Abstract
Introduction
Chondrosarcoma is a malignant cartilage-forming bone tumour in which mutations in IDH1 and IDH2 frequently occur. Previous studies suggest an increased dependency on glutaminolysis in IDH1/2 mutant cells, which resulted in clinical trials with the drugs CB-839, metformin and chloroquine. In this study, the preclinical rationale for using these drugs as a treatment for chondrosarcoma was evaluated.
Methods
Expression of glutaminase was determined in 120 cartilage tumours by immunohistochemistry. Ten chondrosarcoma cell lines were treated with the metabolic compounds CB-849, metformin, phenformin (lipophilic analogue of metformin) and chloroquine.
Results
A difference in glutaminase expression levels between the different tumour grades (p = 0.001, one-way ANOVA) was identified, with the highest expression observed in high-grade chondrosarcomas. Treatment with CB-839, metformin, phenformin or chloroquine revealed that chondrosarcoma cell lines are sensitive to glutaminolysis inhibition. Metformin and phenformin decreased mTOR activity in chondrosarcoma cells, and metformin decreased LC3B-II levels, which is counteracted by chloroquine.
Conclusion
Targeting glutaminolysis with CB-839, metformin, phenformin or chloroquine is a potential therapeutic strategy for a subset of high-grade chondrosarcomas, irrespective of the presence or absence of an IDH1/2 mutation.
Subject terms: Bone cancer, Sarcoma
Introduction
Chondrosarcoma is the second most common primary bone malignancy in humans. It represents a heterogeneous collection of cartilage-forming tumours, which can be divided in several subtypes and histological grades.1 The most common subtype is conventional chondrosarcoma (85%), which arises centrally in the medulla of the bone. Conventional chondrosarcoma is histologically graded to determine treatment strategy and the patient’s prognosis. The atypical cartilaginous tumour (ACT, previously known as chondrosarcoma grade 1), accounts for 61% of cases. First-line treatment consists of curettage with local adjuvant treatment, resulting in a 5-year survival rate of 95%. Grade II (36%) and grade III (3%) chondrosarcomas have a worse 5-year survival of 86% and 58%, respectively, due to the occurrence of metastases.1–3 These tumours are treated with en bloc resection. Dedifferentiated chondrosarcoma is a highly malignant subtype with an overall survival rate of 7–24%.4 Mesenchymal chondrosarcoma has a 10-year survival rate between 44 and 54%.5,6 It is a rare aggressive subtype in which distant metastasis can be identified even after 20 years.5–7 Chondrosarcoma patients with inoperable disease, due to tumour location, tumour size or extensive metastatic disease benefit from a doxorubicin-based chemotherapeutic regimen, which increases the 3-year survival from 8 to 26%.8 As the overall efficacy of chemotherapy is limited, new treatment options are needed, which can be identified by further unravelling the essential driver genes and pathways of these tumours.
Potential driver mutations of central conventional and dedifferentiated chondrosarcoma are gain of function mutations in isocitrate dehydrogenase 1 and 2 (IDH1 and IDH2), which have been identified in 38–70% of the cases.9,10 Its occurrence in the benign precursors lesions (enchondromas), of which 52–87% harbour an IDH1/2 mutation,11,12 further demonstrates that IDH1/2 mutations are an early event in chondrosarcoma genesis. IDH1 and IDH2 are essential enzymes in cell metabolism, as they convert isocitrate to α-ketoglutarate (α-KG) in respectively the cytoplasm and the mitochondria. The mutant enzyme acquires the activity to convert α-KG to D-2-hydroxyglutarate (D-2-HG), an oncometabolite that competitively inhibits the α-KG dependent enzymes by the high structural similarities.13 Processes involved in chondrosarcoma progression make these cells independent of the mutant IDH enzymes, as treatment with AGI-5198, a specific IDH1 mutant inhibitor, did not influence the tumourigenic properties of these cells.14 Therefore, we propose to exploit the metabolic vulnerability caused by the IDH1/2 mutations as therapeutic strategy for chondrosarcoma.
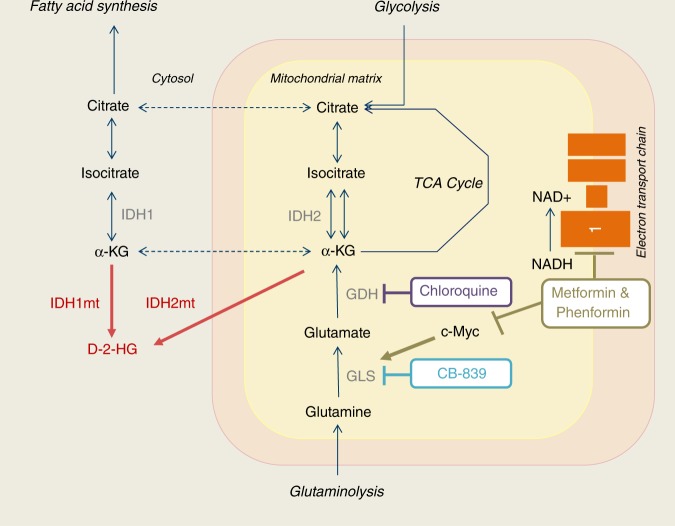
IDH1/2 mutant cells need α-KG for the production of D-2-HG, which can be generated via glycolysis and glutaminolysis. It has been suggested that IDH1/2 mutated tumours depend on glutaminolysis for their α-KG supply,15–17 which led to two clinical trials that were recently started in IDH1/2 mutated solid tumours, including chondrosarcomas. The first one is a phase I trial with the drug CB-839 (NCT02071862 clinicaltrials.gov), an inhibitor of glutaminase (Fig. 1). The second one is a phase IB/II trial with the drugs metformin and chloroquine (NCT02496741 clinicaltrails.gov), after which the feasibility of phenformin may be explored as an alternative to metformin in case of lack of effect of metformin.18 Metformin is a first-in-line drug used for the treatment of type II diabetes mellitus that inhibits gluconeogenesis in the liver. It has several effects on cellular proteins, among which it (1) activates adenosine monophosphate activated protein kinase (AMPK), thereby inhibiting the mammalian target of rapamycin (mTOR);19 (2) inhibits complex 1 of the electron transport chain;20 and (3) indirectly inhibits glutaminase, the enzyme that converts glutamine to glutamate, via c-Myc; (Fig. 1).21,22 Phenformin is a lipophilic analogue of metformin with similar working mechanisms, but in contrast to metformin it does not depend on solute carrier (SLC) 22A1-3 transport to get into cells;20,23 The anti-malaria drug chloroquine, in addition to its well-known anti-autophagy potency, is able to inhibit glutamate dehydrogenase, an enzyme converting glutamate to α-KG (Fig. 1).24,25
Fig. 1.
Schematic representation of glutamine metabolism and the compounds used in this study. IDH isocitrate dehydrogenase, IDHmt mutated IDH, D-2-HG D-2-hydroxyglutarate, α-KG α-ketoglutarate, GLS glutaminase, GDH glutamate dehydrogenase, NAD nicotinamide adenine dinucleotide, TCA tricarboxylic acid
In this study, we evaluate whether there is preclinical rationale to target glutaminolysis as a treatment for chondrosarcoma by determining the expression levels of glutaminase in chondrosarcoma primary tumours and by evaluating the effect of metformin, phenformin, chloroquine and CB-839 on chondrosarcoma cells.
MaterialS and methods
Immunohistochemistry on tissue microarrays
Glutaminase monoclonal antibody (AB156776, Abcam) (1:400) was used for immunohistochemical stainings on previously generated and published formalin-fixed, paraffin-embedded tissue microarrays26 as described.27 Hundred and twenty cartilage tumours could be scored, consisting of 12 benign (enchondromas or osteochondromas), 56 ACTs, 36 grade II and 16 grade III tumours. Two independently operating observers used the following scoring procedure: intensity score (0 negative, 1 weak, 2 moderate, 3 strong) + percentage score (0 = 0%, 1 = 1–24%, 2 = 25–49%, 3 = 50–74% and 4 = 75–100%). Discrepancies were discussed to reach consensus. Of the central cartilage lesions that could be scored, the IDH mutation status was known of 54 tumours, of which 33 harboured an IDH1 or IDH2 mutation and 21 were wildtype.
Statistical analysis
Statistical analysis on immunohistochemistry data was performed using Statistical Package for the Social Sciences 23 (SPSS Statistics, IBM). One-way ANOVA with the Fisher’s least significant difference (LSD) post-hoc analysis was used to compare glutaminase expression levels between different tumour grades. The difference in glutaminase protein expression between high-grade cartilage tumours (grade II and grade III cartilage tumours) and low-grade cartilage tumours (enchondromas, osteochondromas and ACT) was determined using independent-samples T test. Results were considered significant at the α = 0.05 level.
Cell culture
Five IDH1 or IDH2 mutated (JJ012,28 SW1353 (ATCC #HTB-94), L2975,29 L83529 and HT108030) and five IDH1/2 wildtype (CH2879,31 MCS170,32 CH3573,33 NDCS134 and L3252b29) chondrosarcoma cell lines were analysed. Five of these originate from conventional chondrosarcoma (JJ012, SW1353, L835, CH2879 and CH3573), three from dedifferentiated chondrosarcoma (L2975, NDCS1 and L3252b) and one from mesenchymal chondrosarcoma (MCS170). HT1080 was originally reported as a fibrosarcoma of bone. As this is a diagnosis of exclusion and this cell line is now known to harbour an IDH1 mutation, this tumour most probably reflects a dedifferentiated chondrosarcoma.14 Cells were cultured at 5% CO2 and 37 °C in a humidified incubator using RPMI 1640 (Gibco) with 10% (JJ012, SW1353, L2975, HT1080, CH2879 and NDCS1) or 20% (L835, CH3573 and L3252b) heat inactivated foetal bovine serum (FBS) (F7524, Sigma Aldrich). MCS170 was cultured in IMDM (Gibco) with 15% FBS. The authenticity of the cells was confirmed by STR profiling with the GenePrint10 (Promega Benelux BV) and cells were tested for mycoplasma using MycoAlert (Lonza, Switzerland) before the start of the experiments. Cell lines were never cultured for more than three months, and were tested for mycoplasma every 4 weeks (using RT-PCR).
qRT-PCR
RNA isolation of chondrosarcoma cells and the anonymised controls (growth plate and articular cartilage) was performed using TRIzol (Ambion biosystems, Invitrogen) followed by a standard RNA isolation protocol and cDNA synthesis.35 Product size and sequence were validated using Qiaxcel (Qiagen) and Sanger sequencing (Applied Biosystems 48- or 96-cappilary 3730 system, Leiden genome technology centre), respectively. Standard qRT-PCR analyses were performed as described previously36 to determine glutaminase, SLC22A1, SLC22A2 and SLC22A3 expression levels. GPR108, CYPa and CPSF6 were used as housekeeping genes for normalisation.37,38 Data were normalised using the delta-delta Cq method using Bio-Rad CFX Manager (Bio-Rad).
Cell viability assay
Cells were counted with the Muse Cell Analyzer (Millipore BV) using the Muse calibration kit (Millipore BV) according to manufacturer’s instruction. Plating was done in densities optimised for each cell line and condition i.e., 3000–15,000 cells per well for 72 h, 200–400 cells per well for one week incubation in triplicates. CB-839 (s7655, Selleckchem), metformin hydrochloride (215169110, Bioconnect), phenformin hydrochloride (219590, Santa Cruz Biotechnology) and chloroquine diphosphate salt (c6628, Sigma Aldrich) were added after the cells adhered overnight. The metabolic drugs were incubated for 72 h or 1 week after which cell viability was measured using the PrestoBlue Cell Viability Reagent (Promega Benelux BV) according to the manufacturer’s instructions. Colourimetric values in the plates were subsequently measured using a Wallac 1420 VICTOR2 (Perkin Elmer). Data were analysed in Graphpad Prism 5.0 (www.graphpad.com). For the combination of metformin, phenformin and chloroquine with AGI-5198 (14624, Life technologies), cells were pretreated for 72 h with AGI-5198 (1 and 10 µM) or DMSO. For the analyses in which the effect of FBS on CB-839 sensitivity was evaluated, the medium with or without FBS and the corresponding concentrations of the metabolic compounds were added at the same time, so after the cells were allowed to adhere overnight.
Cell count assay
As the PrestoBlue assay measures mitochondrial activity, we confirmed that the effects of metformin, phenformin and chloroquine on cell viability were caused by an absolute decrease in cell number by fixing the cells in 4% paraformaldehyde for 15 min, followed by nuclear staining using Hoechst 33342 (Fischer Scientific). The plates were imaged using a BD Pathway 855 imager (Becton Dickinson), after which the images were processed using an Image-Pro Analyser 7.0 algorithm. Hoechst area was used as a read out to quantify the amount of cells in each well.
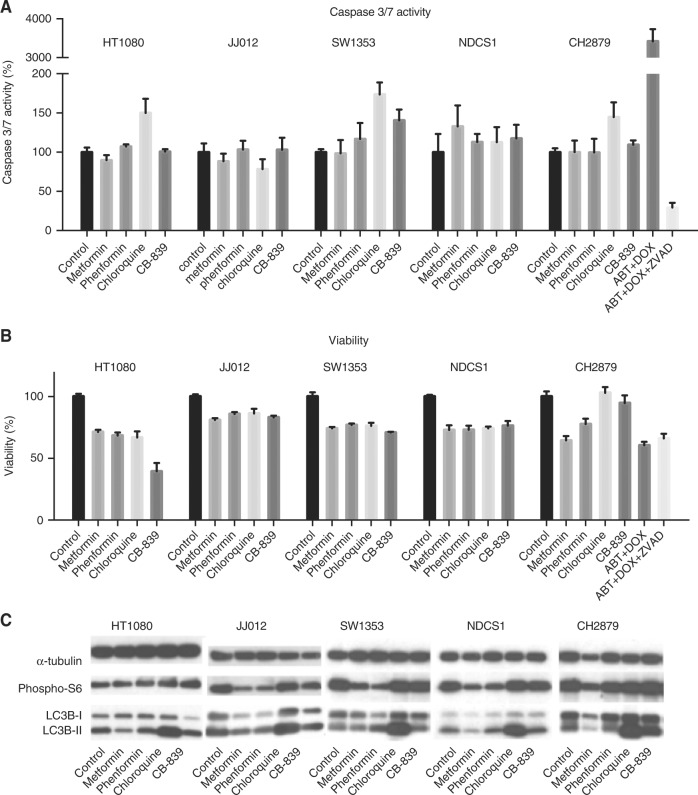
Analysis of apoptosis
For analysis of apoptosis, the caspase-glo 3/7 assay (Promega) was used according to manufacturer’s instructions. Cells were seeded in white walled 96-wells plates (Corning BV Life Sciences) in densities which resulted in 70% confluence after 24 h as described previously.39 HT1080, JJ012, SW1353, NDCS1 and CH2879 cells were treated with their IC75 of metformin, phenformin, chloroquine and CB-839 (based on 72 h dose response curves). The concentration of compounds used was 10 mM metformin, 100 μM phenformin, 50 μM chloroquine and 6 μM CB-839 if IC75, were above these concentrations. CH2879 cells treated with 1 μM doxorubicin (obtained from the in-house hospital pharmacy) and 50 μM ABT-737 (Catalog No. S1002, Selleckchem) were used as positive control. For the negative control doxorubicin and ABT-737 were combined with Z-vad-FMK (550377, BD Biosciences). After 24 h the caspase-glo substrate was added 1:1 followed by incubation of 60 min at room temperature. Wells were analysed using Wallac 1420 VICTOR2. The experiment was performed two times in duplicate. Data was corrected for plane RPMI control and normalised to untreated control for each cell line. Viability was measured on a simultaneously treated plate after 24 h.
Western blot analysis
HT1080, JJ012, SW1353, NDCS1 and CH2879 cells are treated with their half maximal inhibitory concentration (IC50) values (based on dose response curves of 72 h) of metformin, phenformin, chloroquine or CB-839 and lysed after 72 h. A maximum concentration of compounds of 10 mM metformin, 100 μM phenformin and 6 μM CB-839 was used if the IC50 was above these concentrations. Western blotting was performed for LC3B (1:1000, clone D11, #3868, Cell Signaling Technology) and phospho-S6 (1:1000, 2F9, #4856, Cell Signaling Technology). As a loading control, α-tubulin (1:10,000, clone DM1A, Sigma-Aldrich Chemie) expression was used. Cells were lysed using hot-SDS buffer (1% SDS, 10 mM Tris/EDTA with complete inhibitor and phosSTOP). For each sample, 10 μg protein was loaded on TGX Stain-Free™ FastCast™ 12% Acrylamide Gels (Bio-Rad). Proteins were transferred to a Polyvinylidene difluoride (PVDF) membrane using Trans-Blot® Turbo™ Transfer System (Bio-Rad) and Trans-Blot® Turbo™ RTA Transfer kit PVDF (Bio-Rad) and detected using enhanced chemo-luminescence (Pierce ECL Western Blotting Substrate Fisher Scientific), followed by exposure of 30 s to 5 min and development of the film (ECL hyperfilm, Amersham, GE Healthcare).
Cell line metabolic profiling
A Seahorse XFe 96 analyser (Seahorse Bioscience, Agilent) was used to measure the oxygen consumption rate (OCR) and the extracellular acidification rate (ECAR) in chondrosarcoma cell lines JJ012, SW1353 and CH2879 after metformin treatment. Thirty hours prior to the assay, cells were plated in optimised densities being 15,000, 13,000 and 30,000 for JJ012, SW1353 and CH2879, respectively. After 6 h cells were treated with 5 mM metformin for 24 h. Before the measurement, cells were incubated for 1 h in glucose-free RPMI-1640 supplemented with 5% FBS. During the assay, sequential injections of 10 mM glucose (Sigma-Aldrich), 2.0 µM oligomycin A, 2 µM carbonyl cyanide-4-(trifluoromethoxy)phenylhydrazone (FCCP) and 0.5 µM 1:1 rotenone: antimycin A (Cayman Chemicals) established the metabolic profile of all cell lines. Data was normalised to cell numbers measured in each individual well, determined using a Cellomics HCS fluorescent microscope (Thermoe Fisher) after fixation and Hoechst staining. Data represented as the average ± SD of triplicate measurements for metformin treated cells and 5–7 replicates for controls.
Results
Glutaminase is a potential therapeutic target in a subset of chondrosarcomas
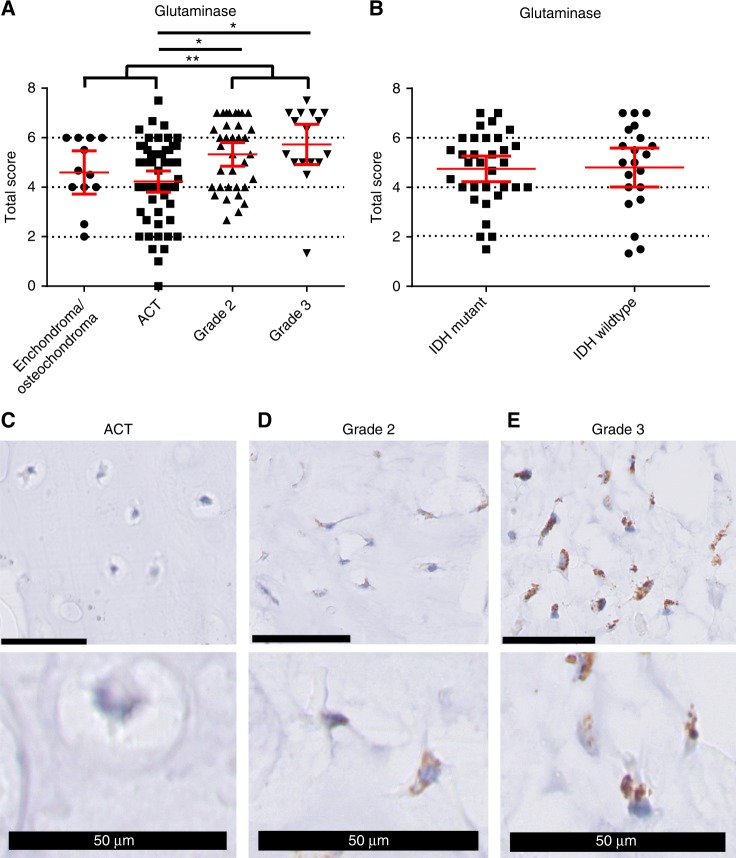
By immunohistochemistry, a difference in glutaminase expression levels between the different tumour grades was identified (ANOVA, p = 0.001), and the post-hoc analysis revealed that specifically the grade II tumours and the grade III tumours had higher expression levels compared to the ACTs (both p = 0.001) (Fig. 2a-e). As no difference between central and peripheral cartilage tumours was observed, these were combined in the analyses. Grouping the high-grade cartilage tumours (grade II and grade III chondrosarcomas) and the low-grade cartilage tumours (ACTs and enchondromas/osteochondromas) further demonstrated the significant difference in glutaminase expression levels between high-grade and low-grade cartilage tumours (p < 0.0001, independent-samples T test) (Fig. 2a). No difference in glutaminase expression between IDH1/2 mutant and IDH1/2 wildtype central cartilage tumours was observed (Fig. 2b). Therefore, glutaminase is higher expressed in high-grade compared to low-grade cartilage tumours but does not correlate to IDH1/2 mutation status.
Fig. 2.
Glutaminase expression correlates to tumour grade but not to IDH1/2 mutation status. a Total score (intensity + percentage) of glutaminase expression. *p = 0.001 by one-way ANOVA with the LSD post-hoc analysis. **p < 0.0001 by independent-samples T test, grouping the high-grade and the low-grade cartilage tumours. b No difference between IDH1/2 mutant and IDH1/2 wildtype central tumours was observed. c ACT without expression of GLS, scored as percentage 0, intensity 0. d Grade II chondrosarcoma with medium expression of GLS, scored as percentage 2, intensity 2. e Grade III chondrosarcoma with high expression of GLS, percentage 4 intensity 3. Black bars represent 50 µm
Using qRT-PCR analyses, we demonstrate that all cell lines have higher expression levels of glutaminase compared to the controls (growth plate and cartilage), although expression levels are variable (Fig. 3a). Inhibition of glutaminase using CB-839 in ten chondrosarcoma cell lines revealed that HT1080 (IDH1R132C), SW1353 (IDH2R172S) and, to a lesser extent, JJ012 (IDH1R132G), were very sensitive for glutaminase inhibition, with IC50 values below 5 μM (Fig. 3b, Table 1). L2975 (IDH2R172W), NDCS1 (IDH1/2WT) and CH3573 (IDH1/2WT) had IC50 values of 10.2, 13.5 and 17.5 μM, while the remaining four cell lines (one IDH1R132C, three IDH1/2WT) had IC50 values above 50 μM. Interestingly, absence of FBS, increased the sensitivity to CB-839 especially in the IDH1/2 mutant cell lines, while there was no clear difference in the cell lines with wildtype IDH1/2 (Fig. 3c). In conclusion, these experiments demonstrate that a subset of chondrosarcoma cell lines is dependent on glutaminase-mediated glutaminolysis to maintain cell viability.
Fig. 3.
The glutaminase inhibitor CB-839 inhibits chondrosarcoma cell viability. a Expression levels of glutaminase in ten chondrosarcoma cell lines and two controls. Glutaminase is higher expressed in chondrosarcoma cell lines compared to growth plate and articular cartilage. b Ten chondrosarcoma cell lines were treated for 72 h with CB-839, a glutaminase inhibitor. Sensitivity differed between the different cell lines. c Indicated cell lines were treated with 0, 20 or 200 nM CB-839 in the presence or absence of FBS. In the absence of FBS, all cell lines are more sensitive for inhibition with CB-839, especially the IDH1/2 mutant cell lines
Table 1.
Absolute IC50 values of CB-839, metformin, phenformin and chloroquine upon 72 h of treatment, as determined by PrestoBlue Cell Viability
| Compound/cell line | CB-839 (μM) | Metformin (mM) | Phenformin (μM) | Chloroquine (μM) | IDH1/2 status | Reference |
|---|---|---|---|---|---|---|
| HT1080 | 0.1 | 1.20 | 17.1 | 19.5 | IDH1 p.Arg132Cys | Rasheed et al.30 |
| JJ012 | 4.6 | 19.0 | 504.1 | 27.1 | IDH1 p.Arg132Gly | Scully et al.28 |
| L835 | >50 | >20 | 870.3 | 31.1 | IDH1 p.Arg132Cys | Van Oosterwijk et al.29 |
| SW1353 | 0.2 | 8.26 | 74.5 | 24.6 | IDH2 p.Arg172Ser | ATCC |
| L2975 | 10.2 | 10.6 | 116.6 | 30.5 | IDH2 p.Arg172Trp | Van Oosterwijk et al.29 |
| CH2879 | >50 | 10.9 | 193.7 | 57.9 | WT | Gil Benso et al.31 |
| NDCS1 | 13.5 | 18.1 | 187.9 | 16.7 | WT | Kudo et al.34 |
| CH3573 | 17.5 | >20 | 343.4 | 34.0 | WT | Calabuig-Farinas et al.33 |
| L3252b | >50 | 16.7 | >1000 | 39.4 | WT | Van Oosterwijk et al.29 |
| MCS170 | >50 | 10.5 | 294.7 | 14.4 | WT | De Jong et al.32 |
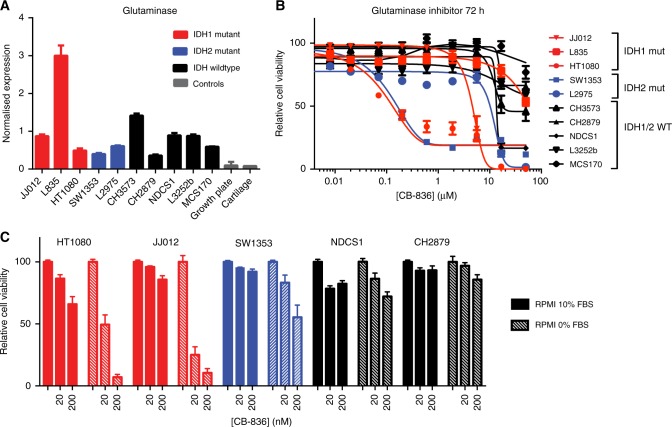
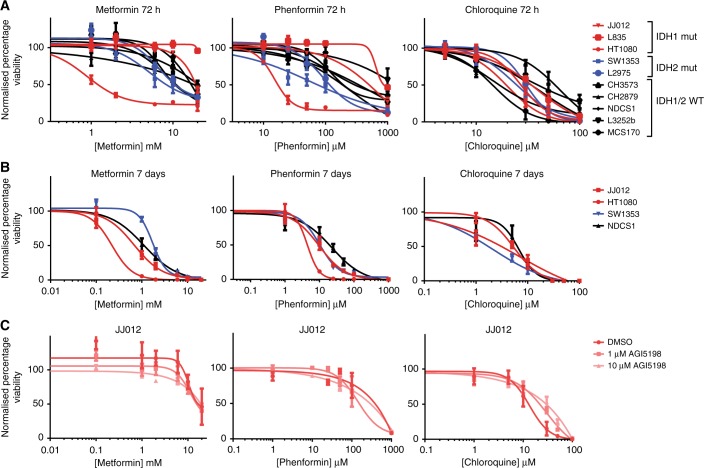
Metformin, phenformin and chloroquine inhibit chondrosarcoma cell viability
Treating the chondrosarcoma cell line panel for 72 h with metformin, phenformin or chloroquine demonstrated that sensitivity for these compounds differed between the different chondrosarcoma cell lines (Fig. 4a). With an IC50 of 1.20 mM and 17.1 μM after 72 h of treatment, HT1080 cells have a higher sensitivity for respectively metformin and phenformin compared to the other cell lines (Table 1). Treating the chondrosarcoma cell lines for 7 days increased the effect of metformin, phenformin and chloroquine on cell viability (Fig. 4b). Hoechst quantification confirmed that the effects on cell viability were caused by an absolute decrease in cell amount (Supplementary Figure 1). No difference between IDH1/2 mutant and IDH1/2 wildtype chondrosarcoma cell lines in sensitivity for metformin, phenformin and chloroquine was observed. To further demonstrate that the IDH1 mutant enzyme does not influence sensitivity to these compounds, the inhibitors were combined with AGI-5198, a specific inhibitor of the mutant IDH1 enzyme, in IDH1 mutant JJ012 and HT1080 cells. Cell viability (Fig. 4c and Supplementary Figure 2) was unaffected by cotreatment with AGI-5198. These results demonstrate that chondrosarcoma cell lines can be targeted by metformin, phenformin and chloroquine and further demonstrates the dependency of chondrosarcoma cell lines on glutaminolysis independent of the presence of the IDH1/2 mutant enzyme.
Fig. 4.
Chondrosarcoma cell lines are sensitive for metformin, phenformin and chloroquine, irrespective of the IDH1/2 mutation. a Chondrosarcoma cell lines were treated for 72 h with corresponding compounds. Cell viability was measured using the PrestoBlue assay. b Four chondrosarcoma cell lines were treated for 7 days with the corresponding inhibitors. c IDH1 mutant JJ012 cells were pretreated for 72 h with 10 µM AGI-5198, 1 µM AGI-5198 or DMSO, after which they were treated with a combination of AGI-5198 and the corresponding compounds for 72 h. No effect of AGI-5198 was observed
Cellular effects of glutaminolysis inhibition
To investigate the effect on apoptosis, caspase-glo 3/7 assays were performed. Chloroquine slightly increased caspase 3/7 activity in three out of five cell lines tested (Fig. 5a). While the other compounds did impact cell viability after 24 h (Fig. 5b), no effect on caspase 3/7 activity was observed. Next, we evaluated the effect of the four metabolic compounds on phosphorylated S6 protein levels, as this is an indicator of mTOR activity. As shown in Fig. 5c, metformin and phenformin decreased phosphorylated S6 levels in four out of five and three out of five cell lines respectively. However, metformin and phenformin did not affect phosphorylated S6 levels in HT1080 cells, the cell line that is most sensitive to metformin. Interestingly, metformin decreased LC3B-II levels in four out of five cell lines, which indicates an increase in autophagy.40 As expected, chloroquine greatly increased LC3B-II levels. CB-839 did not affect phosphorylated S6 or LC3B protein levels. Thus, while the induction of apoptosis is very limited, metformin and phenformin decreased mTOR activity in chondrosarcoma cells, and metformin decreased autophagy, an effect that is counteracted by chloroquine.
Fig. 5.
The different compounds provoke different intracellular responses. a Caspase 3/7 activity of HT1080, JJ012, SW1353, NDCS1 and CH2879 cells after 24 h treatment with the metformin, phenformin, chloroquine and CB-839, as determined by caspase-glo 7/3 assays. Only chloroquine slightly increases Caspase 3/7 activity in 3/5 cell lines. CH2879 cells treated with ABT-737 and doxorubicin were used as positive control. For the negative control these compounds were combined with Z-vad-FMK. b Simultaneously to the measurement of caspase 3/7 activity, cell viability was measured using a Presto-Blue assay. c Western blot to evaluate the effect of metformin, phenformin, chloroquine and CB-839 on phosphorylated S6 and LC3B levels in five chondrosarcoma cell lines. Cell lines were treated for 72 h with their corresponding IC50 values. Metformin and phenformin decreased levels of phosphorylated S6 in 4/5 and 3/5 cell lines, respectively, and decreased levels of LC3B in 4/5 and 1/5 cell lines, respectively. Chloroquine increased LC3B in all cell lines
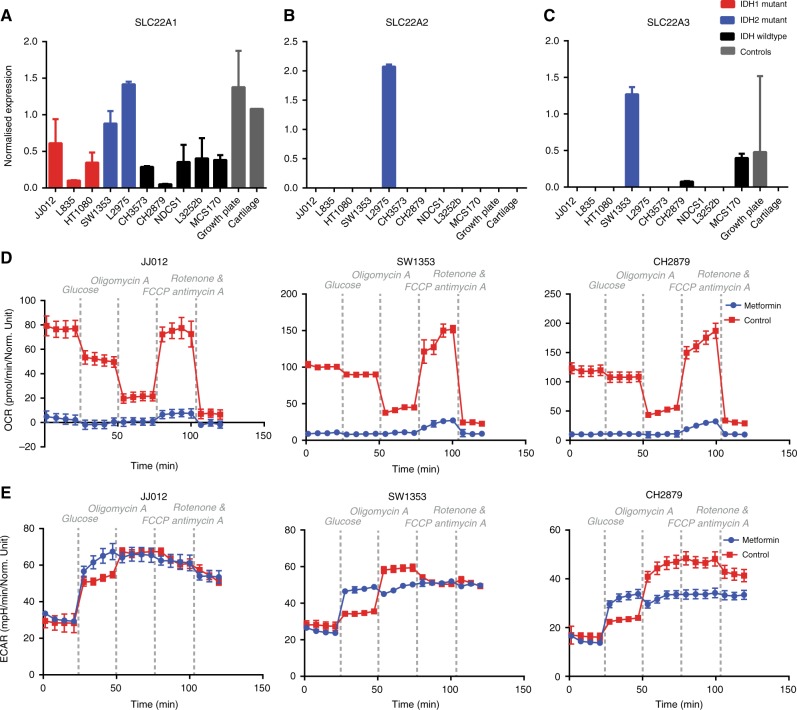
Metformin is sufficiently transported into chondrosarcoma cells to completely inhibit mitochondrial respiration
Next, expression levels of SLC22A1–3 were determined by qRT-PCR analyses, as these transporters are essential for the cellular uptake of metformin and might explain the variability in sensitivity for metformin. Although expression is variable, all cell lines express SLC22A1 (Fig. 6a). Interestingly, the two IDH2 mutated cell lines had the highest expression of SLC22A1. SLC22A2 is only expressed by L2975 (Fig. 6b) and SLC22A3 is only expressed by SW1353, MCS170 and CH2879 (Fig. 6c). This demonstrates that all cell lines express transporters for the cellular uptake of metformin, but expression levels differ.
Fig. 6.
Chondrosarcoma cells sufficiently express SLC22A1 for metformin to completely inhibit mitochondrial respiration. a All chondrosarcoma cell lines express SLC22A1. b SLC22A2 is only expressed by L2975. c Three out of ten chondrosarcoma cell lines express SLC22A3. d, e The impact of 24 h treatment with 5 mM metformin on the Oxygen Consumption Rate (OCR)(D) and extracellular acidification rate (ECAR)(E) of JJ012, SW1353 and CH2879 was measured by Seahorse experiments. Metformin completely blocks mitochondrial respiration, which is only accompanied by a small increase in glycolysis
To evaluate the effect of metformin on chondrosarcoma cell metabolism, seahorse experiments with three chondrosarcoma cell lines (one IDH1 mutated, one IDH2 mutated and one IDH wildtype) were performed. Strikingly, metformin completely inhibited mitochondrial respiration in all cell lines tested independent of IDH1/2 mutation status or SLC22A1 levels (Fig. 6d). The small increase in OCR observed after the addition of FCCP and increased ECAR levels after glucose injection demonstrate that the metformin treated cells are still viable. Interestingly, metformin treated cells showed higher levels of glycolysis when glucose is present compared to the controls. However, oligomycin A injection increased glycolytic levels in controls but not in treated cells, indicating a maximum in glycolytic energy production is achieved in treated cells after glucose addition (Fig. 6e). The small difference in glycolytic activity between treated and untreated cells cannot compensate for the observed loss in ATP production through mitochondrial respiration, suggesting that chondrosarcoma cells utilise other pathways for energy production.
Discussion
In this study, we demonstrated a difference in glutaminase expression levels between the different chondrosarcoma grades, with the highest expression observed in high-grade tumours. We therefore examined whether glutaminolysis could be exploited as a therapeutic target for high-grade chondrosarcoma. Based on current ongoing clinical trials targeting glutaminolysis, to which chondrosarcoma patients can be enrolled, we interfered with glutaminolysis in chondrosacoma cell lines at different levels (Fig. 1).
First, we inhibited glutaminase using the glutaminase inhibitor CB-839, and indeed, six out of ten chondrosarcoma cell lines showed IC50 values below 20 μM. CB-839 did not induce apoptosis, autophagy or mTOR activity, suggesting that it likely impacts cell viability via other mechanisms.
Second, we used the widely used anti-diabetic drug metformin, which, among other effects, indirectly inhibits glutaminase via c-Myc; (Fig. 1),21,22 inhibits complex 1 of the electron transport chain,20 and inhibits mTOR signalling.19 Indeed, a subset of chondrosarcoma cell lines was sensitive to metformin, especially when treated for a longer time period. mTOR signalling was previously shown to be important in chondrosarcoma41 and we confirmed that metformin decreased mTOR activity in all but one chondrosarcoma cell lines tested, which is in line with findings in other studies.19 Interestingly, mTOR activity was not inhibited in HT1080 which is the most sensitive for metformin treatment, suggesting that mTOR inhibition alone cannot explain the impact of metformin on chondrosarcoma cell viability. Furthermore, while apoptosis was absent, metformin seemed to induce autophagy in the majority of cell lines tested, which can likely be linked to the effect of metformin on AMPK.42 In this study, we further demonstrate that metformin completely blocks mitochondrial respiration in chondrosarcoma cells, likely caused by its effect on complex I of the electron transport chain. However, blocking complex I of the electron transfer chain (and therefore oxidative glutaminolysis) alone was not sufficient to inhibit cell viability, as an even higher concentration of metformin only had a small impact on cell viability within the 24-h time frame of the mitochondrial respiration experiments (Fig. 5b). The small difference in glycolysis observed upon treatment with metformin is likely insufficient to compensate for the total los of ATP production through oxidative means, suggesting that chondrosarcoma cells are not dependent on oxidative metabolism and require other sources, in addition to the increased glycolysis, to supply the necessary energy. In prostate cancer cell lines, it was demonstrated that metformin treatment increased the dependency on reductive glutaminolysis.43 Further identifying these pathways might provide interesting targets for combination treatment with metformin.
Third, as an alternative to metformin, we used its lipophilic analogue phenformin. In contrast to metformin, phenformin does not need SLC22A1-3 transport to get into cells.
As expected, the effect of phenformin on cell viability, mTOR activity, and apoptosis was very similar to metformin. Contrary to metformin, phenformin is not used in the clinic due to an increased risk of lactic acidosis. Moreover, we show that all chondrosarcoma cell lines sufficiently express the SLC22A1 transporter that is necessary for metformin uptake, suggesting that there is limited rationale to move to phenformin trials for chondrosarcomas when the metformin trial demonstrates limited efficacy.
Fourth, we evaluated the anti-malaria drug chloroquine, which, in addition to inhibiting glutamate dehydrogenase, is a well-known inhibitor of autophagy and thereby inhibits many other metabolic and signal transduction pathways.44,45 The chondrosarcoma cell lines were sensitive to chloroquine. Also, we confirmed that chloroquine inhibited autophagy in all chondrosarcoma cell lines tested. Moreover, a slight induction of apoptosis was seen in three out of five chondrosarcoma cell lines.
Thus, we used four different drugs to evaluate whether the increased dependence on glutaminolysis could be therapeutically exploited using repurposing of existing drugs, and confirmed that a subset of chondrosarcoma cell lines is indeed sensitive to glutaminolysis inhibition. We could not identify a correlation between levels of glutaminase expression and sensitivity for any of these metabolic compounds in the panel of ten chondrosarcoma cell lines. Of note, there was also no correlation of the IDH1/2 mutation status of chondrosarcoma cells with sensitivity to these compounds, or with the expression levels of glutaminase in primary tumours. We could therefore not confirm the prevailing hypothesis that IDH1/2 mutant chondrosarcoma cells rely on glutaminolysis to generate sufficient α-KG for D-2-HG production,15–17 as it seems that also high-grade chondrosarcomas that are wildtype for IDH1/2 depend on glutaminolysis. To explain this dependency of IDH1/2 wildtype chondrosarcoma on glutaminolysis, it is tempting to speculate that the hypoxic microenvironment, which is a characteristic of chondrosarcoma,46 is equally important or even overrates the effect of the IDH1/2 mutation in chondrosarcoma. HIF-1α activates pyruvate dehydrogenase kinase, which inactivates pyruvate dehydrogenase, thereby inhibiting the influx of pyruvate into the TCA cycle.47 In this context, TCA cycle anaplerosis is required for the synthesis of fatty acids, which is then primarily mediated via glutaminolysis.48 Therefore, the hypoxic microenvironment of chondrosarcomas potentially explains why chondrosarcomas depend on glutaminolysis irrespective of the presence or absence of an IDH1/2 mutation.
Our results indicate that there is limited preclinical rationale to select chondrosarcoma patients for treatment with these compounds based on their IDH1/2 mutation status. This is in contrast to the studies by Cuyas et al.16 and Molenaar et al.,49 where, respectively, an increased sensitivity for metformin was identified in an engineered IDH1 mutant breast cancer cell line, and in an engineered IDH1 mutant colorectal cancer cell line compared to their wildtype parental cells. The differences in tumour types and the fact that these cell lines harbour an engineered instead of an endogenous IDH1/2 mutation likely explain the differences in experimental findings.
In conclusion, our results demonstrate that glutaminase is higher expressed in high-grade compared to low-grade chondrosarcomas. High-grade chondrosarcomas are dependent on glutaminolysis which is independent of IDH1/2 mutation status. This dependence can be therapeutically exploited by repurposing existing drugs that inhibit glutaminolysis, including CB-839, metformin, phenformin and chloroquine.
Electronic supplementary material
Acknowledgements
The authors thank Dr. Joel A. Block (Rush University, Chicago, USA) for providing JJ012, Prof. Antonio Llombart-Bosch (Valencia University, Spain) for CH2879 and CH3573, Dr. M. Namba (Okayama University Medical School, Japan) for OUMS27, and Dr. Naoko Kudo (Niigata University Graduate School of Medical and Dental Sciences, Japan) for NDCS1. In addition, the authors thank Gaia Alberti, Hans Baelde, Pauline Wijers-Koster and Inge Briaire- de Bruijn for technical assistance, Jolieke G. van Oosterwijk for construction of the tissue microarray, and Willem Corver for help with the Seahorse experiments. This study was funded by the Leiden University Medical Center.
Author contributions
B.N., R.D.A., Y.dJ., A.B.K. and B.E.W.Mv.dA. performed the experiments. E.F.P.P. and A.H.G.C. performed all the scoring of the TMA’s. E.F.P.P., B.N., R.J.M., A.M.C.J. and J.V.M.G.B. designed the study. E.F.P.P., A.M.C.J. and J.V.M.G.B. supervised the experiments. E.F.P.P. and J.V.M.G.B. wrote the manuscript. All authors read and approved the final version of the manuscript.
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All samples were handled according to the Dutch code of proper secondary use of human material as accorded by the Dutch society of pathology (Federa). The samples were handled in a coded manner. All study methods were approved by the LUMC ethical board (B17.020 v2).
Availability of data and materials
The manuscript and the supplementary files contain all potential findings based on raw data analysis. Raw data can be obtained from authors on request.
Footnotes
These authors contributed equally: Elisabeth F.P. Peterse, Bertine Niessen.
Electronic supplementary material
Supplementary information is available for this paper at 10.1038/s41416-018-0050-9.
References
- 1.Hogendoorn, P. C. W., Bovée, J. V. M. G. & Nielsen, G. P. in WHO Classification of Tumours of Soft Tissue and Bone (eds Fletcher, C. D. M., Bridge, J. A., Hogendoorn P. C. W. & Mertens, F.) 264–268 (IARC, Lyon, 2013).
- 2.Gelderblom H, et al. The clinical approach towards chondrosarcoma. Oncologist. 2008;13:320–329. doi: 10.1634/theoncologist.2007-0237. [DOI] [PubMed] [Google Scholar]
- 3.Duchman KR, Lynch CF, Buckwalter JA, Miller BJ. Estimated cause-specific survival continues to improve over time in patients with chondrosarcoma. Clin. Orthop. Relat. Res. 2014;472:2516–2525. doi: 10.1007/s11999-014-3600-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inwards, C. & Hogendoorn, P. C. W. in WHO Classification of Tumours of Soft Tissue and Bone (eds Fletcher, C. D. M., Bridge, J. A., Hogendoorn P. C. W. & Mertens, F.) 269–270 (IARC, Lyon, 2013).
- 5.Frezza AM, et al. Mesenchymal chondrosarcoma: prognostic factors and outcome in 113 patients. A European Musculoskeletal Oncology Society study. Eur. J. Cancer. 2015;51:374–381. doi: 10.1016/j.ejca.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 6.Xu J, Li D, Xie L, Tang S, Guo W. Mesenchymal chondrosarcoma of bone and soft tissue: a systematic review of 107 patients in the past 20 years. PLoS ONE. 2015;10:e0122216. doi: 10.1371/journal.pone.0122216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakashima, Y., Pinieux, de, G. & Ladanyi, M. in WHO Classification of Tumours of Soft Tissue and Bone (eds Fletcher, C. D. M., Bridge, J. A., Hogendoorn P. C. W. & Mertens, F.) 271–272 (IARC, Lyon, 2013).
- 8.van Maldegem AM, et al. Outcome of advanced, unresectable conventional central chondrosarcoma. Cancer. 2014;120:159–164. doi: 10.1002/cncr.28845. [DOI] [PubMed] [Google Scholar]
- 9.Amary MF, et al. IDH1 and IDH2 mutations are frequent events in central chondrosarcoma and central and periosteal chondromas but not in other mesenchymal tumours. J. Pathol. 2011;224:334–343. doi: 10.1002/path.2913. [DOI] [PubMed] [Google Scholar]
- 10.Meijer D, et al. Genetic characterization of mesenchymal, clear cell, and dedifferentiated chondrosarcoma. Genes. Chromosomes Cancer. 2012;51:899–909. doi: 10.1002/gcc.21974. [DOI] [PubMed] [Google Scholar]
- 11.Amary MF, et al. Ollier disease and Maffucci syndrome are caused by somatic mosaic mutations of IDH1 and IDH2. Nat. Genet. 2011;43:1262–1265. doi: 10.1038/ng.994. [DOI] [PubMed] [Google Scholar]
- 12.Pansuriya TC, et al. Somatic mosaic IDH1 and IDH2 mutations are associated with enchondroma and spindle cell hemangioma in Ollier disease and Maffucci syndrome. Nat. Genet. 2011;43:1256–1261. doi: 10.1038/ng.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu W, et al. Oncometabolite 2-hydroxyglutarate is a competitive inhibitor of alpha-ketoglutarate-dependent dioxygenases. Cancer Cell. 2011;19:17–30. doi: 10.1016/j.ccr.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suijker J, et al. Inhibition of mutant IDH1 decreases D-2-HG levels without affecting tumorigenic properties of chondrosarcoma cell lines. Oncotarget. 2015;6:12505–12519. doi: 10.18632/oncotarget.3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grassian AR, et al. IDH1 mutations alter citric acid cycle metabolism and increase dependence on oxidative mitochondrial metabolism. Cancer Res. 2014;74:3317–3331. doi: 10.1158/0008-5472.CAN-14-0772-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cuyas E, et al. Oncometabolic mutation IDH1 R132H confers a metformin-hypersensitive phenotype. Oncotarget. 2015;6:12279–12296. doi: 10.18632/oncotarget.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen R, et al. Hominoid-specific enzyme GLUD2 promotes growth of IDH1R132H glioma. Proc. Natl Acad. Sci. USA. 2014;111:14217–14222. doi: 10.1073/pnas.1409653111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Molenaar RJ, et al. Study protocol of a phase IB/II clinical trial of metformin and chloroquine in patients with IDH1-mutated or IDH2-mutated solid tumours. BMJ Open. 2017;7:e014961. doi: 10.1136/bmjopen-2016-014961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jalving M, et al. Metformin: taking away the candy for cancer? Eur. J. Cancer. 2010;46:2369–2380. doi: 10.1016/j.ejca.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 20.Wheaton WW, et al. Metformin inhibits mitochondrial complex I of cancer cells to reduce tumorigenesis. eLife. 2014;3:e02242. doi: 10.7554/eLife.02242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blandino G, et al. Metformin elicits anticancer effects through the sequential modulation of DICER and c-MYC. Nat. Commun. 2012;3:865. doi: 10.1038/ncomms1859. [DOI] [PubMed] [Google Scholar]
- 22.Gao P, et al. c-Myc suppression of miR-23a/b enhances mitochondrial glutaminase expression and glutamine metabolism. Nature. 2009;458:762–765. doi: 10.1038/nature07823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yee SW, et al. Prediction and validation of enzyme and transporter off-targets for metformin. J. Pharmacokinet. Pharmacodyn. 2015;42:463–475. doi: 10.1007/s10928-015-9436-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jarzyna R, Lenarcik E, Bryla J. Chloroquine is a potent inhibitor of glutamate dehydrogenase in liver and kidney-cortex of rabbit. Pharmacol. Res. 1997;35:79–84. doi: 10.1006/phrs.1996.0108. [DOI] [PubMed] [Google Scholar]
- 25.Choi MM, et al. Inhibitory properties of nerve-specific human glutamate dehydrogenase isozyme by chloroquine. J. Biochem. Mol. Biol. 2007;40:1077–1082. doi: 10.5483/bmbrep.2007.40.6.1077. [DOI] [PubMed] [Google Scholar]
- 26.van Oosterwijk JG, et al. Src kinases in chondrosarcoma chemoresistance and migration: dasatinib sensitises to doxorubicin in TP53 mutant cells. Br. J. Cancer. 2013;109:1214–1222. doi: 10.1038/bjc.2013.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baranski Z, et al. Aven-mediated checkpoint kinase control regulates proliferation and resistance to chemotherapy in conventional osteosarcoma. J. Pathol. 2015;236:348–359. doi: 10.1002/path.4528. [DOI] [PubMed] [Google Scholar]
- 28.Scully SP, et al. Marshall Urist Award. Interstitial collagenase gene expression correlates with in vitro invasion in human chondrosarcoma. Clin. Orthop. Relat. Res. 2000;376:291–303. doi: 10.1097/00003086-200007000-00038. [DOI] [PubMed] [Google Scholar]
- 29.van Oosterwijk JG, et al. Three new chondrosarcoma cell lines: one grade III conventional central chondrosarcoma and two dedifferentiated chondrosarcomas of bone. BMC Cancer. 2012;12:375. doi: 10.1186/1471-2407-12-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rasheed S, Nelson-Rees WA, Toth EM, Arnstein P, Gardner MB. Characterization of a newly derived human sarcoma cell line (HT-1080) Cancer. 1974;33:1027–1033. doi: 10.1002/1097-0142(197404)33:4<1027::AID-CNCR2820330419>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 31.Gil-Benso R, et al. Establishment and characterization of a continuous human chondrosarcoma cell line, ch-2879: comparative histologic and genetic studies with its tumor of origin. Lab. Invest. 2003;83:877–887. doi: 10.1097/01.LAB.0000073131.34648.EA. [DOI] [PubMed] [Google Scholar]
- 32.de Jong Y, et al. Inhibition of Bcl-2 family members sensitizes mesenchymal chondrosarcoma to conventional chemotherapy: report on a novel mesenchymal chondrosarcoma cell line. Lab. Invest. 2016;96:1128–1137. doi: 10.1038/labinvest.2016.91. [DOI] [PubMed] [Google Scholar]
- 33.Calabuig-Farinas S, et al. Characterization of a new human cell line (CH-3573) derived from a grade II chondrosarcoma with matrix production. Pathol. Oncol. Res. 2012;18:793–802. doi: 10.1007/s12253-012-9505-0. [DOI] [PubMed] [Google Scholar]
- 34.Kudo N, et al. Establishment of novel human dedifferentiated chondrosarcoma cell line with osteoblastic differentiation. Virchows Arch. 2007;451:691–699. doi: 10.1007/s00428-007-0426-3. [DOI] [PubMed] [Google Scholar]
- 35.Martins-Neves SR, et al. Osteosarcoma Stem Cells Have Active Wnt/beta-catenin and Overexpress SOX2 and KLF4. Journal of cellular physiology. 2016;231:876–886. doi: 10.1002/jcp.25179. [DOI] [PubMed] [Google Scholar]
- 36.Rozeman LB, et al. Absence of IHH and retention of PTHrP signalling in enchondromas and central chondrosarcomas. J. Pathol. 2005;205:476–482. doi: 10.1002/path.1723. [DOI] [PubMed] [Google Scholar]
- 37.Hameetman L, et al. Peripheral chondrosarcoma progression is accompanied by decreased Indian Hedgehog signalling. J. Pathol. 2006;209:501–511. doi: 10.1002/path.2008. [DOI] [PubMed] [Google Scholar]
- 38.van Oosterwijk JG, et al. Restoration of chemosensitivity for doxorubicin and cisplatin in chondrosarcoma in vitro: BCL-2 family members cause chemoresistance. AnnOncol. 2012;23:1617–1626. doi: 10.1093/annonc/mdr512. [DOI] [PubMed] [Google Scholar]
- 39.de Jong Y, et al. Targeting survivin as a potential new treatment for chondrosarcoma of bone. Oncogenesis. 2016;5:e222. doi: 10.1038/oncsis.2016.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barth S, Glick D, Macleod KF. Autophagy: assays and artifacts. J. Pathol. 2010;221:117–124. doi: 10.1002/path.2694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang YX, et al. Functional profiling of receptor tyrosine kinases and downstream signaling in human chondrosarcomas identifies pathways for rational targeted therapy. Clin. Cancer Res. 2013;19:3796–3807. doi: 10.1158/1078-0432.CCR-12-3647. [DOI] [PubMed] [Google Scholar]
- 42.Kim J, Kundu M, Viollet B, Guan KL. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat. Cell Biol. 2011;13:132–141. doi: 10.1038/ncb2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fendt SM, et al. Metformin decreases glucose oxidation and increases the dependency of prostate cancer cells on reductive glutamine metabolism. Cancer Res. 2013;73:4429–4438. doi: 10.1158/0008-5472.CAN-13-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reyjal J, Cormier K, Turcotte S. Autophagy and cell death to target cancer cells: exploiting synthetic lethality as cancer therapies. Adv. Exp. Med. Biol. 2014;772:167–188. doi: 10.1007/978-1-4614-5915-6_8. [DOI] [PubMed] [Google Scholar]
- 45.Pascolo S. Time to use a dose of Chloroquine as an adjuvant to anti-cancer chemotherapies. Eur. J. Pharmacol. 2016;771:139–144. doi: 10.1016/j.ejphar.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 46.Boeuf S, Bovee JV, Lehner B, Hogendoorn PC, Richter W. Correlation of hypoxic signalling to histological grade and outcome in cartilage tumours. Histopathology. 2010;56:641–651. doi: 10.1111/j.1365-2559.2010.03528.x. [DOI] [PubMed] [Google Scholar]
- 47.Kim JW, Tchernyshyov I, Semenza GL, Dang CV. HIF-1-mediated expression of pyruvate dehydrogenase kinase: a metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 2006;3:177–185. doi: 10.1016/j.cmet.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 48.Wise DR, et al. Hypoxia promotes isocitrate dehydrogenase-dependent carboxylation of alpha-ketoglutarate to citrate to support cell growth and viability. Proc. Natl Acad. Sci. USA. 2011;108:19611–19616. doi: 10.1073/pnas.1117773108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Molenaar RJ, et al. Radioprotection of IDH1-mutated cancer cells by the IDH1-mutant inhibitor AGI-5198. Cancer Res. 2015;75:4790–4802. doi: 10.1158/0008-5472.CAN-14-3603. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The manuscript and the supplementary files contain all potential findings based on raw data analysis. Raw data can be obtained from authors on request.