala-azar (visceral leishmaniasis) in parts of Bihar state, India: an RS and GIS approach. J Vector Borne Dis 43: 115–122. [PubMed] [Google Scholar]
- 37.Schlein Y, Jacobson RL, 1999. Sugar meals and longevity of the sand fly Phlebotomus papatasi in an arid focus of Leishmania major in the Jordan Valley. Med Vet Entomol 13: 65–71. [DOI] [PubMed] [Google Scholar]
- 38.Poché D, Garlapati R, Ingenloff K, Remmers J, Poché R, 2011. Bionomics of phlebotomine sand flies from three villages in Bihar, India. J Vector Ecol 36 (Suppl 1): S106–S117. [DOI] [PubMed] [Google Scholar]