Abstract
Objective
To assess the extent to which long‐term care facilities in Japan adhere to blood pressure (BP) measurement guidelines.
Design
Cross‐sectional, observational survey.
Setting
Japan (nationwide).
Participants
Geriatric health service facilities that responded to a questionnaire among 701 facilities that provide short‐time daycare rehabilitation services in Japan.
Methods
A written questionnaire that asked about types of measurement devices, number of measurements used to obtain an average BP, resting time prior to measurement, and measurement methods when patients’ arms were covered with thin (eg, a light shirt) or thick sleeves (eg, a sweater) was administered.
Main outcome measure
Proportion of geriatric health service facilities adherent to BP measurement guidelines.
Results
The response rate was 63.2% (443/701). Appropriate upper‐arm BP measurement devices were used at 302 facilities (68.2%). The number of measurements was appropriate at 7 facilities (1.6%). Pre‐measurement resting time was appropriate (≥5 minutes) at 205 facilities (46.3%). Of the 302 facilities that used appropriate BP measurement devices, 4 (1.3%) measured BP on a bare arm if it was covered with a thin sleeve, while 266 (88.1%) measured BP over a thin sleeve. When arms were covered with thick sleeves, BP was measured on a bare arm at 127 facilities (42.1%) and over a sleeve at 78 facilities (25.8%).
Conclusions
BP measurement guidelines were not necessarily followed by long‐term care service facilities in Japan. Modification of guidelines regarding removing thick sweaters and assessing BP on a visit‐to‐visit basis might be needed.
Keywords: cardiovascular medicine, elderly, nursing care
1. INTRODUCTION
The world's population is aging profoundly, with the population of older persons growing by 2% each year.1 Japan is the most rapidly aging country in the world, with 26.0% of the population aged 65 years or older in 2014.2 Also, the aged population is getting older1 and the percentage of older persons with comorbidities is expected to increase.
Blood pressure (BP) measurement is one of the most basic and simple ways of assessing the health status of the elderly with comorbidities in any setting. As the population ages, continuous monitoring of BP in patients at various settings, including long‐term care facilities and nursing homes, is needed.
Although guidelines outline a standard method for measuring BP, adherence to these guidelines is reportedly difficult. The Eighth Joint National Committee3 recommends that BP should be assessed after at least five minutes of rest in a chair with properly calibrated and validated automated oscillometric devices and an appropriately sized cuff on the bare arm. Two or three measurements are required to obtain an average value. BP measurements over thick clothing were found to be less accurate than measurements on bare arms.4 However, measuring BP according to the guidelines is difficult in the office,5 at home,6 and in inpatient settings.7
Long‐term care facilities are another setting where BP measurements are performed. However, the accuracy of measurements in these settings is unclear. In Japan, many of these facilities also provide visiting rehabilitation services to daycare users.8 BP measurements are needed prior to each visit. Although precise measurements may not be critical for the management of facility users, their physicians sometimes rely on BP reports at each visit as a substitute for BP measurements performed at home. In these facilities, BP measurement guidelines are expected to be particularly difficult to follow, partially because they hire many providers with insufficient professional training, such as nonmedical caregivers. Furthermore, the frailty of residents complicates efforts to remove shirts or sweaters.
The objective of this study was to investigate BP measurement methods at long‐term care facilities in Japan. We aim to provide a foundation for recommending a more accurate and feasible standard for BP measurement at these facilities and thereby contribute to improved care for aging populations.
2. METHODS
2.1. Participants
We investigated 701 geriatric health service facilities in Japan that provide short‐time daycare rehabilitation services (Figure 1). Geriatric health service facility is one type of long‐term care facility in Japan for elderly individuals whose illness is stable and does not require hospital treatment but requires rehabilitation, nursing, or care.9 These facilities offer physical and occupational therapy to maintain or restore physical or mental function and to increase independence in performing activities of daily living,8 which could be provided on either an inpatient or an outpatient basis. In 2014, 3,293 of 4,016 geriatric health service facilities in Japan provided daycare rehabilitation services.10 Short‐time daycare rehabilitation services, which last for less than 4 hours per day, are designed to promote a smooth transition from rehabilitation covered by medical insurance to long‐term care insurance. According to the website of the Japan Association of Geriatric Health Services Facilities,9 as of April 2016, there were 701 geriatric health service facilities providing short‐time daycare rehabilitation services. The present nationwide survey in Japan included these 701 facilities, which covered every prefecture in Japan, because this type of facility is expected to contribute to a smooth transition from care covered by medical insurance, and generally employs a variety of medical professionals. These facilities are nationally regulated, and are therefore assumed to be similar in terms of the quality of care they provide. We asked the manager of each daycare service to complete the questionnaire.
Figure 1.
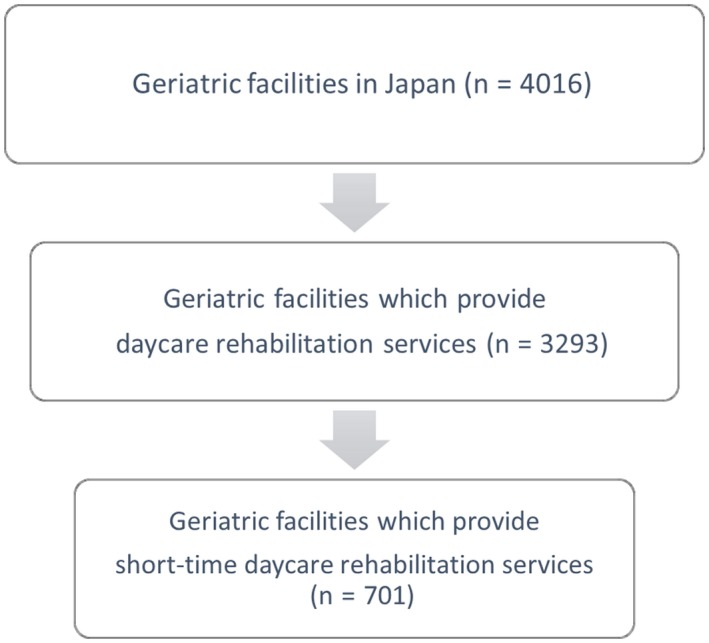
Selection of study participants
2.2. Questionnaire survey
In May and June 2016, a self‐administered questionnaire was sent by mail to the facilities and returned by fax. The questionnaire consisted of five multiple‐choice questions concerning the following aspects of blood measurement during daycare rehabilitation services: (i) type of measurement device used (sphygmomanometer, semiautomated oscillometric device, oscillometric device for the upper arm, oscillometric device for the wrist, or other), (ii) percentage of measurements performed twice or more to obtain the average BP (≥80% of the time, 50 to <80%, 20 to <50%, <20%, or rarely), (iii) mean resting time before measurement (≥5 minutes, 3 to <5 minutes, 1 to <3 minutes, <1 minute, or rarely), (iv) approach to patients wearing thin‐sleeved shirts (remove the shirt sleeve, roll the sleeve up to the upper arm, roll the sleeve up to the elbow, measure over the sleeved arm, or other), and (v) approach to patients wearing thick clothing, for example, a thick swearer (remove the sweater, roll the sleeve up to the upper arm, roll the sleeve up to the elbow, measure over the sleeved arm, or other). Each question had five answer choices.
We tabulated the proportion of facilities that adhered to BP measurement guidelines,3 that is, the adherence ratio. We calculated the adherence ratio as the percentage of facilities that made the appropriate choices. Appropriate choices for each question were based on the following criteria: (i) Upper arm devices were used, (ii) measurement was performed twice or more per sitting to determine the average BP at least 80% of the time, (iii) patients rested for ≥5 minutes prior to the first measurement, (iv) patients removed sleeved shirts, and (v) patients removed thick clothing. Upper arm devices included sphygmomanometers, semiautomated (manual compression and automatic measurement) upper arm oscillometric devices, and automated upper arm oscillometric devices. Facilities that selected one of these upper arm devices were considered to be adherent to the guideline. For the number of measurements performed to obtain average BP, we adopted “measuring twice or more at least 80% of the time” as the standard. Assessment of clothing status was restricted to facilities that used upper arm devices, under the assumption that clothing had less impact when other devices, such as wrist‐type devices, were used. This study was approved by the University of Tsukuba medical ethics board (Approval number 1036).
3. RESULTS
A total of 443 facilities (63.2%) responded to the questionnaire. The adherence ratio for measuring devices was 68.2%. Seventy‐five facilities (16.9%) used sphygmomanometers, 41 (9.3%) used semiautomated oscillometric devices, 232 (52.4%) used upper arm automated oscillometric devices, and 197 (44.5%) used wrist automated oscillometric devices (Table 1). The sum exceeds 443 because multiple answers were allowed.
Table 1.
Blood pressure measurement method used at 443 geriatric daycare rehabilitation and healthcare facilities in Japan
| Blood pressure measurement device used (multiple answers allowed) | N (%) |
|---|---|
| Sphygmomanometer | 75 (16.9) |
| Semiautomateda oscillometric device | 41 (9.3) |
| Oscillometric device (Upper arm) | 232 (52.4) |
| Oscillometric device (Wrist) | 197 (44.5) |
| Other | 10 (2.3) |
| Unknown | 1 (0.2) |
Device involving manual cuff pressurization and automatic measurement.
The adherence ratio for measurement frequency was 1.6%. The percentage of patient encounters at which BP was measured twice or more to obtain an average value was as follows: at least 80% of the time, seven facilities (1.6%); 50%‐80% of the time, 13 (2.9%) facilities; 20%‐50% of the time, 43 (9.7%) facilities; less than 20% of the time, 133 (30.0%) facilities; and rarely, 246 (55.5%) facilities.
The adherence ratio for resting time before measurements was 46.3%. The resting time among facilities was as follows: five minutes or more, 205 (46.3%) facilities; 3‐5 minutes, 176 (39.7%) facilities; 1‐3 minutes, 46 (10.4%) facilities; less than one minute, eight (1.8%) facilities; and no rest, seven (1.6%) facilities.
The adherence ratio for the approach to clothing was assessed in 302 facilities in which upper arm devices were used. The results are shown in Figure 2. The adherence ratio for the approach to thin shirt sleeves was 1.3%. Only four facilities (1.3%) asked patients to remove thin shirts prior to measurement, while 266 (88.1%) measured BP over thin shirt sleeves. The adherence ratio for the approach to thick clothing sleeves was 42.1%. One hundred twenty‐seven facilities (42.1%) asked patients to remove thick sweaters, 57 (18.9%) rolled up the sweater sleeve to the upper arm, and 78 (25.8%) measured BP over the sweater sleeve.
Figure 2.
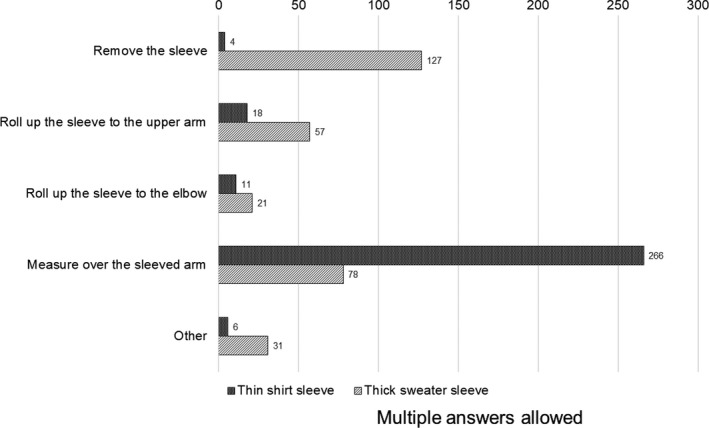
Method of blood pressure (BP) measurement involving clothes at 302 facilities using upper arm BP measurement devices
4. DISCUSSION
This is the first nationwide study in Japan to assess the adherence of long‐term care service providers to BP measurement guidelines. It showed that the guidelines were not necessarily followed, even though the facilities met certain national standards. Considering the time and personnel constraints at long‐term care facilities, we recommend both modification of the guidelines in these settings and improvement of BP measurement methods for accurate measurement within the range of feasibility. More convenient methods that still retain tolerable accuracy, such as one measurement per visit with values compared across visits, or removing thick clothing, may need to be proposed for these settings.
Approximately half of the facilities used wrist BP measurement devices, possibly because they do not require sleeve removal prior to measurement. However, upper arm devices should be recommended. Approximately two‐thirds of the facilities used upper arm BP measurement devices, indicating that use of these devices is sufficiently practical in these settings. Moreover, wrist devices, which have been reported to be inaccurate,11, 12 are not recommended by the guidelines.3 Guggiari and colleagues reported that relative to upper arm devices, validated wrist devices significantly underestimate BP in the elderly.13
Many facilities measured BP over clothing, but removal of thick clothing for measurements should be considered. In a previous study involving elderly people, we showed that systolic BP measured over a sweater sleeve was 3.8 ± 10.0 mm Hg higher than that measured on a bare arm.4 The difference was significant, and variations in BP measured over clothing seemed to increase with age. Moreover, BP measurements over thick sleeves had more variation in BP measurements compared to bare arm or over thin sleeves in frail elderly.14 Our finding that 42% of the facilities that used upper arm devices removed thick sweaters implies that removing such clothing is sometimes feasible. Considering the feasibility of removal of thick clothing and the effect of thick clothing on BP measurement results, we recommend that, as a standard of care, thick clothing should be removed as much as possible. On the other hand, thin shirt sleeves had much smaller difference from bare arm measurements compared to thick sleeves.14 Also, only 1.3% of the facilities that used upper arm devices removed thin sleeves when measuring BP. Due to the low likelihood of removal and relatively small effect on BP measurement results, it is not necessarily required to recommend removal of thin sleeves as a standard of care in these settings.
Most facilities did not compute an average BP value, but there is a possibility that the accuracy of BP measurements is complemented by other methods. BP is recommended to be measured 2‐3 times at each visit and the average recorded.3 We asked how often multiple measurements were performed, as it might be difficult for daycare rehabilitation services to measure participants’ BP multiple times for each assessment, given the participants’ various and frail conditions and time constraints on staff. Although they may not have performed multiple measurements on each occasion, some facilities commented that they reevaluate an individual's BP if the first measurement differed from the usual value or if the person's health status seemed out of the ordinary. These factors, along with the fact that BP was measured at each visit, may compensate for not performing multiple measurements during each visit.
Less than half of the facilities allowed patients to rest properly before measurements, which also may need to be compensated by reevaluating BP when the values are unusual. Providers should consider the possibility of overestimating BP with less resting time, as BP has been reported to continue decreasing for more than 10 minutes after resting begins.15 Given its feasibility and in accordance with the recommendation in the guideline,3 we recommend at least 5 minutes of rest before BP measurement.
Our results imply it might be difficult to accurately assess BP in elderly individuals in long‐term care facilities worldwide. This study was limited to geriatric health service facilities, which are regulated by national standards for staffing. The difficulty in assessing BP accurately in these relatively well‐organized facilities implies that accurate BP measurement in the elderly might also be difficult in other types of long‐term care facilities. The assessment of BP measurement methods in other long‐term care facilities may require further research.
This study has several limitations. To achieve a high response rate, we limited our questions to five items for which we expected adherence to guidelines to be difficult. We only asked the manager to complete the questionnaire, which may lead to positively biased results. We did not assess potential differences in adherence to guidelines by profession, or the time and setting of measurements. The question about frequency computing average measurements might have been confusing, given that it contained two questions. The definition of thin shirt sleeve and thick sweater sleeve was left to the judgment of the respondents. As there were no BP measurement guidelines for long‐term care service facilities, we adopted guidelines for office BP measurements. As the questionnaire focused on adherence to BP measurement guidelines, we did not ask about other possibly relevant factors such as basic knowledge concerning BP measurements. Further studies are needed to assess the difference in adherence by profession and predictors of noncompliance with BP measurement guidelines. In addition, the study was limited to geriatric health service facilities that provided daycare rehabilitation, which are regulated by national standards. If community‐based services had also been included, the BP measurement guideline adherence ratio would probably have been lower.
5. CONCLUSION
In long‐term care facilities in Japan, BP measurement guidelines were not always followed with regard to device type, number of measurements, and approach to thin‐sleeved clothing, with adherence rates of 68.2%, 1.6%, and 1.3%, respectively. We recommend using upper arm devices for BP measurement as recommended by guidelines. We also recommend modifying guidelines regarding removing thick clothing as much as possible and assessing measurements across visits instead of multiple measurements in succession in these types of facilities. Further study may be needed to refine these recommendations.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
ACKNOWLEDGEMENTS
This work was supported by the University of Tsukuba, and the project to develop leaders of next‐generation community medicine, funded by the Ministry of Education, Culture, Sports, Science and Technology.
Ozone S, Sato M, Takayashiki A, Sakamoto N, Yoshimoto H, Maeno T. Adherence to blood pressure measurement guidelines in long‐term care facilities: A cross sectional study. J Gen Fam Med. 2018;19:97–101. https://doi.org/10.1002/jgf2.162
REFERENCES
- 1. World Population Ageing 2015 [internet]. United nations; 2015. [cited 1 Jul 2017]. Available from: http://www.un.org/en/development/desa/population/theme/ageing/WPA2015.shtml.
- 2. Annual Report on the Aging Society: 2015 (Summary) [internet]. Cabinet Office; 2015. [cited 1 Jul 2017]. Available from: http://www8.cao.go.jp/kourei/english/annualreport/2015/2015pdf_e.html.
- 3. James PA, Oparil S, Carter BL, et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20. (supplementary material) [DOI] [PubMed] [Google Scholar]
- 4. Ozone S, Shaku F, Sato M, Takayashiki A, Tsutsumi M, Maeno T. Comparison of blood pressure measurements on the bare arm, over a sleeve and over a rolled‐up sleeve in the elderly. Fam Pract. 2016;33:517–22. [DOI] [PubMed] [Google Scholar]
- 5. Asai Y, Kawamoto R, Nago N, Kajii E. Blood pressure measurement by primary care physicians: comparison with the standard method. Japanese J Public Health. 2000;47:326–36. (Japanese) [PubMed] [Google Scholar]
- 6. Milot JP, Birnbaum L, Larochelle P, et al. Unreliability of home blood pressure measurement and the effect of a patient‐oriented intervention. Can J Cardiol. 2015;31:658–63. [DOI] [PubMed] [Google Scholar]
- 7. Holland M, Lewis PS. An audit and suggested guidelines for in‐patient blood pressure measurement. J Hypertens. 2014;32:2166–70; discussion 70. [DOI] [PubMed] [Google Scholar]
- 8. Survey of Institutions and Establishments for Long‐term Care, 2011 [internet]. Ministry of Health, Labour and Welfare; 2011. [cited 1 Jul 2017]. Available from: http://www.mhlw.go.jp/english/database/db-hss/siel-2011.html.
- 9. Japan Association of Geriatric Health Services Facilities (Japanese) [cited 30 April 2016]. Available from: http://www.roken.or.jp/.
- 10. Survey of Institutions and Establishments for Long‐term Care (Japanese), 2014. [internet]. Ministry of Health, Labour and Welfare; 2014 [cited 1 Jul 2017]. Available from: http://www.mhlw.go.jp/toukei/saikin/hw/kaigo/service14/index.html.
- 11. Latman NS, Latman A. Evaluation of instruments for noninvasive blood pressure monitoring of the wrist. Biomed Instrum Technol. 1997;31:63–8. [PubMed] [Google Scholar]
- 12. Stergiou GS, Christodoulakis GR, Nasothimiou EG, Giovas PP, Kalogeropoulos PG. Can validated wrist devices with position sensors replace arm devices for self‐home blood pressure monitoring? A randomized crossover trial using ambulatory monitoring as reference. Am J Hypertens. 2008;21:753–8. [DOI] [PubMed] [Google Scholar]
- 13. Guggiari C, Buela C, Iglesias K, Waeber B. Measurement with an automated oscillometric wrist device with position sensor leads to lower values than measurements obtained with an automated oscillometric arm device from the same manufacturer in elderly persons. Blood Press Monit. 2014;19:32–7. [DOI] [PubMed] [Google Scholar]
- 14. Ozone S, Sato M, Takayashiki A, et al. Blood pressure measurements over thin and thick sleeves in the frail elderly. Blood Press Monit. 2018;23:9–11. [DOI] [PubMed] [Google Scholar]
- 15. Sala C, Santin E, Rescaldani M, Magrini F. How long shall the patient rest before clinic blood pressure measurement? Am J Hypertens. 2006;19:713–7. [DOI] [PubMed] [Google Scholar]


