Abstract
Benign prostatic hyperplasia (BPH) commonly occurs among elderly males. The condition causes symptoms in the lower urinary tract, thereby reducing the quality of life. BPH includes 2 major treatments: medication and surgery. Surgical treatment is often the most effective and final intervention. Holmium laser enucleation of the prostate (HoLEP), one of the most efficient surgical procedures for BPH, is conducted transurethrally. During surgery, the most important and most difficult part is to locate the surgical capsule of the prostate, which is consistent to the idea of anatomic surgery. Different skills may be needed in treating different parts of the prostate. HoLEP tends to be efficient and safe with good hemostatic properties, and able to treat bladder calculus, which may be the complications of BPH. The technique is particularly suitable for prostate of varying volumes and sizes. Indeed, HoLEP also presents certain disadvantages, such as a long learning curve and costly equipment. Regardless, this method may be the "new standard" and the excellent method for the surgical treatment of BPH.
Keywords: Medicine, Issue 133, benign prostatic hyperplasia (BPH), holmium laser enucleation of the prostate (HoLEP), surgical treatment, lower urinary tract symptoms (LUTS), prostate, elderly male
Introduction
Benign prostatic hyperplasia (BPH), which is hyperplasia of the prostate gland, occurs in elderly males. This condition starts at approximately 40 y old, and morbidity can reach 50%-60% for men in their 60s and 80%-90% for men in their 70s and 80s1. BPH causes progressive obstruction, lower urinary tract symptoms, retention and its complications, and even renal failure, all of which lower the quality of life of the elderly male. After medical therapy, surgical treatment is often used as the most efficient treatment for symptomatic BPH.
Various types of surgery have been developed to treat the symptoms of BPH, including the first open prostatectomy introduced in 18942 and transurethral endoscopic surgery (TURP) a century later. Since its development, TURP has been regarded as the gold standard to surgically alleviate prostate enlargement.
The holmium laser operates at a wavelength of 2120 nm, which is similar to that of the tissue water3, which induces vaporization of water. Tissue penetration reaches 0.4 mm, and coagulation can also be operated with it. The process was first introduced for BPH in 19944. In 1998, Peter Gilling used the device to perform enucleation application5. As proposed by Peter Gilling et al. in the 1990s4, holmium laser enucleation of the prostate (HoLEP) is used to treat BPH by combining the two earlier types of surgery, including the open enucleation and the TURP4. With the development of the hyperplasia process, the prostatic peripheral zone is compassed by the transitional zone (TZ) to form a so-called surgical capsule. HoLEP allows the removal of the hyperplasic part of the prostate, the TZ, which separates the prostate capsule. Thus, HoLEP, as the anatomical surgery, can enucleate the enlarged prostate zone from the formed separation between TZ and capsule. Compared with the traditional surgical method, HoLEP may be safer, more efficient, and thorough with durable outcomes. Compared with TURP, holmium reduced the duration, irrigation time, and catheter time of the procedure and shortened hospital stay.6,7,8 The technique can also be performed safely on patients who are on anticoagulant therapy or with bleeding disorders9. Though there are different kinds of procedures for HoLEP, the main procedure is the same as mentioned in the following. We also introduce our own experiences and the innovation for this method in order to make it easier to accept and shorten the learning curve. The procedure is particularly suitable for large prostates and those combined with bladder stones, given that the holmium laser can also be used for lithotripsy8. This article introduces this technique and the detailed procedure.
Protocol
Ethical approval was obtained from the Ethics Committee of Shanghai Ninth People's Hospital and the written informed consent of each patient were obtained in our study.
1. Patients and Surgical Materials
Notes: Patients diagnosed with BPH and need surgical treatment in accordance with the European Association of Urology (EAU) guidelines can be included10. This surgical procedure requires experience and a long learning curve. The experience of the surgeon is one of the most important factors to accomplish this technique, specifically for prostate with a volume exceeding 100 g. The micro explosion effect of holmium laser is suitable for enucleation.
- Pre-surgical preparation
- Assess patients with BPH who require surgical treatment in accordance with the EAU guidelines10.
- Exclude those with the following conditions: severe urinary infection, severe pulmonary or heart disease, impairment of renal function, severe bleeding disorder, poor blood pressure control, neurogenic bladder dysfunction, bladder cancer, previous prostate surgery, prostate cancer, urethral stricture, and other surgical contraindications mentioned in our previous reports11.
- Perform preoperative evaluations and conduct certain perioperative treatment according to the results.
- Administer lumbar or general anesthesia to the patient and place the patient in the lithotomy position.
- Pre-surgical evaluation Notes: For the preoperative evaluation, perform the followings analyses including the regular surgery check: urinary flow dynamics analysis, prostatic ultrasound analysis, analysis of the prostate specific antigen (PSA) level and the urethroscopy analysis.
- Perform HoLEP using a 550 µm end-firing laser fiber and a 100 W Versa Pulse holmium laser, with power settings of 80-100 Wat 1.6-2 J/s and 40-50 Hz. Perform transurethral morcellation with a 26 F nephroscope using a mechanical morcellator. Use about 1 L of normal saline (0.9%) as the irrigation fluid.
2. Enucleation Procedures
Notes: Use plasma sterilization to sterilize the instruments and put the instruments in aseptic packages until used. Administer lumbar or general anesthesia to the patients and place the patient in the lithotomy position during surgery.
- Observation of the prostate and the urethra
- Insert continuous-flow cystoscope, ensuring minimal tissue damage and observing the prostate, the urethra, and the bladder carefully.
- Locate the ureteral orifices with the use of a visual obturator for a general assessment, including the median lobe volume and the amount of intravesical tissue.
- Identify the verumontanum which is one of the most important landmarks for enucleation. Insert the handpieces with a laser fiber connected to the laser machine with the power of the laser machine set to 80-100 W at 1.6-2 J per second and 40-50 Hz.
- Tunnel the incision around the 6 o'clock position of the prostate with the patients in the lithotomy position.
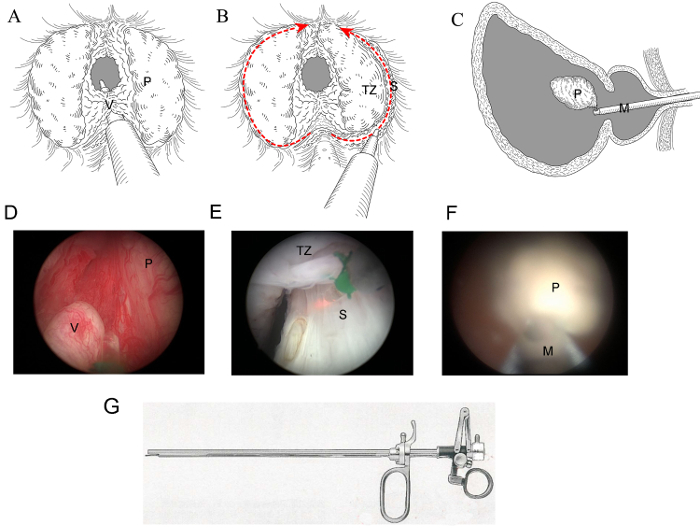
- Using a holmium laser, make a short horizontal incision around the 6 o'clock position in front of the verumontanum (as shown in Figure 1A) to locate the surgical capsule of the prostate.
- Expose the prostate surgical capsule from the verumontanum to the bladder neck. On the layer of the surgical capsule, create a tunnel from the apex toward the back of the bladder neck, as shown in Figure 1A and 1D.
- When the operation is close to the bladder neck, ensure that the mucosa and the muscle are protected to facilitate efficient urinary control.
- Lateral lobe removal Notes: The capsule is characterized by a smooth white tissue with sufficient blood vessels on the surface. Bleeding vessels can also be sealed off by using the laser with a bit further distance than that used in enucleated process (greater distance is suitable for hemostasis, while smaller distance is suitable for cutting). During the procedure, return to the prostatic apex without hesitation to ensure that the exact surgical capsule is located, which is helpful to avoid getting lost in the procedure, when the operator cannot find the clear view.
- First, enucleate the left lateral lobe from the 6 o'clock to the 12 o'clock position at the level of the surgical capsule and then enucleate the other lateral lobe similarly.
- During the procedure, use blur separation by using a scope sheath combined with laser cutting.
- Hang the enlarged prostate in the 12 o'clock position of the bladder neck without cutting down.
- Cut the tissue off from the bladder neck and push it into the bladder at the end of the enucleation procedure.
- Recheck the prostate capsule to ensure no active bleeding occurs. Remove all enlarged glands and stop the severe bleeding points (illustrated in Figure 1A-1F).
3. Morcellation
Notes: There are two gears in the morcellator, which can be shifted according to the foot pressure applied. The first gear uses light pressure to absorb tissue and water, whereas the second gear is used for morcellation. To prevent complications and improve the efficiency of the procedure, we have developed traditional morcellation skills and procedures. The approach to implement in this case is discussed in detail in our previous study12. The tissue taken out of the bladder is shown in Figure 2.

- Morcellation procedure
- Equip the morcellator and the match tube according to the morcellator instruction, regardless of the kind of morcellator used. Remove the prostate tissue from the bladder by using a morcellator efficiently.
- During the procedure, treat the bladder tissue with great caution13. Maintain sufficient irrigation water in the bladder to keep the bladder engorged, thus avoiding bladder injury and to keep the morcellator away from the bladder wall remaining within the bladder, for maximum protection the bladder wall.
- Finally, observe the general condition of the bladder and ensure that no reserved tissue is left in the bladder.
- Morcellation skills
- As reported in our earlier study12, prior to morcellation, evaluate the texture of the gland tissue.
- Dig holes by using laser to provide friction to the surface of the gland and thus obtain a smooth surface.
- Use the inverse technique to morcellate the large and firm tissues as well as fibrotic, spherical glands with smooth surfaces and firm tissues. During the process invert the morcellator for its opening to face downward in the bladder. Ensure that the circulating water is unobstructed, and constantly feel the bladder pressure during morcellation.
4. Post-operative Treatment
After surgery, insert the catheter and then irrigate normal saline into the bladder until the irrigation water is clear or only slightly reddish.
Remove the catheter until the urine becomes clear without gross hematuria.
If no obvious retention is observed and the patient can urinate without assistance after catheter removal, discharge the patient from the hospital14,15.
5. Follow-up Observation
After hospital discharge, examine the follow-up data of the patient for 1, 6, and 12 months, which include the international prostate symptom score (IPSS), over-active bladder scoring system (OABSS), quality of life (QoL), and Qmax. If post-operative complications occur, apply further treatment14.
Representative Results
Retrospective data, collected from 2015 to 2016, were obtained from the clinical database of our department. A total of 100 patients treated for BPH were enrolled in the study. Perioperative outcomes were included: operation time (OT), hemoglobin decrease after surgery, Na+ variation, hospital stay duration, bladder irrigation duration and following-up data. Basic patient characteristics were also collected during our study. In addition, the catheterization time and hospitalization time were noted. Follow-up data and post-operative urinary complications were collected at 1, 4 and 24 weeks after surgery. All data are shown in Table 1.
The prostate tissue can be removed from the bladder by morcellation, as shown in Figure 1C and 1F. Figure 2 shows the prostatic tissue after morcellation. The tissue can be analyzed pathologically after surgery. For prostate exceeding 120 g combined with multiple bladder calculi, making a small suprapubic incision is suggested to remove the enucleated prostate and stones from the bladder. This method can shorten the operating time and provide safety for some patients with poor general condition11.
Figure 1: Schematic of the process of HoLEP. (A, D) Tunnel should be made through the prostatic apex to the bladder neck in the 6 o'clock position. (B, E) Lateral lobes should be enucleated from 6 to 12 o'clock position. (C, F) The entire prostate should be pushed into the bladder for the following morcellation. (G) Sketch of the laser handpiece used in HoLEP. P: prostate tissue, V: verumontanum, TZ: transitional zone, S: surgical capsule, M: morcellator Please click here to view a larger version of this figure.
Figure 2 : Tissue harvested after enucleation and morcellation.
| Median (first quartile, third quartile) | Numbers | |
| Pre-surgical data | ||
| Age | 70.00 (64.00-66.00) | 100 |
| Prostate volume (ml) | 54.15 (35.80-70.03) | 100 |
| PSA (ng/ml) | 3.62 (1.64-7.28) | 94 |
| Pre-surgical IPSS | 23.00 (20.00-26.00) | 100 |
| Post-surgical data | ||
| Operation time | 75.00 (55.00-105.00) | 100 |
| Hemochrome decrease (gm/dl) | 1.20 (0.91-1.69) | 100 |
| Na+ changes (mmol/l) | 3.26 (2.11-4.33) | 100 |
| Hospital stay (day) | 4.00 (3.00-5.00) | 100 |
| Bladder irrigation time (hours) | 17.00 (12.00-29.00) | 83 |
| IPSS 1 week | 7.00 (2.75-8.25) | 54 |
| IPSS 4 weeks | 4.00 (0.00-6.00) | 47 |
| IPSS 24 weeks | 0.00 (0.00-5.00) | 47 |
| The sample median (first quartile, third quartile) is shown as the above. | ||
| IPSS= international prostate symptom score | ||
| PSA= prostate specific antigen |
Table 1: Perioperative data and pre-surgical characteristics of patients
Discussion
In this protocol, we introduce a procedure for the surgical treatment of BPH. HoLEP can be employed in daily clinical practice. As mentioned, the development of BPH surgery includes three landmarks. The first is the open surgery. Retropubic prostatectomy and suprapubic open prostatectomy have extensively been employed in the clinical setting for a long time. Despite this, the technique involves severe adverse side effects, which are often observed during the perioperative period. These side effects include hemorrhage, large scars after surgery, and slow patient recovery. Moreover, the operative field is limited to the pelvic cavity. The second significant period is the development of TURP along with the advances in endoscopic techniques, which is still regarded as the gold standard for the surgical treatment of BPH. However, TURP is still not considered an anatomical surgery, and it is difficult to find the surgical capsule to resect all the hyperplastic prostate tissue. The method is low-efficient for prostate resection because the tissue can only be cut down when the loop passes. Moreover, as the loop cuts tissues back and forth until the blood vessel is sealed, the vessels tend to open up repeatedly, causing bleeding during surgery. Thus, TURP is not suitable for extremely large prostate, particularly when the prostate exceeds 100 g. In the EAU guidelines, TURP is suggested if the prostate volume is less than 80 g16. On the basis of TURP, HoLEP was improved in the 1990s and continues to be important in the development of surgery for BPH4. Plasma kinetic resection of the Prostate (PKRP) and HoLEP data were compared in our prospective study in 20126. Obstructive symptoms are significantly improved compared with the preoperative examination. Patients who underwent HoLEP showed better efficiency and postoperative recovery results, compared with those who received TURP17.
Main complications include: urinary incontinence, urinary retention, hematuresis and urethral stricture18. Careful operative and preoperative assessment can prevent complications at some degree. In any case, treatments for complications are available. For post-surgical urinary incontinence, functional recovery training (such as Levator Ani Sports), medical treatment and pelvic muscle exercise can be used. Most patients with post-surgical urinary incontinence recover without surgery. For those with genuine stress incontinence, surgery may be the remedy. Post-surgical urinary retention can be caused by the poor function of the detrusor muscle. Thus, pre-operative assessment is important to discover these patients. Once this complication occurs, an indwelling catheter can help. Pipe clipping training and a muscarinic receptor agonist can also be used. Hematuresis can be caused by bleeding vessels of the prostate. Thus, for severe bleeding with clots, surgical hemostasis should be applied. For many, continuous bladder irrigation can sufficiently provide hemostasis. Urethral stricture can also occur in a small number of patients, which can be remedied by urethral dilatation. In case the procedure fails to address the problem, transurethral incision is suggested.
This method has certain limitations, including a long learning curve, high cost of the laser machine and noise19. However, HoLEP has been increasingly used in clinical practice to treat enlarged prostate. Urologists may vary in their skills, but the main technical process remains the same. For the prostate with three lobes, a tunnel can be made between the lateral lobe and the median lobe. This position is not exactly in the 6 o'clock but around 5 or 7 o'clock maybe. Regardless, the use of tunnel can still be a good choice for the surgeon as it provides convenience in performing enucleation. Holmium is pulsed solid-state laser with a wavelength of 2140 nm. Although numerous types of laser can be used in prostate surgery, holmium provides advantages, including the preservation of sexual function, efficiency, hemostasis, and lithotripsy. In our department, the skills required for enucleation and morcellation have improved. In our clinic report mentioned in the results section of this passage, as a flaw, no post-surgical PSA was recorded because of the loss to follow-up; otherwise, doctors are suggested to record post-surgical PSA for their clinical follow-up work. For the complications, one patients needed recatheterization because of urine retention after catheter removal. No transfusions were required. Stress incontinence to a certain degree was present in five patients after HoLEP, but these patients recovered within 6 months post-surgically. During follow-up, no patient required repeat surgery due to recurrence.
HoLEP is widely regarded as a suitable procedure for extremely large prostate. The method provides ease in locating the capsule, rendering it more efficient than other methods. HoLEP is more hemostatic and during enucleation the blood vessel could be opened only once at the bottom of the vessel. Compared with TURP, HoLEP is more thorough because the hyperplasic tissue can be separated anatomically. Long-term follow-up analysis indicates that the outcomes are considerable. As reported in a randomized trial in 2012, HoLEP is at least equivalent to TURP with respect to postoperative outcomes, such as erectile function, Qmax, and American Urological Association (AUA) scores in the long run (7 years), with fewer re-operations necessary20. Thus, owing to its efficiency and safety, HoLEP may become the good choice and an excellent surgical treatment for the surgical treatment of BPH.
Disclosures
This research was supported by Key Disciplines Group Construction Project of Pudong Health Bureau of Shanghai (PWZxq2014-11), Program for Outstanding Medical Academic Leader, and Special Construction of Integrated Traditional Chinese Medicine and Western Wedicine in Shanghai General Hospital (ZHYY-ZXYJHZX-1-03).
Acknowledgments
The authors have nothing to disclose.
References
- Bushman W. Etiology, epidemiology, and natural history of benign prostatic hyperplasia. Urol Clin North Am. 2009;36(4):403–415. doi: 10.1016/j.ucl.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Millin T. Retropubic prostatectomy; a new extravesical technique; report of 20 cases. Lancet. 1945;2(6380):693–696. doi: 10.1016/s0140-6736(45)91030-0. [DOI] [PubMed] [Google Scholar]
- Kahokehr AA, Gilling PJ. Which laser works best for benign prostatic hyperplasia? Curr Urol Rep. 2013;14(6):614–619. doi: 10.1007/s11934-013-0351-8. [DOI] [PubMed] [Google Scholar]
- Gilling PJ, Cass CB, Malcolm AR, Fraundorfer MR. Combination holmium and Nd:YAG laser ablation of the prostate: initial clinical experience. J Endourol. 1995;9(2):151–153. doi: 10.1089/end.1995.9.151. [DOI] [PubMed] [Google Scholar]
- Fraundorfer MR, Gilling PJ. Holmium:YAG laser enucleation of the prostate combined with mechanical morcellation: preliminary results. Eur Urol. 1998;33(1):69–72. doi: 10.1159/000019535. [DOI] [PubMed] [Google Scholar]
- Chen YB, et al. A prospective, randomized clinical trial comparing plasmakinetic resection of the prostate with holmium laser enucleation of the prostate based on a 2-year followup. J Urol. 2013;189(1):217–222. doi: 10.1016/j.juro.2012.08.087. [DOI] [PubMed] [Google Scholar]
- Kahokehr A, Gilling PJ. Enucleation techniques for benign prostate obstruction: which one and why? Curr Opin Urol. 2014;24(1):49–55. doi: 10.1097/MOU.0000000000000005. [DOI] [PubMed] [Google Scholar]
- Kuntz RM, Lehrich K. Transurethral holmium laser enucleation versus transvesical open enucleation for prostate adenoma greater than 100 gm.:: a randomized prospective trial of 120 patients. J Urol. 2002;168(4 Pt 1):1465–1469. doi: 10.1016/S0022-5347(05)64475-8. [DOI] [PubMed] [Google Scholar]
- Elzayat E, Habib E, Elhilali M. Holmium laser enucleation of the prostate in patients on anticoagulant therapy or with bleeding disorders. J Urol. 2006;175(4):1428–1432. doi: 10.1016/S0022-5347(05)00645-2. [DOI] [PubMed] [Google Scholar]
- Oelke M, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013;64(1):118–140. doi: 10.1016/j.eururo.2013.03.004. [DOI] [PubMed] [Google Scholar]
- Xu H, et al. Efficacy and safety of an improved technique of holmium laser enucleation of the prostate versus open prostatectomy in treating enlarged prostates combined with multiple bladder stones: one-year of followup. Int J Clin Exp Med. 2016;9(12):23612–23617. [Google Scholar]
- Chen Q, et al. An improved morcellation procedure for holmium laser enucleation of the prostate. J Endourol. 2012;26(12):1625–1628. doi: 10.1089/end.2012.0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Tayeb MM, Borofsky MS, Paonessa JE, Lingeman JE. Wolf Piranha Versus Lumenis Versacut Prostate Morcellation Devices: A Prospective Randomized Trial. J Urol. 2015. [DOI] [PubMed]
- Gilling PJ, Aho TF, Frampton CM, King CJ, Fraundorfer MR. Holmium laser enucleation of the prostate: results at 6 years. Eur Urol. 2008;53(4):744–749. doi: 10.1016/j.eururo.2007.04.052. [DOI] [PubMed] [Google Scholar]
- Shah HN, et al. Prospective evaluation of the learning curve for holmium laser enucleation of the prostate. J Urol. 2007;177(4):1468–1474. doi: 10.1016/j.juro.2006.11.091. [DOI] [PubMed] [Google Scholar]
- Gratzke C, et al. EAU Guidelines on the Assessment of Non-neurogenic Male Lower Urinary Tract Symptoms including Benign Prostatic Obstruction. Eur Urol. 2015;67(6):1099–1109. doi: 10.1016/j.eururo.2014.12.038. [DOI] [PubMed] [Google Scholar]
- Vincent MW, Gilling PJ. HoLEP has come of age. World J Urol. 2015;33(4):487–493. doi: 10.1007/s00345-014-1443-x. [DOI] [PubMed] [Google Scholar]
- Qian X, et al. Functional outcomes and complications following B-TURP versus HoLEP for the treatment of benign prostatic hyperplasia: a review of the literature and Meta-analysis. Aging Male. 2017;20(3):184–191. doi: 10.1080/13685538.2017.1295436. [DOI] [PubMed] [Google Scholar]
- Xu H, Chen YB, Gu M, Chen Q, Wang Z. Evaluation of noise hazard during the holmium laser enucleation of prostate. BMC Urol. 2017;17(1):71. doi: 10.1186/s12894-017-0246-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilling PJ, et al. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: results at 7 years. BJU Int. 2012;109(3):408–411. doi: 10.1111/j.1464-410X.2011.10359.x. [DOI] [PubMed] [Google Scholar]


